Volume 15, Issue 3 (May & June 2025)
J Research Health 2025, 15(3): 247-256 |
Back to browse issues page
Ethics code: 430/KE/06/2024
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pranata S, Armiyati Y, Khoiriyah K, Andaresta Putri N, Rosmayanti M, Seprian D. Diabetes Patients' Preferences and Expectations for Health Services to Prevent Diabetes Complications: A Qualitative Study. J Research Health 2025; 15 (3) :247-256
URL: http://jrh.gmu.ac.ir/article-1-2629-en.html
URL: http://jrh.gmu.ac.ir/article-1-2629-en.html
Satriya Pranata1 

 , Yunie Armiyati2
, Yunie Armiyati2 

 , Khoiriyah Khoiriyah2
, Khoiriyah Khoiriyah2 

 , Novita Andaresta Putri2
, Novita Andaresta Putri2 

 , Maya Rosmayanti2
, Maya Rosmayanti2 

 , Dwin Seprian3
, Dwin Seprian3 




 , Yunie Armiyati2
, Yunie Armiyati2 

 , Khoiriyah Khoiriyah2
, Khoiriyah Khoiriyah2 

 , Novita Andaresta Putri2
, Novita Andaresta Putri2 

 , Maya Rosmayanti2
, Maya Rosmayanti2 

 , Dwin Seprian3
, Dwin Seprian3 


1- Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Indonesia. , satriya.pranata@unimus.ac.id
2- Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Indonesia.
3- Nurse Professional Study Program, Faculty of Medicine, Universitas Tanjungpura, Pontianak, Indonesia.
2- Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Indonesia.
3- Nurse Professional Study Program, Faculty of Medicine, Universitas Tanjungpura, Pontianak, Indonesia.
Full-Text [PDF 589 kb]
(701 Downloads)
| Abstract (HTML) (3187 Views)
Full-Text: (899 Views)
Introduction
Diabetes mellitus is a group of metabolic disorders characterized by elevated blood glucose levels (hyperglycemia) due to defects in insulin secretion, insulin action, or both [1]. A total of 537 million people suffer from diabetes, and this number is projected to reach 643 million in 2030, and 783 million in 2045. The number of diabetes sufferers (aged 20-79) in Indonesia experienced a significant increase from 5.65 million in 2000 to 19.47 million by 2021. It is estimated that this number will increase to 23.33 million by 2030 [2]. The increase in the number of diabetes patients is also accompanied by an increase in the incidence of diabetes-related complications. Complications that often occur due to diabetes include heart and kidney diseases [3]. According to data from the National Health Insurance of Indonesia, there was an increase in total claim costs for national health insurance related to diabetes and its complications, rising from IDR 4.9 trillion in 2018 to IDR 6.4 trillion in 2022 [2]. Appropriate efforts are needed to overcome the increasing number of diabetes sufferers and their complications in the future.
The self-management practice was effective in reducing the risk of complications, especially heart and kidney complications due to diabetes [4, 5]. Self-management includes managing diet, exercise, medication, education, and independent glucose monitoring. If self-management practice can be implemented consistently, blood glucose levels can be stable, thereby reducing the risk of complications in the future [3].
The complications resulting from diabetes are currently dangerous and life-threatening. Ordinary people often believe that the management of diabetes simply involves reducing sugar consumption [6]. However, many additional measures must be taken in the management of this disease. So far, the government, through health agencies, has implemented programs to control diabetes complications [7, 8]. The programs implemented by the government have not been optimal in achieving their desired goals. The lack of optimal implementation is primarily due to a failure to understand the expectations of diabetes sufferers regarding health services [9].
Health professionals have made efforts to improve self-management by providing health education [10, 11]. However, the educational approach still relies on a population-based strategy. Health professionals generally provide health education using leaflets or posters, which are the same for all diabetes patients, even though each diabetes patient has different problems and clinical conditions [12, 13]. The population-based approach was ineffective because it does not directly address the personal issues faced by each diabetes patient [14].
A personalized approach means that medical and nursing interventions are tailored to each patient's clinical problems and preferences precisely [15]. When patient preferences are respected, patients feel more involved in medical and nursing intervention programs, and they feel more appreciated and cared for. As a result, they pay more attention to health workers’ instructions and feel a greater sense of responsibility in self-management [16, 17].
A study shows that important points regarding general patient preferences in diabetes care include the need for information about the types of complications caused by diabetes, the location of endocrinology specialist doctors near their homes, and clarity on what treatments they need and do not need. It is also important to pay attention to the distress patients experience due to diabetes. Health workers also need to carry out health training and education for families, and for the patients themselves. Additionally, information related to kidney disease and heart failure needs to be provided in detail, as it is not yet clearly understood, including guidance on safe physical activity or exercise [17]. Previous studies have been limited in exploring the preferences of diabetes patients in general across various countries. Therefore, it is necessary to investigate the preferences of diabetes patients in Indonesia due to the cultural diversity of each country.
With the findings from research regarding diabetes patients' preferences for diabetes care, it is also necessary to explore more deeply the preferences of diabetes patients for health services aimed at preventing heart and kidney complications [17, 18]. The information obtained from this study will highlight the unique preferences of diabetes patients in preventing heart and kidney complications, which are influenced by their distinct cultural backgrounds. With this information, health workers in Indonesia or other countries in Asia with similar cultures can better understand patients’ wishes and accommodate them in programs that align with their preferences.
Methods
Study design
This qualitative study used a phenomenological approach. The research was conducted using in-depth interviews with each respondent to explore more deeply the meaning of patients' diabetes preferences for health services aimed at preventing heart and kidney complications.
Time and place of study
Data collection was conducted from July to August 2024 in the working area of the Kedungmundu Health facility in Semarang, Central Java, Indonesia.
Sample
The population of this study was all diabetes patients living in the working area of the Kedungmundu Health Center, Semarang City, Central Java, Indonesia. The sample was recruited by purposive sampling technique with the following criteria: Diabetes mellitus patients residing in the Kedungmundu Health Facility’s working area who are not suffering from heart or kidney complications. The number of participants was 25 adults aged between 30 and 50 years.
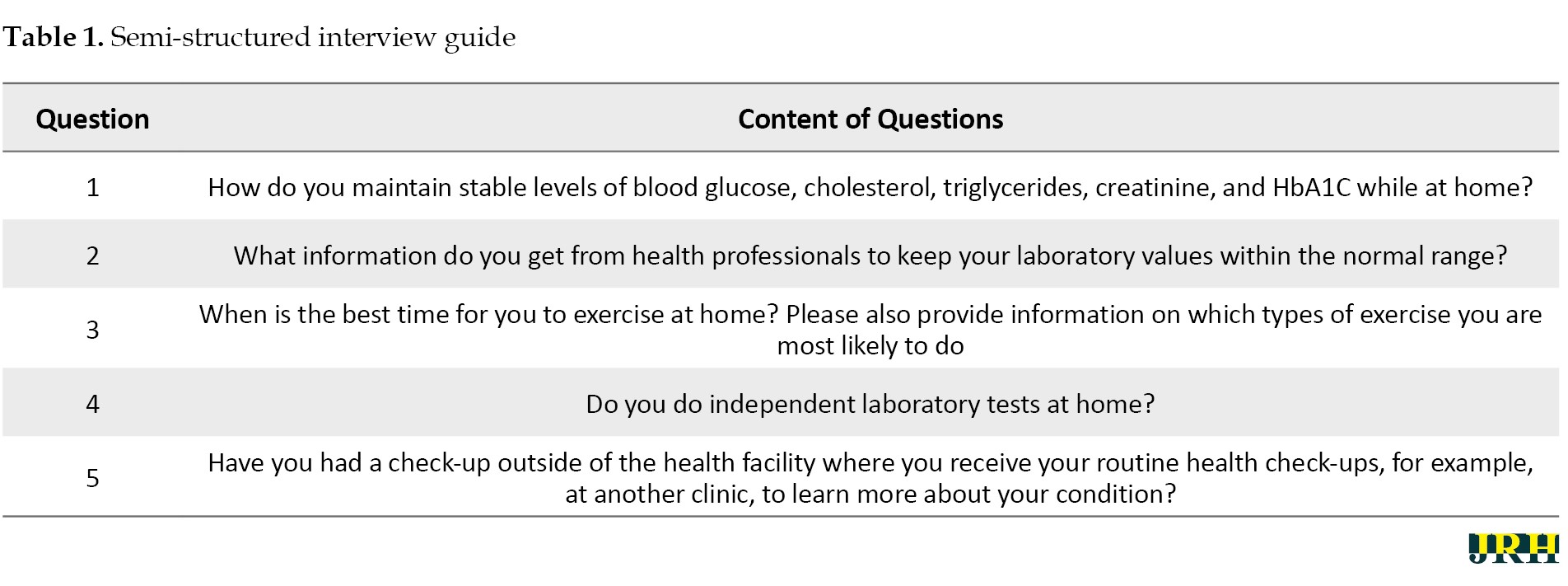
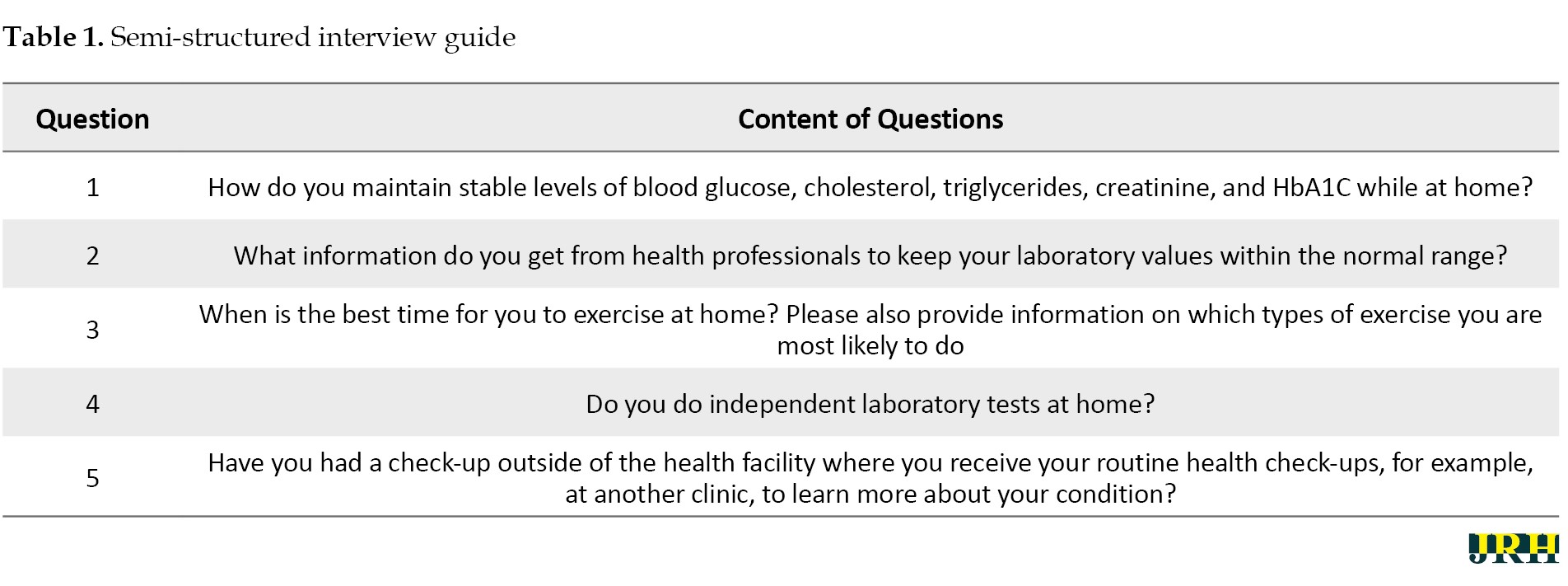
Data collection procedure
The researcher introduced himself and asked for the patient's willingness to participate in the interview. During the interview process, the researcher built a comfortable situation and asked questions according to the interview guidelines presented in Table 1.
The researcher collected data on diabetes patients at community health centers and then selected respondents who met the inclusion criteria. Respondents were asked for their willingness to be interviewed at a location of their choice. Respondents were willing to interview at their homes due to privacy reasons.
Data validity
The determination of data validity in this study followed four criteria: Credibility, which refers to trust in the accuracy of the data and its interpretation. In this study, the researcher rechecked the verbatim transcripts to data conformity between the recordings and the transcripts. The researcher then presented the interview transcripts to each respondent and sought their approval. Afterward, the researcher asked the respondents if any data needed to be added or if they agreed with the content. During the process of data collection, writing transcripts, data analysis, and theme determination, the researcher consulted with other members of the research team [19].
Data analysis
The researcher analyzed the interview results according to the Colaizzi phenomenological analytic method [19]. This method consists of seven steps, as follows: 1) Read all protocols to gain an understanding of them; 2) Review each protocol and extract significant statements; 3) Clarify the meaning of each significant statement; 4) Organize the formulated meanings into clusters of themes; 5) Integrate the results into a comprehensive description of the phenomenon under study; 6) Formulate an exhaustive description of the phenomenon in as clear a statement of identification as possible; 7) Ask participants about the findings thus far as a final validating step. This study validates the data from interviews by triangulation following ways: 1) Comparing observation data with interview data; 2) Comparing what people say about the research situation with what was done throughout the study; 3) Comparing interview results with the contents of an existing document; 4) Comparing interview results with relevant sources.
Results
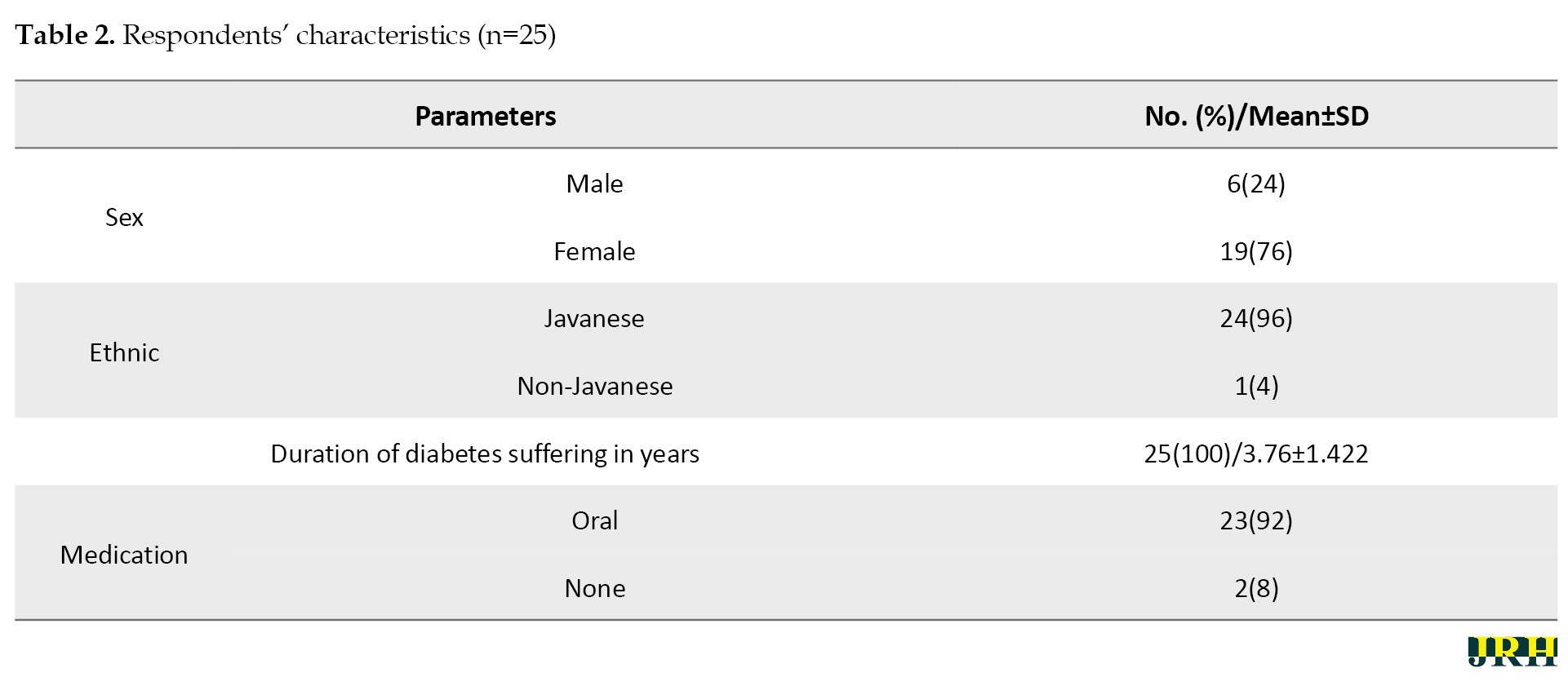
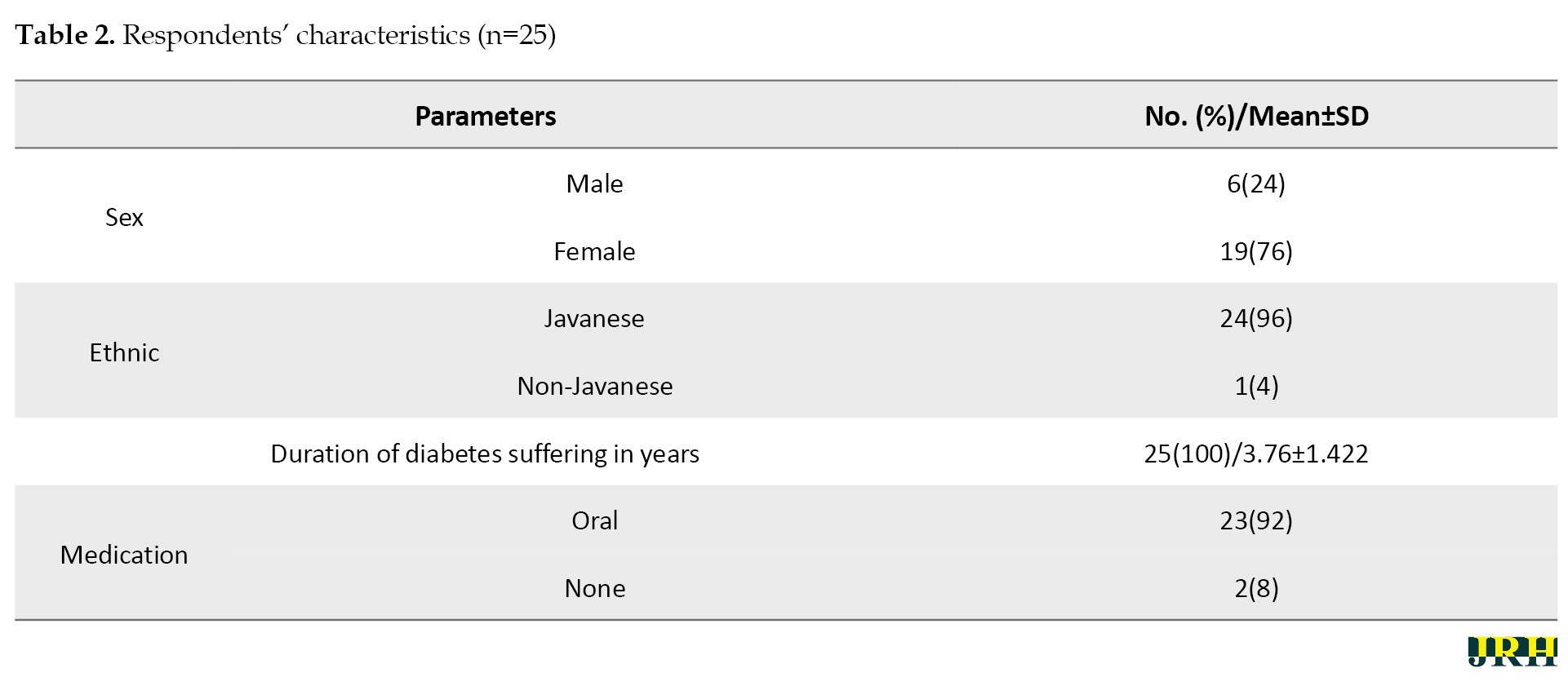
The majority of respondents were women (76%), predominantly from the Javanese ethnicity (96%), had suffered from diabetes for more than three years, and 92% regularly consumed oral medication (Table 2).
Six emergent themes were identified in this study: Diet pattern adjustment, expectations for health information, information on choosing the right medication, need for information on the right type of exercise, biochemical and hemodynamic control, and expectations for healthcare services.
Dietary pattern adjustment
Several health professionals in Indonesia stated that they have educated patients about how to regulate food portions. However, due to minimal levels of knowledge, motivation, and family support, many patients struggle to be consistent in limiting their food portions.
Limiting food portions
Participant 1 (P1) stated to keep food portions small, eat little rice, and include lots of vegetables while continuing to eat fruit and maintaining regular meals for breakfast, lunch, and dinner, along with a mindful diet. P2 mentioned that I still eat one and a half ladles of rice, twice a day, in the morning at 10 and in the afternoon at 5. P3 indicated that I reduce rice portions and sometimes eat two times and sometimes three times a day. P4 stated that I usually eat three times a day, in the morning, afternoon, and evening. P9 noted that I reduce food portions and avoided eating if I want to sleep.
Increasing protein consumption
P13 stated that I include side dishes of tempeh, tofu, and sea fish, and only a little chicken. P12 mentioned that I am looking for alternative sources of carbohydrates, such as eating potatoes and more meat.
Looking for alternative carbohydrate sources
P21 indicated that I reduce my rice consumption and replace it with sweet potatoes. P17 stated that sometimes I feel like eating rice, but I replace it with brown rice, even though it is not tasty; I do this because I want to stay healthy. P23 noted that sometimes I do not eat enough rice but consume more boiled corn to maintain my energy levels.
Limiting sugar consumption
P4 stated that I am reducing sweet drinks but use Tropicana Slim (a sugar product with less glucose) for sweetness and often drink mineral water. P7 mentioned that I cook without sugar and do not consume sweet products. P15 indicated that I never drink sweet products or water with high glucose.
Expectations for health information
Diabetes patients must be provided with information to recognize the signs and symptoms of diabetes emergencies. Therefore, if an emergency or complications occur, patients and their families immediately go to the nearest health service.
Need for information regarding paresthesia of the extremities
Doctors recommend attending prolanis (health program from primary healthcare) events so that patients can have regular check-ups. If there is counseling, they will inform patients that if they feel numbness, they can perform exercises such as squeezing paper; it is not necessary to do it for long, but the important thing is to exercise regularly, according to P9.
Need for information in case of an emergency
P9 stated that I have never had a health check other than at a health center, but if it is urgent, I check at the laboratory clinic. P24 mentioned that I have never had a health check outside the health center; if I am dropped off, I go directly to the hospital.
Need for information on doctors practicing near patient residence
“If there are new complaints, I go to the nearest clinic/doctor, noted P8.
Information on choosing the right medication
Alternative treatments for lowering blood glucose are obtained by patients based on information from the cultural practices they adopt. If the management goals have not been achieved with this first step, the patient’s therapy can be combined with pharmacological measures in the form of oral hypoglycemic drug therapy, insulin therapy, or a combination of both, as recommended by health professionals.
Pharmacological drug management
P6 stated that I take diabetes medicine in the morning before eating and blood pressure medicine in the evening. P11 indicated that I take medicine in the morning before eating and at mealtime. P12 mentioned that I take medicine regularly after dawn and after eating. P13 stated that I keep taking my medicine. P16 mentioned that I take medicine every day. P18 stated that I take my medicine. P24 noted that I take my medicine until it runs out.
Alternative non-pharmacological drug management
One participant stated that I drink juice and papaya leaf decoction mixed with bitter melon (P14). Another participant mentioned that I often drink papaya root (P15). A different participant indicated that I drink boiled water from kenikir (the leaf of a traditional medicine plant) (P20).
Need for information on the right type of exercise
Nurses, as educators, play an important role in providing appropriate information to diabetes patients about the management of this disease, including increasing the patient's ability to assess that he or she has the power to achieve desired outcomes. However, sometimes the physical exercise information provided by health workers does not take into account the patient's health condition, leading to non-compliance with physical exercise due to feelings of fatigue.
Light exercise options
One participant stated that most people walk to the mosque and then return home (P2). Another participant mentioned that I exercise by walking up and down stairs (P6). A different participant noted that I walk in front of the house, routinely every morning during COVID (P10). One participant stated that they performed stretching exercises for hands and feet for 5 minutes (P12). Another participant indicated that I do tiptoe exercises in the yard (P21). One participant mentioned that I walk for 5 to 10 minutes (P23). Lastly, a participant stated that they engage in morning walks around the house (P25).
Moderate exercise options
One participant stated that the easiest exercise is walking for 30 minutes (P1). Another participant mentioned that I walk for 30 minutes in the morning (P3). A different participant indicated that I walk from 5:30 AM to 6:00 AM routinely every day and sometimes cycle. One participant stated that I engage in morning walking exercises for approximately 10 to 20 minutes (P17). Another participant noted that I perform morning walking exercises until their body feels sweaty (P19).
Biochemical and hemodynamic control
Many diabetes sufferers only check their blood sugar when they refer to a clinic or health center for treatment. Complete blood checks and routine health checks at health services are activities that diabetes patients cannot avoid. Currently, health agencies have created a routine examination program for diabetes sufferers.
Self-monitoring biochemical and hemodynamic
One participant stated that I never checked my health independently, including sugar and high blood pressure, and did so routinely once a month; cholesterol checks are rare (P2). Another participant mentioned that I never check independently (P3). A different participant indicated that they check their sugar at home every day (P4). One participant stated that I never do an independent check (P5). Another participant noted that they never check at home (P6). One participant mentioned that I bought a glucometer to check their blood glucose level (P7). Another participant stated that they never check independently (P9, P10, and P11). One participant indicated that I check their blood sugar independently at home once a month and often check blood sugar at the pharmacy clinic (P20). Lastly, one participant stated that I often check their blood sugar at home (P21).
Laboratory monitoring in health facilities
One participant stated that there are sugar checks at health centers and complete laboratory checks every 6 months (P1). Another participant mentioned that I once had a complete laboratory check for sugar and high blood pressure, which I do routinely once a month; cholesterol checks are rare (P2). A different participant indicated that I had a check when my leg hurt, after which I was given a referral to the hospital; however, I check my sugar diligently every month and my blood pressure at the health center (P3). One participant stated that I never check their health condition outside the health center, but at the health center, I had complete checks for blood sugar, blood pressure, cholesterol, intestines, urine, HbA1C, and uric acid (P4).
Expectations for healthcare services
Apart from the role and support of health professionals, most diabetes patients currently expect services that are easy to reach and that provide support group facilitation among diabetes patients to share their experience in diabetes care and management.
Need support group facilitation
One participant stated that regular medical check-ups and monitoring in healthcare are sufficient (P1, P2, and P3). Another participant mentioned that check-ups and monitoring activities are conducted to check blood pressure and sugar (P11). A different participant indicated that there is no need for socialization and that it is better to go to the health center once a month (P15). One participant expressed a desire to go to the health center because there is a community health post near their house in the village hall to check cholesterol and conduct blood glucose tests (P16). Lastly, one participant stated that during regular medical check-ups and monitoring of healthcare events, they can meet friends with the same problem (P20).
Need for empathy and attention from health professionals
One participant stated that there is a doctor who comes to their house once a month (P1). Another participant mentioned that I would like a health worker to visit my house (P4). A different participant indicated that a doctor has come to my house, and when an officer visits, I feel happy because I feel cared for (P8). One participant stated that it would be better if a health worker visited my house once a month (P9). Another participant expressed that I also want a visit from a health worker to my house (P9). One participant mentioned that I wanted a health worker to come to my house (P14). Another participant expressed hope that there would be a visit from a health worker to my house (P17). One participant stated that I do not refuse a visit to my house (P23). Lastly, one participant mentioned that I feel happier when there is a visit to my house (P25).
Need for affordable health facilities
One participant stated that I hope there will be communication, for example, about how to maintain a diet so that blood sugar remains stable (P7). Another participant mentioned that I would be happy if the prolanis event could provide information about blood pressure and blood sugar; sometimes, there are people from Panti Wiroso Hospital who visit the village (P12). A different participant indicated that if there is a health event, it is enjoyable as long as it is not far from home; sometimes, there are integrated health posts that come (P13). One participant stated that I have never wanted to check at the hospital but is constrained by costs (P17). Another participant expressed hope that someone would come to my house to avoid the hassle of going to the health center, which would eliminate transportation costs and long queues (P18). One participant mentioned that I hoped cholesterol checks at the health center would be conducted like those at the hospital every 6 months, and I also hoped that health workers would come to my house (P21). Lastly, one participant stated that I hoped there would be routine checks from health workers (P22).
Discussion
Dietary pattern adjustment is the best way to keep blood glucose levels under control and prevent complications for diabetes patients [20, 21]. The results showed that the majority of patients who maintained a healthy diet experienced better metabolic control [22, 23]. Culture and food availability in Indonesia determine the diet pattern of diabetes patients, which can be seen from the meals chosen. In this study, the average patient adjusted their diet by reducing portions of rice and increasing their consumption of vegetables, fruits, and protein (meat, fish, and tempeh). In Indonesia, there is a cultural belief that “you have not eaten if you have not eaten rice,” even though it is known that rice contains high levels of glucose [24]. Diabetic patients can seek alternatives to rice for carbohydrate intake by consuming other carbohydrate sources, such as sweet potatoes, potatoes, and corn, as was done by the patients in this study. This research shows that patients reported consuming protein from chicken, tofu, tempeh, and seafood. The Indonesian diet is characterized by a culture that is abundant in spices and has a sweet taste, which can increase the risk of complications for diabetes sufferers. Therefore, reducing the consumption of sweet foods and drinks is an effort that patients must make [25, 26].
The second theme was the expectations of diabetes patients regarding the health information they need. Some diabetes mellitus patients have physical limitations that limit their ability to search for or use information related to their disease [27, 28]. Based on information in developing countries, the search for health information and the culture of individual and community use of health information is still limited. Health professionals in the health sector had limited or no access to primary health information sources, especially formal information sources, such as the Internet. The greatest hope for patients suffering from diabetes is information that is easy to access and understand to prevent complications [29, 30].
The third theme is information on choosing the right medication. To achieve the goal of preventing complications in diabetes patients, treatment compliance is essential. Low treatment compliance can result in increased risk of treatment costs, increased disease complications, and an increased likelihood of hospitalization [31]. A lack of information causes patients not to know the dangers of stopping their medication [32, 33]. Additionally, insufficient information about medications, especially if the drugs used do not have an immediate effect or take a long time to show results, can lead patients to feel that the medications are ineffective and to prefer alternative treatments. In general, people in Indonesia now tend to use natural ingredients to treat health problems [34, 35]. The Indonesian Ministry of Health recognizes the importance of integrating pharmacological and non-pharmacological therapies as part of the national health system, particularly in primary health services, such as promotional and preventive efforts [36].
The fourth theme is the need for information on the right type of exercise. Diabetes mellitus is generally directly related to self-management, which includes individual lifestyle management patterns, such as eating patterns and activities [37, 38]. Patients need complex treatment, one of which is physical exercise. The Indonesian Endocrinology Association formulated four pillars of treatment in preventing complications of diabetes mellitus, namely education, meal planning, pharmacological intervention, and physical exercise [36, 39]. A study shows that diabetes mellitus patients who engage in walking can offset decreases in glycemia; even just walking can positively impact optimal energy expenditure. Research proves that respondents with diabetes who exercise regularly have a diabetes management success rate of 50.9% [36].
The fifth theme is biochemical and hemodynamic control. Early detection of diabetes and monitoring of blood glucose levels are important. This is because serious complications do not occur in various organs of the body. Currently, there are blood glucose testing tools available that are easy for people to use, namely glucometers. However, it seems that there are still many people, especially people in Indonesia, who are not skilled at using them [40]. In addition, there are still many people who do not understand diabetes mellitus holistically, making it necessary to provide education about the disease and how to use a glucometer. The phenomenon that occurs is the patient's lack of compliance in controlling their blood glucose levels [40, 41]. Only 21.4% of sufferers monitored their blood sugar properly. Indonesian people have expressed several reasons why some do not comply with blood sugar control. Factors influencing this include level of education, level of knowledge, time or distance traveled, as well as family support and support from health workers. Not infrequently, diabetes mellitus patients only check their blood sugar when they go for treatment [42, 43].
The final theme of this research is expectations for healthcare services. In the last few decades, diabetes mellitus patients' expectations of professional health services have increased rapidly. Improving the quality of services in Indonesia must also be accompanied by an increase in the attention of health workers [17]. The public stated that the increased attention of health workers is related to the quality of education. The information or material provided during education does not meet patients’ expectations and needs. Patients feel that the information provided by health workers is too biomedical and is repeated over and over again at each education, making it too time-consuming and monotonous. Also, the information provided by health workers has not yet been synchronized with patients’ daily lives and culture [14, 44]. In a survey in Indonesia, 56% of diabetes sufferers felt dissatisfied with the intervention they received and felt that nurses had not provided counseling material about diabetes management as expected [45].
Conclusion
The research themes in this study consisted of diet pattern adjustment, expectations for health information, information on choosing the right medication, the need for information on the right type of exercise, biochemical and hemodynamic control, and expectations for healthcare services. The themes identified from exploring patient preferences to reduce the risk of heart and kidney disease complications in diabetic patients provide valuable information for health professionals and the government. This information can help in preparing a national health improvement program that is more optimal and targeted according to the preferences and needs of patients based on the culture in Indonesia.
Limitations and suggestions
This study has some limitations. Patient preferences cannot be generalized to all patients in various countries due to cultural differences in each country. Information from existing research still needs to be adjusted to the culture in Indonesia; therefore, this study is essential for further exploration in the future. The development of a personalized care program to reduce the risk of heart and kidney disease complications needs to be done in the future.
Ethical Considerations
Compliance with ethical guidelines
The researcher explained the purpose of the interview. After receiving an explanation, respondents were willing to fill out the consent form provided by the researcher. Before the interview process, the researcher asked the respondents for permission during the interview process to be recorded using the voice recorder. This study was approved by the ethical review board of Universitas Muhammadiyah Semarang, Semarang, India (430/KE/06/2024).
Funding
This study was financially supported by DRTPM Diktiristek, Indonesia (Code: 023.17.1.690523/2024).
Authors' contributions
Conceptualization and supervision: Satriya Pranata, Yunie Armiyati, and Khoiriyah Khoiriyah; Methodology: Satriya Pranata and Yunie Armiyati; Data collection: Novita Andaresta Putri and Maya Rosmayanti; Data analysis: Satriya Pranata, Yunie Armiyati, Khoiriyah Khoiriyah, and Dwin Seprian; Investigation and writing: Satriya Pranata, Novita Andaresta Putri, Maya Rosmayanti and Dwin Seprian.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the participants for their cooperation and DRTPM Diktiristek, Indonesia for funding support.
References
Diabetes mellitus is a group of metabolic disorders characterized by elevated blood glucose levels (hyperglycemia) due to defects in insulin secretion, insulin action, or both [1]. A total of 537 million people suffer from diabetes, and this number is projected to reach 643 million in 2030, and 783 million in 2045. The number of diabetes sufferers (aged 20-79) in Indonesia experienced a significant increase from 5.65 million in 2000 to 19.47 million by 2021. It is estimated that this number will increase to 23.33 million by 2030 [2]. The increase in the number of diabetes patients is also accompanied by an increase in the incidence of diabetes-related complications. Complications that often occur due to diabetes include heart and kidney diseases [3]. According to data from the National Health Insurance of Indonesia, there was an increase in total claim costs for national health insurance related to diabetes and its complications, rising from IDR 4.9 trillion in 2018 to IDR 6.4 trillion in 2022 [2]. Appropriate efforts are needed to overcome the increasing number of diabetes sufferers and their complications in the future.
The self-management practice was effective in reducing the risk of complications, especially heart and kidney complications due to diabetes [4, 5]. Self-management includes managing diet, exercise, medication, education, and independent glucose monitoring. If self-management practice can be implemented consistently, blood glucose levels can be stable, thereby reducing the risk of complications in the future [3].
The complications resulting from diabetes are currently dangerous and life-threatening. Ordinary people often believe that the management of diabetes simply involves reducing sugar consumption [6]. However, many additional measures must be taken in the management of this disease. So far, the government, through health agencies, has implemented programs to control diabetes complications [7, 8]. The programs implemented by the government have not been optimal in achieving their desired goals. The lack of optimal implementation is primarily due to a failure to understand the expectations of diabetes sufferers regarding health services [9].
Health professionals have made efforts to improve self-management by providing health education [10, 11]. However, the educational approach still relies on a population-based strategy. Health professionals generally provide health education using leaflets or posters, which are the same for all diabetes patients, even though each diabetes patient has different problems and clinical conditions [12, 13]. The population-based approach was ineffective because it does not directly address the personal issues faced by each diabetes patient [14].
A personalized approach means that medical and nursing interventions are tailored to each patient's clinical problems and preferences precisely [15]. When patient preferences are respected, patients feel more involved in medical and nursing intervention programs, and they feel more appreciated and cared for. As a result, they pay more attention to health workers’ instructions and feel a greater sense of responsibility in self-management [16, 17].
A study shows that important points regarding general patient preferences in diabetes care include the need for information about the types of complications caused by diabetes, the location of endocrinology specialist doctors near their homes, and clarity on what treatments they need and do not need. It is also important to pay attention to the distress patients experience due to diabetes. Health workers also need to carry out health training and education for families, and for the patients themselves. Additionally, information related to kidney disease and heart failure needs to be provided in detail, as it is not yet clearly understood, including guidance on safe physical activity or exercise [17]. Previous studies have been limited in exploring the preferences of diabetes patients in general across various countries. Therefore, it is necessary to investigate the preferences of diabetes patients in Indonesia due to the cultural diversity of each country.
With the findings from research regarding diabetes patients' preferences for diabetes care, it is also necessary to explore more deeply the preferences of diabetes patients for health services aimed at preventing heart and kidney complications [17, 18]. The information obtained from this study will highlight the unique preferences of diabetes patients in preventing heart and kidney complications, which are influenced by their distinct cultural backgrounds. With this information, health workers in Indonesia or other countries in Asia with similar cultures can better understand patients’ wishes and accommodate them in programs that align with their preferences.
Methods
Study design
This qualitative study used a phenomenological approach. The research was conducted using in-depth interviews with each respondent to explore more deeply the meaning of patients' diabetes preferences for health services aimed at preventing heart and kidney complications.
Time and place of study
Data collection was conducted from July to August 2024 in the working area of the Kedungmundu Health facility in Semarang, Central Java, Indonesia.
Sample
The population of this study was all diabetes patients living in the working area of the Kedungmundu Health Center, Semarang City, Central Java, Indonesia. The sample was recruited by purposive sampling technique with the following criteria: Diabetes mellitus patients residing in the Kedungmundu Health Facility’s working area who are not suffering from heart or kidney complications. The number of participants was 25 adults aged between 30 and 50 years.
Data collection procedure
The researcher introduced himself and asked for the patient's willingness to participate in the interview. During the interview process, the researcher built a comfortable situation and asked questions according to the interview guidelines presented in Table 1.
The researcher collected data on diabetes patients at community health centers and then selected respondents who met the inclusion criteria. Respondents were asked for their willingness to be interviewed at a location of their choice. Respondents were willing to interview at their homes due to privacy reasons.
Data validity
The determination of data validity in this study followed four criteria: Credibility, which refers to trust in the accuracy of the data and its interpretation. In this study, the researcher rechecked the verbatim transcripts to data conformity between the recordings and the transcripts. The researcher then presented the interview transcripts to each respondent and sought their approval. Afterward, the researcher asked the respondents if any data needed to be added or if they agreed with the content. During the process of data collection, writing transcripts, data analysis, and theme determination, the researcher consulted with other members of the research team [19].
Data analysis
The researcher analyzed the interview results according to the Colaizzi phenomenological analytic method [19]. This method consists of seven steps, as follows: 1) Read all protocols to gain an understanding of them; 2) Review each protocol and extract significant statements; 3) Clarify the meaning of each significant statement; 4) Organize the formulated meanings into clusters of themes; 5) Integrate the results into a comprehensive description of the phenomenon under study; 6) Formulate an exhaustive description of the phenomenon in as clear a statement of identification as possible; 7) Ask participants about the findings thus far as a final validating step. This study validates the data from interviews by triangulation following ways: 1) Comparing observation data with interview data; 2) Comparing what people say about the research situation with what was done throughout the study; 3) Comparing interview results with the contents of an existing document; 4) Comparing interview results with relevant sources.
Results
The majority of respondents were women (76%), predominantly from the Javanese ethnicity (96%), had suffered from diabetes for more than three years, and 92% regularly consumed oral medication (Table 2).
Six emergent themes were identified in this study: Diet pattern adjustment, expectations for health information, information on choosing the right medication, need for information on the right type of exercise, biochemical and hemodynamic control, and expectations for healthcare services.
Dietary pattern adjustment
Several health professionals in Indonesia stated that they have educated patients about how to regulate food portions. However, due to minimal levels of knowledge, motivation, and family support, many patients struggle to be consistent in limiting their food portions.
Limiting food portions
Participant 1 (P1) stated to keep food portions small, eat little rice, and include lots of vegetables while continuing to eat fruit and maintaining regular meals for breakfast, lunch, and dinner, along with a mindful diet. P2 mentioned that I still eat one and a half ladles of rice, twice a day, in the morning at 10 and in the afternoon at 5. P3 indicated that I reduce rice portions and sometimes eat two times and sometimes three times a day. P4 stated that I usually eat three times a day, in the morning, afternoon, and evening. P9 noted that I reduce food portions and avoided eating if I want to sleep.
Increasing protein consumption
P13 stated that I include side dishes of tempeh, tofu, and sea fish, and only a little chicken. P12 mentioned that I am looking for alternative sources of carbohydrates, such as eating potatoes and more meat.
Looking for alternative carbohydrate sources
P21 indicated that I reduce my rice consumption and replace it with sweet potatoes. P17 stated that sometimes I feel like eating rice, but I replace it with brown rice, even though it is not tasty; I do this because I want to stay healthy. P23 noted that sometimes I do not eat enough rice but consume more boiled corn to maintain my energy levels.
Limiting sugar consumption
P4 stated that I am reducing sweet drinks but use Tropicana Slim (a sugar product with less glucose) for sweetness and often drink mineral water. P7 mentioned that I cook without sugar and do not consume sweet products. P15 indicated that I never drink sweet products or water with high glucose.
Expectations for health information
Diabetes patients must be provided with information to recognize the signs and symptoms of diabetes emergencies. Therefore, if an emergency or complications occur, patients and their families immediately go to the nearest health service.
Need for information regarding paresthesia of the extremities
Doctors recommend attending prolanis (health program from primary healthcare) events so that patients can have regular check-ups. If there is counseling, they will inform patients that if they feel numbness, they can perform exercises such as squeezing paper; it is not necessary to do it for long, but the important thing is to exercise regularly, according to P9.
Need for information in case of an emergency
P9 stated that I have never had a health check other than at a health center, but if it is urgent, I check at the laboratory clinic. P24 mentioned that I have never had a health check outside the health center; if I am dropped off, I go directly to the hospital.
Need for information on doctors practicing near patient residence
“If there are new complaints, I go to the nearest clinic/doctor, noted P8.
Information on choosing the right medication
Alternative treatments for lowering blood glucose are obtained by patients based on information from the cultural practices they adopt. If the management goals have not been achieved with this first step, the patient’s therapy can be combined with pharmacological measures in the form of oral hypoglycemic drug therapy, insulin therapy, or a combination of both, as recommended by health professionals.
Pharmacological drug management
P6 stated that I take diabetes medicine in the morning before eating and blood pressure medicine in the evening. P11 indicated that I take medicine in the morning before eating and at mealtime. P12 mentioned that I take medicine regularly after dawn and after eating. P13 stated that I keep taking my medicine. P16 mentioned that I take medicine every day. P18 stated that I take my medicine. P24 noted that I take my medicine until it runs out.
Alternative non-pharmacological drug management
One participant stated that I drink juice and papaya leaf decoction mixed with bitter melon (P14). Another participant mentioned that I often drink papaya root (P15). A different participant indicated that I drink boiled water from kenikir (the leaf of a traditional medicine plant) (P20).
Need for information on the right type of exercise
Nurses, as educators, play an important role in providing appropriate information to diabetes patients about the management of this disease, including increasing the patient's ability to assess that he or she has the power to achieve desired outcomes. However, sometimes the physical exercise information provided by health workers does not take into account the patient's health condition, leading to non-compliance with physical exercise due to feelings of fatigue.
Light exercise options
One participant stated that most people walk to the mosque and then return home (P2). Another participant mentioned that I exercise by walking up and down stairs (P6). A different participant noted that I walk in front of the house, routinely every morning during COVID (P10). One participant stated that they performed stretching exercises for hands and feet for 5 minutes (P12). Another participant indicated that I do tiptoe exercises in the yard (P21). One participant mentioned that I walk for 5 to 10 minutes (P23). Lastly, a participant stated that they engage in morning walks around the house (P25).
Moderate exercise options
One participant stated that the easiest exercise is walking for 30 minutes (P1). Another participant mentioned that I walk for 30 minutes in the morning (P3). A different participant indicated that I walk from 5:30 AM to 6:00 AM routinely every day and sometimes cycle. One participant stated that I engage in morning walking exercises for approximately 10 to 20 minutes (P17). Another participant noted that I perform morning walking exercises until their body feels sweaty (P19).
Biochemical and hemodynamic control
Many diabetes sufferers only check their blood sugar when they refer to a clinic or health center for treatment. Complete blood checks and routine health checks at health services are activities that diabetes patients cannot avoid. Currently, health agencies have created a routine examination program for diabetes sufferers.
Self-monitoring biochemical and hemodynamic
One participant stated that I never checked my health independently, including sugar and high blood pressure, and did so routinely once a month; cholesterol checks are rare (P2). Another participant mentioned that I never check independently (P3). A different participant indicated that they check their sugar at home every day (P4). One participant stated that I never do an independent check (P5). Another participant noted that they never check at home (P6). One participant mentioned that I bought a glucometer to check their blood glucose level (P7). Another participant stated that they never check independently (P9, P10, and P11). One participant indicated that I check their blood sugar independently at home once a month and often check blood sugar at the pharmacy clinic (P20). Lastly, one participant stated that I often check their blood sugar at home (P21).
Laboratory monitoring in health facilities
One participant stated that there are sugar checks at health centers and complete laboratory checks every 6 months (P1). Another participant mentioned that I once had a complete laboratory check for sugar and high blood pressure, which I do routinely once a month; cholesterol checks are rare (P2). A different participant indicated that I had a check when my leg hurt, after which I was given a referral to the hospital; however, I check my sugar diligently every month and my blood pressure at the health center (P3). One participant stated that I never check their health condition outside the health center, but at the health center, I had complete checks for blood sugar, blood pressure, cholesterol, intestines, urine, HbA1C, and uric acid (P4).
Expectations for healthcare services
Apart from the role and support of health professionals, most diabetes patients currently expect services that are easy to reach and that provide support group facilitation among diabetes patients to share their experience in diabetes care and management.
Need support group facilitation
One participant stated that regular medical check-ups and monitoring in healthcare are sufficient (P1, P2, and P3). Another participant mentioned that check-ups and monitoring activities are conducted to check blood pressure and sugar (P11). A different participant indicated that there is no need for socialization and that it is better to go to the health center once a month (P15). One participant expressed a desire to go to the health center because there is a community health post near their house in the village hall to check cholesterol and conduct blood glucose tests (P16). Lastly, one participant stated that during regular medical check-ups and monitoring of healthcare events, they can meet friends with the same problem (P20).
Need for empathy and attention from health professionals
One participant stated that there is a doctor who comes to their house once a month (P1). Another participant mentioned that I would like a health worker to visit my house (P4). A different participant indicated that a doctor has come to my house, and when an officer visits, I feel happy because I feel cared for (P8). One participant stated that it would be better if a health worker visited my house once a month (P9). Another participant expressed that I also want a visit from a health worker to my house (P9). One participant mentioned that I wanted a health worker to come to my house (P14). Another participant expressed hope that there would be a visit from a health worker to my house (P17). One participant stated that I do not refuse a visit to my house (P23). Lastly, one participant mentioned that I feel happier when there is a visit to my house (P25).
Need for affordable health facilities
One participant stated that I hope there will be communication, for example, about how to maintain a diet so that blood sugar remains stable (P7). Another participant mentioned that I would be happy if the prolanis event could provide information about blood pressure and blood sugar; sometimes, there are people from Panti Wiroso Hospital who visit the village (P12). A different participant indicated that if there is a health event, it is enjoyable as long as it is not far from home; sometimes, there are integrated health posts that come (P13). One participant stated that I have never wanted to check at the hospital but is constrained by costs (P17). Another participant expressed hope that someone would come to my house to avoid the hassle of going to the health center, which would eliminate transportation costs and long queues (P18). One participant mentioned that I hoped cholesterol checks at the health center would be conducted like those at the hospital every 6 months, and I also hoped that health workers would come to my house (P21). Lastly, one participant stated that I hoped there would be routine checks from health workers (P22).
Discussion
Dietary pattern adjustment is the best way to keep blood glucose levels under control and prevent complications for diabetes patients [20, 21]. The results showed that the majority of patients who maintained a healthy diet experienced better metabolic control [22, 23]. Culture and food availability in Indonesia determine the diet pattern of diabetes patients, which can be seen from the meals chosen. In this study, the average patient adjusted their diet by reducing portions of rice and increasing their consumption of vegetables, fruits, and protein (meat, fish, and tempeh). In Indonesia, there is a cultural belief that “you have not eaten if you have not eaten rice,” even though it is known that rice contains high levels of glucose [24]. Diabetic patients can seek alternatives to rice for carbohydrate intake by consuming other carbohydrate sources, such as sweet potatoes, potatoes, and corn, as was done by the patients in this study. This research shows that patients reported consuming protein from chicken, tofu, tempeh, and seafood. The Indonesian diet is characterized by a culture that is abundant in spices and has a sweet taste, which can increase the risk of complications for diabetes sufferers. Therefore, reducing the consumption of sweet foods and drinks is an effort that patients must make [25, 26].
The second theme was the expectations of diabetes patients regarding the health information they need. Some diabetes mellitus patients have physical limitations that limit their ability to search for or use information related to their disease [27, 28]. Based on information in developing countries, the search for health information and the culture of individual and community use of health information is still limited. Health professionals in the health sector had limited or no access to primary health information sources, especially formal information sources, such as the Internet. The greatest hope for patients suffering from diabetes is information that is easy to access and understand to prevent complications [29, 30].
The third theme is information on choosing the right medication. To achieve the goal of preventing complications in diabetes patients, treatment compliance is essential. Low treatment compliance can result in increased risk of treatment costs, increased disease complications, and an increased likelihood of hospitalization [31]. A lack of information causes patients not to know the dangers of stopping their medication [32, 33]. Additionally, insufficient information about medications, especially if the drugs used do not have an immediate effect or take a long time to show results, can lead patients to feel that the medications are ineffective and to prefer alternative treatments. In general, people in Indonesia now tend to use natural ingredients to treat health problems [34, 35]. The Indonesian Ministry of Health recognizes the importance of integrating pharmacological and non-pharmacological therapies as part of the national health system, particularly in primary health services, such as promotional and preventive efforts [36].
The fourth theme is the need for information on the right type of exercise. Diabetes mellitus is generally directly related to self-management, which includes individual lifestyle management patterns, such as eating patterns and activities [37, 38]. Patients need complex treatment, one of which is physical exercise. The Indonesian Endocrinology Association formulated four pillars of treatment in preventing complications of diabetes mellitus, namely education, meal planning, pharmacological intervention, and physical exercise [36, 39]. A study shows that diabetes mellitus patients who engage in walking can offset decreases in glycemia; even just walking can positively impact optimal energy expenditure. Research proves that respondents with diabetes who exercise regularly have a diabetes management success rate of 50.9% [36].
The fifth theme is biochemical and hemodynamic control. Early detection of diabetes and monitoring of blood glucose levels are important. This is because serious complications do not occur in various organs of the body. Currently, there are blood glucose testing tools available that are easy for people to use, namely glucometers. However, it seems that there are still many people, especially people in Indonesia, who are not skilled at using them [40]. In addition, there are still many people who do not understand diabetes mellitus holistically, making it necessary to provide education about the disease and how to use a glucometer. The phenomenon that occurs is the patient's lack of compliance in controlling their blood glucose levels [40, 41]. Only 21.4% of sufferers monitored their blood sugar properly. Indonesian people have expressed several reasons why some do not comply with blood sugar control. Factors influencing this include level of education, level of knowledge, time or distance traveled, as well as family support and support from health workers. Not infrequently, diabetes mellitus patients only check their blood sugar when they go for treatment [42, 43].
The final theme of this research is expectations for healthcare services. In the last few decades, diabetes mellitus patients' expectations of professional health services have increased rapidly. Improving the quality of services in Indonesia must also be accompanied by an increase in the attention of health workers [17]. The public stated that the increased attention of health workers is related to the quality of education. The information or material provided during education does not meet patients’ expectations and needs. Patients feel that the information provided by health workers is too biomedical and is repeated over and over again at each education, making it too time-consuming and monotonous. Also, the information provided by health workers has not yet been synchronized with patients’ daily lives and culture [14, 44]. In a survey in Indonesia, 56% of diabetes sufferers felt dissatisfied with the intervention they received and felt that nurses had not provided counseling material about diabetes management as expected [45].
Conclusion
The research themes in this study consisted of diet pattern adjustment, expectations for health information, information on choosing the right medication, the need for information on the right type of exercise, biochemical and hemodynamic control, and expectations for healthcare services. The themes identified from exploring patient preferences to reduce the risk of heart and kidney disease complications in diabetic patients provide valuable information for health professionals and the government. This information can help in preparing a national health improvement program that is more optimal and targeted according to the preferences and needs of patients based on the culture in Indonesia.
Limitations and suggestions
This study has some limitations. Patient preferences cannot be generalized to all patients in various countries due to cultural differences in each country. Information from existing research still needs to be adjusted to the culture in Indonesia; therefore, this study is essential for further exploration in the future. The development of a personalized care program to reduce the risk of heart and kidney disease complications needs to be done in the future.
Ethical Considerations
Compliance with ethical guidelines
The researcher explained the purpose of the interview. After receiving an explanation, respondents were willing to fill out the consent form provided by the researcher. Before the interview process, the researcher asked the respondents for permission during the interview process to be recorded using the voice recorder. This study was approved by the ethical review board of Universitas Muhammadiyah Semarang, Semarang, India (430/KE/06/2024).
Funding
This study was financially supported by DRTPM Diktiristek, Indonesia (Code: 023.17.1.690523/2024).
Authors' contributions
Conceptualization and supervision: Satriya Pranata, Yunie Armiyati, and Khoiriyah Khoiriyah; Methodology: Satriya Pranata and Yunie Armiyati; Data collection: Novita Andaresta Putri and Maya Rosmayanti; Data analysis: Satriya Pranata, Yunie Armiyati, Khoiriyah Khoiriyah, and Dwin Seprian; Investigation and writing: Satriya Pranata, Novita Andaresta Putri, Maya Rosmayanti and Dwin Seprian.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the participants for their cooperation and DRTPM Diktiristek, Indonesia for funding support.
References
- Pranata S, Wu SV, Alizargar J, Liu JH, Liang SY, Lu YY. Precision health care elements, definitions, and strategies for patients with diabetes: A literature review. International Journal of Environmental Research and Public Health. 2021; 18(12):6535. [DOI:10.3390/ijerph18126535] [PMID] [PMCID]
- Kemenkes RI. Profil kesehatan indonesia; Jakarta: Kementerian Kesehatan Republik Indonesia Tahun; 2021. [Link]
- Pranata S, Shing LC, Vranada A, Chun LY, Armiyati Y, Khoiriyah K. The implementation of precision personalized care to improve diabetes patients’ self-management at taipei veteran general hospital: An observational study. Bali Medical Journal. 20210; 10(3):1304-7. [DOI:10.15562/bmj.v10i3.2902]
- Li H, Jiang YF, Lin CC. Factors associated with self-management by people undergoing hemodialysis: A descriptive study. International Journal of Nursing Studies. 2014; 51(2):208-16. [DOI:10.1016/j.ijnurstu.2013.05.012] [PMID]
- Sriprachot N, Seangpraw K, Ong-Artborirak P. Health literacy, self-care behaviors, and biochemical parameters among hypertensive patients with renal complications in the tai lue ethnic community of Thailand. Vascular Health and Risk Management. 2024; 20:97-107. [DOI:10.2147/VHRM.S450775] [PMID] [PMCID]
- Kueh YC, Morris T, Ismail AA. The effect of diabetes knowledge and attitudes on self-management and quality of life among people with type 2 diabetes. Psychology, Health & Medicine. 2017; 22(2):138-44. [DOI:10.1080/13548506.2016.1147055] [PMID]
- Khowaja MA, Rozi S, Sawani S, Ahmed A. Factors associated with Diabetes Empowerment among patients with type 2 diabetes, at OPD setting, Karachi, Pakistan. Scientific Reports. 2023; 13(1):7165. [DOI:10.1038/s41598-023-34385-4] [PMID] [PMCID]
- Singh P, Seth A. Transition of care of pediatric patients with special needs to adult care settings: Children with diabetes mellitus and other endocrine disorders. Indian Journal of Pediatrics. 2023; 90(11):1134-41. [DOI:10.1007/s12098-023-04780-w] [PMID]
- Papatheodorou K, Banach M, Bekiari E, Rizzo M, Edmonds M. Complications of diabetes 2017. Journal of Diabetes Research. 2018; 2018:3086167. [DOI:10.1155/2018/3086167] [PMID] [PMCID]
- Singh A, Nichols M. Nurse-led education and engagement for diabetes care in Sub-Saharan Africa: Protocol for a mixed methods study. JMIR Research Protocols. 2020; 9(6):e15408. [DOI:10.2196/15408] [PMID] [PMCID]
- Grady PA, Gough LL. Self-management: A comprehensive approach to management of chronic conditions. American Journal of Public Health. 2014; 104(8):e25-31. [DOI:10.2105/AJPH.2014.302041] [PMID] [PMCID]
- Pranata S, Vivienne Wu SF, Tiffany Wang TJ, Liang SY, Chuang YH, Lu KC, et al. Discovering elements and developing strategies to implement the tailored care education for patients with diabetes through a systematic review. Nurse Media Journal of Nursing. 2022; 12:75-87. [DOI:10.14710/nmjn.v12i1.44336]
- Hertroijs DFL, Elissen AMJ, Brouwers MCGJ, Schaper NC, Ruwaard D. Relevant patient characteristics for guiding tailored integrated diabetes primary care: A systematic review. Primary Health Care Research & Development. 2018; 19(5):424-47. [DOI: 10.1017/S146342361800004X]
- Pranata S, Vivienne Wu SF, Armiyati Y, Khoiriyah K, Shing LC, Liu JH. Implementing precision health care program at hospitals in Indonesia. Journal of Research and Health. 2023; 13(6):457-66. [DOI:10.32598/JRH.13.6.2183.3]
- Pranata S, Wu SF, Wang TJ, Liang SY, Bistara DN, Chuang YH, et al. Effects of the tailored intervention program in lowering blood glucose levels and diabetes distress among patients with diabetes in Indonesia: A randomized controlled trial. Jurnal Ners. 2023; 18(1):71-9. [DOI:10.20473/jn.v18i1.42714]
- Tinetti ME, Esterson J, Ferris R, Posner P, Blaum CS. Patient priority-directed decision making and care for older adults with multiple chronic conditions. Clinics in Geriatric Medicine. 2016; 32(2):261-75. [DOI:10.1016/j.cger.2016.01.012] [PMID]
- Pranata S, Wu SF, Armiyati Y, Shing LC, Liu JH. Patient preferences in diabetes care: A bibliometric analysis. Babcock University Medical Journal. 2023; 6(2):237-46. [DOI:10.38029/babcockuniv.med.j..v6i2.314]
- Hu L, Jin X, Li Y, Yang D, Zhang Z, He X, et al. A mixed methods assessment of self- management needs and preferences of people with type 2 diabetes mellitus in China. Patient Preference and Adherence. 2023; 17:653-66. [DOI:10.2147/PPA.S394003] [PMID] [PMCID]
- Morrow R, Rodriguez A, King N. Colaizzi’s descriptive phenomenological method. The Psychologist. 2015; 28(8):643-4. [Link]
- Fan Y, Zhao L, Deng Z, Li M, Huang Z, Zhu M, et al. Non-linear association between Mediterranean diet and depressive symptom in U.S. adults: A cross-sectional study. Front Psychiatry. 2022; 13:936283. [DOI:10.3389/fpsyt.2022.936283] [PMID] [PMCID]
- Forouhi NG, Misra A, Mohan V, Taylor R, Yancy W. Dietary and nutritional approaches for prevention and management of type 2 diabetes. BMJ. 2018; 361:k2234. [DOI:10.1136/bmj.k2234] [PMID] [PMCID]
- Berkowitz SA, Delahanty LM, Terranova J, Steiner B, Ruazol MP, Singh R, et L. Medically tailored meal delivery for diabetes patients with food insecurity: A randomized cross-over trial. J Gen Intern Med. 2019; 34(3):396-404. [DOI:10.1007/s11606-018-4716-z] [PMID] [PMCID]
- Choi TST, Walker KZ, Palermo C. Culturally tailored diabetes education for Chinese patients: A qualitative case study. Journal of Transcultural Nursing. 2017; 28(3):315-23. [DOI:10.1177/1043659616677641] [PMID]
- Pranata S, Wu SF, Purwadi H, Putra DG, Wulandari H, Soesanto E. Exploring of self-management experience among health professional survivors from coronavirus disease 2019 in West Nusa Tenggara, Indonesia. Open Access Macedonian Journal of Medical Sciences. 2021; 9(G):19-27. [DOI:10.3889/oamjms.2021.6443]
- Pranata S, Huang XY. Self-management experience of patient with diabetes mellitus type 2. Nursing Current. 2020; 24:7792-801. [DOI:10.19166/nc.v8i1.2717]
- Widayanti AW. Understanding health-seeking behaviours of people in Indonesia; and developing, piloting, and evaluating a culturally appropriate intervention for people with diabetes [doctoral thesis]. Dunedin: University of Otago; 2019. [Link]
- Zampogna G. Physical exercise as treatment for type 2 diabetes distal symmetric polyneuropathy: A systematic review of randomized and controlled studies. Journal of Diabetes Mellitus. 2022; 12(3):167-86. [DOI:10.4236/jdm.2022.123014]
- Dean E. Academy of plant-based physical therapy: Overdue to address a nutrition crisis with a transformative population approach. Journal of Physical Therapy Science. 2023; 35(9):645-58. [DOI:10.1589/jpts.35.645] [PMID] [PMCID]
- Raja SM, Seyoum Y. Intradialytic complications among patients on twice-weekly maintenance hemodialysis: An experience from a hemodialysis center in Eritrea. BMC Nephrology. 2020; 21(1):163. [DOI:10.1186/s12882-020-01806-9] [PMID] [PMCID]
- Nijpels G, Beulens JW, van der Heijden AA, Elders PJ. Innovations in personalised diabetes care and risk management. European Journal of Preventive Cardiology. 2019; 26(2_suppl):125-32. [DOI:10.1177/2047487319880043] [PMID]
- Alanazi M. Determinants of successful diabetes self-management behaviors among women of Arab descent with Type 2 Diabetes. Primary Care Diabetes. 2021; 15(2):306-13. [DOI:10.1016/j.pcd.2020.10.009] [PMID]
- Paul A, Kumar M, Das P, Guha N, Rudrapal M, Zaman MK. Drug repurposing - A search for novel therapy for the treatment of diabetic neuropathy. Biomedicine & Pharmacotherapy. 2022; 156:113846. [DOI:10.1016/j.biopha.2022.113846] [PMID]
- Nirenjen S, Narayanan J, Tamilanban T, Subramaniyan V, Chitra V, Fuloria NK, et al. Exploring the contribution of pro-inflammatory cytokines to impaired wound healing in diabetes. Frontiers in Immunology. 2023; 14:1216321. [DOI:10.3389/fimmu.2023.1216321] [PMID] [PMCID]
- Rayate AS, Nagoba BS, Mumbre SS, Mavani HB, Gavkare AM, Deshpande AS. Current scenario of traditional medicines in management of diabetic foot ulcers: A review. World Journal of Diabetes. 2023; 14(1):1-16. [DOI:10.4239/wjd.v14.i1.1] [PMID] [PMCID]
- Liu FS, Li Y, Guo XS, Liu RC, Zhang HY, Li Z. Advances in traditional Chinese medicine as adjuvant therapy for diabetic foot. World Journal of Diabetes. 2022; 13(10):851-60. [DOI:10.4239/wjd.v13.i10.851] [PMID] [PMCID]
- Ligita T, Wicking K, Francis K, Harvey N, Nurjannah I. How people living with diabetes in Indonesia learn about their disease: A grounded theory study. Plos One. 2019; 14(2):e0212019. [DOI:10.1371/journal.pone.0212019] [PMID] [PMCID]
- Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Hess Fischl A, et al. Diabetes self-management education and support in type 2 diabetes: A joint position statement of the american diabetes association, the american association of diabetes educators, and the academy of nutrition and dietetics. Diabetes Care. 2015; 38(7):1372-82. [DOI:10.2337/dc15-0730] [PMID]
- Badriah S, Sahar J, Gunawijaya J, et al. Pampering older people with diabetes in Sundanese culture: A qualitative study. Enfermería Clínica. 2019; 29(2):733-8. [DOI:10.1016/j.enfcli.2019.04.111]
- Kurnia AD, Amatayakul A, Karuncharernpanit S. Predictors of diabetes self-management among type 2 diabetics in Indonesia: Application theory of the health promotion model. International Journal of Nursing Sciences. 2017; 4(3):260-5. [DOI:10.1016/j.ijnss.2017.06.010] [PMID] [PMCID]
- Weiner M, Adeoye P, Boeh MJ, Bodke K, Broughton J, Butler AR, et al. Continuous glucose monitoring and other wearable devices to assess hypoglycemia among older adult outpatients with diabetes mellitus. Applied Clinical Informatics. 2023; 14(1):37-44. [DOI:10.1055/a-1975-4136] [PMID] [PMCID]
- Cimo A, Dewa CS. Tailoring diabetes education to meet the needs of adults with type 2 diabetes and mental illness: Client and health-care provider perspectives from an exploratory pilot study. Canadian Journal of Diabetes. 2019; 43(6):421-8.e3. [DOI:10.1016/j.jcjd.2018.09.008] [PMID]
- Skoufalos A, Thomas R, Patel R, Mei C, Clarke JL. Continuous glucose monitoring: An opportunity for population-based diabetes management. Population health management. 2022; 25(5):583-91. [DOI:10.1089/pop.2022.0196] [PMID]
- Hermanns N, Ehrmann D, Shapira A, Kulzer B, Schmitt A, Laffel L. Coordination of glucose monitoring, self-care behaviour and mental health: Achieving precision monitoring in diabetes. Diabetologia. 2022; 65(11):1883-94. [DOI:10.1007/s00125-022-05685-7] [PMID]
- Pranata S, Wu SF, Chu CH, Nugroho KH. Precision health care strategies for older adults with diabetes in Indonesia: A Delphi consensus study. Medical Journal of Indonesia. 2021; 30(3):221-7. [DOI:10.13181/mji.oa.215525]
- Kurnia AD, Amatayakul A, Karuncharernpanit S. Factors related to diabetes self- management among adults with type 2 diabetes mellitus in Malang city, East Java, Indonesia. Paper presented at: 2015 ANPOR ANNUAL Conference. 28 November 2015; Bangkok, Thailand. [Link]
Type of Study: Orginal Article |
Subject:
● Service Quality
Received: 2024/09/27 | Accepted: 2024/11/9 | Published: 2025/05/30
Received: 2024/09/27 | Accepted: 2024/11/9 | Published: 2025/05/30
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






