Volume 15, Issue 6 (Nov & Dec 2025)
J Research Health 2025, 15(6): 625-632 |
Back to browse issues page
Ethics code: IR.MEDILAM.REC.1399.264
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Norouzi S, Mohammadyari E, Mohammadyari A, Tavan H. Myocardial Infarction In COVID-19 Patients Admitted to the Shahid Mostafa Khomeini Hospital of Ilam: A Case Series. J Research Health 2025; 15 (6) :625-632
URL: http://jrh.gmu.ac.ir/article-1-2670-en.html
URL: http://jrh.gmu.ac.ir/article-1-2670-en.html
1- ِDepartment of Cardiology, School of Medicine, Shahid Mostafa Khomaeini Hospital, Ilam University of Medical sciences, Ilam, Iran.
2- Department of Cardiology, Non-Communicable Diseases Research Center, School of Medicine, Shahid Mostafa Khomaeini Hospital, Ilam University of Medical sciences, Ilam, Iran.
3- Clinical Research Development Unit, Shahid Mostafa Khomeini Hospital, Ilam University of Medical Sciences, Ilam, Iran.
4- Department of Nursing, Student Research Committee, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran. ,hamedtavan@gmail.com
2- Department of Cardiology, Non-Communicable Diseases Research Center, School of Medicine, Shahid Mostafa Khomaeini Hospital, Ilam University of Medical sciences, Ilam, Iran.
3- Clinical Research Development Unit, Shahid Mostafa Khomeini Hospital, Ilam University of Medical Sciences, Ilam, Iran.
4- Department of Nursing, Student Research Committee, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran. ,
Full-Text [PDF 6626 kb]
(207 Downloads)
| Abstract (HTML) (1952 Views)
Full-Text: (211 Views)
Introduction
COVID-19 primarily affects the respiratory system and causes respiratory disorders, reduced O2 saturation, and respiratory distress in patients [1]. Patients with a history of underlying diseases (heart failure, infarction, hypertension, and heart valve replacement), as well as those with cardiac risk factors (elevated cardiac enzymes such as troponin, LDH, and CPK) and elevated levels of lipids, triglycerides, cholesterol, LDL, and reduced HDL, are more vulnerable to the disease’s complications and have a poorer prognosis [2].
Ruan et al. showed that COVID-19-related mortality was significantly associated with cardiovascular failure [3]. Another study stated that underlying diseases, such as hypertension, can increase the mortality rate in COVID-19 patients by up to 2.5 times [4]. Although the clinical manifestations of COVID-19 in patients with heart failure are unknown, clinical evidence from patients with end-stage heart failure indicates that the virus is associated with direct cardiac damage [5-7].
COVID-19 is also associated with patients’ demographic features. Most deaths occur in older men with a mean age of 75 years who have a history of underlying conditions, such as diabetes, hypertension, heart disease, chronic respiratory disease, cancer, or prior surgeries. COVID-19 also triggers cardiovascular complications by causing arterial and venous thrombosis. The mechanisms of thrombosis in this disease include inducing inflammation, platelet activation, as well as vascular dysfunction and occlusion. Accordingly, antithrombotic drugs constitute a part of the treatments provided to COVID-19 patients [8].
The mechanisms proposed for COVID-19-related cardiovascular diseases suggest that cardiac problems may result from an imbalance between metabolic demand and cardiac reserve. This imbalance, in association with inflammatory conditions and myocardial damage, can increase the risk of acute coronary artery syndrome, heart failure, arrhythmias, and myocardial infarction (MI) [9].
One of the laboratory parameters that predicts cardiac ischemia and mortality in COVID-19 is cardiac troponin I. It should be noted that elevated cardiac troponin I in patients with COVID-19 is merely an indicator of cardiac damage and causes secondary severe hypoxemia [10].
Although most studies regard cardiac damage and heart failure as risk factors for morbidity and mortality, one study declared that the virus itself was the direct cause of death in a patient who had no history of cardiovascular disease and heart failure; nevertheless, the exact mechanisms of heart failure remain to be identified [11].
MI is the most dreadful complication of heart diseases and is responsible for a large number of patients’ deaths. The aim of this report was to describe MI in a series of COVID-19 patients referred to the Shahid Mostafa Khomeini hospital in Ilam from March 2020 to January 2021.
Case Presentations
The selection of cases and samples included patients who had a confirmed diagnosis of MI based on blood tests (troponin) or evident electrocardiogram (ECG) changes, and these individuals also had a positive polymerase chain reaction (PCR) test. The diagnostic criteria for confirming MI included positive troponin (NSTEMI) and ST-segment elevation on ECG (STEMI). The data source was cross-sectional, covering the period from March 2020 to March 2021.
Out of ten COVID-19 patients, 8(80%) were elderly men, and 2(20%) were elderly women, indicating a male/female ratio of 4:1. All the patients were over 60 years old (i.e. elderly). Of these, six (60%) were classified as young elderly (aged 60 to 74 years), one (10%) as middle-aged elderly (aged 75 to 84 years), and three (30%) as very old (over 85 years).
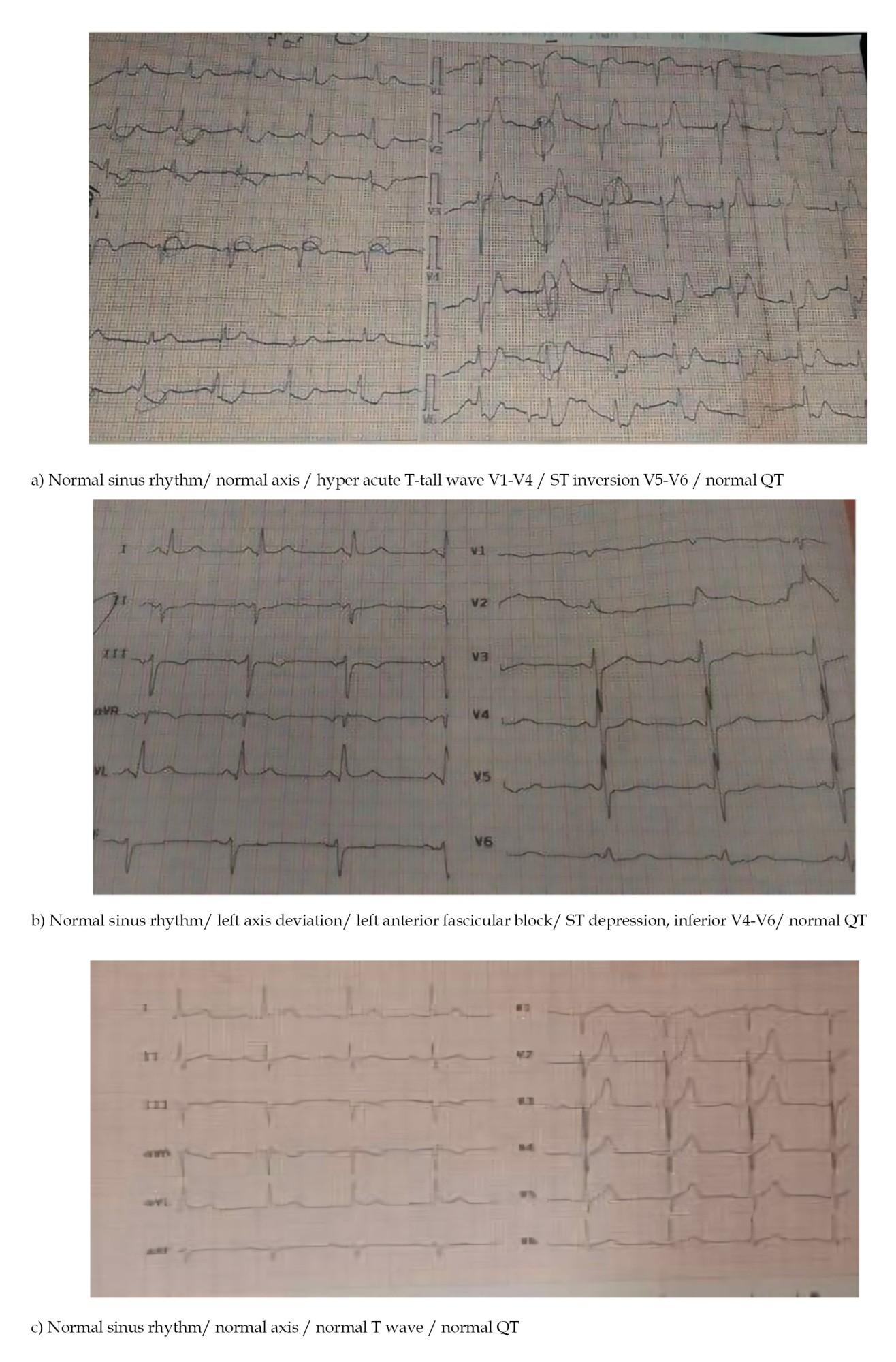
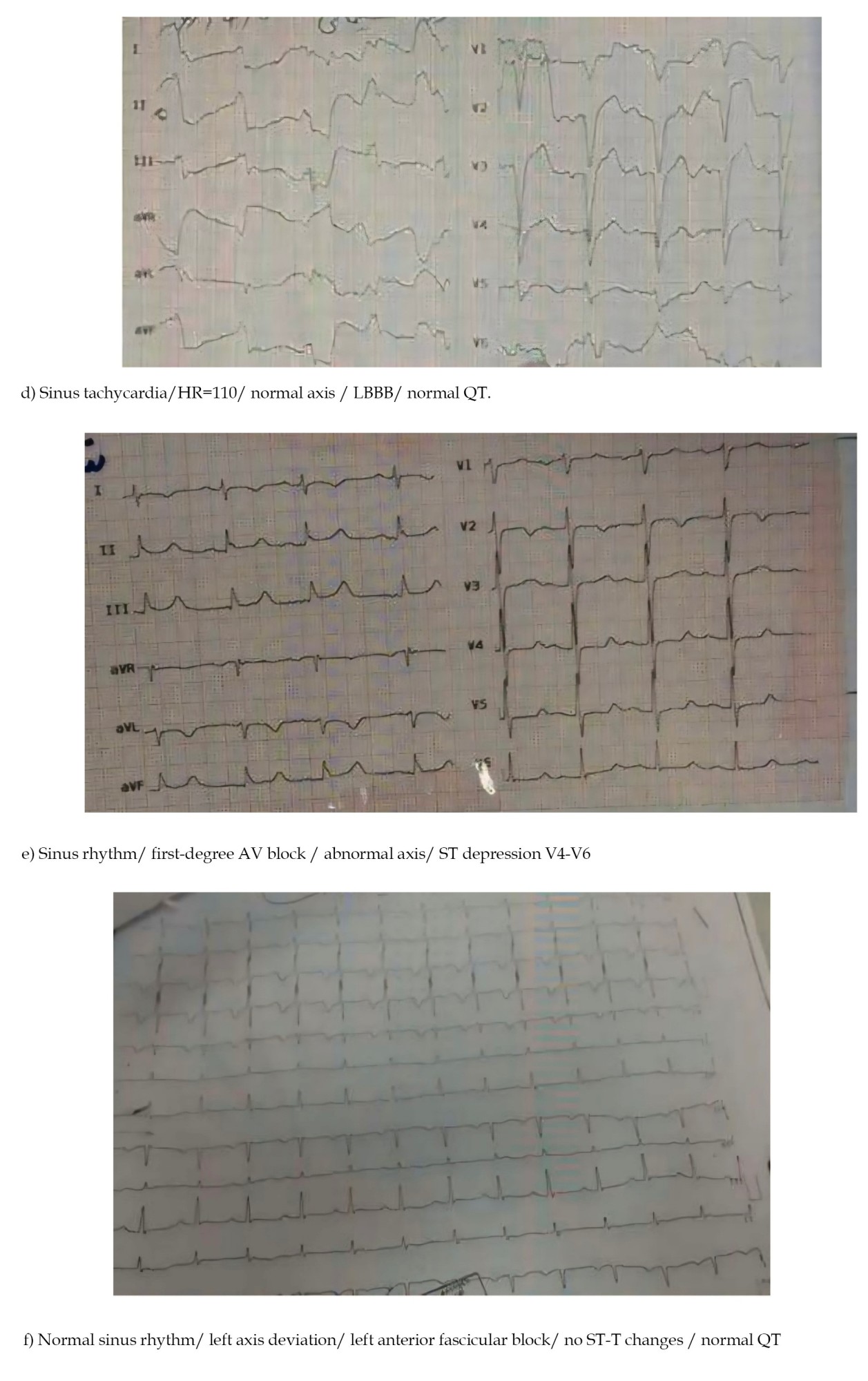
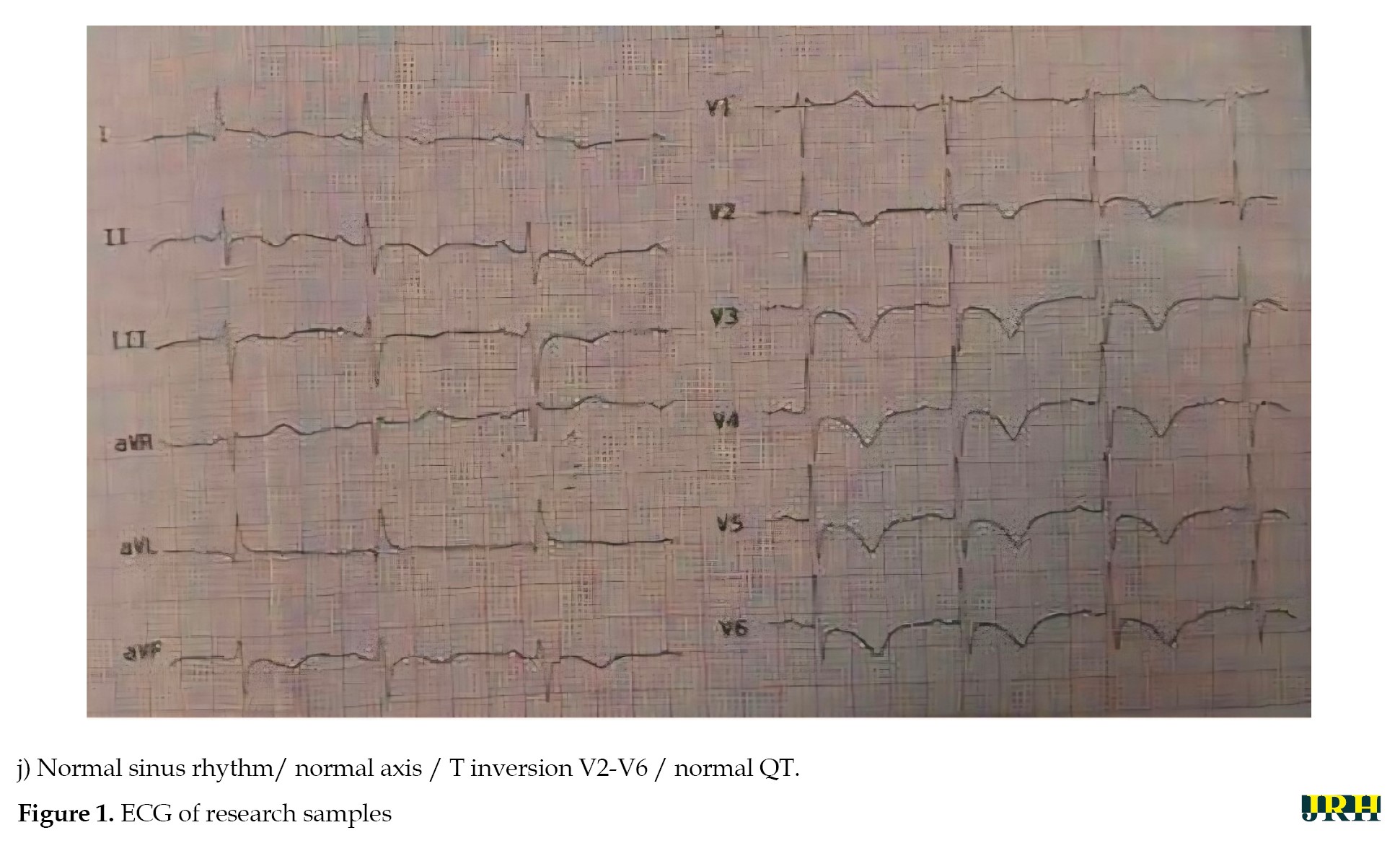
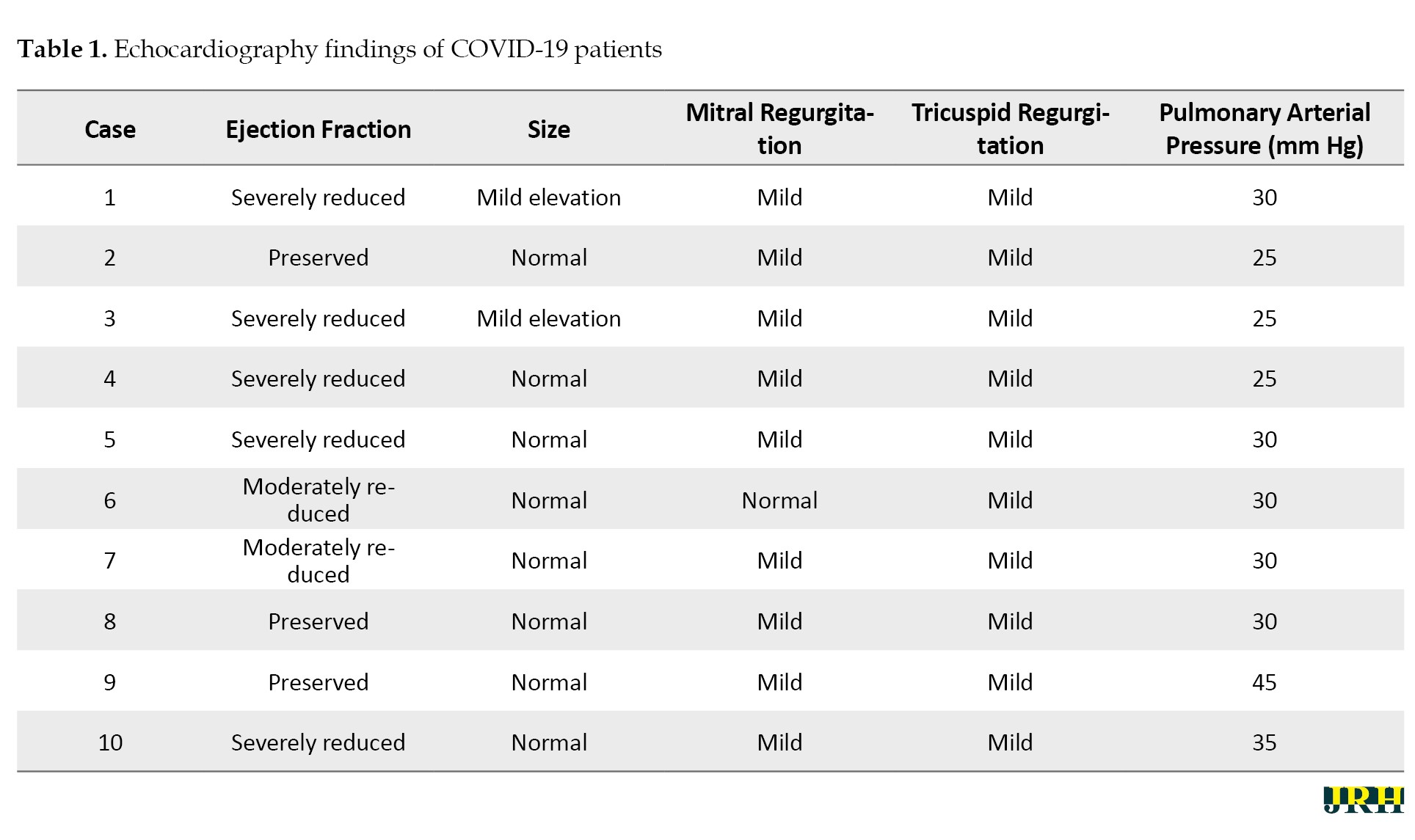
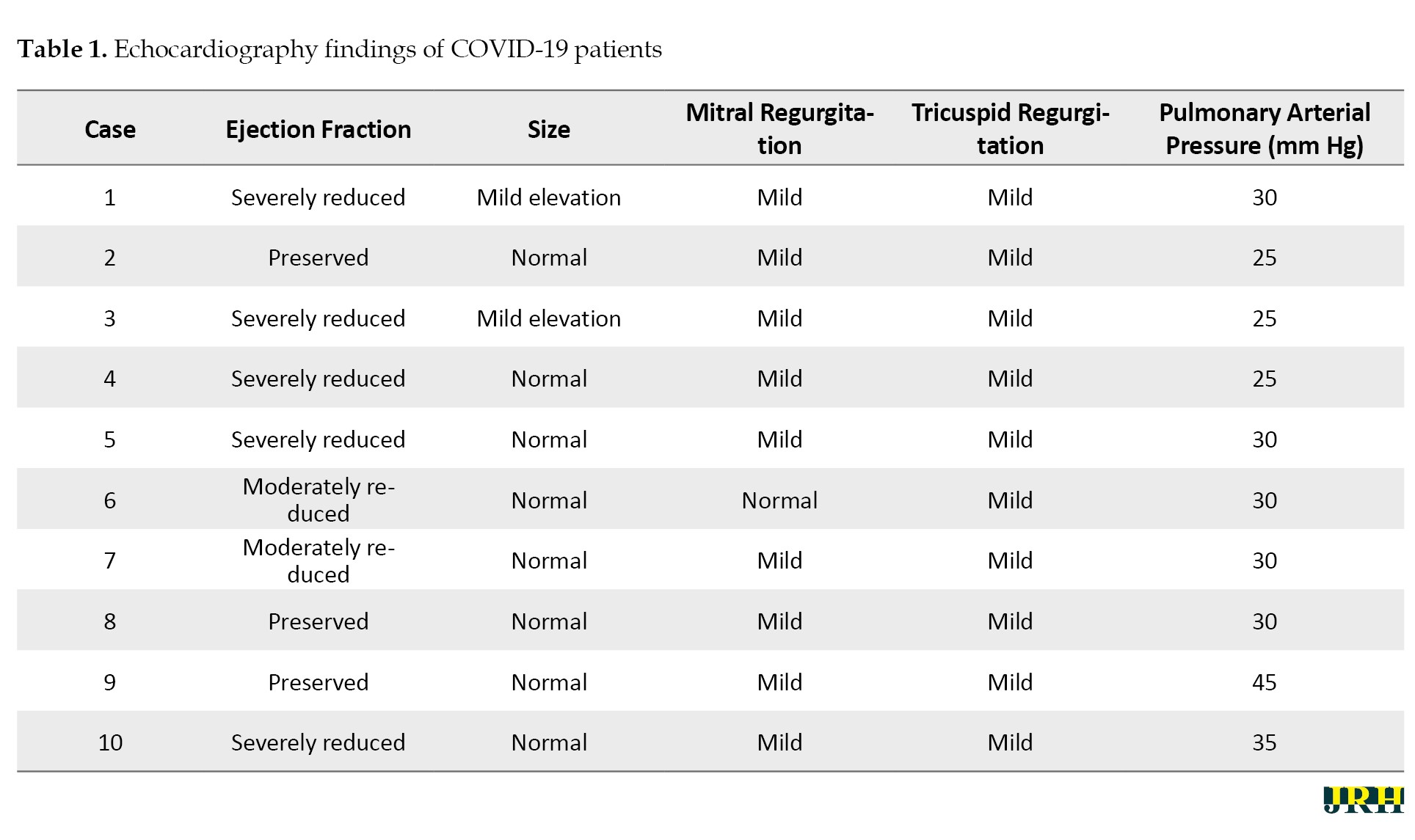
Ten cases of MI were identified by examining COVID-19 patients who complained of chest pain and had ECG abnormalities. Table 1 reports the echocardiographic results of the patients and discusses parameters such as ejection fraction, size, mitral regurgitation, tricuspid regurgitation, and pulmonary arterial pressures.
Case 1: A 92-year-old man was referred to the emergency department with weakness and fatigue. After a positive troponin test, cardiology counseling was requested. Due to the presence of a pacemaker and the poor performance of the instrument, an ECG was not obtained.
Case 2: An 82-year-old man with acute coronary syndrome/possible pulmonary thromboembolism (ACS/RO PTE) was referred to the emergency department. The ECG showed abnormal patterns (Table 1). Troponin and C-reactive protein (CRP) were positive, and the erythrocyte sedimentation rate (ESR) was elevated. A high-resolution computed tomography (HRCT) scan was performed by a cardiologist, and a PCR test returned a positive COVID-19 result.
Case 3: A 90-year-old man with COVID-19 was admitted to the infectious diseases ward. Based on ECG alterations (Table 1) and the results of laboratory tests (positive troponin, high ESR, and positive CRP), a cardiology consultation was requested.
Case 4: A 73-year-old woman was admitted to the infectious diseases ward with a diagnosis of COVID-19. After examining ECG patterns (Table 1) and considering the results of relevant tests (positive troponin, high ESR, and positive CRP), a cardiology consultation was requested.
Case 5: A 67-year-old woman with a diagnosis of COVID-19 was admitted to the infectious diseases ward. Following an assessment of the ECG changes (Table 1) and based on the results of laboratory tests (positive troponin, high ESR, and positive CRP), a cardiology consultation was requested, which resulted in a diagnosis of non-ST-segment elevation MI.
Case 6: A 91-year-old male with a diagnosis of COVID-19 was admitted to the infectious diseases ward. According to ECG findings, positive troponin and CRP tests, and elevated ESR, a cardiology consultation was requested, resulting in the diagnosis of MI.
Case 7: A 73-year-old man was admitted to the infectious diseases ward with a diagnosis of COVID-19. A cardiology consultation was requested because of ECG abnormalities (Table 1), positive troponin and CRP tests, and elevated ESR. The patient ultimately died from complications of the disease.
Case 8: A 63-year-old male with a diagnosis of COVID-19 was admitted to the internal medicine ward. Based on ECG abnormalities (Table 1) and the results of laboratory tests (positive troponin, high ESR, and positive CRP), a cardiology consultation was requested. He was diagnosed with non-ST-segment elevation MI.
Case 9: A 67-year-old man with a diagnosis of COVID-19 was admitted to the infectious diseases ward. According to ECG findings (Table 1), positive troponin and CRP tests, and elevated ESR, a cardiology consultation was requested.
Case 10: A 60-year-old female was admitted to the infectious diseases ward with a diagnosis of COVID-19. Based on ECG findings, positive troponin and CRP tests, and elevated ESR, a cardiology consultation was requested.
ECG images are shown separately in Figure 1.
Discussion
The present study examined MI in COVID-19 patients as a case series. According to a study by Shi et al., elderly cardiac patients with myocardial damage and decreased ejection fraction (EF) who contracted COVID-19 experienced more pronounced cardiac injuries and significantly higher mortality [12]. In a cohort study involving 416 COVID-19 patients, cardiac damage was reported in 19.7% of patients at admission and was identified as an independent risk factor for in-hospital mortality [12]. According to the results of the present study, 3 out of 10 patients (30%) died, while 7 patients (70%) recovered.
The mortality rate was higher among men than women. The mortality and severity of COVID-19 and SARS have been associated with factors, such as age and the presence of comorbidities. Although age was comparable between men and women, men with COVID-19 seem to experience a more severe disease. Overall, the number of men dying from COVID-19 was 2.4 times higher than that of women. While the prevalence of COVID-19 is similar between men and women, men seem to have a poorer prognosis and higher mortality rates independent of their age [13].
Timely diagnosis of MI in COVID-19 patients can help reduce mortality. Therefore, it is essential to identify suspected COVID-19 patients through regular assessment of ECG patterns and serum troponin levels.
New clinical experiences
COVID-19 is a severe inflammatory disease with a relatively high mortality rate. The disease can provoke MI; thus, monitoring patients for this condition can help reduce the mortality and morbidity associated with COVID-19. Due to the complex nature and unknown aspects of the disease, it is important to identify the mechanisms of cardiac and coronary artery involvement. Due to the overlap between the cardiac and pulmonary complications of COVID-19, and because cardiac events may even be asymptomatic, screening cardiac function in all patients and providing timely treatments may significantly reduce mortality in these patients. It is noteworthy that some patients may have no symptoms of myocardial ischemia, and MI may present as the first sign in these patients. Due to the progressive nature of MI in COVID-19 patients, there is a need for early screening and immediate interventions.
Conclusion
Although MI is not common in COVID-19 patients, it has a high mortality rate and should be promptly managed with preventive measures.
Limitations
The small sample size was one of the limitations of the present study.
Recommendations
It is recommended that patients with cardiac conditions be screened for viral infections, especially COVID-19.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Deputy of Research and Technology of Ilam University of Medical Sciences, Ilam, Iran (Code: IR.MEDILAM.REC.1399.264). All participants provided written informed consent.
Funding
This study was supported in part by the Ilam University of Medical Sciences, Ilam, Iran.
Authors' contributions
Conceptualization, methodology, resources and writing: All authors; Experiments, data analysis and interpretation: Siros Noroz and Hamed Tavan.
Conflict of interest
The authors declared no conflict of interest.
References
COVID-19 primarily affects the respiratory system and causes respiratory disorders, reduced O2 saturation, and respiratory distress in patients [1]. Patients with a history of underlying diseases (heart failure, infarction, hypertension, and heart valve replacement), as well as those with cardiac risk factors (elevated cardiac enzymes such as troponin, LDH, and CPK) and elevated levels of lipids, triglycerides, cholesterol, LDL, and reduced HDL, are more vulnerable to the disease’s complications and have a poorer prognosis [2].
Ruan et al. showed that COVID-19-related mortality was significantly associated with cardiovascular failure [3]. Another study stated that underlying diseases, such as hypertension, can increase the mortality rate in COVID-19 patients by up to 2.5 times [4]. Although the clinical manifestations of COVID-19 in patients with heart failure are unknown, clinical evidence from patients with end-stage heart failure indicates that the virus is associated with direct cardiac damage [5-7].
COVID-19 is also associated with patients’ demographic features. Most deaths occur in older men with a mean age of 75 years who have a history of underlying conditions, such as diabetes, hypertension, heart disease, chronic respiratory disease, cancer, or prior surgeries. COVID-19 also triggers cardiovascular complications by causing arterial and venous thrombosis. The mechanisms of thrombosis in this disease include inducing inflammation, platelet activation, as well as vascular dysfunction and occlusion. Accordingly, antithrombotic drugs constitute a part of the treatments provided to COVID-19 patients [8].
The mechanisms proposed for COVID-19-related cardiovascular diseases suggest that cardiac problems may result from an imbalance between metabolic demand and cardiac reserve. This imbalance, in association with inflammatory conditions and myocardial damage, can increase the risk of acute coronary artery syndrome, heart failure, arrhythmias, and myocardial infarction (MI) [9].
One of the laboratory parameters that predicts cardiac ischemia and mortality in COVID-19 is cardiac troponin I. It should be noted that elevated cardiac troponin I in patients with COVID-19 is merely an indicator of cardiac damage and causes secondary severe hypoxemia [10].
Although most studies regard cardiac damage and heart failure as risk factors for morbidity and mortality, one study declared that the virus itself was the direct cause of death in a patient who had no history of cardiovascular disease and heart failure; nevertheless, the exact mechanisms of heart failure remain to be identified [11].
MI is the most dreadful complication of heart diseases and is responsible for a large number of patients’ deaths. The aim of this report was to describe MI in a series of COVID-19 patients referred to the Shahid Mostafa Khomeini hospital in Ilam from March 2020 to January 2021.
Case Presentations
The selection of cases and samples included patients who had a confirmed diagnosis of MI based on blood tests (troponin) or evident electrocardiogram (ECG) changes, and these individuals also had a positive polymerase chain reaction (PCR) test. The diagnostic criteria for confirming MI included positive troponin (NSTEMI) and ST-segment elevation on ECG (STEMI). The data source was cross-sectional, covering the period from March 2020 to March 2021.
Out of ten COVID-19 patients, 8(80%) were elderly men, and 2(20%) were elderly women, indicating a male/female ratio of 4:1. All the patients were over 60 years old (i.e. elderly). Of these, six (60%) were classified as young elderly (aged 60 to 74 years), one (10%) as middle-aged elderly (aged 75 to 84 years), and three (30%) as very old (over 85 years).
Ten cases of MI were identified by examining COVID-19 patients who complained of chest pain and had ECG abnormalities. Table 1 reports the echocardiographic results of the patients and discusses parameters such as ejection fraction, size, mitral regurgitation, tricuspid regurgitation, and pulmonary arterial pressures.
Case 1: A 92-year-old man was referred to the emergency department with weakness and fatigue. After a positive troponin test, cardiology counseling was requested. Due to the presence of a pacemaker and the poor performance of the instrument, an ECG was not obtained.
Case 2: An 82-year-old man with acute coronary syndrome/possible pulmonary thromboembolism (ACS/RO PTE) was referred to the emergency department. The ECG showed abnormal patterns (Table 1). Troponin and C-reactive protein (CRP) were positive, and the erythrocyte sedimentation rate (ESR) was elevated. A high-resolution computed tomography (HRCT) scan was performed by a cardiologist, and a PCR test returned a positive COVID-19 result.
Case 3: A 90-year-old man with COVID-19 was admitted to the infectious diseases ward. Based on ECG alterations (Table 1) and the results of laboratory tests (positive troponin, high ESR, and positive CRP), a cardiology consultation was requested.
Case 4: A 73-year-old woman was admitted to the infectious diseases ward with a diagnosis of COVID-19. After examining ECG patterns (Table 1) and considering the results of relevant tests (positive troponin, high ESR, and positive CRP), a cardiology consultation was requested.
Case 5: A 67-year-old woman with a diagnosis of COVID-19 was admitted to the infectious diseases ward. Following an assessment of the ECG changes (Table 1) and based on the results of laboratory tests (positive troponin, high ESR, and positive CRP), a cardiology consultation was requested, which resulted in a diagnosis of non-ST-segment elevation MI.
Case 6: A 91-year-old male with a diagnosis of COVID-19 was admitted to the infectious diseases ward. According to ECG findings, positive troponin and CRP tests, and elevated ESR, a cardiology consultation was requested, resulting in the diagnosis of MI.
Case 7: A 73-year-old man was admitted to the infectious diseases ward with a diagnosis of COVID-19. A cardiology consultation was requested because of ECG abnormalities (Table 1), positive troponin and CRP tests, and elevated ESR. The patient ultimately died from complications of the disease.
Case 8: A 63-year-old male with a diagnosis of COVID-19 was admitted to the internal medicine ward. Based on ECG abnormalities (Table 1) and the results of laboratory tests (positive troponin, high ESR, and positive CRP), a cardiology consultation was requested. He was diagnosed with non-ST-segment elevation MI.
Case 9: A 67-year-old man with a diagnosis of COVID-19 was admitted to the infectious diseases ward. According to ECG findings (Table 1), positive troponin and CRP tests, and elevated ESR, a cardiology consultation was requested.
Case 10: A 60-year-old female was admitted to the infectious diseases ward with a diagnosis of COVID-19. Based on ECG findings, positive troponin and CRP tests, and elevated ESR, a cardiology consultation was requested.
ECG images are shown separately in Figure 1.
Discussion
The present study examined MI in COVID-19 patients as a case series. According to a study by Shi et al., elderly cardiac patients with myocardial damage and decreased ejection fraction (EF) who contracted COVID-19 experienced more pronounced cardiac injuries and significantly higher mortality [12]. In a cohort study involving 416 COVID-19 patients, cardiac damage was reported in 19.7% of patients at admission and was identified as an independent risk factor for in-hospital mortality [12]. According to the results of the present study, 3 out of 10 patients (30%) died, while 7 patients (70%) recovered.
The mortality rate was higher among men than women. The mortality and severity of COVID-19 and SARS have been associated with factors, such as age and the presence of comorbidities. Although age was comparable between men and women, men with COVID-19 seem to experience a more severe disease. Overall, the number of men dying from COVID-19 was 2.4 times higher than that of women. While the prevalence of COVID-19 is similar between men and women, men seem to have a poorer prognosis and higher mortality rates independent of their age [13].
Timely diagnosis of MI in COVID-19 patients can help reduce mortality. Therefore, it is essential to identify suspected COVID-19 patients through regular assessment of ECG patterns and serum troponin levels.
New clinical experiences
COVID-19 is a severe inflammatory disease with a relatively high mortality rate. The disease can provoke MI; thus, monitoring patients for this condition can help reduce the mortality and morbidity associated with COVID-19. Due to the complex nature and unknown aspects of the disease, it is important to identify the mechanisms of cardiac and coronary artery involvement. Due to the overlap between the cardiac and pulmonary complications of COVID-19, and because cardiac events may even be asymptomatic, screening cardiac function in all patients and providing timely treatments may significantly reduce mortality in these patients. It is noteworthy that some patients may have no symptoms of myocardial ischemia, and MI may present as the first sign in these patients. Due to the progressive nature of MI in COVID-19 patients, there is a need for early screening and immediate interventions.
Conclusion
Although MI is not common in COVID-19 patients, it has a high mortality rate and should be promptly managed with preventive measures.
Limitations
The small sample size was one of the limitations of the present study.
Recommendations
It is recommended that patients with cardiac conditions be screened for viral infections, especially COVID-19.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Deputy of Research and Technology of Ilam University of Medical Sciences, Ilam, Iran (Code: IR.MEDILAM.REC.1399.264). All participants provided written informed consent.
Funding
This study was supported in part by the Ilam University of Medical Sciences, Ilam, Iran.
Authors' contributions
Conceptualization, methodology, resources and writing: All authors; Experiments, data analysis and interpretation: Siros Noroz and Hamed Tavan.
Conflict of interest
The authors declared no conflict of interest.
References
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395(10223):497-506. [DOI:10.1016/S0140-6736(20)30183-5] [PMID]
- Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. Prevalence and impact of cardiovascular metabolic disease on COVID-19 in China. Clinical Research in Cardiology. 2020; 109(5):531-8. [DOI:10.1007/s00392-020-01626-9] [PMID]
- Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Medicine. 2020; 46(5):846-8. [DOI:10.1007/s00134-020-05991-x] [PMID]
- Lippi G, Wong J, Henry BM. Hypertension in patients with coronavirus disease 2019 (COVID-19): A pooled analysis. Polish Archives of Internal Medicine. 2020; 130(4):304-9. [DOI:10.20452/pamw.15272]
- Bansal M. Cardiovascular disease and COVID-19. Diabetes & Metabolic Syndrome. 2020; 14(3):247-50. [DOI:10.1016/j.dsx.2020.03.013] [PMID]
- Dong N, Cai J, Zhou Y, Liu J, Li F. End-stage heart failure with COVID-19: Strong evidence of myocardial injury by 2019-nCoV. JACC. Heart failure. 2020; 8(6):515-7. [DOI:10.1016/j.jchf.2020.04.001] [PMID]
- Hulot JS. COVID-19 in patients with cardiovascular diseases. Archives of Cardiovascular Diseases. 2020; 113(4):225-6. [DOI:10.1016/j.acvd.2020.03.009] [PMID]
- Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. COVID-19 and thrombotic or thromboembolic disease: Implications for prevention, antithrombotic therapy, and follow-up: JACC State-of-the-Art Review. Journal of the American College of Cardiology. 2020; 75(23):2950-73. [DOI:10.1016/j.jacc.2020.04.031] [PMID]
- Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, et al. Impact of coronavirus disease 2019 (covid-19) outbreak on st-segment-elevation myocardial infarction care in Hong Kong, china. Circulation. Cardiovascular Quality and Outcomes. 2020; 13(4):e006631. [DOI:10.1161/CIRCOUTCOMES.120.006631] [PMID]
- Du RH, Liang LR, Yang CQ, Wang W, Cao TZ, Li M, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: A prospective cohort study. The European Respiratory Journal. 2020; 55(5):2000524. [DOI:10.1183/13993003.00524-2020] [PMID]
- Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiology. 2020; 5(7):819-24. [DOI:10.1001/jamacardio.2020.1096] [PMID]
- Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiology. 2020; 5(7):802-10. [DOI:10.1001/jamacardio.2020.0950] [PMID]
- Jin JM, Bai P, He W, Wu F, Liu XF, Han DM, et al. Gender differences in patients with COVID-19: Focus on severity and mortality. Frontiers in Public Health. 2020; 8:152. [DOI:10.3389/fpubh.2020.00152] [PMID]
Type of Study: Short Communication |
Subject:
● Disease Control
Received: 2024/11/8 | Accepted: 2025/03/5 | Published: 2025/11/1
Received: 2024/11/8 | Accepted: 2025/03/5 | Published: 2025/11/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |