Volume 14, Issue 5 (Sep & Oct 2024)
J Research Health 2024, 14(5): 489-496 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Khoiriyah K, Sukraeny N, Harmini S, Noysipoom N, Tumme S, Vranada A et al . Anxiety and Depression Following Traumatic Brain Injury. J Research Health 2024; 14 (5) :489-496
URL: http://jrh.gmu.ac.ir/article-1-2454-en.html
URL: http://jrh.gmu.ac.ir/article-1-2454-en.html
Khoiriyah Khoiriyah1 

 , Nury Sukraeny2
, Nury Sukraeny2 

 , Sri Harmini1
, Sri Harmini1 

 , Nittiya Noysipoom3
, Nittiya Noysipoom3 

 , Suttatip Tumme3
, Suttatip Tumme3 

 , Aric Vranada1
, Aric Vranada1 

 , Satriya Pranata1
, Satriya Pranata1 




 , Nury Sukraeny2
, Nury Sukraeny2 

 , Sri Harmini1
, Sri Harmini1 

 , Nittiya Noysipoom3
, Nittiya Noysipoom3 

 , Suttatip Tumme3
, Suttatip Tumme3 

 , Aric Vranada1
, Aric Vranada1 

 , Satriya Pranata1
, Satriya Pranata1 


1- Faculty of Nursing and Health Science, Universitas Muhammadiyah Semarang, Semarang, Indonesia.
2- Faculty of Nursing and Health Science, Universitas Muhammadiyah Semarang, Semarang, Indonesia. ,nury.sukraeny@unimus.ac.id
3- Boromarajonani College of Nursing Nopparat Vajira, Faculty of Nursing, Praboromarajchanok Institute, Nonthaburi, Thailand.
2- Faculty of Nursing and Health Science, Universitas Muhammadiyah Semarang, Semarang, Indonesia. ,
3- Boromarajonani College of Nursing Nopparat Vajira, Faculty of Nursing, Praboromarajchanok Institute, Nonthaburi, Thailand.
Full-Text [PDF 589 kb]
(570 Downloads)
| Abstract (HTML) (2794 Views)
Full-Text: (757 Views)
Introduction
Traumatic brain injury (TBI) is the main cause of mortality and disability globally [1, 2]. It is estimated that 69 million people worldwide experience TBI each year, with Southeast Asia and the Western Pacific region carrying the highest disease burden [3, 4]. The majority (93%) of road traffic fatalities happen in developing countries [3]. More than 70% of trauma-related deaths are anticipated to occur in low- and middle-income countries, where TBI is notably prevalent [5].
The consequences of TBI can profoundly impair the lives of survivors. Long-term physical, cognitive, psychological, and emotional effects of TBI have been recognized [6-8] including TBI. The psychological issues resulting from TBI have been documented. The four-year aggregate adjusted odds ratios for developing an affective disorder following mild TBI were 1.2 (95% CI, 1.1%, 1.2%; P=0.001) and 1.5 (95% CI, 1.5%, 1.6%; P=0.001) in patients with and without prior affective disorders, respectively [9]. A review of studies found that about 22.6% of patients with a history of mild TBI did not exhibit depression or had minimal symptoms, while about 29% displayed moderate to severe depression. Additionally, around 29.3% of TBI patients experienced extreme anxiety in comparison to the control group [1, 10, 11].
In developed countries where access to essential resources and supportive environments is not limited, previous research has shown overwhelmingly positive results. There is uncertainty regarding the prevalence of psychological disorders in TBI patients in Indonesia, where the post-discharge care conditions vary significantly [12]. Studies predicting the outcomes of TBI have used data from low- and middle-income countries, where most TBIs occur. However, the generalization of these data to such contexts, particularly in Indonesia, cannot be assumed [13]. Further exploration is needed to understand the psychological impact of TBI in Indonesia.
In Indonesia, strong family bonds and support are evident through the prevalence of extended families and adult children living with their parents [14]. Regular visits among family members, especially during times of illness or injury, reflect the deeply rooted social norm of ‘tolong-menolong’ (mutual assistance) within Indonesian village communities [15, 16]. In terms of individualism across cultures, Indonesia was ranked 47th out of 53 countries and regions, indicating a high level of social support [17, 18]. Moreover, Indonesia is home to the world’s largest Muslim population, with Islamic principles influencing various aspects of daily life [19]. However, there are limited hospitals offering rehabilitation programs for patients with TBI post-discharge. Access to central referral or tertiary hospitals is primarily available to those who have sustained injuries. Given the culture of mutual assistance and religious influence, further exploration is needed to understand the potential impact of TBI on anxiety and depression in Indonesia. Thus, this study aimed to investigate the correlation between anxiety, depression, and health-related factors in Indonesia among TBI patients.
Methods
Research design
This descriptive cross-sectional study was conducted on 100 TBI patients hospitalized in the neurosurgery unit at Kariadi Hospital. Total sampling was employed, where every patient meeting the inclusion and exclusion criteria was included in the study. Data collection was conducted from December 2022 until February 2023.
Participants
The study recruited patients who met the following criteria: 1) Being diagnosed with mild to severe TBI but still oriented to time, place, and person when approached, 2) The age of between 18 and 65, 3) Passing at least one-month post-hospital discharge and being available for follow-up, and 4) No spinal cord injury, history of or current psychiatric disease, or terminal illness.
Instruments and data collection
The hospital anxiety and depression scale (HADS) is a self-reported assessment tool used to evaluate psychiatric issues. It consists of 14 items, with seven focusing on anxiety and seven on depression. Each item is rated on a four-point scale from 0 to 3, where a score of 3 indicates more frequent symptoms. The total score for each subscale ranges from 0 to 21 and is categorized as follows: Normal (07), mild (810), moderate (11-14), or severe (15-21). The results of the results of the depression “D” and anxiety “A” scales. Cronbach’s α values for the whole scale and the depression and anxiety subscales were 0.94, 0.88, and 0.92, respectively, demonstrating scale consistency [12].
The disability rating scale (DRS) was used to assess functioning and disability. It consists of eight items with a total score of 29. The DRS was designed to gauge changes in recovery levels among adults with TBI by indicating the degree of disability through total scores. Aligned with the World Health Organization (WHO) categories, the DRS evaluates impairment, activity limitation, and participation restriction. Different clinical levels of functioning and disability can be described using its total score, ranging from none (0), mild (1), partial (2-3), moderate (4-6), moderately severe (7-11), severe (12-16), extremely severe (17-21), vegetative state (22-24), to extreme vegetative state (25-29). In-person assessments using the DRS exhibit high inter-rater reliability (r=0.97-0.98) and strong test re-test reliability [20].
The medical outcomes study-social support survey (MOS-SSS) is a survey designed to evaluate the level of social support available to patients with common and treatable chronic diseases. It comprises 19 items and uses a 5-point rating scale, with responses ranging from 1 (never) to 5 (always). The survey is divided into four subscales, including emotional/informational assistance, practical assistance, affectionate assistance, and positive social contact. More support was indicated by a higher score on an individual scale or the overall support index. The mean of the scores for each item within a subscale was calculated to derive a score for each subscale. The overall support index was determined by averaging the scores from the four subscales and additional items. This survey has been validated in Asian countries and demonstrated strong reliability and validity when administered to an adult sample in Taiwan, with Cronbach’s α coefficients exceeding 0.80. In China, Cronbac’s α for the whole scale was 0.98, and test re-test reliability was determined with an intraclass correlation coefficient of 0.84. Its application in the TBI population has been documented [21] information on the psychometric properties of the MOS-SSS.
Demographic and health status data, including age, gender, religion, marital status, educational level, occupation, average income, family situation, time since injury, access to rehabilitation, and present symptoms, were collected and examined from each patient’s medical record. Furthermore, the Glasgow coma scale (GCS) was used to categorize TBI severity: Mild (GCS 13-15), moderate (GCS 9-12), and severe (GCS 8) [22].
Results
The following information presents the demographic characteristics of 100 participants in the study. The Mean±SD age of the subjects was 32.70±12.26 years, with ages ranging from 18 to 59 years. The majority of participants (78%) were male, and the Mean±SD time since injury was 13.77±6.79 months, with a range of 2-24 months. Approximately 58% of the subjects were married, and 37% had an educational level below junior high school. Before the injury, 67% of the subjects worked as laborers, a figure that decreased to 62% post-injury. Unemployment rates increased from 12% to 21% after the injury. The majority of the subjects were Muslim (98%), and 93% lived with family members, ranging from one to nine individuals. Motor accidents were the primary cause of TBIs. Over half of the participants reported experiencing current symptoms, such as headaches (57%), memory problems (12%), fatigue (5%), and vision issues (1%).
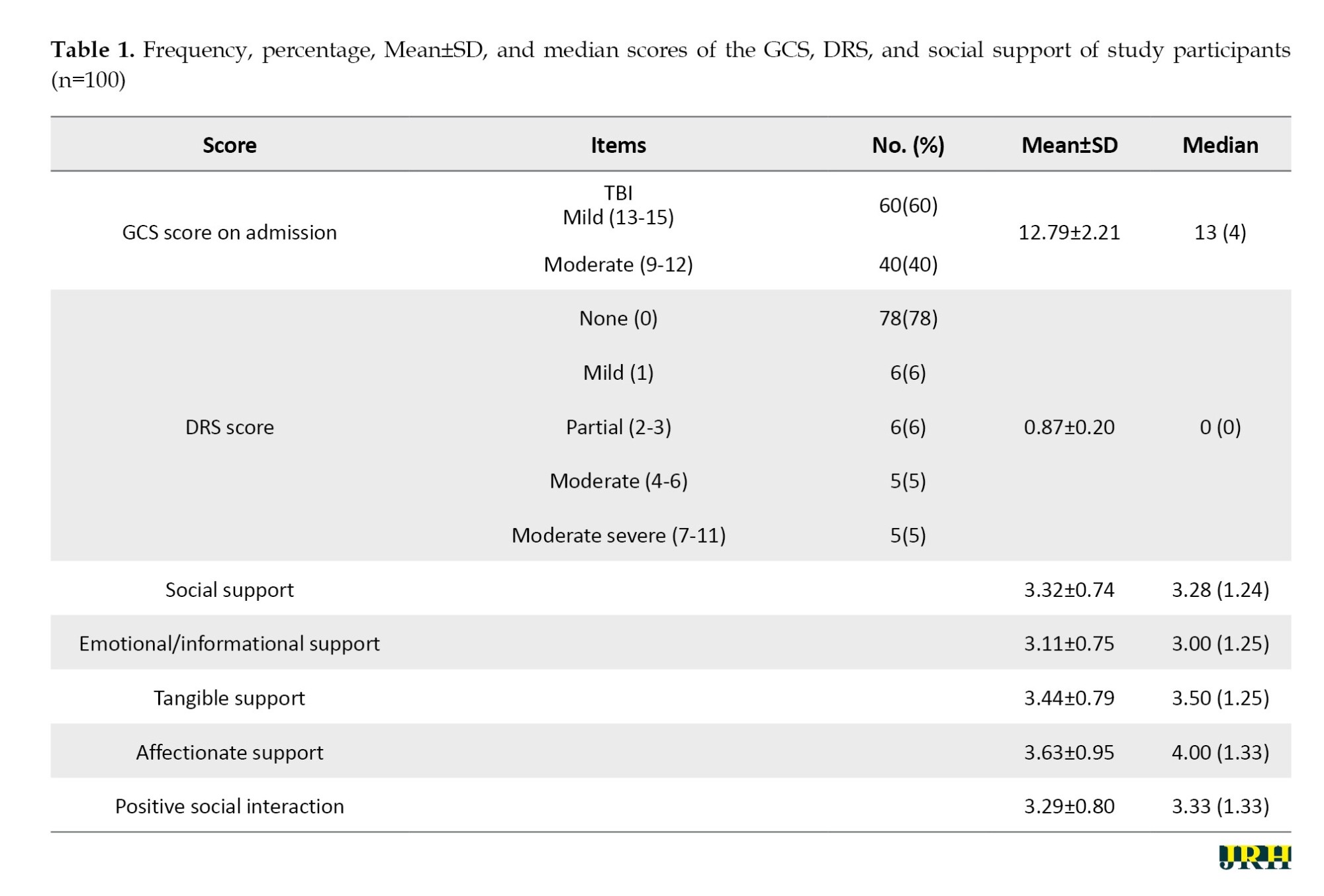
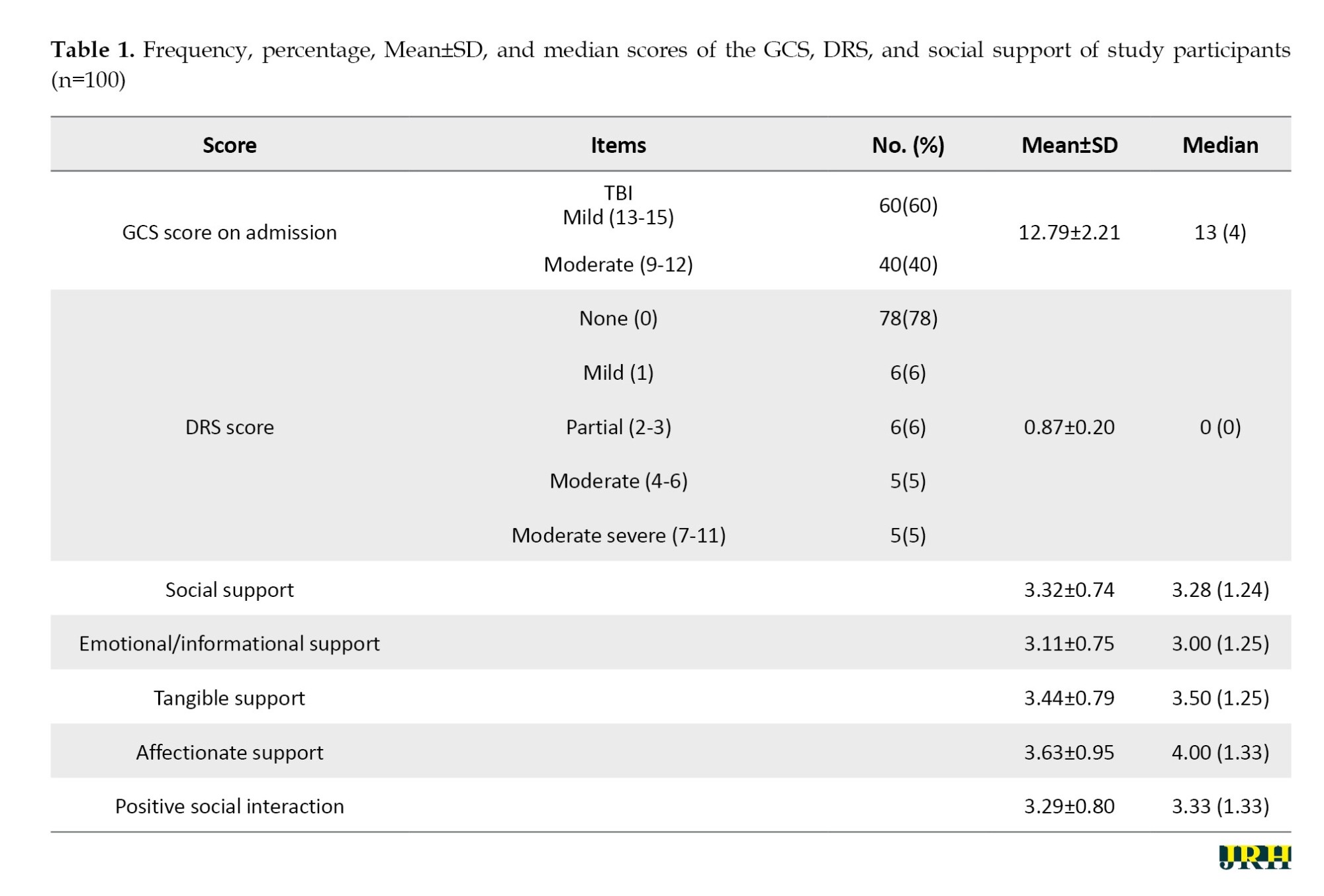
The severity of injury, functioning and disability, and social support
According to the GCS, 60% of the participants were classed as having mild TBI, whereas 40% were diagnosed with moderate TBI. The median GCS score was 13, with an interquartile range (IQR) of four and a range of 6 to 15. Concerning DRS-based functioning and disability, 78% of individuals had no disability, 6% had mild disability, and 10% had moderate to severe disability. The overall mean of social support (3.32±0.74) and four areas of social support, including emotional/informational support (3.11±0.75), tangible support (3.43±0.79), affectionate support (3.63±0.95), and positive social relationship (3.29±0.80), were moderate. Table 1 shows that affectionate support received the highest score, whereas emotional/informational support received the lowest.
The overall mean of social support and the four social support areas, including: 1) Emotional/informational support, 2) Tangible support, 3) Affectionate support, and 4) Positive social relationships, were moderate (Mean±SD social support 3.32±0.74; Mean±SD emotional 3.11±0.75; Mean±SD tangible=3.43±0.79; Mean±SD affectionate 3.63±0.95; Mean±SD positive 3.29±0.80). Table 1 illustrates that affectionate support received the highest score, while emotional/informational support received the lowest.
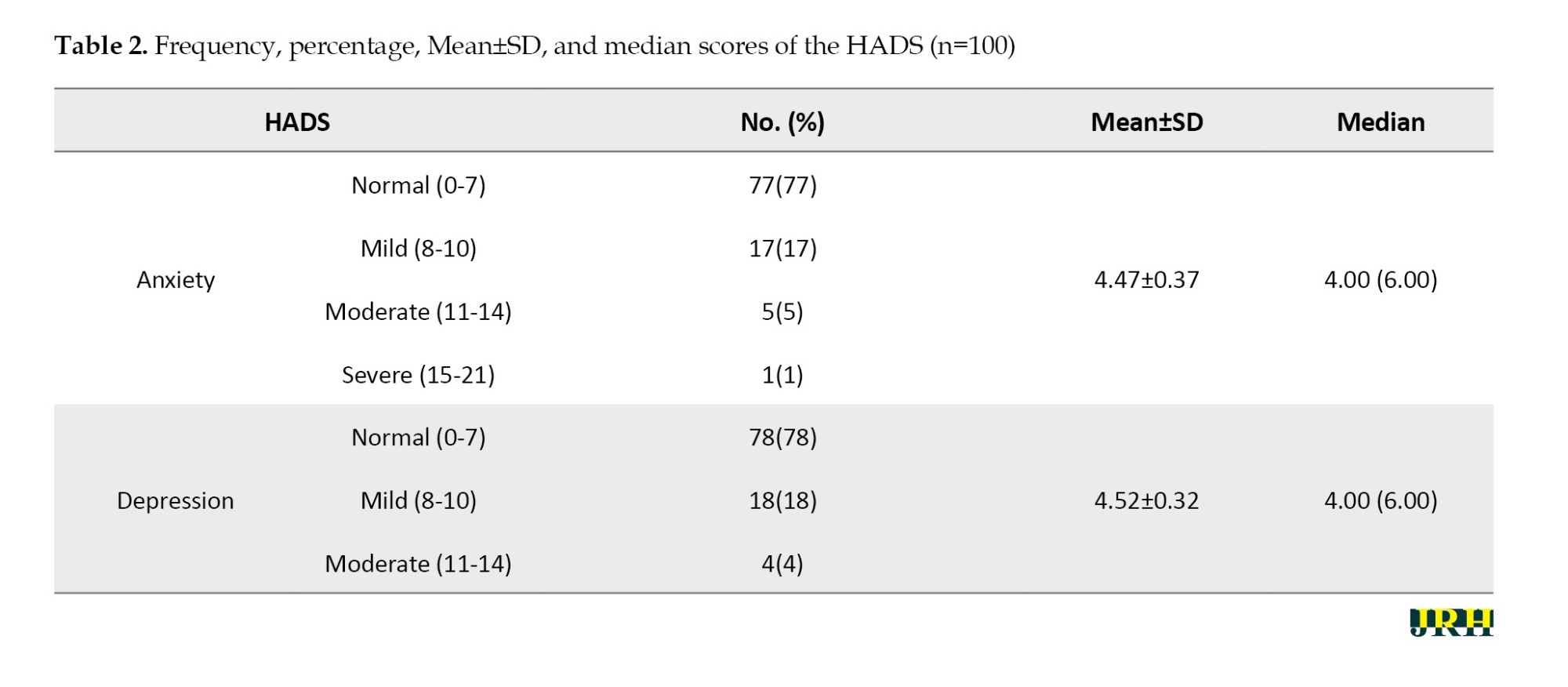
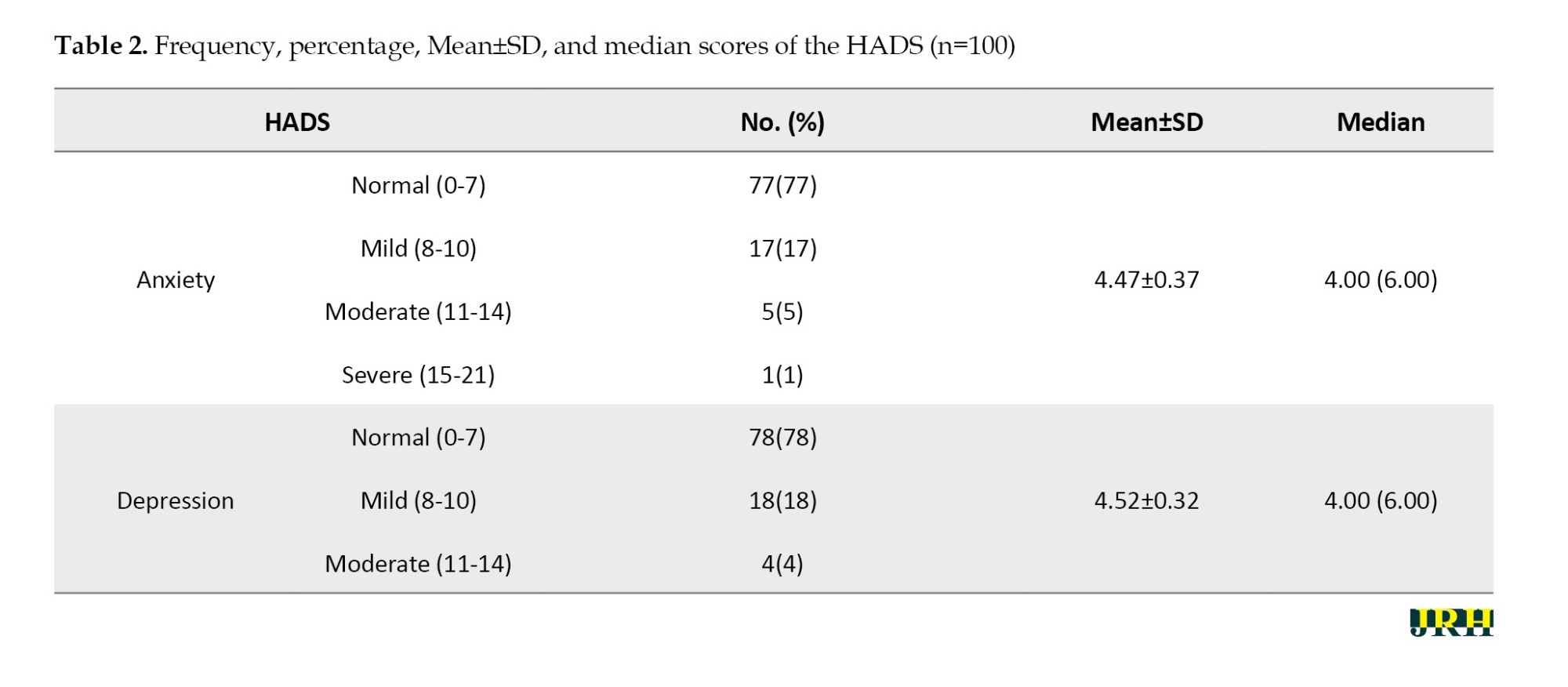
Anxiety and depression
The HADS is divided into two scales: Anxiety and depression. The majority of TBI patients reported normal anxiety levels (77.7%). Furthermore, the majority of the participants exhibited normal levels of depression (78.6%) (Table 2).
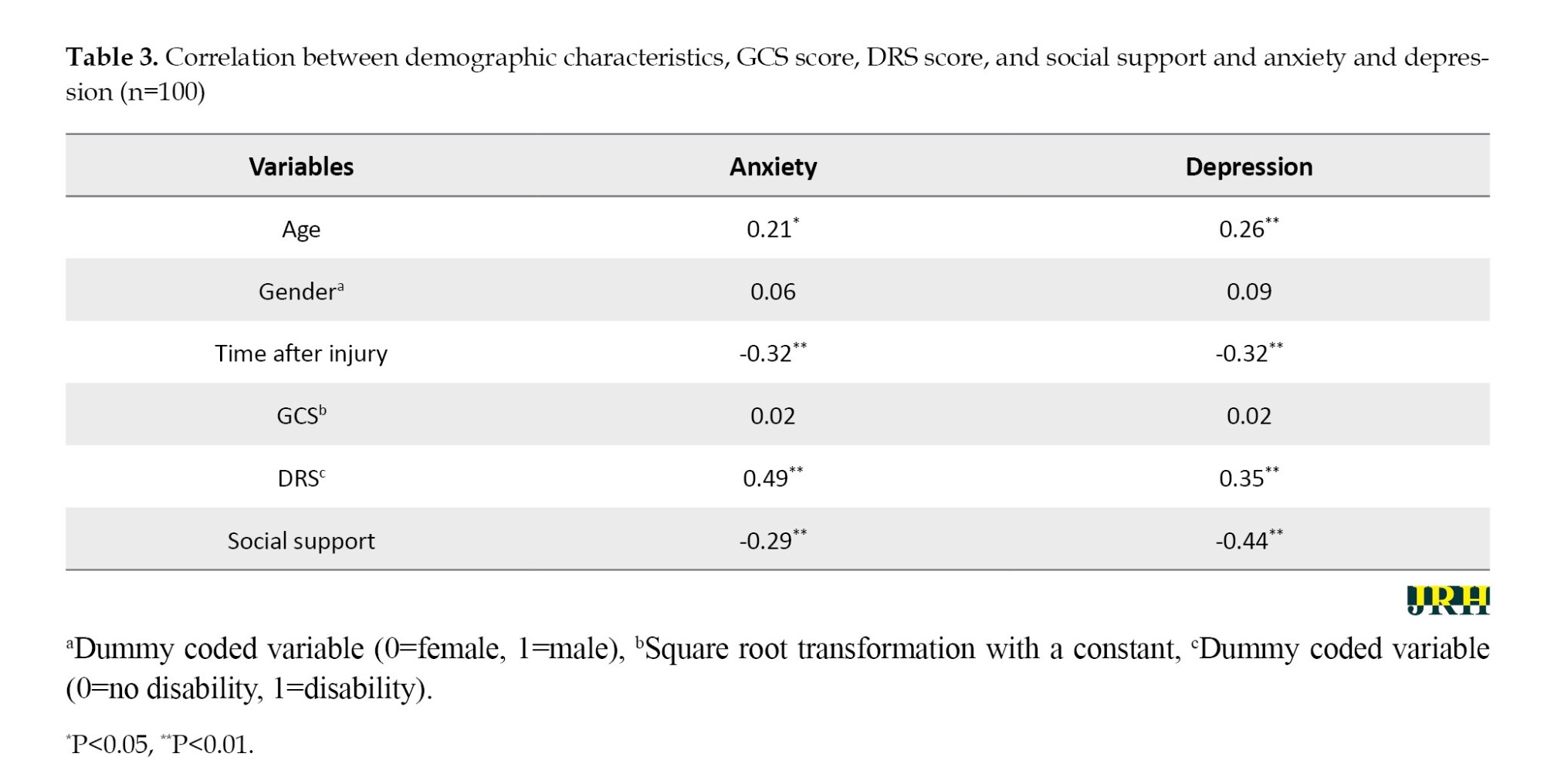
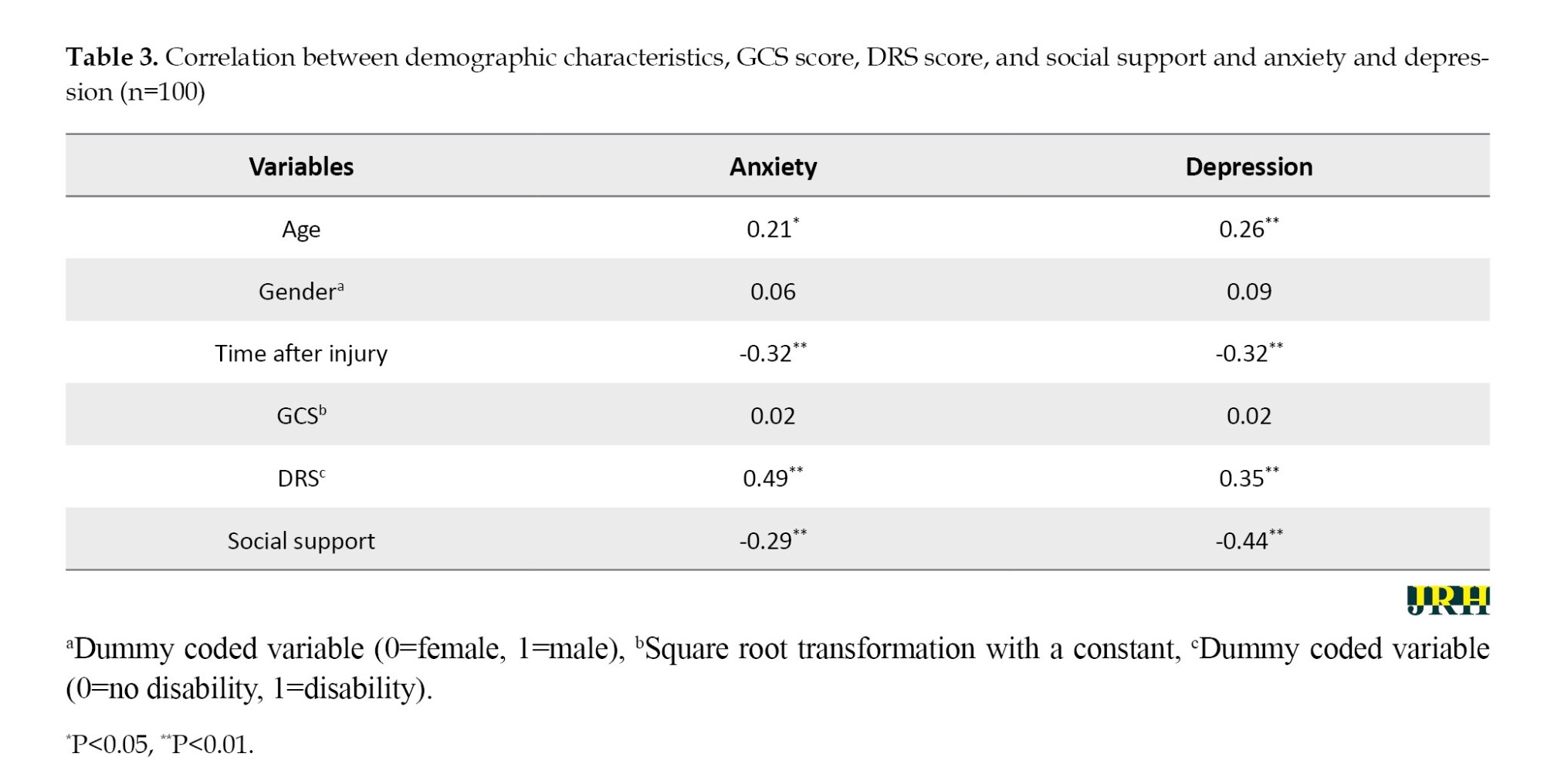
The relationship between the study variables: Social support, functioning and disability, age, and time since injury
Table 3 shows the results of bivariate correlation. Four negative relationships were observed: Time after injury and anxiety, time after injury and depression, social support and anxiety, and social support and depression. Furthermore, four pairs of positive associations were identified: 1) Age and anxiety, 2) Age and depression, 3) Anxiety and functioning and disability, 4) Depression and functioning and disability, and 5) Anxiety and depression.
Discussion
This study supports previous findings regarding anxiety and depression following a TBI. However, the mechanism behind psychological challenges caused by TBI is still unknown. The results showed that anxiety levels among patients after TBI were approximately 22.3%, and depression levels were around 21.4%. A study investigating a potential link between TBI and violent behavior revealed that higher exposure to TBI was indirectly associated with aggressive behavior through negative psychological impacts. According to the findings, the neurological abnormalities usually associated with TBI could result in direct increases in adverse psychological outcomes and indirect increases in subsequent negative behavioral consequences [23, 24]. Physiological changes linked to traumatic brain damage, such as cellular injury, inflammation, and acute stress responses, may also contribute to dysfunctional neuronal networks crucial for emotion regulation [25, 26].
In this study, 22% of participants exhibited depressive symptoms, which were classified as either mild or moderate. The prevalence of depression in the present study was lower than the range of 23 to 64% found in other investigations. Similarly, anxiety symptoms in this study were observed in 23% of participants, which is lower than the range of 40% to 43% seen in other studies. Following a TBI, the occurrence of anxiety and depression has been noted. A comprehensive evaluation indicates that many patients experience anxiety and depression persisting over time after a TBI [27]. Prior to the TBI event, the prevalence estimates for anxiety and depressive disorders were 19% and 13%, respectively. Within the first year post-TBI, the estimates for anxiety and depressive disorders rose to 21% and 17%, respectively. These estimates continued to increase over time, indicating a high long-term prevalence of axis I disorders (54%), encompassing anxiety disorders (36%) and depressive disorders (34%) [27, 28].
The low rates of anxiety and depression in this study could also be due to Indonesia's religious culture. Most subjects in this study were Muslim comprising 98% of the participants. The influence of religious beliefs on daily life is significant. Religion is known to alleviate frustration [29, 30]. Some studies have linked religiosity to increased longevity and disease resistance. Religion facilitates coping with illness and the healing process. Spirituality and religion also aid patients in adapting to illness and finding meaning and purpose [29].
This study found a significant correlation between age and anxiety or depression. This finding aligns with research indicating that older individuals are more prone to developing depression following a TBI [9, 31]. While another study suggested that younger age groups had a higher incidence of depression, older TBI patients may experience slower recovery and are more susceptible to developing complications as they age [32].
This study revealed no relationship between gender and anxiety or depression. This conclusion can be explained by the fact that the majority of individuals who suffered from TBI were male. In males, TBI raised the risk of depression by 2.03 times, with a 95% CI ranging from 1.97 to 2.10. A large-scale longitudinal analysis of adults revealed that males were more likely to suffer from depression following a TBI compared to females. Additionally, a study found that anxiety and depression disorders were more common in females who were unemployed or had psychiatric issues before the TBI event [33].
There was an association between disability and functioning and psychological issues (depression and anxiety). Cross-tabulation revealed that 59% of respondents who reported depressive symptoms had current headaches, memory issues, fatigue, and visual impairments. It was found that 68% of the participants were disabled, and this was accompanied by a rise in the symptoms of depression and anxiety. This association aligns with a previous study’s findings, indicating that changes in daily functioning can impact emotional well-being following a TBI. Another study suggested that depression in TBI patients might be linked to insufficient medical treatment and poor adherence to therapy, although this particular study did not investigate these findings further [34, 35].
This study revealed no correlation between injury severity (as defined by GCS) and anxiety or depression. Regarding TBI severity, conflicting results were obtained. Between 8-18% of patients with mild TBI were diagnosed with severe depression, compared to 7-63% of all TBI patients. Nevertheless, previous research has not established a significant link between TBI severity and the risk of depressive disorders. This suggests that individuals who have experienced mild, moderate, or severe TBI are all susceptible to post-injury psychiatric issues, such as anxiety and depression [9-11].
In this investigation, a negative association was identified between anxiety, depression, and social support. This means that individuals lacking social support are more likely to experience heightened levels of depression and anxiety symptoms. These findings align with the social support buffering model theory [36, 37]. The presence of social support can enhance individuals’ ability to cope with chronic illness by boosting their confidence and reducing their perception of illness-related distress. Family care, which is a form of social support, was found to be particularly beneficial for patients with TBI. In Indonesia, where a majority of patients resided with their families, the strong social support network contributed to lower levels of anxiety and sadness.
Conclusion
Anxiety and depression are prevalent issues among individuals who have suffered from TBI in Indonesia. The study found that 22.3%of participants experienced anxiety, while 21.4% experienced depression. Additionally, anxiety and depression were statistically linked to factors, such as social support, functioning and disability, age, and duration of injury. Early identification and management of these psychological issues are crucial for individuals who have undergone TBI.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from the Research Ethics Committee of Universitas Muhammadiyah Semarang, on October 07, 2022 (Code: INA/078/2022).
Funding
This study was supported by the Universitas Muhammadiyah Semarang, Semarang, Indonesia (Grant No.: 031/UNIMUS/2022).
Authors' contributions
Conceptualization, study design, and writing the first draft and framework: Khoiriyah Khoiriyah, and Nury Sukraeny; Data collection: Aric Vranada, and Satriya Pranata; Data analysis: Khoiriyah Khoiriyah, Nury Sukraeny, and Sri Harmini; Data interpretation: Sri Harmini, Nittiya Noysipoom, Suttatip Tumme; Khoiriyah Khoiriyah, Nury Sukraeny, and Sri Harmini; Supervision: Sri Harmini, Nittiya Noysipoom, and Suttatip Tumme; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their thanks to the Universitas Muhammadiyah Semarang for funding the study.
References
Traumatic brain injury (TBI) is the main cause of mortality and disability globally [1, 2]. It is estimated that 69 million people worldwide experience TBI each year, with Southeast Asia and the Western Pacific region carrying the highest disease burden [3, 4]. The majority (93%) of road traffic fatalities happen in developing countries [3]. More than 70% of trauma-related deaths are anticipated to occur in low- and middle-income countries, where TBI is notably prevalent [5].
The consequences of TBI can profoundly impair the lives of survivors. Long-term physical, cognitive, psychological, and emotional effects of TBI have been recognized [6-8] including TBI. The psychological issues resulting from TBI have been documented. The four-year aggregate adjusted odds ratios for developing an affective disorder following mild TBI were 1.2 (95% CI, 1.1%, 1.2%; P=0.001) and 1.5 (95% CI, 1.5%, 1.6%; P=0.001) in patients with and without prior affective disorders, respectively [9]. A review of studies found that about 22.6% of patients with a history of mild TBI did not exhibit depression or had minimal symptoms, while about 29% displayed moderate to severe depression. Additionally, around 29.3% of TBI patients experienced extreme anxiety in comparison to the control group [1, 10, 11].
In developed countries where access to essential resources and supportive environments is not limited, previous research has shown overwhelmingly positive results. There is uncertainty regarding the prevalence of psychological disorders in TBI patients in Indonesia, where the post-discharge care conditions vary significantly [12]. Studies predicting the outcomes of TBI have used data from low- and middle-income countries, where most TBIs occur. However, the generalization of these data to such contexts, particularly in Indonesia, cannot be assumed [13]. Further exploration is needed to understand the psychological impact of TBI in Indonesia.
In Indonesia, strong family bonds and support are evident through the prevalence of extended families and adult children living with their parents [14]. Regular visits among family members, especially during times of illness or injury, reflect the deeply rooted social norm of ‘tolong-menolong’ (mutual assistance) within Indonesian village communities [15, 16]. In terms of individualism across cultures, Indonesia was ranked 47th out of 53 countries and regions, indicating a high level of social support [17, 18]. Moreover, Indonesia is home to the world’s largest Muslim population, with Islamic principles influencing various aspects of daily life [19]. However, there are limited hospitals offering rehabilitation programs for patients with TBI post-discharge. Access to central referral or tertiary hospitals is primarily available to those who have sustained injuries. Given the culture of mutual assistance and religious influence, further exploration is needed to understand the potential impact of TBI on anxiety and depression in Indonesia. Thus, this study aimed to investigate the correlation between anxiety, depression, and health-related factors in Indonesia among TBI patients.
Methods
Research design
This descriptive cross-sectional study was conducted on 100 TBI patients hospitalized in the neurosurgery unit at Kariadi Hospital. Total sampling was employed, where every patient meeting the inclusion and exclusion criteria was included in the study. Data collection was conducted from December 2022 until February 2023.
Participants
The study recruited patients who met the following criteria: 1) Being diagnosed with mild to severe TBI but still oriented to time, place, and person when approached, 2) The age of between 18 and 65, 3) Passing at least one-month post-hospital discharge and being available for follow-up, and 4) No spinal cord injury, history of or current psychiatric disease, or terminal illness.
Instruments and data collection
The hospital anxiety and depression scale (HADS) is a self-reported assessment tool used to evaluate psychiatric issues. It consists of 14 items, with seven focusing on anxiety and seven on depression. Each item is rated on a four-point scale from 0 to 3, where a score of 3 indicates more frequent symptoms. The total score for each subscale ranges from 0 to 21 and is categorized as follows: Normal (07), mild (810), moderate (11-14), or severe (15-21). The results of the results of the depression “D” and anxiety “A” scales. Cronbach’s α values for the whole scale and the depression and anxiety subscales were 0.94, 0.88, and 0.92, respectively, demonstrating scale consistency [12].
The disability rating scale (DRS) was used to assess functioning and disability. It consists of eight items with a total score of 29. The DRS was designed to gauge changes in recovery levels among adults with TBI by indicating the degree of disability through total scores. Aligned with the World Health Organization (WHO) categories, the DRS evaluates impairment, activity limitation, and participation restriction. Different clinical levels of functioning and disability can be described using its total score, ranging from none (0), mild (1), partial (2-3), moderate (4-6), moderately severe (7-11), severe (12-16), extremely severe (17-21), vegetative state (22-24), to extreme vegetative state (25-29). In-person assessments using the DRS exhibit high inter-rater reliability (r=0.97-0.98) and strong test re-test reliability [20].
The medical outcomes study-social support survey (MOS-SSS) is a survey designed to evaluate the level of social support available to patients with common and treatable chronic diseases. It comprises 19 items and uses a 5-point rating scale, with responses ranging from 1 (never) to 5 (always). The survey is divided into four subscales, including emotional/informational assistance, practical assistance, affectionate assistance, and positive social contact. More support was indicated by a higher score on an individual scale or the overall support index. The mean of the scores for each item within a subscale was calculated to derive a score for each subscale. The overall support index was determined by averaging the scores from the four subscales and additional items. This survey has been validated in Asian countries and demonstrated strong reliability and validity when administered to an adult sample in Taiwan, with Cronbach’s α coefficients exceeding 0.80. In China, Cronbac’s α for the whole scale was 0.98, and test re-test reliability was determined with an intraclass correlation coefficient of 0.84. Its application in the TBI population has been documented [21] information on the psychometric properties of the MOS-SSS.
Demographic and health status data, including age, gender, religion, marital status, educational level, occupation, average income, family situation, time since injury, access to rehabilitation, and present symptoms, were collected and examined from each patient’s medical record. Furthermore, the Glasgow coma scale (GCS) was used to categorize TBI severity: Mild (GCS 13-15), moderate (GCS 9-12), and severe (GCS 8) [22].
Results
The following information presents the demographic characteristics of 100 participants in the study. The Mean±SD age of the subjects was 32.70±12.26 years, with ages ranging from 18 to 59 years. The majority of participants (78%) were male, and the Mean±SD time since injury was 13.77±6.79 months, with a range of 2-24 months. Approximately 58% of the subjects were married, and 37% had an educational level below junior high school. Before the injury, 67% of the subjects worked as laborers, a figure that decreased to 62% post-injury. Unemployment rates increased from 12% to 21% after the injury. The majority of the subjects were Muslim (98%), and 93% lived with family members, ranging from one to nine individuals. Motor accidents were the primary cause of TBIs. Over half of the participants reported experiencing current symptoms, such as headaches (57%), memory problems (12%), fatigue (5%), and vision issues (1%).
The severity of injury, functioning and disability, and social support
According to the GCS, 60% of the participants were classed as having mild TBI, whereas 40% were diagnosed with moderate TBI. The median GCS score was 13, with an interquartile range (IQR) of four and a range of 6 to 15. Concerning DRS-based functioning and disability, 78% of individuals had no disability, 6% had mild disability, and 10% had moderate to severe disability. The overall mean of social support (3.32±0.74) and four areas of social support, including emotional/informational support (3.11±0.75), tangible support (3.43±0.79), affectionate support (3.63±0.95), and positive social relationship (3.29±0.80), were moderate. Table 1 shows that affectionate support received the highest score, whereas emotional/informational support received the lowest.
The overall mean of social support and the four social support areas, including: 1) Emotional/informational support, 2) Tangible support, 3) Affectionate support, and 4) Positive social relationships, were moderate (Mean±SD social support 3.32±0.74; Mean±SD emotional 3.11±0.75; Mean±SD tangible=3.43±0.79; Mean±SD affectionate 3.63±0.95; Mean±SD positive 3.29±0.80). Table 1 illustrates that affectionate support received the highest score, while emotional/informational support received the lowest.
Anxiety and depression
The HADS is divided into two scales: Anxiety and depression. The majority of TBI patients reported normal anxiety levels (77.7%). Furthermore, the majority of the participants exhibited normal levels of depression (78.6%) (Table 2).
The relationship between the study variables: Social support, functioning and disability, age, and time since injury
Table 3 shows the results of bivariate correlation. Four negative relationships were observed: Time after injury and anxiety, time after injury and depression, social support and anxiety, and social support and depression. Furthermore, four pairs of positive associations were identified: 1) Age and anxiety, 2) Age and depression, 3) Anxiety and functioning and disability, 4) Depression and functioning and disability, and 5) Anxiety and depression.
Discussion
This study supports previous findings regarding anxiety and depression following a TBI. However, the mechanism behind psychological challenges caused by TBI is still unknown. The results showed that anxiety levels among patients after TBI were approximately 22.3%, and depression levels were around 21.4%. A study investigating a potential link between TBI and violent behavior revealed that higher exposure to TBI was indirectly associated with aggressive behavior through negative psychological impacts. According to the findings, the neurological abnormalities usually associated with TBI could result in direct increases in adverse psychological outcomes and indirect increases in subsequent negative behavioral consequences [23, 24]. Physiological changes linked to traumatic brain damage, such as cellular injury, inflammation, and acute stress responses, may also contribute to dysfunctional neuronal networks crucial for emotion regulation [25, 26].
In this study, 22% of participants exhibited depressive symptoms, which were classified as either mild or moderate. The prevalence of depression in the present study was lower than the range of 23 to 64% found in other investigations. Similarly, anxiety symptoms in this study were observed in 23% of participants, which is lower than the range of 40% to 43% seen in other studies. Following a TBI, the occurrence of anxiety and depression has been noted. A comprehensive evaluation indicates that many patients experience anxiety and depression persisting over time after a TBI [27]. Prior to the TBI event, the prevalence estimates for anxiety and depressive disorders were 19% and 13%, respectively. Within the first year post-TBI, the estimates for anxiety and depressive disorders rose to 21% and 17%, respectively. These estimates continued to increase over time, indicating a high long-term prevalence of axis I disorders (54%), encompassing anxiety disorders (36%) and depressive disorders (34%) [27, 28].
The low rates of anxiety and depression in this study could also be due to Indonesia's religious culture. Most subjects in this study were Muslim comprising 98% of the participants. The influence of religious beliefs on daily life is significant. Religion is known to alleviate frustration [29, 30]. Some studies have linked religiosity to increased longevity and disease resistance. Religion facilitates coping with illness and the healing process. Spirituality and religion also aid patients in adapting to illness and finding meaning and purpose [29].
This study found a significant correlation between age and anxiety or depression. This finding aligns with research indicating that older individuals are more prone to developing depression following a TBI [9, 31]. While another study suggested that younger age groups had a higher incidence of depression, older TBI patients may experience slower recovery and are more susceptible to developing complications as they age [32].
This study revealed no relationship between gender and anxiety or depression. This conclusion can be explained by the fact that the majority of individuals who suffered from TBI were male. In males, TBI raised the risk of depression by 2.03 times, with a 95% CI ranging from 1.97 to 2.10. A large-scale longitudinal analysis of adults revealed that males were more likely to suffer from depression following a TBI compared to females. Additionally, a study found that anxiety and depression disorders were more common in females who were unemployed or had psychiatric issues before the TBI event [33].
There was an association between disability and functioning and psychological issues (depression and anxiety). Cross-tabulation revealed that 59% of respondents who reported depressive symptoms had current headaches, memory issues, fatigue, and visual impairments. It was found that 68% of the participants were disabled, and this was accompanied by a rise in the symptoms of depression and anxiety. This association aligns with a previous study’s findings, indicating that changes in daily functioning can impact emotional well-being following a TBI. Another study suggested that depression in TBI patients might be linked to insufficient medical treatment and poor adherence to therapy, although this particular study did not investigate these findings further [34, 35].
This study revealed no correlation between injury severity (as defined by GCS) and anxiety or depression. Regarding TBI severity, conflicting results were obtained. Between 8-18% of patients with mild TBI were diagnosed with severe depression, compared to 7-63% of all TBI patients. Nevertheless, previous research has not established a significant link between TBI severity and the risk of depressive disorders. This suggests that individuals who have experienced mild, moderate, or severe TBI are all susceptible to post-injury psychiatric issues, such as anxiety and depression [9-11].
In this investigation, a negative association was identified between anxiety, depression, and social support. This means that individuals lacking social support are more likely to experience heightened levels of depression and anxiety symptoms. These findings align with the social support buffering model theory [36, 37]. The presence of social support can enhance individuals’ ability to cope with chronic illness by boosting their confidence and reducing their perception of illness-related distress. Family care, which is a form of social support, was found to be particularly beneficial for patients with TBI. In Indonesia, where a majority of patients resided with their families, the strong social support network contributed to lower levels of anxiety and sadness.
Conclusion
Anxiety and depression are prevalent issues among individuals who have suffered from TBI in Indonesia. The study found that 22.3%of participants experienced anxiety, while 21.4% experienced depression. Additionally, anxiety and depression were statistically linked to factors, such as social support, functioning and disability, age, and duration of injury. Early identification and management of these psychological issues are crucial for individuals who have undergone TBI.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from the Research Ethics Committee of Universitas Muhammadiyah Semarang, on October 07, 2022 (Code: INA/078/2022).
Funding
This study was supported by the Universitas Muhammadiyah Semarang, Semarang, Indonesia (Grant No.: 031/UNIMUS/2022).
Authors' contributions
Conceptualization, study design, and writing the first draft and framework: Khoiriyah Khoiriyah, and Nury Sukraeny; Data collection: Aric Vranada, and Satriya Pranata; Data analysis: Khoiriyah Khoiriyah, Nury Sukraeny, and Sri Harmini; Data interpretation: Sri Harmini, Nittiya Noysipoom, Suttatip Tumme; Khoiriyah Khoiriyah, Nury Sukraeny, and Sri Harmini; Supervision: Sri Harmini, Nittiya Noysipoom, and Suttatip Tumme; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their thanks to the Universitas Muhammadiyah Semarang for funding the study.
References
- Karr JE, Williams MW, Iverson GL, Huang SJ, Yang CC. Pre-Injury headache and post-traumatic headache in patients with mild traumatic brain injury: Neuropsychological, psychiatric, and post-concussion symptom outcomes. Brain Injury. 2022; 36(2):175-82. [DOI:10.1080/02699052.2022.2043440] [PMID]
- Wilson A, Gicas K, Wojtowicz M. Influence of mild traumatic brain injury history and mental health status on alcohol and cannabis use in university athletes. Clinical Journal of Sport Medicine. 2023; 33(2):145-50. [DOI:10.1097/JSM.0000000000001110] [PMID]
- Raju B, R KT, Konar S, Shukla D, Kukkehalli R. Prehospital impact on family members of road traffic accident. Journal of Neurosciences in Rural Practice. 2021; 12(2):350-5. [DOI:10.1055/s-0041-1723063] [PMID] [PMCID]
- Pan Y, Zhu H, Hou L. Epidemiological analysis and emergency nursing care of oral and craniomaxillofacial trauma: A narrative review. Annals of Palliative Medicine. 2022; 11(4):1518-25. [DOI:10.21037/apm-21-2995] [PMID]
- Kalra S, Banderwal R, Arora K, Kumar S, Singh G, Chawla PA, et al. An update on pathophysiology and treatment of sports-mediated brain injury. Environmental Science and Pollution Research International. 2022; 29(12):16786-98. [DOI:10.1007/s11356-021-18391-5] [PMID]
- Ablin JN, Lang E, Catalogna M, Aloush V, Hadanny A, Doenyas-Barak K, et al. Hyperbaric oxygen therapy compared to pharmacological intervention in fibromyalgia patients following traumatic brain injury: A randomized, controlled trial. Plos One. 2023; 18(3):e0282406. [DOI:10.1371/journal.pone.0282406] [PMID] [PMCID]
- Lequerica AH, Shoval HA, Yalamanchi K, Lengenfelder J, Marchetta C, Ace J, et al. Examining the use of a rest-activity ratio in a pediatric rehabilitation setting. Archives of Physical Medicine and Rehabilitation. 2022; 103(9):1766-70. [DOI:10.1016/j.apmr.2021.12.027] [PMID]
- Perrin PB, Klyce DW, Fisher LB, Juengst SB, Hammond FM, Gary KW, et al. Relations among suicidal ideation, depressive symptoms, and functional independence during the 10 years after traumatic brain injury: A model systems study. Archives of Physical Medicine and Rehabilitation. 2022; 103(1):69-74. [DOI:10.1016/j.apmr.2021.07.790] [PMID]
- Al-Kader DA, Onyechi CI, Ikedum IV, Fattah A, Zafar S, Bhat S, et al. Depression and anxiety in patients with a history of traumatic brain injury: A case-control study. Cureus. 2022; 14(8):e27971. [DOI:10.7759/cureus.27971]
- Keatley ES, Bombardier CH, Watson E, Kumar RG, Novack T, Monden KR, et al. Cognitive performance, depression, and anxiety 1 year after traumatic brain injury. The Journal of Head Trauma Rehabilitation. 2023; 38(3):E195-202. [DOI:10.1097/HTR.0000000000000819] [PMID] [PMCID]
- Lamontagne G, Belleville G, Beaulieu-Bonneau S, Souesme G, Savard J, Sirois MJ, et al. Anxiety symptoms and disorders in the first year after sustaining mild traumatic brain injury. Rehabilitation Psychology. 2022; 67(1):90-9. [DOI:10.1037/rep0000422] [PMID]
- Tiksnadi BB, Triani N, Fihaya FY, Turu' Allo IJ, Iskandar S, Putri DAE. Validation of hospital anxiety and depression scale in an Indonesian population: A scale adaptation study. Family Medicine and Community Health. 2023; 11(2):e001775. [DOI:10.1136/fmch-2022-001775] [PMID] [PMCID]
- Pugh M Jr, Perrin PB, Arango-Lasprilla JC. Predicting caregiver burden over the first 4 months after acute traumatic brain injury in Latin America: A multi-country study. Brain Injury. 2021; 35(7):769-77. [DOI:10.1080/02699052.2021.1907861] [PMID] [PMCID]
- Ross LT, Heming B, Lane A. Family unpredictability and sense of coherence: Relationships with anxiety and depression in two samples. Psychological Reports. 2023; 126(4):1701-24. [DOI:10.1177/00332941221080409] [PMID]
- King G, Nalder E, Stacey L, Hartman LR. Investigating the adaptation of caregivers of people with traumatic brain injury: A journey told in evolving research traditions. Disability and Rehabilitation. 2021; 43(21):3102-16. [DOI:10.1080/09638288.2020.1725158] [PMID]
- Borgen IMH, Kleffelgård I, Hauger SL, Forslund MV, Søberg HL, Andelic N, et al. Patient-reported problem areas in chronic traumatic brain injury. The Journal of Head Trauma Rehabilitation. 2022; 37(5):E336-45. [DOI:10.1097/HTR.0000000000000744] [PMID]
- Mahendradhata Y, Trisnantoro L, Listyadewi S, Soewondo P, Marthias T, Harimurti P, Prawira J. The Republic of Indonesia health system review. Health Systems in Transition. 2017; 7(1): WHO Regional Office for South-East Asia. [Link]
- Priester L De. An approach to the profile of disaster risk of Indonesia. Emergency and Disaster Reports. 2016; 3(2):5-66. [Link]
- Huda N, Nurchayati S, Pranata S, Sansuwito T. Religion and spirituality in coping with cancer among muslims: A literature review. The Malaysian Journal of Nursing. 2022; 14(2):151-6. [DOI:10.31674/mjn.2022.v14i02.025]
- Phedy P, Djaja YP, Tobing SDAL, Gatam L, Librianto D, Fachrisal, et al. Cross-cultural adaptation and psychometric validation of the Indonesian version of the oswestry disability index. European Spine Journal. 2021; 30(4):1053-62. [DOI:10.1007/s00586-020-06690-3] [PMID]
- Merino-Soto C, Núñez Benítez MÁ, Domínguez-Guedea MT, Toledano-Toledano F, Moral de la Rubia J, Astudillo-García CI, et al. Medical outcomes study social support survey (MOS-SSS) in patients with chronic disease: A psychometric assessment. Frontiers in Psychiatry. 2023; 13:1028342. [DOI:10.3389/fpsyt.2022.1028342] [PMID] [PMCID]
- Carmichael J, Hicks AJ, Gould KR, Ponsford J, Spitz G. Ten-Year cohort study of emotional distress trajectories after moderate-severe traumatic brain injury. Archives of Physical Medicine and Rehabilitation. 2023; 104(7):1081-90. [DOI:10.1016/j.apmr.2023.02.008] [PMID]
- Toccalino D, Moore A, Cripps E, Gutierrez SC, Colantonio A, Wickens CM, et al. Exploring the intersection of brain injury and mental health in survivors of intimate partner violence: A scoping review. Frontiers in Public Health. 2023; 11:1100549. [DOI:10.3389/fpubh.2023.1100549] [PMID] [PMCID]
- Jones KM, Ameratunga S, Starkey NJ, Theadom A, Barker-Collo S, Ikeda T, et al. Psychosocial functioning at 4-years after pediatric mild traumatic brain injury. Brain Injury. 2021; 35(4):416-25. [DOI:10.1080/02699052.2021.1878553] [PMID]
- Benavides AM, Finn JA, Tang X, Ropacki S, Brown RM, Smith AN, et al. Psychosocial and functional predictors of depression and anxiety symptoms in veterans and service members with TBI: A VA TBI model systems study. The Journal of Head Trauma Rehabilitation. 2021; 36(6):397-407. [DOI:10.1097/HTR.0000000000000647] [PMID]
- Braun D, Schöniger C, Pyrc J, Petrowski K. Traumatic brain injury as vulnerability factor for the development of psychological disorders in a prospective single-event trauma traffic accident sample. Brain Injury. 2021; 35(5):604-8. [DOI:10.1080/02699052.2021.1894480] [PMID]
- Dromer E, Kheloufi L, Azouvi P. Impaired self-awareness after traumatic brain injury: A systematic review. Part 2. Consequences and predictors of poor self-awareness. Annals of Physical and Rehabilitation Medicine. 2021; 64(5):101542. [DOI:10.1016/j.rehab.2021.101542] [PMID]
- Chan V, Toccalino D, Omar S, Shah R, Colantonio A. A systematic review on integrated care for traumatic brain injury, mental health, and substance use. Plos One. 2022; 17(3):e0264116. [DOI:10.1371/journal.pone.0264116] [PMID] [PMCID]
- Koenig HG, Al Zaben F. Moral injury: An increasingly recognized and widespread syndrome. Journal of Religion and Health. 2021; 60(5):2989-3011. [DOI:10.1007/s10943-021-01328-0] [PMID] [PMCID]
- Ayesha, Ahmad S, Saba S, Kashif M, Khan DA, Haque A, et al. The relationship between psychological disability and religious practice and coping strategies in caregivers of children with traumatic brain injury in Pakistani population. Healthcare. 2022; 10(11):2158. [DOI:10.3390/healthcare10112158] [PMID] [PMCID]
- Katta-Charles S, Adams LM, Chiaravalloti ND, Hammond FM, Perrin PB, Rabinowitz AR, et al. Depression, anxiety, and suicidality in individuals with chronic traumatic brain injury before and during the COVID-19 pandemic: A national institute on disability, independent living, and rehabilitation research traumatic brain injury model systems study. Archives of Physical Medicine and Rehabilitation. 2023; 104(4):619-30. [DOI:10.1016/j.apmr.2022.10.017] [PMID] [PMCID]
- Levin HS, Temkin NR, Barber J, Nelson LD, Robertson C, Brennan J, et al. Association of sex and age with mild traumatic brain injury–related symptoms: A TRACK-TBI study. JAMA Network Open. 2021; 4(4):e213046. [DOI:10.1001/jamanetworkopen.2021.3046]
- Cogan AM, Smith B, Bender Pape TL, Mallinson T, Eapen BC, Scholten J. Self-reported participation restrictions among male and female veterans with traumatic brain injury in veterans health administration outpatient polytrauma programs. Archives of Physical Medicine and Rehabilitation. 2020; 101(12):2071-9. [DOI:10.1016/j.apmr.2020.06.030] [PMID]
- Faulkner JW, Snell DL, Theadom A, Mahon S, Barker-Collo S. The influence of psychological flexibility on persistent post concussion symptoms and functional status after mild traumatic brain injury. Disability and Rehabilitation. 2023; 45(7):1192-201. [DOI:10.1080/09638288.2022.2055167] [PMID]
- Corrigan JD. Traumatic brain injury and treatment of behavioral health conditions. Psychiatric Services. 2021; 72(9):1057-64. [DOI:10.1176/appi.ps.201900561] [PMID]
- Brienza A, Suffoletto BP, Kuhn E, Germain A, Jaramillo S, Repine M, et al. The role of specific sources of social support on postinjury psychological symptoms. Rehabilitation Psychology. 2021; 66(4):600-10. [DOI:10.1037/rep0000388] [PMID] [PMCID]
- Johnson K, Ditchman N. Mediators of quality of life in brain injury. Brain Injury. 2020; 34(12):1636-45. [DOI:10.1080/02699052.2020.1827456] [PMID]
Type of Study: Short Communication |
Subject:
● Service Quality
Received: 2023/10/30 | Accepted: 2023/12/23 | Published: 2024/09/1
Received: 2023/10/30 | Accepted: 2023/12/23 | Published: 2024/09/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |