Volume 15, Issue 6 (Nov & Dec 2025)
J Research Health 2025, 15(6): 633-640 |
Back to browse issues page
Ethics code: IR.MUMS.FHMPM.REC.1402.135
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mousaei I, Moradi A, Taghipour A, Salari M, Nikbakht F, Mosafarkhani E. Food Insecurity and Lifestyle Factors as Predictors of Breast Cancer: An Ecological Study in Khorasan Razavi. J Research Health 2025; 15 (6) :633-640
URL: http://jrh.gmu.ac.ir/article-1-2644-en.html
URL: http://jrh.gmu.ac.ir/article-1-2644-en.html
Iman Mousaei1 

 , Amin Moradi1
, Amin Moradi1 

 , Ali Taghipour1
, Ali Taghipour1 

 , Maryam Salari2
, Maryam Salari2 

 , Fateme Nikbakht3
, Fateme Nikbakht3 

 , Ehsan Mosafarkhani4
, Ehsan Mosafarkhani4 




 , Amin Moradi1
, Amin Moradi1 

 , Ali Taghipour1
, Ali Taghipour1 

 , Maryam Salari2
, Maryam Salari2 

 , Fateme Nikbakht3
, Fateme Nikbakht3 

 , Ehsan Mosafarkhani4
, Ehsan Mosafarkhani4 


1- Department of Epidemiology, Social Determinants of Health Research Center, School of Health, Mashhad University of Medical Sciences, Mashhad, Iran.
2- Department of Biostatistics, Social Determinants of Health Research Center, School of Health, Basic Sciences Research Institute, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Department of Epidemiology, School of Health, Mashhad University of Medical Sciences, Mashhad, Iran
4- Social Determinants of Health Research Center, Mashhad University of Medical Sciences, Mashhad, Iran. ,emf1358@yahoo.com
2- Department of Biostatistics, Social Determinants of Health Research Center, School of Health, Basic Sciences Research Institute, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Department of Epidemiology, School of Health, Mashhad University of Medical Sciences, Mashhad, Iran
4- Social Determinants of Health Research Center, Mashhad University of Medical Sciences, Mashhad, Iran. ,
Full-Text [PDF 578 kb]
(214 Downloads)
| Abstract (HTML) (2153 Views)
Full-Text: (280 Views)
Introduction
Breast cancer ranks as the most common cause of cancer-related deaths among women globally, and is the second leading cause of mortality after lung cancer [1]. While mortality rates have declined in high-income countries due to advances in early detection and treatment, breast cancer incidence and mortality continue to rise in low- and middle-income countries [1]. In Asia alone, breast cancer accounts for approximately 45.4% of all cancers in women [2]. Recent reports indicate that in Iran, there are approximately 16,967 new breast cancer cases annually, resulting in 4,810 related deaths. Projections suggest a 63% increase in breast cancer cases by 2025, with an estimated 25,013 new cases expected that year [3].
The complex relationship between breast cancer and socioeconomic factors is well-documented. Higher socioeconomic status has been associated with an elevated breast cancer risk, likely due to reproductive and lifestyle factors, whereas lower socioeconomic status has been linked to late-stage diagnosis and reduced survival rates [4]. Socioeconomic factors also influence women’s access to cancer screening services and awareness of preventive measures, highlighting the importance of social determinants of health in breast cancer outcomes [5]. Social determinants, defined as the conditions in which people are born, grow, live, work, and age, as well as the broader set of forces influencing these conditions, are recognized by the World Health Organization (WHO) as critical contributors to health disparities [6]. Among these determinants, food insecurity—characterized by uncertain or insufficient access to nutritious and culturally appropriate food—has emerged as a significant public health concern globally. Approximately 852 million people are food insecure, with 9 million in developed countries and the rest in developing regions [7]. Food insecurity is particularly high in the Middle East and North Africa, affecting around 42.2% of the population, with Iran reporting a national prevalence of 49% [8]. This condition has far-reaching health impacts, including associations with chronic diseases, such as diabetes, hypertension, coronary heart disease, and mental health disorders [9, 10].
In Iran, the primary drivers of food insecurity include economic constraints and, more recently, the reimposition of international sanctions, which have sharply increased food prices without corresponding income growth [11]. Food insecurity not only affects dietary quality and nutritional status but may also hinder access to preventive healthcare services, including cancer screenings and early detection programs. These barriers can lead to delays in diagnosis and treatment, contributing to worse outcomes for individuals with cancer. Understanding the role of food insecurity, alongside other social determinants, in relation to cancer risk may provide insights for targeted interventions. Furthermore, investigating the interplay between food insecurity and other risk factors, such as obesity, smoking, and fertility rates, can help clarify their collective impact on breast cancer incidence. Given the lack of empirical evidence on this relationship in Iran, this study aimed to investigate the association between food insecurity and breast cancer incidence in Razavi Khorasan Province, providing valuable information for public health strategies aimed at reducing cancer disparities and promoting equitable health outcomes in low-resource settings.
Methods
Study design and setting
This ecological, cross-sectional study was conducted across 19 cities in Razavi Khorasan Province, Iran, using secondary data from 2017 to 2023. Data were obtained from the electronic health records maintained by Mashhad University of Medical Sciences, covering cities within the university’s healthcare jurisdiction [12]. Only cities with complete data on breast cancer incidence and predictor variables (food insecurity, obesity, smoking prevalence, diabetes prevalence, total fertility rate (TFR), and mean age) were included. Cities with incomplete or missing data for any variable were excluded from the analysis.
Study population
The study focused on all women in the region, specifically including the entire female population registered in the Mashhad University of Medical Sciences system, estimated at 2.7 million, with approximately 1.4 million women aged 30 years and older. Given the comprehensive coverage of the dataset, sampling was not performed; instead, data for the entire population were analyzed at the city level to provide a broad view of breast cancer incidence in relation to various predictors.
Age-standardized breast cancer incidence rate (ASIR)
The ASIR was calculated using data from the National Cancer Registry Center for Khorasan Razavi Province. The ASIR was computed for the period from 2017 to 2023 to ensure a comprehensive assessment of trends over multiple years. Direct age-standardization was performed using the WHO standard population as the reference.
Predictor variables
Food insecurity: Household-level food insecurity was assessed using the Persian-validated household food insecurity access scale (HFIAS), which has been previously validated for Iranian households [13, 14]. This 9-item tool assesses frequency and experience of food insecurity over the past four weeks, yielding a continuous score ranging from 0 to 27, with higher scores indicating more severe food insecurity.
Mean age: The mean age of women in each city was included as a predictor.
Overweight and obesity: Overweight and obesity prevalence (BMI ≥25 kg/m²) was calculated based on electronic health records within the Mashhad University system [12].
Diabetes: Diabetes prevalence among women over 30 was determined using ICD-10 codes (E10 and E11) from primary care visits.
Smoking: Smoking prevalence was based on self-reported data during primary healthcare assessments and recorded in the SinaEHR system, representing the percentage of women identifying as current smokers.
TFR: TFR for each city was calculated using the Spectrum software, version 3 which incorporates demographic components affecting population changes. Population data were sourced from the National Statistics Office, Civil Registration Office, and SinaEHR system census. We used the DemProj system in Spectrum to project TFR for 5 years, based on 5-year age groups. Calculations were performed separately for each city under the jurisdiction of Mashhad University of Medical Sciences.
Statistical analysis
Descriptive statistics were computed for all variables, reporting means and confidence intervals for city-level measures. Multiple linear regression was employed to examine the relationship between the ASIR and the predictor variables. Model coefficients (β), confidence intervals, and P were reported, with a significance threshold set at P<0.01 due to the large sample size. Normality of residuals and multicollinearity were tested before regression analysis to ensure assumptions were met. All analyses were conducted using STATA software, version 16 (STATA Corp, College Station, TX).
Results
Breast cancer incidence across cities
Breast cancer incidence rates varied widely across the 19 cities in Razavi Khorasan Province, ranging from 7.41 per 100,000 in Khalilabad to 41.83 per 100,000 in Shandiz. The analysis revealed significant associations between breast cancer incidence and several sociodemographic and lifestyle factors, including food insecurity, obesity, smoking prevalence, diabetes prevalence, and TFR (Table 1).
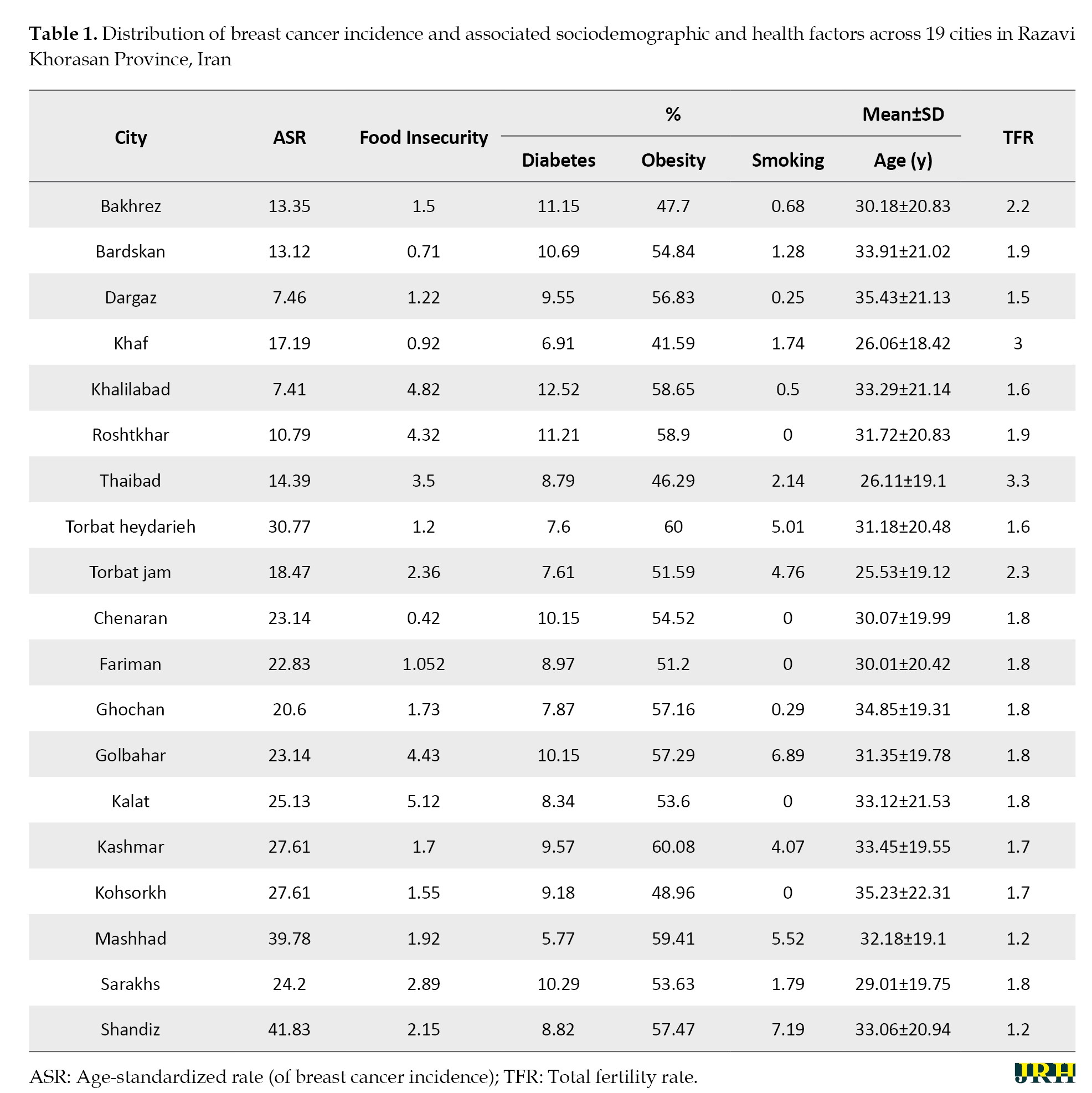
Food insecurity and breast cancer incidence
Among the 19 cities, food insecurity scores varied from 0.42 in Chenaran to 5.12 in Kalat, indicating a range of food security conditions across the region. Obesity rates were high, with Kashmar reporting the highest prevalence at 60.08%. Smoking prevalence also varied, with Shandiz showing the highest rate at 7.19% and cities like Roshtkhar and Chenaran reporting 0%. Diabetes prevalence was highest in Khalilabad (12.52%) and lowest in Khaf (6.91%). Mean age across cities ranged from 26 years in Khaf to 35 years in Kohsorkh and Dargaz. TFR was lowest in Mashhad and Shandiz (1.2) and highest in Thaibad (3.3) (Table 1).
Lifestyle factors and breast cancer risk
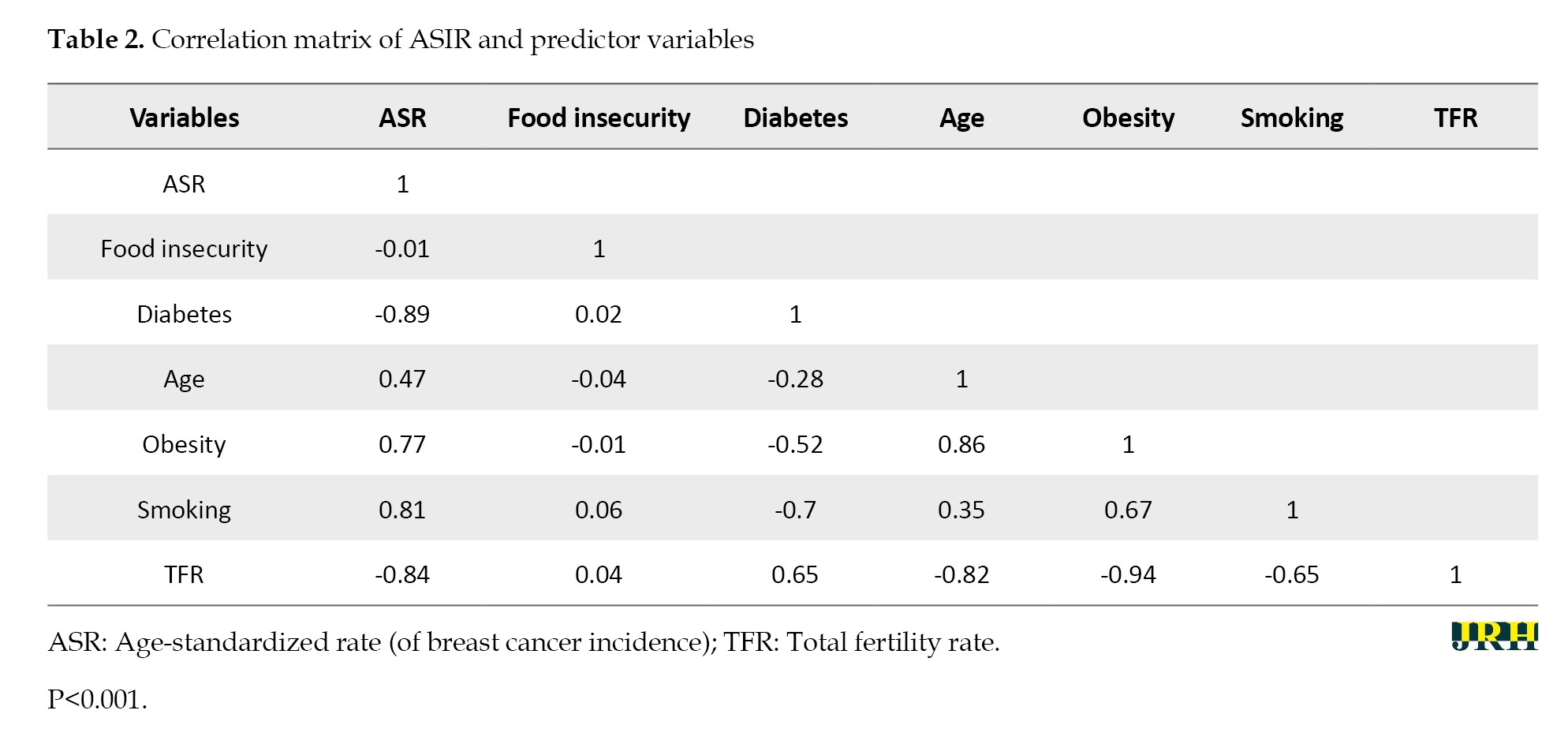
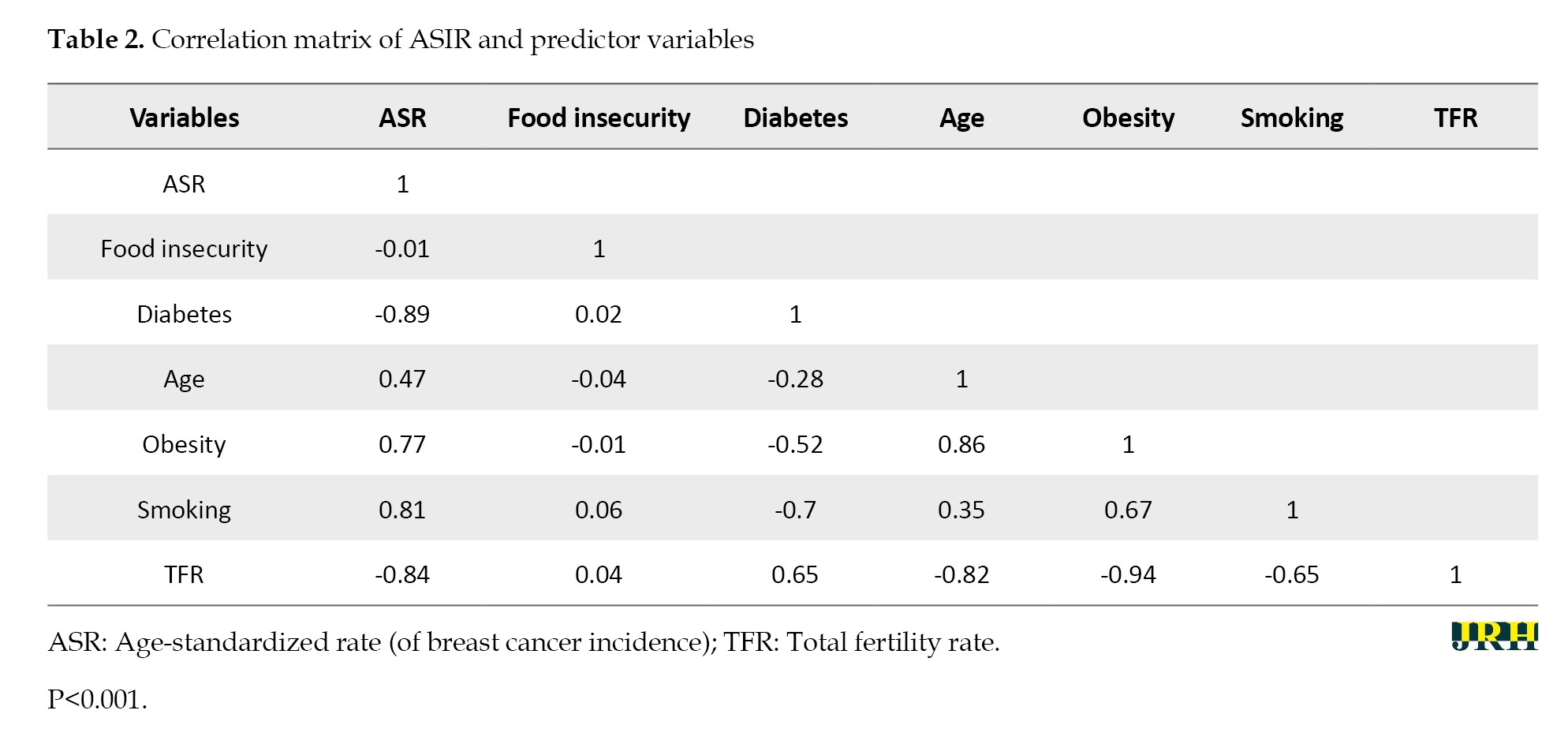
Pearson correlation analysis showed notable associations between the age-standardized incidence rate (ASIR) of breast cancer and predictor variables. A strong positive correlation was observed between breast cancer incidence and obesity (r=0.77, P<0.001) and smoking prevalence (r=0.81, P<0.001). Conversely, ASIR was inversely correlated with diabetes prevalence (r=-0.89, P<0.001) and TFR (r=-0.84, P<0.001). A weak negative correlation was noted between food insecurity and ASIR (r=-0.01, P<0.001), suggesting a complex relationship between food insecurity and breast cancer incidence in this population (Table 2).
Predictors of breast cancer
Table 3 presents the results of the multiple linear regression analysis examining predictors of the ASIR.
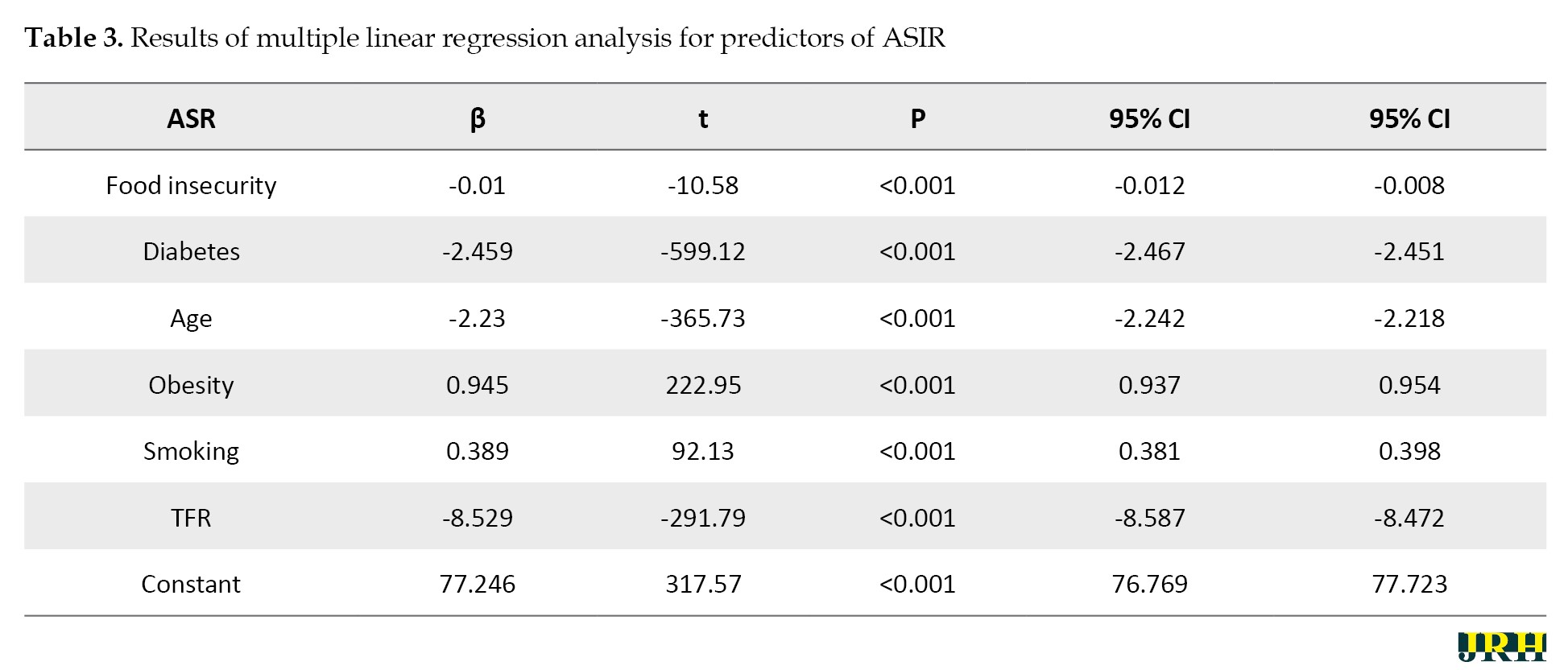
The model explained 96.3% of the variance (R²=0.96), indicating a strong fit. Food insecurity was inversely associated with ASIR (β=-0.01, 95% CI, -0.01%, -0.008%), suggesting that higher food insecurity levels correspond to a lower incidence of breast cancer. Similarly, diabetes prevalence (β=-2.46, 95% CI, -2.47%, -2.45%) and TFR (β=-8.53, 95% CI, -8.59%, -8.47%) were negatively associated with ASIR.
Conversely, obesity (β=0.95, 95% CI, 0.94%, 0.95%) and smoking prevalence (β=0.39, 95% CI, 0.38%, 0.40%) were positively associated with ASIR, indicating that higher levels of these factors are linked to increased breast cancer incidence.
Discussion
This ecological study identified several associations between food insecurity, sociodemographic factors, and ASIRs across cities in Razavi Khorasan Province, Iran. Notably, we found that higher levels of household food insecurity were associated with lower breast cancer incidence rates, even after adjusting for key risk factors. This inverse relationship appears counterintuitive, as food insecurity is often linked to barriers in accessing healthcare services, including cancer screening and early detection, which could lead to delayed diagnosis and poorer outcomes [6, 15]. One plausible explanation is the underreporting of breast cancer cases in food-insecure populations due to limited healthcare access, as financial constraints may prioritize immediate necessities over preventive health measures. Additionally, the dietary patterns of food-insecure households in this region may differ from those observed in other settings, possibly influencing cancer risk in ways that require further investigation [3, 16].
Our findings also showed a positive association between breast cancer incidence and known risk factors, including obesity and smoking prevalence. These results align with extensive literature demonstrating that obesity increases breast cancer risk through mechanisms, such as hormonal dysregulation, chronic inflammation, and increased levels of circulating estrogens [17, 18]. Smoking, similarly, has been identified as a modifiable risk factor due to its carcinogenic effects, which directly contribute to breast tissue damage and inflammation [19]. These associations reinforce the importance of implementing targeted public health interventions, including obesity prevention and smoking cessation programs, as part of breast cancer control strategies.
Interestingly, the analysis revealed an inverse association between breast cancer incidence and diabetes prevalence. This finding may reflect the complex metabolic and hormonal changes associated with diabetes, such as lower circulating estrogen levels, which could have a protective effect against certain types of breast cancer [20, 21]. However, the ecological nature of our study warrants cautious interpretation of these results, as unmeasured factors, such as healthcare access disparities or competing health priorities among individuals with diabetes, may contribute to this observation. The role of diabetes management and its interaction with breast cancer risk remains an area requiring further exploration in individual-level studies.
The inverse association between breast cancer incidence and TFR is consistent with established evidence highlighting the protective effects of higher parity and breastfeeding on breast cancer risk [20, 22]. Pregnancy and breastfeeding are associated with delayed menarche, fewer ovulatory cycles, and protective hormonal changes that reduce lifetime estrogen exposure. In Iran, cultural practices promoting extended breastfeeding may amplify these protective effects, particularly among women in higher fertility groups. These findings suggest that encouraging breastfeeding through public health campaigns could serve as an effective strategy for reducing breast cancer risk.
Our study also found an unexpected negative association between breast cancer incidence and mean age at the city level. While breast cancer risk typically increases with age, this result may reflect unique sociodemographic or healthcare disparities in the study region. For example, older women in some cities may face barriers to accessing screening programs, leading to underdiagnosis or delayed diagnosis. Additionally, variations in age distribution across cities and differences in healthcare utilization patterns may partly explain this association [20, 22]. Further research is needed to disentangle these factors and better understand how age-related patterns influence breast cancer incidence in this population.
Despite these insights, our study has limitations that must be acknowledged. The ecological and cross-sectional design precludes causal inferences and introduces the risk of ecological fallacy, where associations observed at the group level may not accurately reflect individual-level relationships [20, 22]. The small sample size of 19 cities, while adequate for exploratory analysis, limits the generalizability of the findings and the statistical power of the model. Additionally, the use of self-reported data for smoking and obesity may introduce recall bias, and the lack of individual-level data prevents a more nuanced analysis of the observed associations. Future research should employ prospective cohort designs with individual-level data to confirm these findings and investigate the underlying mechanisms.
Conclusion
In conclusion, this study highlights the complex interplay of food insecurity, lifestyle factors, and sociodemographic variables in shaping breast cancer incidence in Razavi Khorasan Province. Addressing food insecurity, promoting access to healthcare, and implementing interventions targeting obesity, smoking, and diabetes management are critical for reducing breast cancer disparities in low-resource settings. Further research should focus on understanding regional and cultural variations in these associations to inform targeted public health strategies that improve cancer prevention and outcomes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Mashhad University of Medical Sciences, Mashhad, Iran (Code: IR.MUMS.FHMPM.REC.1402.135) and followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Funding
This work was supported by the Mashhad University of Medical Sciences, Mashhad, Iran (Grant No.: 4021070).
Authors' contributions
Conceptualization, study design, and writing the original draft: Iman Mousaei and Ehsan Mosafarkhani; Data collection: Amin Moradi, Ali Taghipour, and Fatemeh Nikbakht; Data analysis: Iman Mousaei, Amin Moradi, and Maryam Salari; Data interpretation: Ali Taghipour and Maryam Salari, Iman Mousaei, and Ehsan Mosafarkhani; Review and editing: Ehsan Mosafarkhani, Iman Mousaei; Supervision: Ehsan Mosafarkhani; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors extend their gratitude to the Health Deputy of Mashhad University of Medical Sciences, Mashhad, Iran, for assisting them in data collection.
References
Breast cancer ranks as the most common cause of cancer-related deaths among women globally, and is the second leading cause of mortality after lung cancer [1]. While mortality rates have declined in high-income countries due to advances in early detection and treatment, breast cancer incidence and mortality continue to rise in low- and middle-income countries [1]. In Asia alone, breast cancer accounts for approximately 45.4% of all cancers in women [2]. Recent reports indicate that in Iran, there are approximately 16,967 new breast cancer cases annually, resulting in 4,810 related deaths. Projections suggest a 63% increase in breast cancer cases by 2025, with an estimated 25,013 new cases expected that year [3].
The complex relationship between breast cancer and socioeconomic factors is well-documented. Higher socioeconomic status has been associated with an elevated breast cancer risk, likely due to reproductive and lifestyle factors, whereas lower socioeconomic status has been linked to late-stage diagnosis and reduced survival rates [4]. Socioeconomic factors also influence women’s access to cancer screening services and awareness of preventive measures, highlighting the importance of social determinants of health in breast cancer outcomes [5]. Social determinants, defined as the conditions in which people are born, grow, live, work, and age, as well as the broader set of forces influencing these conditions, are recognized by the World Health Organization (WHO) as critical contributors to health disparities [6]. Among these determinants, food insecurity—characterized by uncertain or insufficient access to nutritious and culturally appropriate food—has emerged as a significant public health concern globally. Approximately 852 million people are food insecure, with 9 million in developed countries and the rest in developing regions [7]. Food insecurity is particularly high in the Middle East and North Africa, affecting around 42.2% of the population, with Iran reporting a national prevalence of 49% [8]. This condition has far-reaching health impacts, including associations with chronic diseases, such as diabetes, hypertension, coronary heart disease, and mental health disorders [9, 10].
In Iran, the primary drivers of food insecurity include economic constraints and, more recently, the reimposition of international sanctions, which have sharply increased food prices without corresponding income growth [11]. Food insecurity not only affects dietary quality and nutritional status but may also hinder access to preventive healthcare services, including cancer screenings and early detection programs. These barriers can lead to delays in diagnosis and treatment, contributing to worse outcomes for individuals with cancer. Understanding the role of food insecurity, alongside other social determinants, in relation to cancer risk may provide insights for targeted interventions. Furthermore, investigating the interplay between food insecurity and other risk factors, such as obesity, smoking, and fertility rates, can help clarify their collective impact on breast cancer incidence. Given the lack of empirical evidence on this relationship in Iran, this study aimed to investigate the association between food insecurity and breast cancer incidence in Razavi Khorasan Province, providing valuable information for public health strategies aimed at reducing cancer disparities and promoting equitable health outcomes in low-resource settings.
Methods
Study design and setting
This ecological, cross-sectional study was conducted across 19 cities in Razavi Khorasan Province, Iran, using secondary data from 2017 to 2023. Data were obtained from the electronic health records maintained by Mashhad University of Medical Sciences, covering cities within the university’s healthcare jurisdiction [12]. Only cities with complete data on breast cancer incidence and predictor variables (food insecurity, obesity, smoking prevalence, diabetes prevalence, total fertility rate (TFR), and mean age) were included. Cities with incomplete or missing data for any variable were excluded from the analysis.
Study population
The study focused on all women in the region, specifically including the entire female population registered in the Mashhad University of Medical Sciences system, estimated at 2.7 million, with approximately 1.4 million women aged 30 years and older. Given the comprehensive coverage of the dataset, sampling was not performed; instead, data for the entire population were analyzed at the city level to provide a broad view of breast cancer incidence in relation to various predictors.
Age-standardized breast cancer incidence rate (ASIR)
The ASIR was calculated using data from the National Cancer Registry Center for Khorasan Razavi Province. The ASIR was computed for the period from 2017 to 2023 to ensure a comprehensive assessment of trends over multiple years. Direct age-standardization was performed using the WHO standard population as the reference.
Predictor variables
Food insecurity: Household-level food insecurity was assessed using the Persian-validated household food insecurity access scale (HFIAS), which has been previously validated for Iranian households [13, 14]. This 9-item tool assesses frequency and experience of food insecurity over the past four weeks, yielding a continuous score ranging from 0 to 27, with higher scores indicating more severe food insecurity.
Mean age: The mean age of women in each city was included as a predictor.
Overweight and obesity: Overweight and obesity prevalence (BMI ≥25 kg/m²) was calculated based on electronic health records within the Mashhad University system [12].
Diabetes: Diabetes prevalence among women over 30 was determined using ICD-10 codes (E10 and E11) from primary care visits.
Smoking: Smoking prevalence was based on self-reported data during primary healthcare assessments and recorded in the SinaEHR system, representing the percentage of women identifying as current smokers.
TFR: TFR for each city was calculated using the Spectrum software, version 3 which incorporates demographic components affecting population changes. Population data were sourced from the National Statistics Office, Civil Registration Office, and SinaEHR system census. We used the DemProj system in Spectrum to project TFR for 5 years, based on 5-year age groups. Calculations were performed separately for each city under the jurisdiction of Mashhad University of Medical Sciences.
Statistical analysis
Descriptive statistics were computed for all variables, reporting means and confidence intervals for city-level measures. Multiple linear regression was employed to examine the relationship between the ASIR and the predictor variables. Model coefficients (β), confidence intervals, and P were reported, with a significance threshold set at P<0.01 due to the large sample size. Normality of residuals and multicollinearity were tested before regression analysis to ensure assumptions were met. All analyses were conducted using STATA software, version 16 (STATA Corp, College Station, TX).
Results
Breast cancer incidence across cities
Breast cancer incidence rates varied widely across the 19 cities in Razavi Khorasan Province, ranging from 7.41 per 100,000 in Khalilabad to 41.83 per 100,000 in Shandiz. The analysis revealed significant associations between breast cancer incidence and several sociodemographic and lifestyle factors, including food insecurity, obesity, smoking prevalence, diabetes prevalence, and TFR (Table 1).
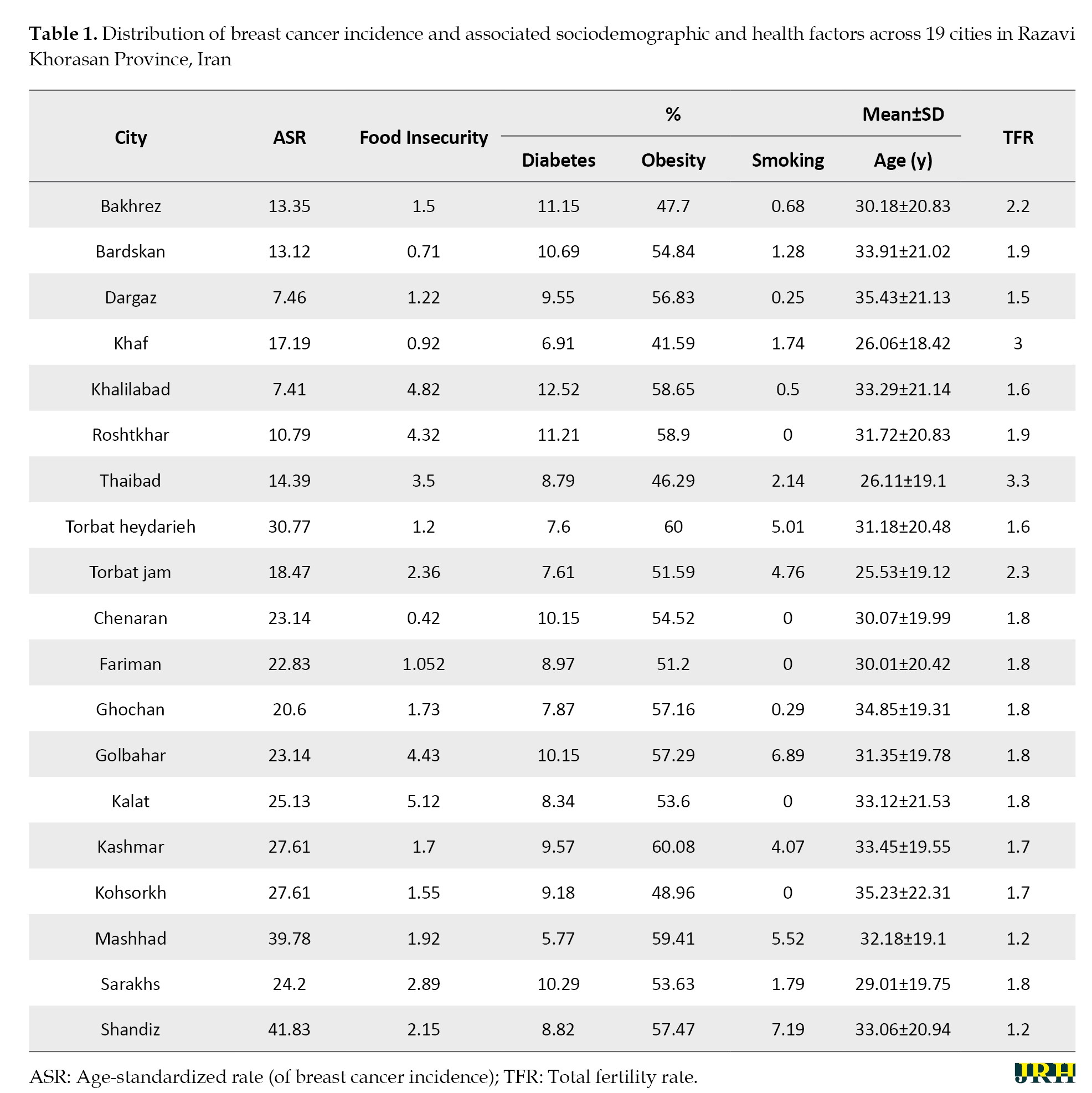
Food insecurity and breast cancer incidence
Among the 19 cities, food insecurity scores varied from 0.42 in Chenaran to 5.12 in Kalat, indicating a range of food security conditions across the region. Obesity rates were high, with Kashmar reporting the highest prevalence at 60.08%. Smoking prevalence also varied, with Shandiz showing the highest rate at 7.19% and cities like Roshtkhar and Chenaran reporting 0%. Diabetes prevalence was highest in Khalilabad (12.52%) and lowest in Khaf (6.91%). Mean age across cities ranged from 26 years in Khaf to 35 years in Kohsorkh and Dargaz. TFR was lowest in Mashhad and Shandiz (1.2) and highest in Thaibad (3.3) (Table 1).
Lifestyle factors and breast cancer risk
Pearson correlation analysis showed notable associations between the age-standardized incidence rate (ASIR) of breast cancer and predictor variables. A strong positive correlation was observed between breast cancer incidence and obesity (r=0.77, P<0.001) and smoking prevalence (r=0.81, P<0.001). Conversely, ASIR was inversely correlated with diabetes prevalence (r=-0.89, P<0.001) and TFR (r=-0.84, P<0.001). A weak negative correlation was noted between food insecurity and ASIR (r=-0.01, P<0.001), suggesting a complex relationship between food insecurity and breast cancer incidence in this population (Table 2).
Predictors of breast cancer
Table 3 presents the results of the multiple linear regression analysis examining predictors of the ASIR.
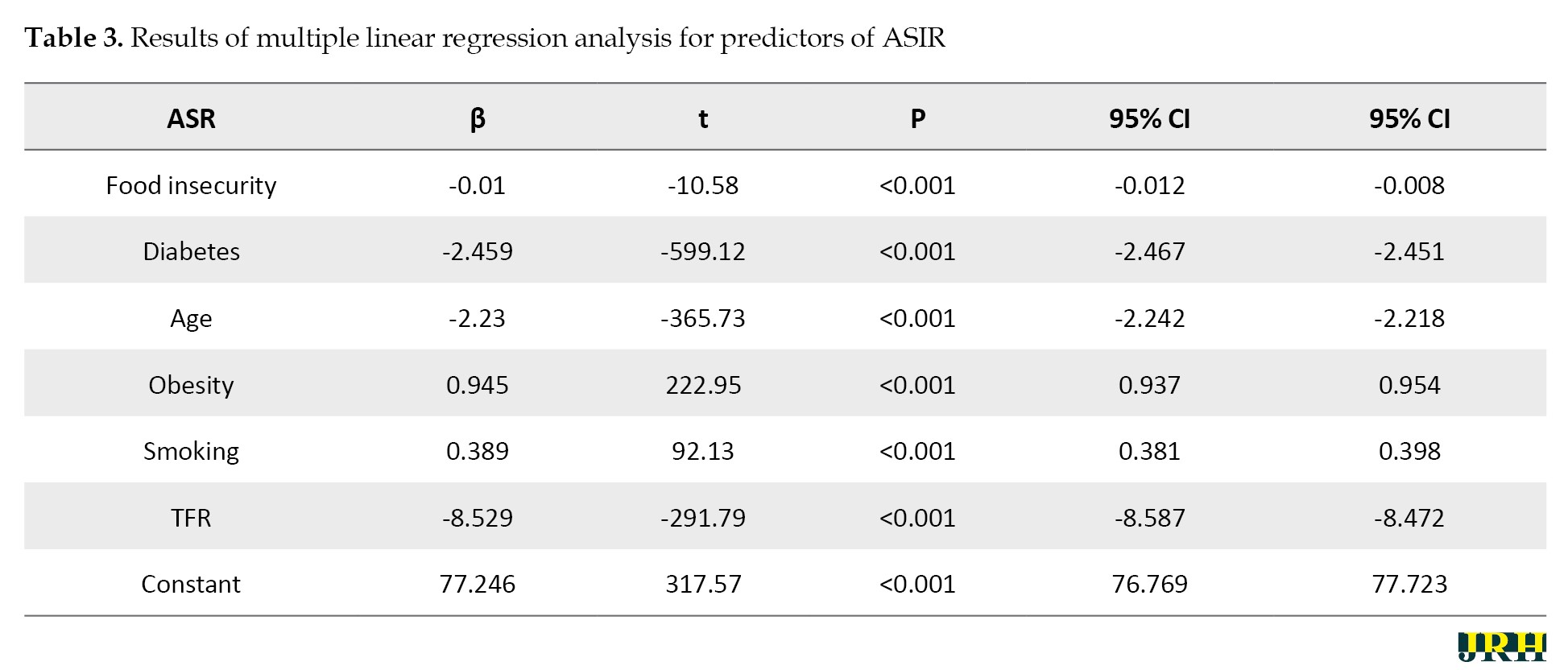
The model explained 96.3% of the variance (R²=0.96), indicating a strong fit. Food insecurity was inversely associated with ASIR (β=-0.01, 95% CI, -0.01%, -0.008%), suggesting that higher food insecurity levels correspond to a lower incidence of breast cancer. Similarly, diabetes prevalence (β=-2.46, 95% CI, -2.47%, -2.45%) and TFR (β=-8.53, 95% CI, -8.59%, -8.47%) were negatively associated with ASIR.
Conversely, obesity (β=0.95, 95% CI, 0.94%, 0.95%) and smoking prevalence (β=0.39, 95% CI, 0.38%, 0.40%) were positively associated with ASIR, indicating that higher levels of these factors are linked to increased breast cancer incidence.
Discussion
This ecological study identified several associations between food insecurity, sociodemographic factors, and ASIRs across cities in Razavi Khorasan Province, Iran. Notably, we found that higher levels of household food insecurity were associated with lower breast cancer incidence rates, even after adjusting for key risk factors. This inverse relationship appears counterintuitive, as food insecurity is often linked to barriers in accessing healthcare services, including cancer screening and early detection, which could lead to delayed diagnosis and poorer outcomes [6, 15]. One plausible explanation is the underreporting of breast cancer cases in food-insecure populations due to limited healthcare access, as financial constraints may prioritize immediate necessities over preventive health measures. Additionally, the dietary patterns of food-insecure households in this region may differ from those observed in other settings, possibly influencing cancer risk in ways that require further investigation [3, 16].
Our findings also showed a positive association between breast cancer incidence and known risk factors, including obesity and smoking prevalence. These results align with extensive literature demonstrating that obesity increases breast cancer risk through mechanisms, such as hormonal dysregulation, chronic inflammation, and increased levels of circulating estrogens [17, 18]. Smoking, similarly, has been identified as a modifiable risk factor due to its carcinogenic effects, which directly contribute to breast tissue damage and inflammation [19]. These associations reinforce the importance of implementing targeted public health interventions, including obesity prevention and smoking cessation programs, as part of breast cancer control strategies.
Interestingly, the analysis revealed an inverse association between breast cancer incidence and diabetes prevalence. This finding may reflect the complex metabolic and hormonal changes associated with diabetes, such as lower circulating estrogen levels, which could have a protective effect against certain types of breast cancer [20, 21]. However, the ecological nature of our study warrants cautious interpretation of these results, as unmeasured factors, such as healthcare access disparities or competing health priorities among individuals with diabetes, may contribute to this observation. The role of diabetes management and its interaction with breast cancer risk remains an area requiring further exploration in individual-level studies.
The inverse association between breast cancer incidence and TFR is consistent with established evidence highlighting the protective effects of higher parity and breastfeeding on breast cancer risk [20, 22]. Pregnancy and breastfeeding are associated with delayed menarche, fewer ovulatory cycles, and protective hormonal changes that reduce lifetime estrogen exposure. In Iran, cultural practices promoting extended breastfeeding may amplify these protective effects, particularly among women in higher fertility groups. These findings suggest that encouraging breastfeeding through public health campaigns could serve as an effective strategy for reducing breast cancer risk.
Our study also found an unexpected negative association between breast cancer incidence and mean age at the city level. While breast cancer risk typically increases with age, this result may reflect unique sociodemographic or healthcare disparities in the study region. For example, older women in some cities may face barriers to accessing screening programs, leading to underdiagnosis or delayed diagnosis. Additionally, variations in age distribution across cities and differences in healthcare utilization patterns may partly explain this association [20, 22]. Further research is needed to disentangle these factors and better understand how age-related patterns influence breast cancer incidence in this population.
Despite these insights, our study has limitations that must be acknowledged. The ecological and cross-sectional design precludes causal inferences and introduces the risk of ecological fallacy, where associations observed at the group level may not accurately reflect individual-level relationships [20, 22]. The small sample size of 19 cities, while adequate for exploratory analysis, limits the generalizability of the findings and the statistical power of the model. Additionally, the use of self-reported data for smoking and obesity may introduce recall bias, and the lack of individual-level data prevents a more nuanced analysis of the observed associations. Future research should employ prospective cohort designs with individual-level data to confirm these findings and investigate the underlying mechanisms.
Conclusion
In conclusion, this study highlights the complex interplay of food insecurity, lifestyle factors, and sociodemographic variables in shaping breast cancer incidence in Razavi Khorasan Province. Addressing food insecurity, promoting access to healthcare, and implementing interventions targeting obesity, smoking, and diabetes management are critical for reducing breast cancer disparities in low-resource settings. Further research should focus on understanding regional and cultural variations in these associations to inform targeted public health strategies that improve cancer prevention and outcomes.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Mashhad University of Medical Sciences, Mashhad, Iran (Code: IR.MUMS.FHMPM.REC.1402.135) and followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Funding
This work was supported by the Mashhad University of Medical Sciences, Mashhad, Iran (Grant No.: 4021070).
Authors' contributions
Conceptualization, study design, and writing the original draft: Iman Mousaei and Ehsan Mosafarkhani; Data collection: Amin Moradi, Ali Taghipour, and Fatemeh Nikbakht; Data analysis: Iman Mousaei, Amin Moradi, and Maryam Salari; Data interpretation: Ali Taghipour and Maryam Salari, Iman Mousaei, and Ehsan Mosafarkhani; Review and editing: Ehsan Mosafarkhani, Iman Mousaei; Supervision: Ehsan Mosafarkhani; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors extend their gratitude to the Health Deputy of Mashhad University of Medical Sciences, Mashhad, Iran, for assisting them in data collection.
References
- Badeleh Shamoshaki M T, Landrani M, Sadeghi E. [Relationship between cognitive flexibility and fear of cancer recurrence in breast cancer patients (Persian)]. Iranian Journal of Cancer Care. 2023; 2(3):3-10. [Link]
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians. 2021; 71(3):209-49. [DOI:10.3322/caac.21660] [PMID]
- Haghighat S, Omidi Z, Ghanbari-Motlagh A. Trend of breast cancer incidence in Iran during a fifteen-year interval according to national cancer registry reports. Iranian Journal of Breast Diseases. 2022; 15(2):4-17. [DOI:10.30699/ijbd.15.2.4]
- Coughlin SS. Social determinants of breast cancer risk, stage, and survival. Breast Cancer Research and Treatment. 2019; 177(3):537-48. [DOI:10.1007/s10549-019-05340-7] [PMID]
- Mahmood A, Kedia S, Dillon PJ, Kim H, Arshad H, Ray M. Food security status and breast cancer screening among women in the United States: Evidence from the Health and Retirement Study and Health Care and Nutrition Study. Cancer Causes & Control. 2023; 34(4):321-35. [DOI:10.1007/s10552-023-01667-1] [PMID]
- Mendoza JA, Miller CA, Martin KJ, Resnicow K, Iachan R, Faseru B, et al. Examining the association of food insecurity and being up-to-date for breast and colorectal cancer screenings. Cancer Epidemiology, Biomarkers & Prevention. 2022; 31(5):1017-25. [DOI:10.1158/1055-9965.EPI-21-1116] [PMID]
- Behzadifar M, Behzadifar M, Abdi S, Malekzadeh R, Arab Salmani M, Ghoreishinia G, et al. Prevalence of food insecurity in Iran: A systematic review and meta-analysis. Archives of Iranian Medicine. 2016; 19(4):288-94. [PMID]
- Barrett CB. Measuring food insecurity. Science. 2010; 327(5967):825-8. [DOI:10.1126/science.1182768] [PMID]
- Gany F, Melnic I, Ramirez J, Wu M, Li Y, Paolantonio L, et al. The association between housing and food insecurity among medically underserved cancer patients. Supportive Care in Cancer. 2021; 29(12):7765-74. [DOI:10.1007/s00520-021-06254-1] [PMID]
- Liu Y, Eicher-Miller HA. Food insecurity and cardiovascular disease risk. Current Atherosclerosis Reports. 2021; 23(6):24. [DOI:10.1007/s11883-021-00923-6] [PMID]
- Hejazi J, Emamgholipour S. The effects of the re-imposition of US sanctions on food security in Iran. International Journal of Health Policy and Management. 2022; 11(5):651-7. [PMID]
- Norouzi M, Amiri Z, Farkhani EM, Hoseini SJ, Khosravi As T. Advancing healthcare infrastructure: The features of Iran’s Sina electronic health record system. Epidemiology and Health System Journal. 2024; 11(2):48-54. [DOI:10.34172/ehsj.26105]
- Moosavian SP, Feizi A, Esmaillzadeh A, Brett NR, Bellissimo N, Azadbakht L. Developing and assessing the validity and reliability of an Iranian food security questionnaire. Archives of Iranian Medicine. 2019; 22(1):11-23. [PMID]
- Amiri Z, Sadeghi M, Moradi A, Paydar M, Norouzi M, Mosafarkhani E. Association between household food insecurity and low birth weight: A population-based case-control study. Journal of Research in Health Sciences. 2024; 24(4):e00630. [DOI:10.34172/jrhs.2024.165] [PMID]
- Xing J, Han X, Nipp RD, Hussaini SMQ, Wang T, Yabroff KR, et al. Food insecurity, housing insecurity, and transportation barriers to care among cancer survivors with medical financial hardship. JCO Oncology Practice. 2025; OP2500045. [DOI:10.1200/OP-25-00045] [PMID]
- No Author. Food insecurity: A public health issue. Public Health Reports. 2016; 131(5):655-7. [DOI:10.1177/0033354916664154] [PMID]
- Borghesan DH, Agnolo CM, Gravena AA, Demitto Mde O, Lopes TC, Carvalho MD, et al. Risk factors for breast cancer in postmenopausal women in Brazil. Asian Pacific Journal of Cancer Prevention. 2016; 17(7):3587-93. [PMID]
- Amini Sani N, Shamshir Garan M, Ghavam Nasiri M, Setayesh Y. [The effect of active and passive smoking associated with breast cancer (Persian)]. Journal of Babol University of Medical Sciences. 2005; 7(1):63-8. [Link]
- Hajian K, Gholizadehpasha A, Bozorgzadeh S. [Association of obesity and central obesity with breast cancer risk in pre- and postmenopausal women (Persian)]. Journal of Babol University of Medical Sciences. 2013; 15(3):7-15. [Link]
- Ghaedi M, Feiz F, Kalani N, Hatami N, Haghbeen M. The relationship between age of disease onset and prognosis of breast cancer in women. Iranian Journal of Obstetrics, Gynecology and Infertility. 2022; 25(12):22-32. [Link]
- Boyle P, Boniol M, Koechlin A, Robertson C, Valentini F, Coppens K, et al. Diabetes and breast cancer risk: A meta-analysis. British Journal of Cancer. 2012; 107(9):1608-17. [DOI:10.1038/bjc.2012.414] [PMID]
- Montazeri V, Jafarpour Sadegh F, Hosseinpour S, Mirzaei H, Akbari E, Ehsani M, et al. Reproductive risk factors of breast cancer among women in Tehran and Northwest of Iran: A case-control study. Iranian Journal of Epidemiology. 2016; 12(1):1-9. [Link]
Type of Study: Short Communication |
Subject:
● Disease Control
Received: 2024/11/8 | Accepted: 2025/03/5 | Published: 2025/11/1
Received: 2024/11/8 | Accepted: 2025/03/5 | Published: 2025/11/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |