Volume 15, Issue 3 (May & June 2025)
J Research Health 2025, 15(3): 237-246 |
Back to browse issues page
Ethics code: No.306/KE/11/2023
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pranata S, Wahyudi M R. The Relationship Between Self-acceptance and Self-management on Diabetes Distress among Diabetes Patients in Indonesia. J Research Health 2025; 15 (3) :237-246
URL: http://jrh.gmu.ac.ir/article-1-2628-en.html
URL: http://jrh.gmu.ac.ir/article-1-2628-en.html
1- Department of Nursing, Faculty of Nursing, Universitas Muhammadiyah Semarang, Semarang, Indonesia.
2- Department of Nursing, Faculty of Nursing, Universitas Muhammadiyah Semarang, Semarang, Indonesia. ,rizkywahyudi976@gmail.com
2- Department of Nursing, Faculty of Nursing, Universitas Muhammadiyah Semarang, Semarang, Indonesia. ,
Full-Text [PDF 585 kb]
(776 Downloads)
| Abstract (HTML) (3454 Views)
Discussion
This study determined the relationship between self-acceptance and self-management of diabetes distress among patients at Roemani Semarang Hospital, Indonesia. The data of this study showed that self-acceptance and self-management are closely related to the incidence of diabetes distress.
The demographic characteristics of respondents showed that most of them were female, with 28 respondents (53.8%). The number of men was lower than that of women because women are prone to diabetes. Both men and women are at risk of developing diabetes mellitus, but women have a greater risk of suffering from diabetes mellitus, than men due to factors such as a higher likelihood of increased body mass index associated with premenstrual syndrome, which places them at risk for the disease. The highest level of education was high school, with 33 respondents (63.5%). High school education is more significant a larger number of respondents at Roemani Hospital Semarang have this level of education, and many do not seek treatment; they are often more unaware of their illness and more focused on work. A previous study states that knowledge is a person’s point of view on various subjects at different levels. Therefore, individuals with a higher level of education tend to have better knowledge, particularly regarding healthy lifestyle practices [13]. A total of 49 respondents (94.2%) were married, and most of the respondents were housewives, totaling 19 respondents (36.5%). Housewives are more susceptible to diabetes distress because they are always at home and do not engage in regular exercise [13]. Patients who have a partner are more concerned about their economic condition; therefore, diabetic patients have a high level of stress. Those with lower economic status may consume unhealthy and irregular meals. This also affects diabetes distress. Therefore, patients with married status (having a partner) may experience higher levels of stress than those who are not married.
The majority of respondents experienced a moderate level of diabetic distress, with 32 respondents (61.5%). Diabetes patients are twice as likely to experience stress than other people who do not have diabetes. This is mainly related to the quantity, type, and unhealthy eating habits before and after being diagnosed with diabetes. Diabetic patients experience high stress because they often desire to eat more than what is recommended. When diabetics experience stress, their urge to consume foods that they should avoid leads them to deviate from the meal plan that has been established [7].
The majority of respondents showed a moderate level of self-acceptance, with 41 respondents (78.9%). This means that patients are more accepting of themselves and resigned to the situation. Self-acceptance is the ability to accept circumstances as they are and realize that there is no alternative but to accept them. Negative self-acceptance makes it difficult to understand one’s condition, especially when their health condition changes. As a result, negative self-acceptance makes diabetics less capable of maintaining their health [14]. Lack of family support will have an impact on the self-acceptance of diabetic patients. Diabetic patients with poor self-acceptance are likely to feel depressed and may engage in self-defense mechanisms by rejection of their condition. This can trigger stress because they reject the reality of their actual shortcomings and weaknesses. Such denial prevents individuals from improving their condition, as they believe that their negative situation does not apply to them [8]. If adverse realities occur for a diabetic patient, they may refuse to acknowledge their illness, leading to a lack of ongoing treatment and potentially worsening physical conditions due to diabetes in the future. Poor self-acceptance can be caused by physical problems or decreased ability. Self-acceptance in the context of diabetes distress is highly correlated with an individual’s ability to respond and their unique perceptions of experiencing various challenges [14]. If individuals cannot accept their circumstances, they will have difficulty adjusting to their condition, which can exacerbate diabetes distress [14].
The majority of respondents showed a good level of self-management, with 439 respondents (75%). People with diabetes require significant time and energy to implement various strategies for managing their disease, such as adhering to rules for managing their disease independently according to their plans, which is called self-management. Self-management is the ability of individuals, families, and communities to improve their health, prevent disease, maintain their health, and cope with illness and disability, with or without support from healthcare providers [15]. Increased self-management behaviors performed by people with diabetes will reduce the risk and level of distress. Adherence to a diabetes self-management regimen will help improve and maintain stable glycemic control, which will prevent the disease condition from getting worse [15]. Good glycemic conditions will also reduce the risk of complications and the psychological burden that can cause greater emotional and psychological distress experienced by people with diabetes mellitus. Other studies indicate a correlation between self-management and diabetes distress. Diabetes distress encompasses the worries that diabetic patients face regarding disease management, obtaining support, experiencing emotional difficulties, and receiving the necessary care. Moreover, a lack of self-management among diabetic patients can cause distress because self-management serves to control blood glucose and prevent complications. When blood glucose levels are well-managed, the negative psychological impacts, such as diabetes distress, can be diminished [16].
Diabetes distress sufferers who accept their illness and have a high level of self-acceptance will likely experience good mental health, which can motivate them to adhere to a healthy diet, increase physical activity, monitor blood glucose levels regularly, take medication consistently, and perform foot care—collectively referred to as diabetes mellitus self-management. This means that the higher the levels of self-acceptance of people with diabetes distress, the better the self-management will be [17]. Health professionals should pay more attention to the patient’s condition in detail regarding diabetes distress because this condition will have an impact on the patient’s ability to engage in effective self-management or lack thereof. Strengthening self-acceptance will help diabetes patients focus more on themselves and their health condition, thereby reducing diabetes distress and allowing them to concentrate more on implementing self-management strategies.
Conclusion
Based on the results of the study, self-acceptance and self-management had a relationship with diabetes distress at Roemani Semarang Hospital, Indonesia. It is expected that patients will be able to accept themselves and engage in self-management practices, such as regulating diet and lifestyle, to decrease diabetes distress. Health professionals are encouraged to pay more attention to the psychological condition of patients with diabetes mellitus during treatment and to provide training in self-management to help reduce diabetes distress in the future.
Ethical Considerations
Compliance with ethical guidelines
Each participant received the study’s explanation (study’s goal and procedures) before completing the questionnaires. Participants were also given a chance to process and ask for clearer explanations for their doubts to facilitate informed consent. Participation was voluntary, and participants had the right to withdraw from the study at any time. Ethical approval was granted by the Health Research Ethics Committee of the Faculty of Nursing and Health Sciences at Universitas Muhammadiyah Semarang, Semarang, Indonesia (No.: 306/KE/11/2023).
Funding
This study was financially supported by the Universitas Muhammadiyah Semarang, Semarang, Indonesia.
Authors' contributions
Conceptualization, methodology, formal analysis, investigation, and writing the original draft: Mohamad Rizky Wahyudi; Data curation, resources, visualization, project administration, review and editing: Satriya Pranata; Validation, supervision, and funding acquisition: Satriya Pranata; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors want to express their gratitude to the respondents and any parties who supported this study.
Full-Text: (1043 Views)
Introduction
Diabetes mellitus is a group of metabolic disorders characterized by elevated blood glucose levels (hyperglycemia) due to defects in insulin secretion, insulin action, or both [1]. Diabetes is divided into type I and type II. Type I diabetes occurs due to insufficient insulin production caused by an autoimmune reaction that destroys pancreatic beta cells. The basic treatment for type I diabetes, even in its earliest stages, is insulin replacement [1]. Moreover, type II diabetes mellitus is also known as adult-onset diabetes, obesity-related diabetes, or non-insulin-dependent diabetes mellitus [2].
According to the World Health Organization (WHO), more than half a billion people worldwide live with diabetes—specifically, 537 million individuals—and this number is projected to reach 643 million by 2030 and 783 million by 2045 [3]. The number of diabetes sufferers aged 20-79 years in Indonesia has experienced a significant increase from 5.65 million in 2000 to 19.47 million by 2021. It is estimated that this figure will rise to 23.33 million by 2030. The prevalence of diabetes increased significantly from 5.1% in 2011 to 10.6% in 2021. In Central Java Province, an estimated 652,822 people suffer from diabetes mellitus, with currently 32,081 reported cases. According to data from the National Health Insurance of Indonesia, the total claim costs for national health insurance related to diabetes increased from IDR 4.9 trillion in 2018 to IDR 6.4 trillion in 2022 [4].
Diabetic patients in hospitals and communities in Indonesia are required to implement self-management over the long term to stabilize their blood glucose levels in accordance with national program requirements by the Ministry of Health [5]. The four domains of diabetes self-management are diet, glucose management, physical activity, and healthcare utilization. An incorrect diet can cause blood sugar levels in patients with diabetes to be uncontrolled. Physical activity or exercise can also reduce weight and improve insulin sensitivity, resulting in better blood glucose control. Unstable blood sugar levels can be caused by uncontrolled food consumption behavior or poor diet, which can lead to various complications in the future. Short-term self-management programs reduce complaints and signs of diabetes, while long-term management reduces complications [6]. However, maintaining controlled blood glucose levels over an extended period can make diabetic patients vulnerable to distress due to the burden of medication. If diabetes distress cannot be managed by patients, self-management may not be achieved [7].
In addition to physical factors related to self-management, physiological factors, such as self-acceptance are also needed for diabetes patients in a comprehensive intervention. Self-acceptance refers to an individual’s ability to accept themselves well, which is facilitated by an attitude that reflects their feelings about their actions [8]. Diabetes patients with poor self-acceptance may develop a negative view of themselves, which can adversely affect their diabetes self-management [9].
The steps to address distress begin with slow but steady lifestyle changes, such as increasing physical activity, observing diet, and monitoring blood sugar closely by self-management. Secondly, improving coping skills involves accepting that not everyone can control everything by self-acceptance. When patients can accept their illness, they tend to feel more relaxed, which reduces the occurrence of stress [10]. For many people who think negatively and struggle to accept that they have diabetes, researchers aim to examine how acceptance can help diabetic patients feel more relaxed and less stressed. It is essential for them to adopt a positive mindset regarding their recovery from diabetes distress. Thus, the purpose of this study was to determine the relationship between acceptance and self-management of diabetes distress in diabetic patients at the Roemani Semarang Hospital, Indonesia.
Methods
Study design
This cross-sectional study measured and collected data only at a single point in time. This design can measure the relationship between self-acceptance and self-management of diabetes distress among diabetes patients. The research setting was the Roemani Semarang Hospital, Indonesia, which is a charitable organization run by the Muhammadiyah regional leadership in the city of Semarang. The research was conducted in the Ayub 2 and Sulaiman 3 to 6 rooms, with 11 participants selected from each room.
Sample and participants
Approximately 60 participants suffering from diabetes distress were included in the study. From this data, sample calculations were performed to determine how many samples needed to be studied. The minimum sample size for this cross-sectional study was calculated to be 60 people using the Lameshow formula (Equation 1), with a degree of confidence (z=1.96), a proportion of respondents with good self-acceptance of 66.2%, and a precision of 5%.
In this formula, n is the number of samples, z is the degree of confidence, P is the proportion of respondents with good self-acceptance, and d is a precision of 5%.
The sampling technique used was consecutive sampling. In this sampling technique, the sample size can range from a few to hundreds. If the results of one sample are inaccurate, the researcher can easily rely on the next sample to get results that are more accurate and representative of the population studied. All subjects who arrived and met the inclusion criteria—diabetes patients aged between 25 and 69 years, with diabetes lasting at least six months, and who were willing to participate—were recruited until the minimum sample size was reached. On the other hand, respondents with significant physical impairments preventing them from participating in the study, such as blindness and deafness, were excluded from the study. These physical limitations would hinder respondents’ ability to fill out questionnaires or answer questions from researchers. Non-probability sampling also has some important drawbacks. The lack of representativeness means that, since the sample is not randomly selected, the results may not be generalizable to the wider population. The selection process may introduce bias, as participants’ choices are influenced by accessibility, referrals, or researcher judgment. Additionally, non-probability sampling may not be applicable or scalable to larger populations. While this approach facilitates the search for participants, it carries a high risk of significant bias, as it does not cover a large proportion of the population of interest. Consequently, the findings might not be generalizable to other settings in different countries.
Data collection
Data were collected from December 2023 to February 2024 at Roemani Semarang Hospital, which served as the location of this study. Participants were recruited based on inclusion and exclusion criteria until the minimum sample size was achieved. During one-on-one interviews, patients provided personal information regarding their gender, marital status, occupation, and education level, and they completed the questionnaires with guidance from the researchers. Prospective participants were then approached, and after the details of the study were explained and written consent obtained, trained researchers administered the questionnaires. Interviews were conducted at the outpatient clinic in the hospital while participants were waiting for their doctors.
Measurement
The instruments used were the acceptance of illness scale (AIS) with indicators rated as follows: 1=strongly agree, 2=agree, 3=don’t know, 4=disagree, and 5=strongly disagree, with total scores ranging from 20 to 40. The category of illness acceptance can be determined based on the scores obtained from the AIS questionnaire: Scores of 8 to 19 indicate low acceptance, scores of 20 to 30 indicate moderate acceptance, and scores above 30 indicate high acceptance. The greater the acceptance of their illness, the better patients adjust and the less grief they experience. The AIS reliability test yielded a Cronbach’s α of 0.628 [9].
The questionnaire used to measure the level of self-management of diabetes mellitus treatment was the diabetes self-management questionnaire (DSMQ). The alternative scoring system indicates: 0=never done, 1=sometimes, 2=ever done, and 3=always done. According to the interpretation of the DSMQ results, scores are categorized as “good” (32-48), “fair” (16-31), and “poor” (0-15). The DSMQ reliability test yielded a Cronbach’s α of 0.861 [11].
The diabetes distress scale (DDS) consists of 17 items that address issues that can cause distress in patients with diabetes. The sum of all items is then divided into 17 to produce a score for the measurement of diabetes stress. Statements are scored as follows: 1 means not appropriate at all or never, 2 means slightly appropriate or sometimes, 3 means appropriate to some degree or sometimes, 4 means appropriate or somewhat often, 5 means appropriate or often, and 6 means very appropriate. The lowest score is 1, and the highest score is 6. Scores of 1-25 indicate low distress, scores of indicate 26-50 moderate distress, and scores of more than 50 indicate high distress. The DDS reliability test yielded a Cronbach’s α of 0.840 [12].
Data analysis
The researcher used descriptive analysis to describe the diabetes distress data. This was accomplished by creating frequency tables for each variable. Numerical data, which included age and duration of suffering, was analyzed and presented as minimum, maximum, mean, and standard deviation. Categorical data, including gender, education level, and occupation, were presented as frequency and percentage.
In the bivariate analysis, the data scale used was ordinal (nonparametric) and the Spearman correlation coefficient was used to assess the relationship between variables. If P<0.05, this indicates a relationship, leading to the acceptance of diabetes distress. Conversely, if P>0.05, it indicates no relationship between self-acceptance and diabetes distress.
The appropriate type of data for ANOVA is nominal and ordinal for the independent variable. The analysis of variance (ANOVA) was used to compare the mean of two or more groups of data, thereby assisting in making more informed decisions and reducing errors. The ANOVA can reduce the possibility of type I errors (false positives) that may occur when performing multiple tests, thereby supporting or rejecting hypotheses. ANOVA can provide strong empirical evidence to support or reject hypotheses and facilitate the analysis of several different sample groups with the least risk of error.
Results
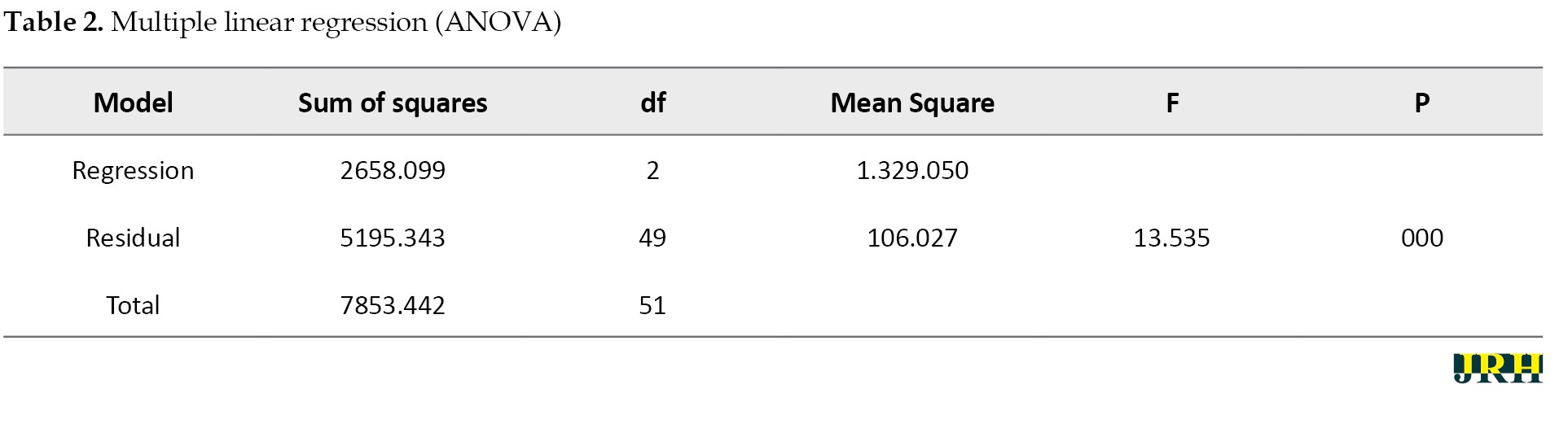
Table 1 displays the demographic characteristics of respondents, including gender, education level, marital status, and occupation, as well as the variables of self-acceptance, self-management, and DDS, to illustrate the percentages and numbers.
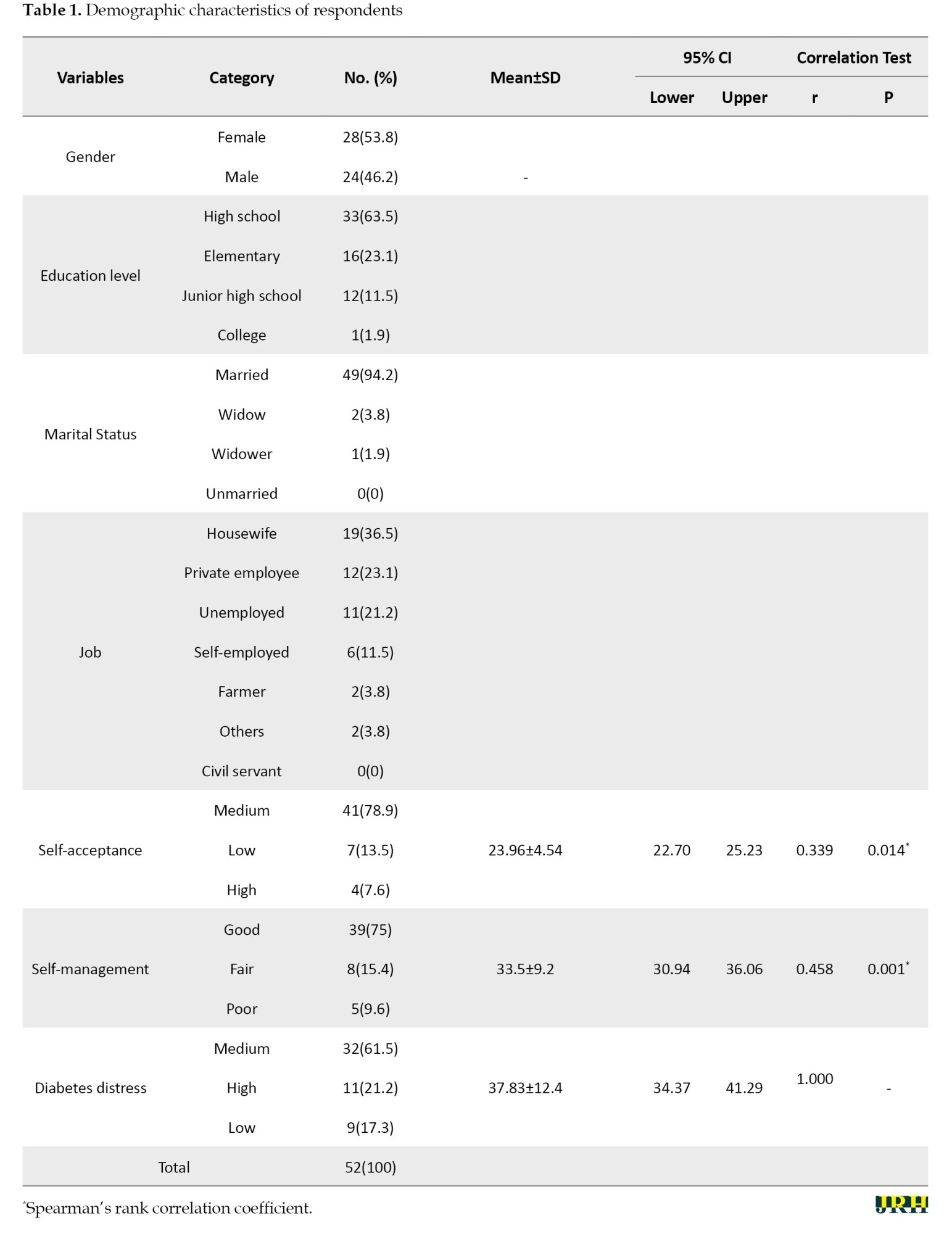
The demographic characteristics of respondents showed that most of them were female, with 28 respondents (53.8%). The education level of the majority was high school, with 33 respondents (63.5%). Additionally, 49 respondents (94.2%) reported being married, and 19 respondents (36.5%) worked as housewives. The majority of respondents showed a moderate level of self-acceptance, with 41 respondents (78.9%), a good level of self-management, with 39 respondents (75%), and a moderate level of diabetic distress, with 32 respondents (61.5%).
The results of the Spearman rank correlation test showed a P of 0.014, which can be interpreted as showing a significant relationship between self-acceptance and diabetes distress. The correlation coefficient obtained from the data was 0.339, suggesting a moderate strength of the relationship between self-acceptance and diabetes distress. Moreover, the positive direction of the relationship coefficient indicates that as self-acceptance increases, diabetes distress decreases. A positive value implies that higher self-acceptance correlates with lower stress levels for the patient.
The results of the Spearman rank correlation test showed a P of 0.001. Thus, there is a significant relationship between self-management and diabetes distress. The strength of the relationship, as indicated by the correlation coefficient of 0.458, suggests a moderate level of association between self-management and diabetes distress. The positive direction of the relationship coefficient indicates that as self-management increases, diabetes distress decreases. A positive value signifies that good self-management implies that the patient is effectively taking care of themselves and is less likely to experience stress due to the manageable nature of the disease.
In addition, the intervals for self-acceptance of diabetes distress and self-management of diabetes distress showed narrow confidence intervals of 22.70-25.23 and 30.94-36.06, respectively. This means a strong level of confidence in the relationship between the variables.
In the Table 2, the significance value (0.000) is <0.05; thus, the null hypothesis is rejected and the alternative hypothesis is accepted.
This indicates that x1 (self-acceptance) and x2 (self-management) together affect variable Y (diabetes distress).
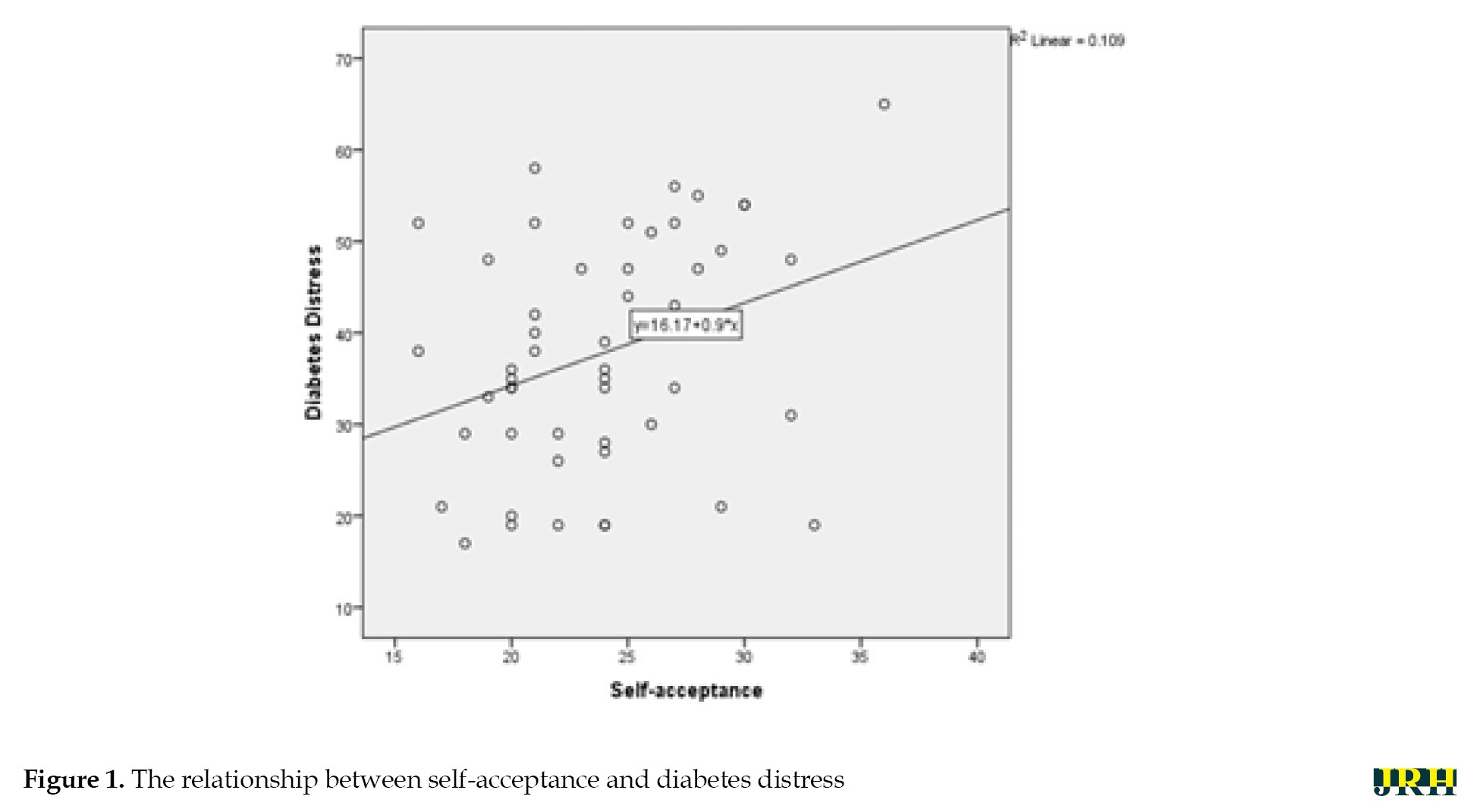
Figure 1 shows a graph that rises from bottom to top, indicating a relationship between self-acceptance and diabetes distress.
Diabetes mellitus is a group of metabolic disorders characterized by elevated blood glucose levels (hyperglycemia) due to defects in insulin secretion, insulin action, or both [1]. Diabetes is divided into type I and type II. Type I diabetes occurs due to insufficient insulin production caused by an autoimmune reaction that destroys pancreatic beta cells. The basic treatment for type I diabetes, even in its earliest stages, is insulin replacement [1]. Moreover, type II diabetes mellitus is also known as adult-onset diabetes, obesity-related diabetes, or non-insulin-dependent diabetes mellitus [2].
According to the World Health Organization (WHO), more than half a billion people worldwide live with diabetes—specifically, 537 million individuals—and this number is projected to reach 643 million by 2030 and 783 million by 2045 [3]. The number of diabetes sufferers aged 20-79 years in Indonesia has experienced a significant increase from 5.65 million in 2000 to 19.47 million by 2021. It is estimated that this figure will rise to 23.33 million by 2030. The prevalence of diabetes increased significantly from 5.1% in 2011 to 10.6% in 2021. In Central Java Province, an estimated 652,822 people suffer from diabetes mellitus, with currently 32,081 reported cases. According to data from the National Health Insurance of Indonesia, the total claim costs for national health insurance related to diabetes increased from IDR 4.9 trillion in 2018 to IDR 6.4 trillion in 2022 [4].
Diabetic patients in hospitals and communities in Indonesia are required to implement self-management over the long term to stabilize their blood glucose levels in accordance with national program requirements by the Ministry of Health [5]. The four domains of diabetes self-management are diet, glucose management, physical activity, and healthcare utilization. An incorrect diet can cause blood sugar levels in patients with diabetes to be uncontrolled. Physical activity or exercise can also reduce weight and improve insulin sensitivity, resulting in better blood glucose control. Unstable blood sugar levels can be caused by uncontrolled food consumption behavior or poor diet, which can lead to various complications in the future. Short-term self-management programs reduce complaints and signs of diabetes, while long-term management reduces complications [6]. However, maintaining controlled blood glucose levels over an extended period can make diabetic patients vulnerable to distress due to the burden of medication. If diabetes distress cannot be managed by patients, self-management may not be achieved [7].
In addition to physical factors related to self-management, physiological factors, such as self-acceptance are also needed for diabetes patients in a comprehensive intervention. Self-acceptance refers to an individual’s ability to accept themselves well, which is facilitated by an attitude that reflects their feelings about their actions [8]. Diabetes patients with poor self-acceptance may develop a negative view of themselves, which can adversely affect their diabetes self-management [9].
The steps to address distress begin with slow but steady lifestyle changes, such as increasing physical activity, observing diet, and monitoring blood sugar closely by self-management. Secondly, improving coping skills involves accepting that not everyone can control everything by self-acceptance. When patients can accept their illness, they tend to feel more relaxed, which reduces the occurrence of stress [10]. For many people who think negatively and struggle to accept that they have diabetes, researchers aim to examine how acceptance can help diabetic patients feel more relaxed and less stressed. It is essential for them to adopt a positive mindset regarding their recovery from diabetes distress. Thus, the purpose of this study was to determine the relationship between acceptance and self-management of diabetes distress in diabetic patients at the Roemani Semarang Hospital, Indonesia.
Methods
Study design
This cross-sectional study measured and collected data only at a single point in time. This design can measure the relationship between self-acceptance and self-management of diabetes distress among diabetes patients. The research setting was the Roemani Semarang Hospital, Indonesia, which is a charitable organization run by the Muhammadiyah regional leadership in the city of Semarang. The research was conducted in the Ayub 2 and Sulaiman 3 to 6 rooms, with 11 participants selected from each room.
Sample and participants
Approximately 60 participants suffering from diabetes distress were included in the study. From this data, sample calculations were performed to determine how many samples needed to be studied. The minimum sample size for this cross-sectional study was calculated to be 60 people using the Lameshow formula (Equation 1), with a degree of confidence (z=1.96), a proportion of respondents with good self-acceptance of 66.2%, and a precision of 5%.
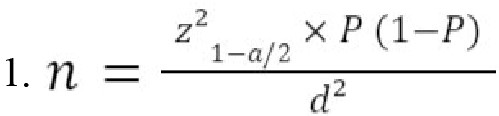
In this formula, n is the number of samples, z is the degree of confidence, P is the proportion of respondents with good self-acceptance, and d is a precision of 5%.
The sampling technique used was consecutive sampling. In this sampling technique, the sample size can range from a few to hundreds. If the results of one sample are inaccurate, the researcher can easily rely on the next sample to get results that are more accurate and representative of the population studied. All subjects who arrived and met the inclusion criteria—diabetes patients aged between 25 and 69 years, with diabetes lasting at least six months, and who were willing to participate—were recruited until the minimum sample size was reached. On the other hand, respondents with significant physical impairments preventing them from participating in the study, such as blindness and deafness, were excluded from the study. These physical limitations would hinder respondents’ ability to fill out questionnaires or answer questions from researchers. Non-probability sampling also has some important drawbacks. The lack of representativeness means that, since the sample is not randomly selected, the results may not be generalizable to the wider population. The selection process may introduce bias, as participants’ choices are influenced by accessibility, referrals, or researcher judgment. Additionally, non-probability sampling may not be applicable or scalable to larger populations. While this approach facilitates the search for participants, it carries a high risk of significant bias, as it does not cover a large proportion of the population of interest. Consequently, the findings might not be generalizable to other settings in different countries.
Data collection
Data were collected from December 2023 to February 2024 at Roemani Semarang Hospital, which served as the location of this study. Participants were recruited based on inclusion and exclusion criteria until the minimum sample size was achieved. During one-on-one interviews, patients provided personal information regarding their gender, marital status, occupation, and education level, and they completed the questionnaires with guidance from the researchers. Prospective participants were then approached, and after the details of the study were explained and written consent obtained, trained researchers administered the questionnaires. Interviews were conducted at the outpatient clinic in the hospital while participants were waiting for their doctors.
Measurement
The instruments used were the acceptance of illness scale (AIS) with indicators rated as follows: 1=strongly agree, 2=agree, 3=don’t know, 4=disagree, and 5=strongly disagree, with total scores ranging from 20 to 40. The category of illness acceptance can be determined based on the scores obtained from the AIS questionnaire: Scores of 8 to 19 indicate low acceptance, scores of 20 to 30 indicate moderate acceptance, and scores above 30 indicate high acceptance. The greater the acceptance of their illness, the better patients adjust and the less grief they experience. The AIS reliability test yielded a Cronbach’s α of 0.628 [9].
The questionnaire used to measure the level of self-management of diabetes mellitus treatment was the diabetes self-management questionnaire (DSMQ). The alternative scoring system indicates: 0=never done, 1=sometimes, 2=ever done, and 3=always done. According to the interpretation of the DSMQ results, scores are categorized as “good” (32-48), “fair” (16-31), and “poor” (0-15). The DSMQ reliability test yielded a Cronbach’s α of 0.861 [11].
The diabetes distress scale (DDS) consists of 17 items that address issues that can cause distress in patients with diabetes. The sum of all items is then divided into 17 to produce a score for the measurement of diabetes stress. Statements are scored as follows: 1 means not appropriate at all or never, 2 means slightly appropriate or sometimes, 3 means appropriate to some degree or sometimes, 4 means appropriate or somewhat often, 5 means appropriate or often, and 6 means very appropriate. The lowest score is 1, and the highest score is 6. Scores of 1-25 indicate low distress, scores of indicate 26-50 moderate distress, and scores of more than 50 indicate high distress. The DDS reliability test yielded a Cronbach’s α of 0.840 [12].
Data analysis
The researcher used descriptive analysis to describe the diabetes distress data. This was accomplished by creating frequency tables for each variable. Numerical data, which included age and duration of suffering, was analyzed and presented as minimum, maximum, mean, and standard deviation. Categorical data, including gender, education level, and occupation, were presented as frequency and percentage.
In the bivariate analysis, the data scale used was ordinal (nonparametric) and the Spearman correlation coefficient was used to assess the relationship between variables. If P<0.05, this indicates a relationship, leading to the acceptance of diabetes distress. Conversely, if P>0.05, it indicates no relationship between self-acceptance and diabetes distress.
The appropriate type of data for ANOVA is nominal and ordinal for the independent variable. The analysis of variance (ANOVA) was used to compare the mean of two or more groups of data, thereby assisting in making more informed decisions and reducing errors. The ANOVA can reduce the possibility of type I errors (false positives) that may occur when performing multiple tests, thereby supporting or rejecting hypotheses. ANOVA can provide strong empirical evidence to support or reject hypotheses and facilitate the analysis of several different sample groups with the least risk of error.
Results
Table 1 displays the demographic characteristics of respondents, including gender, education level, marital status, and occupation, as well as the variables of self-acceptance, self-management, and DDS, to illustrate the percentages and numbers.
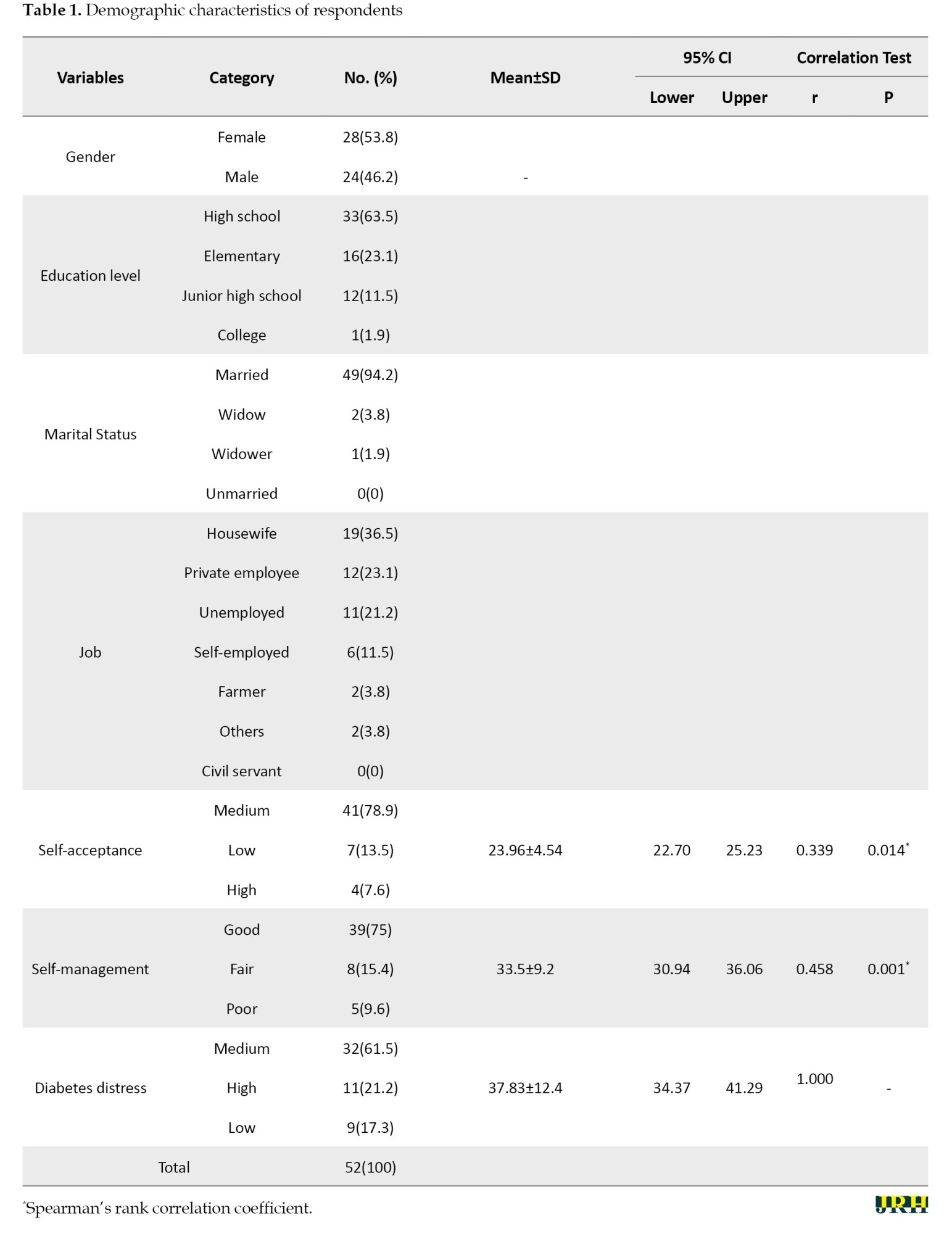
The demographic characteristics of respondents showed that most of them were female, with 28 respondents (53.8%). The education level of the majority was high school, with 33 respondents (63.5%). Additionally, 49 respondents (94.2%) reported being married, and 19 respondents (36.5%) worked as housewives. The majority of respondents showed a moderate level of self-acceptance, with 41 respondents (78.9%), a good level of self-management, with 39 respondents (75%), and a moderate level of diabetic distress, with 32 respondents (61.5%).
The results of the Spearman rank correlation test showed a P of 0.014, which can be interpreted as showing a significant relationship between self-acceptance and diabetes distress. The correlation coefficient obtained from the data was 0.339, suggesting a moderate strength of the relationship between self-acceptance and diabetes distress. Moreover, the positive direction of the relationship coefficient indicates that as self-acceptance increases, diabetes distress decreases. A positive value implies that higher self-acceptance correlates with lower stress levels for the patient.
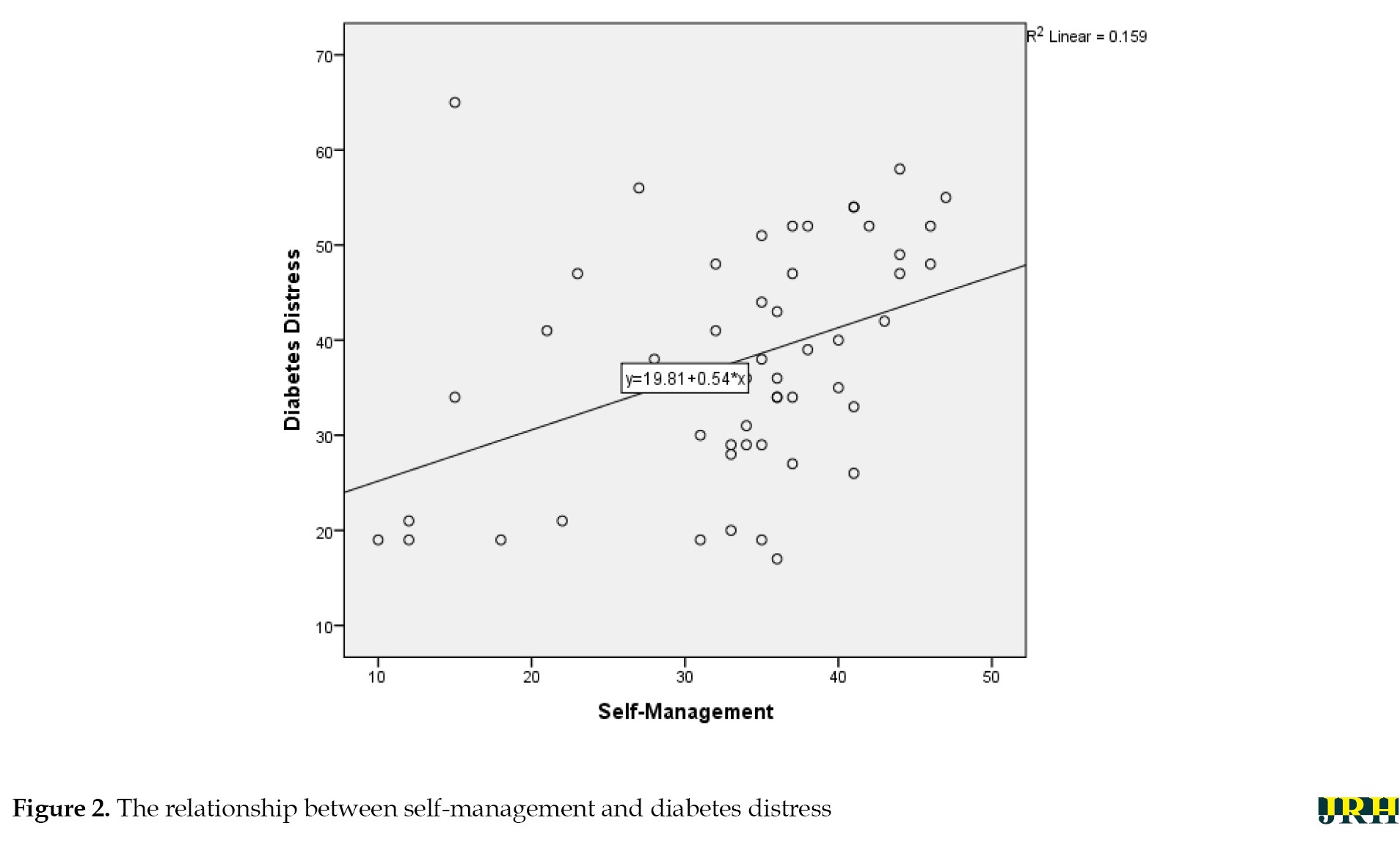
The results of the Spearman rank correlation test showed a P of 0.001. Thus, there is a significant relationship between self-management and diabetes distress. The strength of the relationship, as indicated by the correlation coefficient of 0.458, suggests a moderate level of association between self-management and diabetes distress. The positive direction of the relationship coefficient indicates that as self-management increases, diabetes distress decreases. A positive value signifies that good self-management implies that the patient is effectively taking care of themselves and is less likely to experience stress due to the manageable nature of the disease.
In addition, the intervals for self-acceptance of diabetes distress and self-management of diabetes distress showed narrow confidence intervals of 22.70-25.23 and 30.94-36.06, respectively. This means a strong level of confidence in the relationship between the variables.
In the Table 2, the significance value (0.000) is <0.05; thus, the null hypothesis is rejected and the alternative hypothesis is accepted.
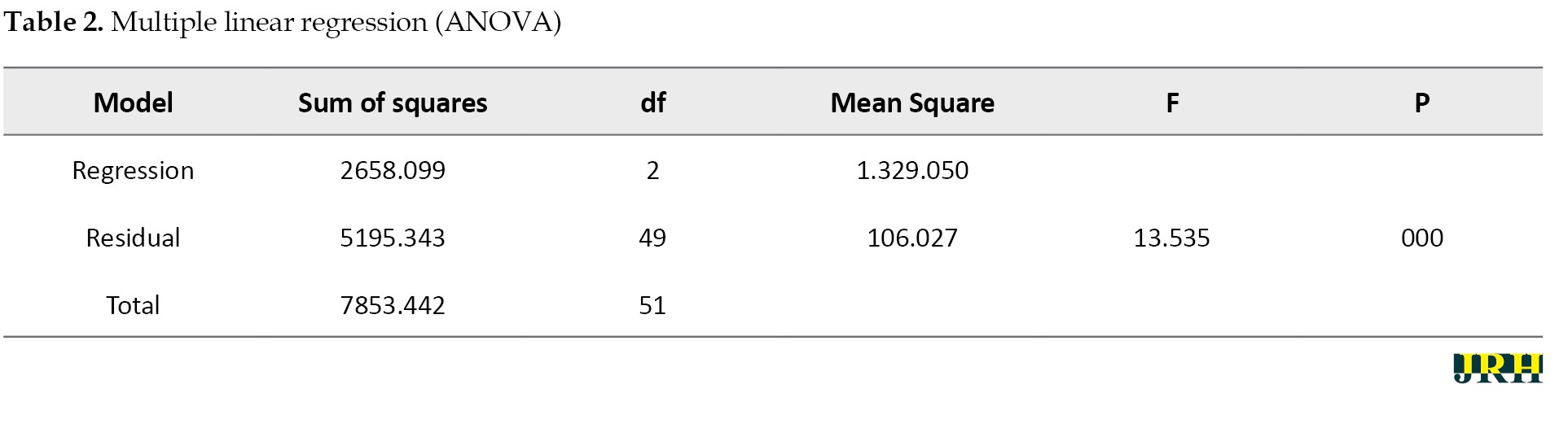
This indicates that x1 (self-acceptance) and x2 (self-management) together affect variable Y (diabetes distress).
Figure 1 shows a graph that rises from bottom to top, indicating a relationship between self-acceptance and diabetes distress.
Similarly, Figure 2 presents a graph that also rises from bottom to top, demonstrating a relationship between self-management and diabetes distress.
Discussion
This study determined the relationship between self-acceptance and self-management of diabetes distress among patients at Roemani Semarang Hospital, Indonesia. The data of this study showed that self-acceptance and self-management are closely related to the incidence of diabetes distress.
The demographic characteristics of respondents showed that most of them were female, with 28 respondents (53.8%). The number of men was lower than that of women because women are prone to diabetes. Both men and women are at risk of developing diabetes mellitus, but women have a greater risk of suffering from diabetes mellitus, than men due to factors such as a higher likelihood of increased body mass index associated with premenstrual syndrome, which places them at risk for the disease. The highest level of education was high school, with 33 respondents (63.5%). High school education is more significant a larger number of respondents at Roemani Hospital Semarang have this level of education, and many do not seek treatment; they are often more unaware of their illness and more focused on work. A previous study states that knowledge is a person’s point of view on various subjects at different levels. Therefore, individuals with a higher level of education tend to have better knowledge, particularly regarding healthy lifestyle practices [13]. A total of 49 respondents (94.2%) were married, and most of the respondents were housewives, totaling 19 respondents (36.5%). Housewives are more susceptible to diabetes distress because they are always at home and do not engage in regular exercise [13]. Patients who have a partner are more concerned about their economic condition; therefore, diabetic patients have a high level of stress. Those with lower economic status may consume unhealthy and irregular meals. This also affects diabetes distress. Therefore, patients with married status (having a partner) may experience higher levels of stress than those who are not married.
The majority of respondents experienced a moderate level of diabetic distress, with 32 respondents (61.5%). Diabetes patients are twice as likely to experience stress than other people who do not have diabetes. This is mainly related to the quantity, type, and unhealthy eating habits before and after being diagnosed with diabetes. Diabetic patients experience high stress because they often desire to eat more than what is recommended. When diabetics experience stress, their urge to consume foods that they should avoid leads them to deviate from the meal plan that has been established [7].
The majority of respondents showed a moderate level of self-acceptance, with 41 respondents (78.9%). This means that patients are more accepting of themselves and resigned to the situation. Self-acceptance is the ability to accept circumstances as they are and realize that there is no alternative but to accept them. Negative self-acceptance makes it difficult to understand one’s condition, especially when their health condition changes. As a result, negative self-acceptance makes diabetics less capable of maintaining their health [14]. Lack of family support will have an impact on the self-acceptance of diabetic patients. Diabetic patients with poor self-acceptance are likely to feel depressed and may engage in self-defense mechanisms by rejection of their condition. This can trigger stress because they reject the reality of their actual shortcomings and weaknesses. Such denial prevents individuals from improving their condition, as they believe that their negative situation does not apply to them [8]. If adverse realities occur for a diabetic patient, they may refuse to acknowledge their illness, leading to a lack of ongoing treatment and potentially worsening physical conditions due to diabetes in the future. Poor self-acceptance can be caused by physical problems or decreased ability. Self-acceptance in the context of diabetes distress is highly correlated with an individual’s ability to respond and their unique perceptions of experiencing various challenges [14]. If individuals cannot accept their circumstances, they will have difficulty adjusting to their condition, which can exacerbate diabetes distress [14].
The majority of respondents showed a good level of self-management, with 439 respondents (75%). People with diabetes require significant time and energy to implement various strategies for managing their disease, such as adhering to rules for managing their disease independently according to their plans, which is called self-management. Self-management is the ability of individuals, families, and communities to improve their health, prevent disease, maintain their health, and cope with illness and disability, with or without support from healthcare providers [15]. Increased self-management behaviors performed by people with diabetes will reduce the risk and level of distress. Adherence to a diabetes self-management regimen will help improve and maintain stable glycemic control, which will prevent the disease condition from getting worse [15]. Good glycemic conditions will also reduce the risk of complications and the psychological burden that can cause greater emotional and psychological distress experienced by people with diabetes mellitus. Other studies indicate a correlation between self-management and diabetes distress. Diabetes distress encompasses the worries that diabetic patients face regarding disease management, obtaining support, experiencing emotional difficulties, and receiving the necessary care. Moreover, a lack of self-management among diabetic patients can cause distress because self-management serves to control blood glucose and prevent complications. When blood glucose levels are well-managed, the negative psychological impacts, such as diabetes distress, can be diminished [16].
Diabetes distress sufferers who accept their illness and have a high level of self-acceptance will likely experience good mental health, which can motivate them to adhere to a healthy diet, increase physical activity, monitor blood glucose levels regularly, take medication consistently, and perform foot care—collectively referred to as diabetes mellitus self-management. This means that the higher the levels of self-acceptance of people with diabetes distress, the better the self-management will be [17]. Health professionals should pay more attention to the patient’s condition in detail regarding diabetes distress because this condition will have an impact on the patient’s ability to engage in effective self-management or lack thereof. Strengthening self-acceptance will help diabetes patients focus more on themselves and their health condition, thereby reducing diabetes distress and allowing them to concentrate more on implementing self-management strategies.
Conclusion
Based on the results of the study, self-acceptance and self-management had a relationship with diabetes distress at Roemani Semarang Hospital, Indonesia. It is expected that patients will be able to accept themselves and engage in self-management practices, such as regulating diet and lifestyle, to decrease diabetes distress. Health professionals are encouraged to pay more attention to the psychological condition of patients with diabetes mellitus during treatment and to provide training in self-management to help reduce diabetes distress in the future.
Ethical Considerations
Compliance with ethical guidelines
Each participant received the study’s explanation (study’s goal and procedures) before completing the questionnaires. Participants were also given a chance to process and ask for clearer explanations for their doubts to facilitate informed consent. Participation was voluntary, and participants had the right to withdraw from the study at any time. Ethical approval was granted by the Health Research Ethics Committee of the Faculty of Nursing and Health Sciences at Universitas Muhammadiyah Semarang, Semarang, Indonesia (No.: 306/KE/11/2023).
Funding
This study was financially supported by the Universitas Muhammadiyah Semarang, Semarang, Indonesia.
Authors' contributions
Conceptualization, methodology, formal analysis, investigation, and writing the original draft: Mohamad Rizky Wahyudi; Data curation, resources, visualization, project administration, review and editing: Satriya Pranata; Validation, supervision, and funding acquisition: Satriya Pranata; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors want to express their gratitude to the respondents and any parties who supported this study.
References
- Zahrun Ni'mah F, Aisah S. Aplication of idabetes foot exercise to increase feet sensitivity patiens type II diabetes melitus. Journal of Vocational Nursing. 2023; 4(2):111-7.[DOI:10.20473/jovin.v4i2.48049]
- Pranata S, Wu SF, Wang TJ, Liang SY, Bistara DN, Chuang YH, et al. Effects of the tailored intervention program in lowering blood glucose levels and diabetes distress among patients with diabetes in Indonesia: A randomized controlled trial. Jurnal Ners. 2023; 18(1):71-9. [DOI:10.20473/jn.v18i2.42714]
- Nurisyah N, Asyikin A, Dewi R. [Edukasi Hidup Sehat Untuk Pencegahan Diabetes Dengan Pemanfaatan Serbuk Instan Kayu Secang, Kayu Manis, Jahe Dan Sereh Bagi Warga Kelurahan Sambung Jawa Kota Makassar (Indonesian)]. Jurnal Pengabdian Kefarmasian.2024; 15(2):1-4. [Link]
- Nuraini I, Febrianti N, Rabiah R, Kalla H. Hubungan diabetes distresss dengan selffcare pada diabetes mellitus. Jurnal Kolaboratif Sains. 2022; 5(5):278-83. [DOI:10.56338/jks.v5i5.2447]
- Muntamah U, Wulansari. [Prevalensi diabetes distress dan analisis faktor yang berhubungan dengan kejadian diabetes distress pada pasien dm tipe 2 di puskesmas kabupaten semarang (Indonesian)]. Media Informasi Penelitian Kabupaten Semarang. 2022; 4(1):44-53. [Link]
- kumalasari R, Asriyadi F. The relationship between self management and self esteem in diabetes mellitus patients in the Palaran Samarinda. Borneo Studies and Research. 2020; 1(3):1490-5. [Link]
- Ningsih R, Deni R. Relationship between knowledge and dietary compliance in type II diabetes mellitus patients at the internal medicine polyclinic of Rsud Dr. Achmad mochtar Bukittinggi city. Jurnal Keperawatan. 2018; 15(1):12-20. [Link]
- Miller TA, Dimatteo MR. Importance of family/social support and impact on adherence to diabetic therapy. Diabetes, Metabolic Syndrome and Obesity. 2013; 6:421-6. [DOI:10.2147/DMSO.S36368] [PMID] [PMCID]
- Inonu VF, Wulan D, Sumekar RW, Rodiani R. Hubungan penerimaan diri dengan self-management diabetes mellitus pada peserta prolanis di puskesmas kedaton bandarlampung. Jurnal Majority. 2018; 7(3):90-4. [Link]
- Saminan S, Rabbany N, Aini Z, Zulkarnain Z, Murzalina C. The relationship between diabetes self-management and blood glucose control in patients with type 2 diabetes mellitus in ulee kareng subdistrict, banda aceh. The International Journal of Tropical Veterinary and Biomedical Research. 2020; 5(2):40-9. [DOI:10.21157/ijtvbr.v5i2.20487]
- Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. The diabetes self-management questionnaire (DSMQ): Development and evaluation of an instrument to assess diabetes self-care activities associated with glycaemic control. Health and Quality of Life Outcomes. 2013; 11(138):1-4. [DOI:10.1186/1477-7525-11-138]
- Febertha Atuh C, Datak G, Utama NR, Inung Sylvia E. The relationship between self-esteem and diabetes distress in type 2 diabetes mellitus patients at pahandut community health center Palangka Raya City. Journal of Midwifery and Nursing. 2024; 6(1):71-7. [Link]
- Adiputra AB, Arifuddin F. Karakteristik dan faktor yang berhubungan dengan distress diabetes penderita DM di Wilayah Kerja Puskesmas Balangnipa Sinjai. Jurnal Kesehatan Panrita Husada. 2021; 6(1):49–59. [Link]
- Pranata S, Huang XY. Self-management experience of patient with type 2 diabetes in sumbawa besar, west nusa tenggara: A qualitative study. Nursing Current. 2020; 8(1):19-33. [DOI:10.19166/nc.v8i1.2717]
- Nugroho FC, Banase EF, Hamu AH, Making MA, Vanchapo AR, Nubi LB, et al. Hubungan antara diabetes distress dengan self care pasien diabetes mellitus tipe II puskesmas oesapa kota kupang. Jurnal Ners. 2024; 8(1):658-66. [DOI:10.31004/jn.v8i1.20248]
- Summers-Gibson L. The relationships between diabetes self-care, diabetes time management, and diabetes distress in women with type 2 diabetes mellitus. The Science of Diabetes Self-Management and Care. 2021; 47(4):245-54. [DOI:10.1177/26350106211014438] [PMID]
- Fitriani M, Muflihatin SK. Hubungan penerimaan diri dengan manajemen diri pada penderita diabetes mellitus tipe ii di wilayah kerja puskesmas palaran kota samarinda. Borneo Studies and Research. 2020; 2(1):144-50. [Link]
Type of Study: Orginal Article |
Subject:
● Psychosocial Health
Received: 2024/09/25 | Accepted: 2024/11/30 | Published: 2025/05/30
Received: 2024/09/25 | Accepted: 2024/11/30 | Published: 2025/05/30
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |