Volume 13, Issue 4 (Jul & Aug 2023)
J Research Health 2023, 13(4): 247-254 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pawestri P, Machmudah M, Rejeki S, Pranata S, Fitria S A N, Fitri M L, et al . Difference Effectiveness of Progressive Muscle Relaxation Therapy and Endorphin Massage Therapy Towards Reducing Menstrual Pain Intensity in Adolescents. J Research Health 2023; 13 (4) :247-254
URL: http://jrh.gmu.ac.ir/article-1-2229-en.html
URL: http://jrh.gmu.ac.ir/article-1-2229-en.html
Pawestri Pawestri1 

 , Machmudah Machmudah1
, Machmudah Machmudah1 

 , Sri Rejeki2
, Sri Rejeki2 

 , Satriya Pranata1
, Satriya Pranata1 

 , Savira Ayu Nur Fitria1
, Savira Ayu Nur Fitria1 

 , Medina Laila Fitri3
, Medina Laila Fitri3 

 , Reina Dhamanik1
, Reina Dhamanik1 

 , Nikmatul Khayati1
, Nikmatul Khayati1 




 , Machmudah Machmudah1
, Machmudah Machmudah1 

 , Sri Rejeki2
, Sri Rejeki2 

 , Satriya Pranata1
, Satriya Pranata1 

 , Savira Ayu Nur Fitria1
, Savira Ayu Nur Fitria1 

 , Medina Laila Fitri3
, Medina Laila Fitri3 

 , Reina Dhamanik1
, Reina Dhamanik1 

 , Nikmatul Khayati1
, Nikmatul Khayati1 


1- Department of Nursing, Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Central Java, Indonesia.
2- Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang City, Central Java, Indonesia. ,srirejeki@unimus.ac.id
3- Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang City, Central Java, Indonesia.
2- Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang City, Central Java, Indonesia. ,
3- Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang City, Central Java, Indonesia.
Full-Text [PDF 544 kb]
(1433 Downloads)
| Abstract (HTML) (3236 Views)
Full-Text: (1716 Views)
1. Introduction
Adolescents are individuals who enter a period of transition from children to adults who are marked by changes in physical, emotional, cognitive, and social growth and development. In adolescent girls, adolescence is marked by enlarged hips and breasts, increased height and weight, hair beginning to grow in the armpit and pubic area, and menstruation [1, 2]. Menstruation is one of the signs of women who have entered adolescence or puberty [3]. Menstruation consists of several cycles that occur every month at the production age. Some women experience discomfort before menstruation [4]. Menstruation is a complex cycle accompanied by monthly bleeding lasting about 3-7 days that occur in women involving several organs, including the hypothalamus, cerebral cortex, ovarian pituitary axis, endometrial uterus, and secondary sex organs in women [2].
Disorders or abnormalities that appear when menstruation arrives, such as pain in the lower abdomen, are called dysmenorrhea [3]. Dysmenorrhea is a pain in the abdomen, precisely in the hypogastric region (pubic region) that radiates to the pelvis (pelvis) this is due to muscle contractions in the uterus (womb) during menstruation. Prostaglandins stimulate the uterus to contract during menstruation (Sylvia, 2017). According to World Health Organization (WHO), 90% or 1 769 425 women experience menstrual pain, with 10%-15% of women with severe menstrual pain [3].
Based on the phenomenon that occurs, most teenagers cannot control their emotions when experiencing dysmenorrhea, they do not go to school and withdraw to affect the psychology of adolescents. Some women experience menstrual pain, overcoming the pain by taking painkillers regularly. However, the nature of the drug only leaves pain and can lead to dependence [5]. In addition to drugs, pain can also be reduced by non-pharmacological methods, such as progressive muscle relaxation (PMR) techniques that can reduce pain whose therapy is focused on maintaining a state of deep relaxation that involves contraction and relaxation of various muscle groups starting from the feet up or from the heads down, in this way, it will be realized where the muscle will be and in this case, the awareness of the body's muscle response increases [6].
Non-pharmacological treatment of dysmenorrhea is with PMR techniques and endorphin massage (EM) therapy. PMR techniques and EM therapy are effective in reducing the degree of dysmenorrhea. Relaxation is a technique of loosening or releasing tension. In addition, it is also useful for treating diseases from within the body, improving physical abilities, and balancing the body and mind [7]. PMR technique is an alternative to reducing pain which is done by relaxing muscle tension. PMR technique is a relaxation technique combining deep breathing exercises and a series of muscle contractions and relaxations [8]. The benefits of PMR relaxation are to reduce tension in muscles, especially the muscles of the extremities, improve circulation, lower blood pressure, reduce anxiety and reduce stress, reduce problems related to stress, overcome insomnia or difficulty sleeping, and reduce muscle pain or cramps [9]. Likewise, EM therapy is a therapy with a light touch technique that stimulates the release of endorphins compounds that function as pain relievers and create a feeling of comfort in women [10]. Based on previous research, as many as 16 respondents were given warm compresses and EM, the results showed a decrease in the menstrual pain scale from moderate to mild [11]. A single study on PMR and EM was investigated but no study has compared the effectiveness of the two interventions. Thus, this study was conducted to determine the difference in the effectiveness of pain intensity performed by PMR therapy and EM therapy.
2. Methods
The research design was a quasi-experiment with a two-group pretest and posttest design approach. The study was conducted at Senior High School 1 Lasem in September 2022. The population consisted of adolescents aged 13-14 years, and female students at Senior High School 1 Lasem. Respondents were selected using a purposive sampling technique with inclusion and exclusion criteria. Students who experienced dysmenorrhea and do not have a genetic abnormality are the inclusion criteria of this study. After selecting based on the criteria set by the researcher from the entire population, the number of respondents who met the criteria was 80 respondents. We randomly divided 80 respondents into two groups using a computer. Forty respondents received PMR intervention and another 40 respondents received EMT intervention.
The way to measure pain intensity is to use a pain scale instrument called the numeric rating scale (NRS) [12]. The act of PMR and EM using standard operating procedures (SOPs) that have been made, for EM using the concept [13] for PMR using theory [14].
Progressive muscle relaxation (PMR) procedure
Procedures for PMR exist. Forehead, squeeze the forehead muscles and hold for 15 s. Feel the muscles getting tighter then slowly release the tension in the forehead while counting for 30 s.
On the jaw, tighten the muscles in the jaw, hold for 15 s then release the tension slowly while counting for 30 s. For the neck and shoulders, increase tension in the neck and shoulders by lifting the shoulders toward the ears and holding for 15 s. For the arms and hands area, slowly pull both hands into fists. Draw a fist to a chest and hold for 15 s, squeezing as tightly then release slowly and count for 30 s. For the leg area, slowly increase the tension in the quadriceps and calves for 15 s. Tighten the muscles as hard as you can. Then release the tension gently for 30 s. Continue breathing slowly and evenly [9].
Endorphin massage (EM) procedures
Instruct the respondent to take a comfortable position, which can be sitting or lying. Instruct the participant to take a deep breath while closing the eyes and exhaling gently. Meanwhile, the nurse stroked the outer surface of the respondent's arm. Caress gently using the back of the finger, or only fingertips. After about 5 minutes, switch to another hand. This technique is also performed on other parts of the body, incl palms, neck, shoulders, and thighs. Advise the respondent to relax and feel the sensation. Massage is done for 15 minutes [11].
IBM SPSS statistics for Windows, version 20.0 (IBM Corporation, Armonk, NY, USA) was used for archiving and statistical analysis. Univariate analysis was performed on the variable intensity of menstrual pain (dysmenorrhea) before and after the intervention of PMR and EM. Bivariate analysis was performed using the Wilcoxon test due to non-parametric data to analyze the difference in the decrease in the intensity of menstrual pain (dysmenorrhea) which was performed by PMR interventions and EM therapy.
3. Results
The results of the study can be presented with Tables and descriptive descriptions of the characteristics of respondents who experience dysmenorrhea as follows:
Table 1 presents the characteristics of respondents based on a minimum age of 13 years and a maximum age of 14, and an average age of 13.28 years with a standard deviation of 0.66.
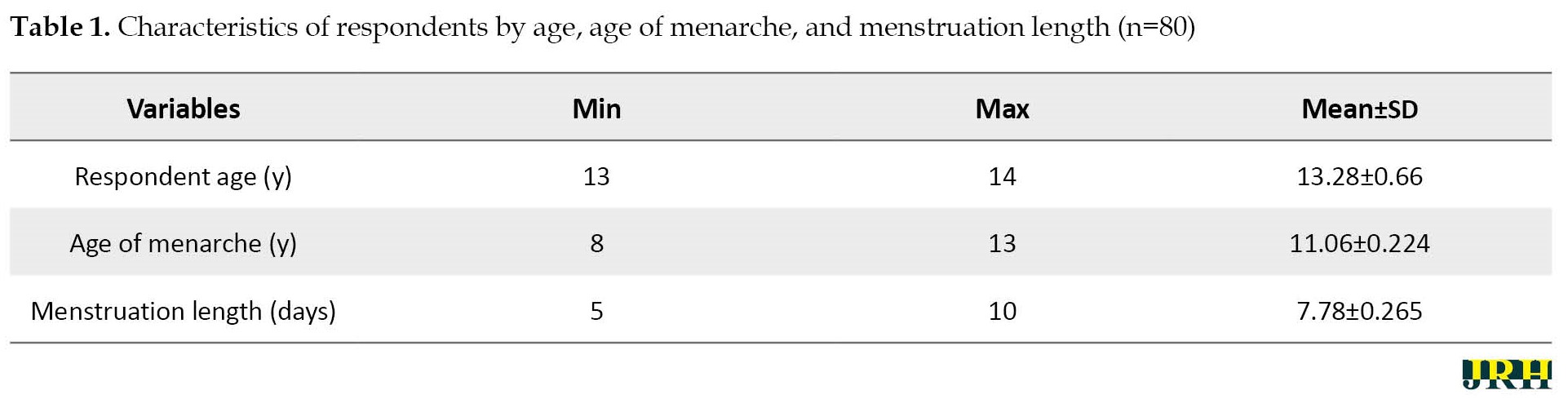
The minimum age of menarche was 8 years and the maximum age was 13, and the average age was 11.06 years with a standard deviation of 0.224. Furthermore, the minimum length of menarche was 5 days, the maximum length of menarche was 10 days, and the average length of menarche was 7.78 years with a standard deviation of 0.265.
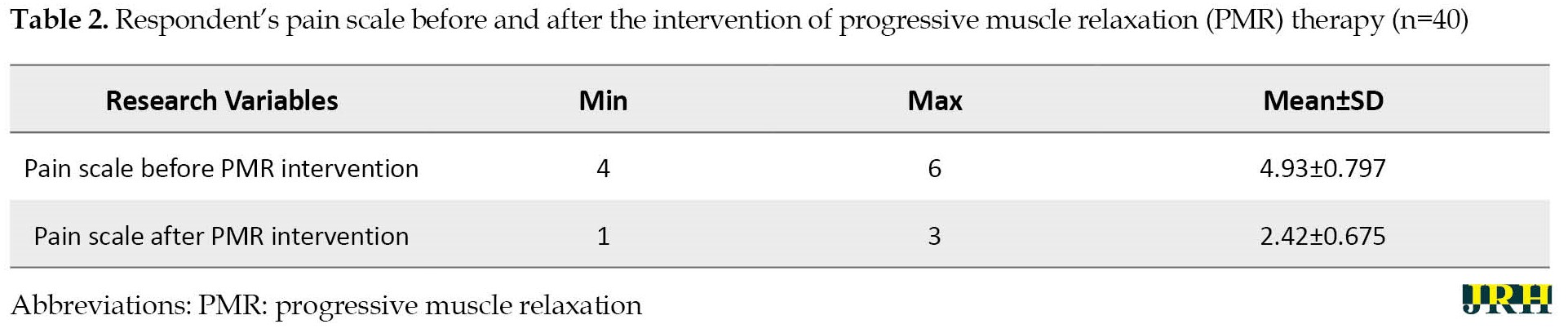
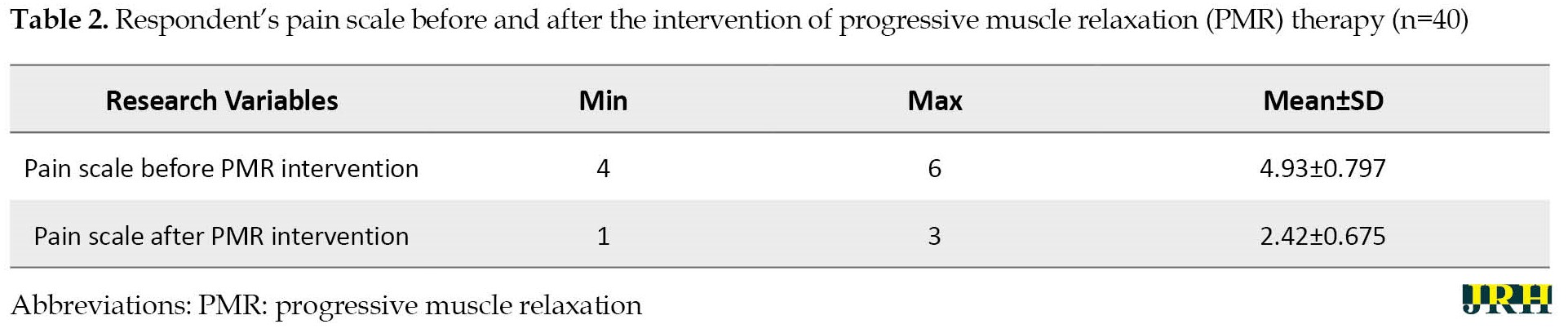
Based on Table 2, the respondent’s pain scale before the PMR intervention was a minimum 4, a maximum 6 and the average pain scale was 4.93 with a standard deviation of 0.797, the respondent’s pain scale after the PMR intervention was a minimum 1, a maximum 3, and, the average pain scale was 2.42 with a standard deviation 0.675.
Based on Table 3, the respondent’s pain scale before the EM intervention was a minimum 4, a maximum 6 and the average pain scale was 4.80 with a standard deviation of 0.687, respondent’s pain scale after the PMR intervention was a minimum 1, a maximum 5 and, the average pain scale was 2.90 with a standard deviation of 0.955.
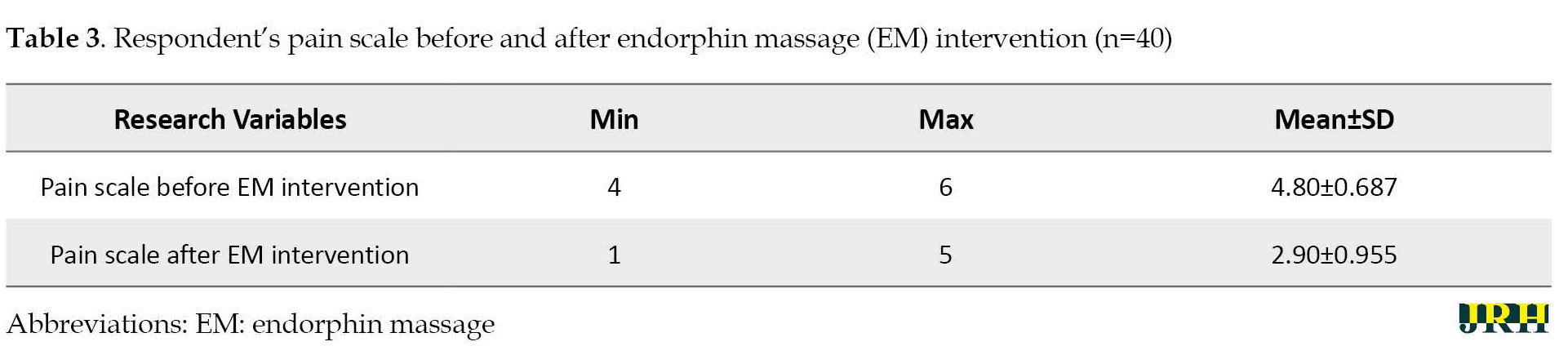
Table 4 presents the average intensity of menstrual pain (dysmenorrhea) after being given PMR intervention with an average pain scale of 2.42±0.675.
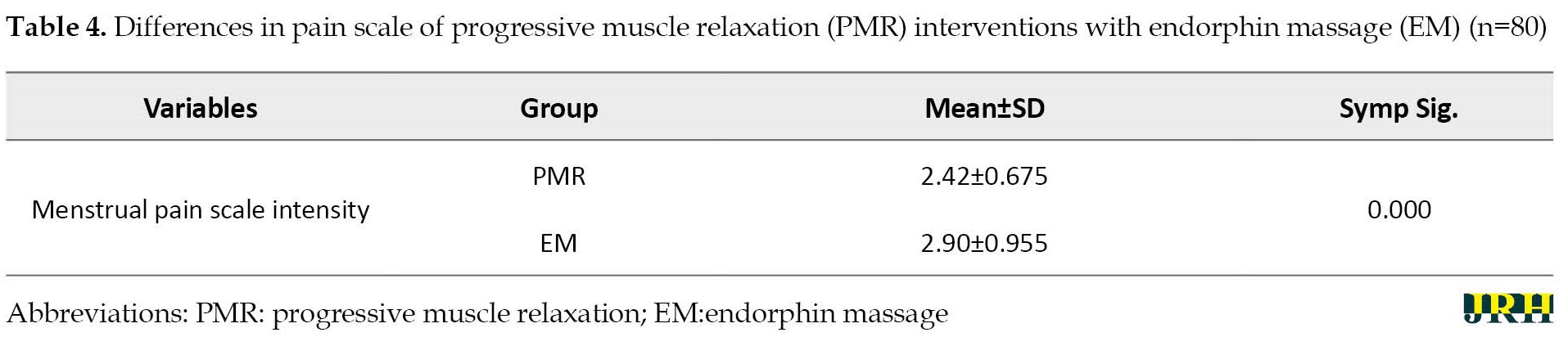
Meanwhile, the average intensity of menstrual pain (dysmenorrhea) after the EM intervention was given with an average pain scale of 2.90 with a standard deviation of 0.955 with a significance level of 0.000.
It can be concluded that the difference in the average intensity of menstrual pain in the intervention and control groups is 4.8 points. Further analysis showed a significant difference in the average pain intensity of menstrual pain in the group that was given the intervention of PMR and EM with a test value of two independent groups (Wilcoxon), the difference in the effectiveness of giving PMR interventions and EM therapy on the intensity of the menstrual pain scale
4. Discussion
The results of the study on the age characteristics of the adolescent respondents of SMP Negeri 1 Lasem as many as 80 respondents showed that the obtained data on the mean age of the respondents was 13.28 years with the youngest age of 13 years and the oldest age of 14 years, with a standard deviation of 0.66. This study showed significant data by the theory of risk factors for dysmenorrhea. Age is one of the prevalent factors in the incidence of dysmenorrhea (menstrual pain) because increasing age affects the response to pain intensity. Menstrual pain occurs due to the dilation of blood vessels due to the sloughing of the epithelial epithelium in the endometrium. Menstrual conditions will stimulate the cervix to dilate, this dilation differs from one woman to another. When a person is in their early teens, they experience menstruation as something new, therefore the cervix is still narrow and then responds with pain, therefore, women in their early teens often experience pain during menstruation compared to late teenage or adult women [15]. In this study, according to WHO, the age of about 13-14 years is still classified as a group of adolescents so that the rate of dysmenorrhea is still high.
The results of the study in terms of the age category of menarche on the respondents obtained data that the mean age of menarche was 11.06 years, the category of the earliest menarche was 8 years, the age of the latest menarche was 13 years, and the standard deviation value was 0.224. First menstruation at an early age of fewer than 11 years [16], at the age of fewer than 11 years, the number of primary ovarian follicles is still in small numbers so that estrogen production is still low [17].
This study contains data that support the theory of risk factors for age at menarche according to the prevalence of dysmenorrhea (menstrual pain). The age of menarche is one of the triggering factors for menstrual pain (dysmenorrhea) due to prolonged exposure to prostaglandins and the occurrence of constriction in the cervix (cervix), resulting in a painful response during menstruation. In adolescents with early menarche, the reproductive organs have not optimally functioned, and also with changes due to the hormones [18].
It has been found that in terms of the category of menstrual duration, the respondents obtained an average menstrual period of 7.78 days, the longest menstrual period was 5 days and the longest period was 10 days with a standard deviation of 0.265. This study is supported by a theory stating that one of the risk factors for dysmenorrhea (menstrual pain) is the abnormal length of menstruation or more than 7 days. From the results of this study, it was found that the average length of menstruation was 7.78, meaning that the length of menstruation was abnormal, which increased in the incidence of menstrual pain. Prolonged causes menstruation contractions of the uterine muscles for a long time so that prostaglandin levels increase, causing menstrual pain. Increased levels of prostaglandins can trigger a pain response during menstruation [19].
Results showed that the average intensity of the menstrual pain scale before PMR was 4.93 with the lowest pain intensity on scale 4 and the highest pain intensity on scale 6, with a standard deviation of 0.151. Meanwhile, after performing PMR, an average of 2.42 was obtained with the lowest pain intensity of scale 1 and the highest pain intensity of scale 3, with a standard deviation of 0.675. The results showed that the mean difference before and after PMR decreased by 2.51 points. This study is supported by the theory that movements in PMR are used to control anxiety or tension when women experience menstruation or dysmenorrhea [20]. Movements in PMR help relax the muscles so that the muscles are relaxed and menstrual pain can be controlled and recognized. Menstrual pain is transmitted by visceral pain impulses originating from the chest and abdominal cavities through sensory nerve fibers that run in the sympathetic nerves and is reduced by PMR interventions that reduce the tension of the muscle fibres, and nerves and reduce pain caused by menstruation. It was further explained that some pain fibers are almost entirely stimulated by excessive mechanical stress or mechanical damage to the tissues referred to as mechanosensitive pain receptors so that PMR interventions can be carried out to reduce excessive mechanical stress.
Results showed that the average intensity of the menstrual pain scale before PMR was 4.93 with the lowest pain intensity on scale 4 and the highest pain intensity on scale 6, with a standard deviation of 0.151. Meanwhile, after performing PMR, an average of 2.42 was obtained with the lowest pain intensity of scale 1 and the highest pain intensity of scale 3, with a standard deviation of 0.675. The results showed that the mean difference before and after PMR decreased by 2.51 points. This study is supported by the theory that movements in PMR are used to control anxiety or tension when women experience menstruation or dysmenorrhea [20]. Movements in PMR help relax the muscles so that the muscles are relaxed and menstrual pain can be controlled and recognized. Menstrual pain is transmitted by visceral pain impulses originating from the chest and abdominal cavities through sensory nerve fibers that run in the sympathetic nerves and is reduced by PMR interventions that reduce the tension of the muscle fibres, and nerves and reduce pain caused by menstruation. It was further explained that some pain fibers are almost entirely stimulated by excessive mechanical stress or mechanical damage to the tissues referred to as mechanosensitive pain receptors so that PMR interventions can be carried out to reduce excessive mechanical stress.
The results showed that the average intensity of the menstrual pain scale before EM therapy was 4.80 with the lowest pain intensity on scale 4 and the highest pain intensity on scale 6, with a standard deviation of 0.687. While after performing PMR, the average was 2.90 with the lowest pain intensity on scale 1 and the highest pain intensity on scale 5, with a standard deviation of 0.955. The results showed that the mean difference before and after EM therapy reduced by 1.90 points. This study is supported by the theory that light touch stimulation on EM can stimulate the release of the beta-endorphin hormone from the body which functions to create a feeling of comfort and relaxation to reduce the body's pain response [21]. EM intervention provides calm and relaxation; therefore the brain secretes endorphins that naturally can reduce pain caused by uterine contractions. Menstrual pain that occurs due to increased prostaglandins in the blood stimulates increased uterine contractions, resulting in decreased blood flow and oxygen to the uterus resulting in ischemia. Pain impulses can be regulated and inhibited by defense mechanisms throughout the central nervous system, pain impulses are transmitted when a barrier is opened and impulses are inhibited when a defense is closed. One way to close this defense is to stimulate the secretion of endorphins, which inhibit the release of pain substances. EM intervention was performed to treat pain to reduce uterine tension via physiological mechanisms, i.e, facilitating blood vessels, inhibiting pain sensations, and providing comfort to the individual. Endorphins are substances associated with pain regulation, functioning as excitation-conducting substances that activate parts of the brain's analgesic system. The release of endorphins into the cerebrospinal fluid of the third ventricle can cause analgesia, thereby inhibiting the delivery of pain impulses to the parietal lobe and reducing pain sensation. Stimulation of nociceptors releases substance P peptide (SP) and peptide associated with the calcitonin gene (CGRP), which increases vascular permeability [22] This neurotransmitter reaches the hypothalamus and midbrain, stimulating the release of endorphins and enkephalins (a neuromodulator) as natural pain controllers.
The results of the study showed that the average intensity of the dysmenorrhea pain scale after PMR intervention was 2.42 with a standard deviation of 0.675. While the average intensity of the dysmenorrhea pain scale after EM intervention was 2.90, with a standard deviation of 0.955. The total number of respondents was 80 respondents. Therefore, it can be concluded that PMR is more effective in reducing the intensity of the dysmenorrhea pain scale in adolescents at SMP Negeri 1 Lasem with an average difference of 4.8 points. This is supported by the concept of a comparative theory of how PMR and EM therapy work as follows:
PMR is more effective in reducing dysmenorrhea pain; this is supported by the theory that the movement in PMR is a combination of deep breath relaxation and muscle relaxation, resulting in a comfortable and relaxed feeling. A series of movements in PMR serves to control tension and anxiety before menstruation and can lower blood pressure [23].
The way EM therapy works is that endorphins are formed from the pituitary gland which is part of the hypothalamus, which is a place to control the hormone system. Several vital hormones exist in the body in dealing with pain, one of which is the beta-endorphin hormone. Beta-endorphin is known as endogenous morphine, which is found in the pituitary gland as morphine, which is naturally released by the human body [24].
Smooth touch stimulation is done at the meridian points to stimulate the process of releasing endorphins. When endorphins are released and flow throughout the body, beta-endorphins receptors act as an analgesic or as a pain reliever and stimulate the brain to create a relaxed feeling [25].
The results of data analysis research showed that the Mann-Whitney test's results were obtained with a Symp Sig. of 0.004 <0.05, the hypothesis was accepted, that is, the effect of providing PMR interventions and endorphin massage therapy on the intensity of the dysmenorrhea (menstrual) pain scale in junior high school adolescents. 1 Lasem. In this study, the concept of PMR and EM is supported.
PMR is a therapy with several movement techniques that work to tighten the muscles and create a relaxed feeling, with movement techniques in PMR can control anxiety and tension before menstruation [20]. While EM therapy is massage with a light touch method to release endorphins from the body as a pain reliever or pain controller by creating a calm and comfortable feeling. EM therapy is mostly used to treat labor pains, postpartum mothers, and breastfeeding mothers [26–28]. This study adds the concept that EM can be used to treat menstrual pain.
In this study, PMR is more effective in dealing with menstrual pain compared to EM because an active process of the respondent to perform muscle relaxant movements coupled with deep breath relaxation exists to provide further increase in muscle relaxation, widen blood vessels, and reduce pain due to spasm or stiffness in muscles. According to Anisa, dysmenorrhea is pain during menstruation caused by uterine muscle spasms [29]. PMR intervention is a series of muscle movements starting from the muscles of the face, hands, arms, neck, chest, abdomen, thighs, and legs. The movement of the performed movements relaxes the muscles coupled with the action of deep breathing in each PMR movement, providing more oxygen in the blood vessels to inhibit and reduce painful stimuli and painful nerve impulses leading to the hypothalamus.
5. Conclusion
Data analysis obtained a Symp Sig. of 0.004 <0.05, therefore a difference is observed in the effectiveness of providing PMR intervention and EM therapy on the intensity of the menstrual pain scale. Menstrual pain can be reduced by blocking nerve impulses from reaching the brain, among others, by providing PMR therapy to control tension and anxiety. In conclusion, PMR therapy is more effective to control menstrual pain compared to EM. It is recommended that PMR therapy can be done by themselves in case of menstrual pain. The limitation of this study was the small samples. More samples are needed in future studies.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from Research Ethics Committee Muhammadiyah University, Semarang on March 18, 2022 (IRB No.: INA/041/2022). The researcher asked the principal for approval if agreed, the child signed the informed consent.
Funding
This study was funded by Muhammadiyah University, Semarang, Indonesia.
Authors' contributions
Conceptualizing, designing, and writing the first draft and framework: Pawestri Pawestri; Interpreting the data, and supervising: Machmudah Machmudah, Sri Rejeki; Collecting the data: Savira Ayu Nur Fitria, Medina Laila Fitri, Reina Dhamanik; Interpreting the data, as well as evaluating the data: Satriya Pranata, Nikmatul Khayati; The published version of the manuscript has been read and approved by all authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We thank the participants and any parties who contribute to this study
References
Adolescents are individuals who enter a period of transition from children to adults who are marked by changes in physical, emotional, cognitive, and social growth and development. In adolescent girls, adolescence is marked by enlarged hips and breasts, increased height and weight, hair beginning to grow in the armpit and pubic area, and menstruation [1, 2]. Menstruation is one of the signs of women who have entered adolescence or puberty [3]. Menstruation consists of several cycles that occur every month at the production age. Some women experience discomfort before menstruation [4]. Menstruation is a complex cycle accompanied by monthly bleeding lasting about 3-7 days that occur in women involving several organs, including the hypothalamus, cerebral cortex, ovarian pituitary axis, endometrial uterus, and secondary sex organs in women [2].
Disorders or abnormalities that appear when menstruation arrives, such as pain in the lower abdomen, are called dysmenorrhea [3]. Dysmenorrhea is a pain in the abdomen, precisely in the hypogastric region (pubic region) that radiates to the pelvis (pelvis) this is due to muscle contractions in the uterus (womb) during menstruation. Prostaglandins stimulate the uterus to contract during menstruation (Sylvia, 2017). According to World Health Organization (WHO), 90% or 1 769 425 women experience menstrual pain, with 10%-15% of women with severe menstrual pain [3].
Based on the phenomenon that occurs, most teenagers cannot control their emotions when experiencing dysmenorrhea, they do not go to school and withdraw to affect the psychology of adolescents. Some women experience menstrual pain, overcoming the pain by taking painkillers regularly. However, the nature of the drug only leaves pain and can lead to dependence [5]. In addition to drugs, pain can also be reduced by non-pharmacological methods, such as progressive muscle relaxation (PMR) techniques that can reduce pain whose therapy is focused on maintaining a state of deep relaxation that involves contraction and relaxation of various muscle groups starting from the feet up or from the heads down, in this way, it will be realized where the muscle will be and in this case, the awareness of the body's muscle response increases [6].
Non-pharmacological treatment of dysmenorrhea is with PMR techniques and endorphin massage (EM) therapy. PMR techniques and EM therapy are effective in reducing the degree of dysmenorrhea. Relaxation is a technique of loosening or releasing tension. In addition, it is also useful for treating diseases from within the body, improving physical abilities, and balancing the body and mind [7]. PMR technique is an alternative to reducing pain which is done by relaxing muscle tension. PMR technique is a relaxation technique combining deep breathing exercises and a series of muscle contractions and relaxations [8]. The benefits of PMR relaxation are to reduce tension in muscles, especially the muscles of the extremities, improve circulation, lower blood pressure, reduce anxiety and reduce stress, reduce problems related to stress, overcome insomnia or difficulty sleeping, and reduce muscle pain or cramps [9]. Likewise, EM therapy is a therapy with a light touch technique that stimulates the release of endorphins compounds that function as pain relievers and create a feeling of comfort in women [10]. Based on previous research, as many as 16 respondents were given warm compresses and EM, the results showed a decrease in the menstrual pain scale from moderate to mild [11]. A single study on PMR and EM was investigated but no study has compared the effectiveness of the two interventions. Thus, this study was conducted to determine the difference in the effectiveness of pain intensity performed by PMR therapy and EM therapy.
2. Methods
The research design was a quasi-experiment with a two-group pretest and posttest design approach. The study was conducted at Senior High School 1 Lasem in September 2022. The population consisted of adolescents aged 13-14 years, and female students at Senior High School 1 Lasem. Respondents were selected using a purposive sampling technique with inclusion and exclusion criteria. Students who experienced dysmenorrhea and do not have a genetic abnormality are the inclusion criteria of this study. After selecting based on the criteria set by the researcher from the entire population, the number of respondents who met the criteria was 80 respondents. We randomly divided 80 respondents into two groups using a computer. Forty respondents received PMR intervention and another 40 respondents received EMT intervention.
The way to measure pain intensity is to use a pain scale instrument called the numeric rating scale (NRS) [12]. The act of PMR and EM using standard operating procedures (SOPs) that have been made, for EM using the concept [13] for PMR using theory [14].
Progressive muscle relaxation (PMR) procedure
Procedures for PMR exist. Forehead, squeeze the forehead muscles and hold for 15 s. Feel the muscles getting tighter then slowly release the tension in the forehead while counting for 30 s.
On the jaw, tighten the muscles in the jaw, hold for 15 s then release the tension slowly while counting for 30 s. For the neck and shoulders, increase tension in the neck and shoulders by lifting the shoulders toward the ears and holding for 15 s. For the arms and hands area, slowly pull both hands into fists. Draw a fist to a chest and hold for 15 s, squeezing as tightly then release slowly and count for 30 s. For the leg area, slowly increase the tension in the quadriceps and calves for 15 s. Tighten the muscles as hard as you can. Then release the tension gently for 30 s. Continue breathing slowly and evenly [9].
Endorphin massage (EM) procedures
Instruct the respondent to take a comfortable position, which can be sitting or lying. Instruct the participant to take a deep breath while closing the eyes and exhaling gently. Meanwhile, the nurse stroked the outer surface of the respondent's arm. Caress gently using the back of the finger, or only fingertips. After about 5 minutes, switch to another hand. This technique is also performed on other parts of the body, incl palms, neck, shoulders, and thighs. Advise the respondent to relax and feel the sensation. Massage is done for 15 minutes [11].
IBM SPSS statistics for Windows, version 20.0 (IBM Corporation, Armonk, NY, USA) was used for archiving and statistical analysis. Univariate analysis was performed on the variable intensity of menstrual pain (dysmenorrhea) before and after the intervention of PMR and EM. Bivariate analysis was performed using the Wilcoxon test due to non-parametric data to analyze the difference in the decrease in the intensity of menstrual pain (dysmenorrhea) which was performed by PMR interventions and EM therapy.
3. Results
The results of the study can be presented with Tables and descriptive descriptions of the characteristics of respondents who experience dysmenorrhea as follows:
Table 1 presents the characteristics of respondents based on a minimum age of 13 years and a maximum age of 14, and an average age of 13.28 years with a standard deviation of 0.66.
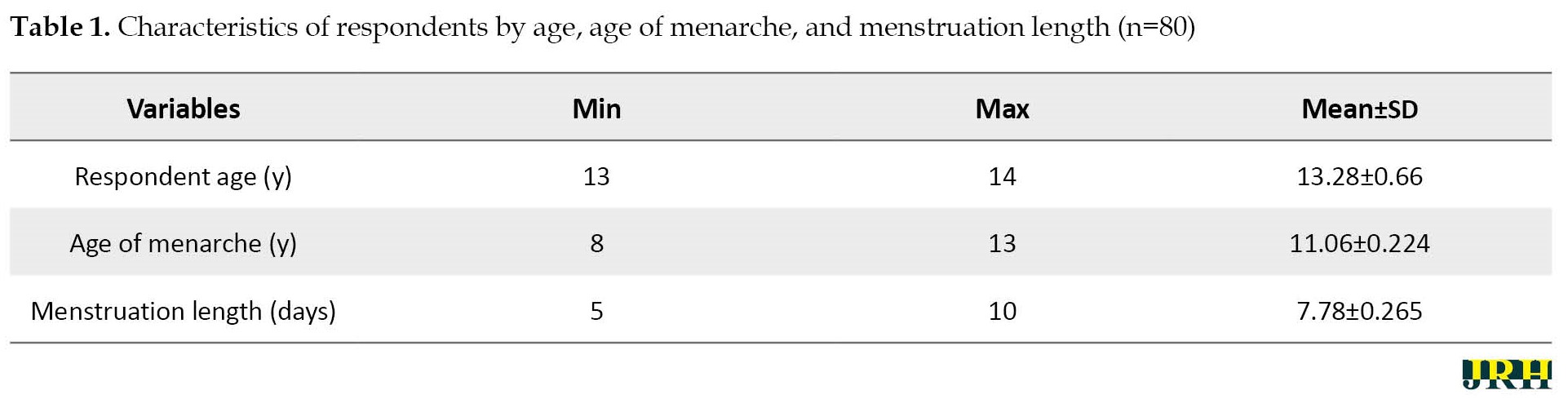
The minimum age of menarche was 8 years and the maximum age was 13, and the average age was 11.06 years with a standard deviation of 0.224. Furthermore, the minimum length of menarche was 5 days, the maximum length of menarche was 10 days, and the average length of menarche was 7.78 years with a standard deviation of 0.265.
Based on Table 2, the respondent’s pain scale before the PMR intervention was a minimum 4, a maximum 6 and the average pain scale was 4.93 with a standard deviation of 0.797, the respondent’s pain scale after the PMR intervention was a minimum 1, a maximum 3, and, the average pain scale was 2.42 with a standard deviation 0.675.
Based on Table 3, the respondent’s pain scale before the EM intervention was a minimum 4, a maximum 6 and the average pain scale was 4.80 with a standard deviation of 0.687, respondent’s pain scale after the PMR intervention was a minimum 1, a maximum 5 and, the average pain scale was 2.90 with a standard deviation of 0.955.
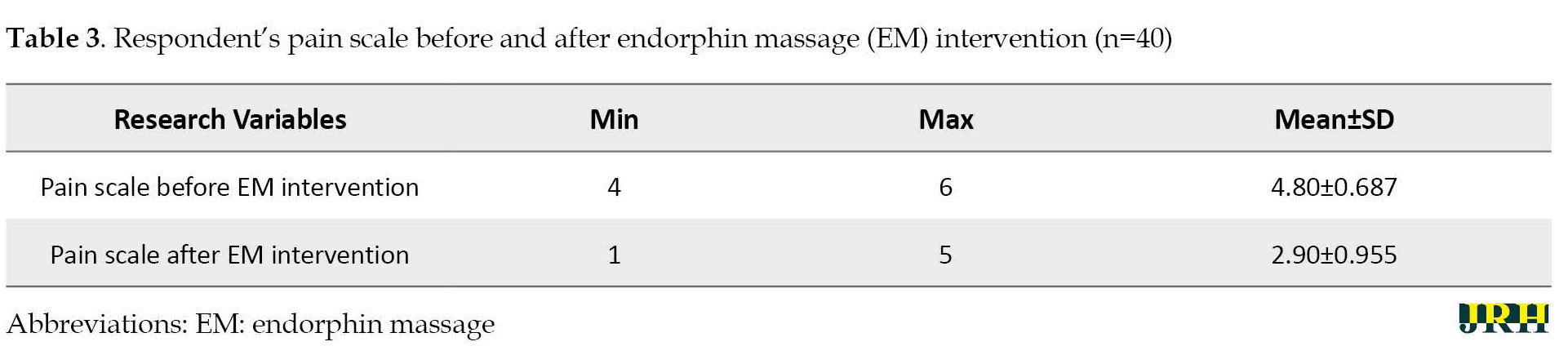
Table 4 presents the average intensity of menstrual pain (dysmenorrhea) after being given PMR intervention with an average pain scale of 2.42±0.675.
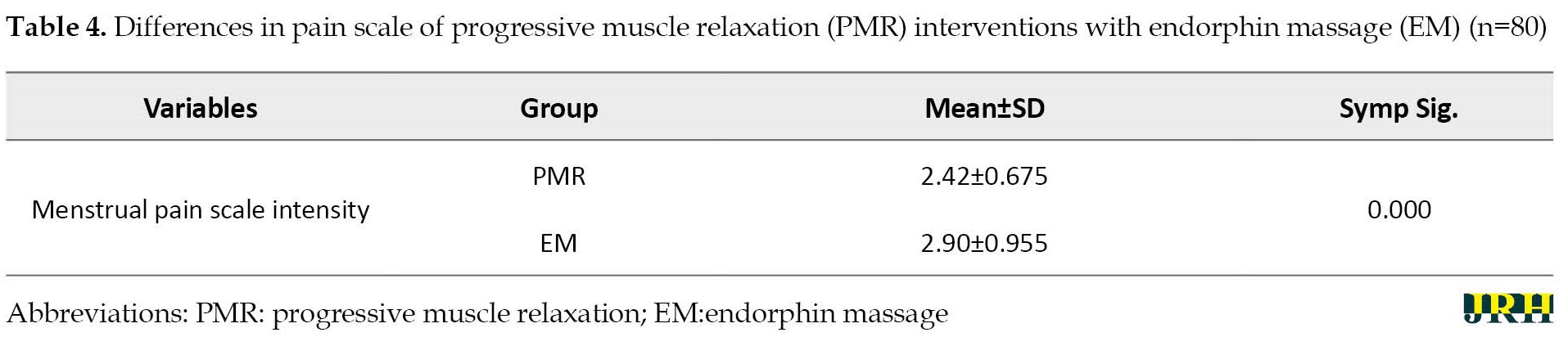
Meanwhile, the average intensity of menstrual pain (dysmenorrhea) after the EM intervention was given with an average pain scale of 2.90 with a standard deviation of 0.955 with a significance level of 0.000.
It can be concluded that the difference in the average intensity of menstrual pain in the intervention and control groups is 4.8 points. Further analysis showed a significant difference in the average pain intensity of menstrual pain in the group that was given the intervention of PMR and EM with a test value of two independent groups (Wilcoxon), the difference in the effectiveness of giving PMR interventions and EM therapy on the intensity of the menstrual pain scale
4. Discussion
The results of the study on the age characteristics of the adolescent respondents of SMP Negeri 1 Lasem as many as 80 respondents showed that the obtained data on the mean age of the respondents was 13.28 years with the youngest age of 13 years and the oldest age of 14 years, with a standard deviation of 0.66. This study showed significant data by the theory of risk factors for dysmenorrhea. Age is one of the prevalent factors in the incidence of dysmenorrhea (menstrual pain) because increasing age affects the response to pain intensity. Menstrual pain occurs due to the dilation of blood vessels due to the sloughing of the epithelial epithelium in the endometrium. Menstrual conditions will stimulate the cervix to dilate, this dilation differs from one woman to another. When a person is in their early teens, they experience menstruation as something new, therefore the cervix is still narrow and then responds with pain, therefore, women in their early teens often experience pain during menstruation compared to late teenage or adult women [15]. In this study, according to WHO, the age of about 13-14 years is still classified as a group of adolescents so that the rate of dysmenorrhea is still high.
The results of the study in terms of the age category of menarche on the respondents obtained data that the mean age of menarche was 11.06 years, the category of the earliest menarche was 8 years, the age of the latest menarche was 13 years, and the standard deviation value was 0.224. First menstruation at an early age of fewer than 11 years [16], at the age of fewer than 11 years, the number of primary ovarian follicles is still in small numbers so that estrogen production is still low [17].
This study contains data that support the theory of risk factors for age at menarche according to the prevalence of dysmenorrhea (menstrual pain). The age of menarche is one of the triggering factors for menstrual pain (dysmenorrhea) due to prolonged exposure to prostaglandins and the occurrence of constriction in the cervix (cervix), resulting in a painful response during menstruation. In adolescents with early menarche, the reproductive organs have not optimally functioned, and also with changes due to the hormones [18].
It has been found that in terms of the category of menstrual duration, the respondents obtained an average menstrual period of 7.78 days, the longest menstrual period was 5 days and the longest period was 10 days with a standard deviation of 0.265. This study is supported by a theory stating that one of the risk factors for dysmenorrhea (menstrual pain) is the abnormal length of menstruation or more than 7 days. From the results of this study, it was found that the average length of menstruation was 7.78, meaning that the length of menstruation was abnormal, which increased in the incidence of menstrual pain. Prolonged causes menstruation contractions of the uterine muscles for a long time so that prostaglandin levels increase, causing menstrual pain. Increased levels of prostaglandins can trigger a pain response during menstruation [19].
Results showed that the average intensity of the menstrual pain scale before PMR was 4.93 with the lowest pain intensity on scale 4 and the highest pain intensity on scale 6, with a standard deviation of 0.151. Meanwhile, after performing PMR, an average of 2.42 was obtained with the lowest pain intensity of scale 1 and the highest pain intensity of scale 3, with a standard deviation of 0.675. The results showed that the mean difference before and after PMR decreased by 2.51 points. This study is supported by the theory that movements in PMR are used to control anxiety or tension when women experience menstruation or dysmenorrhea [20]. Movements in PMR help relax the muscles so that the muscles are relaxed and menstrual pain can be controlled and recognized. Menstrual pain is transmitted by visceral pain impulses originating from the chest and abdominal cavities through sensory nerve fibers that run in the sympathetic nerves and is reduced by PMR interventions that reduce the tension of the muscle fibres, and nerves and reduce pain caused by menstruation. It was further explained that some pain fibers are almost entirely stimulated by excessive mechanical stress or mechanical damage to the tissues referred to as mechanosensitive pain receptors so that PMR interventions can be carried out to reduce excessive mechanical stress.
Results showed that the average intensity of the menstrual pain scale before PMR was 4.93 with the lowest pain intensity on scale 4 and the highest pain intensity on scale 6, with a standard deviation of 0.151. Meanwhile, after performing PMR, an average of 2.42 was obtained with the lowest pain intensity of scale 1 and the highest pain intensity of scale 3, with a standard deviation of 0.675. The results showed that the mean difference before and after PMR decreased by 2.51 points. This study is supported by the theory that movements in PMR are used to control anxiety or tension when women experience menstruation or dysmenorrhea [20]. Movements in PMR help relax the muscles so that the muscles are relaxed and menstrual pain can be controlled and recognized. Menstrual pain is transmitted by visceral pain impulses originating from the chest and abdominal cavities through sensory nerve fibers that run in the sympathetic nerves and is reduced by PMR interventions that reduce the tension of the muscle fibres, and nerves and reduce pain caused by menstruation. It was further explained that some pain fibers are almost entirely stimulated by excessive mechanical stress or mechanical damage to the tissues referred to as mechanosensitive pain receptors so that PMR interventions can be carried out to reduce excessive mechanical stress.
The results showed that the average intensity of the menstrual pain scale before EM therapy was 4.80 with the lowest pain intensity on scale 4 and the highest pain intensity on scale 6, with a standard deviation of 0.687. While after performing PMR, the average was 2.90 with the lowest pain intensity on scale 1 and the highest pain intensity on scale 5, with a standard deviation of 0.955. The results showed that the mean difference before and after EM therapy reduced by 1.90 points. This study is supported by the theory that light touch stimulation on EM can stimulate the release of the beta-endorphin hormone from the body which functions to create a feeling of comfort and relaxation to reduce the body's pain response [21]. EM intervention provides calm and relaxation; therefore the brain secretes endorphins that naturally can reduce pain caused by uterine contractions. Menstrual pain that occurs due to increased prostaglandins in the blood stimulates increased uterine contractions, resulting in decreased blood flow and oxygen to the uterus resulting in ischemia. Pain impulses can be regulated and inhibited by defense mechanisms throughout the central nervous system, pain impulses are transmitted when a barrier is opened and impulses are inhibited when a defense is closed. One way to close this defense is to stimulate the secretion of endorphins, which inhibit the release of pain substances. EM intervention was performed to treat pain to reduce uterine tension via physiological mechanisms, i.e, facilitating blood vessels, inhibiting pain sensations, and providing comfort to the individual. Endorphins are substances associated with pain regulation, functioning as excitation-conducting substances that activate parts of the brain's analgesic system. The release of endorphins into the cerebrospinal fluid of the third ventricle can cause analgesia, thereby inhibiting the delivery of pain impulses to the parietal lobe and reducing pain sensation. Stimulation of nociceptors releases substance P peptide (SP) and peptide associated with the calcitonin gene (CGRP), which increases vascular permeability [22] This neurotransmitter reaches the hypothalamus and midbrain, stimulating the release of endorphins and enkephalins (a neuromodulator) as natural pain controllers.
The results of the study showed that the average intensity of the dysmenorrhea pain scale after PMR intervention was 2.42 with a standard deviation of 0.675. While the average intensity of the dysmenorrhea pain scale after EM intervention was 2.90, with a standard deviation of 0.955. The total number of respondents was 80 respondents. Therefore, it can be concluded that PMR is more effective in reducing the intensity of the dysmenorrhea pain scale in adolescents at SMP Negeri 1 Lasem with an average difference of 4.8 points. This is supported by the concept of a comparative theory of how PMR and EM therapy work as follows:
PMR is more effective in reducing dysmenorrhea pain; this is supported by the theory that the movement in PMR is a combination of deep breath relaxation and muscle relaxation, resulting in a comfortable and relaxed feeling. A series of movements in PMR serves to control tension and anxiety before menstruation and can lower blood pressure [23].
The way EM therapy works is that endorphins are formed from the pituitary gland which is part of the hypothalamus, which is a place to control the hormone system. Several vital hormones exist in the body in dealing with pain, one of which is the beta-endorphin hormone. Beta-endorphin is known as endogenous morphine, which is found in the pituitary gland as morphine, which is naturally released by the human body [24].
Smooth touch stimulation is done at the meridian points to stimulate the process of releasing endorphins. When endorphins are released and flow throughout the body, beta-endorphins receptors act as an analgesic or as a pain reliever and stimulate the brain to create a relaxed feeling [25].
The results of data analysis research showed that the Mann-Whitney test's results were obtained with a Symp Sig. of 0.004 <0.05, the hypothesis was accepted, that is, the effect of providing PMR interventions and endorphin massage therapy on the intensity of the dysmenorrhea (menstrual) pain scale in junior high school adolescents. 1 Lasem. In this study, the concept of PMR and EM is supported.
PMR is a therapy with several movement techniques that work to tighten the muscles and create a relaxed feeling, with movement techniques in PMR can control anxiety and tension before menstruation [20]. While EM therapy is massage with a light touch method to release endorphins from the body as a pain reliever or pain controller by creating a calm and comfortable feeling. EM therapy is mostly used to treat labor pains, postpartum mothers, and breastfeeding mothers [26–28]. This study adds the concept that EM can be used to treat menstrual pain.
In this study, PMR is more effective in dealing with menstrual pain compared to EM because an active process of the respondent to perform muscle relaxant movements coupled with deep breath relaxation exists to provide further increase in muscle relaxation, widen blood vessels, and reduce pain due to spasm or stiffness in muscles. According to Anisa, dysmenorrhea is pain during menstruation caused by uterine muscle spasms [29]. PMR intervention is a series of muscle movements starting from the muscles of the face, hands, arms, neck, chest, abdomen, thighs, and legs. The movement of the performed movements relaxes the muscles coupled with the action of deep breathing in each PMR movement, providing more oxygen in the blood vessels to inhibit and reduce painful stimuli and painful nerve impulses leading to the hypothalamus.
5. Conclusion
Data analysis obtained a Symp Sig. of 0.004 <0.05, therefore a difference is observed in the effectiveness of providing PMR intervention and EM therapy on the intensity of the menstrual pain scale. Menstrual pain can be reduced by blocking nerve impulses from reaching the brain, among others, by providing PMR therapy to control tension and anxiety. In conclusion, PMR therapy is more effective to control menstrual pain compared to EM. It is recommended that PMR therapy can be done by themselves in case of menstrual pain. The limitation of this study was the small samples. More samples are needed in future studies.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from Research Ethics Committee Muhammadiyah University, Semarang on March 18, 2022 (IRB No.: INA/041/2022). The researcher asked the principal for approval if agreed, the child signed the informed consent.
Funding
This study was funded by Muhammadiyah University, Semarang, Indonesia.
Authors' contributions
Conceptualizing, designing, and writing the first draft and framework: Pawestri Pawestri; Interpreting the data, and supervising: Machmudah Machmudah, Sri Rejeki; Collecting the data: Savira Ayu Nur Fitria, Medina Laila Fitri, Reina Dhamanik; Interpreting the data, as well as evaluating the data: Satriya Pranata, Nikmatul Khayati; The published version of the manuscript has been read and approved by all authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We thank the participants and any parties who contribute to this study
References
- Rejeki S, Pratama FY, Ernawati E, Yanto A. Abdominal stretching as a therapy for dysmenorrhea. Open Access Macedonian Journal of Medical Sciences. 2021; 9(G):180-3. [DOI:10.3889/oamjms.2021.6711]
- Abreu-Sánchez A, Parra-Fernández ML, Onieva-Zafra MD, Fernández-Martínez E. Perception of menstrual normality and abnormality in spanish female nursing students. International Journal of Environmental Research and Public Health. 2020; 17(17):6432. [DOI:10.3390/ijerph17176432] [PMID] [PMCID]
- Bernardi M, Lazzeri L, Perelli F, Reis FM, Petraglia F. Dysmenorrhea and related disorders. F1000Research. 2017; 6:1645. [DOI:10.12688/f1000research.11682.1] [PMID] [PMCID]
- Rejeki S, Solichan A, MacHmudah, Safitri DNRP, Poddar S. The profile of interleukin-6, pge2, and menstrual pain levels through the counterpressure regiosacralis therapy. European Journal of Molecular & Clinical Medicine. 2020; 7(6):122-8. [Link]
- Putri NE, Wilson, Putri EA. [The relation of emotional regulation with intensity of menstrual pain (dysmenorrhea) in students of smpn 8 pontianak (Indonesian)]. Jurnal Nasional Ilmu Kesehatan. 2019; 3(2):51-61. [Link]
- Murniati M, Sundari RI, Dewi FK. [Pelatihan relaksaasi otot progresif pada kader posyandu lansia di posyandu lansia RW 05 Desa kalibagor (Indonesian)]. Journal of Community Engagement in Health. 2020; 3(1):74-81. [DOI:10.30994/jceh.v3i1.39]
- Nurrianingsih P, Nurhidayati E. Pengaruh teknik relaksasi terhadap tingkat dismenorea pada siswi sma muhammadiyah 3 yogyakarta (Indonesian) [PhD. Thesis]. Yogyakarta: Aisyiyah University; 2015. [Link]
- Wati YS, Ardini YD. [Efektivitas pemberian aroma terapi lavenderdan massage effleurage terhadap penurunan nyeri menstruasi pada remaja putri di sman 10 pekanbaru (Indonesian)]. Journal of Midwifery Science. 2021; 5(1):42-51. [DOI:10.36341/jomis.v5i1.1445]
- Fitriani H, Achmad A. Perbedaan efektivitas relaksasi otot progresif dan hipnoterapi terhadap disminore primer pada remaja (Indonesian)]. Jurnal Keperawatan BSI. 2017; 5(2):89-95. [Link]
- Kuswandi L. Hypnobirthing a gentle way to give birth. Jakarta: Pustaka Bunda; 2014. [Link]
- Nurhayati N, Akbar N. [Pengaruh Pemberian kompres hangat dan endorphine massage terhadap kejadian dismenorhoe remaja (Indonesian)]. Jurnal Penelitian Kesehatan. 12(1):50-3. [DOI:10.33846/sf12113]
- Rotin M. [Dismenorea cara mudah mengatasi nyeri haid (Indonesian)]. Yogyakarta: Dialektika; 2018. [Link]
- Ramadhani IP. [Penurunan skala nyeri dismenorea dengan pijat endorphine pada mahasiswa stikes alifah yang mengalami dismenorea (Indonesian)]. Jurnal Ilmu Kesehatan. 2019; 4(1):9-13. [DOI:10.33757/jik.v4i1.253]
- Toussaint L, Nguyen QA, Roettger C, Dixon K, Offenbächer M, Kohls N, et al. Effectiveness of progressive muscle relaxation, deep breathing, and guided imagery in promoting psychological and physiological states of relaxation. Evidence-Based Complementary and Alternative Medicine. 2021; 2021:5924040. [PMID]
- Sari AP, Usman A. [Efektifitas terapi akupresur terhadap dismenore pada remaja (Indonesian)]. Jurnal Kedokt teran Dan Kesehatan. 2021; 17(2):196-202. [DOI:10.24853/jkk.17.2.196-202]
- Khayati YN, Veftisia V, Widyaningsih A, Windayanti H, Dewi MK, Hidayanti N, et al. [Peningkatan pengetahuan remaja putri tentang penanganan disminore primer (Indonesian)]. Indonesian Journal of Community Empowerment. 2021; 3(1):20. [DOI:10.35473/ijce.v3i1.964]
- Chon SJ, Umair Z, Yoon MS. Premature ovarian insufficiency: Past, present, and future. Frontiers in Cell and Developmental Biology. 2021; 9:672890. [PMID]
- Wulanda C, Luthfi A, Hidayat R. [Efektifitas senam disminore pada pagi dan sore hari terhadap penanganan nyeri haid pada remaja putri saat haid di smpn 2 bangkinang Kota Thun 2019 (Indonesian)]. Jurnal Kesehatan Tambusai. 2020; 1(1):1-1. [Link]
- Hermawahyuni R, Handayani S, Darmawansyah Alnur R. Risk factors of primary dysmenorrhea in students of SMK PGRI 1 Jakarta Timur. Journal of Community Health. 2022; 8(1):97-101. [DOI:10.25311/keskom.Vol8.Iss1.1079]
- Rahmawati PM, Musviro M, Deviantony F. [Efektifitas progressive muscle relaxation (PMR) terhadap penurunan tekanan darah pada penderita hipertensi (Indonesian)]. The Indonesian Journal Health Science. 2018; 188-93. [DOI:10.32528/ijhs.v0i0.1547]
- Elvira M, Tulkhair A. [Pengaruh pijat endorphine terhadap skala nyeri pada siswi sma yang mengalami disminore (Indonesian)]. Jurnal Iptek Terapan. 2018; 12(2):155-66. [DOI:10.22216/jit.2018.v12i2.1542]
- Bahrudin M. Pathophysiology of pain. Saintika Medika. 2018; 13(1):7-13. [DOI:10.22219/sm.v13i1.5449]
- Kristina C, Hasanah O, Zukhra RM. [Perbandingan teknik relaksasi otot progresif dan akupresur terhadap dismenore pada mahasiswi FKP universitas Riau (Indonesian)]. Health Care: Journal Kesehatan 2021; 10(1):104-14. [DOI:10.36763/healthcare.v10i1.96]
- Cahyani IA, Winarsih S, Arfiana A. The effect of endorphin massage towards decreasing low back pain in third trimester pregnant women. Midwifery and Nursing Research. 2020; 2(1):41–5. [Link]
- Afiyah RK. Effectiveness of endorphin massage against anxiety the face of labor on mother primigravida in the region of Clinics Jagir Surabaya. Proceeding Surabaya International Heal Conference. 2017; 1(1):317–24.
- FitrianaF, Putri NA. [Pengaruh pijat endorphin (endorphin massage) terhadap intensitas nyeri kala I pada ibu primipara (Indonesian)]. Jurnal Ilmian Keperawatan Sai Betik. 2017; 13(1):31-4. [DOI:10.26630/jkep.v13i1.847]
- Septianingrum Y, Hatmanti NM. [Pengaruh endorphin massage terhadap nyeri haid mahasiswi tingkat akhir s1 keperawatan universitas Nahdlatul Ulama Surabaya (Indonesian)]. Jurnal Keperawatan Muhammadiyah. 2019; 4(2):187-92. [DOI:10.30651/jkm.v4i2.3192]
- Yesie A. [Bebastakut hamil dan melahirkan (Indonesian)]. Jakarta: Gramedia Pustaka Utama; 2017. [Link]
- Anisa MV. [The effect of exercises on primary dysmenorrhea (Indonesian)]. Medical Journal of Lampung University. 2015; 4(2):60-5. [Link]
Type of Study: Orginal Article |
Subject:
● Service Quality
Received: 2023/01/8 | Accepted: 2023/03/11 | Published: 2023/06/29
Received: 2023/01/8 | Accepted: 2023/03/11 | Published: 2023/06/29
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






