Volume 15, Issue 1 (Jan & Feb 2025)
J Research Health 2025, 15(1): 27-40 |
Back to browse issues page
Ethics code: IR.GMU.REC.1400.187
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Tavazoi M, Mansoorian M R, Khosravan S, Mohammadzadeh F, Sharifi F. Self-management Education Based Health Promotion Model on the Clinical Manifestations of Patients With Brucellosis. J Research Health 2025; 15 (1) :27-40
URL: http://jrh.gmu.ac.ir/article-1-2478-en.html
URL: http://jrh.gmu.ac.ir/article-1-2478-en.html
Maryam Tavazoi1 

 , Mohammad Reza Mansoorian2
, Mohammad Reza Mansoorian2 

 , Shahla Khosravan3
, Shahla Khosravan3 

 , Fatemeh Mohammadzadeh4
, Fatemeh Mohammadzadeh4 

 , Farnoosh Sharifi5
, Farnoosh Sharifi5 




 , Mohammad Reza Mansoorian2
, Mohammad Reza Mansoorian2 

 , Shahla Khosravan3
, Shahla Khosravan3 

 , Fatemeh Mohammadzadeh4
, Fatemeh Mohammadzadeh4 

 , Farnoosh Sharifi5
, Farnoosh Sharifi5 


1- Department of Community Health Nursing & Management Nursing, Nursing Research Center, School of Nursing, Gonabad University of Medical Sciences, Gonabad, Iran.
2- Department of Community Health Nursing & Management Nursing, Nursing Research Center, School of Nursing, Gonabad University of Medical Sciences, Gonabad, Iran. ,mansooriangmu@gmail.com
3- Nursing Research Center, Gonabad University of Medical Sciences, Gonabad, Iran.
4- Department of Epidemiology & Biostatistics, Social Development & Health Promotion Research Center, School of Health, Gonabad University of Medical Sciences, Gonabad, Iran.
5- Department of Internal Medicine, Infectious Disease Research Center, School of Medicine, Gonabad University of Medical Sciences, Gonabad, Iran.
2- Department of Community Health Nursing & Management Nursing, Nursing Research Center, School of Nursing, Gonabad University of Medical Sciences, Gonabad, Iran. ,
3- Nursing Research Center, Gonabad University of Medical Sciences, Gonabad, Iran.
4- Department of Epidemiology & Biostatistics, Social Development & Health Promotion Research Center, School of Health, Gonabad University of Medical Sciences, Gonabad, Iran.
5- Department of Internal Medicine, Infectious Disease Research Center, School of Medicine, Gonabad University of Medical Sciences, Gonabad, Iran.
Full-Text [PDF 1078 kb]
(651 Downloads)
| Abstract (HTML) (3426 Views)
Full-Text: (890 Views)
Introduction
Brucellosis is an old zoonotic disease. Although the mortality rate of brucellosis is low in humans [1], the disease can become chronic in patients who do not adhere to treatment. This chronic form can cause severe pain, difficulty walking, extreme weakness, and disability, and can significantly reduce quality of life [2]. Therefore, brucellosis is a serious threat to human health and a major concern for public health [1], especially in the Middle East (ME) [3].
According to international public health data, the annual global incidence is 2.1 million cases, which is more than previous estimates. Also, 82.3% of the world’s countries (144/175) are at risk of this disease. By region, Africa and Asia have higher incidences compared to the Americas and Europe [4]. Iran is still one of the endemic areas for brucellosis [5]. Based on the data of the Ministry of Health of Iran, the average incidence of brucellosis in Iran is about 22 cases per 100000 population [6]. The prevalence of this disease is categorized as high (21-30 cases per 100,000 people) and very high (31-40 cases per 100,000 people) in several provinces, such as Razavi Khorasan and South Khorasan [7].
The most common clinical symptoms of this disease are arthralgia and fever [8]. Weight loss, anorexia, sweating and fatigue, and depression are other common symptoms [1]. Brucellosis can be diagnosed with serological tests showing Wright 1:80 or higher, Coombs-Wright 1:80 or higher, and 2ME ≥1.40 [9, 10].
The treatment of the disease involves an antibiotic regimen that is obtained from a combination of several antibiotics [8]. In addition to drug therapy, education is provided to prevent infection in the entire population and to reduce the recurrence of the disease and re-infection of individuals [9]. Although education is now considered a specific goal of disease control and treatment [11], previous studies have shown the inefficacy of therapeutic-medical guidelines provided as mandatory methods for patients to adhere to their medication [12]. Patients tended to forget 40-80% of the information immediately after learning it. Moreover, nearly half of the information they remembered was misleading [11]. To improve patient health, educational programs have shifted from traditional methods to self-management education (SME). SME refers to any educational process that provides people with the knowledge, skills, and motivation needed to make decisions and increases the capacity and confidence of a person to apply these skills in everyday life situations. In other words, these programs entail active participation, responsibility, and daily decision-making by the patient to take health-promoting measures [13, 14]. Thus, patients (especially chronic patients) are taught to take care of themselves rather than relying on others, with the aim of preventing recurrent hospital admissions [15]. The effectiveness of self-management programs and self-management skills for chronic patients has been explored [16, 17]. There are different methods of self-management for physical diseases as the self-management program is based on the 5A model [18]. In patients with diabetes [15], a standard self-management program has been suggested for chronic disease [13], bronchiectasis [14], and even AIDS [19]. However, the effectiveness of self-management in brucellosis has not been investigated, despite the potential for recurrence and chronicity according to the sources reviewed in the present research.
SME programs are individualized, taking into account the type of disease, its specific treatment, the patient‘s culture, literacy level, abilities, motivation, willingness to change and learn, available resources, and the limitations of the patient [20]. In other words, it was developed based on patients’ perceptions of their problems and concerns. Thus, a thorough needs assessment is essential for each disease and population [21]. Following a sound theory to better understand the needs and factors affecting health behaviors helps design a better health education program [22]. Pender’s health promotion model enables nurses to understand patients’ motivations to achieve personal health and serves as a tool for teaching lifestyles that improve patients’ health [23].
Pender has introduced the most important constructs that are effective in explaining behavior based on this model: Previous related behavior constructs, personal factors (perceived health status), perceived benefits, perceived barriers, perceived self-efficacy, and interpersonal influencers [23-25]. According to this model, individuals are more likely to commit to behaviors when they perceive greater benefits, while perceived obstacles can hinder their commitment. Perceived self-efficacy also plays a role in increasing commitment to action. Family, peers, and authorities are interpersonal influencing resources that increase or decrease commitment to action. This model has been used in several previous studies to promote self-care behaviors [26, 27], but its long-term effects and results, particularly in terms of modifying clinical features of health behavior, have received little attention. Specifically, it has not been used to design a SME program for patients with brucellosis. Therefore, the present study aimed to investigate the effect of self-management educational intervention based on Pender’s health promotion model on the clinical symptoms of patients with brucellosis. Additionally, we assessed the self-management behaviors of the participants and the factors related to these behaviors.
Methods
In the present randomized clinical trial, the participants were patients with brucellosis visiting the comprehensive health service centers of Gonabad City in Iran in 2022. The inclusion criteria were as follows: Age between 16 and 55 years, a first-time infection with brucellosis, being within the first two weeks of the acute stage of the disease as diagnosed by a physician, exhibiting clinical symptoms, having positive serology tests, receiving drug treatment, no prior experience with self-management courses, and for women, not being pregnant or breastfeeding. In this randomized clinical trial, the participants were patients with brucellosis who visited the comprehensive health service centers of Gonabad city, Iran, in 2022.
The exclusion criteria were the cessation of medication, unwillingness to participate in the research, hospitalization, and simultaneous participation in similar training programs.
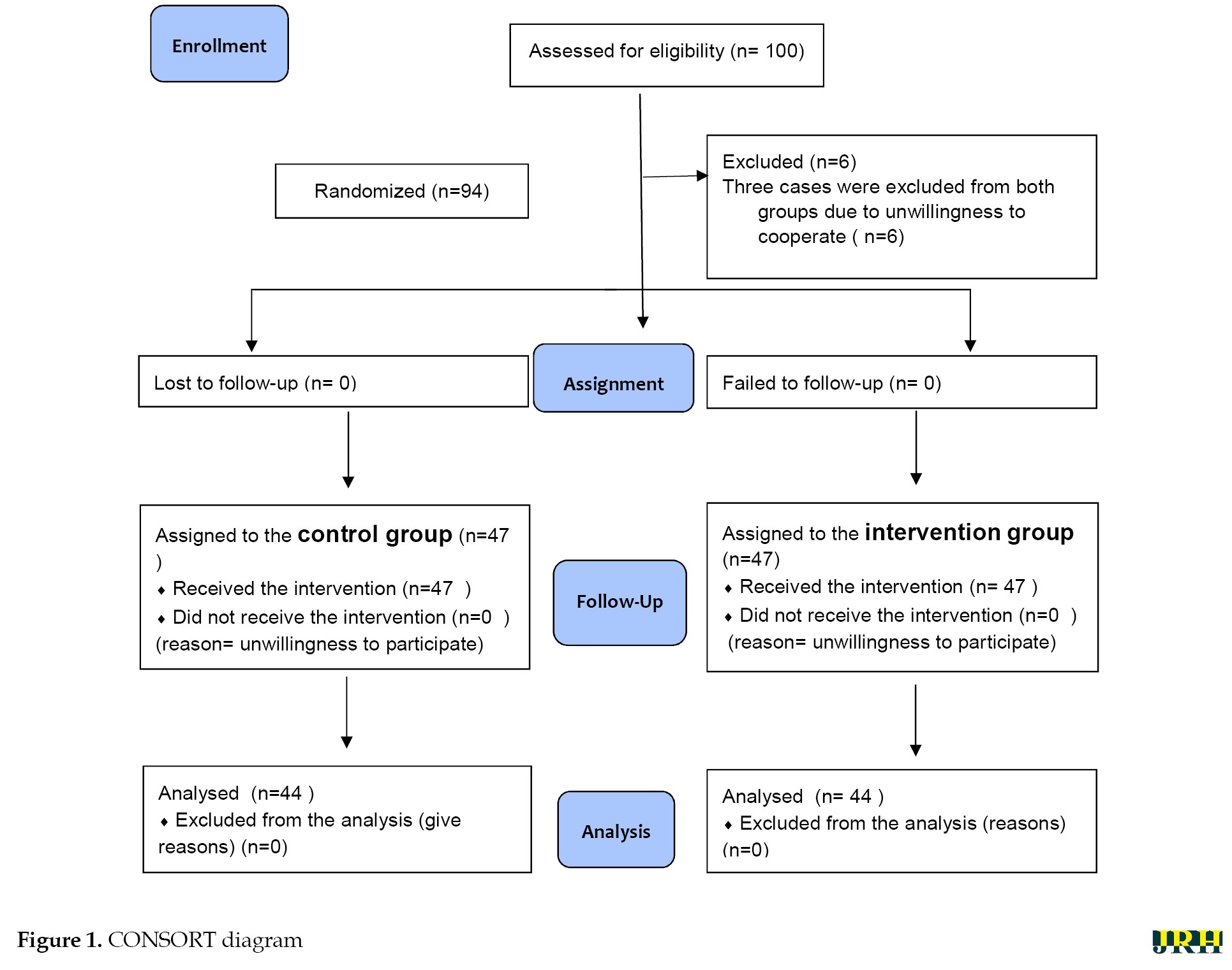
To estimate the sample size, a type I error of 5%, a test power of 80%, and a prevalence of about 60% of clinical symptoms of fever and pain were considered, based on the existing literature [28]. To detect a minimum reduction of 30%, a total of 42 patients were assigned to each research group, with the number increased to 47 to account for a 10% attrition rate. Participants were selected through simple randomization from a list of patients, with each being randomly assigned to either the control or experimental group. Permutation blocks of four were used for randomization. According to Figure 1, during the study, three participants were removed from each group, and the analysis was done on 44 participants.
Data collection tools
The following instruments were used to collect the required data in the present study:
Demographic questionnaire
This questionnaire included questions about age, sex, education, job, place of residence, exposure to livestock, comorbidity, and the use of different drugs (except for brucellosis drug treatment). This information was used to determine constructs related to previous behavior and individual characteristics, such as socioeconomic status and disease management.
Clinical symptoms checklist
This checklist enquired about pain, fever, fatigue, appetite, perspiration, and serological test results for brucellosis. The clinical symptoms were measured as follows:
The pain score was determined using a visual analog scale (VAS), which consists of a 10 cm line printed on a piece of paper with labels at each end: “No pain” at one end and “most pain” or “indescribable pain” at the other. VAS is a standard and valid measure of pain intensity with high test-retest reliability [29].
Fatigue was measured using a VAS for fatigue (VAS-F), ranging from 0 to 10 (no fatigue to severe fatigue). VAS-F is a reliable scale recommended for routine use in clinical care [30], and it has been used commonly in studies in Iran [31, 32].
Appetite was measured using the first three questions of the appetite and diet assessment tool (ADTA) questionnaire, which is a clinically useful mental tool to estimate appetite. Participants were first asked to rate their appetite status over the past one to two weeks using the options in the questionnaire (very good, good, average, bad, very bad). Then, they were asked about the changes in appetite (no change, increase, decrease). Also, a supplemental question about the state of anorexia during the last month was included at the end of the questionnaire (not at all, sometimes, moderately, a lot, very much). This questionnaire has been used and validated in other studies [33, 34].
Body temperature: Body temperature was measured using a manual (mercury) thermometer in the axilla (armpit) to prevent the spread of germs.
Researcher-made self-management behavior questionnaire for brucellosis
This questionnaire was designed by the researcher and includes 19 questions to measure knowledge of brucellosis (2 questions), health status (despite the presence of the disease) (2 questions), success in leading a healthy lifestyle and preventing brucellosis for oneself and others (7 questions), active engagement in treatment (knowledge acquisition, adherence to medication, decision-making and communication with the health staff) (6 questions) and the follow-up of the treatment protocol for the disease (2 questions). Patients answered each question on a Likert scale ranging from really true for me (4) to not true for me at all (1). The content validity of the researcher-made questionnaire was assessed using the content validity ratio (CVR) and content validity index (CVI) guided by the comments of 10 experts. The reliability of the instrument was also substantiated using Cronbach’s α, with estimated values ranging between 0.70 and 0.94 for the subscales.
Researcher-made questionnaire of factors influencing self-management behavior
This questionnaire was also designed by the researcher as a needs assessment tool and a guide for developing the educational program of this research. It measured factors affecting self-management based on the five constructs of Pender’s health promotion model, including perceived barriers (16 items), perceived benefits (7 items), perceived self-efficacy (7 items), individual influences (8 items), and situational influences (6 items). The items were all rated on a 5-point Likert scale (very low=5, low=4, medium=3, high=2 and very high=1). The overall score of each construct was the sum of the scores of the constituent items. A higher score in each construct indicated a better state of self-management of the individual in that particular domain, except for perceived barriers, which were interpreted in an opposite way.
The content validity of the researcher-made questionnaire was confirmed by estimating the CVR and CVI guided by the comments of a panel of 10 experts familiar with Pender’s health promotion model, and brucellosis disease and its care. The reliability of the instrument was also substantiated using Cronbach’s α, with estimated values ranging from 0.52 to 0.92 for the subscales.
The revised brief illness perception questionnaire (R-BIPQ)
This 9-item scale was developed by Broadbent et al. (2006) to evaluate the cognitive-emotional perception of the disease and also its Persian version was developed by Bazzazian and Besharat [35-37].
Scores for the first eight questions ranged from 0 (“very little”, “never”, or “not very well”) to 8 (“always”, “very well”, or “a lot”). Item 9 was open-ended and scored from 1 to 3 based on three items: “Lifestyle”, “stress” or “genetics” as the cause of the participant’s disease. High scores on this questionnaire indicate a threatening perception of the disease.
This instrument assesses how participants perceive brucellosis. It was used in this study as a tool to investigate the psychological dimension of personal characteristics and experiences within Pender’s health promotion model (as a factor influencing self-management behavior) and also served as a guide for developing the educational program for this research [38].
Educational intervention
Drug treatment for patients with Malt fever lasts for two months following positive test results. After completing the course of antibiotic treatment, which is prescribed by the doctor based on national guidelines for the treatment of brucellosis, tests are repeated to assess the patient’s response to treatment. The relevant factors will be evaluated. Based on this defined timeframe, self-management training sessions were designed accordingly.
In the experimental group, the self-management training program, based on the components of the Pender health promotion model and data received from the needs assessment using the researcher-made self-management behavior questionnaire for Brucellosis, researcher-made questionnaire of factors influencing self-management behavior and r-BIPQ, were presented as follows:
First session: Required knowledge about the disease (understanding brucellosis in relation to the demographic characteristics of the participants)
Second session: Disease treatment and adherence to treatment (focusing on the perceived benefits of treatment)
Third session: Management of complications (focusing on perceived barriers to self-management and problem-solving process)
Fourth session: Management of signs and symptoms (focusing on perceived self-efficacy of self-management ability)
This program was presented through the pre-organizer educational model, incorporating interactive lectures and face-to-face encounters in one-on-one or small group settings of 2 to 3 participants. After each session, a question and answer (Q&A) segment was held. Educational videos and interviews were provided for both those attending the class and those with limited access to the Internet during the COVID-19 pandemic. The training consisted of four sessions, each lasting 15-30 minutes, conducted once a week for participants in the intervention group. After each Q&A session, brochures that were mostly illustrated were also distributed to the patients, and the educational content was made available online again if needed. During the educational intervention, usual care continued for the control group.
The questionnaires were completed by the patients before the educational intervention began and also after the end of the intervention (two months later) in both research groups. The clinical symptoms were measured using the aforementioned instruments for both the experimental and control groups, similar to the previous method.
The details of the training sessions are as follows:
Session 1: Knowledge of understanding illness and healing
This session included lectures, slides, educational videos, and educational pamphlets. It incorporated key concepts related to malaria, including clinical symptoms, modes of transmission, and prevention strategies. Emphasis was placed on understanding the concepts of disease and health, developing appropriate guidelines to increase knowledge and commitment, and providing an overview of healthy food and nutritional needs while avoiding unhealthy dairy products. Participants were encouraged to set goals for healthy dairy consumption based on five healthy items.
Session 2: Self-management (problem diagnosis, problem-solving, and decision-making techniques)
This session featured lectures, slides, educational videos, and educational pamphlets. It covered key concepts of self-care and problem recognition, emphasizing the importance of achieving a healthy lifestyle. Participants explored solutions to problems and were guided in developing various decision-making abilities. The goal for participants was to recognize their issues related to Malt fever, examine potential solutions, and choose the best course of action for decision-making.
Session 3: Achieving a healthy life
By applying the knowledge gained in the first session and identifying the participant’s problems, a healthy life can be achieved.
This session included lectures, slides, educational videos, and educational pamphlets. It focused on recognizing unhealthy dairy products, ensuring safe contact with livestock, and safely disposing of intestines and viscera. Additionally, it addressed unhealthy food cultures. Participants utilized the knowledge acquired about malaria to engage in operational training for a healthy lifestyle, with the training localized based on the participants’ needs.
Session 4: Treatment and follow-up of the disease
This session featured lectures, slides, educational videos, and educational pamphlets. It emphasized the importance of taking medications on time, conducting tests as scheduled, and following up on the disease. The purpose of the training was to solve the problems of taking antibiotics on time, visiting the doctor, and ensuring proper disease follow-up.
From sessions 1-4: Consulting support
Consultative support for malaria patients participating in the study was provided through phone calls and Internet messaging services such as Telegram and Incanel. This support helped participants set and review personal goals and strategies to overcome obstacles and make healthier choices. They were reminded how to select appropriate options, identify the problems associated with health-promoting behaviors, determine solutions to these problems, and foster independence in decision-making.
Data analysis
Data were analyzed by SPSS software, version 16. Quantitative variables were described using Mean±SD, and qualitative variables were described using frequency and percentage. The normality of data in both groups was evaluated using the Kolmogorov-Smirnov test. A comparison of qualitative data between the two groups was made using the chi-square and Fisher’s exact tests. An independent-sample t-test was run to compare quantitative variables between the two groups. To compare the variables between two groups To compare the response variables between two groups while adjusting for pre-test values, linear regression analysis was used for quantitative variables. For qualitative variables (bimodal qualitative and ordinal qualitative), logistic regression analysis (bimodal logistic and ordinal logistic regression, respectively) was employed. The significance level for all tests was set at P<0.05. For qualitative variables (bimodal qualitative and ordinal qualitative), logistic regression analysis (bimodal logistic and ordinal logistic regression, respectively) was employed. The significance level for all tests was set at P<0.05.
Results
The between-group comparison of demographic variables, comorbidities, and some high-risk behaviors for transmitting brucellosis are shown in Table 1.
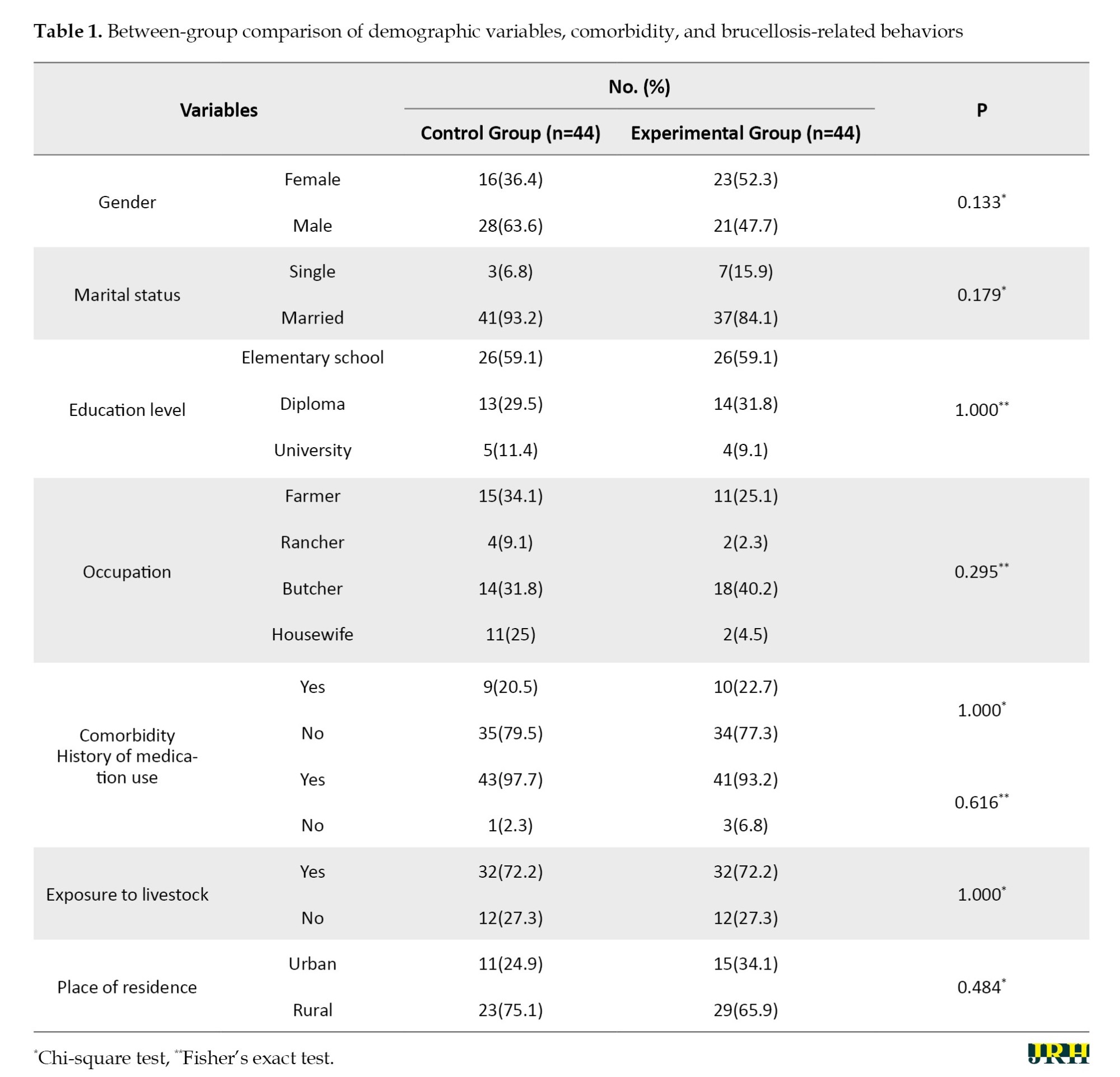
There was no statistically significant difference between the two groups before the intervention(P˃0.05).
The comparison of clinical and paraclinical findings before and after the intervention in the two groups is shown in Table 2.
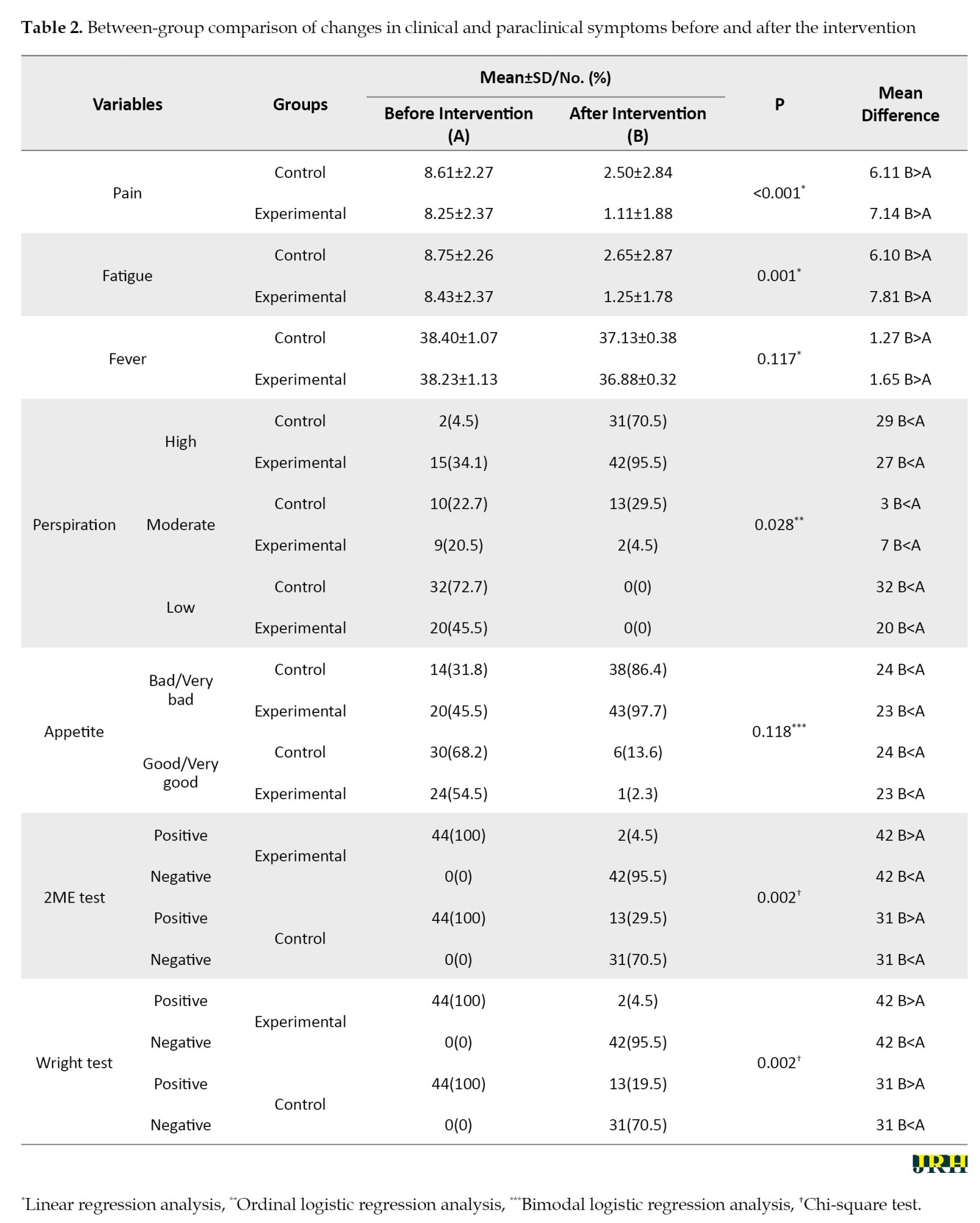
The intervention caused a significant change in all variables except for fever and appetite in the experimental group in comparison to the control group.
Table 3 shows the comparison of mean brucellosis self-management behavior scores between the two groups before and after the educational intervention.
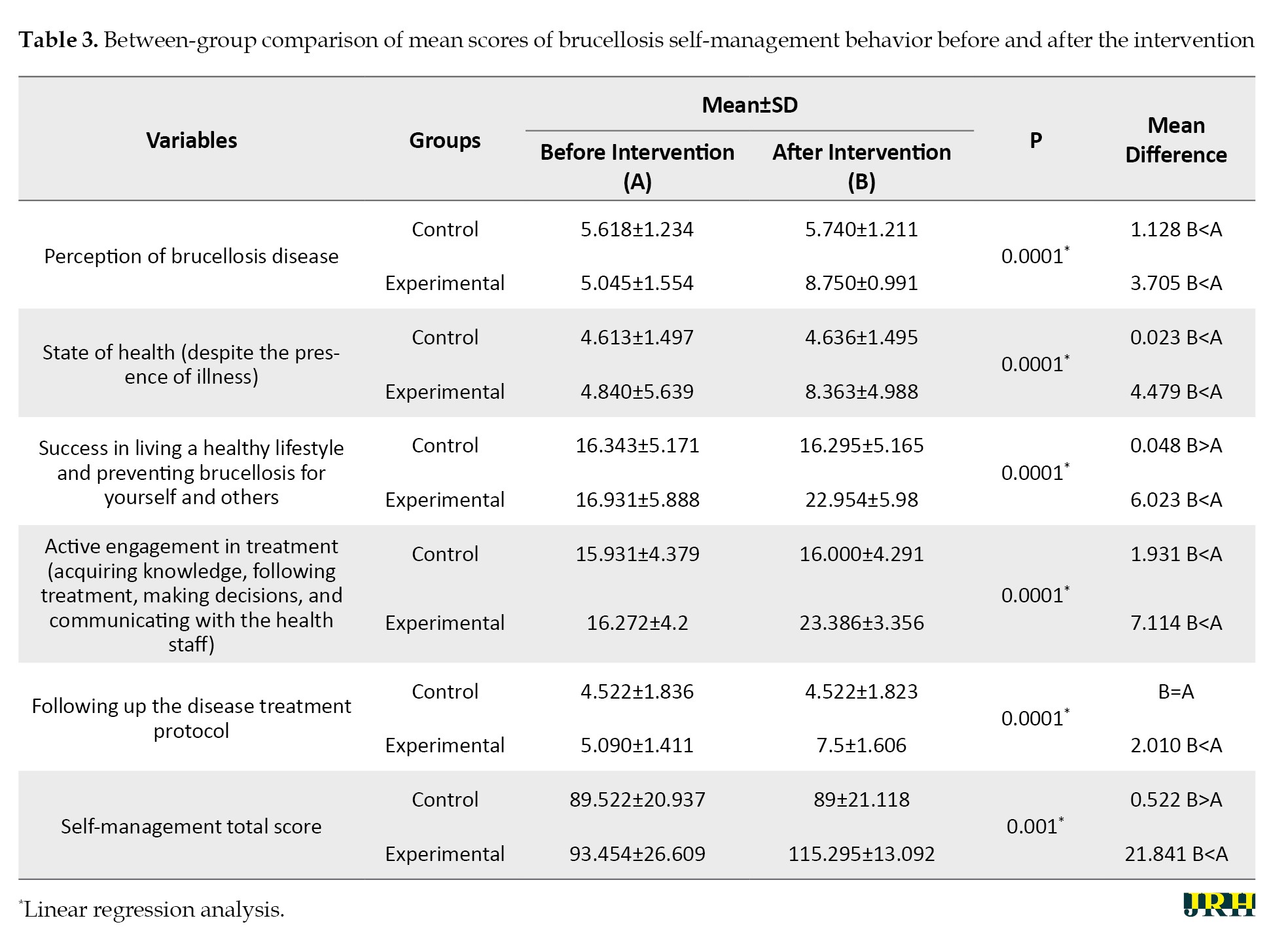
The intervention caused a significant improvement in self-management behavior and its components in the experimental group (P˂0.05).
Table 4 compares the scores of Pender’s health promotion model concerning self-management behavior before and after the intervention in two groups.
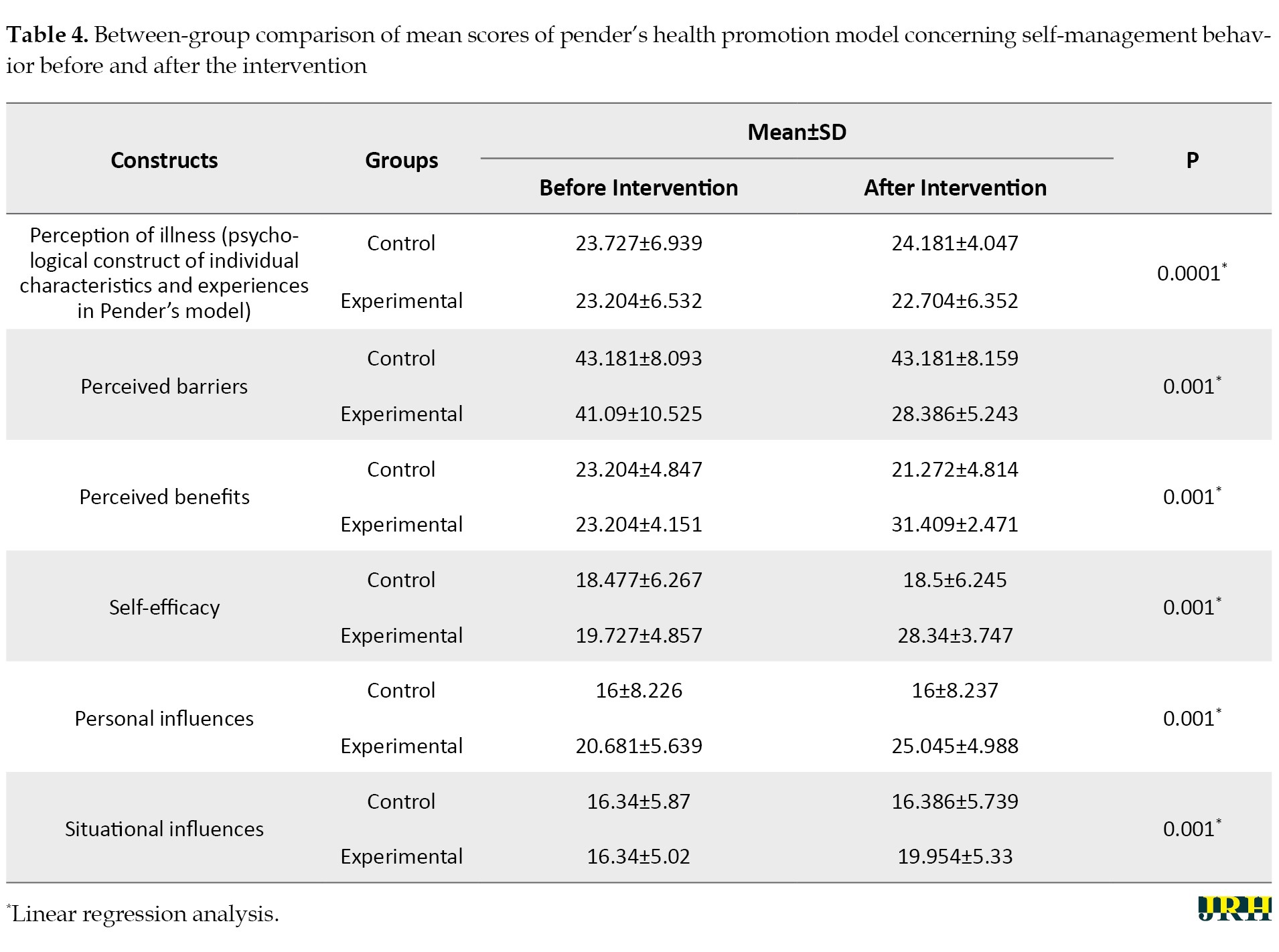
The constructs improved after the intervention in the experimental group compared to the control group.
Discussion
According to the results obtained from this non-pharmacological randomized trial using a self-management educational intervention based on Pender’s health promotion model, there was a statistically significant improvement in clinical findings after two months. Also, the rate of positive serological tests in the experimental group was approximately 4.5 compared to 29.5 in the control group. A temperature of 38.3 °C or higher [39][40], malaise, and myalgia in patients, along with Wright ≥1/320 and 2-ME ≥1/160 at the end of the sixth week of treatment, are considered risk factors for treatment failure and relapse in brucellosis [40, 41]. Brucellosis is a public health problem; therefore, effective treatment and prevention of treatment failure are major issues in controlling the disease [42]. Since there are no reliable laboratory criteria for microbiological therapy, the evaluation of therapeutic effectiveness is based on clinical symptoms and some serological tests [43]. Therefore, it can be concluded that the intervention carried out in our study was effective in achieving the goals of treating brucellosis.
It has been recommended to determine the effect of self-management interventions on the improvement of clinical outcomes [44] and reduce the failure rate of brucellosis, especially in the acute phase [45]. While this variable was examined in our study, our review of the articles showed that despite conducting numerous educational and care models of management studies on patients with brucellosis, the impact of these models on the treatment of the disease has not been measured [46-50]. However, there is evidence of the effectiveness of self-management training for some chronic diseases, such as glycosylated hemoglobin levels and systolic blood pressure in diabetes and hypertension, at low to moderate levels [51].
As the results of our study showed, untreated cases of brucellosis were observed in both groups based on serological test results, which could be explained by the possibility of treatment failure and disease recurrence [42]. Similarly, there is evidence of the ineffectiveness of self-management training interventions on chronic diseases, including arthritis [51] and chronic obstructive airway disease [43]. This result may also be due to the fact that chronic diseases such as arthritis may not fully respond to many treatments [51]. Therefore it is suggested that future research determine which components of self-management can improve the clinical outcomes of this disease [43].
The results of the Researcher-Made Brucellosis Self-Management Behavior Questionnaire in our study indicated an improvement in the total score of self-management behavior and its dimensions, including obtaining information about the disease, following a healthy lifestyle to prevent brucellosis, making informed decisions, and actively participating in treatment, treatment follow-up, and treatment compliance in the experimental group. According to our review, we did not find any study that used the health promotion model to improve self-management behavior in patients with brucellosis; however, a Health Action Process Approach model-based mobile health intervention in China also promoted self-management in these patients through changes in health behavior and health literacy [52]. Overall, it is considered that SME and support facilitate the knowledge, skills, and abilities needed for self-care, as well as actions that help to continuously implement and maintain the behaviors needed to manage the condition [53].
Our study was designed according to patient needs assessment using Pender’s health promotion model and was delivered through an active teaching model. Although a study argued that following specific behavioral theories to develop self-management training programs was not necessarily associated with better results [51], it was recommended that understanding the content of the educational program through a patient needs assessment is essential for implementing an effective educational program that can lead to the recognition of behaviors necessary to change unhealthy habits and adopt appropriate practices [22].
The result of our study showed that the perception of brucellosis, identification, and removal of barriers to self-management of the disease, improving the benefits of self-management, promotion of self-efficacy, and controlling the influence of individual and situational factors related to brucellosis were increased in the experimental group in comparison to the pre-test (within-group comparison) and in comparison to the control group (between-group comparison). In other studies, similar to our study, model-based educational interventions yielded better results compared to traditional teaching methods [18] and routine educational programs [54, 55].
In this study, based on the construct of individual and behavioral characteristics in Pender’s health promotion model, which assessed the primary predictors of health-related behavior [56], we identified several risk factors for brucellosis among our participants, including jobs in butchery and animal husbandry, low education levels, residence in rural areas, failure to maintain a healthy lifestyle to prevent diseases, consumption of non-pasteurized dairy products, and exposure to animals. Several of these factors have been mentioned in the existing literature [57, 58].
The findings of our study also showed a high score for perceived barriers, along with low scores for perceived benefits and self-efficacy, which were identified as perceived interpersonal and situational influences in both groups. After the intervention, there was a significant decrease in the perceived barriers score in the intervention group compared to before the intervention and also compared to the control group, which only used the routine program of the health centers. These findings are consistent with a study by Khodaveisi et al. An improvement in the perceived benefit score in this study was observed in the experimental group similar to other studies, and this was identified as a facilitator for behavior change (self-management) [59-61]. There was a significant increase in the self-efficacy score after the intervention in the experimental group similar to other studies [59, 62]. Self-efficacy was introduced as the best construct and the perceived barriers and benefits as the most important variables for behavior change. The increase in self-efficacy is associated with a decrease in perceived barriers [63, 64]. In this study, individual characteristics were similar to those in other studies [65], and the effect of situational influences [66] significantly increased after the intervention in the experimental group compared to before the intervention.
The present findings showed an increased score in the perception of disease and all components as psychological factors of individual characteristics [23] affecting self-management behavior in the experimental group. In another study, Rees et al. found that personal control and the ability to understand the disease were the main predictors of adherence to treatment. Therefore, increasing the perception of the disease is considered an important strategy in educational interventions [67].
Conclusion
The results of the study showed that compared to the routine training program, the self-management training intervention designed based on Pender’s health promotion model was effective in improving self-management behaviors and clinical and laboratory symptoms of patients with brucellosis. This model effectively explains behavior, needs, and the factors that influence them, providing the capability to design a better self-management training program for patients with brucellosis in the acute stage. Therefore, it is recommended to use this educational program in health centers to prevent the recurrence or chronicity of brucellosis.
By using a comprehensive care model, this study made it possible to design and intervene client-centered self-management training based on needs assessment in patients with brucellosis. In addition to examining changes in self-management behavior, which have often been investigated in previous studies, particularly regarding chronic diseases, this study also evaluated the variable of disease improvement by considering clinical and para-clinical outcomes.
However, this study also has limitations, including reliance on self-reported findings, the short duration of the intervention and follow-up, the lack of assessment of the relapse or chronicity of the disease, and the absence of a cost analysis for the educational intervention compared to other models. Considering the limitations of the research, further studies are suggested.
Ethical Considerations
Compliance with ethical guidelines
This research was reviewed at Gonabad University of Medical Sciences and received an ethical code of approval (Code: IR.GMU.REC.1400.187). Also, this research was registered at the Clinical Trial Registration Center of Iran (IRCT) (Code: IRCT20220205053940N1). The purpose of the study was explained to the participants and they entered the study after signing an informed consent. They were assured of the confidentiality of the information they provided.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sector.
Authors' contributions
Conceptualization and supervision: Shahla Khosrovan and Mohammad Reza Mansourian; Methodology: Maryam Tavazoi, Fatemeh Mohammadzadeh and Farnoosh Sharifi; Data collection: Maryam Tavazoi and Shahla Khosrovan; Data analysis: Fatemeh Mohammadzadeh and Farnoosh Sharifi; Investigation and writing: Maryam Tavazoi and Shahla Khosrovan.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Hereby, the present authors are grateful to the participants of the study and the authorities and financial support of the Nursing Research Center of Gonabad University of Medical Sciences, Gonabad, Iran. Appreciation is also extended to all the staff working in the Health Department of Gonabad City, and the residents are thanked for their assistance in conducting this research.
References
Brucellosis is an old zoonotic disease. Although the mortality rate of brucellosis is low in humans [1], the disease can become chronic in patients who do not adhere to treatment. This chronic form can cause severe pain, difficulty walking, extreme weakness, and disability, and can significantly reduce quality of life [2]. Therefore, brucellosis is a serious threat to human health and a major concern for public health [1], especially in the Middle East (ME) [3].
According to international public health data, the annual global incidence is 2.1 million cases, which is more than previous estimates. Also, 82.3% of the world’s countries (144/175) are at risk of this disease. By region, Africa and Asia have higher incidences compared to the Americas and Europe [4]. Iran is still one of the endemic areas for brucellosis [5]. Based on the data of the Ministry of Health of Iran, the average incidence of brucellosis in Iran is about 22 cases per 100000 population [6]. The prevalence of this disease is categorized as high (21-30 cases per 100,000 people) and very high (31-40 cases per 100,000 people) in several provinces, such as Razavi Khorasan and South Khorasan [7].
The most common clinical symptoms of this disease are arthralgia and fever [8]. Weight loss, anorexia, sweating and fatigue, and depression are other common symptoms [1]. Brucellosis can be diagnosed with serological tests showing Wright 1:80 or higher, Coombs-Wright 1:80 or higher, and 2ME ≥1.40 [9, 10].
The treatment of the disease involves an antibiotic regimen that is obtained from a combination of several antibiotics [8]. In addition to drug therapy, education is provided to prevent infection in the entire population and to reduce the recurrence of the disease and re-infection of individuals [9]. Although education is now considered a specific goal of disease control and treatment [11], previous studies have shown the inefficacy of therapeutic-medical guidelines provided as mandatory methods for patients to adhere to their medication [12]. Patients tended to forget 40-80% of the information immediately after learning it. Moreover, nearly half of the information they remembered was misleading [11]. To improve patient health, educational programs have shifted from traditional methods to self-management education (SME). SME refers to any educational process that provides people with the knowledge, skills, and motivation needed to make decisions and increases the capacity and confidence of a person to apply these skills in everyday life situations. In other words, these programs entail active participation, responsibility, and daily decision-making by the patient to take health-promoting measures [13, 14]. Thus, patients (especially chronic patients) are taught to take care of themselves rather than relying on others, with the aim of preventing recurrent hospital admissions [15]. The effectiveness of self-management programs and self-management skills for chronic patients has been explored [16, 17]. There are different methods of self-management for physical diseases as the self-management program is based on the 5A model [18]. In patients with diabetes [15], a standard self-management program has been suggested for chronic disease [13], bronchiectasis [14], and even AIDS [19]. However, the effectiveness of self-management in brucellosis has not been investigated, despite the potential for recurrence and chronicity according to the sources reviewed in the present research.
SME programs are individualized, taking into account the type of disease, its specific treatment, the patient‘s culture, literacy level, abilities, motivation, willingness to change and learn, available resources, and the limitations of the patient [20]. In other words, it was developed based on patients’ perceptions of their problems and concerns. Thus, a thorough needs assessment is essential for each disease and population [21]. Following a sound theory to better understand the needs and factors affecting health behaviors helps design a better health education program [22]. Pender’s health promotion model enables nurses to understand patients’ motivations to achieve personal health and serves as a tool for teaching lifestyles that improve patients’ health [23].
Pender has introduced the most important constructs that are effective in explaining behavior based on this model: Previous related behavior constructs, personal factors (perceived health status), perceived benefits, perceived barriers, perceived self-efficacy, and interpersonal influencers [23-25]. According to this model, individuals are more likely to commit to behaviors when they perceive greater benefits, while perceived obstacles can hinder their commitment. Perceived self-efficacy also plays a role in increasing commitment to action. Family, peers, and authorities are interpersonal influencing resources that increase or decrease commitment to action. This model has been used in several previous studies to promote self-care behaviors [26, 27], but its long-term effects and results, particularly in terms of modifying clinical features of health behavior, have received little attention. Specifically, it has not been used to design a SME program for patients with brucellosis. Therefore, the present study aimed to investigate the effect of self-management educational intervention based on Pender’s health promotion model on the clinical symptoms of patients with brucellosis. Additionally, we assessed the self-management behaviors of the participants and the factors related to these behaviors.
Methods
In the present randomized clinical trial, the participants were patients with brucellosis visiting the comprehensive health service centers of Gonabad City in Iran in 2022. The inclusion criteria were as follows: Age between 16 and 55 years, a first-time infection with brucellosis, being within the first two weeks of the acute stage of the disease as diagnosed by a physician, exhibiting clinical symptoms, having positive serology tests, receiving drug treatment, no prior experience with self-management courses, and for women, not being pregnant or breastfeeding. In this randomized clinical trial, the participants were patients with brucellosis who visited the comprehensive health service centers of Gonabad city, Iran, in 2022.
The exclusion criteria were the cessation of medication, unwillingness to participate in the research, hospitalization, and simultaneous participation in similar training programs.
To estimate the sample size, a type I error of 5%, a test power of 80%, and a prevalence of about 60% of clinical symptoms of fever and pain were considered, based on the existing literature [28]. To detect a minimum reduction of 30%, a total of 42 patients were assigned to each research group, with the number increased to 47 to account for a 10% attrition rate. Participants were selected through simple randomization from a list of patients, with each being randomly assigned to either the control or experimental group. Permutation blocks of four were used for randomization. According to Figure 1, during the study, three participants were removed from each group, and the analysis was done on 44 participants.
Data collection tools
The following instruments were used to collect the required data in the present study:
Demographic questionnaire
This questionnaire included questions about age, sex, education, job, place of residence, exposure to livestock, comorbidity, and the use of different drugs (except for brucellosis drug treatment). This information was used to determine constructs related to previous behavior and individual characteristics, such as socioeconomic status and disease management.
Clinical symptoms checklist
This checklist enquired about pain, fever, fatigue, appetite, perspiration, and serological test results for brucellosis. The clinical symptoms were measured as follows:
The pain score was determined using a visual analog scale (VAS), which consists of a 10 cm line printed on a piece of paper with labels at each end: “No pain” at one end and “most pain” or “indescribable pain” at the other. VAS is a standard and valid measure of pain intensity with high test-retest reliability [29].
Fatigue was measured using a VAS for fatigue (VAS-F), ranging from 0 to 10 (no fatigue to severe fatigue). VAS-F is a reliable scale recommended for routine use in clinical care [30], and it has been used commonly in studies in Iran [31, 32].
Appetite was measured using the first three questions of the appetite and diet assessment tool (ADTA) questionnaire, which is a clinically useful mental tool to estimate appetite. Participants were first asked to rate their appetite status over the past one to two weeks using the options in the questionnaire (very good, good, average, bad, very bad). Then, they were asked about the changes in appetite (no change, increase, decrease). Also, a supplemental question about the state of anorexia during the last month was included at the end of the questionnaire (not at all, sometimes, moderately, a lot, very much). This questionnaire has been used and validated in other studies [33, 34].
Body temperature: Body temperature was measured using a manual (mercury) thermometer in the axilla (armpit) to prevent the spread of germs.
Researcher-made self-management behavior questionnaire for brucellosis
This questionnaire was designed by the researcher and includes 19 questions to measure knowledge of brucellosis (2 questions), health status (despite the presence of the disease) (2 questions), success in leading a healthy lifestyle and preventing brucellosis for oneself and others (7 questions), active engagement in treatment (knowledge acquisition, adherence to medication, decision-making and communication with the health staff) (6 questions) and the follow-up of the treatment protocol for the disease (2 questions). Patients answered each question on a Likert scale ranging from really true for me (4) to not true for me at all (1). The content validity of the researcher-made questionnaire was assessed using the content validity ratio (CVR) and content validity index (CVI) guided by the comments of 10 experts. The reliability of the instrument was also substantiated using Cronbach’s α, with estimated values ranging between 0.70 and 0.94 for the subscales.
Researcher-made questionnaire of factors influencing self-management behavior
This questionnaire was also designed by the researcher as a needs assessment tool and a guide for developing the educational program of this research. It measured factors affecting self-management based on the five constructs of Pender’s health promotion model, including perceived barriers (16 items), perceived benefits (7 items), perceived self-efficacy (7 items), individual influences (8 items), and situational influences (6 items). The items were all rated on a 5-point Likert scale (very low=5, low=4, medium=3, high=2 and very high=1). The overall score of each construct was the sum of the scores of the constituent items. A higher score in each construct indicated a better state of self-management of the individual in that particular domain, except for perceived barriers, which were interpreted in an opposite way.
The content validity of the researcher-made questionnaire was confirmed by estimating the CVR and CVI guided by the comments of a panel of 10 experts familiar with Pender’s health promotion model, and brucellosis disease and its care. The reliability of the instrument was also substantiated using Cronbach’s α, with estimated values ranging from 0.52 to 0.92 for the subscales.
The revised brief illness perception questionnaire (R-BIPQ)
This 9-item scale was developed by Broadbent et al. (2006) to evaluate the cognitive-emotional perception of the disease and also its Persian version was developed by Bazzazian and Besharat [35-37].
Scores for the first eight questions ranged from 0 (“very little”, “never”, or “not very well”) to 8 (“always”, “very well”, or “a lot”). Item 9 was open-ended and scored from 1 to 3 based on three items: “Lifestyle”, “stress” or “genetics” as the cause of the participant’s disease. High scores on this questionnaire indicate a threatening perception of the disease.
This instrument assesses how participants perceive brucellosis. It was used in this study as a tool to investigate the psychological dimension of personal characteristics and experiences within Pender’s health promotion model (as a factor influencing self-management behavior) and also served as a guide for developing the educational program for this research [38].
Educational intervention
Drug treatment for patients with Malt fever lasts for two months following positive test results. After completing the course of antibiotic treatment, which is prescribed by the doctor based on national guidelines for the treatment of brucellosis, tests are repeated to assess the patient’s response to treatment. The relevant factors will be evaluated. Based on this defined timeframe, self-management training sessions were designed accordingly.
In the experimental group, the self-management training program, based on the components of the Pender health promotion model and data received from the needs assessment using the researcher-made self-management behavior questionnaire for Brucellosis, researcher-made questionnaire of factors influencing self-management behavior and r-BIPQ, were presented as follows:
First session: Required knowledge about the disease (understanding brucellosis in relation to the demographic characteristics of the participants)
Second session: Disease treatment and adherence to treatment (focusing on the perceived benefits of treatment)
Third session: Management of complications (focusing on perceived barriers to self-management and problem-solving process)
Fourth session: Management of signs and symptoms (focusing on perceived self-efficacy of self-management ability)
This program was presented through the pre-organizer educational model, incorporating interactive lectures and face-to-face encounters in one-on-one or small group settings of 2 to 3 participants. After each session, a question and answer (Q&A) segment was held. Educational videos and interviews were provided for both those attending the class and those with limited access to the Internet during the COVID-19 pandemic. The training consisted of four sessions, each lasting 15-30 minutes, conducted once a week for participants in the intervention group. After each Q&A session, brochures that were mostly illustrated were also distributed to the patients, and the educational content was made available online again if needed. During the educational intervention, usual care continued for the control group.
The questionnaires were completed by the patients before the educational intervention began and also after the end of the intervention (two months later) in both research groups. The clinical symptoms were measured using the aforementioned instruments for both the experimental and control groups, similar to the previous method.
The details of the training sessions are as follows:
Session 1: Knowledge of understanding illness and healing
This session included lectures, slides, educational videos, and educational pamphlets. It incorporated key concepts related to malaria, including clinical symptoms, modes of transmission, and prevention strategies. Emphasis was placed on understanding the concepts of disease and health, developing appropriate guidelines to increase knowledge and commitment, and providing an overview of healthy food and nutritional needs while avoiding unhealthy dairy products. Participants were encouraged to set goals for healthy dairy consumption based on five healthy items.
Session 2: Self-management (problem diagnosis, problem-solving, and decision-making techniques)
This session featured lectures, slides, educational videos, and educational pamphlets. It covered key concepts of self-care and problem recognition, emphasizing the importance of achieving a healthy lifestyle. Participants explored solutions to problems and were guided in developing various decision-making abilities. The goal for participants was to recognize their issues related to Malt fever, examine potential solutions, and choose the best course of action for decision-making.
Session 3: Achieving a healthy life
By applying the knowledge gained in the first session and identifying the participant’s problems, a healthy life can be achieved.
This session included lectures, slides, educational videos, and educational pamphlets. It focused on recognizing unhealthy dairy products, ensuring safe contact with livestock, and safely disposing of intestines and viscera. Additionally, it addressed unhealthy food cultures. Participants utilized the knowledge acquired about malaria to engage in operational training for a healthy lifestyle, with the training localized based on the participants’ needs.
Session 4: Treatment and follow-up of the disease
This session featured lectures, slides, educational videos, and educational pamphlets. It emphasized the importance of taking medications on time, conducting tests as scheduled, and following up on the disease. The purpose of the training was to solve the problems of taking antibiotics on time, visiting the doctor, and ensuring proper disease follow-up.
From sessions 1-4: Consulting support
Consultative support for malaria patients participating in the study was provided through phone calls and Internet messaging services such as Telegram and Incanel. This support helped participants set and review personal goals and strategies to overcome obstacles and make healthier choices. They were reminded how to select appropriate options, identify the problems associated with health-promoting behaviors, determine solutions to these problems, and foster independence in decision-making.
Data analysis
Data were analyzed by SPSS software, version 16. Quantitative variables were described using Mean±SD, and qualitative variables were described using frequency and percentage. The normality of data in both groups was evaluated using the Kolmogorov-Smirnov test. A comparison of qualitative data between the two groups was made using the chi-square and Fisher’s exact tests. An independent-sample t-test was run to compare quantitative variables between the two groups. To compare the variables between two groups To compare the response variables between two groups while adjusting for pre-test values, linear regression analysis was used for quantitative variables. For qualitative variables (bimodal qualitative and ordinal qualitative), logistic regression analysis (bimodal logistic and ordinal logistic regression, respectively) was employed. The significance level for all tests was set at P<0.05. For qualitative variables (bimodal qualitative and ordinal qualitative), logistic regression analysis (bimodal logistic and ordinal logistic regression, respectively) was employed. The significance level for all tests was set at P<0.05.
Results
The between-group comparison of demographic variables, comorbidities, and some high-risk behaviors for transmitting brucellosis are shown in Table 1.
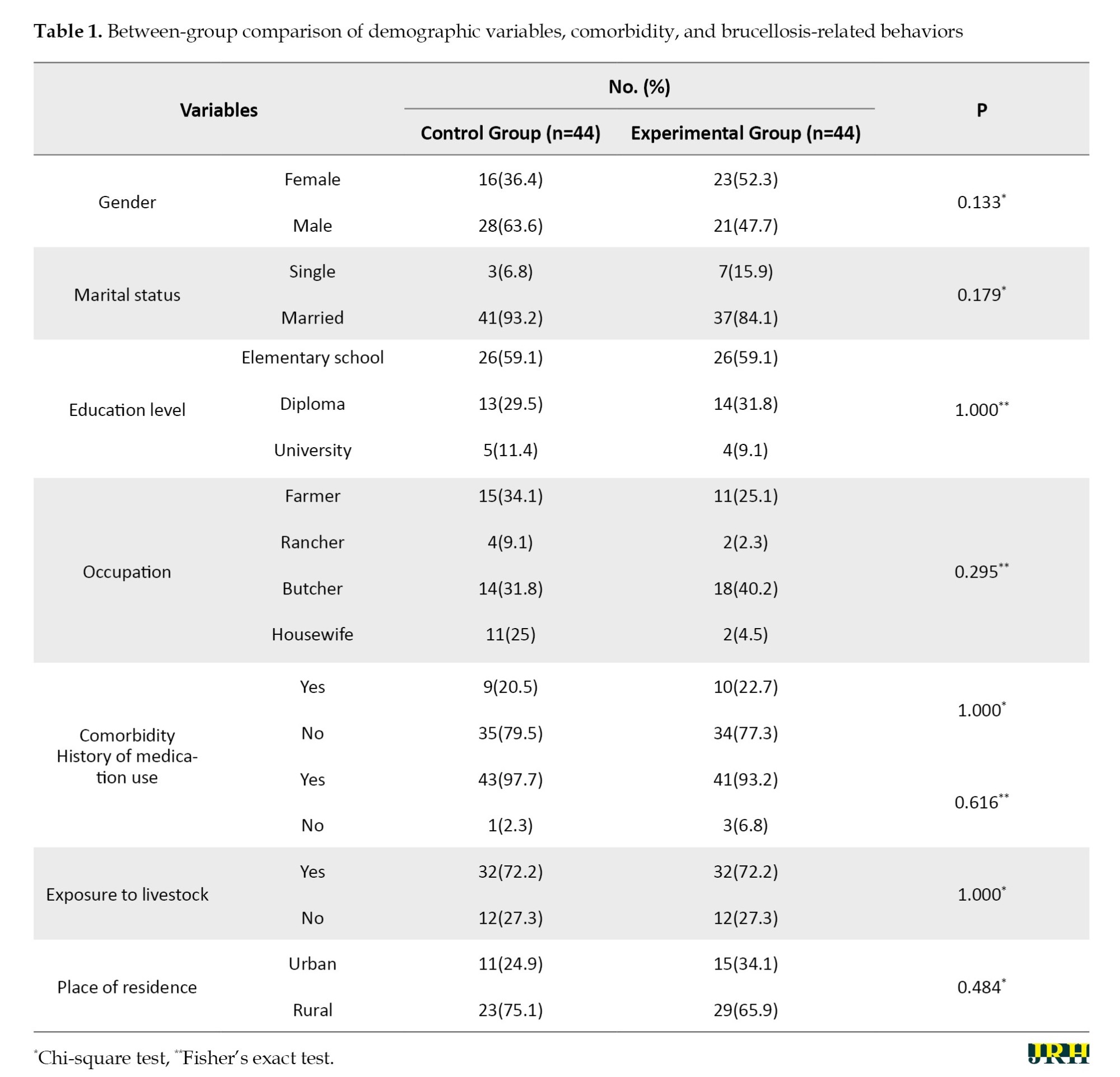
There was no statistically significant difference between the two groups before the intervention(P˃0.05).
The comparison of clinical and paraclinical findings before and after the intervention in the two groups is shown in Table 2.
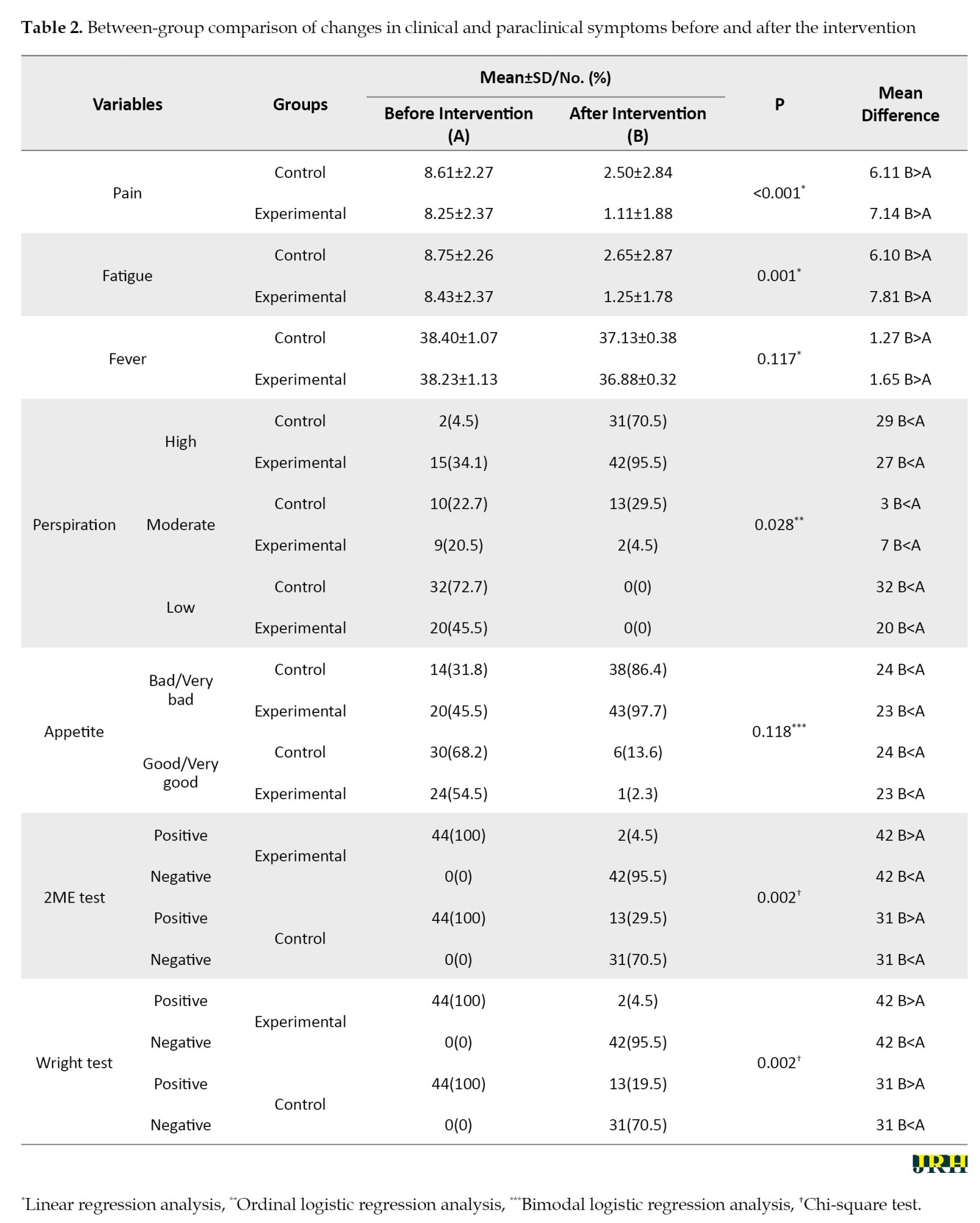
The intervention caused a significant change in all variables except for fever and appetite in the experimental group in comparison to the control group.
Table 3 shows the comparison of mean brucellosis self-management behavior scores between the two groups before and after the educational intervention.
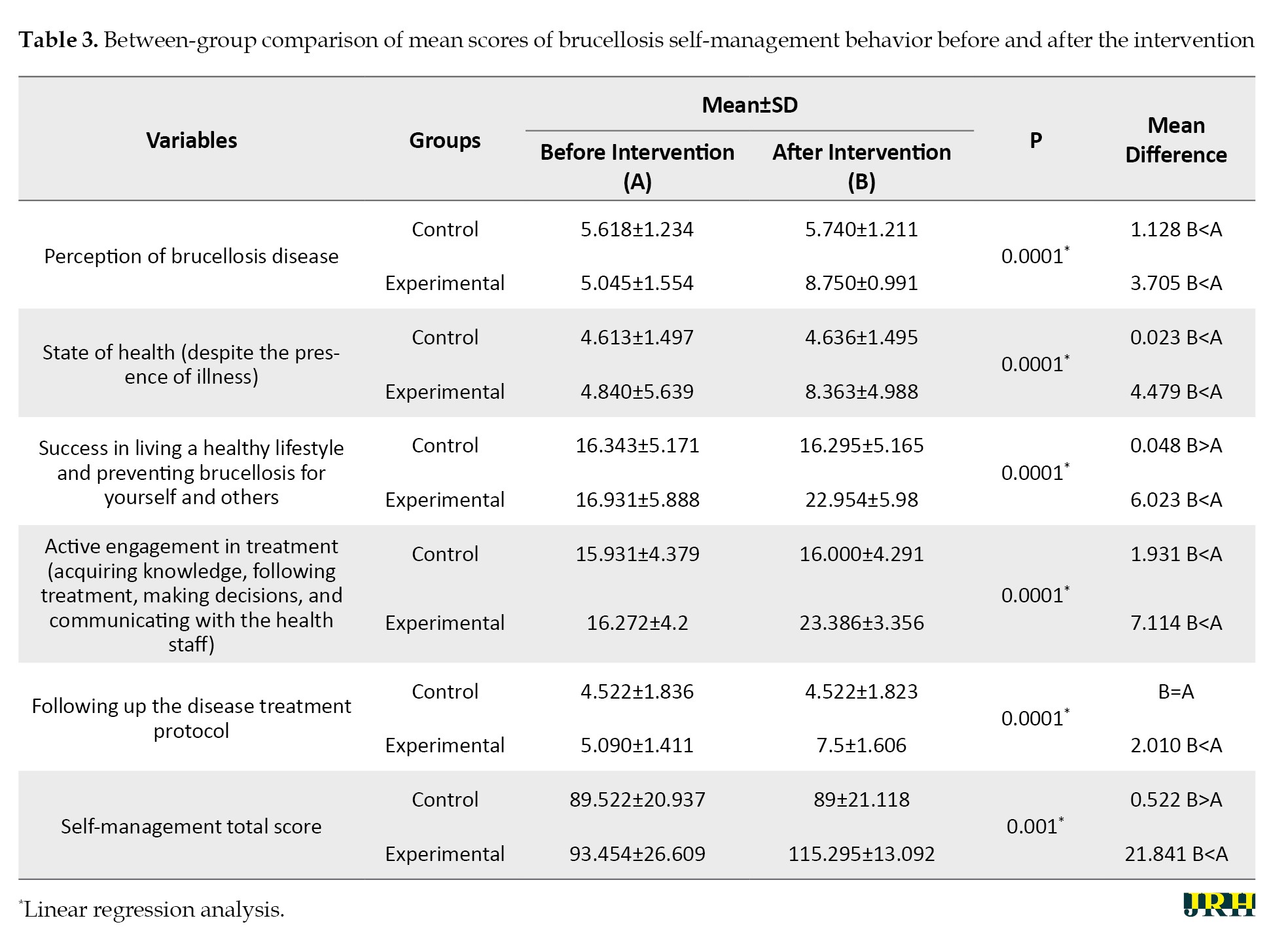
The intervention caused a significant improvement in self-management behavior and its components in the experimental group (P˂0.05).
Table 4 compares the scores of Pender’s health promotion model concerning self-management behavior before and after the intervention in two groups.
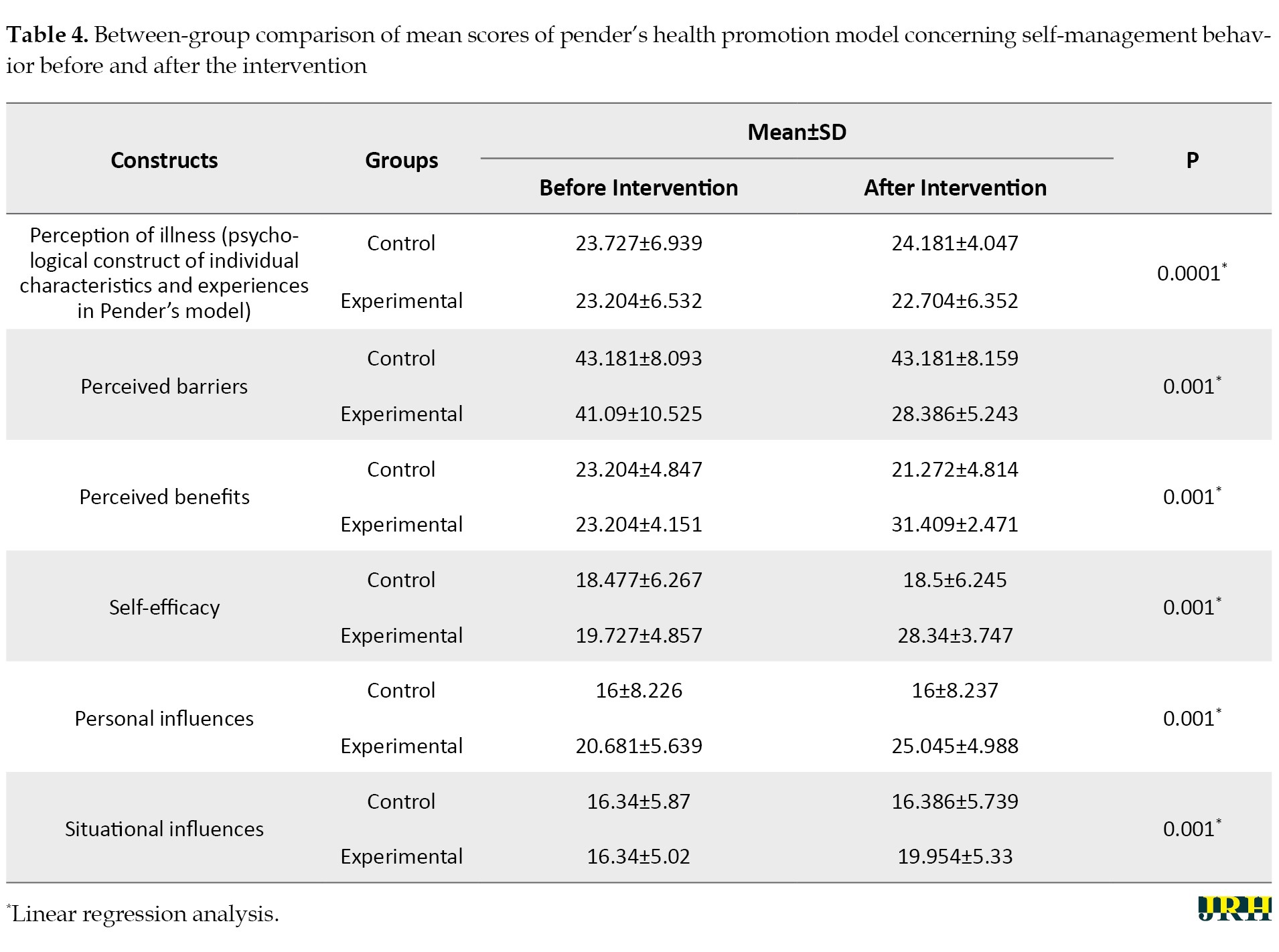
The constructs improved after the intervention in the experimental group compared to the control group.
Discussion
According to the results obtained from this non-pharmacological randomized trial using a self-management educational intervention based on Pender’s health promotion model, there was a statistically significant improvement in clinical findings after two months. Also, the rate of positive serological tests in the experimental group was approximately 4.5 compared to 29.5 in the control group. A temperature of 38.3 °C or higher [39][40], malaise, and myalgia in patients, along with Wright ≥1/320 and 2-ME ≥1/160 at the end of the sixth week of treatment, are considered risk factors for treatment failure and relapse in brucellosis [40, 41]. Brucellosis is a public health problem; therefore, effective treatment and prevention of treatment failure are major issues in controlling the disease [42]. Since there are no reliable laboratory criteria for microbiological therapy, the evaluation of therapeutic effectiveness is based on clinical symptoms and some serological tests [43]. Therefore, it can be concluded that the intervention carried out in our study was effective in achieving the goals of treating brucellosis.
It has been recommended to determine the effect of self-management interventions on the improvement of clinical outcomes [44] and reduce the failure rate of brucellosis, especially in the acute phase [45]. While this variable was examined in our study, our review of the articles showed that despite conducting numerous educational and care models of management studies on patients with brucellosis, the impact of these models on the treatment of the disease has not been measured [46-50]. However, there is evidence of the effectiveness of self-management training for some chronic diseases, such as glycosylated hemoglobin levels and systolic blood pressure in diabetes and hypertension, at low to moderate levels [51].
As the results of our study showed, untreated cases of brucellosis were observed in both groups based on serological test results, which could be explained by the possibility of treatment failure and disease recurrence [42]. Similarly, there is evidence of the ineffectiveness of self-management training interventions on chronic diseases, including arthritis [51] and chronic obstructive airway disease [43]. This result may also be due to the fact that chronic diseases such as arthritis may not fully respond to many treatments [51]. Therefore it is suggested that future research determine which components of self-management can improve the clinical outcomes of this disease [43].
The results of the Researcher-Made Brucellosis Self-Management Behavior Questionnaire in our study indicated an improvement in the total score of self-management behavior and its dimensions, including obtaining information about the disease, following a healthy lifestyle to prevent brucellosis, making informed decisions, and actively participating in treatment, treatment follow-up, and treatment compliance in the experimental group. According to our review, we did not find any study that used the health promotion model to improve self-management behavior in patients with brucellosis; however, a Health Action Process Approach model-based mobile health intervention in China also promoted self-management in these patients through changes in health behavior and health literacy [52]. Overall, it is considered that SME and support facilitate the knowledge, skills, and abilities needed for self-care, as well as actions that help to continuously implement and maintain the behaviors needed to manage the condition [53].
Our study was designed according to patient needs assessment using Pender’s health promotion model and was delivered through an active teaching model. Although a study argued that following specific behavioral theories to develop self-management training programs was not necessarily associated with better results [51], it was recommended that understanding the content of the educational program through a patient needs assessment is essential for implementing an effective educational program that can lead to the recognition of behaviors necessary to change unhealthy habits and adopt appropriate practices [22].
The result of our study showed that the perception of brucellosis, identification, and removal of barriers to self-management of the disease, improving the benefits of self-management, promotion of self-efficacy, and controlling the influence of individual and situational factors related to brucellosis were increased in the experimental group in comparison to the pre-test (within-group comparison) and in comparison to the control group (between-group comparison). In other studies, similar to our study, model-based educational interventions yielded better results compared to traditional teaching methods [18] and routine educational programs [54, 55].
In this study, based on the construct of individual and behavioral characteristics in Pender’s health promotion model, which assessed the primary predictors of health-related behavior [56], we identified several risk factors for brucellosis among our participants, including jobs in butchery and animal husbandry, low education levels, residence in rural areas, failure to maintain a healthy lifestyle to prevent diseases, consumption of non-pasteurized dairy products, and exposure to animals. Several of these factors have been mentioned in the existing literature [57, 58].
The findings of our study also showed a high score for perceived barriers, along with low scores for perceived benefits and self-efficacy, which were identified as perceived interpersonal and situational influences in both groups. After the intervention, there was a significant decrease in the perceived barriers score in the intervention group compared to before the intervention and also compared to the control group, which only used the routine program of the health centers. These findings are consistent with a study by Khodaveisi et al. An improvement in the perceived benefit score in this study was observed in the experimental group similar to other studies, and this was identified as a facilitator for behavior change (self-management) [59-61]. There was a significant increase in the self-efficacy score after the intervention in the experimental group similar to other studies [59, 62]. Self-efficacy was introduced as the best construct and the perceived barriers and benefits as the most important variables for behavior change. The increase in self-efficacy is associated with a decrease in perceived barriers [63, 64]. In this study, individual characteristics were similar to those in other studies [65], and the effect of situational influences [66] significantly increased after the intervention in the experimental group compared to before the intervention.
The present findings showed an increased score in the perception of disease and all components as psychological factors of individual characteristics [23] affecting self-management behavior in the experimental group. In another study, Rees et al. found that personal control and the ability to understand the disease were the main predictors of adherence to treatment. Therefore, increasing the perception of the disease is considered an important strategy in educational interventions [67].
Conclusion
The results of the study showed that compared to the routine training program, the self-management training intervention designed based on Pender’s health promotion model was effective in improving self-management behaviors and clinical and laboratory symptoms of patients with brucellosis. This model effectively explains behavior, needs, and the factors that influence them, providing the capability to design a better self-management training program for patients with brucellosis in the acute stage. Therefore, it is recommended to use this educational program in health centers to prevent the recurrence or chronicity of brucellosis.
By using a comprehensive care model, this study made it possible to design and intervene client-centered self-management training based on needs assessment in patients with brucellosis. In addition to examining changes in self-management behavior, which have often been investigated in previous studies, particularly regarding chronic diseases, this study also evaluated the variable of disease improvement by considering clinical and para-clinical outcomes.
However, this study also has limitations, including reliance on self-reported findings, the short duration of the intervention and follow-up, the lack of assessment of the relapse or chronicity of the disease, and the absence of a cost analysis for the educational intervention compared to other models. Considering the limitations of the research, further studies are suggested.
Ethical Considerations
Compliance with ethical guidelines
This research was reviewed at Gonabad University of Medical Sciences and received an ethical code of approval (Code: IR.GMU.REC.1400.187). Also, this research was registered at the Clinical Trial Registration Center of Iran (IRCT) (Code: IRCT20220205053940N1). The purpose of the study was explained to the participants and they entered the study after signing an informed consent. They were assured of the confidentiality of the information they provided.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sector.
Authors' contributions
Conceptualization and supervision: Shahla Khosrovan and Mohammad Reza Mansourian; Methodology: Maryam Tavazoi, Fatemeh Mohammadzadeh and Farnoosh Sharifi; Data collection: Maryam Tavazoi and Shahla Khosrovan; Data analysis: Fatemeh Mohammadzadeh and Farnoosh Sharifi; Investigation and writing: Maryam Tavazoi and Shahla Khosrovan.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
Hereby, the present authors are grateful to the participants of the study and the authorities and financial support of the Nursing Research Center of Gonabad University of Medical Sciences, Gonabad, Iran. Appreciation is also extended to all the staff working in the Health Department of Gonabad City, and the residents are thanked for their assistance in conducting this research.
References
- Shi C, Wang L, Lv D, Wang G, Mengist HM, Jin T, et al. Epidemiological, clinical and laboratory characteristics of patients with brucella infection in Anhui Province, China. Infection and Drug Resistance. 2021; 14:2741-52. [DOI:10.2147/IDR.S319595] [PMID] [PMCID]
- Eales KM, Norton RE, Ketheesan N. Brucellosis in northern Australia. The American Journal of Tropical Medicine and Hygiene. 2010; 83(4):876-8. [DOI:10.4269/ajtmh.2010.10-0237] [PMID] [PMCID]
- Bagheri Nejad R, Krecek RC, Khalaf OH, Hailat N, Arenas-Gamboa AM. Brucellosis in the middle east: Current situation and a pathway forward. PLoS Neglected Tropical Diseases. 2020; 14(5):e0008071. [DOI:10.1371/journal.pntd.0008071] [PMID] [PMCID]
- Laine CG, Johnson VE, Scott HM, Arenas-Gamboa AM. Global estimate of human brucellosis incidence. Emerging Infectious Diseases. 2023; 29(9):1789-97. [DOI:10.3201/eid2909.230052] [PMID] [PMCID]
- Keramat F, Mamani M, Adabi M, Khazaei S, Shivapoor Z, Karami M. Establishment of brucellosis relapse and complications registry: A study protocol. Journal of Preventive Medicine and Hygiene. 2021; 62(2):E496-500. [DOI:10.15167/2421-4248/jpmh2021.62.2.1422] [PMID]
- Zeinali M, Doosti S, Amiri B, Gouya MM, Godwin GN. Trends in the epidemiology of brucellosis cases in Iran during the last decade. Iranian Journal of Public Health. 2022; 51(12):2791-8. [DOI:10.18502/ijph.v51i12.11470] [PMID] [PMCID]
- Golshani M, Buozari S. A review of brucellosis in Iran: Epidemiology, risk factors, diagnosis, control, and prevention. Iranian Biomedical Journal. 2017; 21(6):349-59. [DOI:10.18869/acadpub.ibj.21.6.349] [PMID]
- Buzgan T, Karahocagil MK, Irmak H, Baran AI, Karsen H, Evirgen O, et al. Clinical manifestations and complications in 1028 cases of brucellosis: A retrospective evaluation and review of the literature. International Journal of Infectious Diseases. 2010; 14(6):e469-78. [DOI:10.1016/j.ijid.2009.06.031] [PMID]
- Akinyemi KO, Fakorede CO, Amisu KO, Wareth G. Human and animal brucellosis in Nigeria: A systemic review and meta-analysis in the last twenty-one years (2001-2021). Veterinary Sciences. 2022; 9(8):384. [DOI:10.3390/vetsci9080384] [PMID] [PMCID]
- Haghdoost M, Ansari L, Owaysee Osquee H. Comparison of brucellacapture and coombs wright and wright in the diagnosis of brucellosis. Journal of Research in Clinical Medicine. 2021; 9(1):15. [DOI:10.34172/jrcm.2021.0015]
- Dalir Z, Reihani Z, Mazlom R, Vakilian F. [Effect of training based on teach back method on self-care in patients with heart failure (Persian)]. Journal of Mazandaran University of Medical Sciences. 2016; 25(134):209-20. [Link]
- Karamghadiri N, Hassanabadi H, Mojtabai R, Hatami M, Nikoosokhan A, Meysamie A. [The expert patient: A new approach to type 2 diabetes self-management based on illness perception and embodied cognition (Persian)]. Clinical Psychology and Personality. 2020; 17(2):47-61. [DOI:10.22070/cpap.2020.2907]
- Tan SS, Pisano MM, Boone AL, Baker G, Pers YM, Pilotto A, et al. Evaluation design of effichronic: The chronic disease self-management programme (CDSMP) intervention for citizens with a low socioeconomic position. International Journal of Environmental Research And Public Health. 2019; 16(11):1883. [DOI:10.3390/ijerph16111883] [PMID] [PMCID]
- Kelly C, Grundy S, Lynes D, Evans DJ, Gudur S, Milan SJ, et al. Self-management for bronchiectasis. The Cochrane Database of Systematic Reviews. 2018; 2(2):CD012528. [DOI:10.1002/14651858.CD012528.pub2] [PMID]
- Mahdifarani M, Rejeh N, Heravi-Karimooi M, Tadrisi SD, Marghob B. [The effect of self-management program based of self-empowerment on the self-efficacy in elderly patients undergoing hemodialysis (Persian)]. Iranian Journal of Nursing Research (IJNR) Original Article. 2020; 15(2):35-44. [Link]
- Powers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, Hess-Fischl A, et al. Diabetes self-management education and support in adults with type 2 diabetes: A consensus report of the american diabetes association, the association of diabetes care & education specialists, the academy of nutrition and dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Journal of the American Pharmacists Association. 2020; 60(6):e1-18. [DOI:10.1016/j.japh.2020.04.018] [PMID]
- Li R, Liang N, Bu F, Hesketh T. The effectiveness of self-management of hypertension in adults using mobile health: Systematic review and meta-analysis. JMIR mHealth and uHealth. 2020; 8(3):e17776. [DOI:10.2196/17776] [PMID] [PMCID]
- Moradi M, Nasiri M, Hajiahmadi M, Jahanshah M. The effect of self-management program based on 5A model on coping strategies in the elderly men patients with hypertension. 2018; 4(1):32-47. [Link]
- Millard T, Elliott J, Girdler S. Self-management education programs for people living with HIV/AIDS: A systematic review. AIDS Patient Care and STDs. 201; 27(2):103-13. [DOI:10.1089/apc.2012.0294] [PMID]
- Canadian Diabetes Association Clinical Practice Guidelines Expert Committee; Jones H, Berard LD, MacNeill G, Whitham D, Yu C. Self-management education. Canadian Journal of Diabetes. 2013; 37(Suppl 1):S26-30. [DOI:10.1016/j.jcjd.2013.01.015] [PMID]
- Rahimian-Boogar I, Besharat MA, Mohajeri-Tehrani MR, Talepasand S. [Diabetes self management: Social, demographical and disease factors (Persian)]. Journal of clinical psychology. 2010; 1(4):43-57. [DOI:10.22075/jcp.2017.1986]
- Amin-Shokravi F, Hashemian AH, Khanian HR. [Impact of Educational Program on Preventive Behavior of Brucellosis. (Persian)]. Health Education and Health Promotionک 2013; 1(3):15-22. [Link]
- Chen HH, Hsieh PL. Applying the pender's health promotion model to identify the factors related to older adults' participation in community-based health promotion activities. International Journal of Environmental Research and Public Health. 2021; 18(19):9985. [DOI:10.3390/ijerph18199985] [PMID] [PMCID]
- Haghi R, Ashouri A, Karimy M, Rouhani-Tonekaboni N, Kasmaei P, Pakdaman F, et al. The role of correlated factors based on Pender health promotion model in brushing behavior in the 13-16 years old students of Guilan, Iran. Italian Journal of Pediatrics. 2021; 47(1):111. [DOI:10.1186/s13052-021-01063-y] [PMID] [PMCID]
- Pouresmali A, Alizadehgoradel J, Molaei B, Vanderhasselt M-A, Fathi D. Self-care behavior prevention of Covid-19 in the general population based on Pender health promotion model. 2021 [Unpublished]. [DOI:10.21203/rs.3.rs-139049/v1]
- Xavier BLS, Santos Id, Silva FVC. Promoting self-care in clients on hemodialysis: Application of the nola pender’s diagram. Revista de Pesquisa: Cuidado é Fundamental Online. 2017; 9(2):545-50. [DOI:10.9789/2175-5361.2017.v9i2.545-550]
- Bijani M, Niknam M, Karimi S, Naderi Z, Dehghan A. The effect of peer education based on Pender’s health promotion model on quality of life, stress management and self-efficacy of patients with multiple sclerosis: A randomized controlled clinical trial. BMC Neurology. 2022; 22(1):144. [DOI:10.1186/s12883-022-02671-9] [PMID] [PMCID]
- Moosazadeh M, Nikaeen R, Abedi G, Kheradmand M, Safiri S. Epidemiological and clinical features of people with malta fever in Iran: A systematic review and meta-analysis. Osong Public Health and Research Perspectives. 2016; 7(3):157-67. [DOI:10.1016/j.phrp.2016.04.009] [PMID] [PMCID]
- Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Annals of the Rheumatic Diseases. 1978; 37(4):378-81. [DOI:10.1136/ard.37.4.378] [PMID] [PMCID]
- Wolfe F. Fatigue assessments in rheumatoid arthritis: Comparative performance of visual analog scales and longer fatigue questionnaires in 7760 patients. The Journal of rheumatology. 2004; 31(10):1896-902. [Link]
- Motaharinezhad F, Parvaneh S, Ghahari S. [Fatigue in people with multiple sclerosis: Cause, evaluation and treatment (Persian)]. Journal of Paramedical Sciences & Rehabilitation. 2016; 5(1):73-80. [DOI:10.22038/jpsr.2016.6386]
- Sayari S, Nobahar M, Ghorbani R. Effect of foot reflexology on sleep quality and severity of fatigue in patients with acute myocardial infarction: A double-blind randomized clinical trial. Koomesh. 2021; 23(3):327-37. [DOI:10.52547/koomesh.23.3.327]
- Burrowes JD, Larive B, Chertow GM, Cockram DB, Dwyer JT, Greene T, et al. Self-reported appetite, hospitalization and death in haemodialysis patients: Findings from the hemodialysis (HEMO) study. Nephrology, Dialysis, Transplantation. 2005; 20(12):2765-74. [DOI:10.1093/ndt/gfi132] [PMID]
- Alipoor E, Hosseinzadeh-Attar MJ, Mahdavi-Mazdeh M, Shadnoush M, Yaseri M. [The comparison of dietary intake and appetite between normal weight and obese patients under hemodialysis (Persian)]. Journal of Medicine and Spiritual Cultivation. 2017; 24(2):83-96. [Link]
- Bazzazian S, Besharat MA. Reliability and validity of a Farsi version of the brief illness perception questionnaire. Procedia-Social and Behavioral Sciences. 2010; 5:962-5. [DOI:10.1016/j.sbspro.2010.07.217]
- Kalantari H, Bagherian Sararoodi R, Afshar H, Khoramian N, Forouzandeh N, Daghagh Zadeh H, et al. [Relationship between illness perceptions and quality of life in patients with irritable bowel syndrome (Persian)]. Journal of Mazandaran University of Medical Sciences. 2012; 22(90):33-41. [Link]
- Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. Journal of Psychosomatic Research. 2006; 60(6):631-7. [DOI:10.1016/j.jpsychores.2005.10.020] [PMID]
- Sakraida TJ. Health promotion model. In: Raile Alligood M, editor. Nursing theorists and their work. Edinburgh: Elsevier; 2010. [Link]
- Solera J, Martínez-Alfaro E, Espinosa A, Castillejos ML, Geijo P, Rodríguez-Zapata M. Multivariate model for predicting relapse in human brucellosis. The Journal of Infection. 1998; 36(1):85-92. [DOI:10.1016/S0163-4453(98)93342-4] [PMID]
- Kayaaslan B, Bastug A, Aydin E, Akinci E, But A, Aslaner H, et al. A long-term survey of brucellosis: Is there any marker to predict the complicated cases? Infectious Diseases. 2016; 48(3):215-21. [DOI:10.3109/23744235.2015.1107187] [PMID]
- Farazi A, Zarrinfar N, Didgar F, Jabbariasl M, Mirzajani P. [Risk factors for failure of treatment and relapse of brucellosis (Persian)]. Journal of Arak University of Medical Sciences. 2014; 17(4):47-53. [Link]
- Alavi SM, Alavi L. Treatment of brucellosis: A systematic review of studies in recent twenty years. Caspian Journal of Internal Medicine. 2013; 4(2):636-41. [PMID]
- Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: A systematic review of randomized controlled trials. BMC Cardiovascular Disorders. 2006; 6:43. [DOI:10.1186/1471-2261-6-43] [PMID] [PMCID]
- Didarloo A, Shojaeizadeh D, Alizadeh M. Impact of educational intervention based on interactive approaches on beliefs, behavior, hemoglobin a1c, and quality of life in diabetic women. International Journal of Preventive Medicine. 2016; 7:38. [DOI:10.4103/2008-7802.176004] [PMID] [PMCID]
- Arkin obol AO, Ayxam kiyom AK, Wang HaiYan WH, Chen PengGao CP, Ripkat abulimit RA, Muhtar hasan MH. Investigation of brucellosis treatment effect and influencing factors in Qapqal Xibe autonomous county of Xinjiang. Disease Surveillance. 2018; 33(11):967-70. [Link]
- Barati M, Shayghan Zahed R, Bakhtiari M, Fathi Y, Afshari M, Taheri-Kharameh Z. Factors Influencing Brucellosis Preventive Behaviors among Marginalized Iranian Women: An application of the health belief model. ScientificWorldJournal. 2022; 2022:5987484. [DOI:10.1155/2022/5987484] [PMID] [PMCID]
- Babazadeh T, Nadrian H, Ranjbaran S, Rezakhani-Moghaddam H, Aghemiri M. Cognitive factors associated with Brucellosis preventive behaviours among diagnosed patients: An application of empowerment model. Eastern Mediterranean Health Journal. 2019; 25(8):567-74. [DOI:10.26719/emhj.18.062] [PMID]
- Fadaei E, Borhani M, Hoseini ZS, Mehri A, Tatari M. Effect of health educational intervention based on the educational phase of the PRECEDE-PROCEED model on the promotion of preventive behaviors of Brucellosis in the villagers of Minoodasht, Iran. Journal of Education and Community Health. 2021; 8(3):203-8. [DOI:10.52547/jech.8.3.203]
- Khosraviasl T, Moshki M, Dogonchi M. The effect of health ambassadors’ training based on social cognitive theory on brucellosis preventive behaviors in rural areas: Randomized controlled trial. 2023 [Unpublished]. [DOI:10.21203/rs.3.rs-2457900/v1]
- Khanian HR, Hashemian AH. [Effect of training on preventive behavior of brucellosis (Persian)]. Iranian Journal of Health Education and Health Promotion. 2013; 1(3):15-22. [Link]
- Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, et al. 2017 National standards for diabetes self-management education and support. The Diabetes Educator. 2018; 44(1):35-50. [DOI:10.1177/0145721718754797] [PMID]
- Wang J, Jiang Y, Yu Z, Chen J, Wu Y. Impact of a Health Action Process Approach model-based mobile health intervention on health behaviours of brucella patients: protocol for an intervention randomized controlled trial. 2023 [Unpublished]. [DOI:10.21203/rs.3.rs-3505558/v1]
- Bosilkovski M, Keramat F, Arapović J. The current therapeutical strategies in human brucellosis. Infection. 2021; 49(5):823-32. [DOI:10.1007/s15010-021-01586-w] [PMID]
- Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: A systematic review and methodological critique of the literature. Archives of Internal Medicine. 2004; 164(15):1641-9. [DOI:10.1001/archinte.164.15.1641] [PMID]
- Hamzaee K, Hossain Zadeh K, Azh N, Mafi M. Efficacy of health belief model compared to the traditional education on Kegel exercises in middle-aged women. Journal of Health. 2018;9(5):576-88. [DOI:10.29252/j.health.9.5.576]
- Soofian M, Ramezani A, Banifazl M, Mohraz M, Velayati A, Aghakhani A, et al. P1230 Risk factors for human brucellosis in Iran: A case-control study. International Journal of Antimicrobial Agents. 2007; 29(2):S337. [DOI:10.1016/S0924-8579(07)71070-1]
- Ramezankhani A, Jahani H, Hatami H, Sharifzadeh G, Hosseini S. Determine the effect of intervention on the adoption of preventive behaviours of the brucellosis was based on the health belief model. Journal of North Khorasan University of Medical Sciences. 2016; 8(1):33-45. [DOI:10.29252/jnkums.8.1.33]
- Sofian M, Aghakhani A, Velayati AA, Banifazl M, Eslamifar A, Ramezani A. Risk factors for human brucellosis in Iran: A case-control study. International Journal of Infectious Diseases. 2008; 12(2):157-61. [DOI:10.1016/j.ijid.2007.04.019] [PMID]
- TeshomeYimer B, Feleke BE, Bogale KA, Tsegaye GW. Factors associated with human brucellosis among patients attending in ayu primary Hospital, North Showa, Ethiopia: A case control study. Ethiopian Journal of Health Sciences. 2021; 31(4):709-18. [DOI:10.4314/ejhs.v31i4.4] [PMID] [PMCID]
- Srof BJ, Velsor-Friedrich B. Health promotion in adolescents: A review of Pender’s health promotion model. Nursing Science Quarterly. 2006; 19(4):366-73. [DOI:10.1177/0894318406292831] [PMID]
- Khodaveisi M, Omidi A, Farokhi S, Soltanian A. [Dietary behavior status and its predictors based on the penders health promotion model constructs among overweight women referred to Fatemieh hospital clinics in Hamedan, 2014 (Persian)]. Journal of Nursing Education. 2016; 5(2):31-9. [Link]
- Zare M, Asadi Z, Vahedian Shahroodi M, Bahrami-Taghanaki H. Investigating the relationship between components of Pender’s health promotion model and self-care behaviors among patients with smear-positive pulmonary tuberculosis. Evidence Based Care. 2017; 6(4):7-17. [Link]
- Pouya HM, Majlessi F, Shojaeizadeh D, Forooshani AR. The effect of educational intervention based on the Pender’s Health Promotion Model on patients’ self-efficacy for self-care behaviors following heart surgery. Iranian Journal of Nursing Research. 2017; 12(3):16-23. [DOI:10.21859/ijnr-12033]
- Wallace LS, Buckworth J, Kirby TE, Sherman WM. Characteristics of exercise behavior among college students: Application of social cognitive theory to predicting stage of change. Preventive Medicine. 2000; 31(5):494-505. [DOI:10.1006/pmed.2000.0736] [PMID]
- Berry T, Naylor P, Wharf-Higgins J. Stages of change in adolescents: an examination of self-efficacy, decisional balance, and reasons for relapse. Journal of Adolescent Health. 2005; 37(6):452-9. [DOI:10.1016/j.jadohealth.2004.09.019] [PMID]
- Taymoori P, Niknami S, Berry T, Ghofranipour F, Kazemnejad A. Application of the health promotion model to predict stages of exercise behaviour in Iranian adolescents. EMHJ-Eastern Mediterranean Health Journal. 15(5):1215-25. [Link]
- Rees S, Williams A. Promoting and supporting self-management for adults living in the community with physical chronic illness: A systematic review of the effectiveness and meaningfulness of the patient-practitioner encounter. JBI Evidence Synthesis. 2009; 7(13):492-582. [DOI:10.11124/jbisrir-2009-194] [PMID]
Type of Study: Orginal Article |
Subject:
● Health Education
Received: 2023/12/4 | Accepted: 2024/03/12 | Published: 2025/01/1
Received: 2023/12/4 | Accepted: 2024/03/12 | Published: 2025/01/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |