Volume 14, Issue 5 (Sep & Oct 2024)
J Research Health 2024, 14(5): 497-504 |
Back to browse issues page
Ethics code: 0140/KEPK/VII/2022
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nurhidayati T, Rahayu D A, Kurnia A, Yusuf A, Indarwati R, Pranata S et al . Assessment of Sociodemographic Factors Influencing Depression in Elderly in Rural Communities. J Research Health 2024; 14 (5) :497-504
URL: http://jrh.gmu.ac.ir/article-1-2512-en.html
URL: http://jrh.gmu.ac.ir/article-1-2512-en.html
Tri Nurhidayati1 

 , Desy Ariyana Rahayu2
, Desy Ariyana Rahayu2 

 , Anna Kurnia2
, Anna Kurnia2 

 , Ah Yusuf3
, Ah Yusuf3 

 , Retno Indarwati3
, Retno Indarwati3 

 , Satriya Pranata2
, Satriya Pranata2 

 , Lalu Muhammad Irham4
, Lalu Muhammad Irham4 




 , Desy Ariyana Rahayu2
, Desy Ariyana Rahayu2 

 , Anna Kurnia2
, Anna Kurnia2 

 , Ah Yusuf3
, Ah Yusuf3 

 , Retno Indarwati3
, Retno Indarwati3 

 , Satriya Pranata2
, Satriya Pranata2 

 , Lalu Muhammad Irham4
, Lalu Muhammad Irham4 


1- Faculty of Nursing, Universitas Airlangga, Surabaya, Indonesia. , tnh@unimus.ac.id
2- Department of Nursing, Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Indonesia.
3- Faculty of Nursing, Universitas Airlangga, Surabaya, Indonesia.
4- Department of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, Universitas Ahmad Dahlan, Yogyakarta, Indonesia.
2- Department of Nursing, Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Indonesia.
3- Faculty of Nursing, Universitas Airlangga, Surabaya, Indonesia.
4- Department of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, Universitas Ahmad Dahlan, Yogyakarta, Indonesia.
Full-Text [PDF 550 kb]
(667 Downloads)
| Abstract (HTML) (3126 Views)
Full-Text: (877 Views)
Introduction
The world’s population is aging rapidly. In 2020, there were 1 billion people in the world who were elderly (seniors) or aged 60 years and over. That figure will rise to 1.4 billion by 2030, representing one in six people globally. By 2050, the number of individuals aged 60 years and over is expected to double to 2.1 billion. The number of older people is estimated to nearly quadruple to about 2.1 billion by 2050, with 79% of those aged 60 and older living in developing countries [1]. In Indonesia, the elderly population has nearly doubled. Badan Pusat statistic (BPS) reports that the percentage of the elderly population in Indonesia will be 11.75% in 2023. This figure represents an increase of 1.27 percentage points compared to the previous year, which was 10.48%. This situation indicates that Indonesia is transitioning to an aging population structure, as the percentage of the population over 60 years is now over 7%. It will become a country with an aging population structure if this percentage surpasses 10% [2].
Although most elderly populations are in good health, many are at risk of developing mental health conditions, such as depression and anxiety disorders [3]. The World Health Organization (WHO) states that there are 100 million cases of depression each year. According to the Non-communicable Diseases Information Center, the prevalence of depression in Indonesia shows that 11.6% of elderly individuals experience depression [4].
Mental health conditions among the elderly are often poorly recognized and undertreated. Depression is prevalent among the elderly [5]. According to the 2019 global health estimates (GHE), this condition accounts for 10.6% of total disability (measured in disability-adjusted life years (DALYs)) among the elderly. The most common mental health conditions in this age group are depression and anxiety. The 2019 GHE shows that globally, approximately a quarter of deaths due to suicide (27.2%) occur in individuals aged 60 years and over. The rate of depression is twice as high among the elderly compared to younger adults, with 10%-15% of all individuals over 65 years old living in the community exhibiting symptoms of depression [1]. Fortunately, depression is treatable. When someone is diagnosed with depression, almost 80% can achieve complete recovery [6]. The impact of depression on the elderly is severe. Untreated depression leads to increased use of medical facilities, negatively affects quality of life (QoL), and increases mortality. However, depression is often misdiagnosed and overlooked [7-9]. Symptoms of depression are often associated with internal medical problems aging process [5].
Many studies have examined depression in the elderly, but none have investigated the variables that contribute to it. The purpose of this study was to identify the factors influencing depression among the elderly in rural communities. The importance of the community lies in its rural nature, which preserves the traditions and culture of the Javanese people, yet it also carries a stigma surrounding depression. Additionally, rural Indonesia is often distant from health facilities.
Methods
Study design
This descriptive study with a cross-sectional design was conducted in a rural community in Central Java, Indonesia from January to April 2023. This served as initial data for a preliminary study.
Samples and locations
The statistical population was all elderly in a rural community in Central Java, Indonesia. The study sample included elderly individuals who met the inclusion criteria, which specified that participants must reside in rural communities.
On the other hand, elderly individuals who declined to participate were excluded from the study. Therefore, 247 respondents were obtained using a consecutive sampling approach. The advantage of using consecutive sampling is that all subjects who came and met the selection criteria were included in the research until the required number of subjects was reached. Data collection was carried out by 98 cadres, with each cadre gathering data from 2-3 elderly individuals
Data collection
Researchers collected data over four months from January to April 2023. Data collection was carried out by distributing questionnaires to the research subjects. The completed questionnaires were checked for completeness by the researcher before data entry.
Research tools
There were two measurements: A sociodemographic checklist to assess data on gender, age, education, marital status, insurance, occupation, and medical complaints, and the geriatric depression scale (GDS-15), with a scoring system where “yes” received a score of 1 and “no” received a score of 0. The categories for depression were as follows: Normal (0-4), mild depression (5-8), moderate depression (9-11), and severe depression (12-15). Furthermore, the GDS-SF demonstrated reliability and homogeneity, with Cronbach’s α=0.836 and McDonald’s Omega=0.841, and no floor or ceiling effects were observed [10] Bangladesh. Data of 377 elderly were collected, including socio-demographic characteristics, social supports, comorbidities, sleep behaviours, and depression (as measured by the GDS-SF).
Data analysis
SPSS software, version 22 was used to analyze the data. To assist with the analysis, descriptive statistics were calculated and tabulated. The chi-square bivariate analysis was performed to assess the relationship between socio-demographics and depression. The significance level was set at P<0.05 for all statistical tests.
Results
This research was conducted in Banyuroto Village, located on the slope of Merapi Mountain in Magelang, Central Java, Indonesia. The study was carried out as planned, with a total of 247 research subjects.
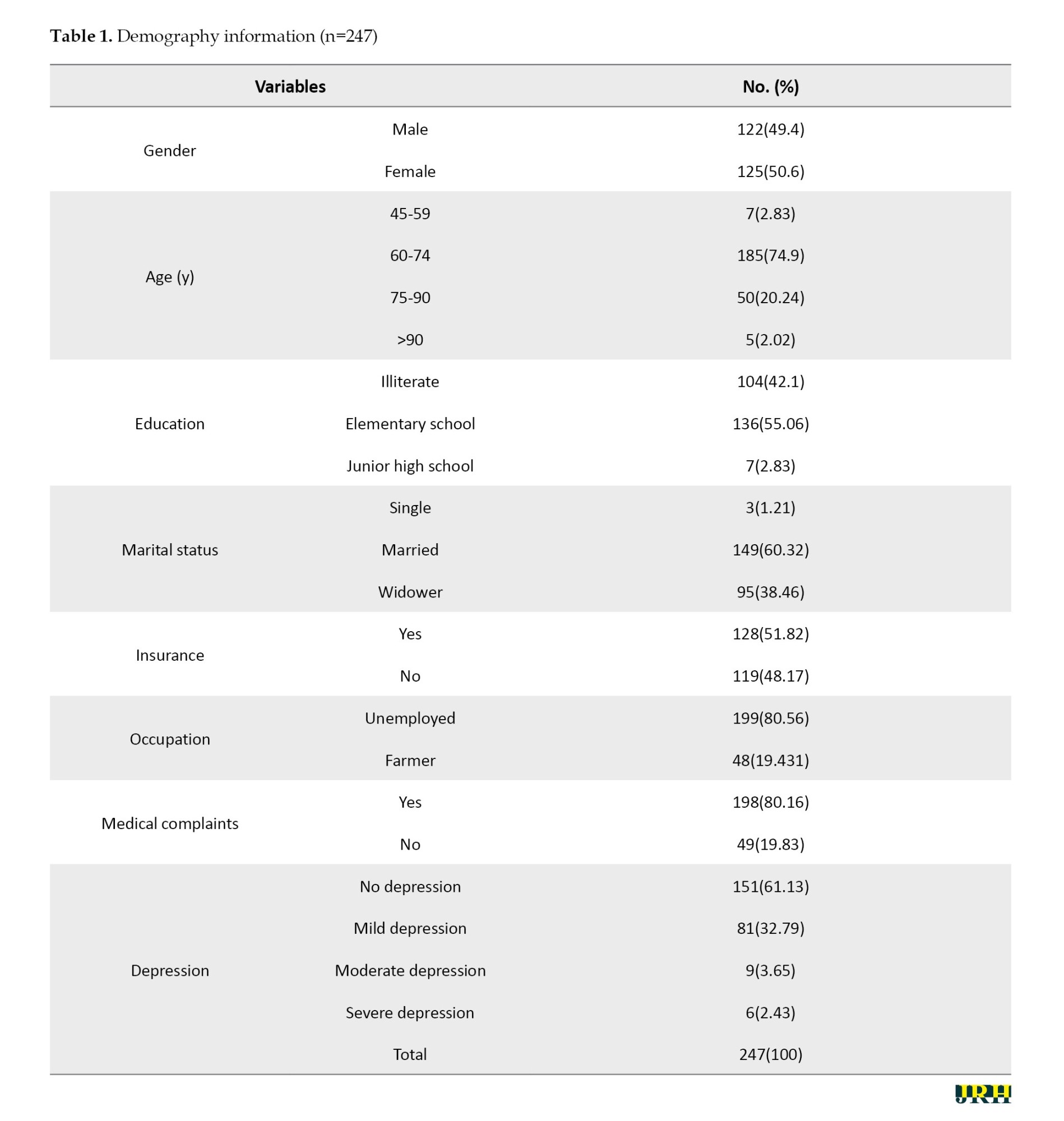
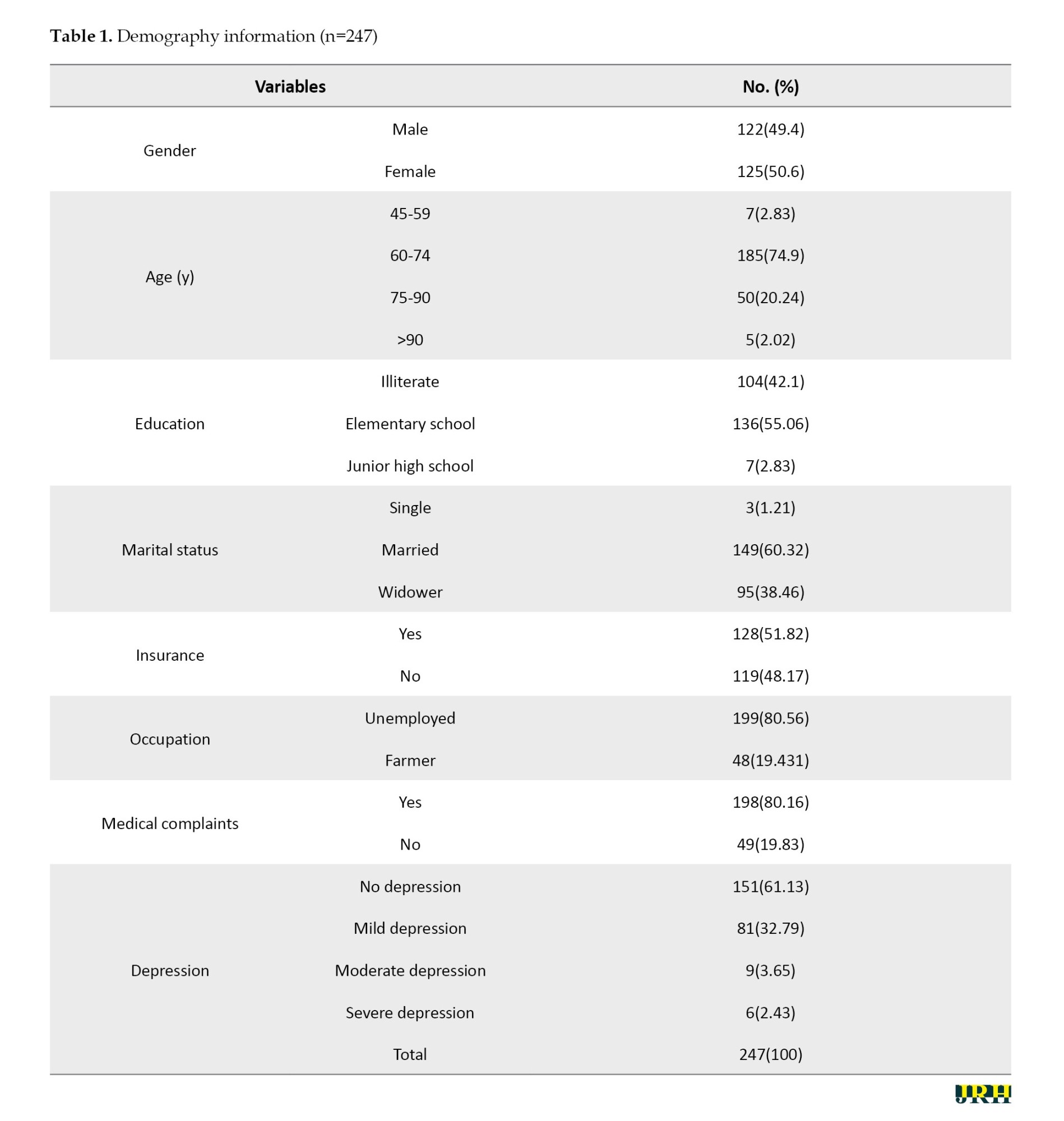
Most participants were women 50.60%, had completed elementary school (55.06%), were married (60.32%), did not have insurance (51.82%), were unemployed (80.56%), and reported no medical complaints (80.16%) (Table 1). Age was analyzed in four categories, with the dominant age group being 60-74 years (74.90%). Moreover, the research showed that most participants had no depression 61.13%.
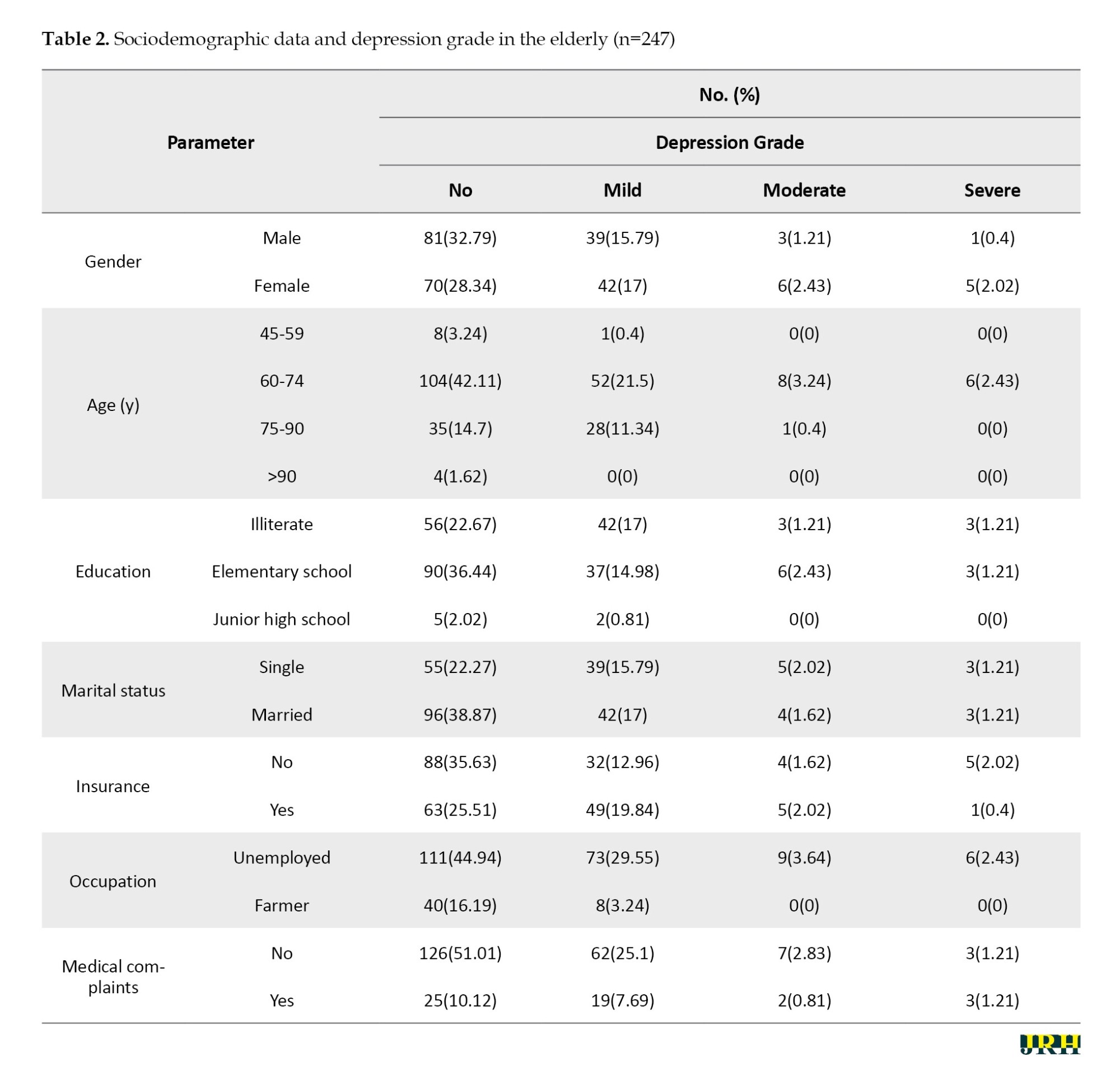
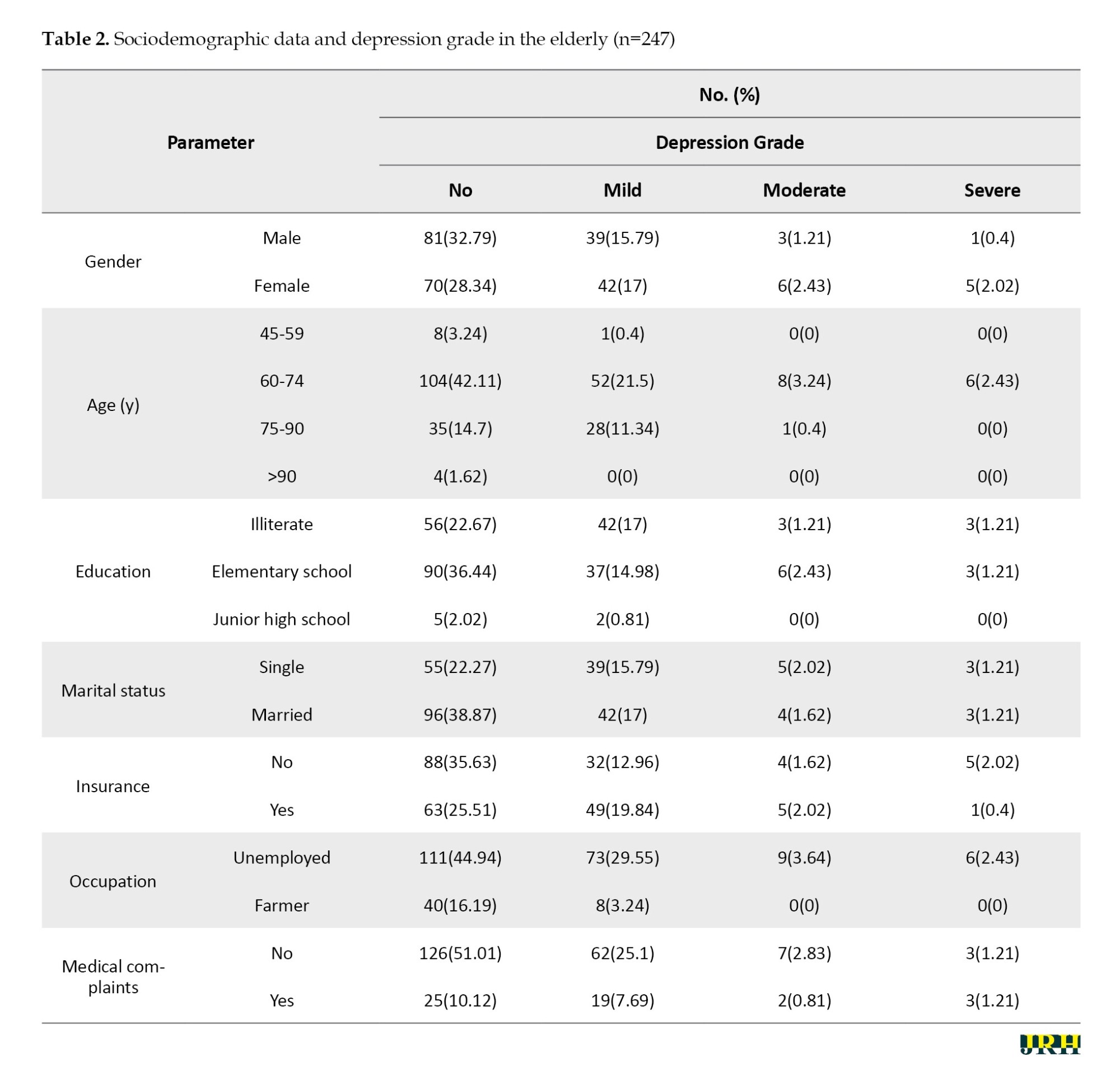
Most participants were men, aged 60-74 years, had completed elementary school, were married, did not have insurance, were unemployed, reported no medical complaints, and did not experience depression (Table 2).
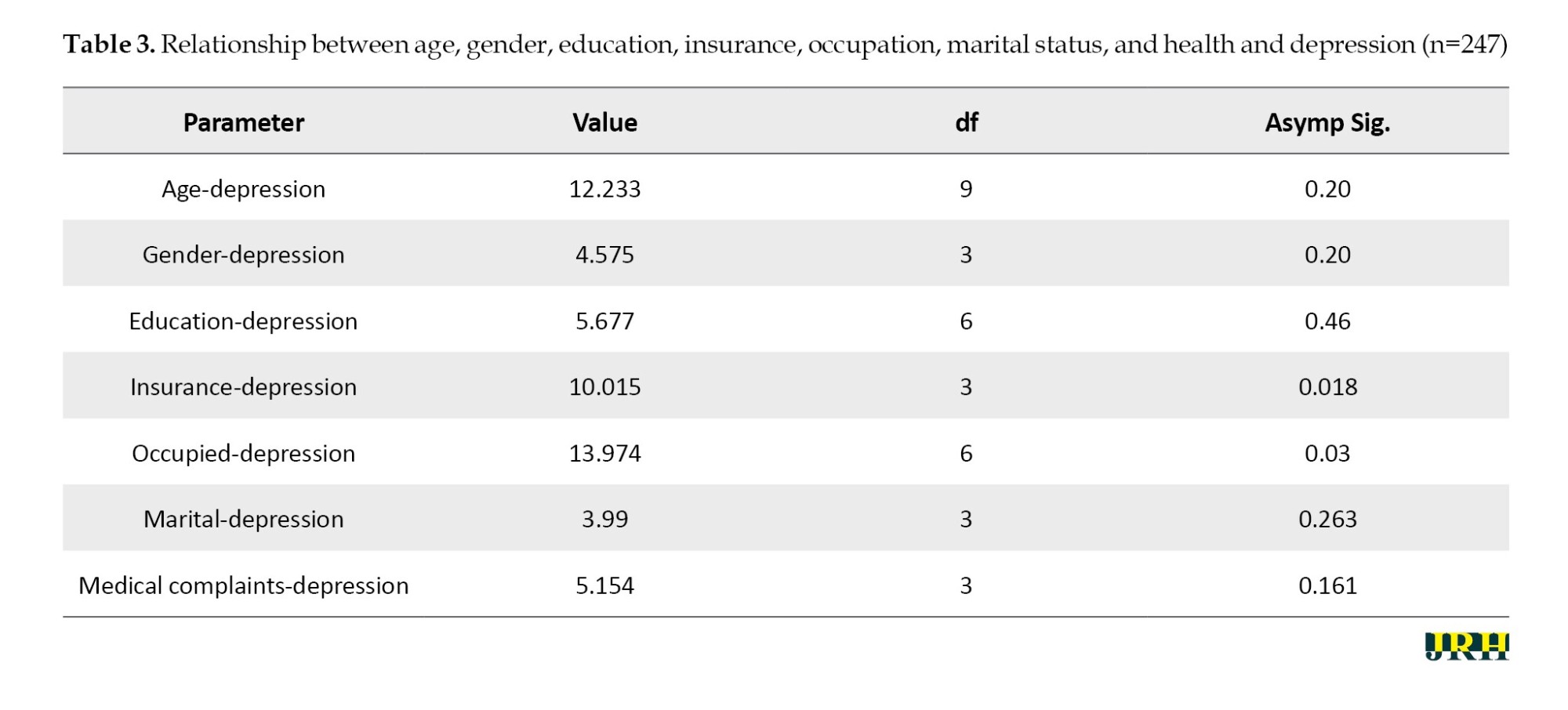
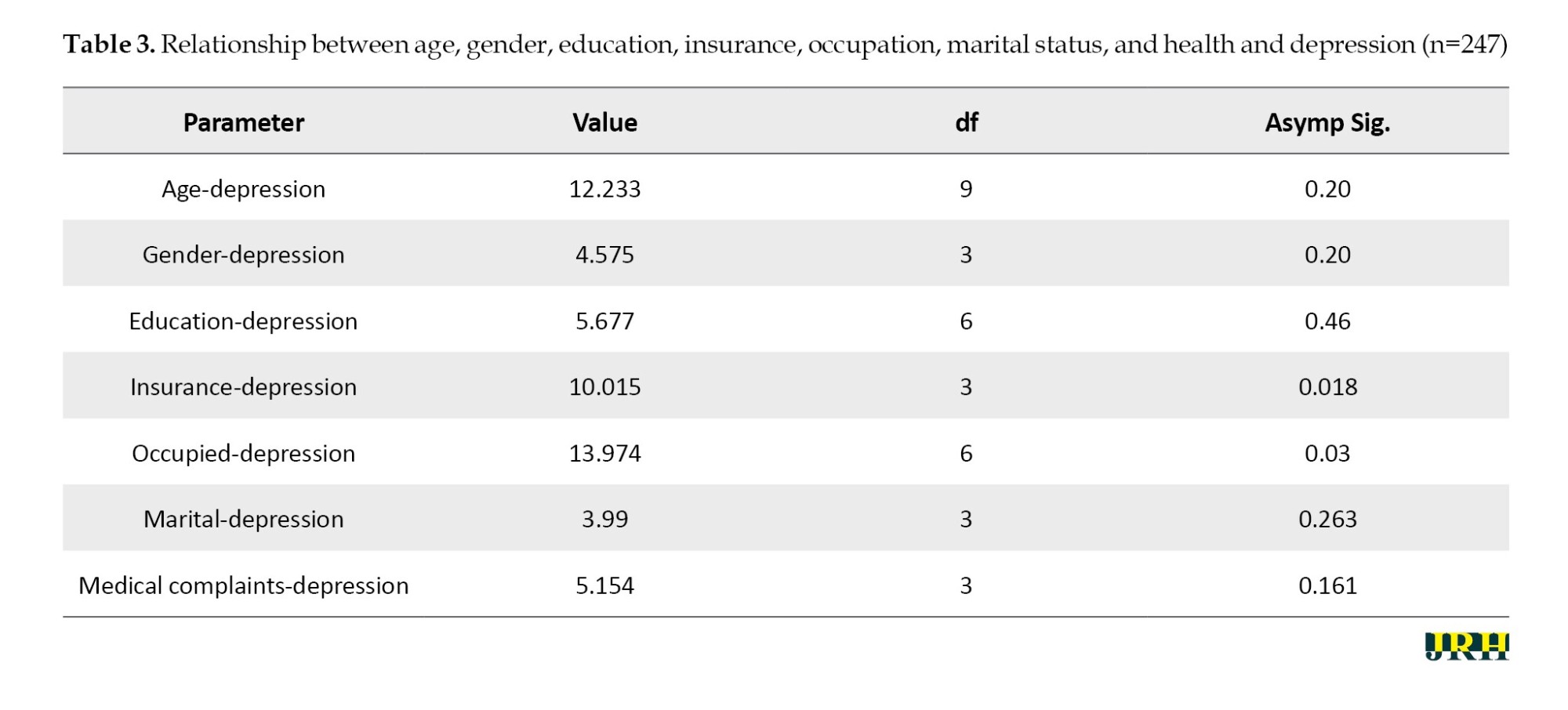
The relationship between insurance and occupation and depression was assessed through correlation analysis, specifically a chi-square correlation analysis. Table 3 shows the results of the statistical tests, indicating a significant relationship between insurance and occupation and depression in rural communities in Central Java, Indonesia, as evidenced by P of 0.018 and 0.03, respectively.
Discussion
This study aimed to assess depression among the elderly in rural communities. Symptoms of depression that manifest in the elderly include feelings of depression, anxiety, and cognitive disorders [11]. The most common symptoms are feelings of depression, which are often expressed as helplessness, sadness, and hopelessness [3, 12, 13].
The results of the study provide evidence of a relationship between insurance and depression. Most old individuals also have more than one disease [14]. Chronic and painful conditions have the potential to become significant stressors. Health-related problems often arise in old age, and these changes can make adaptation difficult, serving as stressors that trigger depression in the elderly [15]. Uncertain physical conditions require financial resources and health insurance [16]. Insurance is very important to cover medical costs; however, most participants reported having no insurance [16]. If medical costs increase, the incidence of depression among the elderly is likely to increase [17]. Unfortunately, many elderly individuals experience a decrease in income because they are unable to work easily. The majority of the elderly have low levels of education, which influences their ability to receive and understand information [18].
The life expectancy of the elderly is quite high; however, most participants were 60-74 years old. The oldest participant was 110 years old. During this period, there are changes—physically, psychologically, socially, and spiritually—that affect the quality of human life [19]. Old people experience various changes that are unavoidable, progressive, and irreversible [20-22]. The physical and functional condition of the elderly tends to decline, which increases the risk of depression [6].
Most old individuals, both men and women, still have partners, who support them. However, some elderly individuals do not have a life partner due to divorce or the death of a partner [22]. Being can significantly impact the psychology of the elderly because of the loss of emotional support, appreciation, information, and instrumental assistance [23]. This situation is further exacerbated if there is no supportive family and if the individual belongs to a lower middle economic status [24].
In general, depression among elderly men and women is the same; however, men are less likely to seek help to address the problem [25]. Elderly women are more susceptible to factors that cause depression. Women tend to cope better than men by surrendering to their feelings and seeking help from others. Early detection of depression in the elderly within rural communities is crucial for promoting a positive mental health lifestyle among this population. The community is rural and retains the traditions and culture of the Javanese people, but it also harbors a stigma surrounding depression. Rural areas in Indonesia are often far from health facilities. The relationship between insurance and occupation and depression affects the elderly as they prepare for old age with adequate financial resources, including retirement savings, to ensure financial stability. Seniors can prepare for old age by calculating their retirement fund needs, saving, investing, and obtaining insurance for pension and health fund protection.
Conclusion
Only two factors affect depression: insurance and occupation. However, the disparity in the number of respondents across each sociodemographic group made the results of this study less representative. As a result, further research on the factors that contribute to depression is necessary. Seniors can prepare for old age by calculating their retirement fund needs, saving, investing, and obtaining insurance for pension and health fund protection.
Ethical Considerations
Compliance with ethical guidelines
This paper was ethically approved by the Health Research Ethics Committee, Faculty of Nursing and Health Science, Universitas Muhammadiyah Semarang (Code: 0140/KEPK/VII/2023). Respondents were informed about the study and invited to participate. Each participant received a study instrument that included a questionnaire and signed informed consent.
Funding
This study was financially supported by the Universitas Muhammadiyah Semarang (Grant No.: 326/UNIMUS/2023).
Authors' contributions
Conceptualization and data analysis: Tri Nurhidayati and Satriya Pranata; Methodology: Tri Nurhidayati, Desy Ariyana Rahayu and Anna Kurnia and Lalu Muhammad Irham; Data collection and writing the original draft: Tri Nurhidayati; Investigation, review and editing: Satriya Pranata; Funding administration: Tri Nurhidayati, Desy Ariyana Rahayu and Anna Kurnia; Supervision: Ah Yusuf and Retno Indarwati.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants and Universitas Muhammadiyah Semarang for grant support in this research.
References
The world’s population is aging rapidly. In 2020, there were 1 billion people in the world who were elderly (seniors) or aged 60 years and over. That figure will rise to 1.4 billion by 2030, representing one in six people globally. By 2050, the number of individuals aged 60 years and over is expected to double to 2.1 billion. The number of older people is estimated to nearly quadruple to about 2.1 billion by 2050, with 79% of those aged 60 and older living in developing countries [1]. In Indonesia, the elderly population has nearly doubled. Badan Pusat statistic (BPS) reports that the percentage of the elderly population in Indonesia will be 11.75% in 2023. This figure represents an increase of 1.27 percentage points compared to the previous year, which was 10.48%. This situation indicates that Indonesia is transitioning to an aging population structure, as the percentage of the population over 60 years is now over 7%. It will become a country with an aging population structure if this percentage surpasses 10% [2].
Although most elderly populations are in good health, many are at risk of developing mental health conditions, such as depression and anxiety disorders [3]. The World Health Organization (WHO) states that there are 100 million cases of depression each year. According to the Non-communicable Diseases Information Center, the prevalence of depression in Indonesia shows that 11.6% of elderly individuals experience depression [4].
Mental health conditions among the elderly are often poorly recognized and undertreated. Depression is prevalent among the elderly [5]. According to the 2019 global health estimates (GHE), this condition accounts for 10.6% of total disability (measured in disability-adjusted life years (DALYs)) among the elderly. The most common mental health conditions in this age group are depression and anxiety. The 2019 GHE shows that globally, approximately a quarter of deaths due to suicide (27.2%) occur in individuals aged 60 years and over. The rate of depression is twice as high among the elderly compared to younger adults, with 10%-15% of all individuals over 65 years old living in the community exhibiting symptoms of depression [1]. Fortunately, depression is treatable. When someone is diagnosed with depression, almost 80% can achieve complete recovery [6]. The impact of depression on the elderly is severe. Untreated depression leads to increased use of medical facilities, negatively affects quality of life (QoL), and increases mortality. However, depression is often misdiagnosed and overlooked [7-9]. Symptoms of depression are often associated with internal medical problems aging process [5].
Many studies have examined depression in the elderly, but none have investigated the variables that contribute to it. The purpose of this study was to identify the factors influencing depression among the elderly in rural communities. The importance of the community lies in its rural nature, which preserves the traditions and culture of the Javanese people, yet it also carries a stigma surrounding depression. Additionally, rural Indonesia is often distant from health facilities.
Methods
Study design
This descriptive study with a cross-sectional design was conducted in a rural community in Central Java, Indonesia from January to April 2023. This served as initial data for a preliminary study.
Samples and locations
The statistical population was all elderly in a rural community in Central Java, Indonesia. The study sample included elderly individuals who met the inclusion criteria, which specified that participants must reside in rural communities.
On the other hand, elderly individuals who declined to participate were excluded from the study. Therefore, 247 respondents were obtained using a consecutive sampling approach. The advantage of using consecutive sampling is that all subjects who came and met the selection criteria were included in the research until the required number of subjects was reached. Data collection was carried out by 98 cadres, with each cadre gathering data from 2-3 elderly individuals
Data collection
Researchers collected data over four months from January to April 2023. Data collection was carried out by distributing questionnaires to the research subjects. The completed questionnaires were checked for completeness by the researcher before data entry.
Research tools
There were two measurements: A sociodemographic checklist to assess data on gender, age, education, marital status, insurance, occupation, and medical complaints, and the geriatric depression scale (GDS-15), with a scoring system where “yes” received a score of 1 and “no” received a score of 0. The categories for depression were as follows: Normal (0-4), mild depression (5-8), moderate depression (9-11), and severe depression (12-15). Furthermore, the GDS-SF demonstrated reliability and homogeneity, with Cronbach’s α=0.836 and McDonald’s Omega=0.841, and no floor or ceiling effects were observed [10] Bangladesh. Data of 377 elderly were collected, including socio-demographic characteristics, social supports, comorbidities, sleep behaviours, and depression (as measured by the GDS-SF).
Data analysis
SPSS software, version 22 was used to analyze the data. To assist with the analysis, descriptive statistics were calculated and tabulated. The chi-square bivariate analysis was performed to assess the relationship between socio-demographics and depression. The significance level was set at P<0.05 for all statistical tests.
Results
This research was conducted in Banyuroto Village, located on the slope of Merapi Mountain in Magelang, Central Java, Indonesia. The study was carried out as planned, with a total of 247 research subjects.
Most participants were women 50.60%, had completed elementary school (55.06%), were married (60.32%), did not have insurance (51.82%), were unemployed (80.56%), and reported no medical complaints (80.16%) (Table 1). Age was analyzed in four categories, with the dominant age group being 60-74 years (74.90%). Moreover, the research showed that most participants had no depression 61.13%.
Most participants were men, aged 60-74 years, had completed elementary school, were married, did not have insurance, were unemployed, reported no medical complaints, and did not experience depression (Table 2).
The relationship between insurance and occupation and depression was assessed through correlation analysis, specifically a chi-square correlation analysis. Table 3 shows the results of the statistical tests, indicating a significant relationship between insurance and occupation and depression in rural communities in Central Java, Indonesia, as evidenced by P of 0.018 and 0.03, respectively.
Discussion
This study aimed to assess depression among the elderly in rural communities. Symptoms of depression that manifest in the elderly include feelings of depression, anxiety, and cognitive disorders [11]. The most common symptoms are feelings of depression, which are often expressed as helplessness, sadness, and hopelessness [3, 12, 13].
The results of the study provide evidence of a relationship between insurance and depression. Most old individuals also have more than one disease [14]. Chronic and painful conditions have the potential to become significant stressors. Health-related problems often arise in old age, and these changes can make adaptation difficult, serving as stressors that trigger depression in the elderly [15]. Uncertain physical conditions require financial resources and health insurance [16]. Insurance is very important to cover medical costs; however, most participants reported having no insurance [16]. If medical costs increase, the incidence of depression among the elderly is likely to increase [17]. Unfortunately, many elderly individuals experience a decrease in income because they are unable to work easily. The majority of the elderly have low levels of education, which influences their ability to receive and understand information [18].
The life expectancy of the elderly is quite high; however, most participants were 60-74 years old. The oldest participant was 110 years old. During this period, there are changes—physically, psychologically, socially, and spiritually—that affect the quality of human life [19]. Old people experience various changes that are unavoidable, progressive, and irreversible [20-22]. The physical and functional condition of the elderly tends to decline, which increases the risk of depression [6].
Most old individuals, both men and women, still have partners, who support them. However, some elderly individuals do not have a life partner due to divorce or the death of a partner [22]. Being can significantly impact the psychology of the elderly because of the loss of emotional support, appreciation, information, and instrumental assistance [23]. This situation is further exacerbated if there is no supportive family and if the individual belongs to a lower middle economic status [24].
In general, depression among elderly men and women is the same; however, men are less likely to seek help to address the problem [25]. Elderly women are more susceptible to factors that cause depression. Women tend to cope better than men by surrendering to their feelings and seeking help from others. Early detection of depression in the elderly within rural communities is crucial for promoting a positive mental health lifestyle among this population. The community is rural and retains the traditions and culture of the Javanese people, but it also harbors a stigma surrounding depression. Rural areas in Indonesia are often far from health facilities. The relationship between insurance and occupation and depression affects the elderly as they prepare for old age with adequate financial resources, including retirement savings, to ensure financial stability. Seniors can prepare for old age by calculating their retirement fund needs, saving, investing, and obtaining insurance for pension and health fund protection.
Conclusion
Only two factors affect depression: insurance and occupation. However, the disparity in the number of respondents across each sociodemographic group made the results of this study less representative. As a result, further research on the factors that contribute to depression is necessary. Seniors can prepare for old age by calculating their retirement fund needs, saving, investing, and obtaining insurance for pension and health fund protection.
Ethical Considerations
Compliance with ethical guidelines
This paper was ethically approved by the Health Research Ethics Committee, Faculty of Nursing and Health Science, Universitas Muhammadiyah Semarang (Code: 0140/KEPK/VII/2023). Respondents were informed about the study and invited to participate. Each participant received a study instrument that included a questionnaire and signed informed consent.
Funding
This study was financially supported by the Universitas Muhammadiyah Semarang (Grant No.: 326/UNIMUS/2023).
Authors' contributions
Conceptualization and data analysis: Tri Nurhidayati and Satriya Pranata; Methodology: Tri Nurhidayati, Desy Ariyana Rahayu and Anna Kurnia and Lalu Muhammad Irham; Data collection and writing the original draft: Tri Nurhidayati; Investigation, review and editing: Satriya Pranata; Funding administration: Tri Nurhidayati, Desy Ariyana Rahayu and Anna Kurnia; Supervision: Ah Yusuf and Retno Indarwati.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants and Universitas Muhammadiyah Semarang for grant support in this research.
References
- Handajani YS, Schröder-Butterfill E, Hogervorst E, Turana Y, Hengky A. Depression among older adults in indonesia: prevalence, role of chronic conditions and other associated factors. Clinical Practice and Epidemiology in Mental Health. 2022; 18:e174501792207010. [DOI:10.2174/17450179-v18-e2207010] [PMID] [PMCID]
- Djamhari, E; Ramdlaningrum, H;Layyinah, A; Prasetya D. Research Report on the welfare conditions of the elderly and social protection of the elderly in Indonesia. Jakarta: Prakarsa; 2020. [Link]
- Huda N, Shaw MK, Chang HJ, Erwin, Putri ST, Pranata S. The mediating role of coping styles in the relationship between fear of COVID-19 and mental health problems: A cross-sectional study among nurses. BMC Public Health. 2024; 24(1):545. [DOI:10.1186/s12889-024-17863-w] [PMID] [PMCID]
- World Health Organization (WHO). Ageing and health. Website [Internet]. 2022 [Updated 2022 October 1]. Available from: [Link]
- Daher-Nashif S, Hammad SH, Kane T, Al-Wattary N. Islam and mental disorders of the older adults: Religious text, belief system and caregiving practices. Journal of Religion and Health. 2021; 60(3):2051-65. [DOI:10.1007/s10943-020-01094-5] [PMID] [PMCID]
- Zenebe Y, Akele B, W/Selassie M, Necho M. Prevalence and determinants of depression among old age: A systematic review and meta-analysis. Annals of General Psychiatry. 2021; 20(1):55. [DOI:10.1186/s12991-021-00375-x] [PMID] [PMCID]
- Amir SN, Juliana N, Azmani S, Abu IF, Talib AHQA, Abdullah F, et al. Impact of religious activities on quality of life and cognitive function among elderly. Journal of Religion and Health. 2022; 61(2):1564-84. [DOI:10.1007/s10943-021-01408-1] [PMID] [PMCID]
- Iinuma T, Arai Y, Takayama M, Takayama M, Abe Y, Osawa Y, et al. Satisfaction with dietary life affects oral health-related quality of life and subjective well-being in very elderly people. Journal of Oral Science. 2017; 59(2):207-13. [DOI:10.2334/josnusd.16-0414] [PMID]
- Fadila M, Argarini D, Widiastuti S. Factors related to quality of life among elderly during COVID-19 pandemic. International Journal of Nursing and Health Services. 2022; 5(1):45-55. [DOI:10.35654/ijnhs.v5i1.567]
- Sultana N, Nguyen TTP, Hossain A, Asaduzzaman M, Nguyen MH, Jahan I, et al. Psychometric properties of the short-form geriatric depression scale (GDS-SF) and its associated factors among the elderly in Bangladesh. International Journal of Environmental Research and Public Health. 2022; 19(13):7935. [DOI:10.3390/ijerph19137935] [PMID] [PMCID]
- Lueckenotte AG. Gerontologic nursing. Philadelphia: Mosby; 2000. [Link]
- Hidayat J, Chen MY, Pranata S. The effect of yoga on reducing stress and improving CD4 counts among people with HIV: A systematic review and meta-analysis. Jurnal Keperawatan Soedirman. 2023; 18(2):101-10. [DOI:10.20884/1.jks.2023.18.2.7331]
- Huda N, Nurchayati S, Pranata S, Sansuwito T. Religion and spirituality in coping with cancer among muslims: A literature review. The Malaysian Journal of Nursing. 2022; 14(2):151-6. [DOI:10.31674/mjn.2022.v14i02.025]
- Sayin Kasar K, Karaman E. Life in lockdown: Social isolation, loneliness and quality of life in the elderly during the COVID-19 pandemic: A scoping review. Geriatric Nursing. 2021; 42(5):1222-9. [DOI:10.1016/j.gerinurse.2021.03.010] [PMID] [PMCID]
- Heidari T, Mousavi SM, Mousavinasab SN, AzimiLolaty H. Effect of family and patient centered empowerment program on depression, anxiety and stress in patients with obsessive-compulsive disorder and their caregivers' burden. Iranian Journal of Nursing and Midwifery Research. 2020; 25(6):482-9. [DOI:10.4103/ijnmr.IJNMR_161_19] [PMID] [PMCID]
- Prasetiawan MJ, Mulyadi DE, Aliftitah S. Understanding the rights and obligations of BPJS health participants at the ganding community health center, sumenep. Journal of Health Science. 2019; 4(2):25-7. [DOI:10.24929/jik.v4i2.708]
- Otieno P, Angeles G, Quiñones S, van Halsema V, Novignon J, Palermo T, et al. Health services availability and readiness moderate cash transfer impacts on health insurance enrolment: Evidence from the LEAP 1000 cash transfer program in Ghana. BMC Health Services Research. 2022; 22(1):599. [DOI:10.1186/s12913-022-07964-w] [PMID] [PMCID]
- Wu YT, Kralj C, Acosta D, Guerra M, Huang Y, Jotheeswaran AT, et al. The association between, depression, anxiety, and mortality in older people across eight low- and middle-income countries: Results from the 10/66 cohort study. International Journal of Geriatric Psychiatry. 2020; 35(1):29-36. [DOI:10.1002/gps.5211] [PMID] [PMCID]
- Hollister B, Crabb R, Kaplan S, Brandner M, Areán P. Effectiveness of case management with problem-solving therapy for rural older adults with depression. The American Journal of Geriatric Psychiatry. 2022; 30(10):1083-92. [DOI:10.1016/j.jagp.2022.03.001] [PMID]
- Tallutondok EB, Hsieh CJ, Shih YL, Pranata S. Sexual harassment prevention program for Indonesian nursing aides: A mixed-methods study. International Journal of Public Health Science. 2023; 12(1):252-60. [DOI:10.11591/ijphs.v12i1.21988]
- Pranata S, Harriami DR, Kurnia A, Wulandari H, Seprian D, Bistara DN. Sociological public perception of the coronavirus disease 2019 situation in Indonesia: A phenomenological study. Iranian Journal of Psychiatry and Clinical Psychology. 2022; 28(1):9. [Link]
- Sutapa P, Pratama KW, Mustapha A. The relationship between the level of physical fitness and the level of depression in elderly age based on gender and marital status. Retos. 2024; 53:36-44. [DOI:10.47197/retos.v53.102488]
- Cong L, Dou P, Chen D, Cai L. Depression and associated factors in the elderly cadres in Fuzhou, China: A community-based study. International Journal of Gerontology. 2015; 9(1):29-33. [DOI:10.1016/j.ijge.2015.02.001]
- Perez-Sousa MA, Olivares PR, Gonzalez-Guerrero JL, Gusi N. Effects of an exercise program linked to primary care on depression in elderly: Fitness as mediator of the improvement. Quality of Life Research. 2020; 29(5):1239-46. [DOI:10.1007/s11136-019-02406-3] [PMID]
- Luo M, Ding D, Bauman A, Negin J, Phongsavan P. Social engagement pattern, health behaviors and subjective well-being of older adults: An international perspective using WHO-SAGE survey data. BMC Public Health. 2020; 20(1):99. [DOI:10.1186/s12889-019-7841-7] [PMID] [PMCID]
Type of Study: Short Communication |
Subject:
● Psychosocial Health
Received: 2024/02/25 | Accepted: 2024/04/21 | Published: 2024/09/1
Received: 2024/02/25 | Accepted: 2024/04/21 | Published: 2024/09/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






