Volume 14, Issue 2 (Mar & Apr 2024)
J Research Health 2024, 14(2): 189-198 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zargar F, Salmani A, Tarrahi M J. Online Self-management Training and Play Therapy for Treating Behavioral Problems of Children With T1DM. J Research Health 2024; 14 (2) :189-198
URL: http://jrh.gmu.ac.ir/article-1-2257-en.html
URL: http://jrh.gmu.ac.ir/article-1-2257-en.html
1- Behavioral Sciences Research Center, Department of Health Psychology, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Behavioral Sciences Research Center, Department of Health Psychology, Isfahan University of Medical Sciences, Isfahan, Iran. ,ailin.salmani@yahoo.com
3- Department of Epidemiology and Biostatistics, School of Health, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Behavioral Sciences Research Center, Department of Health Psychology, Isfahan University of Medical Sciences, Isfahan, Iran. ,
3- Department of Epidemiology and Biostatistics, School of Health, Isfahan University of Medical Sciences, Isfahan, Iran.
Keywords: Internet-based intervention, Self-management, Play therapy, Behavioral symptoms, Children, Type 1 diabetes
Full-Text [PDF 718 kb]
(733 Downloads)
| Abstract (HTML) (3372 Views)
Full-Text: (1096 Views)
Introduction
Type 1 diabetes mellitus (T1DM) is an autoimmune disease in which the body is unable to make insulin and it is one of the most common chronic diseases in childhood and adolescence [1]. The number of infected children worldwide is 3%-5%. The average annual incidence of T1DM in Iran is increasing and ranges from 0.8 to 50 per hundred thousand children or young adults [2].
Children with T1DM have more psychological distress and risk of emotional, behavioral, and psychiatric disorders than others. In particular, the prevalence of depression and anxiety (as internalizing problems) and eating disorders in these children increases. They may be anxious in social interactions due to fear of high blood sugar and understanding their differences with peers [3]. On the other hand, externalizing behavior problems (such as aggression) lead to poorer glycemic control. Diabetic treatment guidelines include metabolic goals, as well as facilitation of normal social and emotional development [4, 5].
In the treatments used for diabetics, especially in children and adolescents, interventions for their psychological and self-management (SM) problems, have often been neglected. Psychoeducation is the main element of most self-management training (SMT) in many chronic diseases as well as diabetes in children [6, 7]. SM has been defined as the actions that an individual takes in a daily routine to effectively manage their chronic condition [8]. The results of studies indicate the effect of psychoeducation and SMT on glycemic control, level of compliance, anxiety, psychological adaptation, and social competence in diabetic children [9, 10]. Previous studies have guided SMT for parents of children with chronic conditions and their psychological problems, especially children’s externalizing problems [11, 12]. Also, studies about the effect of SMT on mental health and internalizing problems of children with T1DM have focused on their depression and quality of life [6, 13]. Hence, it is essential to research to evaluate the effect of SMT on the other mental problems of these children. On the other hand, web-based interventions increased recently in the relationship between people with diabetes and healthcare professionals. Many web-based programs also allow people with diabetes to submit diabetes data (e.g. glucose data), which can then be discussed online with the healthcare provider. A meta-analysis of 19 studies on type 2 diabetes demonstrated a rather large reduction in HbA1c in these web-based interventions [10]. It showed the impact of SMT on psychosocial outcomes is lower than its impact on glycemic control. The crucial reason for this low effect is the lack of therapeutic provisions related to improving mental and communication status in educational protocols. Furthermore, the focus of previous studies for self-management training has been on parents, and few studies have involved children. One study showed an increase in diabetes knowledge through a personal robot playing a self-management education game with children with T1DM, but this study did not evaluate the children’s mental problems [14].
On the other hand, play therapy (PT) is one of the common interventions for teaching SM in children. Because children have less verbal and cognitive ability than adults to express their emotions, play is a means for them to deal with problems [15]. Studies showed PT can decrease externalizing problems [16, 17], especially children’s social problems that are measured by the child behavior checklist (CBCL) as well as their internalizing problems. PT is effective in learning SM in a wide range of chronic diseases, including T1DM [18]. Various studies have shown the effect of PT on better control of blood sugar, reduction of anxiety, reduction of fear of insulin injection, and improvement of quality of life in children with T1DM [19, 20, 21].
In the present study, compared to previous studies, instead of using conventional approaches to PT, serious games and board games have been used. The “patient child” play (PCP) set has been designed to increase self-control and emotional recognition skills in children 6 years and older, and so far its effectiveness in improving self-control, and controlling aggression, and teaching patience to children has been evaluated in a few preliminary studies [22, 23].
In the present study, PCP was adapted to teach children with T1DM how to perform routine medical care and deal with psychological problems. They were taught to recognize and manage anger, aggression, depression, and anxiety as well as assertiveness training and critical thinking. Also, the SMT protocol used in this study combines the physical SM skills with the psychological skills that these children need. To increase the effect on children’s psychological conditions compared to previous studies [21], it has added related treatment provisions to the protocol. Previous studies have separately shown the effect of PT or SMT on improving the condition of these children, especially in the physical dimension, such as blood sugar control, but no study compares the effects of these two common methods. On the other hand, examining the complete psychological condition of these children has been given very little attention in previous studies, and usually, states, such as anxiety and depression have been investigated. Therefore, this study was conducted to compare the effect of internet-delivered SMT and PCP on externalizing and internalizing problems of children with T1DM.
Methods
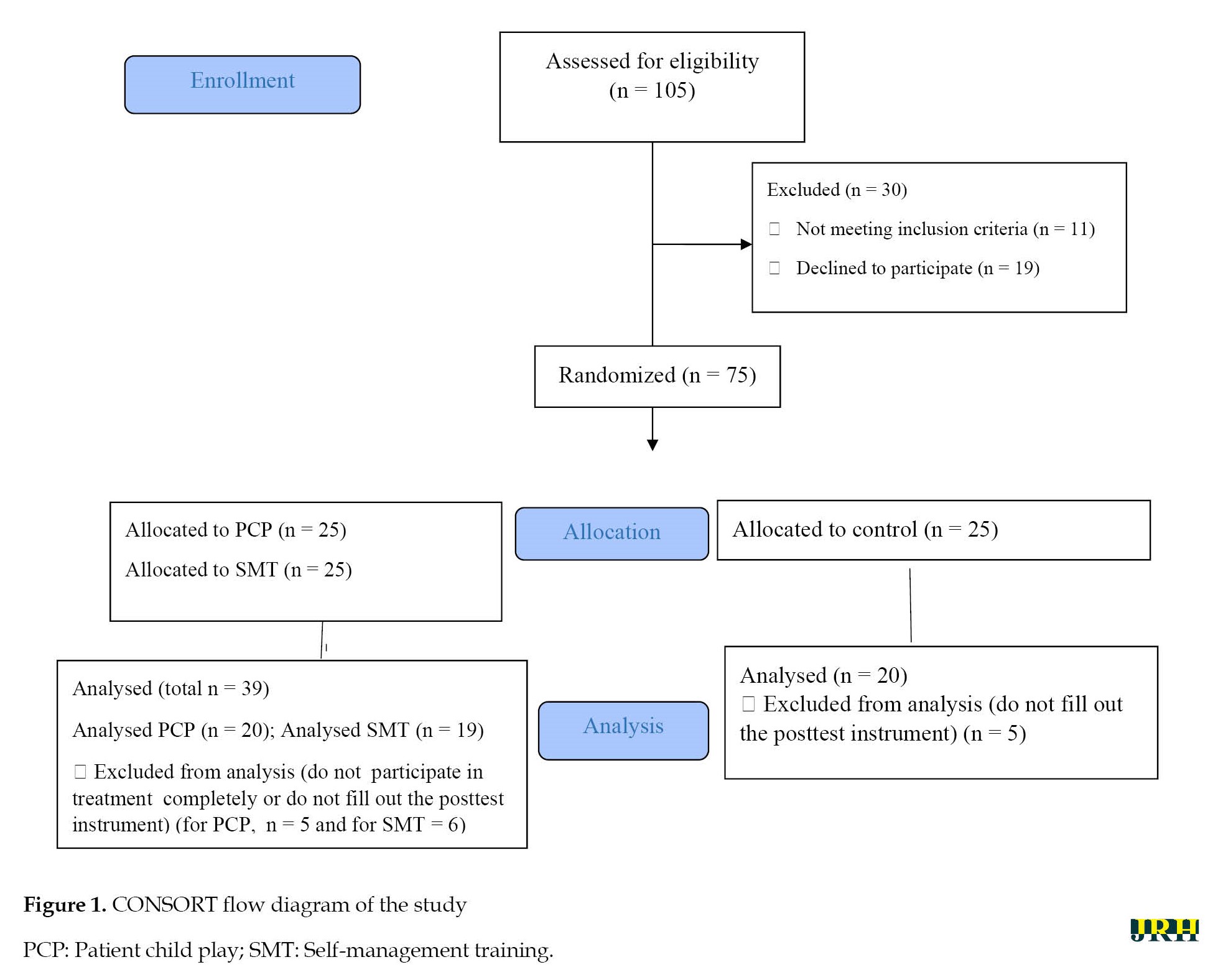
This study is a randomized clinical trial Among children aged 8 to 11 years with T1DM who were referred to Isfahan diabetes center from June to March 2019 and received a diagnosis of T1DM based on the opinion of a pediatric endocrinologist, 75 children were selected based on inclusion and exclusion criteria. They were randomly assigned to three groups, internet-delivered self-management training (iSMT), PCP, and control. The flow diagram of the study has been shown in Figure 1.
Type 1 diabetes mellitus (T1DM) is an autoimmune disease in which the body is unable to make insulin and it is one of the most common chronic diseases in childhood and adolescence [1]. The number of infected children worldwide is 3%-5%. The average annual incidence of T1DM in Iran is increasing and ranges from 0.8 to 50 per hundred thousand children or young adults [2].
Children with T1DM have more psychological distress and risk of emotional, behavioral, and psychiatric disorders than others. In particular, the prevalence of depression and anxiety (as internalizing problems) and eating disorders in these children increases. They may be anxious in social interactions due to fear of high blood sugar and understanding their differences with peers [3]. On the other hand, externalizing behavior problems (such as aggression) lead to poorer glycemic control. Diabetic treatment guidelines include metabolic goals, as well as facilitation of normal social and emotional development [4, 5].
In the treatments used for diabetics, especially in children and adolescents, interventions for their psychological and self-management (SM) problems, have often been neglected. Psychoeducation is the main element of most self-management training (SMT) in many chronic diseases as well as diabetes in children [6, 7]. SM has been defined as the actions that an individual takes in a daily routine to effectively manage their chronic condition [8]. The results of studies indicate the effect of psychoeducation and SMT on glycemic control, level of compliance, anxiety, psychological adaptation, and social competence in diabetic children [9, 10]. Previous studies have guided SMT for parents of children with chronic conditions and their psychological problems, especially children’s externalizing problems [11, 12]. Also, studies about the effect of SMT on mental health and internalizing problems of children with T1DM have focused on their depression and quality of life [6, 13]. Hence, it is essential to research to evaluate the effect of SMT on the other mental problems of these children. On the other hand, web-based interventions increased recently in the relationship between people with diabetes and healthcare professionals. Many web-based programs also allow people with diabetes to submit diabetes data (e.g. glucose data), which can then be discussed online with the healthcare provider. A meta-analysis of 19 studies on type 2 diabetes demonstrated a rather large reduction in HbA1c in these web-based interventions [10]. It showed the impact of SMT on psychosocial outcomes is lower than its impact on glycemic control. The crucial reason for this low effect is the lack of therapeutic provisions related to improving mental and communication status in educational protocols. Furthermore, the focus of previous studies for self-management training has been on parents, and few studies have involved children. One study showed an increase in diabetes knowledge through a personal robot playing a self-management education game with children with T1DM, but this study did not evaluate the children’s mental problems [14].
On the other hand, play therapy (PT) is one of the common interventions for teaching SM in children. Because children have less verbal and cognitive ability than adults to express their emotions, play is a means for them to deal with problems [15]. Studies showed PT can decrease externalizing problems [16, 17], especially children’s social problems that are measured by the child behavior checklist (CBCL) as well as their internalizing problems. PT is effective in learning SM in a wide range of chronic diseases, including T1DM [18]. Various studies have shown the effect of PT on better control of blood sugar, reduction of anxiety, reduction of fear of insulin injection, and improvement of quality of life in children with T1DM [19, 20, 21].
In the present study, compared to previous studies, instead of using conventional approaches to PT, serious games and board games have been used. The “patient child” play (PCP) set has been designed to increase self-control and emotional recognition skills in children 6 years and older, and so far its effectiveness in improving self-control, and controlling aggression, and teaching patience to children has been evaluated in a few preliminary studies [22, 23].
In the present study, PCP was adapted to teach children with T1DM how to perform routine medical care and deal with psychological problems. They were taught to recognize and manage anger, aggression, depression, and anxiety as well as assertiveness training and critical thinking. Also, the SMT protocol used in this study combines the physical SM skills with the psychological skills that these children need. To increase the effect on children’s psychological conditions compared to previous studies [21], it has added related treatment provisions to the protocol. Previous studies have separately shown the effect of PT or SMT on improving the condition of these children, especially in the physical dimension, such as blood sugar control, but no study compares the effects of these two common methods. On the other hand, examining the complete psychological condition of these children has been given very little attention in previous studies, and usually, states, such as anxiety and depression have been investigated. Therefore, this study was conducted to compare the effect of internet-delivered SMT and PCP on externalizing and internalizing problems of children with T1DM.
Methods
This study is a randomized clinical trial Among children aged 8 to 11 years with T1DM who were referred to Isfahan diabetes center from June to March 2019 and received a diagnosis of T1DM based on the opinion of a pediatric endocrinologist, 75 children were selected based on inclusion and exclusion criteria. They were randomly assigned to three groups, internet-delivered self-management training (iSMT), PCP, and control. The flow diagram of the study has been shown in Figure 1.
In this study, assuming that the minimum detectable effect size is ∆=0.9 (considering α=0.05 and 1-β=0.8) [22], the sample size to each group is at least 20 patients. Considering the possible dropout, 25 people were assigned in each group.
The inclusion criteria included the children ages between 8-11 years old, not receiving further psychotherapy for the past 6 months, and completing the informed consent form by the child’s parents. The exclusion criteria included the absence of more than 2 treatment sessions and hospitalization during the intervention.
Parents of all participants filled out the study questionnaire online in the pre-test and post-test stages. The following tool was used to collect data:
Child behavior checklist (CBCL)
CBCL with 113 questions assesses the problems of children and adolescents aged 6 to 18 in 8 domains: anxiety/depression (AD), withdrawal/depression (WD), somatic complaints (SC), social problems (SP), thought problems (TP), attention problems (AP), rule-breaking behaviors (RB), and aggressive behavior (AG). The school-age assessment forms are the CBCL/6-18, completed by parents or surrogates; the teacher report form (TRF)/6-18, completed by teachers and other school staff; and the youth self-report (YSR)/11-18 completed by youths. The validity coefficients of CBCL forms were reported to be 0.97 using Cronbach’s α and 0.94 using re-test validity. The content validity, criterion validity, and structural validity of these forms were reported to be favorable [24]. The Persian version of this tool has a suitable reliability (Cronbach’s α 0.63 to 0.95 and the range of temporal stability coefficients 0.32 to 0.67) [25]. In the present study, the reliability of CBCL using Cronbach’s α was obtained between 0.68 to 0.93 for subscales and 0.78 for the total scale.
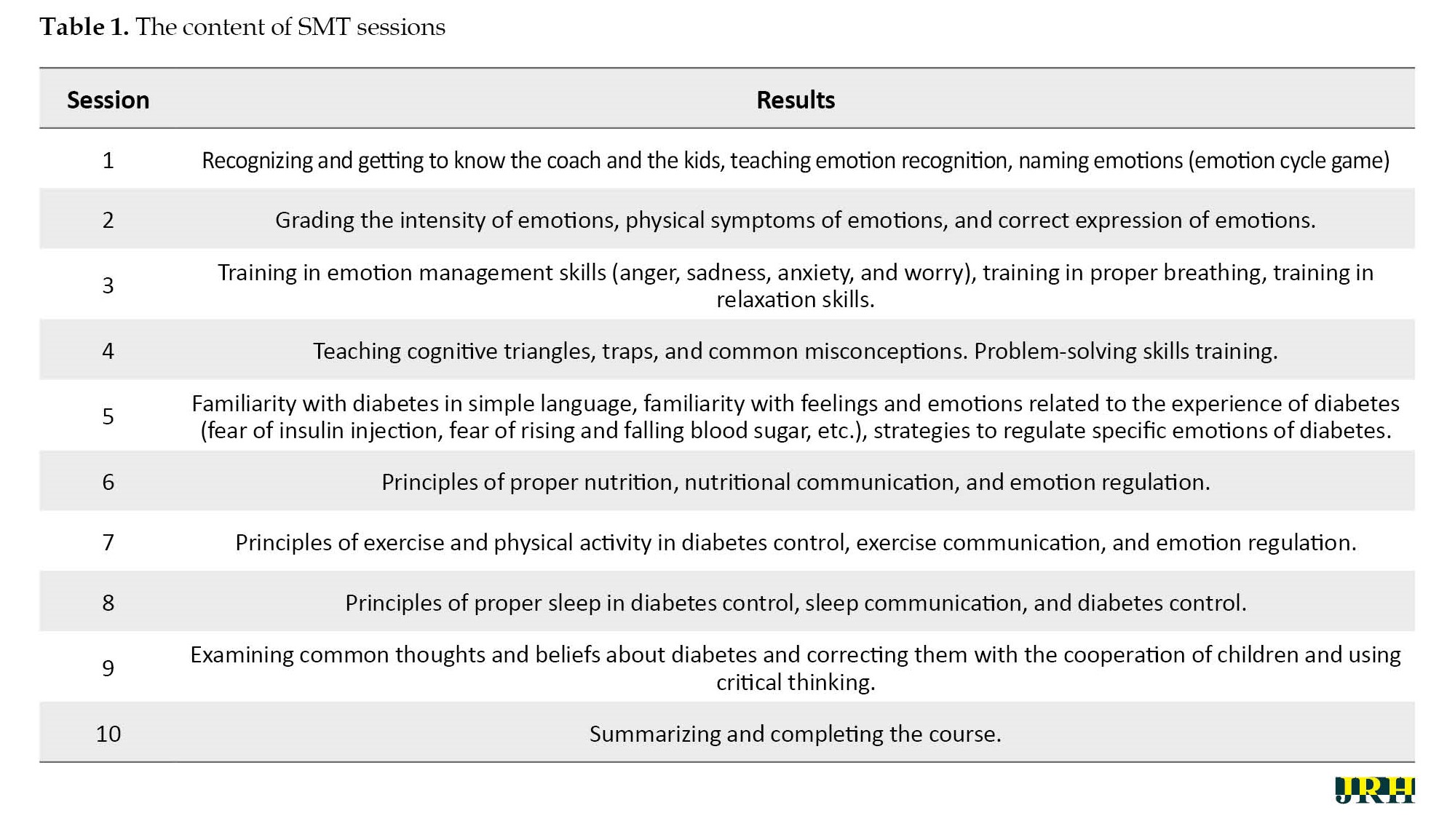
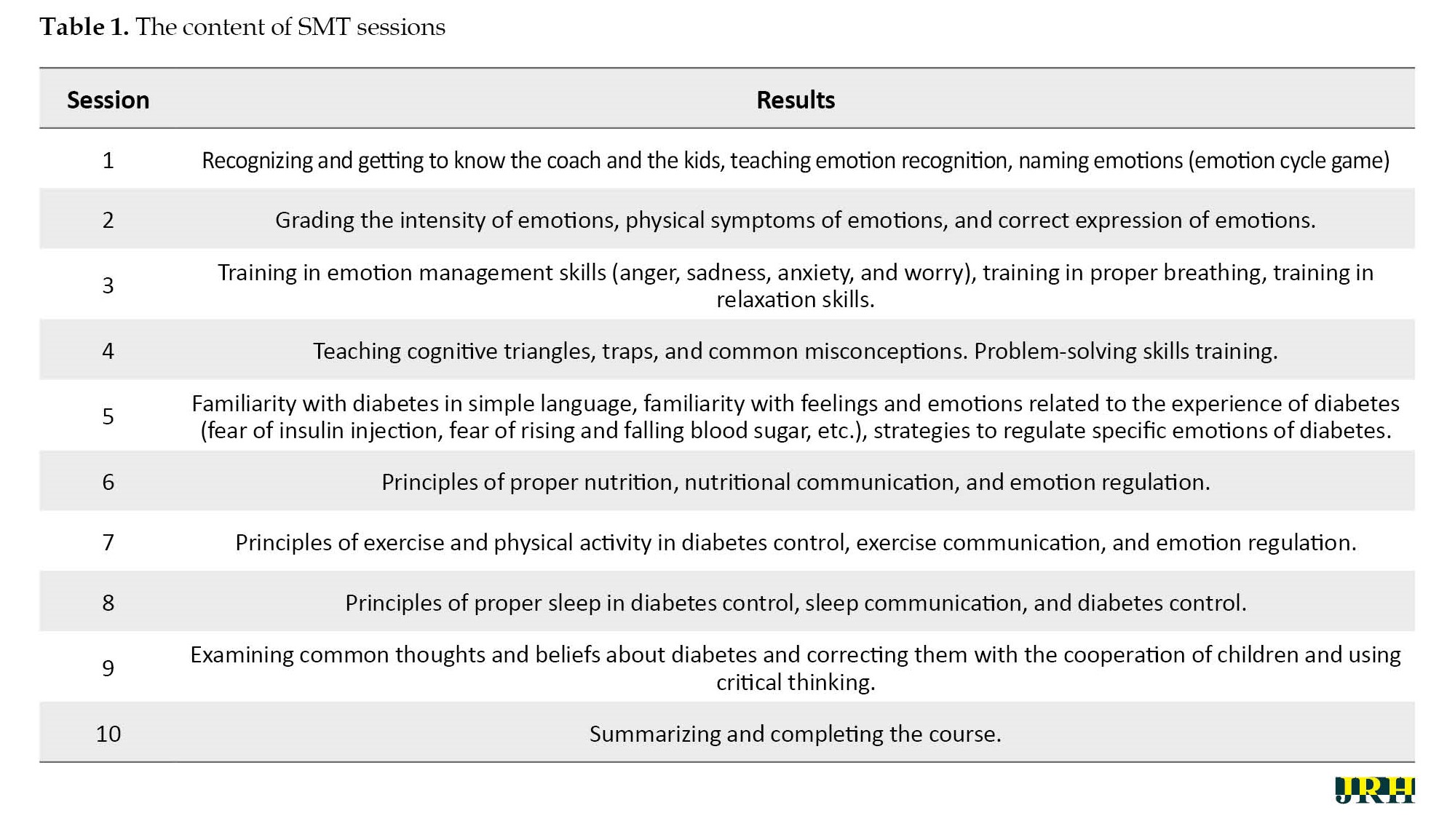
The iSMT group received online training for 10 2-hour sessions online via the Skyroom platform. In each session, mothers and children participated. The training protocol taught by an educated health psychologist included training in the physical care required for diabetes (principles of proper nutrition, familiarity with different food groups, principles of physical activity and exercise, insulin injection, and blood sugar testing). The protocol was collected from the educational resources of the Gabric Diabetes Education Association (GDEA) [26], handbooks for T1DM in children and adolescents, and guidelines for type 1 diabetes in children and adolescents [27]. It also included training in recognizing emotions and feelings, problem-solving, relaxation, assertiveness skills, anger and anxiety management, and identifying erroneous and dysfunctional thoughts and beliefs about diabetes, which were collected from sources, such as the application of cognitive-behavioral therapy (CBT) in psychological problems of type 1 diabetes [28] and the books, such as compatible cat [29] and teaching life skills through ancient Iranian tales [30]. The sessions were interactive and active learning, and the children were given exercises to do at home. The content of the 10 sessions is entered in the Table 1.
The game used in the PT group PCP from Shadram’s educational and therapeutic games company. This game is specially designed to help children who have problems with self-control for various reasons. In this game, children learn crucial social skills, such as taking turns, listening to others, following the rules of the game, etc. PCP consists of two games, feeling alarm, and watchtower. The feeling alarm consists of 3 groups of cards, say no firmly- for saying no and assertiveness training, world of emotions- for identifying emotions in different situations, and the magic trio- for training cognitive triangle thoughts, emotions, and behaviors based on cognitive-behavioral therapy (CBT). The watchtower game consists of 3 sets of cards named prediction- for training self-control skills in different situations, my police- for training the importance of order, timing, physical and mental care of the body, relaxation training, etc. and magic of words for teaching recognition and correction dysfunctional thoughts and beliefs [31]. The content of the cards was changed to suit for problems of children with diabetes. The play group performed PCP for 10 sessions. The play was posted for each child and they were asked to play it with their parents twice a week for 5 weeks. The play has a guide that fully explains how to do it. Furthermore, the researcher sent short videos to mothers about how to do different parts of the play. The control group received only routine diabetes interventions.
Statistical analysis
The collected data were analyzed using analysis of variance (ANOVA) with SPSS software, version 26. In statistical tests, the significance
level was 0.05.
Results
Participants included 24 boys (40%) and 35 girls (60%). A total of 19 children (30.5%) were 8 years old (iSMT=6, 33.3%; PCP=5, 27.8%; control=7, 38.9%). The number of 9-year-old children was 11(18.6%; iSMT=4, 36.36%; PCP=4, 36.36%; control=3, 27.28%), the number of 10-year-old children was 11(18.6%; iSMT=3, 27.28%; PCP=4, 36.36%; control=4, 36.36%), and the number of 11-year-old children was 19(32.3%; iSMT=6, 31.58%; PCP=7, 36.84% ; control=6, 31.58%).
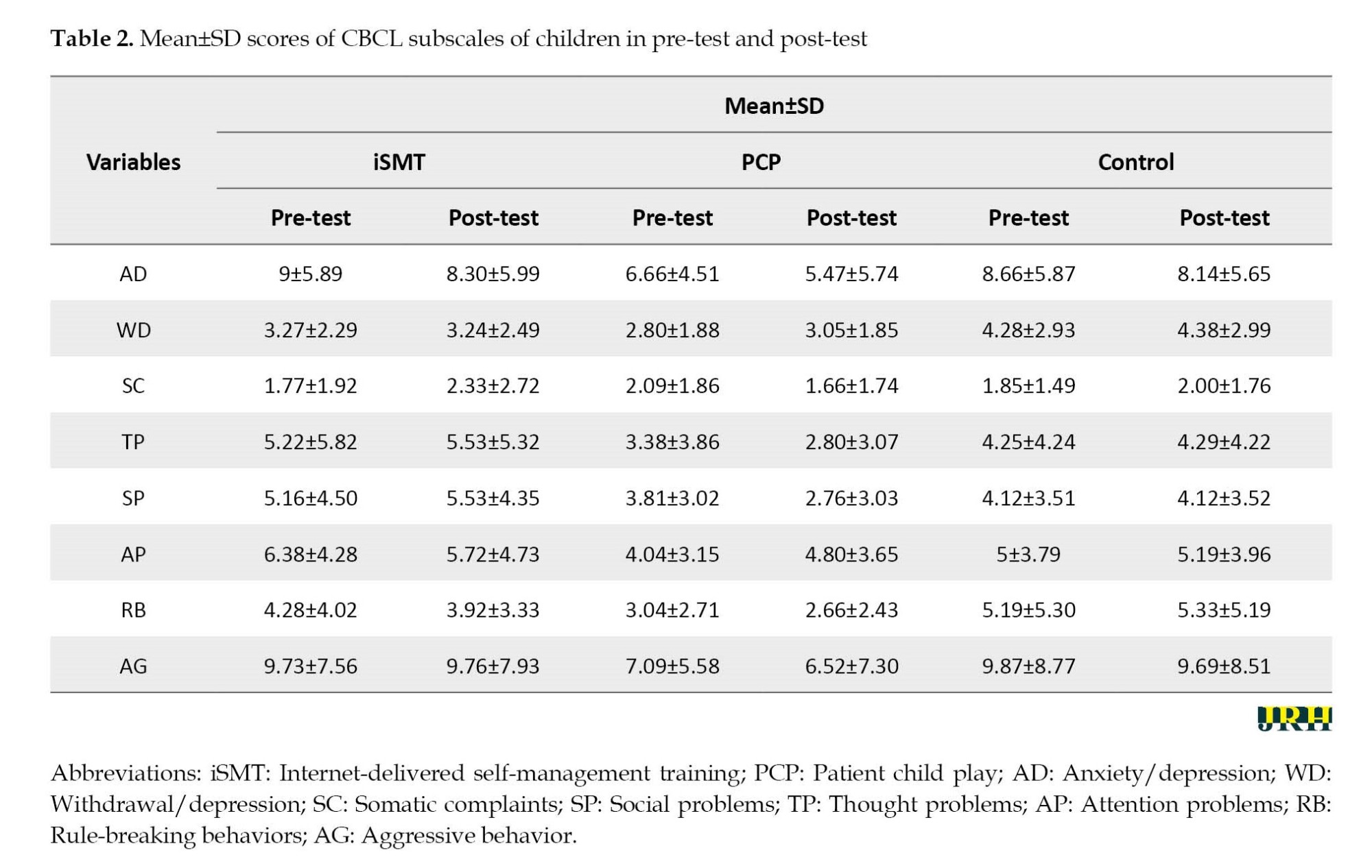
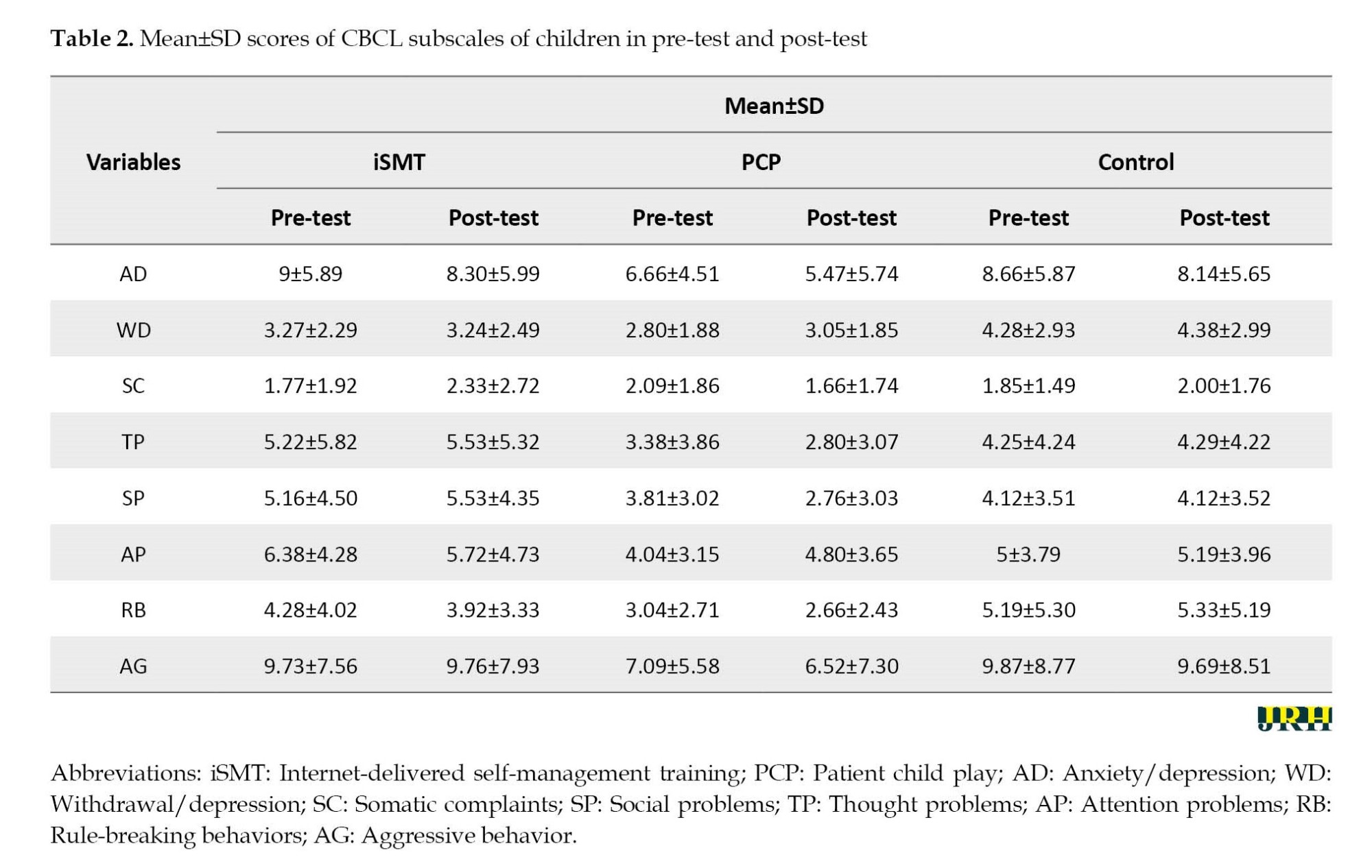
Table 2 presents the descriptive indices of the mean and standard deviation of the CBCL and its subscales.
To check the assumption of normality of the distribution of scores in the groups, the Kolmogorov-Smirnov test was used. The results showed that the distribution of scores is not normal, and for this reason, non-parametric tests were used to compare the differences in the scores of the groups. To make pairwise comparisons between the three groups in a significant subscale, the Mann-Whitney U test was used. It showed no significant differences between the 3 groups except in SP and PB subscales (Table 3).

Table 3 presented that the PCP group had more improvement in SP compared to the SMT group as well as a significant improvement in RB compared to the control group.
Discussion
The present study showed that the PCP group had more improvement in SP compared to the iSMT group. Although no significant differences were observed between iSM and the control group as well as PCP and the control group, the mean scores of SP in the control group were more than intervention groups. It shows both PCP and iSM can decrease SP in diabetic children. This result is consistent with other studies showing that PT can decrease the externalizing problems, especially social problems and aggression of children with T1DM [16, 17, 31]. On the other hand, the non-significant effect of iSMT is not consistent with the previous studies that showed decreasing externalizing and internalizing problems of children with T1DM [6, 11-13]. A common feature of previous studies was that the training was implemented for parents of children and the materials were related to self-help components for parents (not the children). Therefore, the different results can be related to the different samples. In the present study, the ages of children were between 8 to 11 years. Perhaps children in these ages are not completely suitable for training based on theoretical components or mutual conversation. Studies on SMT in children have evaluated older children than children in the present study. For example, Guner reported the impact of SMT among asthmatic children and adolescents aged 10-18 years on self-efficacy and disease course [32]. On the other hand, the previous studies did not use internet-delivered SMT for children in the way that the present study used. One study that measured the effectiveness of SMT for diabetic children used a robot that was more a form of PT than pure theoretical training. Although it showed an increase in children’s diabetes knowledge, it has not investigated the internalizing and externalizing problems of these children. Therefore, based on the results of this study and our results, it seems PT is more useful for the management of somatic needs and mental problems of children with T1DM. Furthermore, it can be concluded that internet-delivered training for children at these ages has fewer effects than at older ages. A meta-analysis of digital technologies for SMT in children and parents showed that the age range of most children in various studies includes late childhood and adolescence [33]. In pre-adolescent children, parents play a prominent role in diabetes self-management.
The present study showed PCP decreased SP and RB subscales of CBCL. These two subscales are related to externalizing problems. Therefore, it can be concluded that PCP is more effective in externalizing problems of children with T1DM than their internalizing problems. A look at the SP subscale of CBCL shows that it has the domains included too dependent, lonely, not get along, jealous, others out to get him/her, accident-prone, clumsy, getting teased, prefer younger kids, and speech problems. In the SMT group, children entered into negotiations with their peers, gave opinions, asked questions, and got to know each other’s similar problems. It seems that the cooperative atmosphere of the group can reduce the feeling of loneliness and difficulty in getting along with others or problems in getting teased the others. They also received training on how to control their blood sugar independently. Therefore, this issue can reduce the dependency of the participants. However, the results of the research showed that the PCP group had a more significant decrease than the training group. It seems that training blood sugar control and conveying psychological concepts, such as assertiveness, saying no, recognizing emotions, etc. through games, has a greater effect on children than mere education, which has a structure similar to their conventional education.
The other result of the present study was that the PCP group had significant improvement in RB compared to the control group. Also, no significant differences were observed between PCP and SMT groups in RB in the posttest. Although no significant differences were observed between the iSMT and the control group, the mean scores of RB in the control group were more than SMT group. It shows that PCP and SMT can decrease RB in diabetic children.
The domains of RB in CBCL included using drugs, alcohol, and tobacco, lacking guilt, breaking rules, having bad friends, lying, cheating, preferring older kids, running away, setting fires, having sex problems, stealing at home/outside the home, etc. Although some cases, such as drug use were not relevant in the sample group, it seems PT targets areas, such as choosing friends of the same age, following rules, and not lying.
The results of the present study showed that PCP is more effective in reducing externalizing problems of children with T1DM. The result of our study can be related to the mechanisms of PT. Some of them are self-expression, competence, self-control, and creative problem-solving, which are related to external behaviors [34]. On the other hand, the vital issue in play is to follow the rules of the game. Therefore, through PT, children learn to follow the rules and become more social.
Conclusion
The present study showed that although iSMT can decrease the scores of internalizing and externalizing problems of children with T1DM compared to the control group, these differences are not statistically significant. Also, PT through PCP is a more effective intervention than iSMT for externalizing problems of children with T1DM especially their social problems and rule-breaking behaviors.
Limitations and implications
One of the limitations of the present study was the difficulty in transferring educational concepts due to the virtual training situation. Also, the PCP was not held in the peer groups. It was sent to the participants, and the game was played at home with the cooperation of the parents. Although the researcher made sure that the child-parent does PCP at home as often as needed for the study by constantly calling the participating parents, these conditions can have different results than play with other children. Another limitation of the present study is that no intervention was done to eliminate the placebo effect of the treatment for the control group. Also, due to the lack of a follow-up phase, it is not possible to check the continuity of treatment effects in the groups.
Ethical Considerations
Compliance with ethical guidelines
The research was conducted by the tents of the Declaration of Helsinki. The Ethics Committee of Isfahan University of Medical Sciences approved this study (Code: IR.ARI.MUI.REC.1400.056). The trial protocol was approved in the Iranian Registry of Clinical Trials (IRCT) (Code: IRCT20180909040974N3). A written and fully informed consent form was obtained from the participants. Also, privacy was maintained and the data of the participants was anonymized to maintain confidentiality.
Funding
This article is extracted from a project supported by Isfahan University of Medical Sciences (Code: 2400225).
Authors' contributions
Resources and supervision: Ailin Salmani and Fatemeh Zargar; Methodology: Fatemeh Zargar and Mohammad Javad Tarrahi; Investigation and writing the original draft: Ailin Salmani; Review, editing and conceptualization: Fatemeh Zargar.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate the children and their mothers who took part in this study.
The inclusion criteria included the children ages between 8-11 years old, not receiving further psychotherapy for the past 6 months, and completing the informed consent form by the child’s parents. The exclusion criteria included the absence of more than 2 treatment sessions and hospitalization during the intervention.
Parents of all participants filled out the study questionnaire online in the pre-test and post-test stages. The following tool was used to collect data:
Child behavior checklist (CBCL)
CBCL with 113 questions assesses the problems of children and adolescents aged 6 to 18 in 8 domains: anxiety/depression (AD), withdrawal/depression (WD), somatic complaints (SC), social problems (SP), thought problems (TP), attention problems (AP), rule-breaking behaviors (RB), and aggressive behavior (AG). The school-age assessment forms are the CBCL/6-18, completed by parents or surrogates; the teacher report form (TRF)/6-18, completed by teachers and other school staff; and the youth self-report (YSR)/11-18 completed by youths. The validity coefficients of CBCL forms were reported to be 0.97 using Cronbach’s α and 0.94 using re-test validity. The content validity, criterion validity, and structural validity of these forms were reported to be favorable [24]. The Persian version of this tool has a suitable reliability (Cronbach’s α 0.63 to 0.95 and the range of temporal stability coefficients 0.32 to 0.67) [25]. In the present study, the reliability of CBCL using Cronbach’s α was obtained between 0.68 to 0.93 for subscales and 0.78 for the total scale.
The iSMT group received online training for 10 2-hour sessions online via the Skyroom platform. In each session, mothers and children participated. The training protocol taught by an educated health psychologist included training in the physical care required for diabetes (principles of proper nutrition, familiarity with different food groups, principles of physical activity and exercise, insulin injection, and blood sugar testing). The protocol was collected from the educational resources of the Gabric Diabetes Education Association (GDEA) [26], handbooks for T1DM in children and adolescents, and guidelines for type 1 diabetes in children and adolescents [27]. It also included training in recognizing emotions and feelings, problem-solving, relaxation, assertiveness skills, anger and anxiety management, and identifying erroneous and dysfunctional thoughts and beliefs about diabetes, which were collected from sources, such as the application of cognitive-behavioral therapy (CBT) in psychological problems of type 1 diabetes [28] and the books, such as compatible cat [29] and teaching life skills through ancient Iranian tales [30]. The sessions were interactive and active learning, and the children were given exercises to do at home. The content of the 10 sessions is entered in the Table 1.
The game used in the PT group PCP from Shadram’s educational and therapeutic games company. This game is specially designed to help children who have problems with self-control for various reasons. In this game, children learn crucial social skills, such as taking turns, listening to others, following the rules of the game, etc. PCP consists of two games, feeling alarm, and watchtower. The feeling alarm consists of 3 groups of cards, say no firmly- for saying no and assertiveness training, world of emotions- for identifying emotions in different situations, and the magic trio- for training cognitive triangle thoughts, emotions, and behaviors based on cognitive-behavioral therapy (CBT). The watchtower game consists of 3 sets of cards named prediction- for training self-control skills in different situations, my police- for training the importance of order, timing, physical and mental care of the body, relaxation training, etc. and magic of words for teaching recognition and correction dysfunctional thoughts and beliefs [31]. The content of the cards was changed to suit for problems of children with diabetes. The play group performed PCP for 10 sessions. The play was posted for each child and they were asked to play it with their parents twice a week for 5 weeks. The play has a guide that fully explains how to do it. Furthermore, the researcher sent short videos to mothers about how to do different parts of the play. The control group received only routine diabetes interventions.
Statistical analysis
The collected data were analyzed using analysis of variance (ANOVA) with SPSS software, version 26. In statistical tests, the significance
level was 0.05.
Results
Participants included 24 boys (40%) and 35 girls (60%). A total of 19 children (30.5%) were 8 years old (iSMT=6, 33.3%; PCP=5, 27.8%; control=7, 38.9%). The number of 9-year-old children was 11(18.6%; iSMT=4, 36.36%; PCP=4, 36.36%; control=3, 27.28%), the number of 10-year-old children was 11(18.6%; iSMT=3, 27.28%; PCP=4, 36.36%; control=4, 36.36%), and the number of 11-year-old children was 19(32.3%; iSMT=6, 31.58%; PCP=7, 36.84% ; control=6, 31.58%).
Table 2 presents the descriptive indices of the mean and standard deviation of the CBCL and its subscales.
To check the assumption of normality of the distribution of scores in the groups, the Kolmogorov-Smirnov test was used. The results showed that the distribution of scores is not normal, and for this reason, non-parametric tests were used to compare the differences in the scores of the groups. To make pairwise comparisons between the three groups in a significant subscale, the Mann-Whitney U test was used. It showed no significant differences between the 3 groups except in SP and PB subscales (Table 3).

Table 3 presented that the PCP group had more improvement in SP compared to the SMT group as well as a significant improvement in RB compared to the control group.
Discussion
The present study showed that the PCP group had more improvement in SP compared to the iSMT group. Although no significant differences were observed between iSM and the control group as well as PCP and the control group, the mean scores of SP in the control group were more than intervention groups. It shows both PCP and iSM can decrease SP in diabetic children. This result is consistent with other studies showing that PT can decrease the externalizing problems, especially social problems and aggression of children with T1DM [16, 17, 31]. On the other hand, the non-significant effect of iSMT is not consistent with the previous studies that showed decreasing externalizing and internalizing problems of children with T1DM [6, 11-13]. A common feature of previous studies was that the training was implemented for parents of children and the materials were related to self-help components for parents (not the children). Therefore, the different results can be related to the different samples. In the present study, the ages of children were between 8 to 11 years. Perhaps children in these ages are not completely suitable for training based on theoretical components or mutual conversation. Studies on SMT in children have evaluated older children than children in the present study. For example, Guner reported the impact of SMT among asthmatic children and adolescents aged 10-18 years on self-efficacy and disease course [32]. On the other hand, the previous studies did not use internet-delivered SMT for children in the way that the present study used. One study that measured the effectiveness of SMT for diabetic children used a robot that was more a form of PT than pure theoretical training. Although it showed an increase in children’s diabetes knowledge, it has not investigated the internalizing and externalizing problems of these children. Therefore, based on the results of this study and our results, it seems PT is more useful for the management of somatic needs and mental problems of children with T1DM. Furthermore, it can be concluded that internet-delivered training for children at these ages has fewer effects than at older ages. A meta-analysis of digital technologies for SMT in children and parents showed that the age range of most children in various studies includes late childhood and adolescence [33]. In pre-adolescent children, parents play a prominent role in diabetes self-management.
The present study showed PCP decreased SP and RB subscales of CBCL. These two subscales are related to externalizing problems. Therefore, it can be concluded that PCP is more effective in externalizing problems of children with T1DM than their internalizing problems. A look at the SP subscale of CBCL shows that it has the domains included too dependent, lonely, not get along, jealous, others out to get him/her, accident-prone, clumsy, getting teased, prefer younger kids, and speech problems. In the SMT group, children entered into negotiations with their peers, gave opinions, asked questions, and got to know each other’s similar problems. It seems that the cooperative atmosphere of the group can reduce the feeling of loneliness and difficulty in getting along with others or problems in getting teased the others. They also received training on how to control their blood sugar independently. Therefore, this issue can reduce the dependency of the participants. However, the results of the research showed that the PCP group had a more significant decrease than the training group. It seems that training blood sugar control and conveying psychological concepts, such as assertiveness, saying no, recognizing emotions, etc. through games, has a greater effect on children than mere education, which has a structure similar to their conventional education.
The other result of the present study was that the PCP group had significant improvement in RB compared to the control group. Also, no significant differences were observed between PCP and SMT groups in RB in the posttest. Although no significant differences were observed between the iSMT and the control group, the mean scores of RB in the control group were more than SMT group. It shows that PCP and SMT can decrease RB in diabetic children.
The domains of RB in CBCL included using drugs, alcohol, and tobacco, lacking guilt, breaking rules, having bad friends, lying, cheating, preferring older kids, running away, setting fires, having sex problems, stealing at home/outside the home, etc. Although some cases, such as drug use were not relevant in the sample group, it seems PT targets areas, such as choosing friends of the same age, following rules, and not lying.
The results of the present study showed that PCP is more effective in reducing externalizing problems of children with T1DM. The result of our study can be related to the mechanisms of PT. Some of them are self-expression, competence, self-control, and creative problem-solving, which are related to external behaviors [34]. On the other hand, the vital issue in play is to follow the rules of the game. Therefore, through PT, children learn to follow the rules and become more social.
Conclusion
The present study showed that although iSMT can decrease the scores of internalizing and externalizing problems of children with T1DM compared to the control group, these differences are not statistically significant. Also, PT through PCP is a more effective intervention than iSMT for externalizing problems of children with T1DM especially their social problems and rule-breaking behaviors.
Limitations and implications
One of the limitations of the present study was the difficulty in transferring educational concepts due to the virtual training situation. Also, the PCP was not held in the peer groups. It was sent to the participants, and the game was played at home with the cooperation of the parents. Although the researcher made sure that the child-parent does PCP at home as often as needed for the study by constantly calling the participating parents, these conditions can have different results than play with other children. Another limitation of the present study is that no intervention was done to eliminate the placebo effect of the treatment for the control group. Also, due to the lack of a follow-up phase, it is not possible to check the continuity of treatment effects in the groups.
Ethical Considerations
Compliance with ethical guidelines
The research was conducted by the tents of the Declaration of Helsinki. The Ethics Committee of Isfahan University of Medical Sciences approved this study (Code: IR.ARI.MUI.REC.1400.056). The trial protocol was approved in the Iranian Registry of Clinical Trials (IRCT) (Code: IRCT20180909040974N3). A written and fully informed consent form was obtained from the participants. Also, privacy was maintained and the data of the participants was anonymized to maintain confidentiality.
Funding
This article is extracted from a project supported by Isfahan University of Medical Sciences (Code: 2400225).
Authors' contributions
Resources and supervision: Ailin Salmani and Fatemeh Zargar; Methodology: Fatemeh Zargar and Mohammad Javad Tarrahi; Investigation and writing the original draft: Ailin Salmani; Review, editing and conceptualization: Fatemeh Zargar.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate the children and their mothers who took part in this study.
References
- Brunetti G, D’Amato G, De Santis S, Grano M, Faienza MF. Mechanisms of altered bone remodeling in children with type 1 diabetes. World Journal of Diabetes. 2021; 12(7):997-1009. [DOI:10.4239/wjd.v12.i7.997] [PMID]
- Hajinia Z, Alaee Karahroudy F, Zaeri H, Ghasemi E. Effect of self-care education on self-management behaviors of children with type 1 diabetes. Journal of Modern Family Medicine. 2021; 1(1):E104. [Link]
- Cutler JL. Kaplan and Sadock’s synopsis of psychiatry. Journal of Psychiatric Practice. 2016; 22(1):68-9. [DOI:10.1097/PRA.0000000000000126]
- Khandelwal S, Sengar GS, Sharma M, Choudhary S, Nagaraj N. Psychosocial illness in children with type 1 diabetes mellitus: prevalence, pattern and risk factors. Journal of Clinical and Diagnostic Research. 2016; 10(9):SC05-8. [DOI:10.7860/JCDR/2016/21666.8549] [PMID]
- Eilander MM, de Wit M, Rotteveel J, Snoek FJ. Low self-confidence and diabetes mismanagement in youth with type 1 diabetes mediate the relationship between behavioral problems and elevated HbA1c. Journal of Diabetes Research. 2016; 2016:3159103. [DOI:10.1155/2016/3159103] [PMID]
- Charalampopoulos D, Hesketh KR, Amin R, Paes VM, Viner RM, Stephenson T. Psycho-educational interventions for children and young people with type 1 diabetes in the UK: How effective are they? A systematic review and meta-analysis. Plos One. 2017; 12(6):e0179685. [DOI:10.1371/journal.pone.0179685] [PMID]
- Saxby N, Beggs S, Battersby M, Lawn S. What are the components of effective chronic condition self-management education interventions for children with asthma, cystic fibrosis, and diabetes? A systematic review. Patient Education and Counseling. 2019; 102(4):607-22. [DOI:10.1016/j.pec.2018.11.001] [PMID]
- Henry HK, Schor EL. Supporting self-management of chronic health problems. Pediatrics. 2015; 135(5):789-92. [DOI:10.1542/peds.2014-3431] [PMID]
- Moeini Koochaksaraee F, Mohammadi Shirmahaleh F, Tajeri B, Shirafkan Kopkan A, Jianbagheri M. Effectiveness of cognitive-behavioral therapy in diabetes self-management and HbA1C level in patients with type 2 diabetes. Razavi International Journal of Medicine. 2022; 10(2):45-51. [DOI:10.30483/RIJM.2022.254335.1161]
- Hermanns N, Ehrmann D, Finke-Groene K, Kulzer B. Trends in diabetes self-management education: Where are we coming from and where are we going? A narrative review. Diabetic Medicine. 2020; 37(3):436-47. [DOI:10.1111/dme.14256] [PMID]
- de Jong SR, van den Hoofdakker BJ, Van Der Veen-Mulders L, Veenman B, Twisk JW, Oosterlaan J, et al. The efficacy of a self-help parenting program for parents of children with externalizing behavior: A randomized controlled trial. European Child & Adolescent Psychiatry. 2023; 32(10):2031-42. [DOI:10.1007/s00787-022-02028-0] [PMID]
- Hautmann C, Dose C, Duda-Kirchhof K, Greimel L, Hellmich M, Imort S, et al. Behavioral versus nonbehavioral guided self-help for parents of children with externalizing disorders in a randomized controlled trial. Behavior Therapy. 2018; 49(6):951-65. [DOI:10.1016/j.beth.2018.02.002] [PMID]
- Pillay J, Armstrong MJ, Butalia S, Donovan LE, Sigal RJ, Chordiya P, et al. Behavioral programs for type 1 diabetes mellitus: A systematic review and meta-analysis. Annals of Internal Medicine. 2015; 163(11):836-47. [PMID]
- Henkemans OAB, Bierman BPB, Janssen J, Looije R, Neerincx MA, van Dooren MMM, et al. Design and evaluation of a personal robot playing a self-management education game with children with diabetes type 1. International Journal of Human-Computer Studies. 2017; 106:63-76. [DOI:10.1016/j.ijhcs.2017.06.001]
- Ortiz La Banca R, Butler DA, Volkening LK, Laffel LM. Play-based interventions delivered by child life Specialists: Teachable moments for youth with type 1 diabetes. Journal of Pediatric Health Care. 2020; 34(4):356-65. [DOI:10.1016/j.pedhc.2020.02.002] [PMID]
- Ritzi RM, Ray DC, Schumann BR. Intensive short-term child-centered play therapy and externalizing behaviors in children. International Journal of Play Therapy. 2017; 26(1):33-46. [DOI:10.1037/pla0000035]
- Cheng WY, Tsai MH. The effect of play therapy on socially withdrawn children’s behaviors and self-concept. Bulletin of Educational Psychology. 2014; 46(2):165–85. [Link]
- La Banca RO, Laffel LMB, Volkening LK, C Sparapani V, de Carvalho EC, Nascimento LC. Therapeutic play to teach children with type 1 diabetes insulin self-injection: A pilot trial in a developing country. Journal for Specialists in Pediatric Nursing. 2021; 26(1):e12309. [DOI:10.1111/jspn.12309] [PMID]
- Carroll NC. Adapting child-centered play therapy for children with type 1 diabetes. International Journal of Play Therapy. 2021; 30(3):187-94. [DOI:10.1037/pla0000158]
- Salmani A, Zargar F, Bagherian R, Mostofizadeh N, Heydari Rarani Z. [The effectiveness of play therapy in improving the mental health of children with type 1 diabetes (Persian)]. Journal of Research in Behavioural Sciences. 2022; 20(3):438-46. [DOI:10.52547/rbs.20.3.438]
- Sadeghi F, Mousavi S, Goudarzi A, Shahsavari MR. The effect of cognitive-behavioral play therapy on emotion regulation and separation anxiety: A quasi-experimental study in elementary-school children in Isfahan. Caspian Journal of Pediatrics. 2022; 8(2):730-8. [Link]
- Lotfi Z. [Evaluation of the effectiveness of patience training through “Shakiba game” on promoting patience in girls (Persian)]. Isfahan: Isfahan university; 2019.
- Ashuri S. [Evaluation of the effectiveness of Shakiba child play therapy(PCP) on controlling aggression in children aged 7-11 years (Persian)]. Tehran: Kharazmi; 2018.
- Neo WS, Suzuki T, Kelleher BL. Structural validity of the Child Behavior Checklist (CBCL) for preschoolers with neurogenetic syndromes. Research in Developmental Disabilities. 2021; 109:103834. [DOI:10.1016/j.ridd.2020.103834] [PMID]
- Shahrivar Z, Shirazi E, Yazdi AB, Alghband-Rad J. Validity of the child behavior Checklist-Persian version in a community sample of Iranian youths. Iranian Journal of Psychiatry and Behavioral Sciences. 2011; 5(1):45-9. [Link]
- No Author. [Gabric Diabetes Education Association (Persian)] [Internet]. 2021 [Updated 18 February 2024]. Available from : [Link]
- Saeid-Rezaei Z, Ghaemi N. [Guidelines for type 1 diabetes in children and adolescents (Persian)]. Mashhad: Mashhad University of Medical Sciences; 2016.
- Afshari M, Gorgi Y. [Application of cognitive-behavioral therapy in psychological problems of type 1 diabetes (Persian)]. Isfahan: Neveshte; 2019.
- Molavi P, Shahrivar Z. [The coping cat (Persian)]. Tehran: Arjmand; 2020.
- Refaghat E. [Teaching life skills using old Iranian stories for children and teenagers (Persian)]. Tehran: Arjmand; 2021.
- Rostami R, Mojtahedy SH, Heidari Z, Ranjbari G, Sadeghi-Firoozabadi V, Ahmadi M. Investigation of cognitive-behavioral play therapy effectiveness on cognitive functions in aggressive children. International Journal of Educational and Psychological Researches. 2017; 3(3):186-91. [DOI:10.4103/jepr.jepr_18_16]
- Cevik Guner U, Celebioglu A. Impact of symptom management training among asthmatic children and adolescents on self-efficacy and disease course. Journal of Asthma. 2015; 52(8):858-65. [DOI:10.3109/02770903.2015.1010732] [PMID]
- Edwards J, Waite-Jones J, Schwarz T, Swallow V. Digital technologies for children and parents sharing self-management in childhood chronic or long-term conditions: A scoping review. Children. 2021; 8(12):1203. [DOI:10.3390/children8121203] [PMID]
- Shrinivasa B, Bukhari M, Ragesh G, Hamza A. Therapeutic intervention for children through play: An overview. Archives of Mental Health. 2018; 19(2):82-9. [Link]
Type of Study: Orginal Article |
Subject:
● Health Education
Received: 2023/01/27 | Accepted: 2023/07/30 | Published: 2024/03/1
Received: 2023/01/27 | Accepted: 2023/07/30 | Published: 2024/03/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |