Volume 13, Issue 6 (Nov & Dec 2023)
J Research Health 2023, 13(6): 417-426 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sarani M, Heydari A, Isfahani P. Investigating the Effects of Educational Intervention Based on the Health Belief Model in Adopting Healthy Behaviors by Type 2 Diabetic Patients in 2021. J Research Health 2023; 13 (6) :417-426
URL: http://jrh.gmu.ac.ir/article-1-2158-en.html
URL: http://jrh.gmu.ac.ir/article-1-2158-en.html
1- Department of Public Health, School of Public Health, Zabol University of Medical Sciences, Zabol, Iran.
2- Department of Health Services Management, School of Public Health, Zabol University of Medical Sciences, Zabol, Iran. ,p.isfehani@gmail.com
2- Department of Health Services Management, School of Public Health, Zabol University of Medical Sciences, Zabol, Iran. ,
Full-Text [PDF 703 kb]
(952 Downloads)
| Abstract (HTML) (3338 Views)
Full-Text: (1188 Views)
1. Introduction
Diabetes mellitus is a prevalent non-communicable disease worldwide [1] and the 4th or 5th cause of death in wealthy countries, with ample evidence indicating the outbreak of diabetes in industrialized and developing countries [2]. The overall commonness of this disease is observing an uptrend, especially in developing countries. Due to the significant prevalence of obesity and, consequently, diabetes, in most countries, obesity and diabetes are called the twin epidemics of the 21st century [3]. In low- and middle-income countries, an increase is observed in the prevalence and socioeconomic burden of diabetes. Accordingly, about 80% of people with diabetes live in such countries [4].
Diabetes is a severe health and social problem globally [5]. It is also a significant cause of blindness, advanced kidney disease, amputation, and cardiovascular issues, particularly during the active ages of life [6]. Type 2 diabetes is often referred to as adult-onset diabetes or lifestyle diabetes, which accounts for up to 95% of all types of diabetes [7] and affects approximately 15% of society members [8]. It loses the body’s ability to effectively produce and use insulin due to a sedentary lifestyle, inadequate nutrition, and poor lifestyle [9].
The International Diabetes Federation (IDF) has recently assessed the prevalence of diabetes in 216 countries. Accordingly, the global prevalence of diabetes is estimated at 8.3% among the 4.4 billion people with 20 to 79 years of age. Meanwhile, 6.4% of the population suffers from impaired glucose tolerance. These figures are predicted to reach 9.9% and 7.1% in 2030, respectively. Half of the people with diabetes are unaware of their situation [10]. Diabetes causes more than 4.6 million deaths a year, half of which are individuals under the age of 60 [11].
Given the increasing statistics and worldwide trends of this disease, diabetes was declared a latent epidemic by the World Health Organization (WHO) [12]. The global prevalence of this condition in the adult population was 285 million in 2010 (6.4%), grew to nearly 371 million in 2012, and is predicted to rise to 552 million by 2030 [13]. According to WHO, the prevalence of diabetes was estimated at 10.3% in the Iranian adult population in 2011, accounting for 10% in men and 10.4% in women [14, 15].
There are many strategies for controlling the disease in all strategies. Education creates new behaviors and trends in people’s lifestyles [16]. Patient education is an essential component of diabetes control [17]. Health education is one of the most practical intervention techniques to create and sustain healthy behavior and lifestyle changes to prevent and control diseases. Health education aims to change behavior so that one’s health and quality of life are promoted [18]. Therefore, for health education programs to be effective, theories and learning models must be utilized. An educational model initiates the program and guides it on the right path to the ultimate evaluation stage [19]. Different models, such as the beliefs, attitudes, subjective norms, enabling factors model, social support, and innovation diffusion theory, can be a potential capacity for diabetic patients to learn more about their disease and prevent its complications [19-22].
The health belief model (HBM) is a theoretical framework for disease prevention. This model is rooted in the theory that one’s willingness to change health behaviors primarily depends on health perceptions. HBM focuses on changing the beliefs causing behavior [23].
The model’s philosophy is that training leads to the creation or alteration in the behavior of learners that have the following four characteristics: 1) Performing the desired health behavior that has benefits for them from economic, social, cultural, and family; 2) Educators should identify the existing barriers for learners, including individual and social, economic, cultural and familial to adopt healthy behaviors and plan accordingly; 3) Educational programs should create the necessary sensitivity in learners about the complications and risks caused by not performing healthy behaviors, including economic, social, cultural, familial aspects; 4) To adopt healthy behaviors, it is necessary to use guidelines for actions, including the recommendations of health care center employees, medical doctors, mass communication devices, posters, pamphlets, and reminder cards [24].
According to this model, a person must undergo several stages to employ preventive behaviors. First, they ought to feel threatened by the subjective perception of the risk of type 2 diabetes (perceived susceptibility). Next, they must comprehend the severity of the disease complications, namely medical and social consequences (perceived severity). Then, through positive external stimulus (cues to action), they must believe that the type 2 diabetes prevention program is feasible and effective (perceived benefits). Subsequently, they weigh the benefits against barriers to action (perceived barriers) and regard them as less costly. Eventually, one takes measures of precaution against type 2 diabetes. Moreover, positive judgment about one’s ability to develop type 2 diabetes preventive behaviors (perceived self-efficacy) is also a reviving force that leads to a person’s demand to adopt disease-preventive behaviors [17, 25].
Various studies have been conducted in this field. For instance, in 2021, Mahmoudian showed that in the intervention group, the scores for knowledge (P=0.01), performance (P=0.01), and self-efficacy (P=0.04) increased significantly, while the score for perceived barriers significantly decreased (P=0.02). This article also showed that education, based on the health belief model, effectively promotes self-care behaviors and controls metabolic complications in diabetic patients [26]. In 2019, Dadkhah Tehrani showed that after the intervention, a significant difference was observed between experimental and control groups in terms of scores of awareness, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and eating behavior (P<0.05) [27].
With the intervention of health education and the application of the health belief model to increase the healthy behaviors of diabetic patients, we aim to investigate the impact of education based on the health belief model in individuals with type 2 diabetes.
2. Methods
This quasi-experimental study included 110 type 2 diabetic patients referred to comprehensive healthcare centers in Zabol, Sistan, and Baluchestan Province, Iran, in 2021. Interventional studies are standard studies to measure the effectiveness of an intervention in people’s health status. Nevertheless, in some cases, the random division of people or communities under investigation into two intervention and control groups becomes impossible. For example, to evaluate the effectiveness of a public health program, it is not possible to randomly divide people into intervention and control groups. In such a case, the design of interventional studies can be used, and due to the limitation, the design of such studies is done in a quasi-experimental fashion [28, 29].
The inclusion criteria were being over 30 years of age, having the ability to read and write, being under the coverage of health centers, having a complete file and specifications in the integrated health systems, and lacking severe complications of diabetes, such as diabetic foot amputation and eye and heart diseases. On the other hand, the individuals unwilling to continue participating in the study had severe disease complications with the doctor’s diagnosis. They were immigrants who were excluded from the study.
The participants selected via convenience sampling were randomly assigned to experimental (n=55) and control groups (n=55). Table 1 shows the number of patients for each center separately.

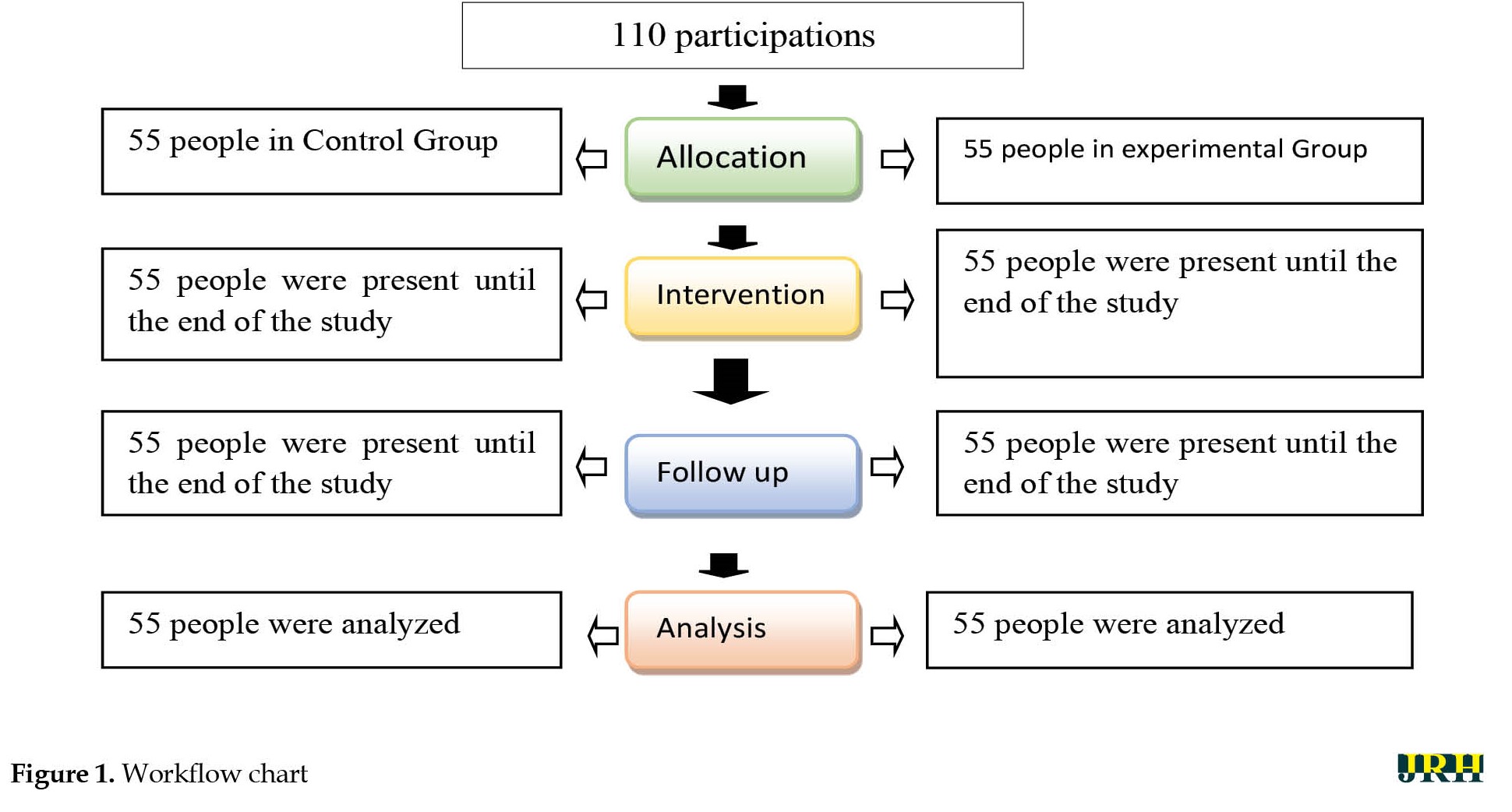
Figure 1 shows the flow chart of the study. The final data analysis was done with 55 samples.
In both groups, after obtaining consent to participate in the study, people were matched in terms of some demographic variables, such as age, education status, occupation status, and duration of diabetes, after entering several patients in the intervention group by matching method. According to the demographic characteristics, a control sample group was also selected and included in the research.
The required data were collected through a standard questionnaire [19] consisting of the following two parts: Demographic characteristics and the constructs of the health belief model. The first part (demographic characteristics) consisted of information on age, sex, marital status, education status, occupation status, and the duration of diabetes. The second part (the constructs of the health belief model) measured perceived susceptibility (n=13), perceived severity (n=15), perceived benefits (n=6), perceived barriers (n=13), cues to action (n=2), and self-efficacy (n=10). The replies were scored on a 3-point Likert scale, resulting in the maximum scores of 39, 18, 45, and 60 in the construct of perceived susceptibility and perceived barriers, perceived benefits, perceived severity, and self-efficacy, respectively. The content validity of this instrument was confirmed in a study by Shojaeezadeh, obtained at 76% [19].
The educational intervention was performed for the experimental group (n=55) by holding three 60-min training sessions in a month in the training room of health centers. Various educational methods were employed in these sessions, such as lectures, group discussions, and modeling successful experiences for the participants. The content of the educational program included the following items: The definitions of diabetes, causes of diabetes, complications of diabetes, diagnosis and treatment methods of diabetes, how to care for diabetes, referring to a healthcare provider, physician, and specialist to perform the necessary regular tests; regular blood sugar control; how to use urine glucose test strips and hemoglucotest; and healthy lifestyle (diet, calorie calculation, and exercise as well as their role in controlling diabetes).
In the last session, one of the patient’s family members participated in the training program, aiming to involve them in training as the best cue to action. Training sessions on the health belief model were performed for the intervention group based on the needs analysis (pre-test). The questionnaire was completed 3 and 6 months after the intervention in both groups, and a fasting glucose test was performed once more; the results were then compared.
To comply with the ethical principles in the research, a pamphlet containing the provided educational materials was provided to the control group.
Data analysis was performed using the SPSS software, version 20, through the chi-square test, paired t-test, Fisher exact test, and independent t-test at a significance level 0.05.
3. Results
The Mean±SD age scores of the participants in the control and intervention groups were obtained at 55.06±1.72 and 54.00±1.69, respectively. Also, this number was 54.50±1.70 years for all participants, which was not significantly different (P=0.35). In this study, most participants were female and married with primary education. A significant difference was found between the study groups regarding gender (P=0.02). Table 1 compares other demographic characteristics of the subjects in the two study groups. Accordingly, the study groups were homogeneous in age, marital status, and educational and occupation status (Table 2).

Based on the findings, the mean score of health belief model constructs was not significantly different in patients in two study groups before the intervention (P>0.05); however, a significant difference was observed after the intervention (P<0.05) (Table 3).
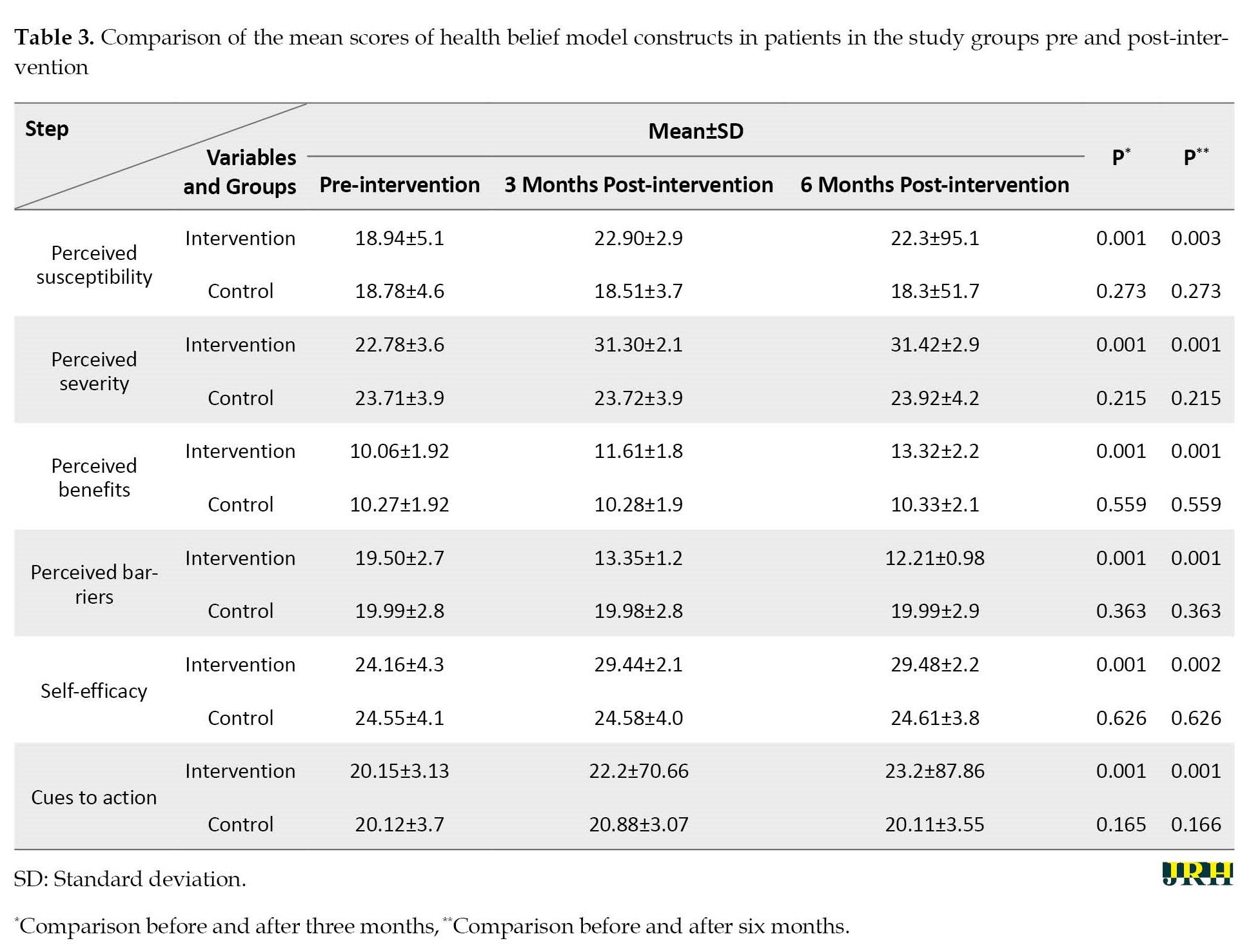
The mean value of perceived susceptibility boosted in the intervention group, reaching from 18.94 before the training to 22.90 and 22.3 after 3 and 6 months of the intervention, respectively.
Before the educational intervention, no significant difference existed in the mean scores of perceived severity between the intervention and control groups. Nonetheless, implementing education based on the health belief model increased the mean score perceived severity in patients in the intervention group to 31.30 and 31.42 after 3 and 6 months of the intervention, respectively, which was significantly different (P=0.001).
Educational programs based on the health belief model improved the mean score of perceived benefits in performing healthy and self-care behaviors in patients in the intervention group from 10.06 before the training to 11.61 and 13.32 after 3 and 6 months of the intervention, respectively. The differences were statistically significant (P=0.001).
Implementing an educational program based on the health belief model decreased the mean score of perceived barriers in diabetic patients in the intervention group from 19.50 before the training to 13.35 and 12.21 after 3 and 6 months of the intervention, respectively, which was statistically significant (P=0.001).
Implementing an educational program based upon the health belief model led to an increase in the mean score of perceived self-efficacy in the group of intervention from 24.16 before the training to 29.44 and 29.48 after 3 and 6 months of the intervention, respectively, which was significantly different (P<0.001).
The mean value of cues to action boosted in the intervention group, reaching from 20.15 before the training to 22.2 and 23.2 after 3 and 6 months of the intervention, respectively, which was significantly different (P=0.001).
4. Discussion
This study investigated the effects of an educational program based on the health belief model on adopting healthy behaviors by type 2 diabetic patients referred to comprehensive healthcare centers in Zabol City, Iran, in 2021. Based on the results, training based on the health belief model could promote healthy behaviors in people with type 2 diabetes.
Moreover, the mean scores of perceived susceptibility were the same in both groups before the educational intervention. Before the educational intervention in the two groups, this score indicated that the mean value of patients’ perceived susceptibility to the disease development was at a moderate level. Nevertheless, with the implementation of the training program, the mean score of perceived susceptibility was significant in the intervention group (P<0.001) 3 and 6 months later.
This result is in line with the results of studies by Tan [30] and Kashfi [31]. Accordingly, in a study conducted by Tan [30], the mean score of perceived susceptibility was not statistically significant before training; however, it increased in the intervention group after the intervention, which was also statistically significant. Additionally, the findings of a study by Bayat on 120 patients with diabetes indicated that the mean value of perceived susceptibility boosted in the intervention group, reaching from 15.85 before the training to 17.77 and 17.78 after 3 and 6 months of the intervention, respectively, which was consistent with the results of the present study [32].
Considering the positive impact of the educational program designed following the health belief model in increasing the perceived susceptibility of diabetic patients in the present study, it is essential to note that perceived susceptibility, as an influential construct in the periods of 3 and 6 months after adopting healthy behaviors by diabetic patients, depends on applicable educational packages about patients’ mental sensitivity toward the possibility of developing diabetes or the harmful conditions resulting from adopting consistent and healthy behaviors. The reason is that as long as patients do not feel the consequences of the disease, they will not seek ways to lessen the disease complications. Consequently, an increase in the perceived susceptibility of patients confirmed the impact of educational programs based on the constructs of this health belief model.
Before the educational intervention, no significant difference existed in the mean scores of perceived severity between the intervention and control groups. Nonetheless, the findings of this study demonstrated that the design of education based on the health belief model effectively increased the perceived severity of diabetic patients after 3 and 6 months, which was significantly different. Based on the findings of other studies by Baghiani [33] and Bayat [32], the perceived severity score in the intervention group followed a rising trend after training, which was consistent with the results of the present study. This score rose due to the patient’s participation in the health belief model training sessions over 3 and 6 months. In this model, the consequences of the disease, such as disability and high treatment costs, are key variables that can affect the level of perceived severity. The training based upon the health belief model over 3 and 6 months increased the mean score of perceived severity in diabetic patients, ultimately leading to adopting healthy behavior, a lifestyle change, and a reduction of the disease consequences.
Our findings indicated that educational programs based on the health belief model improved the mean score of perceived benefits in performing healthy and self-care behaviors in patients in the intervention group over 3 and 6 months, which was significantly different; however, this score did not change significantly in the control group. According to the results of studies conducted by Zigheymat [34] and Shamsi [35], based on the health belief model on 88 diabetic patients, the mean score of perceived benefits improved in patients in the intervention group after the training, which was significantly different and in line with the results of a study by Bayat [32] and the current study.
The findings of this study indicated that the design and implementation of an educational program based on the health belief model boosted the level of susceptibility and severity and, eventually, decreased the mean score of perceived barriers in diabetic patients in the intervention group, which was statistically significant; nonetheless, no such significant differences were detected in the control group.
The training program designed over 3 and 6 months was effective in reducing the perceived barriers in diabetic patients so that it increased patients’ beliefs in the intervention group about the real costs of the disease and its consequences, which was in line with the findings of previous studies, including Bayat [32], Baghiani [33], Shamsi [35], and Mohammadi [36], regarding a reduction in perceived barriers. Moreover, Mohebbi [37] conducted a study on 110 diabetic patients (2019) and reported that the mean scores of the patients in the intervention groups were significantly different at baseline and after 3 and 6 months post-intervention (P<0.001), while the observed differences in the control group were not significant.
The results of the present study also suggested that designing an educational program based on the health belief model led to an increase in the mean score of perceived self-efficacy in the group of intervention after 3 and 6 months, which was significantly different (P<0.001); however, the control group showed no such significant differences. Based on the findings of a study conducted by Dehghan on 110 subjects with diabetes in 2015, self-efficacy and social support could predict 33.5% of the observed variance of self-care behaviors [38].
Accordingly, the perceived self-efficacy showed no significant difference before the intervention in both study groups; nevertheless, the differences were statistically significant following the implementation of the training program after 3 and 6 months (P<0.001). Dehghani et al. investigated the necessity of using appropriate educational methods for students, which revealed significant differences in the improvement of self-efficacy in the intervention group [38], confirming the findings reported by Choi et al. [39].
On the other hand, the findings of this study indicated that self-efficacy could be the strongest predictive construct of this model. Usually, people who showed the most changes had a higher level of self-efficacy for performing a specific behavior. People with high self-efficacy seem to have a higher inclination to adopt measures regarding self-management healthcare and react more appropriately in dealing with health-threatening factors.
The essential goals of education are to promote health and improve people’s self-efficacy. In the present study, in line with the results reported by Choi et al., it was revealed that cues to action and the participation of family members were among the strongest and most crucial external practice guides. In the mentioned research, people with diabetes learn about health concepts more from family members who are respectful of them. Identifying influential local people and leaders among families of diabetes people could influence health education [39].
The educational intervention based on the health belief model showed the positive effects of education on perceived susceptibility, severity, threat, benefits, barriers, and self-efficacy. These positive effects were more evident in perceived severity, benefits, and self-efficacy. The current study’s findings demonstrated the impact and efficiency of the health belief model on adopting healthy behaviors by type 2 diabetic patients.
The present study had several strengths, such as matching the control and intervention groups and adopting a community-based approach to implementing the care program. This educational model plays a significant role in the health system’s services to society members. Accordingly, it is suggested that health education programs based upon the health belief model be included in healthcare programs as an intervention with easy, effective implementation.
5. Conclusion
The present study’s findings confirmed the importance of implementing educational programs based upon the health belief model constructs in adopting healthy behaviors by type 2 diabetic patients. Moreover, given the efficacy of the health belief model, especially the constructs of perceived severity, perceived barriers, and perceived self-efficacy as the most powerful predictors found in this study in descending order, it is recommended that this model be implemented to teach primary and secondary prevention to diabetic patients. The results of this study revealed that educating diabetic patients, conducting active follow-up, and trying to remove the perceived barriers of patients could pave the way to improving the skills of people with diabetes in adopting healthy behaviors and decreasing the complications of the disease.
Study limitations
Among the limitations of the present study were the previous knowledge and experiences of diabetic patients, interest in accepting the type of education, educational media and their features, and cognitive and emotional characteristics of patients. The other limitation of this study was the non-completion of the questionnaire by the subjects due to their very low literacy. However, the researchers tried to minimize the effect of this limitation by encouraging the patients to participate in the training course, ensuring them that the training content would benefit their health, and interviewing illiterate people.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Zabol University of Medical Sciences (Code: IR.ZBMU.REC.1398.127) and informed consent was obtained from every participant.
Funding
This study was financially supported by the Zabol University of Medical Science.
Authors' contributions
Study design and data extraction: Mohammad Saran; Study conduction: Azadeh Heydari and Mohammad Saran; Drafting the manuscript: Azadeh Heydari and Parvaneh Isfahani; Review and editing: Parvaneh Isfahani; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank and appreciate all the participants who took part in this research.
References
Diabetes mellitus is a prevalent non-communicable disease worldwide [1] and the 4th or 5th cause of death in wealthy countries, with ample evidence indicating the outbreak of diabetes in industrialized and developing countries [2]. The overall commonness of this disease is observing an uptrend, especially in developing countries. Due to the significant prevalence of obesity and, consequently, diabetes, in most countries, obesity and diabetes are called the twin epidemics of the 21st century [3]. In low- and middle-income countries, an increase is observed in the prevalence and socioeconomic burden of diabetes. Accordingly, about 80% of people with diabetes live in such countries [4].
Diabetes is a severe health and social problem globally [5]. It is also a significant cause of blindness, advanced kidney disease, amputation, and cardiovascular issues, particularly during the active ages of life [6]. Type 2 diabetes is often referred to as adult-onset diabetes or lifestyle diabetes, which accounts for up to 95% of all types of diabetes [7] and affects approximately 15% of society members [8]. It loses the body’s ability to effectively produce and use insulin due to a sedentary lifestyle, inadequate nutrition, and poor lifestyle [9].
The International Diabetes Federation (IDF) has recently assessed the prevalence of diabetes in 216 countries. Accordingly, the global prevalence of diabetes is estimated at 8.3% among the 4.4 billion people with 20 to 79 years of age. Meanwhile, 6.4% of the population suffers from impaired glucose tolerance. These figures are predicted to reach 9.9% and 7.1% in 2030, respectively. Half of the people with diabetes are unaware of their situation [10]. Diabetes causes more than 4.6 million deaths a year, half of which are individuals under the age of 60 [11].
Given the increasing statistics and worldwide trends of this disease, diabetes was declared a latent epidemic by the World Health Organization (WHO) [12]. The global prevalence of this condition in the adult population was 285 million in 2010 (6.4%), grew to nearly 371 million in 2012, and is predicted to rise to 552 million by 2030 [13]. According to WHO, the prevalence of diabetes was estimated at 10.3% in the Iranian adult population in 2011, accounting for 10% in men and 10.4% in women [14, 15].
There are many strategies for controlling the disease in all strategies. Education creates new behaviors and trends in people’s lifestyles [16]. Patient education is an essential component of diabetes control [17]. Health education is one of the most practical intervention techniques to create and sustain healthy behavior and lifestyle changes to prevent and control diseases. Health education aims to change behavior so that one’s health and quality of life are promoted [18]. Therefore, for health education programs to be effective, theories and learning models must be utilized. An educational model initiates the program and guides it on the right path to the ultimate evaluation stage [19]. Different models, such as the beliefs, attitudes, subjective norms, enabling factors model, social support, and innovation diffusion theory, can be a potential capacity for diabetic patients to learn more about their disease and prevent its complications [19-22].
The health belief model (HBM) is a theoretical framework for disease prevention. This model is rooted in the theory that one’s willingness to change health behaviors primarily depends on health perceptions. HBM focuses on changing the beliefs causing behavior [23].
The model’s philosophy is that training leads to the creation or alteration in the behavior of learners that have the following four characteristics: 1) Performing the desired health behavior that has benefits for them from economic, social, cultural, and family; 2) Educators should identify the existing barriers for learners, including individual and social, economic, cultural and familial to adopt healthy behaviors and plan accordingly; 3) Educational programs should create the necessary sensitivity in learners about the complications and risks caused by not performing healthy behaviors, including economic, social, cultural, familial aspects; 4) To adopt healthy behaviors, it is necessary to use guidelines for actions, including the recommendations of health care center employees, medical doctors, mass communication devices, posters, pamphlets, and reminder cards [24].
According to this model, a person must undergo several stages to employ preventive behaviors. First, they ought to feel threatened by the subjective perception of the risk of type 2 diabetes (perceived susceptibility). Next, they must comprehend the severity of the disease complications, namely medical and social consequences (perceived severity). Then, through positive external stimulus (cues to action), they must believe that the type 2 diabetes prevention program is feasible and effective (perceived benefits). Subsequently, they weigh the benefits against barriers to action (perceived barriers) and regard them as less costly. Eventually, one takes measures of precaution against type 2 diabetes. Moreover, positive judgment about one’s ability to develop type 2 diabetes preventive behaviors (perceived self-efficacy) is also a reviving force that leads to a person’s demand to adopt disease-preventive behaviors [17, 25].
Various studies have been conducted in this field. For instance, in 2021, Mahmoudian showed that in the intervention group, the scores for knowledge (P=0.01), performance (P=0.01), and self-efficacy (P=0.04) increased significantly, while the score for perceived barriers significantly decreased (P=0.02). This article also showed that education, based on the health belief model, effectively promotes self-care behaviors and controls metabolic complications in diabetic patients [26]. In 2019, Dadkhah Tehrani showed that after the intervention, a significant difference was observed between experimental and control groups in terms of scores of awareness, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and eating behavior (P<0.05) [27].
With the intervention of health education and the application of the health belief model to increase the healthy behaviors of diabetic patients, we aim to investigate the impact of education based on the health belief model in individuals with type 2 diabetes.
2. Methods
This quasi-experimental study included 110 type 2 diabetic patients referred to comprehensive healthcare centers in Zabol, Sistan, and Baluchestan Province, Iran, in 2021. Interventional studies are standard studies to measure the effectiveness of an intervention in people’s health status. Nevertheless, in some cases, the random division of people or communities under investigation into two intervention and control groups becomes impossible. For example, to evaluate the effectiveness of a public health program, it is not possible to randomly divide people into intervention and control groups. In such a case, the design of interventional studies can be used, and due to the limitation, the design of such studies is done in a quasi-experimental fashion [28, 29].
The inclusion criteria were being over 30 years of age, having the ability to read and write, being under the coverage of health centers, having a complete file and specifications in the integrated health systems, and lacking severe complications of diabetes, such as diabetic foot amputation and eye and heart diseases. On the other hand, the individuals unwilling to continue participating in the study had severe disease complications with the doctor’s diagnosis. They were immigrants who were excluded from the study.
The participants selected via convenience sampling were randomly assigned to experimental (n=55) and control groups (n=55). Table 1 shows the number of patients for each center separately.

Figure 1 shows the flow chart of the study. The final data analysis was done with 55 samples.
In both groups, after obtaining consent to participate in the study, people were matched in terms of some demographic variables, such as age, education status, occupation status, and duration of diabetes, after entering several patients in the intervention group by matching method. According to the demographic characteristics, a control sample group was also selected and included in the research.
The required data were collected through a standard questionnaire [19] consisting of the following two parts: Demographic characteristics and the constructs of the health belief model. The first part (demographic characteristics) consisted of information on age, sex, marital status, education status, occupation status, and the duration of diabetes. The second part (the constructs of the health belief model) measured perceived susceptibility (n=13), perceived severity (n=15), perceived benefits (n=6), perceived barriers (n=13), cues to action (n=2), and self-efficacy (n=10). The replies were scored on a 3-point Likert scale, resulting in the maximum scores of 39, 18, 45, and 60 in the construct of perceived susceptibility and perceived barriers, perceived benefits, perceived severity, and self-efficacy, respectively. The content validity of this instrument was confirmed in a study by Shojaeezadeh, obtained at 76% [19].
The educational intervention was performed for the experimental group (n=55) by holding three 60-min training sessions in a month in the training room of health centers. Various educational methods were employed in these sessions, such as lectures, group discussions, and modeling successful experiences for the participants. The content of the educational program included the following items: The definitions of diabetes, causes of diabetes, complications of diabetes, diagnosis and treatment methods of diabetes, how to care for diabetes, referring to a healthcare provider, physician, and specialist to perform the necessary regular tests; regular blood sugar control; how to use urine glucose test strips and hemoglucotest; and healthy lifestyle (diet, calorie calculation, and exercise as well as their role in controlling diabetes).
In the last session, one of the patient’s family members participated in the training program, aiming to involve them in training as the best cue to action. Training sessions on the health belief model were performed for the intervention group based on the needs analysis (pre-test). The questionnaire was completed 3 and 6 months after the intervention in both groups, and a fasting glucose test was performed once more; the results were then compared.
To comply with the ethical principles in the research, a pamphlet containing the provided educational materials was provided to the control group.
Data analysis was performed using the SPSS software, version 20, through the chi-square test, paired t-test, Fisher exact test, and independent t-test at a significance level 0.05.
3. Results
The Mean±SD age scores of the participants in the control and intervention groups were obtained at 55.06±1.72 and 54.00±1.69, respectively. Also, this number was 54.50±1.70 years for all participants, which was not significantly different (P=0.35). In this study, most participants were female and married with primary education. A significant difference was found between the study groups regarding gender (P=0.02). Table 1 compares other demographic characteristics of the subjects in the two study groups. Accordingly, the study groups were homogeneous in age, marital status, and educational and occupation status (Table 2).

Based on the findings, the mean score of health belief model constructs was not significantly different in patients in two study groups before the intervention (P>0.05); however, a significant difference was observed after the intervention (P<0.05) (Table 3).
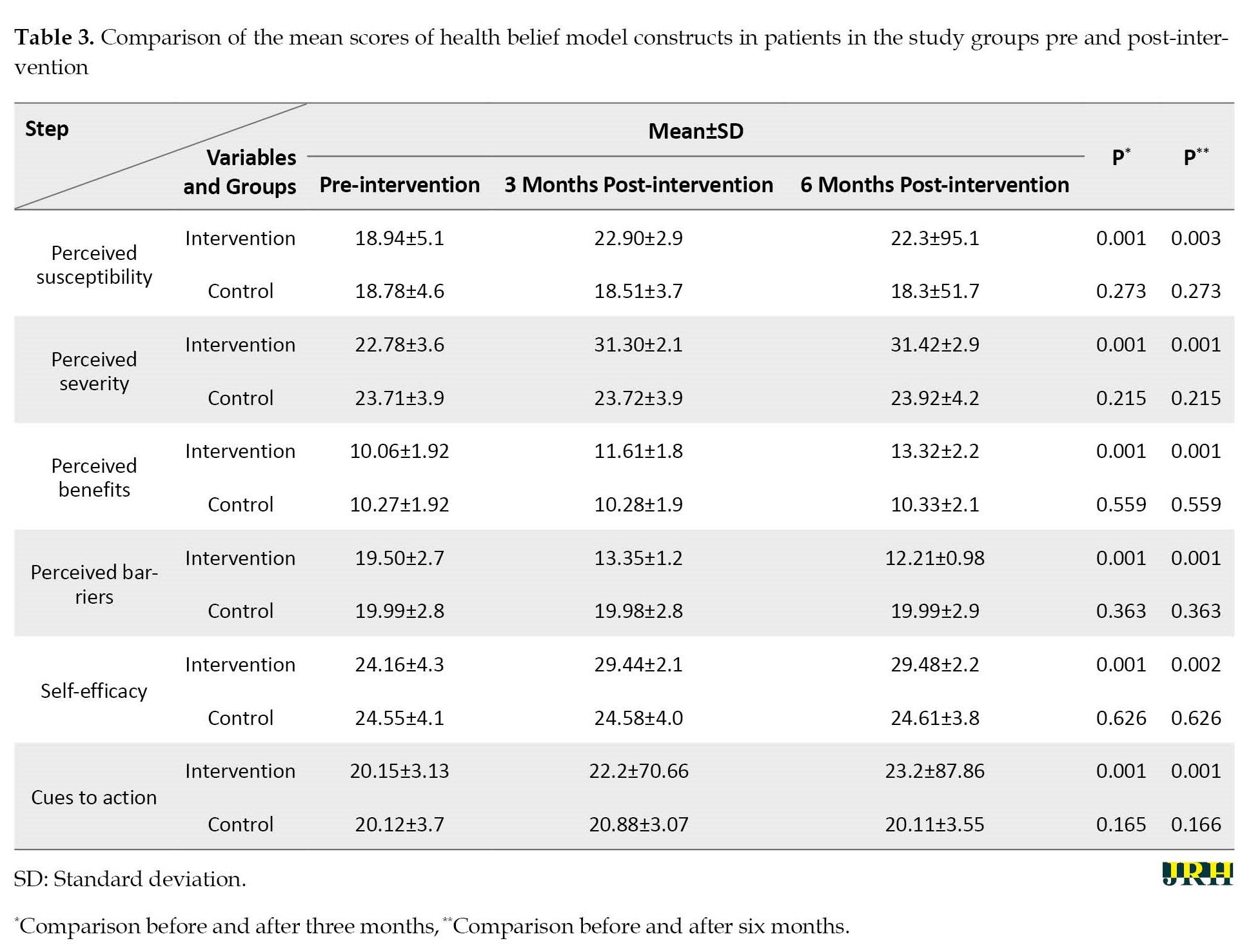
The mean value of perceived susceptibility boosted in the intervention group, reaching from 18.94 before the training to 22.90 and 22.3 after 3 and 6 months of the intervention, respectively.
Before the educational intervention, no significant difference existed in the mean scores of perceived severity between the intervention and control groups. Nonetheless, implementing education based on the health belief model increased the mean score perceived severity in patients in the intervention group to 31.30 and 31.42 after 3 and 6 months of the intervention, respectively, which was significantly different (P=0.001).
Educational programs based on the health belief model improved the mean score of perceived benefits in performing healthy and self-care behaviors in patients in the intervention group from 10.06 before the training to 11.61 and 13.32 after 3 and 6 months of the intervention, respectively. The differences were statistically significant (P=0.001).
Implementing an educational program based on the health belief model decreased the mean score of perceived barriers in diabetic patients in the intervention group from 19.50 before the training to 13.35 and 12.21 after 3 and 6 months of the intervention, respectively, which was statistically significant (P=0.001).
Implementing an educational program based upon the health belief model led to an increase in the mean score of perceived self-efficacy in the group of intervention from 24.16 before the training to 29.44 and 29.48 after 3 and 6 months of the intervention, respectively, which was significantly different (P<0.001).
The mean value of cues to action boosted in the intervention group, reaching from 20.15 before the training to 22.2 and 23.2 after 3 and 6 months of the intervention, respectively, which was significantly different (P=0.001).
4. Discussion
This study investigated the effects of an educational program based on the health belief model on adopting healthy behaviors by type 2 diabetic patients referred to comprehensive healthcare centers in Zabol City, Iran, in 2021. Based on the results, training based on the health belief model could promote healthy behaviors in people with type 2 diabetes.
Moreover, the mean scores of perceived susceptibility were the same in both groups before the educational intervention. Before the educational intervention in the two groups, this score indicated that the mean value of patients’ perceived susceptibility to the disease development was at a moderate level. Nevertheless, with the implementation of the training program, the mean score of perceived susceptibility was significant in the intervention group (P<0.001) 3 and 6 months later.
This result is in line with the results of studies by Tan [30] and Kashfi [31]. Accordingly, in a study conducted by Tan [30], the mean score of perceived susceptibility was not statistically significant before training; however, it increased in the intervention group after the intervention, which was also statistically significant. Additionally, the findings of a study by Bayat on 120 patients with diabetes indicated that the mean value of perceived susceptibility boosted in the intervention group, reaching from 15.85 before the training to 17.77 and 17.78 after 3 and 6 months of the intervention, respectively, which was consistent with the results of the present study [32].
Considering the positive impact of the educational program designed following the health belief model in increasing the perceived susceptibility of diabetic patients in the present study, it is essential to note that perceived susceptibility, as an influential construct in the periods of 3 and 6 months after adopting healthy behaviors by diabetic patients, depends on applicable educational packages about patients’ mental sensitivity toward the possibility of developing diabetes or the harmful conditions resulting from adopting consistent and healthy behaviors. The reason is that as long as patients do not feel the consequences of the disease, they will not seek ways to lessen the disease complications. Consequently, an increase in the perceived susceptibility of patients confirmed the impact of educational programs based on the constructs of this health belief model.
Before the educational intervention, no significant difference existed in the mean scores of perceived severity between the intervention and control groups. Nonetheless, the findings of this study demonstrated that the design of education based on the health belief model effectively increased the perceived severity of diabetic patients after 3 and 6 months, which was significantly different. Based on the findings of other studies by Baghiani [33] and Bayat [32], the perceived severity score in the intervention group followed a rising trend after training, which was consistent with the results of the present study. This score rose due to the patient’s participation in the health belief model training sessions over 3 and 6 months. In this model, the consequences of the disease, such as disability and high treatment costs, are key variables that can affect the level of perceived severity. The training based upon the health belief model over 3 and 6 months increased the mean score of perceived severity in diabetic patients, ultimately leading to adopting healthy behavior, a lifestyle change, and a reduction of the disease consequences.
Our findings indicated that educational programs based on the health belief model improved the mean score of perceived benefits in performing healthy and self-care behaviors in patients in the intervention group over 3 and 6 months, which was significantly different; however, this score did not change significantly in the control group. According to the results of studies conducted by Zigheymat [34] and Shamsi [35], based on the health belief model on 88 diabetic patients, the mean score of perceived benefits improved in patients in the intervention group after the training, which was significantly different and in line with the results of a study by Bayat [32] and the current study.
The findings of this study indicated that the design and implementation of an educational program based on the health belief model boosted the level of susceptibility and severity and, eventually, decreased the mean score of perceived barriers in diabetic patients in the intervention group, which was statistically significant; nonetheless, no such significant differences were detected in the control group.
The training program designed over 3 and 6 months was effective in reducing the perceived barriers in diabetic patients so that it increased patients’ beliefs in the intervention group about the real costs of the disease and its consequences, which was in line with the findings of previous studies, including Bayat [32], Baghiani [33], Shamsi [35], and Mohammadi [36], regarding a reduction in perceived barriers. Moreover, Mohebbi [37] conducted a study on 110 diabetic patients (2019) and reported that the mean scores of the patients in the intervention groups were significantly different at baseline and after 3 and 6 months post-intervention (P<0.001), while the observed differences in the control group were not significant.
The results of the present study also suggested that designing an educational program based on the health belief model led to an increase in the mean score of perceived self-efficacy in the group of intervention after 3 and 6 months, which was significantly different (P<0.001); however, the control group showed no such significant differences. Based on the findings of a study conducted by Dehghan on 110 subjects with diabetes in 2015, self-efficacy and social support could predict 33.5% of the observed variance of self-care behaviors [38].
Accordingly, the perceived self-efficacy showed no significant difference before the intervention in both study groups; nevertheless, the differences were statistically significant following the implementation of the training program after 3 and 6 months (P<0.001). Dehghani et al. investigated the necessity of using appropriate educational methods for students, which revealed significant differences in the improvement of self-efficacy in the intervention group [38], confirming the findings reported by Choi et al. [39].
On the other hand, the findings of this study indicated that self-efficacy could be the strongest predictive construct of this model. Usually, people who showed the most changes had a higher level of self-efficacy for performing a specific behavior. People with high self-efficacy seem to have a higher inclination to adopt measures regarding self-management healthcare and react more appropriately in dealing with health-threatening factors.
The essential goals of education are to promote health and improve people’s self-efficacy. In the present study, in line with the results reported by Choi et al., it was revealed that cues to action and the participation of family members were among the strongest and most crucial external practice guides. In the mentioned research, people with diabetes learn about health concepts more from family members who are respectful of them. Identifying influential local people and leaders among families of diabetes people could influence health education [39].
The educational intervention based on the health belief model showed the positive effects of education on perceived susceptibility, severity, threat, benefits, barriers, and self-efficacy. These positive effects were more evident in perceived severity, benefits, and self-efficacy. The current study’s findings demonstrated the impact and efficiency of the health belief model on adopting healthy behaviors by type 2 diabetic patients.
The present study had several strengths, such as matching the control and intervention groups and adopting a community-based approach to implementing the care program. This educational model plays a significant role in the health system’s services to society members. Accordingly, it is suggested that health education programs based upon the health belief model be included in healthcare programs as an intervention with easy, effective implementation.
5. Conclusion
The present study’s findings confirmed the importance of implementing educational programs based upon the health belief model constructs in adopting healthy behaviors by type 2 diabetic patients. Moreover, given the efficacy of the health belief model, especially the constructs of perceived severity, perceived barriers, and perceived self-efficacy as the most powerful predictors found in this study in descending order, it is recommended that this model be implemented to teach primary and secondary prevention to diabetic patients. The results of this study revealed that educating diabetic patients, conducting active follow-up, and trying to remove the perceived barriers of patients could pave the way to improving the skills of people with diabetes in adopting healthy behaviors and decreasing the complications of the disease.
Study limitations
Among the limitations of the present study were the previous knowledge and experiences of diabetic patients, interest in accepting the type of education, educational media and their features, and cognitive and emotional characteristics of patients. The other limitation of this study was the non-completion of the questionnaire by the subjects due to their very low literacy. However, the researchers tried to minimize the effect of this limitation by encouraging the patients to participate in the training course, ensuring them that the training content would benefit their health, and interviewing illiterate people.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Zabol University of Medical Sciences (Code: IR.ZBMU.REC.1398.127) and informed consent was obtained from every participant.
Funding
This study was financially supported by the Zabol University of Medical Science.
Authors' contributions
Study design and data extraction: Mohammad Saran; Study conduction: Azadeh Heydari and Mohammad Saran; Drafting the manuscript: Azadeh Heydari and Parvaneh Isfahani; Review and editing: Parvaneh Isfahani; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank and appreciate all the participants who took part in this research.
References
- Udedi M, Pence BW, Stewart RC, Muula AS. Detection and prevalence of depression among adult type 2 diabetes mellitus patients attending non-communicable diseases clinics in Lilongwe, Malawi. International Journal of Mental Health Systems. 2020; 14(1):79. [DOI:10.1186/s13033-020-00413-3] [PMID]
- Selvin E, Juraschek SP. Diabetes Epidemiology in the COVID-19 Pandemic. Diabetes Care. 2020; 43(8):1690-4.[DOI:10.2337/dc20-1295] [PMID]
- Chobot A, Górowska-Kowolik K, Sokołowska M, Jarosz-Chobot P. Obesity and diabetes—not only a simple link between two epidemics. Diabetes/Metabolism Research and Reviews. 2018; 34(7):e3042. [DOI:10.1002/dmrr.3042] [PMID]
- Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes - global burden of disease and forecasted trends. Journal of Epidemiology and Global Health. 2020; 10(1):107-11. [DOI:10.2991/jegh.k.191028.001] [PMID]
- Longato E, Di Camillo B, Sparacino G, Saccavini C, Avogaro A, Fadini GP. Diabetes diagnosis from administrative claims and estimation of the true prevalence of diabetes among 4.2 million individuals of the Veneto region (North East Italy). Nutrition, Metabolism, and Cardiovascular Diseases. 2020; 30(1):84-91. [DOI:10.1016/j.numecd.2019.08.017] [PMID]
- Ampofo AG, Boateng EB. Beyond 2020: Modelling obesity and diabetes prevalence. Diabetes Research and Clinical Practice. 2020; 167:108362. [DOI:10.1016/j.diabres.2020.108362] [PMID]
- Centers for Disease Control and Prevention. National diabetes statistics report. Atlanta: Centers for Disease Control and Prevention; 2020. [Link]
- Nasiri Ziba F, Meresht F, Seyedfatemi N, Haghani H. The effect of life skills training program on quality of life and its dimensions in patients with type 2 diabetes. Annals of Tropical Medicine and Public Health. 2017; 10(5):1174. [DOI:0.4103/ATMPH.ATMPH_276_17]
- Sankar P, Ahmed WN, Mariam Koshy V, Jacob R, Sasidharan S. Effects of COVID-19 lockdown on type 2 diabetes, lifestyle and psychosocial health: A hospital-based cross-sectional survey from South India. Diabetes & Metabolic Syndrome. 2020; 14(6):1815-9. [DOI:10.1016/j.dsx.2020.09.005] [PMID]
- Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271-281. [DOI:10.1016/j.diabres.2018.02.023] [PMID]
- Tancredi M, Rosengren A, Svensson AM, Kosiborod M, Pivodic A, Gudbjörnsdottir S, et al. Excess mortality among persons with type 2 diabetes. The New England Journal of Medicine. 2015; 373(18):1720-32. [DOI:10.1056/NEJMoa1504347] [PMID]
- Guariguata L. By the numbers: New estimates from the IDF Diabetes Atlas Update for 2012. Diabetes Research and Clinical Practice. 2012; 98(3):524-5. [DOI:10.1016/j.diabres.2012.11.006] [PMID]
- Pérez-Sánchez H, den-Haan H, Peña-García J, Lozano-Sánchez J, Martínez Moreno ME, Sánchez-Pérez A, et al. DIA-DB: A database and web server for the prediction of diabetes drugs. Journal of Chemical Information and Modeling. 2020; 60(9):4124-30. [DOI:10.1021/acs.jcim.0c00107] [PMID]
- Vanitha SS, Javalkar SR. A cross-sectional study on risk factors for Type 2 diabetes mellitus in rural population of Davangere. International Journal of Medical Science and Public Health. 2017; 6(7):1163-8. [DOI:10.5455/ijmsph.2017.0409212042017]
- Kaveeshwar SA, Cornwall J. The current state of diabetes mellitus in India. The Australasian Medical Journal. 2014; 7(1):45-8. [DOI:10.4066/AMJ.2014.1979] [PMID]
- Bantle JP, Wylie-Rosett J, Albright AL, Apovian CM, Clark NG, Franz MJ, et al. Nutrition recommendations and interventions for diabetes--2006: A position statement of the American Diabetes Association. Diabetes Care. 2006; 29(9):2140-57. [DOI:10.2337/dc06-9914] [PMID]
- Edelman C, Kudzma EC. Health promotion, through out the lifespan. Edinburgh: Elsevier Health Sciences; 1986. [Link]
- Hajizadeh Y, Rezaei M, Poureshgh Y, Vahid Dastjerdi M. [Heavy metals in industrial wastewater especially chromium (VI) are considered as the main environmental pollutants (Persian)]. Journal of Health System Research. 2014; 10(2):362-75. [Link]
- Saffari M, Shojaeezadeh D, Ghoranipour F, Heidarnia A, Pakpour Hagiagha A. [Theories, models and methods of health education and health promotion (Persian)]. Tehran: Aasar Sobhan; 2000. [Link]
- Dickinson JK. A critical social theory approach to nursing care of adolescents with diabetes. Issues in Comprehensive Pediatric Nursing. 1999; 22(4):143-52. [DOI:10.1080/014608699265248] [PMID]
- De Civita M, Dasgupta K. Using diffusion of innovations theory to guide diabetes management program development: An illustrative example. Journal of Public Health. 2007; 29(3):263-8. [DOI:10.1093/pubmed/fdm033] [PMID]
- Jeihooni AK, Barati M, Kouhpayeh A, Kashfi SM, Harsini PA, Rahbar M. The effect of educational intervention based on BASNEF model on self-medication behavior of type 2 diabetic patients. Indian Journal of Endocrinology and Metabolism. 2019; 23(6):616-22. [DOI:10.4103/ijem.IJEM_436_19] [PMID]
- Sharifirad G, Entezari MH, Kamran A, Azadbakht L. The effectiveness of nutritional education on the knowledge of diabetic patients using the health belief model. Journal of Research in Medical Sciences. 2009; 14(1):1-6. [PMID] [PMCID]
- Spikmans FJ, Brug J, Doven MM, Kruizenga HM, Hofsteenge GH, van Bokhorst-van der Schueren MA. Why do diabetic patients not attend appointments with their dietitian? Journal of Human Nutrition and Dietetics. 2003; 16(3):151-8. [DOI:10.1046/j.1365-277X.2003.00435.x] [PMID]
- Khazaee-Pool M, Shahrousvand S, Naghibi S A. [Predicting Covid-19 preventive behaviors based on health belief model: An internet-based study in Mazandaran Province, Iran (Persian)]. Journal of Mazandaran University of Medical Sciences. 2020; 30(190):56-66. [Link]
- Mahmoudian A, Golshiri P, Rejali M. [Effect of education based on health belief model on self-care behavior and metabolic indices in patients with type 2 diabetes: A clinical research trial (Persian)]. Journal of Mazandaran University of Medical Sciences. 2021; 31(202):71-9. [Link]
- Dadkhah Tehrani B, Tavakoli R, Jazayeri S A. The effect of an educational intervention based on health belief model on nutritional behaviors in type 2 diabetics (Persian)]. Journal of Military Caring Sciences. 2019; 5(4):303-11. [DOI:10.29252/mcs.5.4.303]
- Rezaeian M. [Quasi-experimental study design (Persian)]. Journal of Rafsanjan University of Medical Sciences. 2018; 17(8):697-8. [Link]
- Richard TC, Mark MM. Quasi-experimentation. In: Wholey J, Hatry H, Newcomer K, editors. Handbook of practical program evaluations. Hoboken: Wiley; 2004. [Link]
- Tan MY. The relationship of health beliefs and complication prevention behaviors of Chinese individuals with Type 2 Diabetes Mellitus. Diabetes Research and Clinical Practice. 2004; 66(1):71-7. [DOI:10.1016/j.diabres.2004.02.021] [PMID]
- Kashfi SM, Khani Jeihooni A, Rezaianzadeh A, Amini Sh. The effect of health belief model educational program and jogging on control of sugar in type 2 diabetic patients. Iranian Red Crescent Medical Journal. 2012; 14(7):442-6. [PMID] [PMCID]
- Bayat F, Shojaeezadeh D, Baikpour M, Heshmat R, Baikpour M, Hosseini M. The effects of education based on extended health belief model in type 2 diabetic patients: A randomized controlled trial. Journal of Diabetes and Metabolic Disorders. 2013; 12(1):45. [DOI:10.1186/2251-6581-12-45] [PMID]
- Baghianimoghadam MH, Hadavand Khani M, Mohammadi SM, Fallahzade H, khabiri F. [Status of walking behavior in patients with type 2 diabetes in Yazd based on health belief model (Persian)]. Journal of Health System Research. 2011; 6(3):425-35. [Link]
- Zigheymat F, Ebadi A, Motahedian TE, Alaf JM, Hamedanizadeh F. [Effect of training according to health belief model (HBM) on health believing, knowledge and behavior of patients under CABG (Persian)]. Kowsar Medical Journal. 2009; 13(4):1-6. [Link]
- Shamsi M, Sharifirad G, Kachoyee A, Hassanzadeh A. [The effect of educational program walking based on health belief model on control suger in woman by type 2 diabetics(Persian)]. Iranian Journal of Endocrinology and Metabolism. 2010; 11(5):490-9. [Link]
- Mohammadi S, Karim NA, Talib RA, Amani R. The impact of self-efficacy education based on the health belief model in Iranian patients with type 2 diabetes: A randomised controlled intervention study. Asia Pacific Journal of Clinical Nutrition. 2018; 27(3):546-55. [DOI: 10.6133/apjcn.072017.07]
- Mohebbi B, Tol A, Sadeghi R, Mohtarami SF, Shamshiri A. Self-management Intervention Program Based on the Health Belief Model (HBM) among Women with Gestational Diabetes Mellitus: A quazi-experimental study. Archives of Iranian Medicine. 2019; 22(4):168-73. [PMID]
- Dehghani-Tafti A, Mazloomy Mahmoodabad SS, Morowatisharifabad MA, Afkhami Ardakani M, Rezaeipandari H, Lotfi MH. Determinants of self-care in diabetic patients based on health belief model. Global Journal of Health Science. 2015; 7(5):33-42. [DOI:10.5539/gjhs.v7n5p33] [PMID]
- Choi HS, Ahn HY. Effects of mothers involved in dental health program for their children. Journal of Korean Academy of Nursing. 2012; 42(7):1050-61. [DOI:10.4040/jkan.2012.42.7.1050] [PMID]
Type of Study: Orginal Article |
Subject:
● Health Education
Received: 2022/11/21 | Accepted: 2023/04/29 | Published: 2023/10/3
Received: 2022/11/21 | Accepted: 2023/04/29 | Published: 2023/10/3
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |