Volume 15, Issue 2 (March & April 2025)
J Research Health 2025, 15(2): 165-174 |
Back to browse issues page
Ethics code: 313/KE/11/2023
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pranata S, Keysha N. The Use of Electronic Information Technology on Self-management Among Diabetes Patients: A Qualitative Study. J Research Health 2025; 15 (2) :165-174
URL: http://jrh.gmu.ac.ir/article-1-2532-en.html
URL: http://jrh.gmu.ac.ir/article-1-2532-en.html
1- Department of Nursing, Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Indonesia.
2- Department of Nursing, Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Indonesia. ,keyshanayandra@gmail.com
2- Department of Nursing, Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Indonesia. ,
Full-Text [PDF 564 kb]
(495 Downloads)
| Abstract (HTML) (2986 Views)
Full-Text: (856 Views)
Introduction
Diabetes is currently one of the chronic diseases that Indonesians are most concerned about. Indonesia is ranked fifth, with approximately 19.5 million people suffering from diabetes in 2021 [1]. Diabetes is a chronic metabolic disorder characterized by high blood sugar levels due to insufficient insulin function [2, 3].
According to the International Diabetes Federation (IDF), 537 million adults worldwide aged 20-79 years suffer from diabetes, and this number is expected to increase to 643 million (one in nine elderly) by 2030 and 784 million (one in eight elderly) by 2045 [1]. The estimated number of people with diabetes in Central Java Province in 2021 was 618,546 people, and 91.5% had received health services according to standards. There are 11 districts/cities with a percentage of health services for people with diabetes greater than 100%, while the district/city with the lowest achievement is Pemalang [4].
To improve the self-management of diabetic patients, the government has five pillars: Education, nutrition, diet, physical exercise and pharmacology [5, 6]. Diabetes self-management has been developed to improve the quality of life of diabetic patients, one of which is self-management [7–9]. These efforts still focus on the patient’s perspective; however, self-management can help patients with diabetes at hospital discharge. Utilizing current electronic information technology (EIT) is one of the many ways to teach self-management [10–12]. One example is the development of EIT at an urban university hospital in Japan, Tokyo University Hospital, which treats patients with diabetes older than 20 years. The results showed that 16% of patients used information and communication technology (ICT)-based self-management tools, which made it easier and more effective for healthcare providers to disseminate such tools to patients [11].
Studies have shown that EIT can increase hospital productivity [11]. Android-based electronic information technologies can be developed, including diabetes care applications [13–15]. This application can be used as a reference for controlling blood glucose levels during type 2 diabetes treatment to reduce complications caused by uncontrolled blood glucose levels [16–18]. This indicates that there have been many studies and that EIT has become a trend in hospitals and various countries. However, many hospitals have not yet developed EIT as a key technology in the delivery of improved quality of care to diabetes patients. Before implementing EIT in Indonesia, there may be a need to change policymakers’ views on EIT for diabetes patients to find gaps and solutions [19]. This research is crucial for addressing the issues that occur in Indonesia, specifically regarding diabetes control programs that exist in various health facilities but have not been fully optimized. Thus, the purpose of this study was to explore perspectives on improving diabetes self-management using EIT at hospitals in Semarang, Indonesia, by conducting in-depth interviews.
Methods
Study design
This qualitative research used a phenomenological approach.
Sample and location
The participants in this study were 15 policymakers at hospitals in Semarang City, including the general director, head of nursing, head of management information system (SIM), head of hospital health promotion, nurses, specialist doctors, pharmacists, and dieticians. The inclusion criterion was heads of the health sector and nurses with a work experience of at least five years. The samples were selected using purposive sampling. The method used for qualitative analysis was inductive. This research was conducted at Roemani Semarang Hospital. The in-depth interviews lasted approximately 20 minutes.
Data collection
This research was conducted from November 2023 to February 2024 at hospitals in Semarang. During data collection, the researcher began by identifying the location for the interviews. Each interview lasted approximately 20 minutes, and the information was gathered through both recording and note-taking. Before conducting the in-depth interviews, the researcher met with the participants in the designated room and provided informed consent forms, which were then signed by the participants to indicate their agreement to participate in the interviews. The researcher prepared interview aids and then conducted in-depth interviews with participants using the following questions) What do you think about the patient’s perspective on the use of Android-based technology to improve the self-management of diabetic patients?; 2) What do you think about the use of Android-based technology to improve the self-management of diabetic patients, and what percentage of the recovery rate do you believe diabetic patients achieve?; 3) Is there EIT in this hospital that can improve the self-management of diabetic patients?; 4) Do you think EIT in this hospital can improve the self-management of diabetic patients?; 5) Is the use of EIT in this hospital effective for diabetic patients to improve self-management?; 6) Are there any impacts or complications for diabetic patients regarding the use of EIT in this hospital? If so, please mention and explain.; 7) Why do you think EIT has not been able to be implemented in this hospital? The interview was conducted to explore participants’ perspectives on efforts to improve self-management of diabetic patients using EIT. The interview activity concluded after all required information had been completely obtained.
Data analysis
Data analysis in this phenomenological research used the Collaizzi method, which aims to describe the meaning of an experience identified through the important themes of a phenomenon consisting of seven stages [20]: 1) Re-reading all interview data and field notes repeatedly to get a full understanding of what is contained in the interview results, without adding personal assumptions from the researcher; 2) The researcher reviewed the data and made a list of specific and significant questions about the phenomena presented by each participant; 3) The researcher articulated the meaning of each specific and significant question by selecting keywords; 4) The researcher grouped the keywords into categories and themes and also reviewed the original data to validate the groupings and noted the differences between the various groups to avoid the possibility of incompatible data or themes; 5) The researcher integrated the results into a description based on the themes that have been compiled; 6) The researcher formulated a complete description of the phenomenon under study in the form of clear statements and a basic structure; 7) The researcher validated the findings of the themes with the participants to ensure alignment with the circumstances experienced by them.
In qualitative research, saturated data are obtained when the data collected are sufficient to draw the necessary conclusions, and further data collection will not yield additional valuable insights. Data analysis in this study was manual. The interviewer was confident that the opinions expressed were authentic because they fully understood the content and what data were needed to address the questions posed to the researcher. Informed consent was provided to the researcher to ensure that no information was added or omitted. The information obtained was analyzed using open coding.
Rigor of study
The researcher obtained data through interviews with credentialed policymakers at the hospital. The participants consisted of both men and women. The participants included both men and women, with general occupations such as managing director, head of nursing, specialist, doctor, dietician, administrator, and pharmacist. They were researchers who have conducted many studies published in many journals. The participants were not related to each other. After an explanation from the researcher, the participants understood that the purpose of the study was to explore policymakers’ perspectives on EIT and self-management among diabetic patients. A potential bias in this study is that the interviewer believes the opinions expressed are authentic because they fully understand the content and what data is needed to address the questions posed to the researcher. The methodology used in this study was phenomenology, and the sampling method was purposive sampling which involved face-to-face interviews with a total of 15 participants. None of the participants refused to participate; however, some preferred not to be recorded and requested that their responses be noted by hand instead.
The data were collected at the hospital, with important characteristics of the participants being assessed through demographic data, including age, gender and education. During the data collection process, there was no one present other than the researcher and the intended participants. The questions, instructions and guidelines provided by the researcher did not require testing; instead, repeated interviews were conducted 14 times. After identifying similarities with previous interviews, the researcher would stop the interviews to avoid wasting data in the future. This data collection utilized audio recordings and field notes made during interviews, which lasted approximately 20 minutes. In qualitative research, saturated data were obtained when the collected data were sufficient to draw necessary conclusions and further data collection will not yield additional valuable insights. Transcripts were returned to the researcher and corrected by the researcher to ensure no information was added or subtracted. In this study, three codes were obtained, which included themes, sub-themes and example quotes. The themes formed were derived from descriptions based on participant quotes, and the data was processed manually. Participants were asked to confirm that what they described reflected their own findings.
The themes were derived from the sub-themes, which were short descriptions derived from the participants’ quotes. The researcher ensured that the data were consistent with the findings. Major themes were clearly presented in the findings, and four themes and minor themes derived from the descriptions of participant quotes were found.
Results
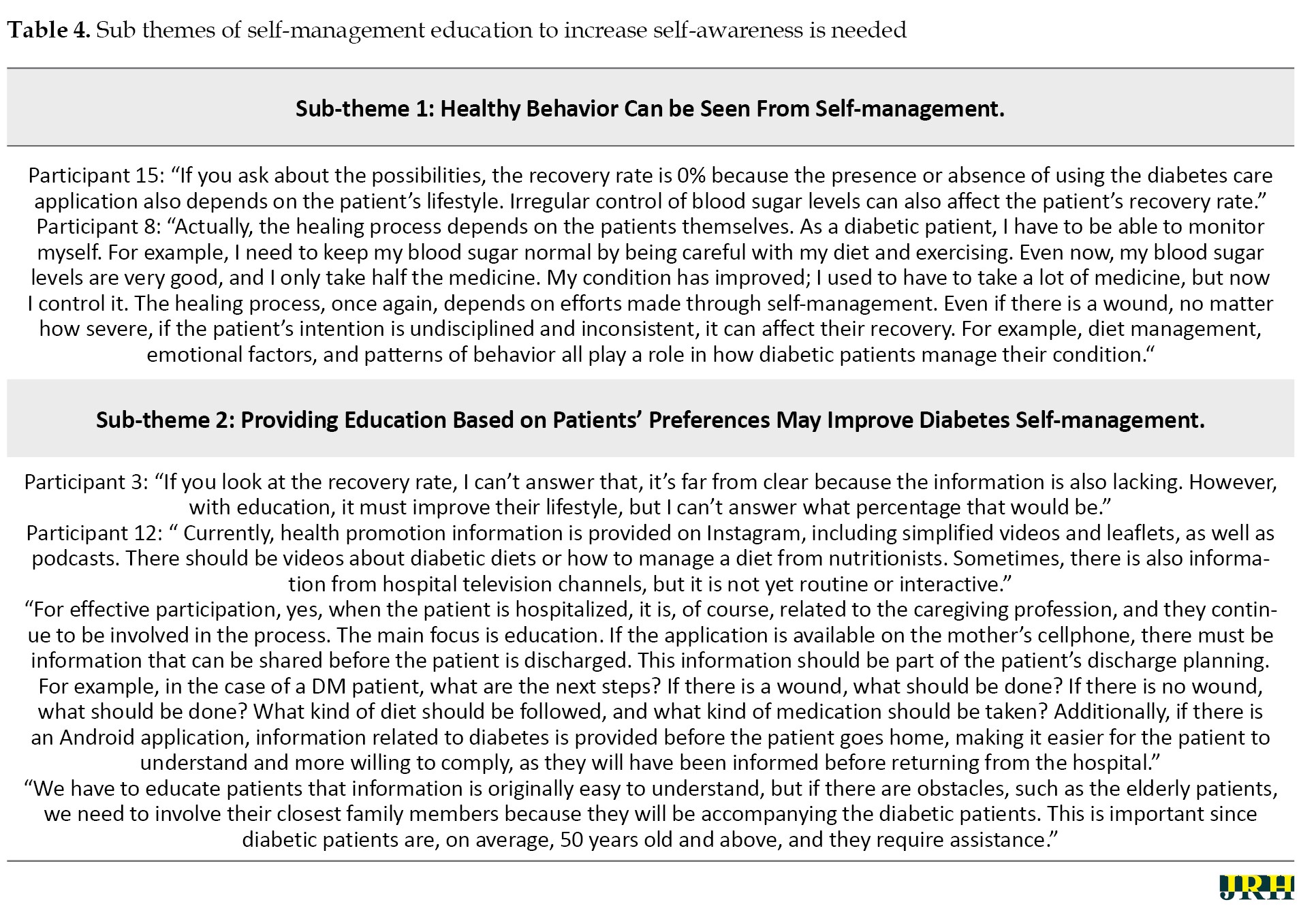
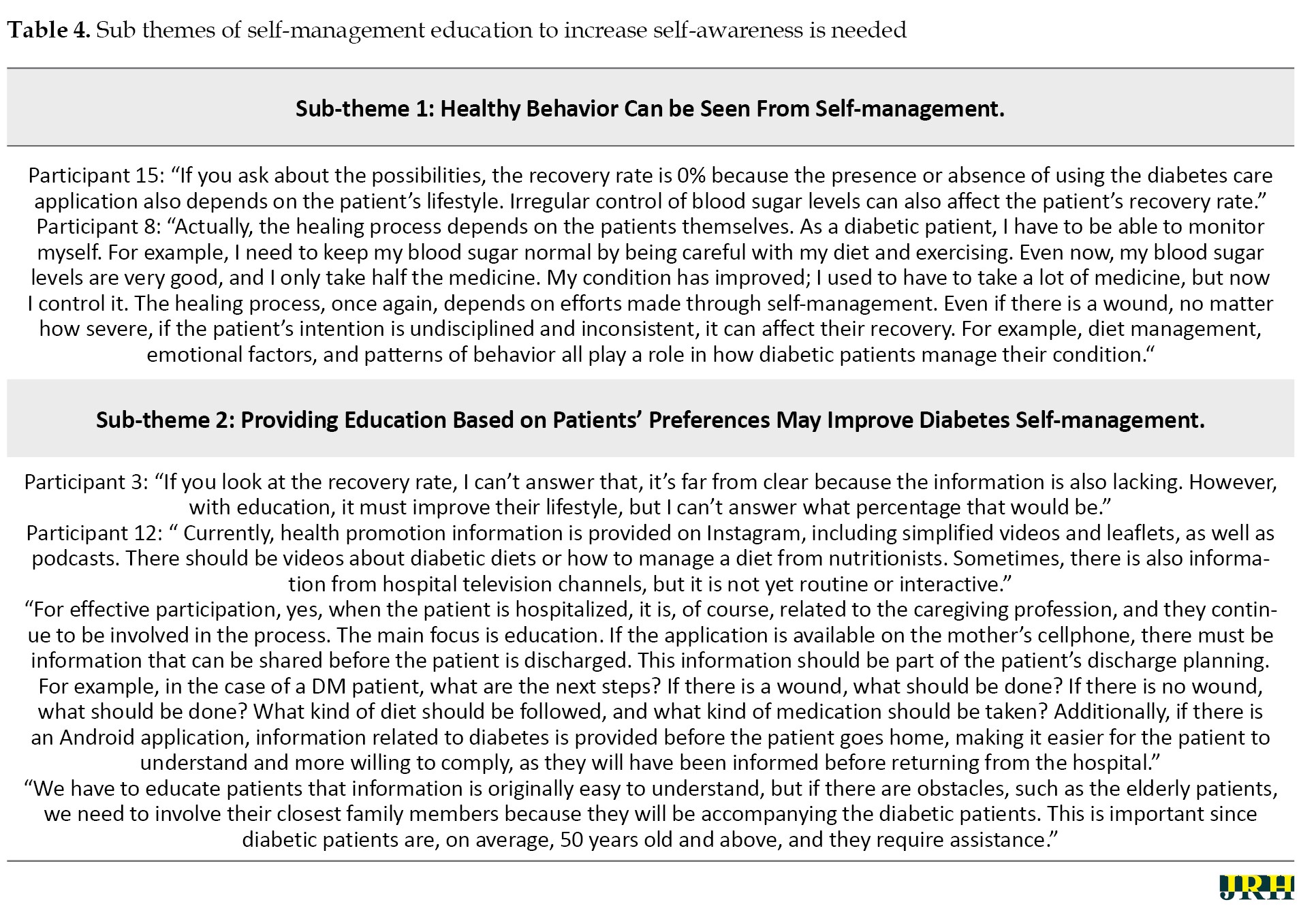
The participants in this study were heads of the health sector and nurses with a work experience of five years with an average age of 25 years and over. Characteristic of respondents presented in Table 1, further sub-theme of each theme presented in Tables 2, 3 and 4.



Understanding of the use of media to improve self-management through health information
The researcher identified the theme: Information through existing media is not effective.
Reasons for using EIT at hospitals for diabetic patients
Researchers identified a theme: The pros and cons of digital technology in hospitals. Patient understanding in recovery and the importance of providing education to diabetic patients. The researchers identified a theme: Self-management education to increase self-awareness is needed.
Discussion
Diabetic patients can obtain additional information through applications that provide monitoring and education. However, information obtained through social media is not recommended at several hospitals, as the primary source of information for patient education is video content from hospitals. Although there are no special media for diabetic patients, a need for the development of information tailored to the needs of diabetic patients in the hospital. Research supports the use of ICT in healthcare, but there is no research that demonstrates it is necessary. In Europe, only 14% of type 2 diabetes patients who used the web app consented to the study, while the rest did not consent due to lack of access to the Internet [21–23]. Therefore, it is essential to determine who is willing to use such tools for effective and low-cost diabetes management [24–27].
The use of technology in healthcare has both positive and negative impacts. Based on the results of this study, on the positive side, technology can improve the efficiency and accessibility of information. The effectiveness of digital technology is also evident in enhancing the self-management skills of diabetic patients, particularly in controlling their nutrition and diet. On the negative side, various constraints, including limited human resources, finances, and technological readiness, are obstacles to realizing the implementation of technology in hospitals in Semarang. There is supporting research on patients' willingness to use ICT in diabetes self-control [28–30]. With the rapid advancement of ICT, the use of the Internet and mobile devices is expected to help diabetes management. By enabling real-time and remote monitoring of data, such as blood glucose levels at home, these technologies can address time and location challenges. However, some patients are not willing to use ICT-based self-management tools for several reasons, including feelings of burden, satisfaction with their current management activities, perceptions of difficulty in using the tools, boredom, lack of time, beliefs about ineffectiveness and concerns that their health condition is too poor to utilize them [31, 32].
Self-management efforts play an important role for patients in managing their condition. Involving social media as a tool to provide health education can be a fairly effective strategy, allowing patients to get more extensive and in-depth information. In diabetes self-management efforts, self-readiness and family support also play an important role [33, 34]. The presence of family as a source of support can provide motivation and practical assistance for patients, strengthening their ability to manage their diabetes more effectively. In Japan, only 36% of hospitalized diabetic patients were able to maintain improved hemoglobin (HbA1c) levels for two years, suggesting that self-management education and family support are essential for diabetic patients [5, 35, 36]. One way that nurses can assist diabetic clients in gaining knowledge and skills for diabetes self-management to prevent long-term complications is by providing health education [10, 37]. Understanding the importance of self-understanding is crucial for diabetes patients, especially in terms of maintaining a regular schedule, type, and amount of food, particularly for those taking blood glucose-lowering drugs or insulin. The extent, to which patients are self-aware and able to perform self-care aimed at controlling their symptoms and preventing complications is key to successful diabetes treatment. Self-awareness is important for people with diabetes to improve adherence to dietary management, physical activity, consumption of anti-diabetic medications, and the prevention of disease complications.
Conclusion
Several hospitals have not recommended the use of EIT for diabetic patients, even though there is some video content from hospital health promotion that does not fully meet the needs of diabetes patients. While digital technology can improve collaboration between health workers and patients, its effectiveness may be reduced for those less familiar with technology. Constraints, such as human resources, finances, and technology readiness can hinder the implementation of technology in hospitals. Education is recognized as key to improving patient understanding, especially in the context of diabetes self-management among the elderly. Social media can be a fairly effective strategy f for providing broader and deeper education. Family support and self-readiness also play an important role in motivating and assisting patients in managing their diabetes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Universitas Muhammadiyah Semarang, Semarang, Indonesia (Code: 313/KE/11/2023; dated December 11, 2023). Furthermore, during the study, the participants were in contact with the researcher by phone to solve possible problems and answer questions. To comply with ethical principles, participants were well-informed about the research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and writing: All authors; Methodology, investigation, and resources: Nayandra Keysha; Validation, formal analysis, data curation and supervision: Satriya Pranata.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their gratitude to all participants in this study.
References
Diabetes is currently one of the chronic diseases that Indonesians are most concerned about. Indonesia is ranked fifth, with approximately 19.5 million people suffering from diabetes in 2021 [1]. Diabetes is a chronic metabolic disorder characterized by high blood sugar levels due to insufficient insulin function [2, 3].
According to the International Diabetes Federation (IDF), 537 million adults worldwide aged 20-79 years suffer from diabetes, and this number is expected to increase to 643 million (one in nine elderly) by 2030 and 784 million (one in eight elderly) by 2045 [1]. The estimated number of people with diabetes in Central Java Province in 2021 was 618,546 people, and 91.5% had received health services according to standards. There are 11 districts/cities with a percentage of health services for people with diabetes greater than 100%, while the district/city with the lowest achievement is Pemalang [4].
To improve the self-management of diabetic patients, the government has five pillars: Education, nutrition, diet, physical exercise and pharmacology [5, 6]. Diabetes self-management has been developed to improve the quality of life of diabetic patients, one of which is self-management [7–9]. These efforts still focus on the patient’s perspective; however, self-management can help patients with diabetes at hospital discharge. Utilizing current electronic information technology (EIT) is one of the many ways to teach self-management [10–12]. One example is the development of EIT at an urban university hospital in Japan, Tokyo University Hospital, which treats patients with diabetes older than 20 years. The results showed that 16% of patients used information and communication technology (ICT)-based self-management tools, which made it easier and more effective for healthcare providers to disseminate such tools to patients [11].
Studies have shown that EIT can increase hospital productivity [11]. Android-based electronic information technologies can be developed, including diabetes care applications [13–15]. This application can be used as a reference for controlling blood glucose levels during type 2 diabetes treatment to reduce complications caused by uncontrolled blood glucose levels [16–18]. This indicates that there have been many studies and that EIT has become a trend in hospitals and various countries. However, many hospitals have not yet developed EIT as a key technology in the delivery of improved quality of care to diabetes patients. Before implementing EIT in Indonesia, there may be a need to change policymakers’ views on EIT for diabetes patients to find gaps and solutions [19]. This research is crucial for addressing the issues that occur in Indonesia, specifically regarding diabetes control programs that exist in various health facilities but have not been fully optimized. Thus, the purpose of this study was to explore perspectives on improving diabetes self-management using EIT at hospitals in Semarang, Indonesia, by conducting in-depth interviews.
Methods
Study design
This qualitative research used a phenomenological approach.
Sample and location
The participants in this study were 15 policymakers at hospitals in Semarang City, including the general director, head of nursing, head of management information system (SIM), head of hospital health promotion, nurses, specialist doctors, pharmacists, and dieticians. The inclusion criterion was heads of the health sector and nurses with a work experience of at least five years. The samples were selected using purposive sampling. The method used for qualitative analysis was inductive. This research was conducted at Roemani Semarang Hospital. The in-depth interviews lasted approximately 20 minutes.
Data collection
This research was conducted from November 2023 to February 2024 at hospitals in Semarang. During data collection, the researcher began by identifying the location for the interviews. Each interview lasted approximately 20 minutes, and the information was gathered through both recording and note-taking. Before conducting the in-depth interviews, the researcher met with the participants in the designated room and provided informed consent forms, which were then signed by the participants to indicate their agreement to participate in the interviews. The researcher prepared interview aids and then conducted in-depth interviews with participants using the following questions) What do you think about the patient’s perspective on the use of Android-based technology to improve the self-management of diabetic patients?; 2) What do you think about the use of Android-based technology to improve the self-management of diabetic patients, and what percentage of the recovery rate do you believe diabetic patients achieve?; 3) Is there EIT in this hospital that can improve the self-management of diabetic patients?; 4) Do you think EIT in this hospital can improve the self-management of diabetic patients?; 5) Is the use of EIT in this hospital effective for diabetic patients to improve self-management?; 6) Are there any impacts or complications for diabetic patients regarding the use of EIT in this hospital? If so, please mention and explain.; 7) Why do you think EIT has not been able to be implemented in this hospital? The interview was conducted to explore participants’ perspectives on efforts to improve self-management of diabetic patients using EIT. The interview activity concluded after all required information had been completely obtained.
Data analysis
Data analysis in this phenomenological research used the Collaizzi method, which aims to describe the meaning of an experience identified through the important themes of a phenomenon consisting of seven stages [20]: 1) Re-reading all interview data and field notes repeatedly to get a full understanding of what is contained in the interview results, without adding personal assumptions from the researcher; 2) The researcher reviewed the data and made a list of specific and significant questions about the phenomena presented by each participant; 3) The researcher articulated the meaning of each specific and significant question by selecting keywords; 4) The researcher grouped the keywords into categories and themes and also reviewed the original data to validate the groupings and noted the differences between the various groups to avoid the possibility of incompatible data or themes; 5) The researcher integrated the results into a description based on the themes that have been compiled; 6) The researcher formulated a complete description of the phenomenon under study in the form of clear statements and a basic structure; 7) The researcher validated the findings of the themes with the participants to ensure alignment with the circumstances experienced by them.
In qualitative research, saturated data are obtained when the data collected are sufficient to draw the necessary conclusions, and further data collection will not yield additional valuable insights. Data analysis in this study was manual. The interviewer was confident that the opinions expressed were authentic because they fully understood the content and what data were needed to address the questions posed to the researcher. Informed consent was provided to the researcher to ensure that no information was added or omitted. The information obtained was analyzed using open coding.
Rigor of study
The researcher obtained data through interviews with credentialed policymakers at the hospital. The participants consisted of both men and women. The participants included both men and women, with general occupations such as managing director, head of nursing, specialist, doctor, dietician, administrator, and pharmacist. They were researchers who have conducted many studies published in many journals. The participants were not related to each other. After an explanation from the researcher, the participants understood that the purpose of the study was to explore policymakers’ perspectives on EIT and self-management among diabetic patients. A potential bias in this study is that the interviewer believes the opinions expressed are authentic because they fully understand the content and what data is needed to address the questions posed to the researcher. The methodology used in this study was phenomenology, and the sampling method was purposive sampling which involved face-to-face interviews with a total of 15 participants. None of the participants refused to participate; however, some preferred not to be recorded and requested that their responses be noted by hand instead.
The data were collected at the hospital, with important characteristics of the participants being assessed through demographic data, including age, gender and education. During the data collection process, there was no one present other than the researcher and the intended participants. The questions, instructions and guidelines provided by the researcher did not require testing; instead, repeated interviews were conducted 14 times. After identifying similarities with previous interviews, the researcher would stop the interviews to avoid wasting data in the future. This data collection utilized audio recordings and field notes made during interviews, which lasted approximately 20 minutes. In qualitative research, saturated data were obtained when the collected data were sufficient to draw necessary conclusions and further data collection will not yield additional valuable insights. Transcripts were returned to the researcher and corrected by the researcher to ensure no information was added or subtracted. In this study, three codes were obtained, which included themes, sub-themes and example quotes. The themes formed were derived from descriptions based on participant quotes, and the data was processed manually. Participants were asked to confirm that what they described reflected their own findings.
The themes were derived from the sub-themes, which were short descriptions derived from the participants’ quotes. The researcher ensured that the data were consistent with the findings. Major themes were clearly presented in the findings, and four themes and minor themes derived from the descriptions of participant quotes were found.
Results
The participants in this study were heads of the health sector and nurses with a work experience of five years with an average age of 25 years and over. Characteristic of respondents presented in Table 1, further sub-theme of each theme presented in Tables 2, 3 and 4.



Understanding of the use of media to improve self-management through health information
The researcher identified the theme: Information through existing media is not effective.
Reasons for using EIT at hospitals for diabetic patients
Researchers identified a theme: The pros and cons of digital technology in hospitals. Patient understanding in recovery and the importance of providing education to diabetic patients. The researchers identified a theme: Self-management education to increase self-awareness is needed.
Discussion
Diabetic patients can obtain additional information through applications that provide monitoring and education. However, information obtained through social media is not recommended at several hospitals, as the primary source of information for patient education is video content from hospitals. Although there are no special media for diabetic patients, a need for the development of information tailored to the needs of diabetic patients in the hospital. Research supports the use of ICT in healthcare, but there is no research that demonstrates it is necessary. In Europe, only 14% of type 2 diabetes patients who used the web app consented to the study, while the rest did not consent due to lack of access to the Internet [21–23]. Therefore, it is essential to determine who is willing to use such tools for effective and low-cost diabetes management [24–27].
The use of technology in healthcare has both positive and negative impacts. Based on the results of this study, on the positive side, technology can improve the efficiency and accessibility of information. The effectiveness of digital technology is also evident in enhancing the self-management skills of diabetic patients, particularly in controlling their nutrition and diet. On the negative side, various constraints, including limited human resources, finances, and technological readiness, are obstacles to realizing the implementation of technology in hospitals in Semarang. There is supporting research on patients' willingness to use ICT in diabetes self-control [28–30]. With the rapid advancement of ICT, the use of the Internet and mobile devices is expected to help diabetes management. By enabling real-time and remote monitoring of data, such as blood glucose levels at home, these technologies can address time and location challenges. However, some patients are not willing to use ICT-based self-management tools for several reasons, including feelings of burden, satisfaction with their current management activities, perceptions of difficulty in using the tools, boredom, lack of time, beliefs about ineffectiveness and concerns that their health condition is too poor to utilize them [31, 32].
Self-management efforts play an important role for patients in managing their condition. Involving social media as a tool to provide health education can be a fairly effective strategy, allowing patients to get more extensive and in-depth information. In diabetes self-management efforts, self-readiness and family support also play an important role [33, 34]. The presence of family as a source of support can provide motivation and practical assistance for patients, strengthening their ability to manage their diabetes more effectively. In Japan, only 36% of hospitalized diabetic patients were able to maintain improved hemoglobin (HbA1c) levels for two years, suggesting that self-management education and family support are essential for diabetic patients [5, 35, 36]. One way that nurses can assist diabetic clients in gaining knowledge and skills for diabetes self-management to prevent long-term complications is by providing health education [10, 37]. Understanding the importance of self-understanding is crucial for diabetes patients, especially in terms of maintaining a regular schedule, type, and amount of food, particularly for those taking blood glucose-lowering drugs or insulin. The extent, to which patients are self-aware and able to perform self-care aimed at controlling their symptoms and preventing complications is key to successful diabetes treatment. Self-awareness is important for people with diabetes to improve adherence to dietary management, physical activity, consumption of anti-diabetic medications, and the prevention of disease complications.
Conclusion
Several hospitals have not recommended the use of EIT for diabetic patients, even though there is some video content from hospital health promotion that does not fully meet the needs of diabetes patients. While digital technology can improve collaboration between health workers and patients, its effectiveness may be reduced for those less familiar with technology. Constraints, such as human resources, finances, and technology readiness can hinder the implementation of technology in hospitals. Education is recognized as key to improving patient understanding, especially in the context of diabetes self-management among the elderly. Social media can be a fairly effective strategy f for providing broader and deeper education. Family support and self-readiness also play an important role in motivating and assisting patients in managing their diabetes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Universitas Muhammadiyah Semarang, Semarang, Indonesia (Code: 313/KE/11/2023; dated December 11, 2023). Furthermore, during the study, the participants were in contact with the researcher by phone to solve possible problems and answer questions. To comply with ethical principles, participants were well-informed about the research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and writing: All authors; Methodology, investigation, and resources: Nayandra Keysha; Validation, formal analysis, data curation and supervision: Satriya Pranata.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their gratitude to all participants in this study.
References
- IDF. International diabetes federation diabetes atlas 2021. Brussels: IDF; 2021. [Link]
- Hassan S, Gujral UP, Quarells RC, Rhodes EC, Shah MK, Obi J, et al. Disparities in diabetes prevalence and management by race and ethnicity in the USA: Defining a path forward. The lancet. Diabetes & Endocrinology. 2023; 11(7):509-24. [DOI:10.1016/S2213-8587(23)00129-8] [PMID]
- Kposowa AJ, Aly Ezzat D, Breault K. Diabetes mellitus and marital status: Evidence from the national longitudinal mortality study on the effect of marital dissolution and the death of a spouse. International Journal of General Medicine. 2021; 14:1881-8. [DOI:10.2147/IJGM.S307436] [PMID]
- Database Peraturan. Pedoman Nasional pelayanan kedokteran tata laksana stunting [Internet]. 2022 [Updated 2022 November 23]. Available from: [Link]
- Pranata S, Wu S V, Wang T T, Liang S, Chuang Y, Lu K et al. Effectiveness of tailored care intervention program on biochemical outcomes of patients with diabetes in Indonesia: A Randomized Controlled Trial. Journal of Client-Centered Nursing Care. 2023; 9(2):123-34. [DOI:10.32598/JCCNC.9.2.428.1]
- Alam AS, Samiasih A, Mubin MF, Pranata S, Dhamanik R. Types of nursing intervention on improving quality of life among patients with diabetes mellitus: A systematic review. Current Diabetes Reviews. 2024; 20(3):e290823220467. [DOI:10.2174/1573399820666230829103016] [PMID]
- Pranata S, Wu SV, Alizargar J, Liu JH, Liang SY, Lu YY. Precision health care elements, definitions, and strategies for patients with diabetes: A literature review. International Journal of Environmental Research and Public Health. 2021; 18(12):6535. [DOI:10.3390/ijerph18126535] [PMID]
- Pranata S. Self-management experience of patient with diabetes mellitus type 2. International Journal of Psychosocial Rehabilitation. 2021; 24(4):7792-801. [Link]
- Pranata S. Pilot study: Self-management among diabetes mellitus patients at HL. Manambai Abdulkadir. Jurnal Ilmiah Keperawatan. 2019; 5(2):107-13. [DOI:10.33023/jikep.v5i2.258]
- Zwane J, Modjadji P, Madiba S, Moropeng L, Mokgalaboni K, Mphekgwana PM, et al. Self-management of diabetes and associated factors among patients seeking chronic care in Tshwane, South Africa: A facility-based study. International Journal of Environmental Research and Public Health. 2023; 20(10):5887. [DOI:10.3390/ijerph20105887] [PMID]
- Kawai Y, Waki K, Yamaguchi S, Shibuta T, Miyake K, Kimura S, et al. The use of information and communication technology-based self-management system dialbeticslite in treating abdominal obesity in Japanese office workers: Prospective single-arm pilot intervention study. JMIR Diabetes. 2022; 7(4):e40366. [DOI:10.2196/40366] [PMID]
- Samal L, Fu HN, Camara DS, Wang J, Bierman AS, Dorr DA. Health information technology to improve care for people with multiple chronic conditions. Health Services Research. 2021; 56(Suppl 1):1006-36. [DOI:10.1111/1475-6773.13860] [PMID]
- Prihatin Putri DM, Suhoyo Y, Putri Pertiwi AA, Effendy C. Integrated diabetes self-management (IDSM) mobile application to improve self-management and glycemic control among patients with type 2 diabetes mellitus (T2DM) in Indonesia: A mixed methods study protocol. Plos One. 2022; 17(11):e0277127. [DOI:10.1371/journal.pone.0277127] [PMID]
- Sesaria TG, Kusnanto K, Bakar A. Mobile smartphone intervention for managing glycaemia control in the patients with diabetes mellitus: A systematic review. Nurse and Health. 2020; 9(2):70-9. [DOI:10.36720/nhjk.v9i2.164]
- Jeon E, Park HA, Jo S, et al. Mobile apps providing tailored nursing interventions for patients with metabolic syndrome. Studies in Health Technology and Informatics. 2016; 225:510-4. [DOI:10.3233/978-1-61499-658-3-510]
- Otu AA, Effa EE, Onwusaka O, Omoyele C, Arakelyan S, Okuzu O, et al. mHealth guideline training for non-communicable diseases in primary care facilities in Nigeria: A mixed methods pilot study. BMJ Open. 2022; 12(8):e060304. [DOI:10.1136/bmjopen-2021-060304] [PMID]
- Fraiwan L, Ninan J, Al-Khodari M. Mobile application for ulcer detection. The Open Biomedical Engineering Journal. 2018; 12:16-26. [DOI:10.2174/1874120701812010016] [PMID]
- Lim S, Kang SM, Kim KM, Moon JH, Choi SH, Hwang H, et al. Multifactorial intervention in diabetes care using real-time monitoring and tailored feedback in type 2 diabetes. Acta Diabetologica. 2016; 53(2):189-98. [DOI:10.1007/s00592-015-0754-8] [PMID]
- Pranata S, Vivienne Wu S, Armiyati Y, Khoiriyah K, Shing L C, Liu J. Implementing precision health care program at hospitals in Indonesia. Journal of Research and Health. 2023; 13(6):457-66 [DOI:10.32598/JRH.13.6.2183.3]
- Polit DF, Beck CT. Essentials of nursing research:Appraising evidence for nursing practice (8th ed.). Philadelphia: Lippincott Williams & Wilkins; 2014. [Link]
- Guo SH, Lin JL, Hsing HC, Lee CC, Chuang SM. The effect of mobile ehealth education to improve knowledge, skills, self-care, and mobile ehealth literacies among patients with diabetes: Development and evaluation study. Journal of Medical Internet Research. 2023; 25:e42497. [DOI:10.2196/42497] [PMID]
- Farooq MS, Riaz S, Tehseen R, Farooq U, Saleem K. Role of internet of things in diabetes healthcare: Network infrastructure, taxonomy, challenges, and security model. Digital Health. 2023; 9:20552076231179056. [DOI:10.1177/20552076231179056] [PMID]
- Deshpande N, Wu M, Kelly C, Woodrick N, Werner DA, Volerman A, et al. Video-based educational interventions for patients with chronic illnesses: Systematic review. Journal of Medical Internet Research. 2023; 25:e41092. [DOI:10.2196/41092] [PMID]
- Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Hess Fischl A, et al. Diabetes self-management education and support in type 2 diabetes: A joint position statement of the American Diabetes Association, the American Association of diabetes educators, and the academy of nutrition and dietetics. Diabetes Care. 2015; 38(7):1372-82. [DOI:10.2337/dc15-0730] [PMID]
- Sherifali D. Diabetes coaching for individuals with type 2 diabetes: A state-of-the-science review and rationale for a coaching model. Journal of Diabetes. 2017; 9(6):547-54. [DOI:10.1111/1753-0407.12528] [PMID]
- Almohanna AA, Win KT, Meedya S. Effectiveness of internet-based electronic technology interventions on breastfeeding outcomes: Systematic review. Journal of Medical Internet Research. 2020; 22(5):e17361. [DOI:10.2196/17361] [PMID]
- Zhao X, Huang H, Zheng S. Effectiveness of internet and phone-based interventions on diabetes management of children and adolescents with type 1 diabetes: A systematic review. Worldviews on Evidence-Based Nursing. 2021; 18(3):217-25. [DOI:10.1111/wvn.12511] [PMID]
- de Sequeira S, Halperin I, Lipscombe LL. Culturally tailored resources for South Asian immigrant women with gestational diabetes: Do they work and what's missing? A qualitative study. Canadian Journal of Diabetes. 2019; 43(8):573-9. [DOI:10.1016/j.jcjd.2019.09.007] [PMID]
- Arnett DK, Claas SA. Precision medicine, genomics, and public health. Diabetes Care. 2016; 39(11):1870-3. [DOI:10.2337/dc16-1763] [PMID]
- Holmen H, Wahl AK, Cvancarova Småstuen M, Ribu L. Tailored communication within mobile apps for diabetes self-management: A systematic review. Journal of Medical Internet Research. 2017; 19(6):e227. [DOI:10.2196/jmir.7045] [PMID]
- Shibuta T, Waki K, Tomizawa N, Igarashi A, Yamamoto-Mitani N, Yamaguchi S, et al. Willingness of patients with diabetes to use an ICT-based self-management tool: A cross-sectional study. BMJ Open Diabetes Research & Care. 2017; 5(1):e000322. [DOI:10.1136/bmjdrc-2016-000322] [PMID]
- Kim J, Bae YH, Ho SH, Lee H, Park H. Feasibility and outcomes of a community-based, mobile health system-monitored lifestyle intervention in chronic stroke: A pilot study. Technology and Health Care. 2024; 32(4):2159-70. [DOI:10.3233/THC-230857] [PMID]
- Vas A, Devi ES, Vidyasagar S, Acharya R, Rau NR, George A, et al. Effectiveness of self-management programmes in diabetes management: A systematic review. International Journal of Nursing Practice. 2017; 23(5):1-8. [DOI:10.1111/ijn.12571] [PMID]
- Asmat K, Dhamani K, Froelicher ES, Gul R. A patient-centered self-management intervention to improve glycemic control, self-efficacy and self-care behaviors in adults with type 2 diabetes mellitus: A SPIRIT compliant study protocol for randomized controlled trial. Diabetes, Metabolic Syndrome and Obesity. 2023; 16:225-36. [DOI:10.2147/DMSO.S385715] [PMID]
- Pranata S, Shing LC, Vranada A, et al. The implementation of precision personalized care to improve diabetes patients ‘ self-management at taipei veteran general hospital: An observational study. Bali Medical Journal. 2021; 10(3):1304-7. [DOI:10.15562/bmj.v10i3.2902]
- Pranata S, Wu SF, Chu CH, Nugroho KH. Precision health care strategies for older adults with diabetes in Indonesia: A Delphi consensus study. Medical Journal of Indonesia. 2021; 30(3):221-7. [DOI:10.13181/mji.oa.215525]
- Rawat S, Yadav R, Goyal S, Nagpal J. Estimated risk of cardiovascular events and long-term complications: The projected future of diabetes patients in Delhi from the DEDICOM-II survey. Diabetes & Metabolic Syndrome. 2023; 17(11):102880. [DOI:10.1016/j.dsx.2023.102880] [PMID]
Type of Study: Orginal Article |
Subject:
● Service Quality
Received: 2024/04/14 | Accepted: 2024/08/31 | Published: 2025/03/2
Received: 2024/04/14 | Accepted: 2024/08/31 | Published: 2025/03/2
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |