Volume 14, Issue 6 (Nov & Dec 2024)
J Research Health 2024, 14(6): 547-554 |
Back to browse issues page
Ethics code: Not applicable
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Marku E, Miska X, Vyshka G. Impact of Stress Perception Among Nursing Students in Albania During the COVID-19 Pandemic. J Research Health 2024; 14 (6) :547-554
URL: http://jrh.gmu.ac.ir/article-1-2539-en.html
URL: http://jrh.gmu.ac.ir/article-1-2539-en.html
1- Department of Pre-clinical Subjects, Faculty of Technical Medical Sciences, University of Medicine, Tirana, Albania.
2- Ophthalmology Section, French Hospital, Mother Theresa Hospital Center, Tirana, Albania.
3- Department of Biomedical and Experimental, Faculty of Medicine, University of Medicine, Tirana, Albania. ,gvyshka@gmail.com
2- Ophthalmology Section, French Hospital, Mother Theresa Hospital Center, Tirana, Albania.
3- Department of Biomedical and Experimental, Faculty of Medicine, University of Medicine, Tirana, Albania. ,
Keywords: COVID-19, Perceived stress scale-4 (PSS-4), Cross-sectional cohort study, Survey methodology, Nursing students, Psychosocial impact
Full-Text [PDF 820 kb]
(714 Downloads)
| Abstract (HTML) (3660 Views)
Full-Text: (817 Views)
Introduction
The COVID-19 pandemic aggressively affected the world for two consecutive years, impacting our daily lives. Its outbreak, first discovered in Wuhan, China, in December 2019, evolved rapidly. On January 30, 2020, the Director-General of the World Health Organization (WHO) declared this situation a public health emergency of international concern, and on March 12, 2020, the COVID-19 outbreak was declared a pandemic [1]. COVID-19 affected a large number of people, with reports in around 200 countries and territories [2]. Significant mental and social consequences were observed not only in individuals who experienced symptoms or severe illness but across the general population. The negative effects on mental health due to social isolation have been particularly pronounced among the elderly, families, and adolescents—groups already at risk for depression or suicidal tendencies [3].
A study conducted in China during the initial outbreak of COVID-19 found that its impact on psychological states varied, with up to 53.8% of the population reporting psychological effects: 16.5% reported moderate to severe depression, 28.8% reported moderate to severe anxiety, and 8.1% reported moderate to severe stress [4]. Other studies using a narrative thematic approach have demonstrated that the COVID-19 pandemic initiated a multitude of perceived psychological stressors and poor social networks, highlighting socio-economic problems, including family structures and their role in children’s anxiety responses. All these factors are argued to have caused many physical and mental symptoms of distress and unease, including apprehension, anxiety, extreme fear, and insecurity [5, 6]. Another large cross-sectional study conducted among university students in Malaysia showed a significant increase in stress and anxiety during the COVID-19 lockdown. Anxiety and stress levels were more pronounced in females than males and were more present in the 17-18 years of age subgroup of students. This is likely due to the increased use of social media platforms among younger students that portrayed the pandemic as omnipresent and without an escape route in dealing with it [7, 8].
The continued spread of the novel coronavirus (COVID-19), strict isolation measures, and delays in the start of schools, colleges, and universities directly or indirectly influenced the mental health of students as reported in many international studies [9-11]. Despite the well-documented psychological impact of the COVID-19 pandemic that took the world by storm, no detailed study has been conducted in our country on university students and its broader implications. In this aspect, we aimed to demonstrate the perceived stress impact of the COVID-19 outbreak on nursing students at the Medical University of Tirana. This study may be helpful in advocating for better mental health care policies in universities across our country, as well as in focusing on future health care practitioners (nursing students) as a vulnerable group in terms of mental health. Their future profession is reported to be an additional independent risk factor for stress, anxiety, and depression as reported by many other studies [12-15]. We aimed to assess the need for psycho-emotional support for nursing students and suggest that other third parties implement potential therapeutic interventions.
Methods
This is a cross-sectional cohort study, using survey methodology. We relied on a large sample of students to identify the psycho-emotional and perceived stress impact during the period of the pandemic. We selected only the first-year nursing students in the academic year 2020-2021, during which teaching was implemented online. The same cohort was used in their second academic year, 2021-2022, upon their return to university for on-campus teaching.
Study population and sampling
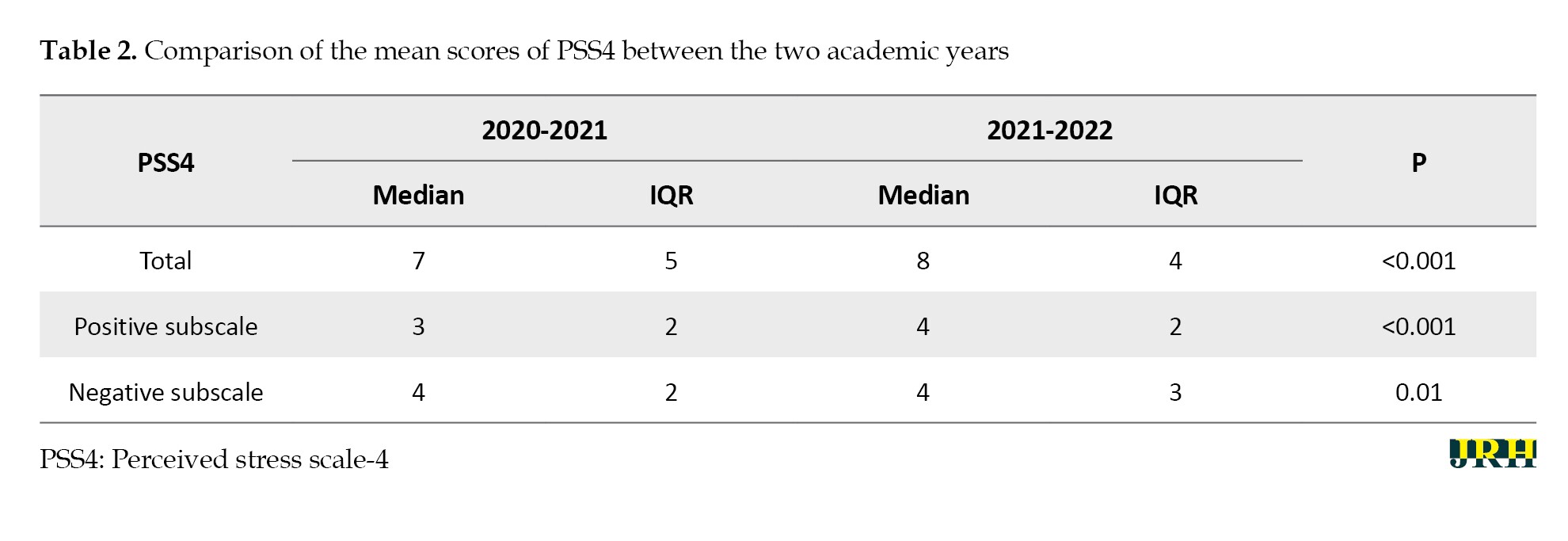
The target population was first-year bachelor nursing students at the Medical University of Tirana during the academic year 2020-2021, who underwent online teaching, as shown in Table 1.
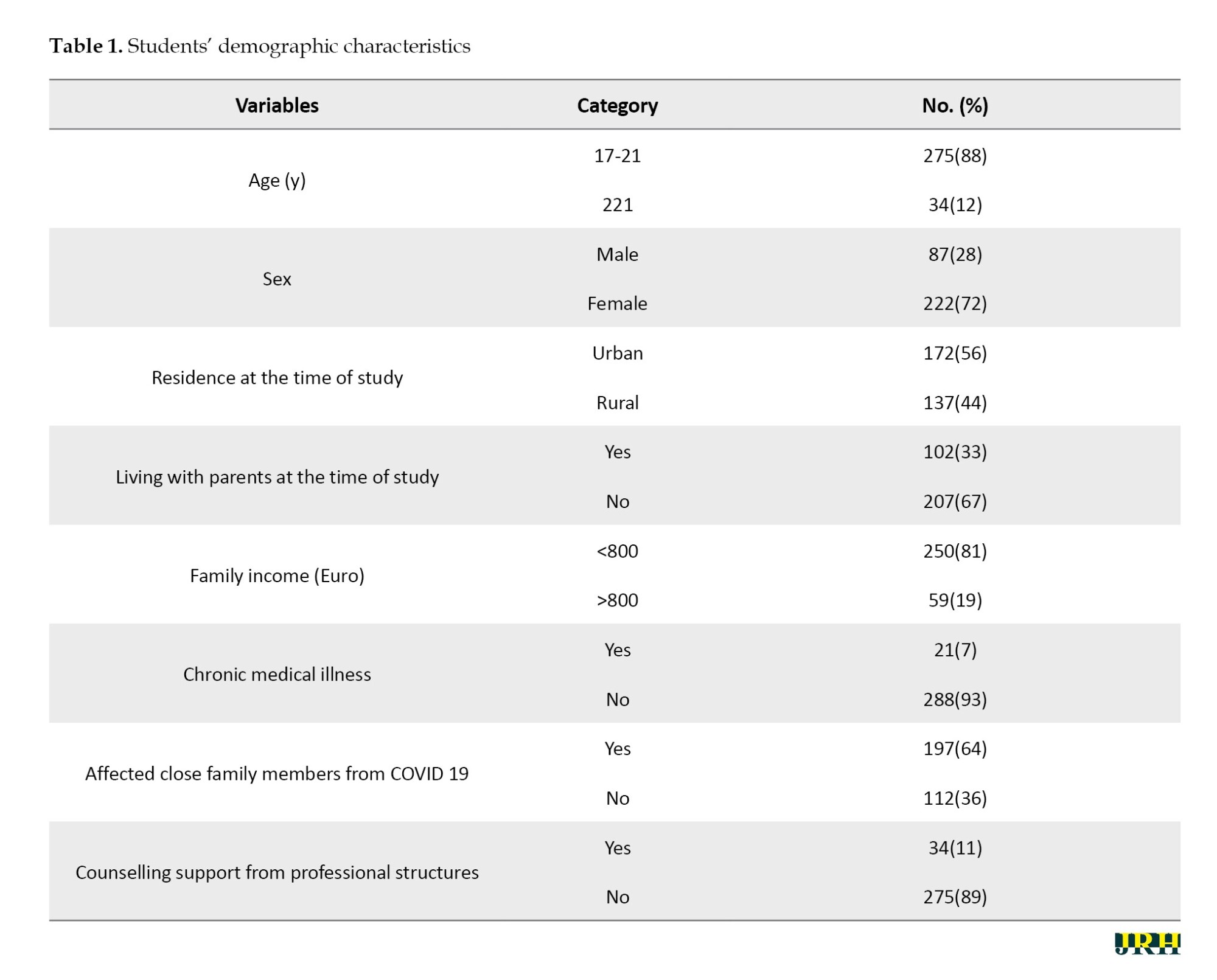
Students were selected using a random sampling technique. The number of students included in the first questionnaire was 309 out of 450 initially recruited, while in the second study, there were 299 participants from the same cohort, with ten having dropped out of the nursing course. The study was conducted from October to December of 2020 and during the same period in the following year, 2021.
Inclusion criteria
To be part of the study, the inclusion criteria were being a nursing student at the Medical University of Tirana, participating in the online university education system during the COVID-19 pandemic, and being a second-year student during the academic year 2021-2022.
Data collection
Data were collected from the questionnaire prepared for randomly selected students using the perceived stress scale-4 (PSS4) [12], via the Google Forms program, while maintaining anonymity. According to the scoring of the PSS-4, a short version of the PSS-10 proposed by Cohen et al. (1983), students rated their perceived stress level on a scale of 0-4 for four questions (a description of the test and the specific questions are provided at the end of the article). The questions in this scale inquire about feelings and thoughts during the last month, with students indicating their response by selecting the option that represents how often they felt or thought a certain way (never, almost never, sometimes; fairly often and very often) Scoring instructions were provided for each question.
Statistical analysis
Data were analyzed using SPSS software, version 25. The Shapiro-Wilk test was used to test the normality of distribution of the PSS4 scores and data were reported as the median and interquartile range (IQR). The Wilcoxon nonparametric test was used to compare the median of the scores of the overall scale and subscales between two academic years. The chi-square test was used to compare the proportion of students between the two academic years. A P≤0.05 was considered significant. All tests were two-tailed and translated into Albanian.
Results
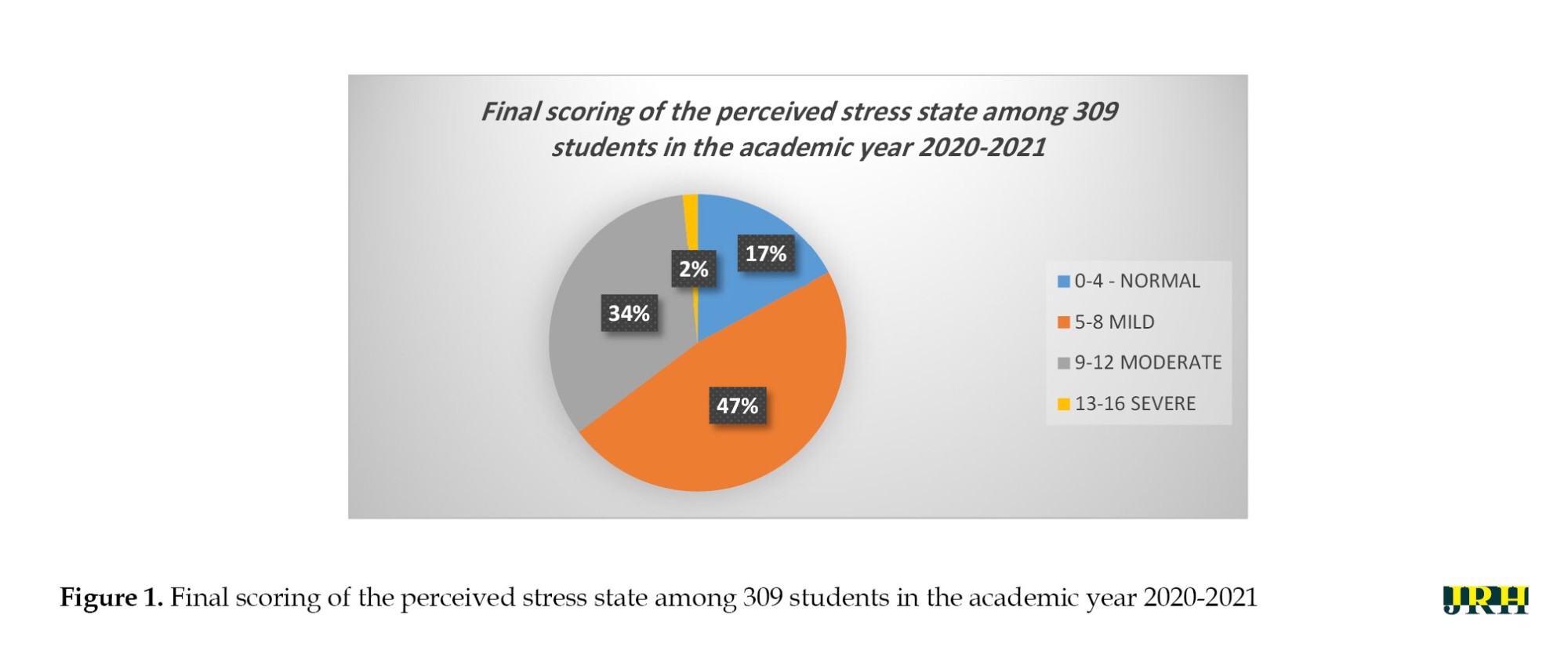
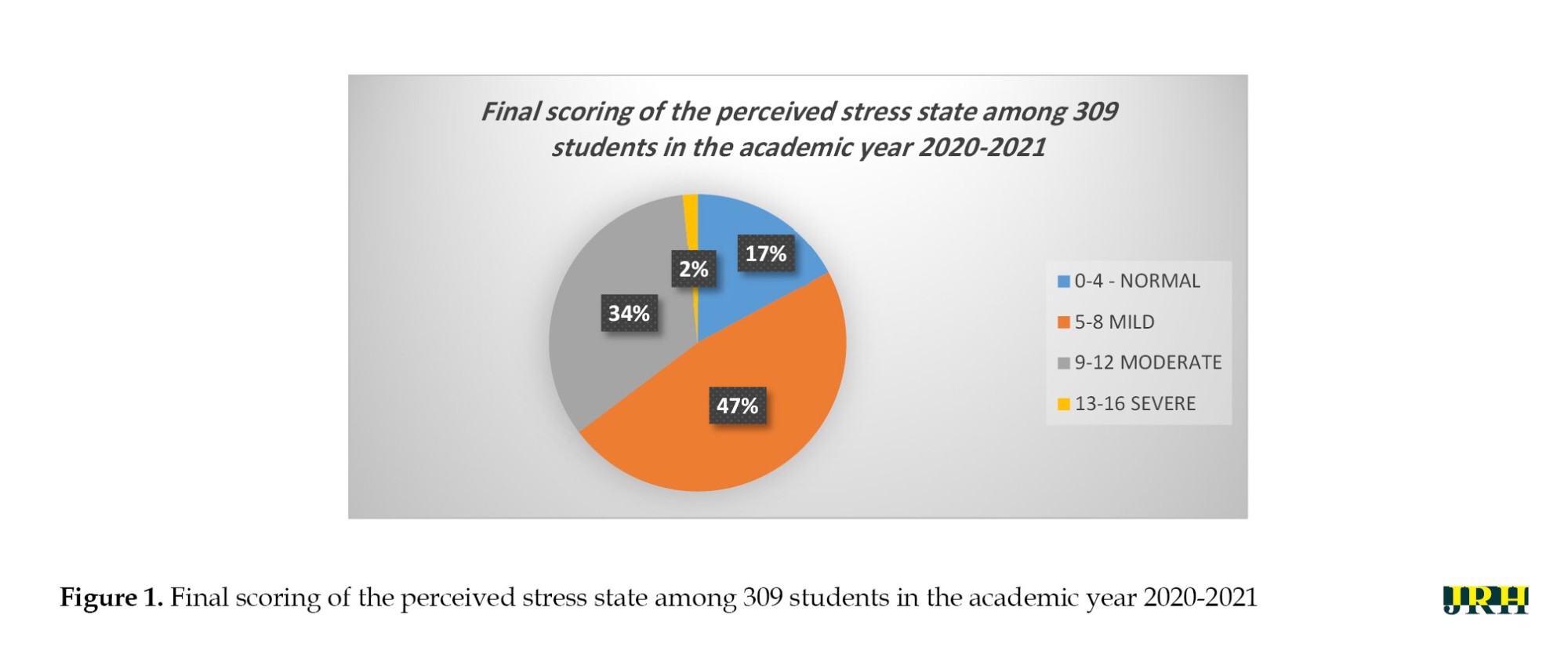
Out of the 450 students of the first academic year 2020-2021, only 309 were accepted to take the PSS-4 test. The final scoring of this group ranked their perceived emotional and stress state (Figure 1). The final scoring from 0-4 indicated that these students (17%) had no changes in their perceived stress; scores from 9-12 indicated a moderately elevated stress state among students (34%), and scores from 13-16 (the highest score) indicated that these students (2%) were in a severe emotional stress state.
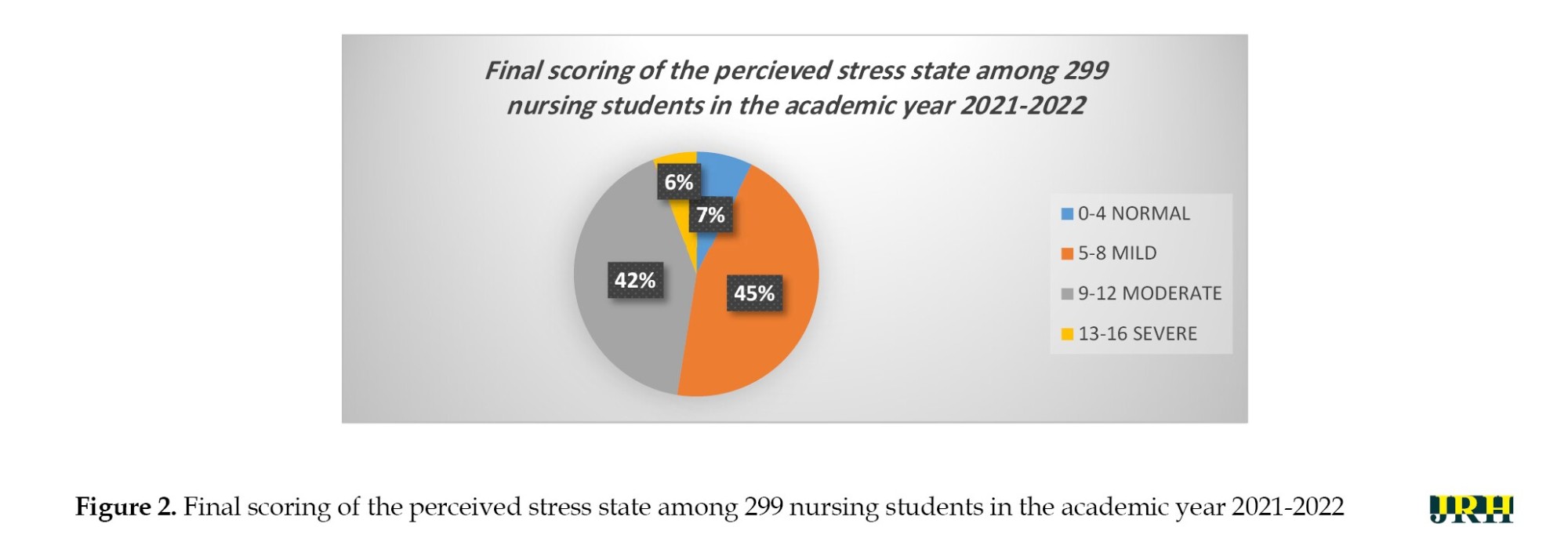
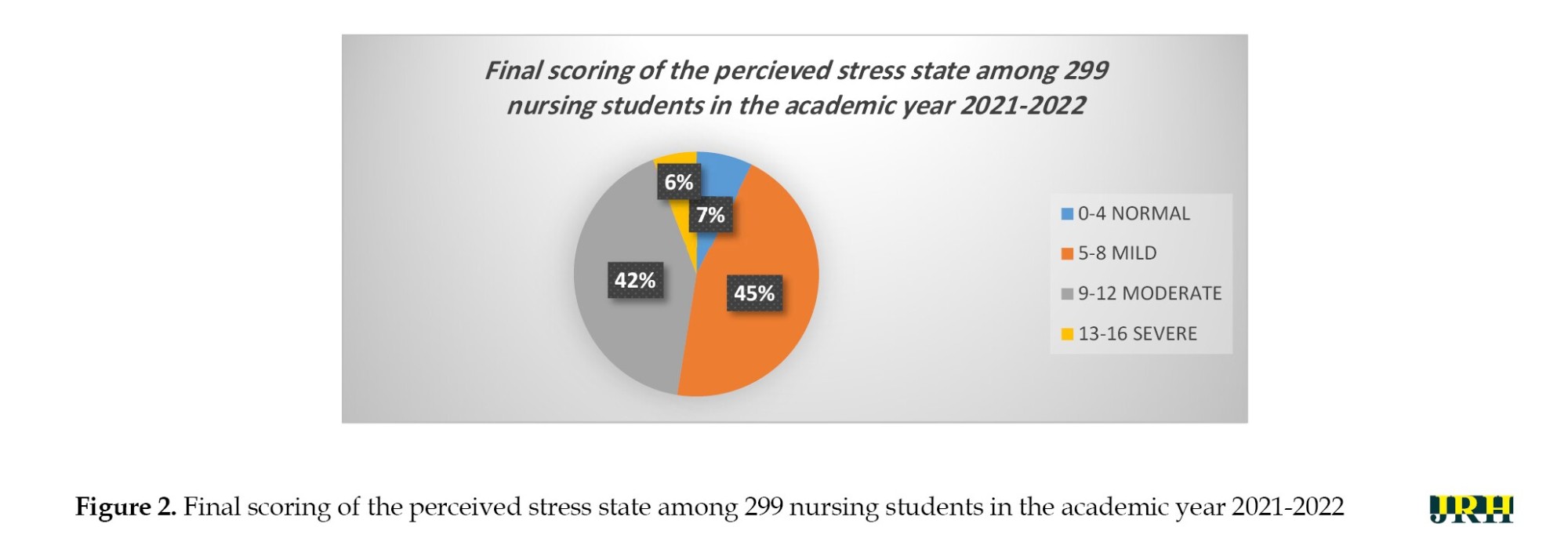
The same cohort of students, with a negligible change in numbers (299), took the PSS-4 test in the next academic year, 2021-2022, and the distribution of their final scoring results is shown in Figure 2. This time, 7% fell within the normal range according to their PSS-4 answers, 45% reported mild stress, 42% reported moderate levels of stress perception and 6% reported being under severe stress based on the results obtained.
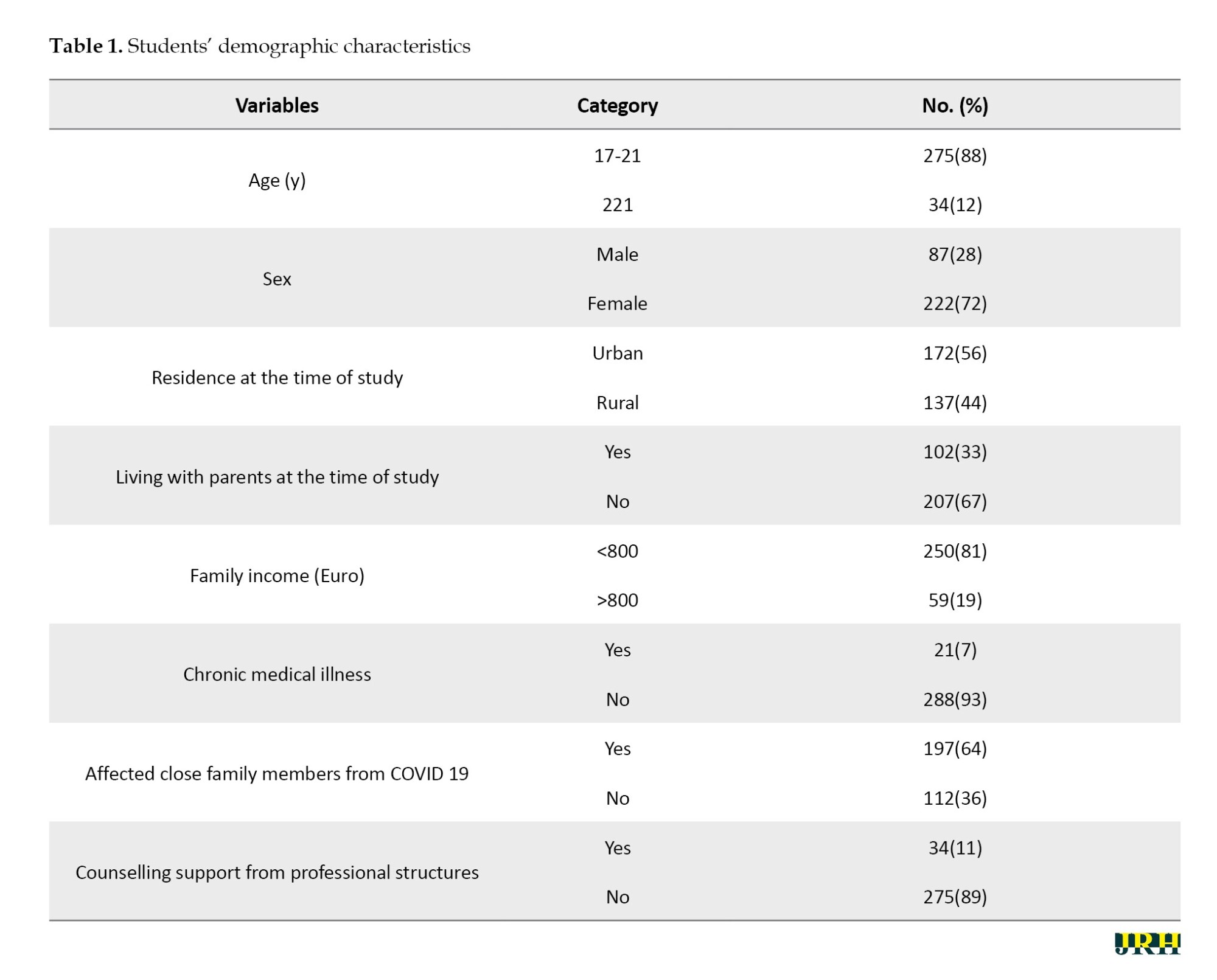
Overall the level of stress was significantly higher among students in the academic year 2021-2022, Me (IQR)=8.0 (4.0), compared to the academic year 2020-2021, Me (IQR)=7.0 (5.0) (P<0.001).
Also, the level of stress regarding the negative subscale was significantly higher among students in the academic year 2021-2022, Me (IQR)=4.0 (3.0), compared to the academic year 2020-2021, Me (IQR)=4.0 (3.0), (P=0.01; Table 2).
On the contrary, the level of stress regarding the positive subscale was significantly higher among students in the academic year 2020-2021, Me (IQR)=3.0 (2.0), compared to the academic year 2021-2022, Me (IQR)=4.0 (2.0) (P<0.001). Significantly more students in the academic year 2020-2021 had a normal level of stress (17.2%) compared to 8.4% of the students in the subsequent year (8.4%) (P<0.01). No significant difference was found regarding the mild (P=0.5) and moderate (P=0.06) levels of stress between the two academic years, although the difference was nearly significant for the moderate stress. A significantly higher number of students in the academic year 2021-2022 reported an increased level of stress compared to the previous academic year 2020-2021 (1.6%) (P<0.01).
Discussion
The COVID-19 pandemic affected the world aggressively for two consecutive years, impacting our daily lives. The aim of this study was to assess the stress levels of nursing students over two consecutive academic years during the COVID-19 pandemic and to address potential mental health issues that could arise from it. As reported by many studies, the mental health impact of the COVID-19 pandemic on university students, and specifically on nursing students, was clearly evident and of major concern [9-11, 15]. To our knowledge, no detailed study has been conducted in our country on the stress impact of university nursing students and its broader implications. Our study used a cross-sectional cohort methodology with a large sample size of nursing students and was carried out from September 2020 to June 2022. Significant data regarding the perceived stress state during the COVID-19 pandemic were retrieved from the study, showing a notable increase in stress levels concerning all the implicit factors that the pandemic introduced into students’ lives and their broader social environments. These results were in line with other similar studies performed in many other countries reporting an increase in mental health problems among college students, including nursing majors [18-22].
Overall, the results obtained from our cohort of nursing students showed an increased level of stress perception in the academic year 2021-2022 upon their return to normal on-campus teaching after a year of being mostly away due to online instruction as a direct result of the COVID-19 pandemic. We suggest that the major factor at play here is the social isolation that COVID-19 imposed on students, which resulted in a lack of normal social interactions and its implicit consequences on stress and mental health, as reported in other studies [22, 26]. In addition to online teaching and social isolation, there are a multitude of possible factors contributing to the elevated stress levels among the second-year nursing student cohort. One major reason, as reported in the literature, is the stress associated with the transition to college [24]. Being part of a young generation with a mean age of 18 years old, they were more prone to obtain information from social media outlets that were filled with negative news, conspiracy theories, and other disinformation [27-30]. Another factor that we believe has played a significant role in the nursing major, reflects a future profession that carries a substantial amount of stress and anxiety during public health crises, as reported in other studies, along with a tendency to consider dropping out of their nursing program [10]. However, other important factors are at play here, independent of COVID-19, that predispose this young generation to mental health problems, like burnout, depression, and anxiety, as demonstrated in many studies in this area. Some of these factors include childhood abuse and adversity; coming from rural areas and adjusting to urban dynamics; being female; and having lower family incomes [18, 19, 21]. We are confident that a combination of genetics, life experiences, and other environmental factors—such as family structures and socioeconomic background—contributes significantly as independent risk factors for experiencing stress, anxiety, depression, and other mental health problems, independent of the pandemic. The ramifications of these studies, including our study and others to come, should be the preparation of specific implementation strategies to address these problems. Numerous intervention models aimed at improving college students’ mental health have been proposed and will continue to be proposed in the future [31-34]. In this regard, various stakeholders must come together in order to assess the potential benefits of different approaches, keeping in mind that an integrated systems approach may be the most beneficial.
Conclusion
Based on the results of this paper and the relevant international literature, it is imperative to emphasize that students need immediate collaboration with the relevant faculty structures to help improve their psychoemotional state. For this purpose, we recommend the implementation of psychological counseling structures at the University of Medicine in Tirana, as well as specialized structures to address post-COVID stress and trauma issues among students. This should include identifying individuals and groups who are more prone to stress vulnerability while also considering other potential mental health conditions among students. In this regard, as part of stress management interventions, we propose the development of specific strategies involving highly trained professionals in order to promote healthy recreational habits and lifestyle modification patterns supported by the medical university.
This study is the first of its kind in Albania with limited resources, and more studies using different methods to assess stress and psychoemotional problems need to be performed in the future. We note that our study only provides a very general idea of the mental health problems that stress can induce among students, especially due to external factors that we cannot control, as was the case with the COVID-19 pandemic and its many consequences. We understand that the responses provided on the PSS-4 are too general and subjective, varying from student to student depending on their experiences and psychoemotional states, and also influenced by other unspecified external factors or underlying health conditions.
Ethical Considerations
Compliance with ethical guidelines
All participants agreed via respective emails to complete the Google Form questionnaire. All collected data were treated with full anonymity.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Data extraction: Ervin Marku and Xhesika Miska; Review and editing: Gentian Vyshka; Conceptualization, supervision and writing the original draft: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors extend sincere thanks to all students who volunteered to complete the questionnaires online.
References
The COVID-19 pandemic aggressively affected the world for two consecutive years, impacting our daily lives. Its outbreak, first discovered in Wuhan, China, in December 2019, evolved rapidly. On January 30, 2020, the Director-General of the World Health Organization (WHO) declared this situation a public health emergency of international concern, and on March 12, 2020, the COVID-19 outbreak was declared a pandemic [1]. COVID-19 affected a large number of people, with reports in around 200 countries and territories [2]. Significant mental and social consequences were observed not only in individuals who experienced symptoms or severe illness but across the general population. The negative effects on mental health due to social isolation have been particularly pronounced among the elderly, families, and adolescents—groups already at risk for depression or suicidal tendencies [3].
A study conducted in China during the initial outbreak of COVID-19 found that its impact on psychological states varied, with up to 53.8% of the population reporting psychological effects: 16.5% reported moderate to severe depression, 28.8% reported moderate to severe anxiety, and 8.1% reported moderate to severe stress [4]. Other studies using a narrative thematic approach have demonstrated that the COVID-19 pandemic initiated a multitude of perceived psychological stressors and poor social networks, highlighting socio-economic problems, including family structures and their role in children’s anxiety responses. All these factors are argued to have caused many physical and mental symptoms of distress and unease, including apprehension, anxiety, extreme fear, and insecurity [5, 6]. Another large cross-sectional study conducted among university students in Malaysia showed a significant increase in stress and anxiety during the COVID-19 lockdown. Anxiety and stress levels were more pronounced in females than males and were more present in the 17-18 years of age subgroup of students. This is likely due to the increased use of social media platforms among younger students that portrayed the pandemic as omnipresent and without an escape route in dealing with it [7, 8].
The continued spread of the novel coronavirus (COVID-19), strict isolation measures, and delays in the start of schools, colleges, and universities directly or indirectly influenced the mental health of students as reported in many international studies [9-11]. Despite the well-documented psychological impact of the COVID-19 pandemic that took the world by storm, no detailed study has been conducted in our country on university students and its broader implications. In this aspect, we aimed to demonstrate the perceived stress impact of the COVID-19 outbreak on nursing students at the Medical University of Tirana. This study may be helpful in advocating for better mental health care policies in universities across our country, as well as in focusing on future health care practitioners (nursing students) as a vulnerable group in terms of mental health. Their future profession is reported to be an additional independent risk factor for stress, anxiety, and depression as reported by many other studies [12-15]. We aimed to assess the need for psycho-emotional support for nursing students and suggest that other third parties implement potential therapeutic interventions.
Methods
This is a cross-sectional cohort study, using survey methodology. We relied on a large sample of students to identify the psycho-emotional and perceived stress impact during the period of the pandemic. We selected only the first-year nursing students in the academic year 2020-2021, during which teaching was implemented online. The same cohort was used in their second academic year, 2021-2022, upon their return to university for on-campus teaching.
Study population and sampling
The target population was first-year bachelor nursing students at the Medical University of Tirana during the academic year 2020-2021, who underwent online teaching, as shown in Table 1.
Students were selected using a random sampling technique. The number of students included in the first questionnaire was 309 out of 450 initially recruited, while in the second study, there were 299 participants from the same cohort, with ten having dropped out of the nursing course. The study was conducted from October to December of 2020 and during the same period in the following year, 2021.
Inclusion criteria
To be part of the study, the inclusion criteria were being a nursing student at the Medical University of Tirana, participating in the online university education system during the COVID-19 pandemic, and being a second-year student during the academic year 2021-2022.
Data collection
Data were collected from the questionnaire prepared for randomly selected students using the perceived stress scale-4 (PSS4) [12], via the Google Forms program, while maintaining anonymity. According to the scoring of the PSS-4, a short version of the PSS-10 proposed by Cohen et al. (1983), students rated their perceived stress level on a scale of 0-4 for four questions (a description of the test and the specific questions are provided at the end of the article). The questions in this scale inquire about feelings and thoughts during the last month, with students indicating their response by selecting the option that represents how often they felt or thought a certain way (never, almost never, sometimes; fairly often and very often) Scoring instructions were provided for each question.
Statistical analysis
Data were analyzed using SPSS software, version 25. The Shapiro-Wilk test was used to test the normality of distribution of the PSS4 scores and data were reported as the median and interquartile range (IQR). The Wilcoxon nonparametric test was used to compare the median of the scores of the overall scale and subscales between two academic years. The chi-square test was used to compare the proportion of students between the two academic years. A P≤0.05 was considered significant. All tests were two-tailed and translated into Albanian.
Results
Out of the 450 students of the first academic year 2020-2021, only 309 were accepted to take the PSS-4 test. The final scoring of this group ranked their perceived emotional and stress state (Figure 1). The final scoring from 0-4 indicated that these students (17%) had no changes in their perceived stress; scores from 9-12 indicated a moderately elevated stress state among students (34%), and scores from 13-16 (the highest score) indicated that these students (2%) were in a severe emotional stress state.
The same cohort of students, with a negligible change in numbers (299), took the PSS-4 test in the next academic year, 2021-2022, and the distribution of their final scoring results is shown in Figure 2. This time, 7% fell within the normal range according to their PSS-4 answers, 45% reported mild stress, 42% reported moderate levels of stress perception and 6% reported being under severe stress based on the results obtained.
Overall the level of stress was significantly higher among students in the academic year 2021-2022, Me (IQR)=8.0 (4.0), compared to the academic year 2020-2021, Me (IQR)=7.0 (5.0) (P<0.001).
Also, the level of stress regarding the negative subscale was significantly higher among students in the academic year 2021-2022, Me (IQR)=4.0 (3.0), compared to the academic year 2020-2021, Me (IQR)=4.0 (3.0), (P=0.01; Table 2).
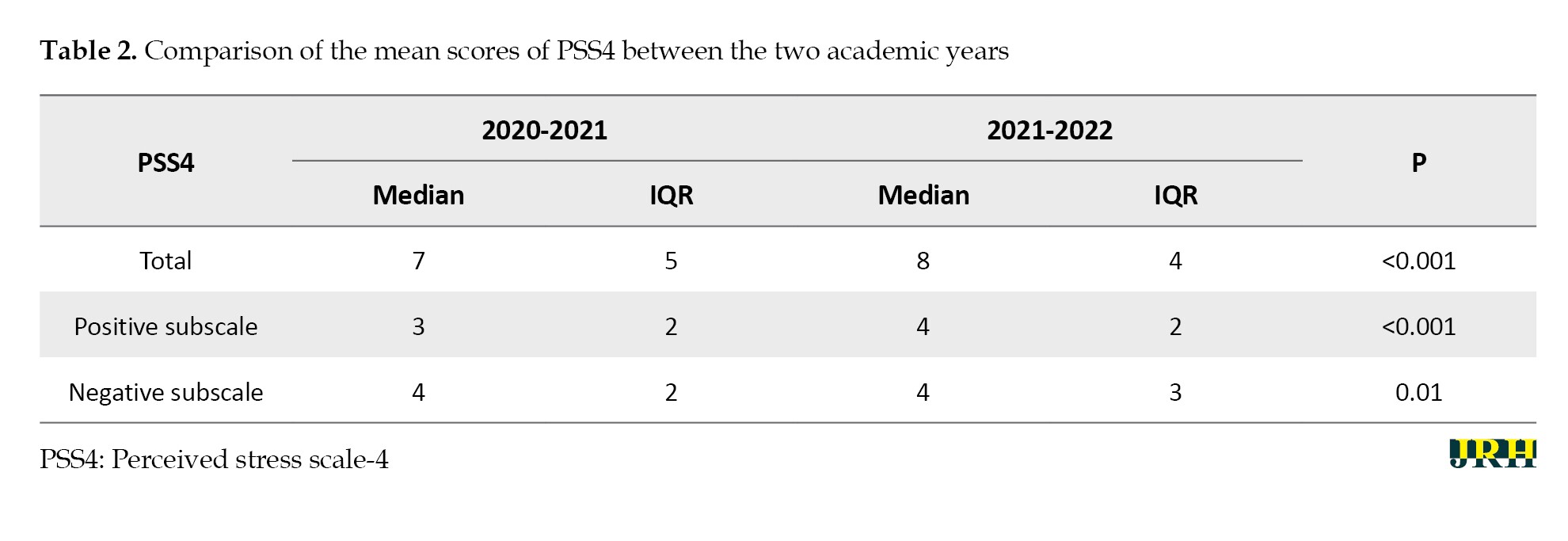
On the contrary, the level of stress regarding the positive subscale was significantly higher among students in the academic year 2020-2021, Me (IQR)=3.0 (2.0), compared to the academic year 2021-2022, Me (IQR)=4.0 (2.0) (P<0.001). Significantly more students in the academic year 2020-2021 had a normal level of stress (17.2%) compared to 8.4% of the students in the subsequent year (8.4%) (P<0.01). No significant difference was found regarding the mild (P=0.5) and moderate (P=0.06) levels of stress between the two academic years, although the difference was nearly significant for the moderate stress. A significantly higher number of students in the academic year 2021-2022 reported an increased level of stress compared to the previous academic year 2020-2021 (1.6%) (P<0.01).
Discussion
The COVID-19 pandemic affected the world aggressively for two consecutive years, impacting our daily lives. The aim of this study was to assess the stress levels of nursing students over two consecutive academic years during the COVID-19 pandemic and to address potential mental health issues that could arise from it. As reported by many studies, the mental health impact of the COVID-19 pandemic on university students, and specifically on nursing students, was clearly evident and of major concern [9-11, 15]. To our knowledge, no detailed study has been conducted in our country on the stress impact of university nursing students and its broader implications. Our study used a cross-sectional cohort methodology with a large sample size of nursing students and was carried out from September 2020 to June 2022. Significant data regarding the perceived stress state during the COVID-19 pandemic were retrieved from the study, showing a notable increase in stress levels concerning all the implicit factors that the pandemic introduced into students’ lives and their broader social environments. These results were in line with other similar studies performed in many other countries reporting an increase in mental health problems among college students, including nursing majors [18-22].
Overall, the results obtained from our cohort of nursing students showed an increased level of stress perception in the academic year 2021-2022 upon their return to normal on-campus teaching after a year of being mostly away due to online instruction as a direct result of the COVID-19 pandemic. We suggest that the major factor at play here is the social isolation that COVID-19 imposed on students, which resulted in a lack of normal social interactions and its implicit consequences on stress and mental health, as reported in other studies [22, 26]. In addition to online teaching and social isolation, there are a multitude of possible factors contributing to the elevated stress levels among the second-year nursing student cohort. One major reason, as reported in the literature, is the stress associated with the transition to college [24]. Being part of a young generation with a mean age of 18 years old, they were more prone to obtain information from social media outlets that were filled with negative news, conspiracy theories, and other disinformation [27-30]. Another factor that we believe has played a significant role in the nursing major, reflects a future profession that carries a substantial amount of stress and anxiety during public health crises, as reported in other studies, along with a tendency to consider dropping out of their nursing program [10]. However, other important factors are at play here, independent of COVID-19, that predispose this young generation to mental health problems, like burnout, depression, and anxiety, as demonstrated in many studies in this area. Some of these factors include childhood abuse and adversity; coming from rural areas and adjusting to urban dynamics; being female; and having lower family incomes [18, 19, 21]. We are confident that a combination of genetics, life experiences, and other environmental factors—such as family structures and socioeconomic background—contributes significantly as independent risk factors for experiencing stress, anxiety, depression, and other mental health problems, independent of the pandemic. The ramifications of these studies, including our study and others to come, should be the preparation of specific implementation strategies to address these problems. Numerous intervention models aimed at improving college students’ mental health have been proposed and will continue to be proposed in the future [31-34]. In this regard, various stakeholders must come together in order to assess the potential benefits of different approaches, keeping in mind that an integrated systems approach may be the most beneficial.
Conclusion
Based on the results of this paper and the relevant international literature, it is imperative to emphasize that students need immediate collaboration with the relevant faculty structures to help improve their psychoemotional state. For this purpose, we recommend the implementation of psychological counseling structures at the University of Medicine in Tirana, as well as specialized structures to address post-COVID stress and trauma issues among students. This should include identifying individuals and groups who are more prone to stress vulnerability while also considering other potential mental health conditions among students. In this regard, as part of stress management interventions, we propose the development of specific strategies involving highly trained professionals in order to promote healthy recreational habits and lifestyle modification patterns supported by the medical university.
This study is the first of its kind in Albania with limited resources, and more studies using different methods to assess stress and psychoemotional problems need to be performed in the future. We note that our study only provides a very general idea of the mental health problems that stress can induce among students, especially due to external factors that we cannot control, as was the case with the COVID-19 pandemic and its many consequences. We understand that the responses provided on the PSS-4 are too general and subjective, varying from student to student depending on their experiences and psychoemotional states, and also influenced by other unspecified external factors or underlying health conditions.
Ethical Considerations
Compliance with ethical guidelines
All participants agreed via respective emails to complete the Google Form questionnaire. All collected data were treated with full anonymity.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Data extraction: Ervin Marku and Xhesika Miska; Review and editing: Gentian Vyshka; Conceptualization, supervision and writing the original draft: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors extend sincere thanks to all students who volunteered to complete the questionnaires online.
References
- World Health Organization (WHO). WHO director-general› s opening remarks at the mission briefing on COVID-19 [Internet]; 2020 [Update 2020 March 12]. Available from: [Link]
- Sanyaolu A, Okorie C, Hosein Z, Patidar R, Desai P, Prakash S, Jaferi U, Mangat J, Marinkovic A. Global pandemicity of COVID-19: situation report as of June 9, 2020. Infectious Diseases: Research and Treatment. 2021; 14:1178633721991260. [DOI:10.1177/1178633721991260]
- Xiong J, Lipsitz O, Nasri F, Lui LM, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of affective disorders. 2020; 277:55-64. [DOI:10.1016/j.jad.2020.08.001]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020; 17(5):1729. [DOI:10.3390/ijerph17051729]
- Tiwari GK, Rai PK, Dwivedi A, Ray B, Pandey A, Pandey R. A narrative thematic analysis of the perceived psychological distress and health outcomes in Indian adults during the early phase of the COVID-19 pandemic. Psychology. 2023; 28(1):213-29. [DOI:10.12681/psy_hps.28062]
- Tiwari GK, Tiwari PP, Pandey R, Ray B, Dwived A, Nandan Sharma D, et al. Perceived life outcomes of indian children during the early phase of the COVID-19 lockdown: The protective roles of joint and nuclear families. Journal of Research & Health. 2024; 14(1):43-54. [DOI:10.32598/JRH.14.1.1992.4]
- Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. Journal of Medical Internet Research. 2020; 22(9):e21279. [DOI:10.2196/21279]
- Aylie NS, Mekonen MA, Mekuria RM. The psychological impacts of COVID-19 pandemic among university students in Bench-Sheko Zone, South-west Ethiopia: A community-based cross-sectional study. Psychology Research and Behavior Management. 2020; 13:813-21. [DOI:10.2147/PRBM.S275593]
- Hamasha MM, Alomari AJ, Bani-Irshid AH. The effect of the COVID-19 pandemic crisis on the Jordanian higher education system. Plos One. 2024; 19(4):e0299531. [DOI:10.1371/journal.pone.0299531]
- Thorigny M, Didelot P, Bouazzi L, Pham BN, Barbe C. Reinforcement during the COVID-19 pandemic: Perception of nursing students and impact on intention to drop-out of nursing education. Heliyon. 2024; 10(8):e29316. [DOI:10.1016/j.heliyon.2024.e29316]
- Bani I, Mohamed Y, Andrade G. Evaluation of the impact of COVID-19 on stress and burnout among Ajman university (AU) medical students. Acta Psychologica. 2024; 246:104245. [DOI:10.1016/j.actpsy.2024.104245]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983; 24(4):385-96. [DOI:10.2307/2136404]
- Vallejo MA, Vallejo-Slocker L, Fernández-Abascal EG, Mañanes G. Determining factors for stress perception assessed with the perceived stress scale (PSS-4) in Spanish and Other European samples. Frontiers in Psychology. 2018; 9:37. [DOI:10.3389/fpsyg.2018.00037]
- Li J, Luo R, Guo P, Zhang D, Mo PKH, Wu AMS, et al. Effectiveness of a WHO self-help psychological intervention to alleviate stress among healthcare workers in the context of COVID-19 in China: A randomised controlled trial. Epidemiology and Psychiatric Sciences. 2024; 33:e11. [DOI:10.1017/S2045796024000106]
- Alayadi H, Talakey A, Alsadon O, Vellappally S, Naik S. Psychological impact of COVID-19 lockdown period on students of healthcare colleges. Journal of Family Medicine and Primary Care. 2024; 13(1):199-207. [DOI:10.4103/jfmpc.jfmpc_719_23] [PMID]
- Bruffaerts R, Mortier P, Kiekens G, Auerbach RP, Cuijpers P, Demyttenaere K, et al. Mental health problems in college freshmen: Prevalence and academic functioning. Journal of Affective Disorders. 2018; 225:97-103. [DOI:10.1016/j.jad.2017.07.044]
- Duffy A, Keown-Stoneman C, Goodday S, Horrocks J, Lowe M, King N, et al. Predictors of mental health and academic outcomes in first-year university students: Identifying prevention and early-intervention targets. BJPsych Open. 2020; 6(3):e46. [DOI:10.1192/bjo.2020.24]
- Auerbach RP, Alonso J, Axinn WG, Cuijpers P, Ebert DD, Green JG, Hwang I, et al. Mental disorders among college students in the world health organization world mental health surveys. Psychological Medicine. 2016; 46(14):2955-70. [DOI: 10.1017/S0033291716001665] [PMID]
- Brandy JM, Penckofer S, Solari-Twadell PA, Velsor-Friedrich B. Factors predictive of depression in first-year college students. Journal of Psychosocial Nursing and Mental Health Services. 2015; 53(2):38-44. [DOI:10.3928/02793695-20150126-03]
- Conley CS, Travers LV, Bryant FB. Promoting psychosocial adjustment and stress management in first-year college students: The benefits of engagement in a psychosocial wellness seminar. Journal of American College Health. 2013; 61(2):75-86. [DOI:10.1080/07448481.2012.754757]
- Husky MM, Sadikova E, Lee S, Alonso J, Auerbach RP, Bantjes J, et al. Childhood adversities and mental disorders in first-year college students: Results from the world mental health international college student initiative. Psychological Medicine. 2023; 53(7):2963-73. [DOI:10.1017/S0033291721004980]
- Kim H, Rackoff GN, Fitzsimmons-Craft EE, Shin KE, Zainal NH, Schwob JT, et al. College mental health before and during the COVID-19 pandemic: Results from a nationwide survey. Cognitive Therapy and Research. 2022; 46(1):1-0. [DOI:10.1007/s10608-021-10241-5]
- Koydemir S, Sun-Selışık ZE. Well-being on campus: Testing the effectiveness of an online strengths-based intervention for first year college students. British Journal of Guidance & Counselling. 2016; 44(4):434-46. [DOI:10.1080/03069885.2015.1110562]
- Kroshus E, Hawrilenko M, Browning A. Stress, self-compassion, and well-being during the transition to college. Social Science & Medicine. 2021; 269:113514. [DOI:10.1016/j.socscimed.2020.113514]
- Hersi L, Tesfay K, Gesesew H, Krahl W, Ereg D, Tesfaye M. Mental distress and associated factors among undergraduate students at the University of Hargeisa, Somaliland: A cross-sectional study. International Journal of Mental Health Systems. 2017; 11(39):1-8. [DOI:10.1186/s13033-017-0146-2]
- Erol S, Gur K, Karaca S, Çalık KB, Uzuner A, Apaydın Kaya Ç. Risk factors affecting the mental health of first-year university students on a health sciences campus and related factors. The Journal of Mental Health Training, Education and Practice. 2023; 18(2):146-57. [DOI:10.1108/JMHTEP-03-2022-0015]
- Phalswal U, Pujari V, Sethi R, Verma R. Impact of social media on mental health of the general population during Covid-19 pandemic: A systematic review. Journal of Education and Health Promotion. 2023; 12(1):23. [DOI:10.4103/jehp.jehp_460_22]
- Lelisho ME, Pandey D, Alemu BD, Pandey BK, Tareke SA. The negative impact of social media during covid-19 pandemic. Trends in Psychol. 2023; 31(1):123-42. [DOI:10.1007/s43076-022-00192-5]
- Kramer ADI, Guillory JE, Hancock JT. Experimental evidence of massive-scale emotional contagion through social networks. Psychological and Cognitive Sciences. 2014; 111(24):8788-90. [DOI:10.1073/pnas.1320040111]
- Mahevish R, Khan A, Mahmood HR, Qazi S, Fakhoury HMA, Tamim H. The impact of social media on the physical and mental well-being of medical students during the COVID-19 pandemic. Journal of Epidemiology and Global Health. 2023; 13(4):902-10. [DOI:10.1007/s44197-023-00164-7]
- Seppälä EM, Bradley C, Moeller J, Harouni L, Nandamudi D, Brackett MA. Promoting mental health and psychological thriving in university students: A randomized controlled trial of three well-being interventions. Frontiers in Psychiatry. 2020; 11:590. [DOI:10.3389/fpsyt.2020.00590]
- Harrer M, Adam SH, Baumeister H, Cuijpers P, Karyotaki E, Auerbach RP, et al. Internet interventions for mental health in university students: A systematic review and meta-analysis. International Journal of Methods in Psychiatric Research. 2019; 28(2):e1759. [DOI:10.1002/mpr.1759]
- Haug T, Nordgreen T, Öst LG, Havik OE. Self-help treatment of anxiety disorders: A meta-analysis and meta-regression of effects and potential moderators. Clinical Psychology Review. 2012; 32(5):425-45. [DOI:10.1016/j.cpr.2012.04.002]
- Donnelly S, Penny K, Kynn M. The effectiveness of physical activity interventions in improving higher education students› mental health: A systematic review. Health Promotion International. 2024; 39(2):daae027. [DOI:10.1093/heapro/daae027]
Type of Study: Orginal Article |
Subject:
● International Health
Received: 2024/04/29 | Accepted: 2024/06/5 | Published: 2024/10/28
Received: 2024/04/29 | Accepted: 2024/06/5 | Published: 2024/10/28
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |