Volume 15, Issue 2 (March & April 2025)
J Research Health 2025, 15(2): 145-154 |
Back to browse issues page
Ethics code: IR.SBU.REC.1400.253
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Melhi E, Zarani F, Panaghi L, Harirchian M H. Multiple Sclerosis as a Moderator in the Dynamics of Interoceptive Awareness and Emotion Dysregulation. J Research Health 2025; 15 (2) :145-154
URL: http://jrh.gmu.ac.ir/article-1-2500-en.html
URL: http://jrh.gmu.ac.ir/article-1-2500-en.html
1- Department of Psychology, School of Education and Psychology, Shahid Beheshti University, Tehran, Iran.
2- Department of Psychology, School of Education and Psychology, Shahid Beheshti University, Tehran, Iran. ,f_zarani@sbu.ac.ir
3- Department of Family Health, Family Research Institute, Shahid Beheshti University, Tehran, Iran.
4- Iranian Centre of Neurological Research, Neuroscience Institute, Tehran University of Medical Sciences, Tehran, Iran.
2- Department of Psychology, School of Education and Psychology, Shahid Beheshti University, Tehran, Iran. ,
3- Department of Family Health, Family Research Institute, Shahid Beheshti University, Tehran, Iran.
4- Iranian Centre of Neurological Research, Neuroscience Institute, Tehran University of Medical Sciences, Tehran, Iran.
Keywords: Interoceptive awareness, Emotion dysregulation, MAIA-2, Relapsing-remitting multiple sclerosis (RRMS)
Full-Text [PDF 648 kb]
(613 Downloads)
| Abstract (HTML) (3100 Views)
Full-Text: (856 Views)
Introduction
Emotions play a pivotal role in human functioning and well-being, making effective emotion regulation imperative for managing them [1]. Emotion regulation pertains to the mechanisms, by which individuals exert influence over the emergence, intensity, duration and manifestation of their emotions [2]. Emotional dysregulation, however, presents significant challenges. It encompasses a deficiency in awareness, understanding, and acceptance of emotions, difficulty in controlling behaviors when distressed, restricted access to adaptive strategies and a tendency to avoid emotional distress [3]. A person’s health status has a significant impact on emotion regulation because illnesses can cause cognitive-emotional and behavioral changes. A chronic and progressive illness, such as multiple sclerosis (MS), presents emotional challenges for individuals, resulting in a potential negative impact on their emotional well-being based on its chronicity and their perception of the disease’s nature, in which the immune system acts against them [4]. MS is an autoimmune disorder affecting the central nervous system, marked by the demyelination of nerve fibers, which leads to the disruption of neural communication. The symptoms of MS are diverse and can encompass mobility impairments, fatigue, pain and cognitive dysfunction [5].
MS affects individuals’ emotional functions in two main ways. As an inflammatory disease, MS is characterized by a loss of white matter throughout the brain and damage to the emotion regulation networks. It alters individuals’ ability to self-regulate and process emotion by altering the subcortical circuitry in the frontal lobe, the cingulate gyrus, and the insula. Furthermore, impaired processing speed, active memory capacity and cognitive processes involved in emotion regulation, such as cognitive reappraisal and attentional deployment, which require greater cognitive ability, are disrupted in individuals with MS [6]. Consequently, common emotional issues, such as depression, irritability, anhedonia, inappropriate crying and laughing, severe mood swings, and a general sense of emotional dysregulation are prevalent among MS patients. Emotional dysregulation and ineffective emotion regulation strategies can result in emotional problems, such as depression, anxiety and stress, irrespective of the severity of the disease and executive function capabilities [7].
The capacity to recognize and comprehend emotions has been linked to the ability to identify bodily sensations, a concept known as interoception [8]. Interoceptive awareness refers to the ability to perceive and recognize internal bodily sensations and signals, such as heartbeat, breathing, hunger, and pain. It involves being aware of and accurately interpreting these bodily sensations, which can provide valuable information about one’s physical and emotional state [9]. This concept is based on James and Lange’s theory of emotion, which posits that, regardless of how emotions are triggered, they result in changes in the body—including facial expressions, tone of voice, body gestures, heart rate rhythm, muscle tension, digestive activity, and hormonal levels—and subsequently trigger sensory perceptions of these changes [10]. These conceptualizations emphasize that physiological changes are integral to the recognition and understanding of emotions. They enhance the capacity to respond physiologically to emotions and to modulate them effectively. This process includes being aware of one’s emotional states, identifying emotional triggers, and understanding the root causes of particular emotional reactions [11]. Elevated levels of interoceptive awareness are linked to improved skills in emotion regulation, as individuals with a profound comprehension of their emotions are better equipped to control them [12]. In contrast, individuals with restricted interoceptive awareness may find it challenging to recognize and govern their emotions, which could result in increased difficulties in emotion regulation [13]. Lower interoception scores are associated with alexithymia, emotion dysregulation, and depression [14]. The multidimensional assessment of interoceptive awareness (MAIA) is one of the most widely used self-report questionnaires to measure interoception, which includes several dimensions, including noticing, not-distracting, not-worrying, attention regulation, emotional awareness, self-regulation, body listening, and trusting [15].
Interoceptive awareness has been investigated in various mental health conditions. In individuals with alcohol use disorder, higher interoceptive accuracy is linked to improved acceptance of negative emotions, while higher interoceptive sensibility is associated with difficulties in impulse control during negative emotions [11]. Children with autism spectrum disorder exhibit comparable interoceptive awareness but demonstrate enhanced sustained attention to internal cues [16]. Individuals with schizophrenia exhibit deficits in interoceptive accuracy and sensibility but not in interoceptive awareness [17]. In those with anorexia nervosa and their relatives, certain aspects of interoceptive awareness, such as increased bodily sensations and diminished trust in their bodies, may contribute to the symptomatology and elevate the risk of developing the disorder [18]. Research on interoceptive awareness disorder in MS is limited and existing studies predominantly focus on its neuroanatomical aspects, such as the damage to brain regions involved in interoceptive awareness and its correlation with fatigue in MS patients [19]. However, research has shown difficulties in the awareness of emotions and their bodily symptoms and worries about bodily symptoms, which often is associated with anxiety and difficulties in self-regulation in MS patients [20].
In addition to emotional dysregulation, individuals with MS may also experience alterations in their ability to recognize and process internal bodily signals. Interoceptive awareness, which depends on the integration of multisensory bodily signals, is compromised in MS due to disruptions in multisensory integration, particularly in brain regions associated with the immune system. Giurgola et al. [21] found impaired multisensory integration in relapsing-remitting MS patients, indicating a significant impact on interoceptive processing. Moreover, various studies have reported changes in the perception of physiological bodily signals among MS patients, including disruptions in olfaction, taste, body temperature processing, chronic pain, and fatigue. These disruptions are linked to mechanisms involved in interoceptive awareness processing, such as the monitoring of autonomic bodily information. Additionally, structural alterations have been observed in key brain regions responsible for processing internal bodily signals, notably the right insula and anterior cingulate cortex (ACC), in individuals with MS [22]. These structural changes reflect disturbances in the internal processing system, ultimately leading to alterations in interoceptive awareness [21].
It appears MS not only causes emotional problems and disorders of emotional regulation but also affects the body’s awareness and its components. The impact of MS on emotion regulation becomes particularly important as studies have shown that emotional awareness and emotional control difficulties negatively affect the well-being of healthy individuals and clinical populations. As a result of emotional dysregulation, individuals with MS may have difficulty with other social and occupational functions, treatment adherence, life quality and life satisfaction [23]. A number of studies utilizing self-report measures of emotional dysregulation suggest that MS patients use ineffective emotion regulation strategies during stressful diagnosis and treatment situations. Consequently, using body-based approaches and increasing interoceptive awareness can improve emotion regulation mechanisms and reduce emotional problems such as anxiety and depression in MS patients [24].
In some clinical and non-clinical populations, links have been established between interoception and emotion regulation difficulty; however, MS’s moderating role has not been explored. The MAIA, version 2 (MAIA-2) questionnaire has not yet been used to examine the moderating effect of MS on interoceptive body awareness and emotional regulation compared to a healthy group. Thus, in this study, we examined the relationship between interoceptive awareness and difficulty regulating emotions among patients with MS compared to healthy individuals. This study aimed to determine whether MS acts as a moderator between interoceptive awareness and difficulty regulating emotions. This study provides important insights into the relationship between these constructs. Furthermore, it can be utilized to prioritize interventions for this specific population and to emphasize the importance of paying attention to bodily and interoceptive awareness in order to manage emotional problems in this population.
Methods
This cross-sectional study employed a purposive sampling strategy to recruit a cohort of 429 participants. Among all MS patients who visited Emma Khomeini and Sina Hospitals, we specifically targeted individuals diagnosed with RRMS. Concurrently, healthy subjects were recruited through purposive sampling from healthy caregivers and/or companions of MS patients, ensuring matching in age, education level and gender with the MS patient group. All questionnaires were computerized and completed online via a secure digital survey platform (Porsall). RRMS patients at these clinics were first referred to the researcher by a neurologist. Afterward, the researcher offered a concise overview of the research goals to both patients and their caregivers or companions. Those willing to participate and meet the inclusion criteria were chosen. They were then provided with a secure online survey link to engage in the study and asked to complete the questionnaires during their clinic visit. Inclusion criteria for healthy participants necessitated an age range between 18 and 45 years old, the absence of physical and neurological disease and psychiatric disorders, and no history of substance abuse. MS patient’s inclusion criteria considered age range between 18 and 45, diagnosis confirmation of RRMS by a neurologist, absence of psychotic psychiatric disorders, exclusion of other neurological diseases and no history of substance abuse. Participants, both patients and healthy individuals were apprised of the voluntary nature of their involvement, with the option to decline participation and assurance of confidentiality for all provided information. The conclusive dataset comprised 161 individuals with RRMS and 268 healthy counterparts, forming the basis for subsequent analyses.
Research tools
MAIA-2
The original MAIA measures multiple dimensions of interoception bodily awareness developed by Mehling et al. [15]. It consists of 32 items and eight distinct subscales: 1) Noticing (i.e. the self-reported tendency to be aware of one’s body sensations, regardless of how comfortable or uncomfortable they are); 2) Not-distracting (i.e. the tendency to not ignore pain or uncomfortable body sensations); 3) Not-worrying (i.e. the tendency to not worry or feel distressed about pain or uncomfortable sensations); 4) Attention regulation (i.e. the ability to pay attention to bodily sensations); 5) Emotional awareness (i.e. the extent to which emotional states are perceived as connected to bodily sensations); 6) Self-regulation (i.e. the ability to use attention to bodily sensations (e.g. breathing-as a regulatory pathway of distress); 7) Body listening (i.e. listening actively to the body for insight); and 8) Trusting (i.e. the extent to which the body is experienced as trustworthy). The MAIA-2 includes five additional items over the MAIA, which improve the MAIA’s internal consistency and reliability. MAIA-2 retains the eight subscales of the original but contains 37 items. Three new items have been added to the not-distracting scale: 1) I try to ignore pain (R); 2) I push discomfort away by focusing on something else (R); and 3) When I feel unpleasant body sensations, I occupy myself with something else so I do not have to feel them (R). On the not-worrying scale, the two new items are 1) I can stay calm and not worry when I have discomfort or pain, and 2) When I am in discomfort or pain, I cannot get it out of my mind (R). Reverse scoring is indicated by R. MAIA-2 items range from zero “never” to five “always,” with nine reversed items (items 5, 6, 7, 8, 9, 10, 11, 12 and 15 are reversed). Cronbach’s α determined MAIA-2’s reliability. The number of items varies for each subscale: noticing (four items, α=0.64), not-distracting (six items, α=0.74), not-worrying (five items, α=0.67), attention regulation (seven items, α=0.83), emotional awareness (five items, α=0.79), self-regulation (four items, α=0.79), body listening (three items, α=0.80) and trusting (three items, α=0.83). The arithmetic average of the items is taken to calculate the subscale scores. The higher the score, the better the self-reported interoception [25]. The Persian version of MAIA-2 also exhibited significant divergent validity (-0.20 to -0.59) with the difficulties in emotion regulation scale (DERS) and significant convergent validity (0.18 to 0.38) with the mindful attention awareness scale, both at the 0.01 significance level. The reliability of the Persian version of the questionnaire, with Cronbach’s α ranging from 0.58 to 0.88, is satisfactory [26]. According to Cronbach’s α, this questionnaire had an internal consistency of 0.90 in the present study.
DERS
The DERS was developed by Gratz and Roemer in 2004. On a five-point Likert scale (ranging from zero (almost never [0–10%]) to five (almost always [91–100%]), higher scores indicate greater difficulty in emotion regulation (i.e. total score from 36 to 180). Six components make up this questionnaire: 1) Nonacceptance of emotional responses, 2) Difficulty engaging in goal-directed behavior, 3) Difficulty controlling impulses, 4) Lack of emotional awareness, 5) Limited access to emotion regulation strategies and 6) Lack of emotional clarity. Using factor analysis, six factors were identified. The results show that this scale has a high internal consistency of 0.93 and all six scales have a Cronbach’s α >0.80 [27]. Previous research has confirmed the construct and predictive validity of the model in clinical and non-clinical samples. According to Besharat [28], Cronbach’s α coefficients for the components of this questionnaire ranged from 0.73 to 0.92, and the re-test reliability was also between 0.69 and 0.87. The convergence and discriminant validity of a differentiating emotion regulation difficulty scale were calculated and confirmed using the mental health inventory, cognitive emotion regulation questionnaire, and positive and negative affect schedule for various samples from clinical and non-clinical groups at the same time. Using factor analysis and internal consistency coefficients, the test results were also valid and reliable and >0.93 [27]. In addition, the Persian version of the DERS had an internal consistency of 0.79 to 0.92. In the present study, the internal consistency of this questionnaire was 0.94 using Cronbach’s α method.
Results
In the present study, which sought to determine the moderating role of MS in the relationship between interoceptive awareness and emotion regulation difficulty, 429 people were examined. A sample of the present study, in terms of health condition (suffering from MS or not), consisted of 161 MS patients (37.5%) and 268 healthy people (62.5%). In terms of gender, 345 cases were women (80.4%) and 84 cases were men (19.6%), and in terms of education level 49 cases (11.4%) had diploma, 11 people (2.6%) had an associate degree, 69 cases (16.1%) had bachelor’s education, 84 cases (19.6%) had master’s education, 180 cases (42%) had doctorate education and 36 cases (8.4%) were missing. Regarding the marital status, 215 individuals (51.1%) were single, and 214 people (49.9%) were married. Also, the Mean±SD of the age of the participants were 33.27 and 7.58, respectively.
In Table 1, the indicators of central tendency and dispersion, as well as the correlation of research variables, are presented.
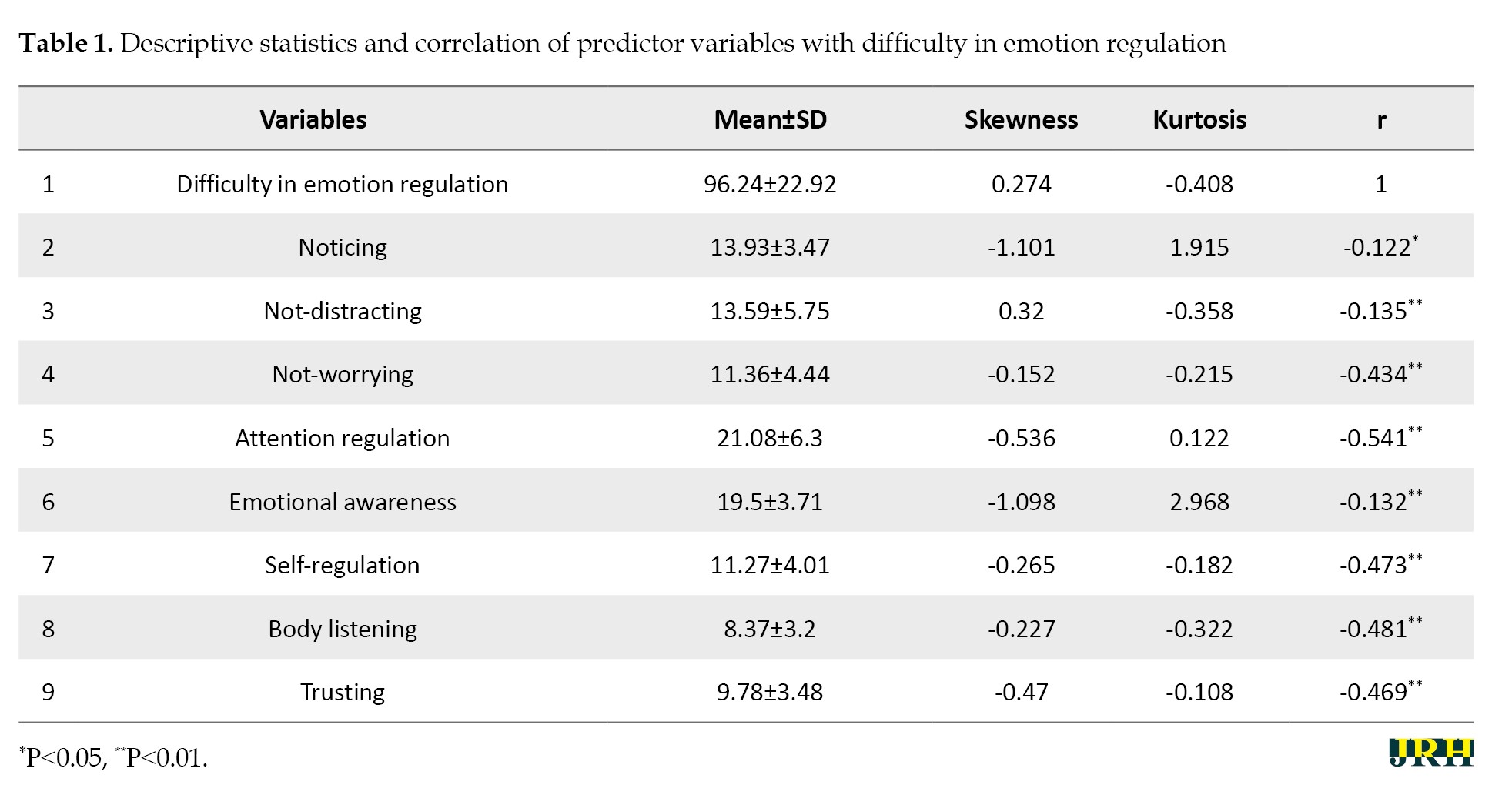
According to Table 1, all interoceptive awareness components had an inverse and significant relationship with difficulty in emotion regulation. Also, among the components of interoceptive awareness, attention regulation, body listening, and self-regulation had the highest correlation with emotion regulation difficulties. Before analyzing the data, the assumptions of normality were checked. The skewness and kurtosis indices were investigated to assess the normality of the distribution of the variables. Chou and Bentler [29] consider a cutoff point of ±3 to be appropriate for the skewness value. For the kurtosis index, values exceeding ±10 are generally problematic in multivariate research. The values obtained for the skewness and kurtosis indicated that the assumption of normality is fulfilled. Examining the correlation matrix between the observed variables indicated the absence of multi-collinearity between them. The correlation coefficients for research variables were <0.80. Correlation coefficients >0.85 create problems in the correct estimation of the model by creating multiple collinearity problems. Also, to check the hypothesis of non-collinearity, the variance inflation factor (VIF) and tolerance index were also used, with none of the tolerance index values being <0.40. Furthermore, none of the VIF values exceeded 10; based on this, it is possible to ensure the assumption of non-collinearity.
Hierarchical regression was used to determine the moderating effect of health condition (suffering from MS or not) between interoceptive awareness components with emotion regulation difficulty, so that in the first block, variables of gender and interoceptive awareness components (separately) were entered into the regression equation, and in the second block, the interaction variable was entered into the regression equation. To avoid increasing the number of tables, only the second block of hierarchical regression analysis results for each of the interoceptive awareness components is presented separately in Table 2.
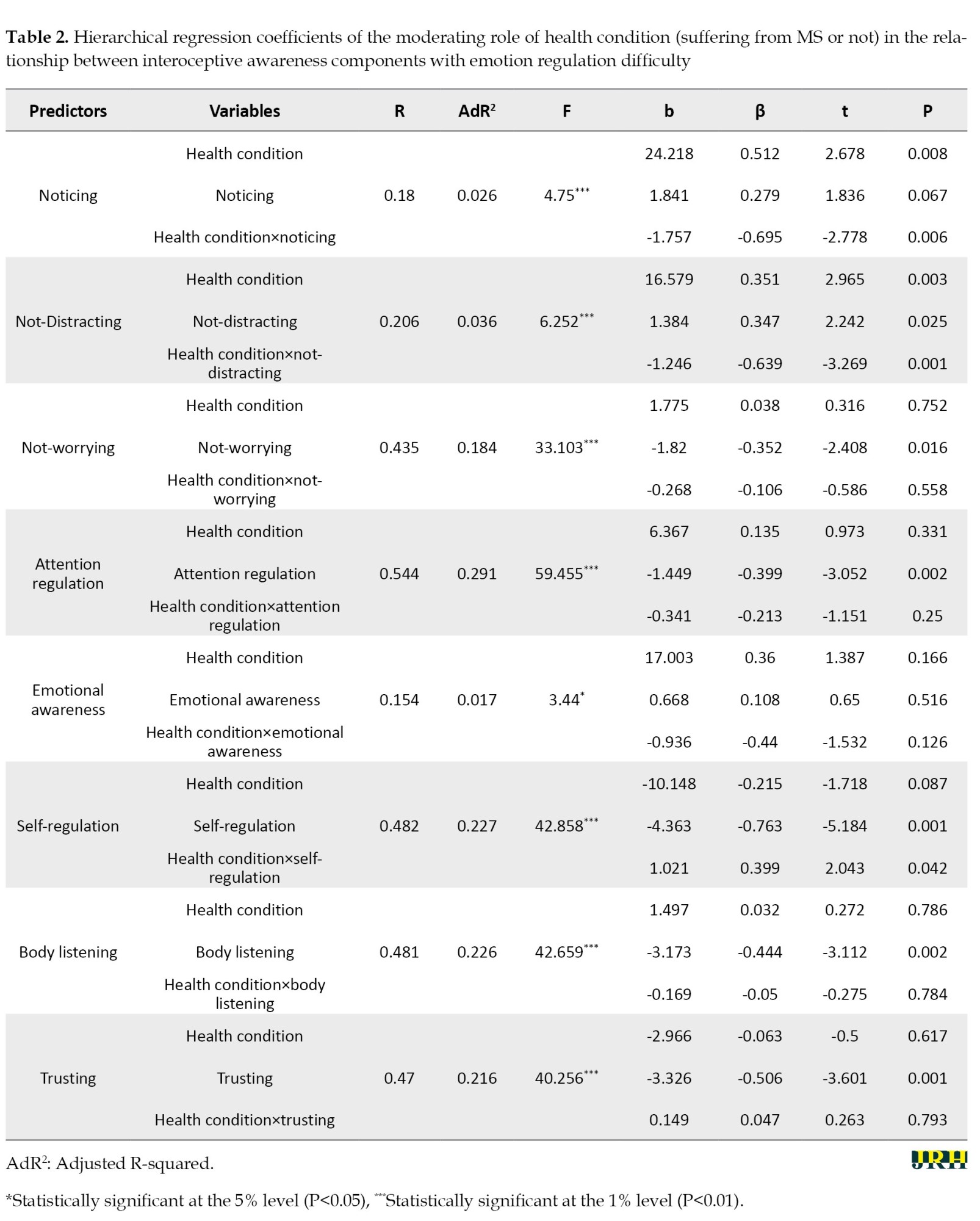
As can be seen in Table 2, the interaction effect of health condition×noticing played a significant role in predicting emotion regulation difficulty (β=-0.695, t=-2.778). Hence, it can be stated that MS plays a moderating role in noticing and emotion regulation difficulty. The results of the regression slope comparisons of emotion regulation difficulty based on noticing in the MS group (b=0.084, P=0.853) and the healthy group (b=-1.673, P=0.001) showed that the intensity of the relationship in the healthy group was more than MS group.
The interaction effect of health condition×not-distracting played a significant role in predicting emotion regulation difficulty (β=-0.639, t=-3.269). Hence, it can be stated MS plays a moderating role between not-distracting and emotion regulation difficulty. The results of the regression slope comparisons of emotion regulation difficulty based on not-distracting in the MS group (b=0.138, P=0.622) and the healthy group (b=-1.107, P=0.001) showed that the intensity of the relationship in the healthy group was more than MS group.
The interaction effect of health condition×self-regulation played a significant role in predicting the variable of emotion regulation difficulty (β=0.399, t=2.043). Hence, MS plays a moderating role between self-regulation and emotion regulation difficulty. The results of the regression slope comparisons of emotion regulation difficulty based on self-regulation in the MS group (b=-3.138, P=0.001) and healthy group (b=-2.320, P=0.001) showed that the intensity of the relationship in the MS group was more than the healthy group.
Discussion
The present study aimed to investigate the relationship between interoceptive awareness and difficulty in emotion regulation in individuals diagnosed with MS and healthy controls. Overall, the results suggest a negative and significant relationship between all components of interoceptive awareness and difficulty in emotion regulation, indicating that an increase in interoceptive awareness is associated with a decrease in difficulty in emotion regulation for both groups.
Interestingly, the moderating effect of MS on this relationship varied across the subscales of MAIA-2. Specifically, in the subscales of not-worrying, attention regulation, emotional awareness, body listening, and trusting, there was no significant difference between the healthy group and the group diagnosed with MS. This suggests that individuals with MS experienced similar benefits as the healthy group in terms of reduced emotion regulation difficulty when they exhibited higher levels of attention regulation, emotional awareness, body listening, trust, and a lack of worry. In other words, the presence of MS did not moderate the relationship between these subscales of interoceptive awareness and difficulty in emotion regulation. Comparing this finding with previous related studies, research on the relationship between interoceptive awareness and emotion regulation in individuals with MS is limited. However, there have been studies examining the relationship between interoceptive awareness and emotion regulation in other populations, such as individuals with chronic pain, such as fibromyalgia [30, 31], chronic low back pain patients (CBP) [32], and tension headache [33], somatoform disorders [34], cardiac chest pain [16], and individual with alcohol use disorder, alexithymia [14]. These studies have found that reduced interoceptive awareness is associated with difficulties in emotion regulation in these populations. This result implies that individuals with MS who have higher levels of interoceptive awareness in these particular areas may have a similar capacity to regulate their emotions as healthy individuals. With respect to the extended emotion regulation model by Gross [2], it is reasonable to argue that interoceptive awareness plays an important role in the identification of the emotion to be regulated (or not). Interoceptive accuracy and negative affect downregulation were linked, according to Füstös et al. [24]. Additionally, interoceptive sensibility deficits have been associated with difficulty regulating emotions in both sick and healthy populations [35]. It suggests that certain aspects of interoceptive awareness can have a positive impact on emotion regulation regardless of the presence of MS.
However, in the subscales of noticing and not distracting, a significant moderating effect of MS was observed. In the healthy group, an increase in attention to oneself and a decrease in distraction were associated with a reduction in difficulty in emotion regulation. Surprisingly, this relationship was not significant in the group diagnosed with MS. It appears that the role of inattention and distractibility in regulating anxiety and other unpleasant emotions in patients with MS may serve as a defense mechanism and maladaptive emotion regulation strategy. Studies indicate that individuals with MS utilize avoidance mechanisms, externally oriented thinking, distancing themselves from their emotions, and focusing on external realities instead of inner conflicts and emotions to regulate unpleasant emotions and reduce anxiety [36, 37]. Therefore, when the mechanism of inattention and distractibility effectively addresses physical symptoms and internal sensations, unpleasant emotions are temporarily and, in a bad way, regulated. Comparing these findings with previous research, while increased attention to oneself and decreased distraction may be beneficial for emotion regulation in healthy individuals, this relationship may not hold true for individuals with MS. Therefore, there may be unique factors specific to MS that affect the relationship between interoceptive awareness, and emotion regulation and more research is needed to understand the dynamics of this relationship.
In contrast, the self-regulation subscale demonstrated a significant relationship with difficulty in emotion regulation for both groups. However, the intensity of this relationship was stronger in the MS group than in the healthy group. This implies that self-regulation may play a more crucial role in emotion regulation for individuals diagnosed with MS in comparison to others. MAIA-2 defines self-regulation as the ability to regulate psychological distress by paying attention to body sensations [15]. It involves listening to the body, identifying bodily signals, becoming aware of their emotional significance, not avoiding or worrying about them, and regulating emotions through the regulation of these body sensations. According to previous research, MS patients have difficulty identifying body signals, worry about them, and prefer to avoid noticing them [36, 38, 39]. Therefore, it appears that for this population, to benefit from interoceptive awareness for emotion regulation, it is necessary to develop self-regulation skills so that they can pay attention to body sensations moment by moment and nonjudgmentally and understand their emotional significance to regulate emotions in a more adaptive manner [40]. The findings highlight the importance of addressing self-regulation abilities in interventions for individuals with MS to improve their emotion regulation.
Overall, these findings enhance our understanding of the complex relationship between interoceptive awareness and difficulty in emotion regulation among individuals diagnosed with MS and healthy individuals. The results underscore the importance of self-regulation in managing emotions, especially for individuals with MS. However, ‘noticing’ and ‘not distracting’ were not significant within the group diagnosed with MS, contrary to the healthy group, showing that ‘noticing’ and ‘not distracting’ did not have any impact on emotion regulation for those with MS. The findings suggest that interventions and therapeutic approaches for individuals diagnosed with MS should be designed to meet their unique needs. These strategies should focus on enhancing interoceptive awareness and self-regulation skills to improve their ability to regulate emotions.
Conclusion
In summary, this research contributes valuable insights into the intricate interplay of interoceptive awareness and emotion regulation in MS, emphasizing the need for tailored interventions that prioritize self-regulation skills. Psychotherapeutic approaches based on body and embodiment are those that promote self-regulation and emotion regulation through bodily awareness and interoceptive awareness. First of all, this is accomplished through exercises that focus on various sensory signals, such as bodily sensations, movements and touch, through practices such as body scanning in mindfulness exercises, meditation, and other techniques. Second, it is important to understand authentic emotional responses and modify and regulate them through sensory experiences, such as breathing, movement, gaze, and touch. Lastly, a focus will be placed on how discrete emotions are perceived, expressed, clarified, and regulated. As part of this final stage, individuals need to establish a link between their emotions and their goals in order to achieve a sense of meaning in their lives. Patients with MS will benefit from these kinds of approaches since psychological factors can contribute to the precipitation, exacerbation, perpetuation, or amelioration of their physical symptoms. Furthermore, enhancing physical skills can result in numerous psychological benefits.
Study limitation
Some limitations must be acknowledged in the present study. While the current research illuminates the specific dimension of interoceptive awareness and emotional challenges in RRMS, it is crucial to recognize that future inquiries should extend their scope to encompass other forms of MS and a diverse range of expanded disability status scale (EDSS) scores for a more comprehensive comprehension of the subject matter. A further distinction between individuals with elevated EDSS scores and those with lower scores could reveal the nuanced effects of MS severity and progression on interoceptive awareness and emotional challenges. With this enhanced understanding, targeted interventions and support mechanisms can be tailored to meet the needs of individuals across the spectrum of MS subtypes and disability levels. Furthermore, in subsequent research endeavors, it is essential to consider the potential impact of treatment regimens, such as mind-body approaches and embodiment-based psychotherapy that emphasize body awareness and its effect on emotional well-being on both interoceptive awareness and emotion regulation. Providing individuals with MS with personalized and effective support, which ultimately enhances their emotional well-being and quality of life, future studies can contribute to a more nuanced understanding by considering the impact of therapeutic approaches.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Beheshti University, Tehran, Iran (Code: IR.SBU.REC.1400.253).
Funding
This article was extracted from the PhD dissertation of Elnaz Melhi, approved by the Department of Psychology, School of Education and Psychology, Shahid Beheshti University, Tehran, Iran.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interpretation of the results, and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their gratitude to Abdorreza Naser Moghadasi at the MS Research Center of Sina Hospital in Tehran, Iran, for providing access to MS patients.
References
Emotions play a pivotal role in human functioning and well-being, making effective emotion regulation imperative for managing them [1]. Emotion regulation pertains to the mechanisms, by which individuals exert influence over the emergence, intensity, duration and manifestation of their emotions [2]. Emotional dysregulation, however, presents significant challenges. It encompasses a deficiency in awareness, understanding, and acceptance of emotions, difficulty in controlling behaviors when distressed, restricted access to adaptive strategies and a tendency to avoid emotional distress [3]. A person’s health status has a significant impact on emotion regulation because illnesses can cause cognitive-emotional and behavioral changes. A chronic and progressive illness, such as multiple sclerosis (MS), presents emotional challenges for individuals, resulting in a potential negative impact on their emotional well-being based on its chronicity and their perception of the disease’s nature, in which the immune system acts against them [4]. MS is an autoimmune disorder affecting the central nervous system, marked by the demyelination of nerve fibers, which leads to the disruption of neural communication. The symptoms of MS are diverse and can encompass mobility impairments, fatigue, pain and cognitive dysfunction [5].
MS affects individuals’ emotional functions in two main ways. As an inflammatory disease, MS is characterized by a loss of white matter throughout the brain and damage to the emotion regulation networks. It alters individuals’ ability to self-regulate and process emotion by altering the subcortical circuitry in the frontal lobe, the cingulate gyrus, and the insula. Furthermore, impaired processing speed, active memory capacity and cognitive processes involved in emotion regulation, such as cognitive reappraisal and attentional deployment, which require greater cognitive ability, are disrupted in individuals with MS [6]. Consequently, common emotional issues, such as depression, irritability, anhedonia, inappropriate crying and laughing, severe mood swings, and a general sense of emotional dysregulation are prevalent among MS patients. Emotional dysregulation and ineffective emotion regulation strategies can result in emotional problems, such as depression, anxiety and stress, irrespective of the severity of the disease and executive function capabilities [7].
The capacity to recognize and comprehend emotions has been linked to the ability to identify bodily sensations, a concept known as interoception [8]. Interoceptive awareness refers to the ability to perceive and recognize internal bodily sensations and signals, such as heartbeat, breathing, hunger, and pain. It involves being aware of and accurately interpreting these bodily sensations, which can provide valuable information about one’s physical and emotional state [9]. This concept is based on James and Lange’s theory of emotion, which posits that, regardless of how emotions are triggered, they result in changes in the body—including facial expressions, tone of voice, body gestures, heart rate rhythm, muscle tension, digestive activity, and hormonal levels—and subsequently trigger sensory perceptions of these changes [10]. These conceptualizations emphasize that physiological changes are integral to the recognition and understanding of emotions. They enhance the capacity to respond physiologically to emotions and to modulate them effectively. This process includes being aware of one’s emotional states, identifying emotional triggers, and understanding the root causes of particular emotional reactions [11]. Elevated levels of interoceptive awareness are linked to improved skills in emotion regulation, as individuals with a profound comprehension of their emotions are better equipped to control them [12]. In contrast, individuals with restricted interoceptive awareness may find it challenging to recognize and govern their emotions, which could result in increased difficulties in emotion regulation [13]. Lower interoception scores are associated with alexithymia, emotion dysregulation, and depression [14]. The multidimensional assessment of interoceptive awareness (MAIA) is one of the most widely used self-report questionnaires to measure interoception, which includes several dimensions, including noticing, not-distracting, not-worrying, attention regulation, emotional awareness, self-regulation, body listening, and trusting [15].
Interoceptive awareness has been investigated in various mental health conditions. In individuals with alcohol use disorder, higher interoceptive accuracy is linked to improved acceptance of negative emotions, while higher interoceptive sensibility is associated with difficulties in impulse control during negative emotions [11]. Children with autism spectrum disorder exhibit comparable interoceptive awareness but demonstrate enhanced sustained attention to internal cues [16]. Individuals with schizophrenia exhibit deficits in interoceptive accuracy and sensibility but not in interoceptive awareness [17]. In those with anorexia nervosa and their relatives, certain aspects of interoceptive awareness, such as increased bodily sensations and diminished trust in their bodies, may contribute to the symptomatology and elevate the risk of developing the disorder [18]. Research on interoceptive awareness disorder in MS is limited and existing studies predominantly focus on its neuroanatomical aspects, such as the damage to brain regions involved in interoceptive awareness and its correlation with fatigue in MS patients [19]. However, research has shown difficulties in the awareness of emotions and their bodily symptoms and worries about bodily symptoms, which often is associated with anxiety and difficulties in self-regulation in MS patients [20].
In addition to emotional dysregulation, individuals with MS may also experience alterations in their ability to recognize and process internal bodily signals. Interoceptive awareness, which depends on the integration of multisensory bodily signals, is compromised in MS due to disruptions in multisensory integration, particularly in brain regions associated with the immune system. Giurgola et al. [21] found impaired multisensory integration in relapsing-remitting MS patients, indicating a significant impact on interoceptive processing. Moreover, various studies have reported changes in the perception of physiological bodily signals among MS patients, including disruptions in olfaction, taste, body temperature processing, chronic pain, and fatigue. These disruptions are linked to mechanisms involved in interoceptive awareness processing, such as the monitoring of autonomic bodily information. Additionally, structural alterations have been observed in key brain regions responsible for processing internal bodily signals, notably the right insula and anterior cingulate cortex (ACC), in individuals with MS [22]. These structural changes reflect disturbances in the internal processing system, ultimately leading to alterations in interoceptive awareness [21].
It appears MS not only causes emotional problems and disorders of emotional regulation but also affects the body’s awareness and its components. The impact of MS on emotion regulation becomes particularly important as studies have shown that emotional awareness and emotional control difficulties negatively affect the well-being of healthy individuals and clinical populations. As a result of emotional dysregulation, individuals with MS may have difficulty with other social and occupational functions, treatment adherence, life quality and life satisfaction [23]. A number of studies utilizing self-report measures of emotional dysregulation suggest that MS patients use ineffective emotion regulation strategies during stressful diagnosis and treatment situations. Consequently, using body-based approaches and increasing interoceptive awareness can improve emotion regulation mechanisms and reduce emotional problems such as anxiety and depression in MS patients [24].
In some clinical and non-clinical populations, links have been established between interoception and emotion regulation difficulty; however, MS’s moderating role has not been explored. The MAIA, version 2 (MAIA-2) questionnaire has not yet been used to examine the moderating effect of MS on interoceptive body awareness and emotional regulation compared to a healthy group. Thus, in this study, we examined the relationship between interoceptive awareness and difficulty regulating emotions among patients with MS compared to healthy individuals. This study aimed to determine whether MS acts as a moderator between interoceptive awareness and difficulty regulating emotions. This study provides important insights into the relationship between these constructs. Furthermore, it can be utilized to prioritize interventions for this specific population and to emphasize the importance of paying attention to bodily and interoceptive awareness in order to manage emotional problems in this population.
Methods
This cross-sectional study employed a purposive sampling strategy to recruit a cohort of 429 participants. Among all MS patients who visited Emma Khomeini and Sina Hospitals, we specifically targeted individuals diagnosed with RRMS. Concurrently, healthy subjects were recruited through purposive sampling from healthy caregivers and/or companions of MS patients, ensuring matching in age, education level and gender with the MS patient group. All questionnaires were computerized and completed online via a secure digital survey platform (Porsall). RRMS patients at these clinics were first referred to the researcher by a neurologist. Afterward, the researcher offered a concise overview of the research goals to both patients and their caregivers or companions. Those willing to participate and meet the inclusion criteria were chosen. They were then provided with a secure online survey link to engage in the study and asked to complete the questionnaires during their clinic visit. Inclusion criteria for healthy participants necessitated an age range between 18 and 45 years old, the absence of physical and neurological disease and psychiatric disorders, and no history of substance abuse. MS patient’s inclusion criteria considered age range between 18 and 45, diagnosis confirmation of RRMS by a neurologist, absence of psychotic psychiatric disorders, exclusion of other neurological diseases and no history of substance abuse. Participants, both patients and healthy individuals were apprised of the voluntary nature of their involvement, with the option to decline participation and assurance of confidentiality for all provided information. The conclusive dataset comprised 161 individuals with RRMS and 268 healthy counterparts, forming the basis for subsequent analyses.
Research tools
MAIA-2
The original MAIA measures multiple dimensions of interoception bodily awareness developed by Mehling et al. [15]. It consists of 32 items and eight distinct subscales: 1) Noticing (i.e. the self-reported tendency to be aware of one’s body sensations, regardless of how comfortable or uncomfortable they are); 2) Not-distracting (i.e. the tendency to not ignore pain or uncomfortable body sensations); 3) Not-worrying (i.e. the tendency to not worry or feel distressed about pain or uncomfortable sensations); 4) Attention regulation (i.e. the ability to pay attention to bodily sensations); 5) Emotional awareness (i.e. the extent to which emotional states are perceived as connected to bodily sensations); 6) Self-regulation (i.e. the ability to use attention to bodily sensations (e.g. breathing-as a regulatory pathway of distress); 7) Body listening (i.e. listening actively to the body for insight); and 8) Trusting (i.e. the extent to which the body is experienced as trustworthy). The MAIA-2 includes five additional items over the MAIA, which improve the MAIA’s internal consistency and reliability. MAIA-2 retains the eight subscales of the original but contains 37 items. Three new items have been added to the not-distracting scale: 1) I try to ignore pain (R); 2) I push discomfort away by focusing on something else (R); and 3) When I feel unpleasant body sensations, I occupy myself with something else so I do not have to feel them (R). On the not-worrying scale, the two new items are 1) I can stay calm and not worry when I have discomfort or pain, and 2) When I am in discomfort or pain, I cannot get it out of my mind (R). Reverse scoring is indicated by R. MAIA-2 items range from zero “never” to five “always,” with nine reversed items (items 5, 6, 7, 8, 9, 10, 11, 12 and 15 are reversed). Cronbach’s α determined MAIA-2’s reliability. The number of items varies for each subscale: noticing (four items, α=0.64), not-distracting (six items, α=0.74), not-worrying (five items, α=0.67), attention regulation (seven items, α=0.83), emotional awareness (five items, α=0.79), self-regulation (four items, α=0.79), body listening (three items, α=0.80) and trusting (three items, α=0.83). The arithmetic average of the items is taken to calculate the subscale scores. The higher the score, the better the self-reported interoception [25]. The Persian version of MAIA-2 also exhibited significant divergent validity (-0.20 to -0.59) with the difficulties in emotion regulation scale (DERS) and significant convergent validity (0.18 to 0.38) with the mindful attention awareness scale, both at the 0.01 significance level. The reliability of the Persian version of the questionnaire, with Cronbach’s α ranging from 0.58 to 0.88, is satisfactory [26]. According to Cronbach’s α, this questionnaire had an internal consistency of 0.90 in the present study.
DERS
The DERS was developed by Gratz and Roemer in 2004. On a five-point Likert scale (ranging from zero (almost never [0–10%]) to five (almost always [91–100%]), higher scores indicate greater difficulty in emotion regulation (i.e. total score from 36 to 180). Six components make up this questionnaire: 1) Nonacceptance of emotional responses, 2) Difficulty engaging in goal-directed behavior, 3) Difficulty controlling impulses, 4) Lack of emotional awareness, 5) Limited access to emotion regulation strategies and 6) Lack of emotional clarity. Using factor analysis, six factors were identified. The results show that this scale has a high internal consistency of 0.93 and all six scales have a Cronbach’s α >0.80 [27]. Previous research has confirmed the construct and predictive validity of the model in clinical and non-clinical samples. According to Besharat [28], Cronbach’s α coefficients for the components of this questionnaire ranged from 0.73 to 0.92, and the re-test reliability was also between 0.69 and 0.87. The convergence and discriminant validity of a differentiating emotion regulation difficulty scale were calculated and confirmed using the mental health inventory, cognitive emotion regulation questionnaire, and positive and negative affect schedule for various samples from clinical and non-clinical groups at the same time. Using factor analysis and internal consistency coefficients, the test results were also valid and reliable and >0.93 [27]. In addition, the Persian version of the DERS had an internal consistency of 0.79 to 0.92. In the present study, the internal consistency of this questionnaire was 0.94 using Cronbach’s α method.
Results
In the present study, which sought to determine the moderating role of MS in the relationship between interoceptive awareness and emotion regulation difficulty, 429 people were examined. A sample of the present study, in terms of health condition (suffering from MS or not), consisted of 161 MS patients (37.5%) and 268 healthy people (62.5%). In terms of gender, 345 cases were women (80.4%) and 84 cases were men (19.6%), and in terms of education level 49 cases (11.4%) had diploma, 11 people (2.6%) had an associate degree, 69 cases (16.1%) had bachelor’s education, 84 cases (19.6%) had master’s education, 180 cases (42%) had doctorate education and 36 cases (8.4%) were missing. Regarding the marital status, 215 individuals (51.1%) were single, and 214 people (49.9%) were married. Also, the Mean±SD of the age of the participants were 33.27 and 7.58, respectively.
In Table 1, the indicators of central tendency and dispersion, as well as the correlation of research variables, are presented.
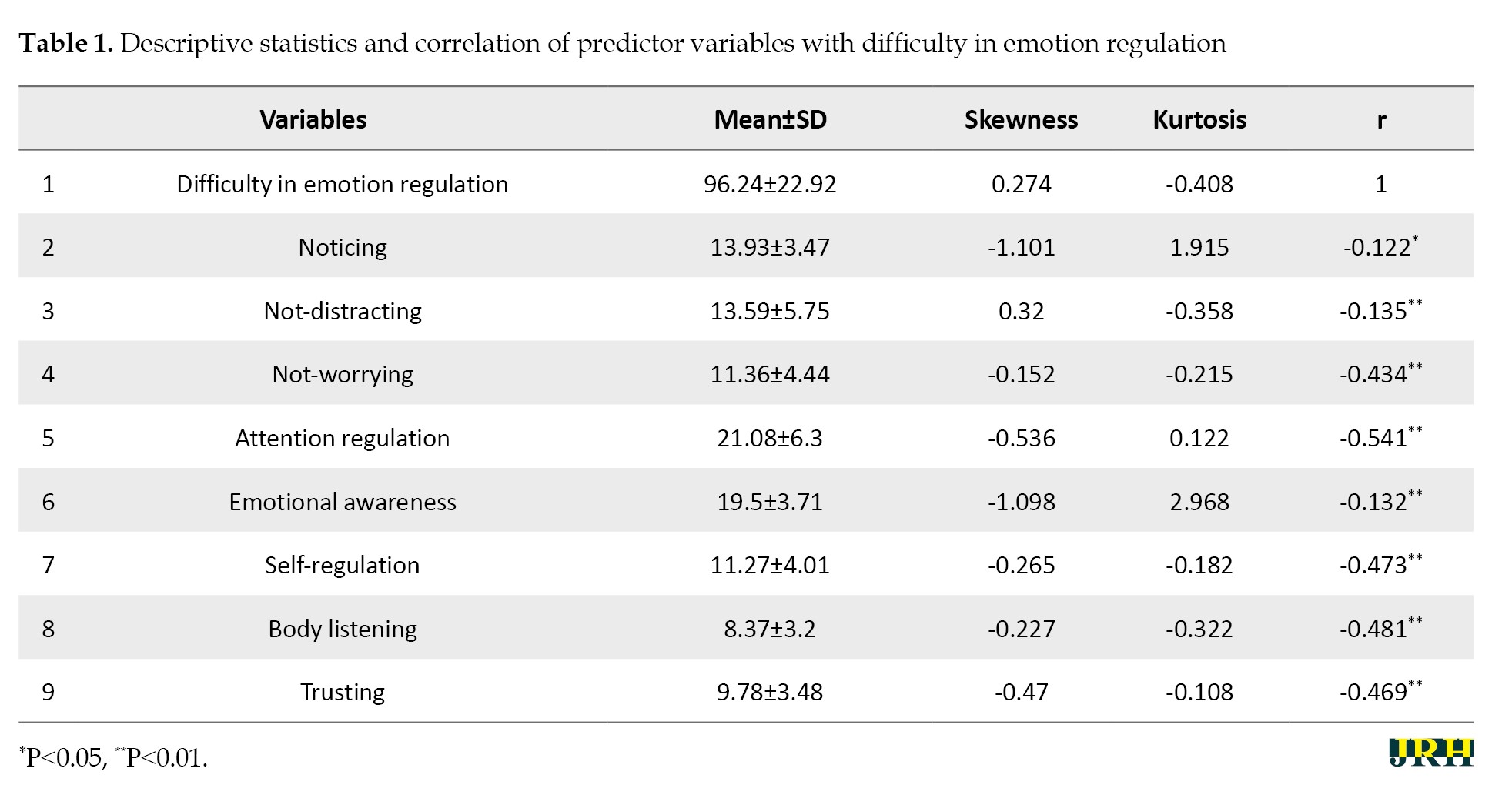
According to Table 1, all interoceptive awareness components had an inverse and significant relationship with difficulty in emotion regulation. Also, among the components of interoceptive awareness, attention regulation, body listening, and self-regulation had the highest correlation with emotion regulation difficulties. Before analyzing the data, the assumptions of normality were checked. The skewness and kurtosis indices were investigated to assess the normality of the distribution of the variables. Chou and Bentler [29] consider a cutoff point of ±3 to be appropriate for the skewness value. For the kurtosis index, values exceeding ±10 are generally problematic in multivariate research. The values obtained for the skewness and kurtosis indicated that the assumption of normality is fulfilled. Examining the correlation matrix between the observed variables indicated the absence of multi-collinearity between them. The correlation coefficients for research variables were <0.80. Correlation coefficients >0.85 create problems in the correct estimation of the model by creating multiple collinearity problems. Also, to check the hypothesis of non-collinearity, the variance inflation factor (VIF) and tolerance index were also used, with none of the tolerance index values being <0.40. Furthermore, none of the VIF values exceeded 10; based on this, it is possible to ensure the assumption of non-collinearity.
Hierarchical regression was used to determine the moderating effect of health condition (suffering from MS or not) between interoceptive awareness components with emotion regulation difficulty, so that in the first block, variables of gender and interoceptive awareness components (separately) were entered into the regression equation, and in the second block, the interaction variable was entered into the regression equation. To avoid increasing the number of tables, only the second block of hierarchical regression analysis results for each of the interoceptive awareness components is presented separately in Table 2.
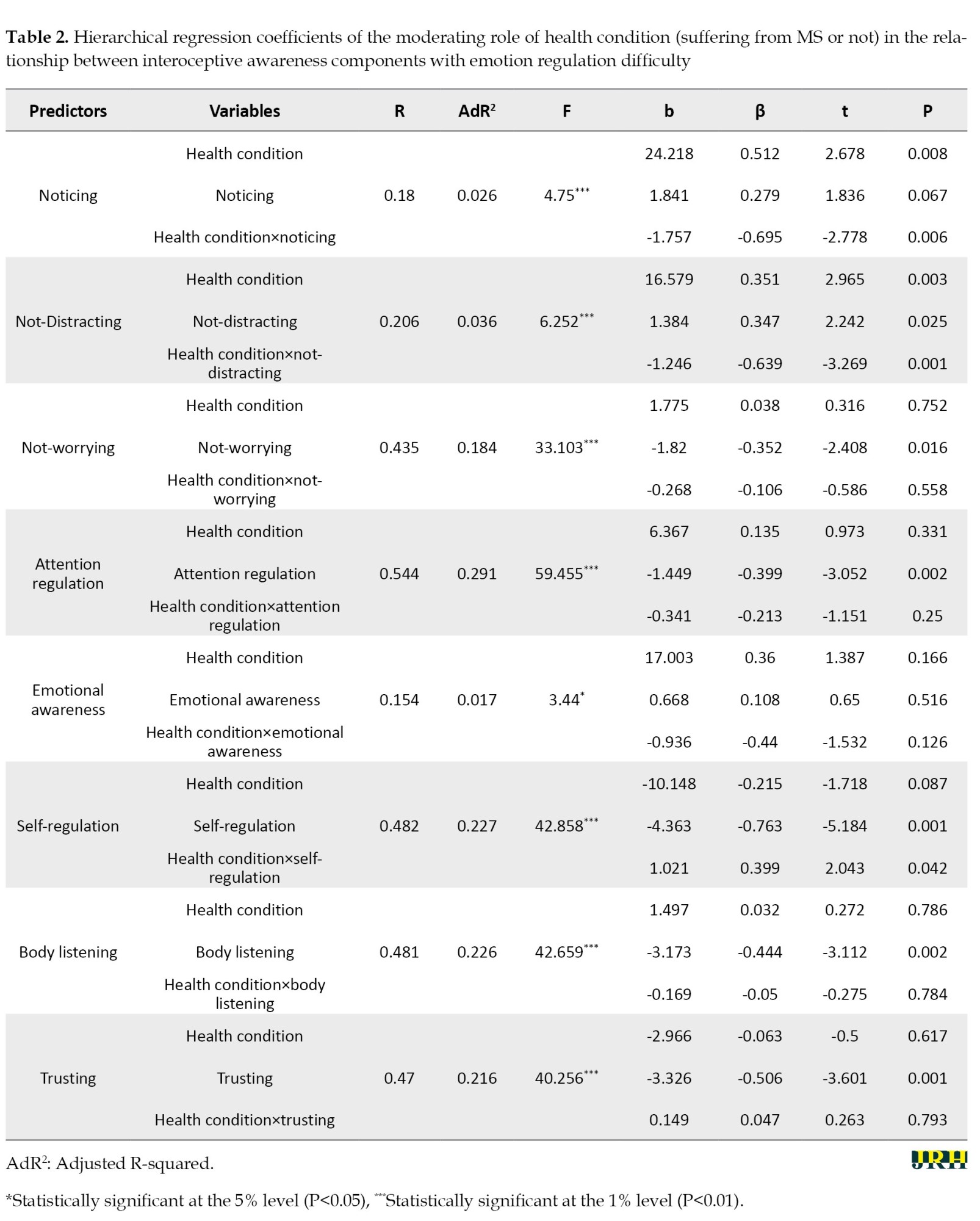
As can be seen in Table 2, the interaction effect of health condition×noticing played a significant role in predicting emotion regulation difficulty (β=-0.695, t=-2.778). Hence, it can be stated that MS plays a moderating role in noticing and emotion regulation difficulty. The results of the regression slope comparisons of emotion regulation difficulty based on noticing in the MS group (b=0.084, P=0.853) and the healthy group (b=-1.673, P=0.001) showed that the intensity of the relationship in the healthy group was more than MS group.
The interaction effect of health condition×not-distracting played a significant role in predicting emotion regulation difficulty (β=-0.639, t=-3.269). Hence, it can be stated MS plays a moderating role between not-distracting and emotion regulation difficulty. The results of the regression slope comparisons of emotion regulation difficulty based on not-distracting in the MS group (b=0.138, P=0.622) and the healthy group (b=-1.107, P=0.001) showed that the intensity of the relationship in the healthy group was more than MS group.
The interaction effect of health condition×self-regulation played a significant role in predicting the variable of emotion regulation difficulty (β=0.399, t=2.043). Hence, MS plays a moderating role between self-regulation and emotion regulation difficulty. The results of the regression slope comparisons of emotion regulation difficulty based on self-regulation in the MS group (b=-3.138, P=0.001) and healthy group (b=-2.320, P=0.001) showed that the intensity of the relationship in the MS group was more than the healthy group.
Discussion
The present study aimed to investigate the relationship between interoceptive awareness and difficulty in emotion regulation in individuals diagnosed with MS and healthy controls. Overall, the results suggest a negative and significant relationship between all components of interoceptive awareness and difficulty in emotion regulation, indicating that an increase in interoceptive awareness is associated with a decrease in difficulty in emotion regulation for both groups.
Interestingly, the moderating effect of MS on this relationship varied across the subscales of MAIA-2. Specifically, in the subscales of not-worrying, attention regulation, emotional awareness, body listening, and trusting, there was no significant difference between the healthy group and the group diagnosed with MS. This suggests that individuals with MS experienced similar benefits as the healthy group in terms of reduced emotion regulation difficulty when they exhibited higher levels of attention regulation, emotional awareness, body listening, trust, and a lack of worry. In other words, the presence of MS did not moderate the relationship between these subscales of interoceptive awareness and difficulty in emotion regulation. Comparing this finding with previous related studies, research on the relationship between interoceptive awareness and emotion regulation in individuals with MS is limited. However, there have been studies examining the relationship between interoceptive awareness and emotion regulation in other populations, such as individuals with chronic pain, such as fibromyalgia [30, 31], chronic low back pain patients (CBP) [32], and tension headache [33], somatoform disorders [34], cardiac chest pain [16], and individual with alcohol use disorder, alexithymia [14]. These studies have found that reduced interoceptive awareness is associated with difficulties in emotion regulation in these populations. This result implies that individuals with MS who have higher levels of interoceptive awareness in these particular areas may have a similar capacity to regulate their emotions as healthy individuals. With respect to the extended emotion regulation model by Gross [2], it is reasonable to argue that interoceptive awareness plays an important role in the identification of the emotion to be regulated (or not). Interoceptive accuracy and negative affect downregulation were linked, according to Füstös et al. [24]. Additionally, interoceptive sensibility deficits have been associated with difficulty regulating emotions in both sick and healthy populations [35]. It suggests that certain aspects of interoceptive awareness can have a positive impact on emotion regulation regardless of the presence of MS.
However, in the subscales of noticing and not distracting, a significant moderating effect of MS was observed. In the healthy group, an increase in attention to oneself and a decrease in distraction were associated with a reduction in difficulty in emotion regulation. Surprisingly, this relationship was not significant in the group diagnosed with MS. It appears that the role of inattention and distractibility in regulating anxiety and other unpleasant emotions in patients with MS may serve as a defense mechanism and maladaptive emotion regulation strategy. Studies indicate that individuals with MS utilize avoidance mechanisms, externally oriented thinking, distancing themselves from their emotions, and focusing on external realities instead of inner conflicts and emotions to regulate unpleasant emotions and reduce anxiety [36, 37]. Therefore, when the mechanism of inattention and distractibility effectively addresses physical symptoms and internal sensations, unpleasant emotions are temporarily and, in a bad way, regulated. Comparing these findings with previous research, while increased attention to oneself and decreased distraction may be beneficial for emotion regulation in healthy individuals, this relationship may not hold true for individuals with MS. Therefore, there may be unique factors specific to MS that affect the relationship between interoceptive awareness, and emotion regulation and more research is needed to understand the dynamics of this relationship.
In contrast, the self-regulation subscale demonstrated a significant relationship with difficulty in emotion regulation for both groups. However, the intensity of this relationship was stronger in the MS group than in the healthy group. This implies that self-regulation may play a more crucial role in emotion regulation for individuals diagnosed with MS in comparison to others. MAIA-2 defines self-regulation as the ability to regulate psychological distress by paying attention to body sensations [15]. It involves listening to the body, identifying bodily signals, becoming aware of their emotional significance, not avoiding or worrying about them, and regulating emotions through the regulation of these body sensations. According to previous research, MS patients have difficulty identifying body signals, worry about them, and prefer to avoid noticing them [36, 38, 39]. Therefore, it appears that for this population, to benefit from interoceptive awareness for emotion regulation, it is necessary to develop self-regulation skills so that they can pay attention to body sensations moment by moment and nonjudgmentally and understand their emotional significance to regulate emotions in a more adaptive manner [40]. The findings highlight the importance of addressing self-regulation abilities in interventions for individuals with MS to improve their emotion regulation.
Overall, these findings enhance our understanding of the complex relationship between interoceptive awareness and difficulty in emotion regulation among individuals diagnosed with MS and healthy individuals. The results underscore the importance of self-regulation in managing emotions, especially for individuals with MS. However, ‘noticing’ and ‘not distracting’ were not significant within the group diagnosed with MS, contrary to the healthy group, showing that ‘noticing’ and ‘not distracting’ did not have any impact on emotion regulation for those with MS. The findings suggest that interventions and therapeutic approaches for individuals diagnosed with MS should be designed to meet their unique needs. These strategies should focus on enhancing interoceptive awareness and self-regulation skills to improve their ability to regulate emotions.
Conclusion
In summary, this research contributes valuable insights into the intricate interplay of interoceptive awareness and emotion regulation in MS, emphasizing the need for tailored interventions that prioritize self-regulation skills. Psychotherapeutic approaches based on body and embodiment are those that promote self-regulation and emotion regulation through bodily awareness and interoceptive awareness. First of all, this is accomplished through exercises that focus on various sensory signals, such as bodily sensations, movements and touch, through practices such as body scanning in mindfulness exercises, meditation, and other techniques. Second, it is important to understand authentic emotional responses and modify and regulate them through sensory experiences, such as breathing, movement, gaze, and touch. Lastly, a focus will be placed on how discrete emotions are perceived, expressed, clarified, and regulated. As part of this final stage, individuals need to establish a link between their emotions and their goals in order to achieve a sense of meaning in their lives. Patients with MS will benefit from these kinds of approaches since psychological factors can contribute to the precipitation, exacerbation, perpetuation, or amelioration of their physical symptoms. Furthermore, enhancing physical skills can result in numerous psychological benefits.
Study limitation
Some limitations must be acknowledged in the present study. While the current research illuminates the specific dimension of interoceptive awareness and emotional challenges in RRMS, it is crucial to recognize that future inquiries should extend their scope to encompass other forms of MS and a diverse range of expanded disability status scale (EDSS) scores for a more comprehensive comprehension of the subject matter. A further distinction between individuals with elevated EDSS scores and those with lower scores could reveal the nuanced effects of MS severity and progression on interoceptive awareness and emotional challenges. With this enhanced understanding, targeted interventions and support mechanisms can be tailored to meet the needs of individuals across the spectrum of MS subtypes and disability levels. Furthermore, in subsequent research endeavors, it is essential to consider the potential impact of treatment regimens, such as mind-body approaches and embodiment-based psychotherapy that emphasize body awareness and its effect on emotional well-being on both interoceptive awareness and emotion regulation. Providing individuals with MS with personalized and effective support, which ultimately enhances their emotional well-being and quality of life, future studies can contribute to a more nuanced understanding by considering the impact of therapeutic approaches.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Beheshti University, Tehran, Iran (Code: IR.SBU.REC.1400.253).
Funding
This article was extracted from the PhD dissertation of Elnaz Melhi, approved by the Department of Psychology, School of Education and Psychology, Shahid Beheshti University, Tehran, Iran.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interpretation of the results, and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their gratitude to Abdorreza Naser Moghadasi at the MS Research Center of Sina Hospital in Tehran, Iran, for providing access to MS patients.
References
- Benita M, Benish-Weisman M, Matos L, Torres C. Integrative and suppressive emotion regulation differentially predict well-being through basic need satisfaction and frustration: A test of three countries. Motivation and Emotion. 2020; 44:67-81. [DOI:10.1007/s11031-019-09781-x]
- Gross JJ. Emotion regulation: Current status and future prospects. Psychological Inquiry. 2015; 26(1):1-26. [DOI:10.1080/1047840X.2014.940781]
- Thompson RA. Emotion dysregulation: A theme in search of definition. Development and Psychopathology. 2019; 31(3):805-15. [DOI:10.1017/S0954579419000282] [PMID]
- Lakin L, Davis BE, Binns CC, Currie KM, Rensel MR. Comprehensive approach to management of multiple sclerosis: Addressing invisible symptoms-A narrative review. Neurology and Therapy 2021; 10(1):75-98. [DOI:10.1007/s40120-021-00239-2] [PMID]
- McGinley MP, Goldschmidt CH, Rae-Grant AD. Diagnosis and treatment of multiple sclerosis: A review. JAMA. 2021; 325(8):765-79. [DOI:10.1001/jama.2020.26858] [PMID]
- Boron B. Neural correlates of emotion regulation in multiple sclerosis [Research Thesis]. Columbus: Ohio State University; 2019. [Link]
- Prakash RS, Schirda B, Valentine TR, Crotty M, Nicholas JA. Emotion dysregulation in multiple sclerosis: Impact on symptoms of depression and anxiety. Multiple Sclerosis and Related Disorders. 2019; 36:101399. [DOI:10.1016/j.msard.2019.101399] [PMID]
- Ventura-Bort C, Wendt J, Weymar M. The role of interoceptive sensibility and emotional conceptualization for the experience of emotions. Frontiers in Psychology. 2021; 12:712418. [DOI:10.3389/fpsyg.2021.712418] [PMID]
- Murphy J, Catmur C, Bird G. Classifying individual differences in interoception: Implications for the measurement of interoceptive awareness. Psychonomic Bulletin & Review. 2019; 26(5):1467-71. [DOI:10.3758/s13423-019-01632-7] [PMID]
- Smith R, Lane RD. The neural basis of one's own conscious and unconscious emotional states. Neuroscience and Biobehavioral Reviews. 2015; 57:1-29. [DOI:10.1016/j.neubiorev.2015.08.003] [PMID]
- Jakubczyk A, Trucco EM, Klimkiewicz A, Skrzeszewski J, Suszek H, Zaorska J, et al. Association between interoception and emotion regulation in individuals with alcohol use disorder. Frontiers in Psychiatry. 2020; 10:1028. [DOI:10.3389/fpsyt.2019.01028] [PMID]
- Price C, Smith-DiJulio K. Interoceptive awareness is important for relapse prevention: Perceptions of women who received mindful body awareness in substance use disorder treatment. Journal of Addictions Nursing. 2016; 27(1):32-8. [DOI:10.1097/JAN.0000000000000109] [PMID]
- Willem C, Gandolphe MC, Roussel M, Verkindt H, Pattou F, Nandrino JL. Difficulties in emotion regulation and deficits in interoceptive awareness in moderate and severe obesity. Eating and Weight Disorders. 2019; 24(4):633-44. [DOI:10.1007/s40519-019-00738-0] [PMID]
- Desdentado L, Miragall M, Llorens R, Baños RM. Disentangling the role of interoceptive sensibility in alexithymia, emotion dysregulation, and depression in healthy individuals. Current Psychology. 2023; 42(24):20570-82. [DOI:10.1007/s12144-022-03153-4]
- Mehling WE, Price C, Daubenmier JJ, Acree M, Bartmess E, Stewart A. The multidimensional assessment of interoceptive awareness (MAIA). Plos One. 2012; 7(11):e48230. [DOI:10.1371/journal.pone.0048230] [PMID]
- Schauder KB, Mash LE, Bryant LK, Cascio CJ. Interoceptive ability and body awareness in autism spectrum disorder. Journal of Experimental Child Psychology. 2015; 131:193-200. [DOI:10.1016/j.jecp.2014.11.002] [PMID]
- Torregrossa LJ, Amedy A, Roig J, Prada A, Park S. Interoceptive functioning in schizophrenia and schizotypy. Schizophrenia Research. 2022; 239:151-9. [DOI:10.1016/j.schres.2021.11.046] [PMID]
- Wollast R, Fossion P, Kotsou I, Rebrassé A, Leys C. Interoceptive awareness and anorexia nervosa: When emotions influence the perception of physiological sensations. The Journal of Nervous and Mental Disease. 2022; 210(5):390-3. [DOI:10.1097/NMD.0000000000001458] [PMID]
- Ware M, O'Connor P, Bub K, Backus D, McCully K. Investigating relationships among interoceptive awareness, emotional susceptibility, and fatigue in persons with multiple sclerosis. International Journal of MS Care. 2023; 25(2):75-81. [DOI:10.7224/1537-2073.2022-007] [PMID]
- Eboni ACB, Cardoso M, Dias FM, da Gama PD, Gomes S, Goncalves MVM, et al. High levels of alexithymia in patients with multiple sclerosis. Dementia & Neuropsychologia. 2018; 12(2):212-5. [DOI:10.1590/1980-57642018dn12-020015] [PMID]
- Giurgola S, Casati C, Stampatori C, Perucca L, Mattioli F, Vallar G, et al. Abnormal multisensory integration in relapsing-remitting multiple sclerosis. Experimental Brain Research. 2022; 240(3):953-68. [DOI:10.1007/s00221-022-06310-0] [PMID]
- Haider L, Zrzavy T, Hametner S, Höftberger R, Bagnato F, Grabner G, et al. The topograpy of demyelination and neurodegeneration in the multiple sclerosis brain. Brain. 2016; 139(Pt 3):807-15. [DOI:10.1093/brain/awv398] [PMID]
- Schirda B, Nicholas JA, Prakash RS. Examining trait mindfulness, emotion dysregulation, and quality of life in multiple sclerosis. Health Psychology. 2015; 34(11):1107-15. [DOI:10.1037/hea0000215] [PMID]
- Füstös J, Gramann K, Herbert BM, Pollatos O. On the embodiment of emotion regulation: Interoceptive awareness facilitates reappraisal. Social Cognitive and Affective Neuroscience. 2013; 8(8):911-7. [DOI:10.1093/scan/nss089] [PMID]
- Mehling WE, Acree M, Stewart A, Silas J, Jones A. The multidimensional assessment of interoceptive awareness, version 2 (MAIA-2). Plos One. 2018; 13(12):e0208034. [DOI:10.1371/journal.pone.0208034] [PMID]
- Melhi E, Zarani F, Panaghi L, Harirchian M. Psychometric properties of the persian version of the multidimensional assessment of interoceptive awareness, version 2 (MAIA-2. International Journal of Behavioral Sciences, 2023; 17(3):165-73. [DOI:10.30491/ijbs.2023.394681.1946]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004; 26:41-54. [DOI:10.1023/B:JOBA.0000007455.08539.94]
- Besharat M. [Difficulties in emotion regulation scale (Persian)]. Thought & Behavior in Clinical Psychology. 2018; 12(47):89-92. [Link]
- Chou CP, Bentler PM. Estimates and tests in structural equation modeling. In: Hoyle RH, editors. Structural equation modeling: Concepts, issues, and applications. Los Angeles: Sage Publications; 1995. [Link]
- Duschek S, Montoro CI, Reyes Del Paso GA. Diminished interoceptive awareness in fibromyalgia syndrome. Behavioral Medicine. 2017; 43(2):100-7. [DOI:10.1080/08964289.2015.1094442] [PMID]
- Borg C, Emond FC, Colson D, Laurent B, Michael GA. Attentional focus on subjective interoceptive experience in patients with fibromyalgia. Brain and Cognition. 2015; 101:35-43. [DOI:10.1016/j.bandc.2015.10.002] [PMID]
- Mehling WE, Daubenmier J, Price CJ, Acree M, Bartmess E, Stewart AL. Self-reported interoceptive awareness in primary care patients with past or current low back pain. Journal of Pain Research. 2013:403-18. [DOI:10.2147/JPR.S42418] [PMID]
- d’Alcalà CR, Webster DG, Esteves JE. Interoception, body awareness and chronic pain: Results from a case-control study. International Journal of Osteopathic Medicine. 2015;18(1):22-32. [DOI:10.1016/j.ijosm.2014.08.003]
- Schaefer M, Egloff B, Witthöft M. Is interoceptive awareness really altered in somatoform disorders? Testing competing theories with two paradigms of heartbeat perception. Journal of Abnormal Psychology. 2012; 121(3):719-24. [DOI:10.1037/a0028509] [PMID]
- Zamariola G, Frost N, Van Oost A, Corneille O, Luminet O. Relationship between interoception and emotion regulation: New evidence from mixed methods. Journal of Affective Disorders. 2019; 246:480-5. [DOI:10.1016/j.jad.2018.12.101] [PMID]
- Gil-González I, Martín-Rodríguez A, Conrad R, Pérez-San-Gregorio MÁ. Quality of life in adults with multiple sclerosis: A systematic review. BMJ Open. 2020; 10(11):e041249. [DOI:10.1136/bmjopen-2020-041249] [PMID]
- Chahraoui K, Duchene C, Rollot F, Bonin B, Moreau T. Longitudinal study of alexithymia and multiple sclerosis. Brain and Behavior. 2014; 4(1):75-82. [DOI:10.1002/brb3.194] [PMID]
- Calsius J, Courtois I, Feys P, Van Asch P, De Bie J, D'hooghe M. How to conquer a mountain with multiple sclerosis. How a climbing expedition to Machu Picchu affects the way people with multiple sclerosis experience their body and identity: A phenomenological analysis. Disability and Rehabilitation. 2015; 37(26):2393-9. [DOI:10.3109/09638288.2015.1027003] [PMID]
- Bonaz B, Lane RD, Oshinsky ML, Kenny PJ, Sinha R, Mayer EA, et al. Diseases, disorders, and comorbidities of interoception. Trends in Neurosciences. 2021; 44(1):39-51. [DOI:10.1016/j.tins.2020.09.009] [PMID]
- Weiss H, Johanson G, Monda L. Hakomi mindfulness-centered somatic psychotherapy: A comprehensive guide to theory and practice. New York: W. W. Norton; 2015. [Link]
Type of Study: Orginal Article |
Subject:
● Health Education
Received: 2024/01/26 | Accepted: 2024/05/25 | Published: 2025/03/2
Received: 2024/01/26 | Accepted: 2024/05/25 | Published: 2025/03/2
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









