Volume 13, Issue 4 (Jul & Aug 2023)
J Research Health 2023, 13(4): 255-262 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kalpana L, Panda S. Effectiveness of Cognitive Behavior Therapy on Depression and Quality of Life in Spouse Caregivers of Inpatients With Substance Use Disorders. J Research Health 2023; 13 (4) :255-262
URL: http://jrh.gmu.ac.ir/article-1-2240-en.html
URL: http://jrh.gmu.ac.ir/article-1-2240-en.html
1- Department of Psychology, Sikkim University, Gangtok (Sikkim), India. , kalpanalangkham@gmail.com
2- Department of Psychology, Sikkim University, Gangtok (Sikkim), India.
2- Department of Psychology, Sikkim University, Gangtok (Sikkim), India.
Full-Text [PDF 514 kb]
(1174 Downloads)
| Abstract (HTML) (3072 Views)
Full-Text: (1028 Views)
1. Introduction
In India, a significant portion of the population suffers from substance use disorders. All demographic groups use drugs; however, adult men in India are the group most affected by substance use disorders. Undoubtedly, substance use problems constitute a serious public health issue in the nation [1]. Substance use disorders have a significant impact on family members in many ways. This may be more relevant in countries with close-knit families, such as India. In the process of treating substance use disorders, family members also play a critical social support role that must be recognized and valued. The impact of substance use disorders on the family and the part played by the family in seeking treatment can both be impacted by recent changes in societal structures [2]. Substance dependence not only adversely affects the social and economic well-being of the drug- or alcohol-dependent individual but also has
a hurtful and adverse effect on the psychosocial health of the family. The disorders caused by dependents are a problem for people and a threat to society. Dependent people in the family negatively affect their psychological well-being and increase their risk of depression.
It can negatively affect a person’s quality of life (QoL), particularly for wives whose husbands are substance dependent. A person’s perspective of their situation in life concerning their objectives, aspirations, standards, and worries is what is referred to as their QoL. As a result, a wide range of physical, psychological, environmental, and social factors make up the QoL. Therefore, this phenomenon can be considered one of the vital and complex social issues in the world.
Depression is one of the most common mental disorders, and typical symptoms of depression are a low mood, a loss of interest or pleasure, and a drop in energy in daily activities. In 2017, more than 300 million people were estimated to suffer from depression, equivalent to 4.4% of the population. It is a leading cause of disability worldwide and a major contributor to the overall global burden of diseases. The risk of depression increases with poor socioeconomic conditions, unemployment, traumatic life events, such as the death of a loved one or divorce, chronic medical illness, and issues related to substance dependence. Even though depression affects individuals of all ages and genders, the prevalence of depression is higher among women than among men. Severe depression can be continuous or recurrent, with severe cases significantly diminishing an individual’s ability to function at a job or cope with daily life activities. Depression can lead to suicide if it is chronic [3].
Cognitive therapy (CT) is an active, short-term, present-oriented, structured approach used to treat depression and other mental disorders. According to Beck’s cognitive theory of depression, depression is a pathological disorder in which an individual’s affect and behaviour are largely determined by how that individual interprets the world. Individuals’ cognitions (verbal or pictorial “events” in the stream of consciousness) are based on attitudes or assumptions (schemas), developed from previous experiences. A psychotherapist helps in solving present problems and altering maladaptive (faulty and or inappropriate) thinking and behavior. Cognitive conceptualization of psychopathology and the therapeutic change process is the defining characteristic of cognitive behavior therapy (CBT). Pharmacotherapy and CBT are the most commonly used and empirically supported treatments for depressive disorders. Several studies revealed that CBT is more effective than the control, pharmacotherapy alone, and nonspecific treatments, and it is equally effective compared to other psychological interventions in different populations. For example, CBT and pharmacotherapy have demonstrated superiority in reducing symptoms relative to other interventions and waitlist conditions [4]. Experimental studies have shown that CBT is effective in reducing the carer burden in drug addiction [5].
The husband’s substance dependence exposes the wife’s mental health to risk. A negative correlation was observed between the poor QoL among wives and the severity and duration of alcohol dependence in husbands across all four domains of QoL [6]. Mindfulness training may be particularly beneficial for the quality of the marital relationship and psychological well-being among women with substance dependence [7]. The prevalence of depression and anxiety in women with a drug-dependent husband is also high [8]. Similarly, spouses of alcohol-dependent men experience higher rates of common mental disorders, low marital satisfaction, and poor well-being [9, 10, 11, 12, 13]. Mood disorders, anxiety disorders, and stress-related disorders are the most common psychiatric morbidities [14, 15, 16]. Women’s negative experiences with substance-dependent spouses make them extremely vulnerable to a variety of psychological and social problems [17]. Moreover, substance dependence affects the family in different ways, stress, financial constraint, stigma, psychiatric symptoms, conflicts, and caregiving burden [18]. According to earlier studies on the negative effects of addiction, addiction has a high psychiatric comorbidity rate in the wife. Poor QoL is always one of the effects of substance abuse disorders in the family. Several studies have separately examined the effects of CBT on QoL and depression. Based on the literature review above, a gap exists in evaluating the effectiveness of CBT on depression and QoL in the wife of a husband with substance use disorders. As a result, this study was conducted to examine the effect of cognitive-behavioral intervention in treating depression and improving the QoL in spouse caregivers.
2. Methods
The study was quasi-experimental, and a pre-test and post-test with a control group. The sample of the study included 60 spouse carers of inpatients with substance use disorders treated at the Regional Institute of Medical Sciences (RIMS), Department of Psychiatry, Lamphelpat, Imphal West, Manipur, in 2022. A purposive sampling method was used to select the sample [18]. The protocol of this study was approved by the 11th Institutional Ethical Committee of Sikkim University (No. SU/REG/F-1/03/2019/Vol-II/891). Inclusion criteria included aged 19 years or older and being the wife of an inpatient with substance use disorders who completed a treatment consent form. The exclusion criteria included participants suffering from chronic disease or mental illness or co-dependent on substances and with previous and concurrent psychotherapy experience. In this study, to apply the independent variable, the experimental group received eight sessions over the course of two months for the thirty experimental groups, which lasted from 45 to 60 minutes for each participant, and each mindful breathing exercise session lasted five minutes, while the control group did not. A pre-test of the depression, anxiety, and stress scale (DASS-21) and the World Health Organization Quality of Life-BREF (WHOQoL-BREF) were administered before CBT intervention. After the CBT intervention, DASS-21 and WHOQoL-BREF were re-administered. The results of each experimental group were compared to the control group. To comply with ethical considerations, the control group received a session of CBT at the end of the intervention.
The following tools are used to collect data:
Depression, anxiety, and stress scale-21 (DASS-21)
Lovibond and Lovibond in 1995 developed a 21-item measure of depression, anxiety, and stress used to screen for depression. It is a set of three self-report scales intended to measure the emotional states of depression, anxiety, and stress. Each index consists of 7 items. A 4-point Likert scale from zero to three. Scores for depression, anxiety, and stress were multiplied by two to calculate the final score. Total scores for each indicator ranged from 0 to 42, with higher scores indicating a higher level of psychological distress. The depressive levels were defined as normal: 0–9, mild: 10–13, moderate: 14–20, severe: 21–27, and extremely severe: > 27. The DASS-21 demonstrated high internal consistency and test-retest reliability scores of 0.89 and 0.96, respectively, as well as criterion validity and construct validity [19].
The World Health Organization Quality of Life- BREF (WHOQoL-BREF)
The World Health Organization group in 1995 developed the WHOQoL-BREF. It contains 26 items and a self-report questionnaire assessing four domains of QoL, physical health, psychological health, social relationships, and environment. In addition, two items are examined separately, question 1 asks about an individual’s overall perception of QoL, and question 2 asks about an individual’s overall perception of their health, which measures QoL and health. The four domain scores are scaled in a positive direction (i.e. higher scores denote a higher QoL). WHOQoL-BREF domain scores demonstrated good content validity, discriminant validity, and internal consistency for domains, 0.80 for physical health, 0.76 for psychological, 0.66 for social relationships, and 0.83 for environment. The test–retest reliability for domains was 0.66 for physical health, 0.72 for psychological, 0.76 for social relationships, and 0.87 for the environment [20].
In the present study, the goal of the researchers was to administer CBT. To achieve the goal, Beck’s CBT model was used. The intervention programme was run by the present researcher, who is a licensed clinical psychologist.
The content of the CBT programme was as follows:
Session 1: Introduction and education on the impact of substance use disorders on family members; discussion on depression and QoL; psychoeducation on the role of CBT and the mindful breathing exercise model in the treatment of depression and their potential benefits for well-being.
Session 2: Mindful breathing exercise examines the client’s meaning system in a collaborative style, which is a better approach that clients can enforce both during and after therapy. To help the client recognize the salient connections between thinking, feeling, and behaving to their challenges, usually through obtaining real-life examples.
Session 3: Examine or explore the evidence for their beliefs and assumptions based on their behavioral experiments.
Session 4: Help the client recognize perceptual attention leading to impractical interpretation. Impart the cognitive model in a way inferring that the client is thinking inadequately rather than “irrationally”.
Session 5: Guiding discovery: To help the client discover useful information that can be used to help gain a better level of understanding (and to help the client adopt this strategy for themselves as the basis for exploring their own beliefs).
Session 6: Identifying and noting central cognitions (involuntary thoughts or pictures). Assist the client in acquiring alternative explanations to issues focused on assisting the client in reconceptualizing their problems (i.e. by analyzing the validity of specific thoughts and central beliefs that engage in each circumstance). Record dysfunctional thinking and reactions to these thoughts to help clients learn to self-appraise evidence and generate alternative interpretations.
Session 7: Identification and modification of dysfunctional assumptions (“intermediate beliefs”). Help the client apply and test out new methods using homework. Behavioral activation: an activity schedule.
Session 8: Closing therapy and encouraging the client to shield against relapse. The client learned how to become a therapist.
The current study compared the efficacy of CBT intervention on depression and QoL in women with substance use disorders to a control group.
Statistical analyses
The collected data were analyzed using multivariate analysis of covariance (MANCOVA) with SPSS software, version 26. In statistical tests, the significance level was 0.05.
3. Results
The percentage of young adults in the experiment group was 46.67%, while the percentage of old adults was 3.33%. In the control group, young adults made up 41.67% of the population, while old adults made up 8.33%.
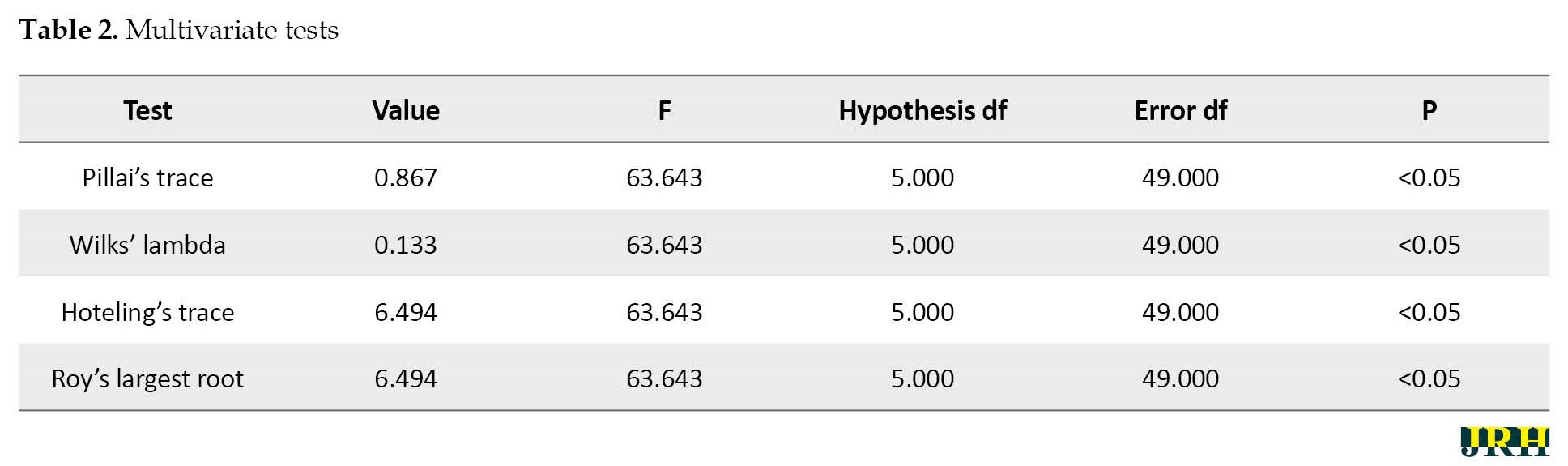
Table 1 presents the descriptive information of the variables; Tables 2 and 3 present the pre and post-test, which represent the treatment efficacy of the cognitive behavior intervention.
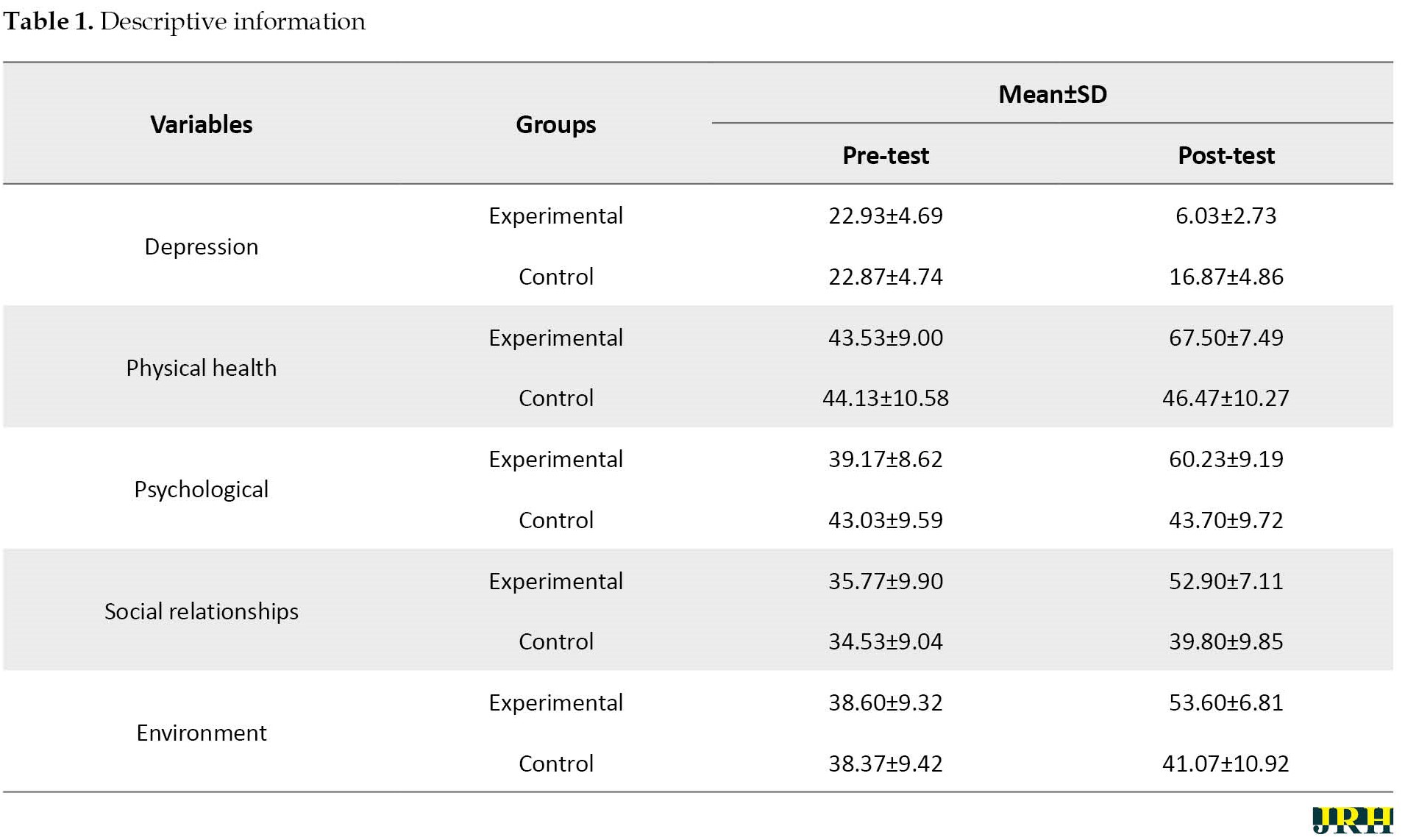

Before the intervention, no discernible variations existed in the participants’ characteristics between the experimental and control groups. As can be seen in Table 1 above, the mean scores in the control group showed little difference, but the difference is visible in the experimental group. Levine’s test was used to observe the assumptions of the covariance. Depression (F=5.95, P=0.018), physical health domain (F=7.96, P=0.007), psychological domain (F=15.69, P=0.007), social relationships (F=7.94, P=0.007), and environment domain (F=1.13, P=0.29) and error variances do not differ between participants (experimental and control group), and variances are equal. Box’s M test was used to study the homogeneity of the covariance. The results showed that Box’s M was significant, establishing the assumption of a difference in covariance (F=2.75, P=0.00). Tables 2 and 3 present the results of the multivariate analysis of covariance (MANCOVA).
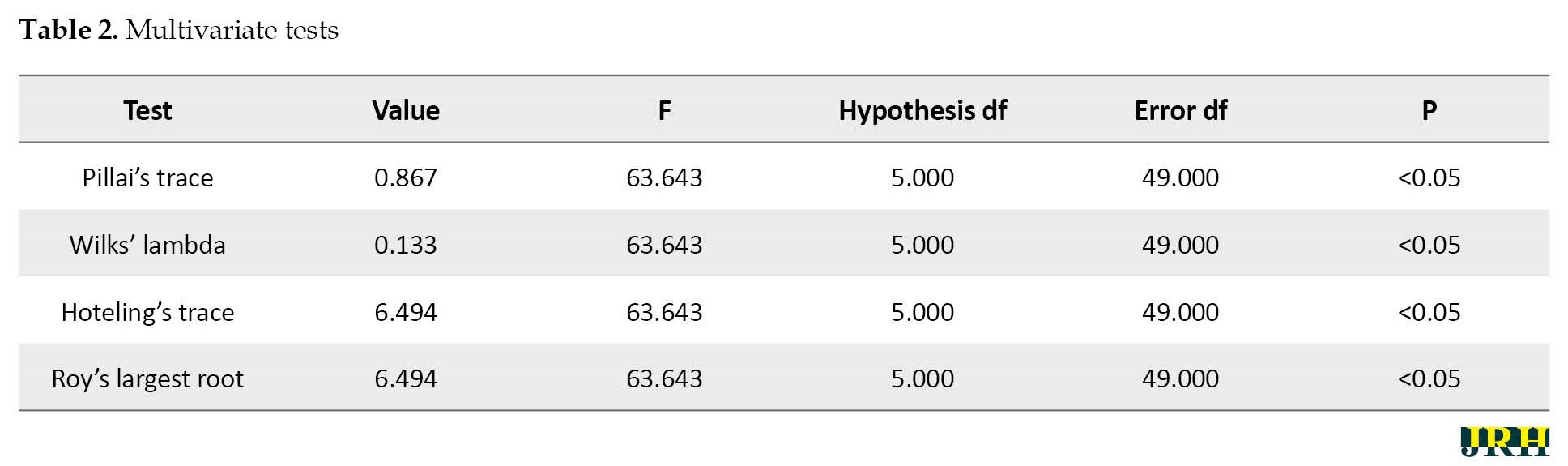
Table 2 presents that at a significance level of 0.05, the observed F for Pillai’s trace, Wilks’ lambda, Hoteling’s trace, and Roy’s largest root is 63.643. This means that a significant difference is observed at least in one of the comparable variables between the two groups.
The findings showed a significant difference between the groups in four areas of QoL, including physical, psychological, social relationship, and environmental domains, as well as in terms of depression. This indicates that the experimental group experiences better results in the physical (F=78.13, P<0.05), psychological (F=65.68, P<0.05), social relationship (F=46.69, P<0.05), and environment (F=58.59, P<0.05) domains compared to the control group. Regarding the size of the effect, it can be concluded that the cognitive behavioral intervention had the most positive effects on depression and QoL.
4. Discussion
The current research indicates that CBT considerably reduces depression and enhances QoL. These results, which were consistent with the results of other studies, demonstrated that cognitive behavior intervention can reduce depression [5]. Several studies have found that cognitive-behavioral interventions reduce carer burden in drug-addicted people [6], improve the QoL in the wives of alcohol dependence syndrome patients [7], and reduce depression, anxiety, and stress in family carers [21, 22]. In addition, other studies have shown that mindfulness interventions have also had a significant impact on reducing marital issues and improving the psychosocial well-being of addicted women [8, 23]. The present study’s results suggest cognitive behavior intervention, which helps the client recognize the salient connections between thinking, feeling, motivation, and behaviour to their challenges, usually through obtaining real-life examples. One of the crucial features of a CBT intervention is that participants can examine or explore the evidence for their beliefs and assumptions based on their behavioral experiments. The typical stress and reactions to challenging situations, alternate attitudes and emotions, and helpful information supplied are all crucial abilities that individuals have gained via cognitive behaviour therapies, such as mindful breathing exercises. Practicing mindfulness through behaviour activities enables one to maintain the present moment by avoiding ruminations. The exercises were carried over into daily life, and the individual realized that when confronted with unpleasant events, such as a spouse’s drug or alcohol problems, she should choose proactive behaviours rather than reactive ones, which usually result in sadness, disappointment, and stress. In addition, this helps women adapt to and efficiently deal with the current situation, which is challenging and unpleasant. Moreover, planning to do pleasant activities helps women activate behaviors that increase enjoyment and well-being. In addition, this helps women adapt to and efficiently deal with the current situation, which is challenging and unpleasant. Moreover, planning pleasurable activities helps women activate those behaviors that increase enjoyment and well-being.
5. Conclusion
The results of this study indicated the importance of cognitive behavior intervention in reducing depression and improving the QoL of married women with substance use disorders. They are vulnerable in terms of common mental health issues, such as depression and QoL. Participants learned adaptive thinking processes and positive appraisals of life events. This skill leads to improved experience, recognition of one’s cognitive activity and behavior, positive problem-solving of the situation, and the application and consolidation of new skills and strategies in therapy sessions to generalize them across situations. As a result, they can foster the ability to make healthy coping strategies, and they are better able to deal with the situation.
Limitations and Implications
A main weakness of the study was that the sample was exclusively drawn from female spouses who were primary carers for male inpatients seeking treatment at a tertiary care hospital and therefore maybe not typical of the general community.
To minimize psychological issues and enhance the health of this underserved population, the current study emphasizes the importance of recognizing the needs of spouse carers and giving aid as soon as practical. This study also emphasizes the necessity for further investigation using various culturally appropriate therapy in various settings.
Ethical Considerations
Compliance with ethical guidelines
The protocol of this study was approved by the 11th Institutional Ethical Committee of Sikkim University (No. SU/REG/F-1/03/2019/Vol-II/891). A written and fully informed consent form was obtained from the participants. Also, privacy was maintained and the data of the participants was anonymized to maintain confidentiality.
Funding
The paper was extracted from the doctoral thesis of Langkham Kalpana, Department of Psychology, Sikkim University, Gangtok (Sikkim), India.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We appreciate the women who took part in this study.
References
In India, a significant portion of the population suffers from substance use disorders. All demographic groups use drugs; however, adult men in India are the group most affected by substance use disorders. Undoubtedly, substance use problems constitute a serious public health issue in the nation [1]. Substance use disorders have a significant impact on family members in many ways. This may be more relevant in countries with close-knit families, such as India. In the process of treating substance use disorders, family members also play a critical social support role that must be recognized and valued. The impact of substance use disorders on the family and the part played by the family in seeking treatment can both be impacted by recent changes in societal structures [2]. Substance dependence not only adversely affects the social and economic well-being of the drug- or alcohol-dependent individual but also has
a hurtful and adverse effect on the psychosocial health of the family. The disorders caused by dependents are a problem for people and a threat to society. Dependent people in the family negatively affect their psychological well-being and increase their risk of depression.
It can negatively affect a person’s quality of life (QoL), particularly for wives whose husbands are substance dependent. A person’s perspective of their situation in life concerning their objectives, aspirations, standards, and worries is what is referred to as their QoL. As a result, a wide range of physical, psychological, environmental, and social factors make up the QoL. Therefore, this phenomenon can be considered one of the vital and complex social issues in the world.
Depression is one of the most common mental disorders, and typical symptoms of depression are a low mood, a loss of interest or pleasure, and a drop in energy in daily activities. In 2017, more than 300 million people were estimated to suffer from depression, equivalent to 4.4% of the population. It is a leading cause of disability worldwide and a major contributor to the overall global burden of diseases. The risk of depression increases with poor socioeconomic conditions, unemployment, traumatic life events, such as the death of a loved one or divorce, chronic medical illness, and issues related to substance dependence. Even though depression affects individuals of all ages and genders, the prevalence of depression is higher among women than among men. Severe depression can be continuous or recurrent, with severe cases significantly diminishing an individual’s ability to function at a job or cope with daily life activities. Depression can lead to suicide if it is chronic [3].
Cognitive therapy (CT) is an active, short-term, present-oriented, structured approach used to treat depression and other mental disorders. According to Beck’s cognitive theory of depression, depression is a pathological disorder in which an individual’s affect and behaviour are largely determined by how that individual interprets the world. Individuals’ cognitions (verbal or pictorial “events” in the stream of consciousness) are based on attitudes or assumptions (schemas), developed from previous experiences. A psychotherapist helps in solving present problems and altering maladaptive (faulty and or inappropriate) thinking and behavior. Cognitive conceptualization of psychopathology and the therapeutic change process is the defining characteristic of cognitive behavior therapy (CBT). Pharmacotherapy and CBT are the most commonly used and empirically supported treatments for depressive disorders. Several studies revealed that CBT is more effective than the control, pharmacotherapy alone, and nonspecific treatments, and it is equally effective compared to other psychological interventions in different populations. For example, CBT and pharmacotherapy have demonstrated superiority in reducing symptoms relative to other interventions and waitlist conditions [4]. Experimental studies have shown that CBT is effective in reducing the carer burden in drug addiction [5].
The husband’s substance dependence exposes the wife’s mental health to risk. A negative correlation was observed between the poor QoL among wives and the severity and duration of alcohol dependence in husbands across all four domains of QoL [6]. Mindfulness training may be particularly beneficial for the quality of the marital relationship and psychological well-being among women with substance dependence [7]. The prevalence of depression and anxiety in women with a drug-dependent husband is also high [8]. Similarly, spouses of alcohol-dependent men experience higher rates of common mental disorders, low marital satisfaction, and poor well-being [9, 10, 11, 12, 13]. Mood disorders, anxiety disorders, and stress-related disorders are the most common psychiatric morbidities [14, 15, 16]. Women’s negative experiences with substance-dependent spouses make them extremely vulnerable to a variety of psychological and social problems [17]. Moreover, substance dependence affects the family in different ways, stress, financial constraint, stigma, psychiatric symptoms, conflicts, and caregiving burden [18]. According to earlier studies on the negative effects of addiction, addiction has a high psychiatric comorbidity rate in the wife. Poor QoL is always one of the effects of substance abuse disorders in the family. Several studies have separately examined the effects of CBT on QoL and depression. Based on the literature review above, a gap exists in evaluating the effectiveness of CBT on depression and QoL in the wife of a husband with substance use disorders. As a result, this study was conducted to examine the effect of cognitive-behavioral intervention in treating depression and improving the QoL in spouse caregivers.
2. Methods
The study was quasi-experimental, and a pre-test and post-test with a control group. The sample of the study included 60 spouse carers of inpatients with substance use disorders treated at the Regional Institute of Medical Sciences (RIMS), Department of Psychiatry, Lamphelpat, Imphal West, Manipur, in 2022. A purposive sampling method was used to select the sample [18]. The protocol of this study was approved by the 11th Institutional Ethical Committee of Sikkim University (No. SU/REG/F-1/03/2019/Vol-II/891). Inclusion criteria included aged 19 years or older and being the wife of an inpatient with substance use disorders who completed a treatment consent form. The exclusion criteria included participants suffering from chronic disease or mental illness or co-dependent on substances and with previous and concurrent psychotherapy experience. In this study, to apply the independent variable, the experimental group received eight sessions over the course of two months for the thirty experimental groups, which lasted from 45 to 60 minutes for each participant, and each mindful breathing exercise session lasted five minutes, while the control group did not. A pre-test of the depression, anxiety, and stress scale (DASS-21) and the World Health Organization Quality of Life-BREF (WHOQoL-BREF) were administered before CBT intervention. After the CBT intervention, DASS-21 and WHOQoL-BREF were re-administered. The results of each experimental group were compared to the control group. To comply with ethical considerations, the control group received a session of CBT at the end of the intervention.
The following tools are used to collect data:
Depression, anxiety, and stress scale-21 (DASS-21)
Lovibond and Lovibond in 1995 developed a 21-item measure of depression, anxiety, and stress used to screen for depression. It is a set of three self-report scales intended to measure the emotional states of depression, anxiety, and stress. Each index consists of 7 items. A 4-point Likert scale from zero to three. Scores for depression, anxiety, and stress were multiplied by two to calculate the final score. Total scores for each indicator ranged from 0 to 42, with higher scores indicating a higher level of psychological distress. The depressive levels were defined as normal: 0–9, mild: 10–13, moderate: 14–20, severe: 21–27, and extremely severe: > 27. The DASS-21 demonstrated high internal consistency and test-retest reliability scores of 0.89 and 0.96, respectively, as well as criterion validity and construct validity [19].
The World Health Organization Quality of Life- BREF (WHOQoL-BREF)
The World Health Organization group in 1995 developed the WHOQoL-BREF. It contains 26 items and a self-report questionnaire assessing four domains of QoL, physical health, psychological health, social relationships, and environment. In addition, two items are examined separately, question 1 asks about an individual’s overall perception of QoL, and question 2 asks about an individual’s overall perception of their health, which measures QoL and health. The four domain scores are scaled in a positive direction (i.e. higher scores denote a higher QoL). WHOQoL-BREF domain scores demonstrated good content validity, discriminant validity, and internal consistency for domains, 0.80 for physical health, 0.76 for psychological, 0.66 for social relationships, and 0.83 for environment. The test–retest reliability for domains was 0.66 for physical health, 0.72 for psychological, 0.76 for social relationships, and 0.87 for the environment [20].
In the present study, the goal of the researchers was to administer CBT. To achieve the goal, Beck’s CBT model was used. The intervention programme was run by the present researcher, who is a licensed clinical psychologist.
The content of the CBT programme was as follows:
Session 1: Introduction and education on the impact of substance use disorders on family members; discussion on depression and QoL; psychoeducation on the role of CBT and the mindful breathing exercise model in the treatment of depression and their potential benefits for well-being.
Session 2: Mindful breathing exercise examines the client’s meaning system in a collaborative style, which is a better approach that clients can enforce both during and after therapy. To help the client recognize the salient connections between thinking, feeling, and behaving to their challenges, usually through obtaining real-life examples.
Session 3: Examine or explore the evidence for their beliefs and assumptions based on their behavioral experiments.
Session 4: Help the client recognize perceptual attention leading to impractical interpretation. Impart the cognitive model in a way inferring that the client is thinking inadequately rather than “irrationally”.
Session 5: Guiding discovery: To help the client discover useful information that can be used to help gain a better level of understanding (and to help the client adopt this strategy for themselves as the basis for exploring their own beliefs).
Session 6: Identifying and noting central cognitions (involuntary thoughts or pictures). Assist the client in acquiring alternative explanations to issues focused on assisting the client in reconceptualizing their problems (i.e. by analyzing the validity of specific thoughts and central beliefs that engage in each circumstance). Record dysfunctional thinking and reactions to these thoughts to help clients learn to self-appraise evidence and generate alternative interpretations.
Session 7: Identification and modification of dysfunctional assumptions (“intermediate beliefs”). Help the client apply and test out new methods using homework. Behavioral activation: an activity schedule.
Session 8: Closing therapy and encouraging the client to shield against relapse. The client learned how to become a therapist.
The current study compared the efficacy of CBT intervention on depression and QoL in women with substance use disorders to a control group.
Statistical analyses
The collected data were analyzed using multivariate analysis of covariance (MANCOVA) with SPSS software, version 26. In statistical tests, the significance level was 0.05.
3. Results
The percentage of young adults in the experiment group was 46.67%, while the percentage of old adults was 3.33%. In the control group, young adults made up 41.67% of the population, while old adults made up 8.33%.
Table 1 presents the descriptive information of the variables; Tables 2 and 3 present the pre and post-test, which represent the treatment efficacy of the cognitive behavior intervention.
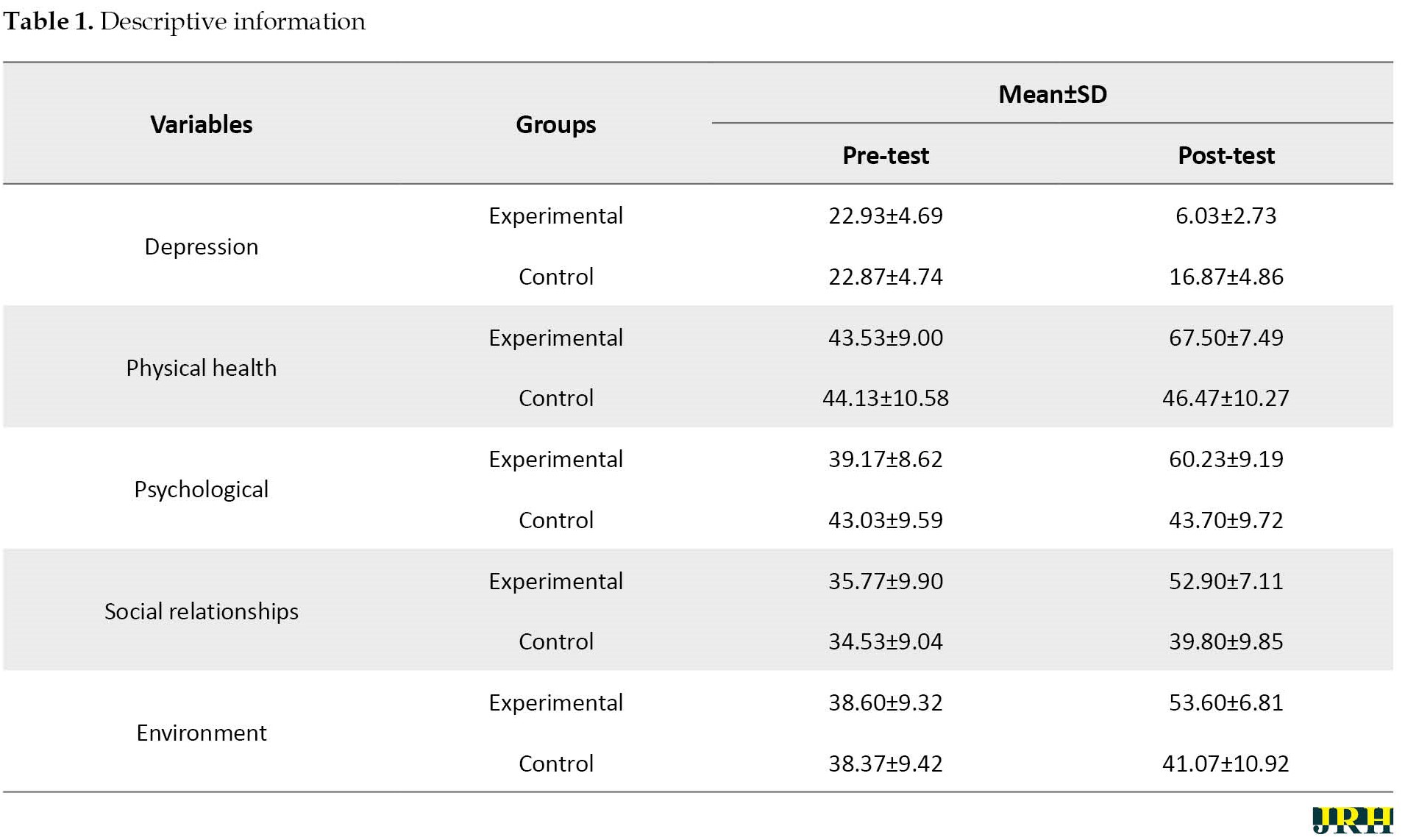

Before the intervention, no discernible variations existed in the participants’ characteristics between the experimental and control groups. As can be seen in Table 1 above, the mean scores in the control group showed little difference, but the difference is visible in the experimental group. Levine’s test was used to observe the assumptions of the covariance. Depression (F=5.95, P=0.018), physical health domain (F=7.96, P=0.007), psychological domain (F=15.69, P=0.007), social relationships (F=7.94, P=0.007), and environment domain (F=1.13, P=0.29) and error variances do not differ between participants (experimental and control group), and variances are equal. Box’s M test was used to study the homogeneity of the covariance. The results showed that Box’s M was significant, establishing the assumption of a difference in covariance (F=2.75, P=0.00). Tables 2 and 3 present the results of the multivariate analysis of covariance (MANCOVA).
Table 2 presents that at a significance level of 0.05, the observed F for Pillai’s trace, Wilks’ lambda, Hoteling’s trace, and Roy’s largest root is 63.643. This means that a significant difference is observed at least in one of the comparable variables between the two groups.
The findings showed a significant difference between the groups in four areas of QoL, including physical, psychological, social relationship, and environmental domains, as well as in terms of depression. This indicates that the experimental group experiences better results in the physical (F=78.13, P<0.05), psychological (F=65.68, P<0.05), social relationship (F=46.69, P<0.05), and environment (F=58.59, P<0.05) domains compared to the control group. Regarding the size of the effect, it can be concluded that the cognitive behavioral intervention had the most positive effects on depression and QoL.
4. Discussion
The current research indicates that CBT considerably reduces depression and enhances QoL. These results, which were consistent with the results of other studies, demonstrated that cognitive behavior intervention can reduce depression [5]. Several studies have found that cognitive-behavioral interventions reduce carer burden in drug-addicted people [6], improve the QoL in the wives of alcohol dependence syndrome patients [7], and reduce depression, anxiety, and stress in family carers [21, 22]. In addition, other studies have shown that mindfulness interventions have also had a significant impact on reducing marital issues and improving the psychosocial well-being of addicted women [8, 23]. The present study’s results suggest cognitive behavior intervention, which helps the client recognize the salient connections between thinking, feeling, motivation, and behaviour to their challenges, usually through obtaining real-life examples. One of the crucial features of a CBT intervention is that participants can examine or explore the evidence for their beliefs and assumptions based on their behavioral experiments. The typical stress and reactions to challenging situations, alternate attitudes and emotions, and helpful information supplied are all crucial abilities that individuals have gained via cognitive behaviour therapies, such as mindful breathing exercises. Practicing mindfulness through behaviour activities enables one to maintain the present moment by avoiding ruminations. The exercises were carried over into daily life, and the individual realized that when confronted with unpleasant events, such as a spouse’s drug or alcohol problems, she should choose proactive behaviours rather than reactive ones, which usually result in sadness, disappointment, and stress. In addition, this helps women adapt to and efficiently deal with the current situation, which is challenging and unpleasant. Moreover, planning to do pleasant activities helps women activate behaviors that increase enjoyment and well-being. In addition, this helps women adapt to and efficiently deal with the current situation, which is challenging and unpleasant. Moreover, planning pleasurable activities helps women activate those behaviors that increase enjoyment and well-being.
5. Conclusion
The results of this study indicated the importance of cognitive behavior intervention in reducing depression and improving the QoL of married women with substance use disorders. They are vulnerable in terms of common mental health issues, such as depression and QoL. Participants learned adaptive thinking processes and positive appraisals of life events. This skill leads to improved experience, recognition of one’s cognitive activity and behavior, positive problem-solving of the situation, and the application and consolidation of new skills and strategies in therapy sessions to generalize them across situations. As a result, they can foster the ability to make healthy coping strategies, and they are better able to deal with the situation.
Limitations and Implications
A main weakness of the study was that the sample was exclusively drawn from female spouses who were primary carers for male inpatients seeking treatment at a tertiary care hospital and therefore maybe not typical of the general community.
To minimize psychological issues and enhance the health of this underserved population, the current study emphasizes the importance of recognizing the needs of spouse carers and giving aid as soon as practical. This study also emphasizes the necessity for further investigation using various culturally appropriate therapy in various settings.
Ethical Considerations
Compliance with ethical guidelines
The protocol of this study was approved by the 11th Institutional Ethical Committee of Sikkim University (No. SU/REG/F-1/03/2019/Vol-II/891). A written and fully informed consent form was obtained from the participants. Also, privacy was maintained and the data of the participants was anonymized to maintain confidentiality.
Funding
The paper was extracted from the doctoral thesis of Langkham Kalpana, Department of Psychology, Sikkim University, Gangtok (Sikkim), India.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We appreciate the women who took part in this study.
References
- Ambekar A, Agrawal A, Rao R, Mishra AK, Khandelwal SK, Chadda RK. Magnitude of Substance use in India. New Delhi: Ministry of Social Justice and Empowerment, Government of India; 2019.
- Sarkar S, Patra BN, Kattimani S. Substance use disorder and the family: An Indian perspective. Medical Journal of Dr. D.Y. Patil University. 2016; 9(1):7-14. [DOI:10.4103/0975-2870.172413]
- World Health Organization (WHO). Depression and other common mental disorders: Global health estimates. Geneva: World Health Organization; 2017. [Link]
- Rush AJ, Beck AT, Kovacs M, Hollon S. Comparative efficacy of cognitive therapy and pharmacotherapy in the treatment of depressed outpatients. Cognitive Therapy and Research. 1977; 1(1):17-37. [DOI:10.1007/BF01173502]
- Kovacs M, Rush AJ, Beck AT, Hollon SD. Depressed outpatients treated with cognitive therapy or pharmacotherapy. A one-year follow-up. Archives of General Psychiatry. 1981; 38(1):33-9. [DOI:10.1001/archpsyc.1981.01780260035003] [PMID]
- Faghih M, Pahlavanzadeh S. The effect of cognitive behavioral therapy on the burden in drug dependent persons' caregivers: A randomized controlled clinical trial. Iranian Journal of Nursing and Midwifery Research. 2019; 24(2):131-6. [DOI:10.4103/ijnmr.IJNMR_86_18] [PMID] [PMCID]
- Gaikwad SJ, Kulkarni S, Chaturvedi V. Quality of life in wives of alcohol dependence syndrome patients. International Journal of Psychology. 2018; 7(2):13-6. [DOI:10.26611/107723]
- Gharibboluk M, Hosseinzadeh S. The effectiveness of mindfulness training on quality of perceptual marital relationship and psychological well-being of women with addicted wife. Revista Romaneasca pentru Educatie Multidimensionala. 2018; 10(1):34-46. [DOI:10.18662/rrem/35]
- Noori R, Jafari F, Moazen B, Khoddami Vishteh HR, Farhoudian A, Narenjiha H, et al. Evaluation of anxiety and depression among female spouses of Iranian male drug dependents. International Journal of High Risk Behaviors & Addiction. 2015; 4(1):e21624. [DOI:10.5812/ijhrba.21624] [PMID] [PMCID]
- Kishor M, Pandit LV, Raguram R. Psychiatric morbidity and marital satisfaction among spouses of men with alcohol dependence. Indian Journal of Psychiatry. 2013; 55(4):360-5. [DOI:10.4103/0019-5545.120557] [PMID] [PMCID]
- Revs IJ. Psychiatric morbidity in spouses of patients with alcohol dependence syndrome. International Journal of Modern Research and Reviews. 2015; 3(10):876-81.
- Dandu A, Bharathi S, Dudala SR. Psychiatric morbidity in spouses of patients with alcohol related disorders. Journal of Family Medicine and Primary Care. 2017; 6(2):305-10. [DOI:10.4103/jfmpc.jfmpc_331_16] [PMID] [PMCID]
- Ghosh P, Victor R, Das H, Sharma S. Psychiatric morbidity and marital satisfaction: Anempirical study on the spouse of alcohol-dependent cases in Barak valley, North-East India. International Journal of Research in Medical Sciences. 2017; 5(4):1600-6. [DOI:10.18203/2320-6012.ijrms20171272]
- Gandhi RR, Suthar MA, Pal S, Rathod AJ. Anxiety and depression in spouses of males diagnosed with alcohol dependence: A comparative study. Archives of Psychiatry and Psychotherapy. 2017; 4(1):51-6. [DOI:10.12740/APP/79459]
- Ponnu MM, Pradeep T, Susan S. Pattern of psychiatric morbidity in spouses of patients with alcohol dependence syndrome. Journal of Evolution of Medical and Dental Sciences. 2015; 4(71):12309-15. [DOI:10.14260/jemds/2015/1778]
- Shah VA, Behere P, Mishra KK, Sharma A, Kumar K. Psychiatric morbidity among spouses of men alcohol dependence. International Journal of Recent Surgical and Medical. 2017; 3(1):10-4. [DOI:10.5005/jp-journals-10053-0030]
- Ólafsdóttir J, Hrafnsdóttir S, Orjasniemi T. Depression, anxiety, and stress from substance-use disorder among family members in Iceland. Nordisk Alkohol- & Narkotikatidskrift. 2018; 35(3):165-78. [DOI:10.1177/1455072518766129] [PMID] [PMCID]
- Maghsoudi J, Alavi M, Sabzi Z, Mancheri H. Experienced psychosocial problems of women with spouses of substance abusers: A qualitative study. Open Access Macedonian Journal of Medical Sciences. 2019; 7(21):3584-91. [DOI:10.3889/oamjms.2019.729] [PMID] [PMCID]
- Lovibond SH, Lovibond PF. Depression anxiety stress scales. Sydney: Psychology Foundation of Australia; 1995. [Link]
- World Health Organization (WHO). WHOQoL-BREF: Introduction, administration, scoring and generic version of the assessment : Field trial version, December 1996. Geneva: World Health Organization; 1996. [Link]
- Borji M, Nourmohammadi H, Otaghi M, Salimi AH, Tarjoman A. Positive effects of cognitive behavioral therapy on depression, anxiety and stress of family caregivers of patients with prostate cancer: A randomized clinical trial. Asian Pacific Journal of Cancer Prevention. 2017; 18(12):3207-12. [DOI:10.22034/APJCP.2017.18.12.3207] [PMID] [PMCID]
- Secker DL, Brown RG. Cognitive behavioural therapy (CBT) for carers of patients with parkinson's disease: A preliminary randomised controlled trial. Journal of Neurology, Neurosurgery, and Psychiatry. 2005; 76(4):491-7. [DOI:10.1136/jnnp.2004.042291] [PMID] [PMCID]
- Ghasemi Jobaneh R, Nazari A, Sanai Zaker B. The effect of mindfulness training on reducing couple burnout of addict’s wife. Journal of Research & Health. 2018; 8(6):506-12. [DOI:10.29252/jrh.8.6.506]
Type of Study: Orginal Article |
Subject:
● Service Quality
Received: 2023/01/17 | Accepted: 2023/04/9 | Published: 2023/06/29
Received: 2023/01/17 | Accepted: 2023/04/9 | Published: 2023/06/29
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |