Volume 11, Issue 6 (Nov & Dec 2021)
J Research Health 2021, 11(6): 365-374 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bagheri Sheykhangafshe F, Hajialiani V, Hasani J. The Role of Resilience and Emotion Regulation in Psychological Distress of Hospital Staff During the COVID-19 Pandemic: A Systematic Review Study. J Research Health 2021; 11 (6) :365-374
URL: http://jrh.gmu.ac.ir/article-1-1984-en.html
URL: http://jrh.gmu.ac.ir/article-1-1984-en.html
1- Department of Psychology, Faculty of Humanities, Tarbiat Modares University, Tehran, Iran.
2- Department of Clinical Psychology, Faculty of Psychology and Educational Sciences, Kharazmi University, Tehran, Iran.
3- Department of Clinical Psychology, Faculty of Psychology and Educational Sciences, Kharazmi University, Tehran, Iran. ,hasanimehr57@khu.ac.ir
2- Department of Clinical Psychology, Faculty of Psychology and Educational Sciences, Kharazmi University, Tehran, Iran.
3- Department of Clinical Psychology, Faculty of Psychology and Educational Sciences, Kharazmi University, Tehran, Iran. ,
Full-Text [PDF 791 kb]
(1244 Downloads)
| Abstract (HTML) (3192 Views)
Full-Text: (2722 Views)
1. Introduction
Coronaviruses are single-stranded ribonucleic acid viruses belonging to the coronavirus family. Although primarily known as enzootic infections, they have evolved over the past few decades to infect humans [1]. The severity of coronavirus diseases ranges from the common cold to more serious illnesses, such as acute respiratory syndrome and the Middle East respiratory syndrome. The coronavirus 2019 first broke out on December 17, 2019, in Wuhan, China, and the World Health Organization declared it a pandemic on March 11, 2020 [2]. During the outbreak of COVID-19, the medical staff of hospitals was under a lot of pressure because of the heavy workload and dangerous work environment [3]. Harsh conditions can cause mental health problems, such as anxiety and depression. These problems affect the attention span, comprehension, and decision-making ability of the staff, which may impede their ability to treat patients with COVID-19. These mental problems may also have long-term effects on their physical and psychological health [4].
After facing natural disasters and unexpected events, medical staff usually demonstrate different psychological reactions [5]. During the COVID-19 outbreak, hospital staff worked around the clock, had no definitive treatment for the disease, and faced challenges they had not experienced before. For this reason, they may suffer from various mental injuries [6]. High workload, night shifts, lack of equipment, lack of familiarity and training in the face of disasters that kill the people who may not have normally passed away, the fear of being infected with COVID-19 and passing it on to family and relatives, witnessing the death of patients and prolonged separation from family can lead to psychological distress and increase the risk of posttraumatic stress in hospital staff [7, 8]. Psychological distress is used to describe a condition in which a person becomes emotionally disturbed and loses his or her normal functioning levels. These conditions are usually characterized by symptoms of stress, anxiety, and depression [9]. Numerous factors, such as underlying disease, gender, age, and low education, can predict psychological distress in turbulent and stressful situations [10]. The prevalence of COVID-19, as well as strict measures and rules to control it, have caused changes in the lifestyle, social and occupational interactions of hospital staff, which increase the personnel’s psychological distress [7]. Similarly, Elbay et al. [11], in a study on the medical staff of Turkish hospitals during the outbreak of COVID-19, concluded that 64% of the symptoms of the staff were depression, 51% anxiety, and 42% stress. Also, the findings of this study indicate a high correlation of female gender, low work experience, and being single with higher psychological distress in the medical staff.
In contrast, some studies have also reported that various interpersonal factors, such as resilience and emotion regulation, promote the mental health of medical staff during the COVID-19 pandemic [12, 13]. Hospital staff uses different coping strategies in facing shocking, destructive, and stressful events [14]. Some people respond to stressful situations by giving in to psychological disorders, such as anxiety and depression, while others quickly adjust to the situation and resume their normal lives. This ability, which improves the mental state of individuals, is known in the positive psychological approach as resilience [15].
Resilience is the process of optimal adaptation in the face of difficulties, traumatic events, calamities, threats, or any tense situation. Resilient people return to an average level of performance after facing difficult life situations. Resilient people readily accept the realities of life and believe that life is meaningful [16]. Resilience refers to an individual’s practical ability to adapt or cope with adverse conditions. This virtue may help maintain a person’s mental health during a deadly pandemic [17]. The concept of resilience among the medical staff of hospitals facing natural disasters has drawn the attention of many researchers [18]. During the COVID-19 pandemic, resilience was also found to improve mental health [19] and reduce anxiety, stress, and burnout in hospital staff [20].
In this regard, Tam et al. [4] investigated the psychological distress of the medical staff during the COVID-19 outbreak with the mediating role of resilience. According to results, 38% of medical staff had psychological distress. But, people who received adequate social support and were highly resilient experienced less stress, depression, and anxiety. In another study, Luceño-Moreno et al. [8] examined posttraumatic stress, anxiety, depression, resilience, and burnout during the COVID-19 pandemic. In total, 56.6% reported posttraumatic stress symptoms, 58.6% anxiety, 46% depression, and 41.1% burnout.
In contrast, people with good levels of resilience reported fewer psychological problems. Being a woman and working in the COVID-19 ward increase in psychological distress in the medical staff of hospitals. Sinichi et al. [21] also showed that nurses suffer from many psychological problems. Symptoms of stress were observed in 48.7%, anxiety in 77.6%, and depression in 60.5% of nurses. The most important strategy used in them was the emotion-focused type. There was a positive correlation between psychological disorders and emotion-based approaches, as well as a negative correlation between problem-based skills and the incidence of depression.
The ability to regulate emotion is critical to effective and successful performance in difficult and stressful situations, such as the COVID-19 pandemic [22]. Researchers have identified various cognitive and behavioral strategies for regulating emotions that can generally be divided into adaptive and incompatible strategies [23, 24].
Strategies such as acceptance, cognitive reassessment, and positively refocusing on planning or focusing on finding a solution to a problem are typically considered adaptive strategies, leading to reduced emotion and negative feelings [23]. In contrast, repression of emotions, self-blame, rumination, and catastrophizing are recognized as maladaptive emotion regulation strategies that exacerbate and prolong negative emotions [24]. In the COVID-19 pandemic, emotion regulation strategies also play an important role in treating depression, anxiety, and stress in medical staff [13]. Investigations conducted during the outbreak of COVID-19 have shown that people with self-blame, rumination, and rejection experience high levels of anxiety and depression [25, 26]. In contrast, therapeutic staff who used adaptive cognitive-emotional regulation, such as positive reassessment and refocused on positive planning, had better mental and physical health [27]. In a similar study, Wang et al. [28]examined anxiety, depression, and cognitive emotion regulation in nurses during the COVID-19 outbreak. This study showed that 27.6% and 32.8% of nurses have symptoms of anxiety and depression, respectively. Also, low self-blame, lack of rumination, and positive acceptance decreased anxiety and depression in nurses. In another study, Zhu et al. [29] examined nurses’ mental health and emotion regulation strategies during the COVID-19 outbreak. The results showed that 55% had anxiety, and 56.4% had depression. Also, 31.6% reported simultaneous symptoms of anxiety and depression. Nurses who used negative emotion regulation strategies had lower mental health. Safa et al. [30] also reported that a significant number of nurses had severe posttraumatic stress. There was a significant difference between different age groups in terms of the depression absence scale and between individuals with different marital statuses in terms of pervasive memories subscales and inability to control emotions and total posttraumatic stress score. Because the medical staff of the hospitals was at risk of developing COVID-19 from the very first days, they suffered from extensive psychological damage, such as posttraumatic stress, anxiety, depression, burnout, and insomnia. If these problems are not taken into account, they may create irreparable consequences for these people [31, 32]. On the other hand, more than a year after the outbreak of COVID-19, we are still witnessing the mutation of this deadly virus on a global scale, and a definite date for the post-corona era is inconceivable [33, 34]. Thus, it is necessary to seek solutions to improve the mental health of hospital nurses and doctors. For this purpose, the present review study was conducted to investigate the role of resilience and emotion regulation in the psychological distress of medical staff during the COVID-19 pandemic.
2. Methods
The present study is a systematic review study that, through PRISMA (The Preferred Reporting Items for Systematic Reviews and Meta-Analysis) [35] model, examined the research findings related to the role of resilience and emotion regulation on the psychological distress of the medical staff of hospitals during the COVID-19 pandemic. In the present study, using the keywords of “coronavirus 2019”, “COVID-19”, “depression”, “anxiety”, “stress”, “resilience”, “emotion regulation”, “mental health”, “medical staff”, and “psychological distress”, we searched in English databases of Google Scholar, PubMed, Scopus, ScienceDirect, as well as Iranian databases of Scientific Information Database (SID) of Jahad Daneshgahi, Iranian Publications (Magiran) and Iranian Medical Sciences articles from February 2020 to July 2021. After collecting the articles, irrelevant and duplicate papers were removed by the researchers. In the next step, the full texts of the remaining articles were examined, and after removing the irrelevant items, the remaining articles were categorized and analyzed. Research articles were selected based on the inclusion criteria (relevance to the purpose of the research, having a structured research framework and publication in a valid journal) and exclusion criteria (unavailability of full text of the article, letter to the editor, and no abstract). The quality of articles was evaluated using the Gifford et al. criteria [36]. Based on the criteria provided for quantitative (6 criteria), qualitative (11 criteria), quasi-experimental (8 criteria), and experimental (7 criteria) studies, the articles were evaluated on a 2-point scale (0 and 1). Out of 593 articles related to the role of resilience and emotion regulation in the psychological distress of hospital staff during the COVID-19 pandemic, 30 completely related articles were included in the study. Then, they were studied thoroughly and accurately (Figure 1). 3. Results
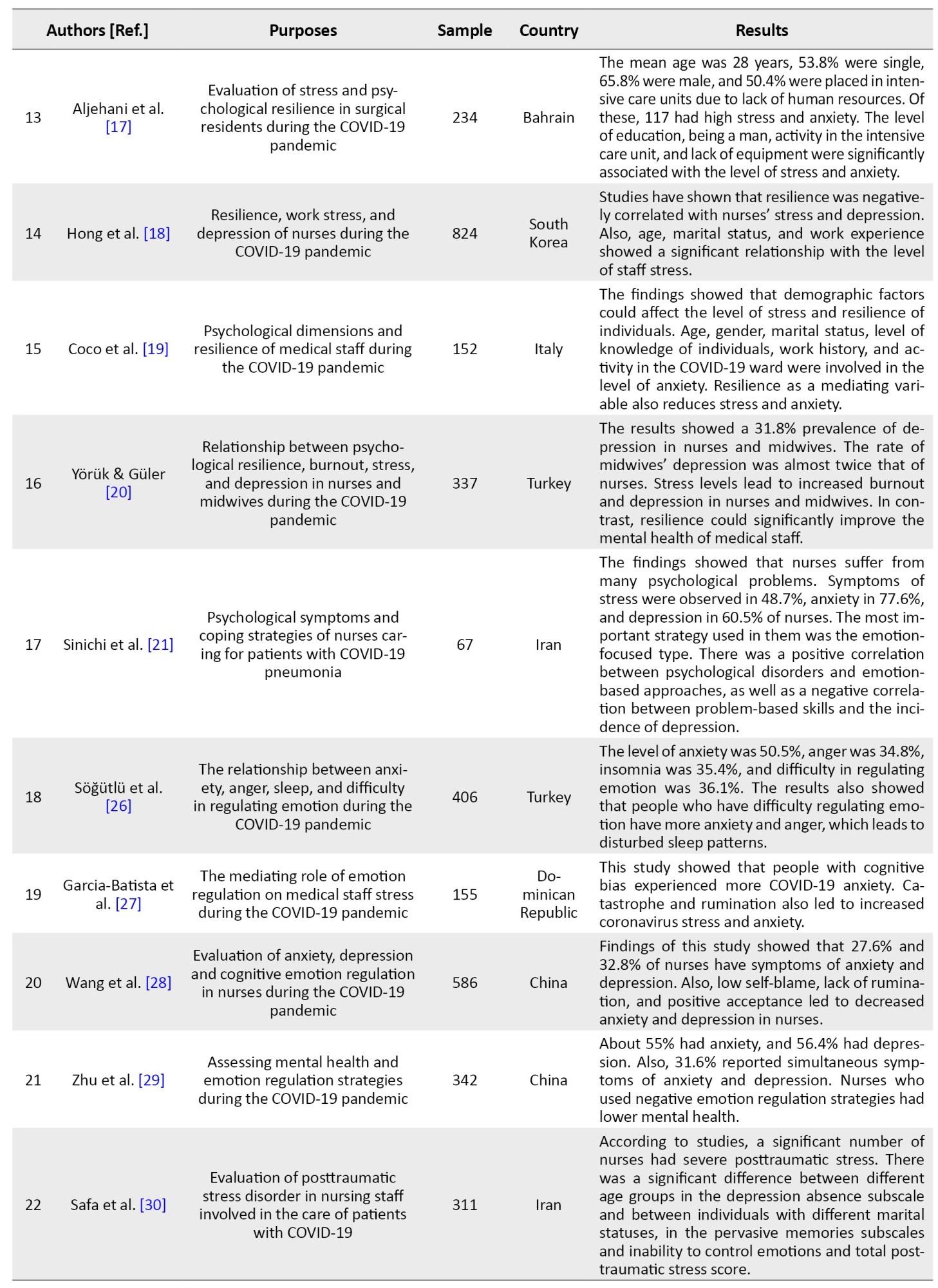
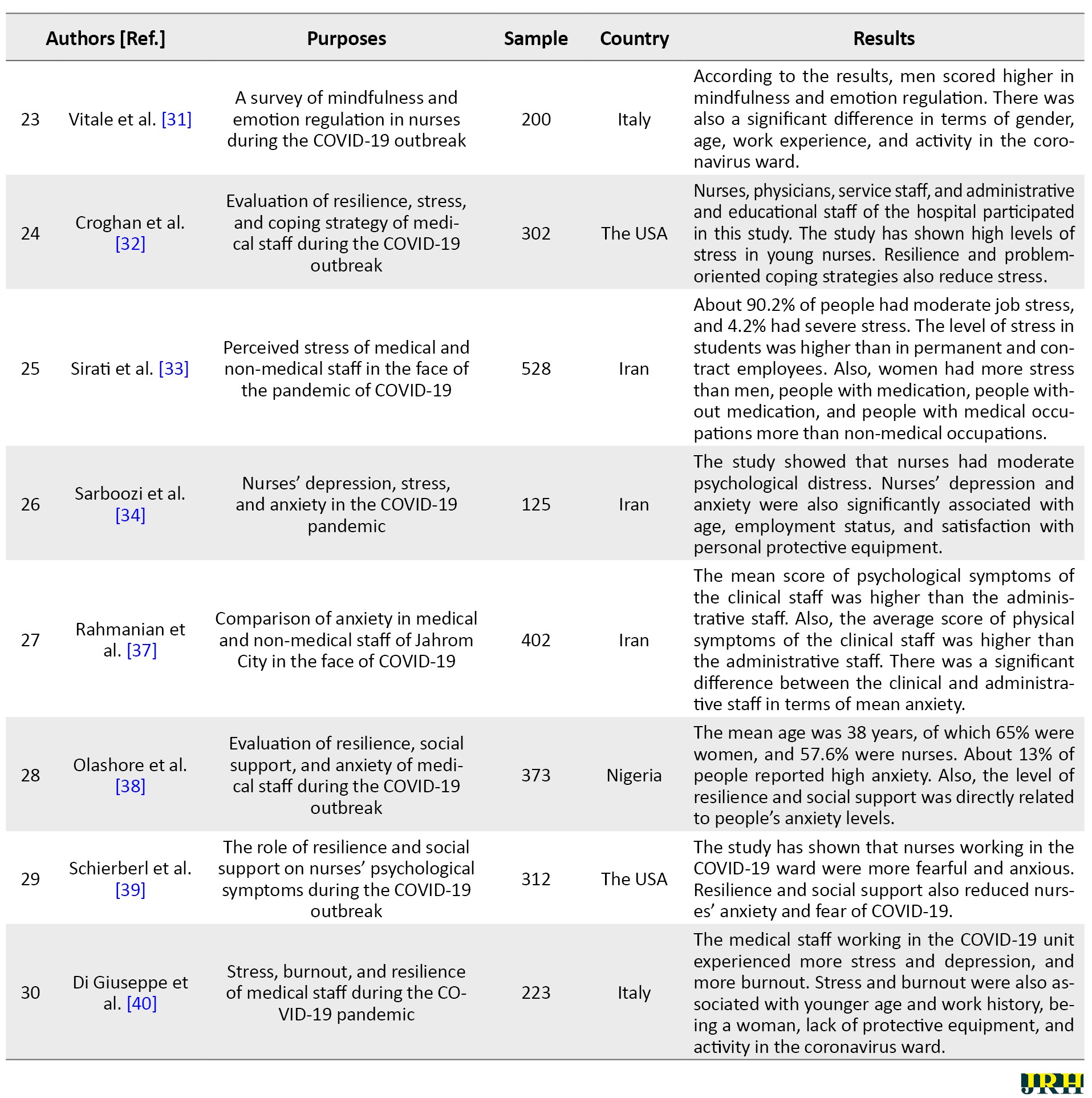
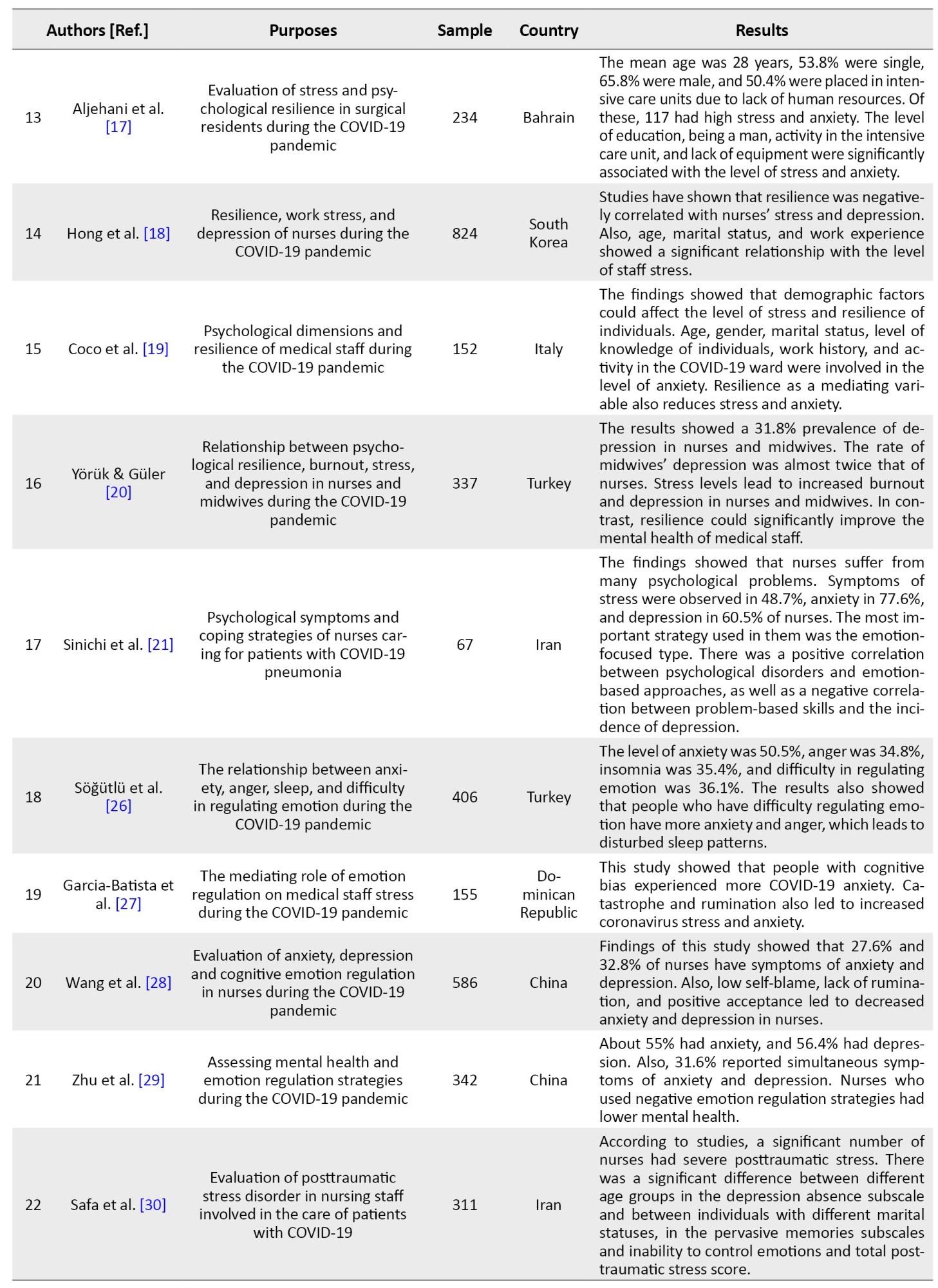
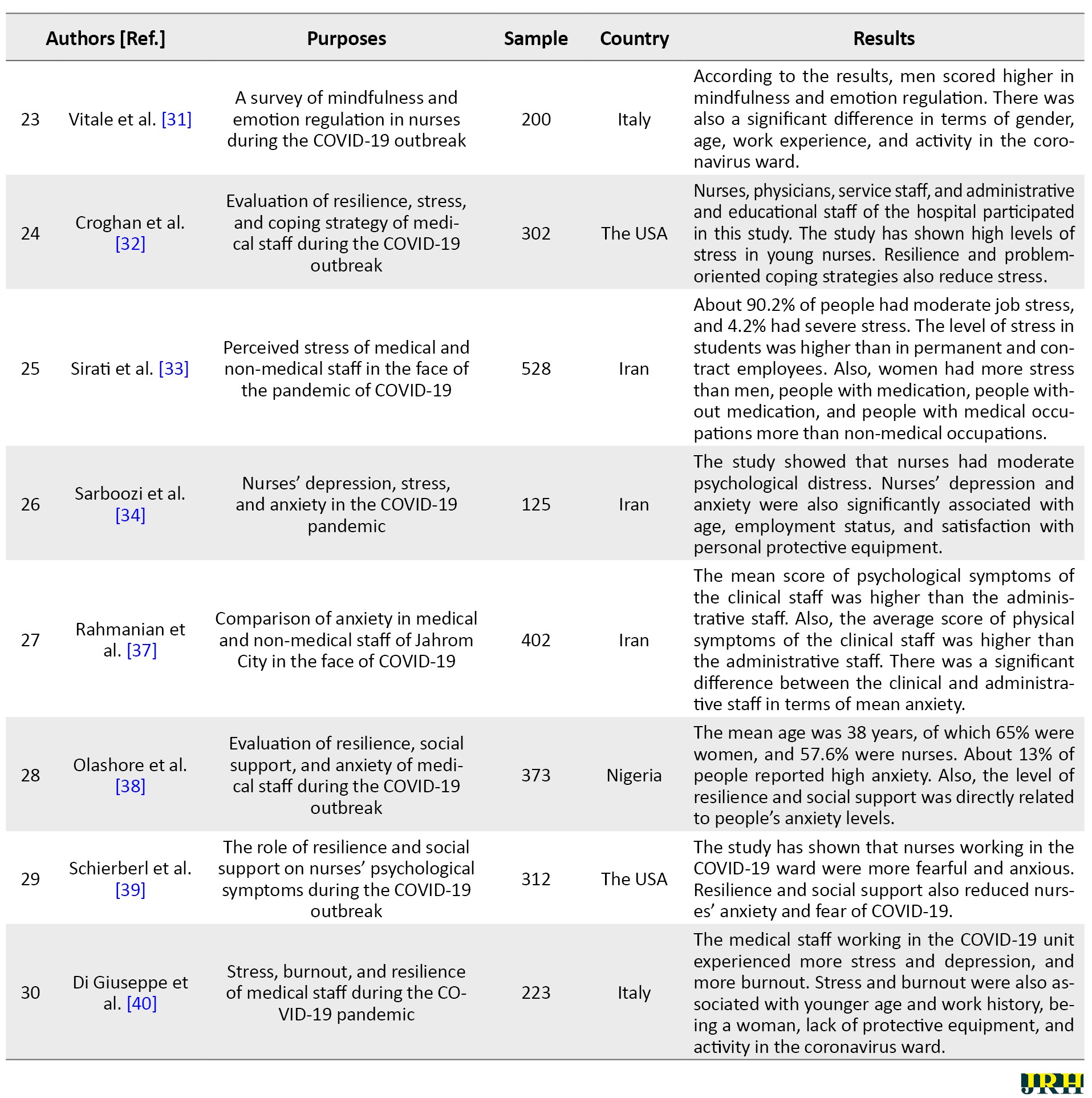
In this study, 30 qualified research articles in Persian and English were reviewed. Table 1 presents the findings from the reviewed articles on the role of resilience and emotion regulation in the psychological distress of hospital staff during the COVID-19 pandemic.

Out of 593 articles related to the role of resilience and emotion regulation in the psychological distress of hospital staff during the COVID-19 pandemic, 30 articles with a total of 13902 samples were selected and reviewed based on the inclusion and exclusion criteria. The studies were collected from 16 countries: Iran, Italy, the Dominican Republic, China, Romania, Turkey, the United States, Nigeria, South Korea, Bahrain, Serbia, Indonesia, the United Kingdom, Portugal, Oman, and Spain. Of the 30 articles reviewed, 24 were quantitative articles, and one was a review article. Also, 36.6% and 63.4% of articles were published in 2020 and 2021, respectively.
Studies have shown that resilience and emotion regulation strategies during the outbreak of COVID-19 had positive effects on nurses, physicians, hospital staff, and medical students. Most studies have shown that good resilience and the use of adaptive emotion regulation strategies can reduce anxiety, depression, insomnia, fear, and rumination, which results in increased well-being and psychological health of hospital staff during the COVID-19 pandemic.
4. Discussion
This study aimed to investigate the role of resilience and emotion regulation in the psychological distress of hospital staff during the COVID-19 pandemic. The present study results showed that medical staff with high resilience performed better in the face of COVID-19 stress and anxiety and had good mental health [6, 7, 8, 9, 10].
In explaining these findings, it can be acknowledged that coping strategies help hospital staff when they face stressful and anxious issues, such as the outbreak of COVID-19 and the high volume of hospitalized patients, positive behaviors are not observed. show good coping styles and have more flexibility [4]. This ability helps nurses and physicians to accept existing conditions and perform at their best [8]. In contrast, low resilience leads to anxiety, stress, and burnout in hospital staff, result in reduced efficiency of services provided by hospital staff. Because resilience includes positive patterns of adaptation to hardships and difficulties over time, nurses and physicians with good resilience are expected to show better flexibility over time [12]. In other words, people with good resilience endure hardships, cope better with threatening situations, cope more effectively with stress and problems, and have a greater capacity to respond to life stressors and cope with everyday problems [17]. This ability causes hospital staff to adapt better to the anxious conditions (such as hospital overcrowding, equipment shortages, and medication) created by the COVID-19 pandemic [3]. In other words, the dimensions of resilience, such as personal competence, trust in instincts, positive acceptance of change, self-confidence, control, and spiritual impact when in stressful and difficult situations, help people to show the necessary flexibility, adapt to the current situation and use effective coping strategies better [14, 15, 16, 17, 18, 19, 20].
On the other hand, the findings showed that medical staff who used adaptive emotion regulation strategies, such as positive reassessment and refocusing on planning, positively coped with COVID-19 anxiety and stress. In contrast, the use of maladaptive emotion regulation strategies, such as catastrophe, rumination, and blaming others, negatively aggravates psychological disorders during the coronavirus 2019 pandemic.
Explaining these findings, it can be acknowledged that people who manage and control their emotions during the COVID-19 outbreak have better mental health. When a person is faced with an emotional situation, feeling good and optimistic is not enough to control the emotion, but he needs to have the best cognitive function in these situations. In regulating emotion, an optimal interaction of cognition and emotion is required to deal with adverse conditions because people interpret every stimulus and situation they encounter, and cognitive interpretations determine people’s reactions [29]. For this reason, people who use negative and weak cognitive styles, such as rumination, catastrophizing, and self-blame during the COVID-19 pandemic are more vulnerable to emotional problems than others [27]. In other words, people who could not properly manage their emotions in the face of stress caused by COVID-19 show more stress, depression, and anxiety. When people with high anxiety symptoms have more difficulty regulating their emotional functions, they are less able to recognize and accept their emotions and are more likely to show negative emotions in ambiguous emotional situations [26, 27, 28, 29, 30, 31].
5. Conclusion
The present study results showed that resilience and emotion regulation play an important role in reducing depression, anxiety, and stress of hospital staff during the COVID-19 pandemic. People with high resilience are well aware of the situation and do their best to accept it and show their best performance. Emotion regulation also allows nurses and physicians to manage and control their emotions. This strategy prevents them from engaging in negative emotions and helps them show their best performance. In this regard, it is suggested to use appropriate psychological services in hospitals to promote the mental health of nurses and physicians.
One of the limitations of the present review study is the unavailability of the full text of some articles, which led to the non-inclusion of these articles in the review process. Also, due to the filtering of some scientific databases, researchers could not access them. In addition, some studies were descriptive and should be cautious in generalizing their results. In this regard, it is suggested that descriptive studies be conducted on the role of resilience and emotion regulation in promoting the mental health of nurses and medical staff of hospitals during the COVID-19 outbreak in the country. These studies improve the physical and psychological function of medical staff in Iran.
Ethical Considerations
Compliance with ethical guidelines
Ethical principles in writing the article have been observed according to the instructions of the National Ethics Committee and the COPE regulations.
Funding
The present study was self-funded.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
Coronaviruses are single-stranded ribonucleic acid viruses belonging to the coronavirus family. Although primarily known as enzootic infections, they have evolved over the past few decades to infect humans [1]. The severity of coronavirus diseases ranges from the common cold to more serious illnesses, such as acute respiratory syndrome and the Middle East respiratory syndrome. The coronavirus 2019 first broke out on December 17, 2019, in Wuhan, China, and the World Health Organization declared it a pandemic on March 11, 2020 [2]. During the outbreak of COVID-19, the medical staff of hospitals was under a lot of pressure because of the heavy workload and dangerous work environment [3]. Harsh conditions can cause mental health problems, such as anxiety and depression. These problems affect the attention span, comprehension, and decision-making ability of the staff, which may impede their ability to treat patients with COVID-19. These mental problems may also have long-term effects on their physical and psychological health [4].
After facing natural disasters and unexpected events, medical staff usually demonstrate different psychological reactions [5]. During the COVID-19 outbreak, hospital staff worked around the clock, had no definitive treatment for the disease, and faced challenges they had not experienced before. For this reason, they may suffer from various mental injuries [6]. High workload, night shifts, lack of equipment, lack of familiarity and training in the face of disasters that kill the people who may not have normally passed away, the fear of being infected with COVID-19 and passing it on to family and relatives, witnessing the death of patients and prolonged separation from family can lead to psychological distress and increase the risk of posttraumatic stress in hospital staff [7, 8]. Psychological distress is used to describe a condition in which a person becomes emotionally disturbed and loses his or her normal functioning levels. These conditions are usually characterized by symptoms of stress, anxiety, and depression [9]. Numerous factors, such as underlying disease, gender, age, and low education, can predict psychological distress in turbulent and stressful situations [10]. The prevalence of COVID-19, as well as strict measures and rules to control it, have caused changes in the lifestyle, social and occupational interactions of hospital staff, which increase the personnel’s psychological distress [7]. Similarly, Elbay et al. [11], in a study on the medical staff of Turkish hospitals during the outbreak of COVID-19, concluded that 64% of the symptoms of the staff were depression, 51% anxiety, and 42% stress. Also, the findings of this study indicate a high correlation of female gender, low work experience, and being single with higher psychological distress in the medical staff.
In contrast, some studies have also reported that various interpersonal factors, such as resilience and emotion regulation, promote the mental health of medical staff during the COVID-19 pandemic [12, 13]. Hospital staff uses different coping strategies in facing shocking, destructive, and stressful events [14]. Some people respond to stressful situations by giving in to psychological disorders, such as anxiety and depression, while others quickly adjust to the situation and resume their normal lives. This ability, which improves the mental state of individuals, is known in the positive psychological approach as resilience [15].
Resilience is the process of optimal adaptation in the face of difficulties, traumatic events, calamities, threats, or any tense situation. Resilient people return to an average level of performance after facing difficult life situations. Resilient people readily accept the realities of life and believe that life is meaningful [16]. Resilience refers to an individual’s practical ability to adapt or cope with adverse conditions. This virtue may help maintain a person’s mental health during a deadly pandemic [17]. The concept of resilience among the medical staff of hospitals facing natural disasters has drawn the attention of many researchers [18]. During the COVID-19 pandemic, resilience was also found to improve mental health [19] and reduce anxiety, stress, and burnout in hospital staff [20].
In this regard, Tam et al. [4] investigated the psychological distress of the medical staff during the COVID-19 outbreak with the mediating role of resilience. According to results, 38% of medical staff had psychological distress. But, people who received adequate social support and were highly resilient experienced less stress, depression, and anxiety. In another study, Luceño-Moreno et al. [8] examined posttraumatic stress, anxiety, depression, resilience, and burnout during the COVID-19 pandemic. In total, 56.6% reported posttraumatic stress symptoms, 58.6% anxiety, 46% depression, and 41.1% burnout.
In contrast, people with good levels of resilience reported fewer psychological problems. Being a woman and working in the COVID-19 ward increase in psychological distress in the medical staff of hospitals. Sinichi et al. [21] also showed that nurses suffer from many psychological problems. Symptoms of stress were observed in 48.7%, anxiety in 77.6%, and depression in 60.5% of nurses. The most important strategy used in them was the emotion-focused type. There was a positive correlation between psychological disorders and emotion-based approaches, as well as a negative correlation between problem-based skills and the incidence of depression.
The ability to regulate emotion is critical to effective and successful performance in difficult and stressful situations, such as the COVID-19 pandemic [22]. Researchers have identified various cognitive and behavioral strategies for regulating emotions that can generally be divided into adaptive and incompatible strategies [23, 24].
Strategies such as acceptance, cognitive reassessment, and positively refocusing on planning or focusing on finding a solution to a problem are typically considered adaptive strategies, leading to reduced emotion and negative feelings [23]. In contrast, repression of emotions, self-blame, rumination, and catastrophizing are recognized as maladaptive emotion regulation strategies that exacerbate and prolong negative emotions [24]. In the COVID-19 pandemic, emotion regulation strategies also play an important role in treating depression, anxiety, and stress in medical staff [13]. Investigations conducted during the outbreak of COVID-19 have shown that people with self-blame, rumination, and rejection experience high levels of anxiety and depression [25, 26]. In contrast, therapeutic staff who used adaptive cognitive-emotional regulation, such as positive reassessment and refocused on positive planning, had better mental and physical health [27]. In a similar study, Wang et al. [28]examined anxiety, depression, and cognitive emotion regulation in nurses during the COVID-19 outbreak. This study showed that 27.6% and 32.8% of nurses have symptoms of anxiety and depression, respectively. Also, low self-blame, lack of rumination, and positive acceptance decreased anxiety and depression in nurses. In another study, Zhu et al. [29] examined nurses’ mental health and emotion regulation strategies during the COVID-19 outbreak. The results showed that 55% had anxiety, and 56.4% had depression. Also, 31.6% reported simultaneous symptoms of anxiety and depression. Nurses who used negative emotion regulation strategies had lower mental health. Safa et al. [30] also reported that a significant number of nurses had severe posttraumatic stress. There was a significant difference between different age groups in terms of the depression absence scale and between individuals with different marital statuses in terms of pervasive memories subscales and inability to control emotions and total posttraumatic stress score. Because the medical staff of the hospitals was at risk of developing COVID-19 from the very first days, they suffered from extensive psychological damage, such as posttraumatic stress, anxiety, depression, burnout, and insomnia. If these problems are not taken into account, they may create irreparable consequences for these people [31, 32]. On the other hand, more than a year after the outbreak of COVID-19, we are still witnessing the mutation of this deadly virus on a global scale, and a definite date for the post-corona era is inconceivable [33, 34]. Thus, it is necessary to seek solutions to improve the mental health of hospital nurses and doctors. For this purpose, the present review study was conducted to investigate the role of resilience and emotion regulation in the psychological distress of medical staff during the COVID-19 pandemic.
2. Methods
The present study is a systematic review study that, through PRISMA (The Preferred Reporting Items for Systematic Reviews and Meta-Analysis) [35] model, examined the research findings related to the role of resilience and emotion regulation on the psychological distress of the medical staff of hospitals during the COVID-19 pandemic. In the present study, using the keywords of “coronavirus 2019”, “COVID-19”, “depression”, “anxiety”, “stress”, “resilience”, “emotion regulation”, “mental health”, “medical staff”, and “psychological distress”, we searched in English databases of Google Scholar, PubMed, Scopus, ScienceDirect, as well as Iranian databases of Scientific Information Database (SID) of Jahad Daneshgahi, Iranian Publications (Magiran) and Iranian Medical Sciences articles from February 2020 to July 2021. After collecting the articles, irrelevant and duplicate papers were removed by the researchers. In the next step, the full texts of the remaining articles were examined, and after removing the irrelevant items, the remaining articles were categorized and analyzed. Research articles were selected based on the inclusion criteria (relevance to the purpose of the research, having a structured research framework and publication in a valid journal) and exclusion criteria (unavailability of full text of the article, letter to the editor, and no abstract). The quality of articles was evaluated using the Gifford et al. criteria [36]. Based on the criteria provided for quantitative (6 criteria), qualitative (11 criteria), quasi-experimental (8 criteria), and experimental (7 criteria) studies, the articles were evaluated on a 2-point scale (0 and 1). Out of 593 articles related to the role of resilience and emotion regulation in the psychological distress of hospital staff during the COVID-19 pandemic, 30 completely related articles were included in the study. Then, they were studied thoroughly and accurately (Figure 1). 3. Results
In this study, 30 qualified research articles in Persian and English were reviewed. Table 1 presents the findings from the reviewed articles on the role of resilience and emotion regulation in the psychological distress of hospital staff during the COVID-19 pandemic.

Out of 593 articles related to the role of resilience and emotion regulation in the psychological distress of hospital staff during the COVID-19 pandemic, 30 articles with a total of 13902 samples were selected and reviewed based on the inclusion and exclusion criteria. The studies were collected from 16 countries: Iran, Italy, the Dominican Republic, China, Romania, Turkey, the United States, Nigeria, South Korea, Bahrain, Serbia, Indonesia, the United Kingdom, Portugal, Oman, and Spain. Of the 30 articles reviewed, 24 were quantitative articles, and one was a review article. Also, 36.6% and 63.4% of articles were published in 2020 and 2021, respectively.
Studies have shown that resilience and emotion regulation strategies during the outbreak of COVID-19 had positive effects on nurses, physicians, hospital staff, and medical students. Most studies have shown that good resilience and the use of adaptive emotion regulation strategies can reduce anxiety, depression, insomnia, fear, and rumination, which results in increased well-being and psychological health of hospital staff during the COVID-19 pandemic.
4. Discussion
This study aimed to investigate the role of resilience and emotion regulation in the psychological distress of hospital staff during the COVID-19 pandemic. The present study results showed that medical staff with high resilience performed better in the face of COVID-19 stress and anxiety and had good mental health [6, 7, 8, 9, 10].
In explaining these findings, it can be acknowledged that coping strategies help hospital staff when they face stressful and anxious issues, such as the outbreak of COVID-19 and the high volume of hospitalized patients, positive behaviors are not observed. show good coping styles and have more flexibility [4]. This ability helps nurses and physicians to accept existing conditions and perform at their best [8]. In contrast, low resilience leads to anxiety, stress, and burnout in hospital staff, result in reduced efficiency of services provided by hospital staff. Because resilience includes positive patterns of adaptation to hardships and difficulties over time, nurses and physicians with good resilience are expected to show better flexibility over time [12]. In other words, people with good resilience endure hardships, cope better with threatening situations, cope more effectively with stress and problems, and have a greater capacity to respond to life stressors and cope with everyday problems [17]. This ability causes hospital staff to adapt better to the anxious conditions (such as hospital overcrowding, equipment shortages, and medication) created by the COVID-19 pandemic [3]. In other words, the dimensions of resilience, such as personal competence, trust in instincts, positive acceptance of change, self-confidence, control, and spiritual impact when in stressful and difficult situations, help people to show the necessary flexibility, adapt to the current situation and use effective coping strategies better [14, 15, 16, 17, 18, 19, 20].
On the other hand, the findings showed that medical staff who used adaptive emotion regulation strategies, such as positive reassessment and refocusing on planning, positively coped with COVID-19 anxiety and stress. In contrast, the use of maladaptive emotion regulation strategies, such as catastrophe, rumination, and blaming others, negatively aggravates psychological disorders during the coronavirus 2019 pandemic.
Explaining these findings, it can be acknowledged that people who manage and control their emotions during the COVID-19 outbreak have better mental health. When a person is faced with an emotional situation, feeling good and optimistic is not enough to control the emotion, but he needs to have the best cognitive function in these situations. In regulating emotion, an optimal interaction of cognition and emotion is required to deal with adverse conditions because people interpret every stimulus and situation they encounter, and cognitive interpretations determine people’s reactions [29]. For this reason, people who use negative and weak cognitive styles, such as rumination, catastrophizing, and self-blame during the COVID-19 pandemic are more vulnerable to emotional problems than others [27]. In other words, people who could not properly manage their emotions in the face of stress caused by COVID-19 show more stress, depression, and anxiety. When people with high anxiety symptoms have more difficulty regulating their emotional functions, they are less able to recognize and accept their emotions and are more likely to show negative emotions in ambiguous emotional situations [26, 27, 28, 29, 30, 31].
5. Conclusion
The present study results showed that resilience and emotion regulation play an important role in reducing depression, anxiety, and stress of hospital staff during the COVID-19 pandemic. People with high resilience are well aware of the situation and do their best to accept it and show their best performance. Emotion regulation also allows nurses and physicians to manage and control their emotions. This strategy prevents them from engaging in negative emotions and helps them show their best performance. In this regard, it is suggested to use appropriate psychological services in hospitals to promote the mental health of nurses and physicians.
One of the limitations of the present review study is the unavailability of the full text of some articles, which led to the non-inclusion of these articles in the review process. Also, due to the filtering of some scientific databases, researchers could not access them. In addition, some studies were descriptive and should be cautious in generalizing their results. In this regard, it is suggested that descriptive studies be conducted on the role of resilience and emotion regulation in promoting the mental health of nurses and medical staff of hospitals during the COVID-19 outbreak in the country. These studies improve the physical and psychological function of medical staff in Iran.
Ethical Considerations
Compliance with ethical guidelines
Ethical principles in writing the article have been observed according to the instructions of the National Ethics Committee and the COPE regulations.
Funding
The present study was self-funded.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Fung TS, Liu DX. Human coronavirus: Host-pathogen interaction. Annual Review of Microbiology. 2019; 73:529-57. [DOI:10.1146/annurev-micro-020518-115759] [PMID]
- Cucinotta D, Vanelli M. Who declares covid-19 a Pandemic. Acta Biomedica. 2020; 91(1):157-60. [DOI:10.23750/abm.v91i1.9397] [PMID] [PMCID]
- Lorente L, Vera M, Peiró T. Nurses´ stressors and psychological distress during the covid-19 pandemic: The mediating role of coping and resilience. Journal of Advanced Nursing. 2021; 77(3):1335-44. [DOI:10.1111/jan.14695] [PMID][PMCID]
- Tam CC, Sun S, Yang X, Li X, Zhou Y, Shen Z. Psychological distress among hiv healthcare providers during the covid-19 pandemic in China: Mediating roles of institutional support and resilience. AIDS and Behavior. 2021; 25(1):9-17. [DOI:10.1007/s10461-020-03068-w] [PMID] [PMCID]
- Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the covid-19 pandemic: A systematic review of quantitative studies. Journal of Nursing Management. 2021; 29(7):1893-1905. [DOI:10.1111/jonm.13336] [PMID] [PMCID]
- Collantoni E, Saieva AM, Meregalli V, Girotto C, Carretta G, Boemo DG, et al. Psychological distress, fear of covid-19, and resilient coping abilities among healthcare workers in a tertiary first-line hospital during the coronavirus pandemic. Journal of Clinical Medicine. 2021; 10(7):1465. [DOI:10.3390/jcm10071465] [PMID][PMCID]
- Serrão C, Duarte I, Castro L, Teixeira A. Burnout and depression in portuguese healthcare workers during the covid-19 pandemic-the mediating role of psychological resilience. International journal of environmental research and public health. 2021; 18(2):636. [DOI:10.3390/ijerph18020636] [PMID] [PMCID]
- Luceño-Moreno L, Talavera-Velasco B, García-Albuerne Y, Martín-García J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the covid-19 pandemic. International Journal of Environmental Research and Public Health. 2020; 17(15):5514. [DOI:10.3390/ijerph17155514] [PMID] [PMCID]
- Bagheri Sheykhangafshe F, Tajbakhsh K, Abolghasemi A. [Comparison of covid-19 anxiety, coping styles and health anxiety in athletic and non-athletic students (Persian)]. Sport Psychology Studies (ie, mutaleat ravanshenasi varzeshi). 2020; 9(32):283-306. [DOI:10.22089/spsyj.2020.9377.2027]
- Huang L, Wang Y, Liu J, Ye P, Cheng B, Xu H, et al. Factors associated with resilience among medical staff in radiology departments during the outbreak of 2019 novel coronavirus disease (covid-19): A cross-sectional study. Medical Science Monitor. 2020; 26:e925669. [DOI:10.12659/MSM.925669] [PMID] [PMCID]
- Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in covid-19 pandemics. Psychiatry Research. 2020; 290:113130. [DOI:10.1016/j.psychres.2020.113130] [PMID] [PMCID]
- Roberts NJ, McAloney-Kocaman K, Lippiett K, Ray E, Welch L, Kelly C. Levels of resilience, anxiety and depression in nurses working in respiratory clinical areas during the covid pandemic. Respiratory Medicine. 2021; 176:106219. [DOI:10.1016/j.rmed.2020.106219] [PMID] [PMCID]
- Man MA, Toma C, Motoc NS, Necrelescu OL, Bondor CI, Chis AF, et al. Disease perception and coping with emotional distress during covid-19 pandemic: A survey among medical staff. International Journal of Environmental Research and Public Health. 2020; 17(13):4899. [DOI:10.3390/ijerph17134899] [PMID] [PMCID]
- Chang MC, Chen PF, Lee TH, Lin CC, Chiang KT, Tsai MF, et al. The effect of religion on psychological resilience in healthcare workers during the coronavirus disease 2019 pandemic. Frontiers in Psychology. 2021; 12:628894. [DOI:10.3389/fpsyg.2021.628894] [PMID] [PMCID]
- Setiawati Y, Wahyuhadi J, Joestandari F, Maramis MM, Atika A. Anxiety and resilience of healthcare workers during covid-19 pandemic in indonesia. Journal of Multidisciplinary Healthcare. 2021; 14:1-8. [DOI:10.2147/JMDH.S276655] [PMID] [PMCID]
- Ignjatović Ristić D, Hinić D, Banković D, Kočović A, Ristić I, Rosić G,et al. Levels of stress and resilience related to the covid-19 pandemic among academic medical staff in Serbia. Psychiatry and Clinical Neurosciences. 2020; 74(11):604-5. [DOI:10.1111/pcn.13124] [PMID] [PMCID]
- Aljehani YM, Othman SA, Telmesani NK, Alghamdi RA, AlBuainain HM, Alghamdi ZM, et al. [Stress and psychological resilience among general surgery residents during covid-19 pandemic (Persian)]. Saudi Medical Journal. 2020; 41(12):1344-9. [DOI:10.15537/smj.2020.12.25577] [PMID] [PMCID]
- Hong Y, Lee J, Lee HJ, Kim K, Cho IK, Ahn MH, et al. Resilience and work-related stress may affect depressive symptoms in nursing professionals during the covid-19 pandemic era. Psychiatry Investigation. 2021; 18(4):357-63. [DOI:10.30773/pi.2021.0019] [PMID] [PMCID]
- Coco M, Guerrera CS, Santisi G, Riggio F, Grasso R, Di Corrado D, et al T. Psychosocial impact and role of resilience on healthcare workers during covid-19 pandemic. Sustainability. 2021; 13(13):7096. [Doi:10.3390/su13137096]
- Yörük S, Güler D. The relationship between psychological resilience, burnout, stress, and sociodemographic factors with depression in nurses and midwives during the covid-19 pandemic: A cross-sectional study in Turkey. Perspectives In Psychiatric Care. 2021; 57(1):390-8. [DOI:10.1111/ppc.12659] [PMID]
- Sinichi F, Faridhosseini F, Hajebi Khaniki S, Chalakinia N, Saadati Z, Tara F. [Psychological symptoms and coping strategies of nurses caring for patients with covid-19 pneumonia (Persian)]. Journal of Fundamentals of Mental Health. 2020; 22(6):481-89. [DOI:10.22038/jfmh.2020.17817]
- Garnefski N, Kraaij V. Cognitive emotion regulation questionnaire–development of a short 18-item version (CERQ-short). Personality and Individual Differences. 2006; 41(6):1045-53. [DOI:10.1016/j.paid.2006.04.010]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003; 85(2):348-62. [DOI:10.1037/0022-3514.85.2.348] [PMID]
- Sheppes G, Suri G, Gross JJ. Emotion regulation and psychopathology. Annual review of clinical psychology. 2015; 11:379-405. [DOI:10.1146/annurev-clinpsy-032814-112739] [PMID]
- Bagheri Sheykhangafshe F, Esmaeilinasab M. [Psychological implications of coronavirus 2019 (covid-19) outbreak in chronic diseases Patients: A systematic review article (Persian)]. Chronic Diseases Journal. 2021; 9(3). [DOI:10.22122/cdj.v9i3.629]
- Söğütlü Y, Söğütlü L, Göktaş Sş. Relationship of covid-19 pandemic with anxiety, anger, sleep and emotion regulation in healthcare professionals. Journal of Contemporary Medicine. 2021; 11(1):41-9. [DOI:10.16899/jcm.804329] https://dergipark.org.tr/en/pub/jcm/issue/57927/804329
- García-Batista ZE, Guerra-Peña K, Nouri Kandany V, Marte MI, Garrido LE, Cantisano-Guzmán LM, et al. Covid-19 pandemic and health worker stress: The mediating effect of emotional regulation. PLoS One. 2021; 16(11):e0259013. [DOI:10.1371/journal.pone.0259013] [PMID] [PMCID]
- Wang QQ, Fang YY, Huang HL, Lv WJ, Wang XX, Yang TT, et al. Anxiety, depression and cognitive emotion regulation strategies in Chinese nurses during the covid-19 outbreak. Journal of Nursing Management. 2021; 29(5):1263-74. [DOI:10.1111/jonm.13265] [PMID] [PMCID]
- Zhu Y, Wang H, Wang A. An evaluation of mental health and emotion regulation experienced by undergraduate nursing students in China during the covid-19 pandemic: A cross-sectional study. International Journal of Mental Health Nursing. 2021; 30(5):1160-9. [DOI:10.1111/inm.12867] [PMID] [PMCID]
- Safa M, Ismaili Dolabi Nejad Sh, Qasem Boroujerdi F, Hajizadeh F, Mirabzadeh Ardakani B. [Incidence of post-traumatic stress disorder after covid-19 among medical staff of Masih Daneshvari hospital (Persian)]. Journal of Medical Council of Iran. 2020; 38(1):27-33. http://jmciri.ir/article-1-2980-en.html
- Vitale E. The mindfulness and the emotional regulation skills in Italian nurses during the covid-19 pandemic: A descriptive survey-correlational study. Journal of Holistic Nursing. 2021; 39(4):345-55. [DOI:10.1177/08980101211015804] [PMID]
- Croghan IT, Chesak SS, Adusumalli J, Fischer KM, Beck EW, Patel SR, et al. Stress, resilience, and coping of healthcare workers during the covid-19 pandemic. Journal of Primary Care & Community Health. 2021; 12:21501327211008448. [DOI:10.1177/21501327211008448] [PMID] [PMCID]
- Sirati Nir M, Karimi L, Khalili R. [The perceived stress level of health care and non-health care in exposed to covid-19 pandemic (Persian)]. Iranian Journal of Psychiatry & Clinical Psychology. 2020; 26(3):294-305. [DOI:10.32598/ijpcp.26.3405.1]
- Sarboozi Hosein Abadi T, Askari M, Miri K, Namazi Nia M. [Depression, stress and anxiety of nurses in covid-19 pandemic in Nohe-Dey hospital in Torbat-e-Heydariyeh city, Iran (Persian)]. Journal of Military Medicine. 2020; 22(6):526-33. [DOI:10.30491/JMM.22.6.526]
- Moher D, Liberati A, Tetzlaff J, Altman DG; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery. 2010; 8(5):336-41. [DOI:10.1016/j.ijsu.2010.02.007] [PMID]
- Gifford W, Davies B, Edwards N, Griffin P, Lybanon V. Managerial leadership for nurses’ use of research evidence: An integrative review of the literature. Worldviews on Evidence-Based Nursing. 2007; 4(3):126-45. [DOI:10.1111/j.1741-6787.2007.00095.x] [PMID]
- Rahmanian M, Kamali A R, Mosalanezhad H, Foroughian M, Kalani N, Hatami N, et al . [A comparative study on anxiety of medical and non-medical staff due to exposure and non-exposure to the novel coronavirus disease (Persian)]. Journal of Arak University of Medical Sciences. 2020; 23(5):710-23. [DOI:10.32598/JAMS.23.COV.3577.3]
- Olashore AA, Akanni OO, Oderinde KO. Neuroticism, resilience, and social support: Correlates of severe anxiety among hospital workers during the covid-19 pandemic in Nigeria and Botswana. BMC Health Services Research. 2021; 21(1):398. [DOI:10.1186/s12913-021-06358-8] [PMID] [PMCID]
- Schierberl Scherr AE, Ayotte BJ, Kellogg MB. Moderating roles of resilience and social support on psychiatric and practice outcomes in nurses working during the covid-19 pandemic. SAGE Open Nursing. 2021; 7:23779608211024213. [DOI:10.1177/23779608211024213] [PMID] [PMCID]
- Di Giuseppe M, Nepa G, Prout TA, Albertini F, Marcelli S, Orrù G, et al. Stress, burnout, and resilience among healthcare workers during the covid-19 emergency: The role of defense mechanisms. International Journal of Environmental Research and Public Health. 2021; 18(10):5258. [DOI:10.3390/ijerph18105258] [PMID] [PMCID]
Type of Study: Review Article |
Subject:
● International Health
Received: 2021/07/10 | Accepted: 2021/09/4 | Published: 2021/12/1
Received: 2021/07/10 | Accepted: 2021/09/4 | Published: 2021/12/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








.jpg)

