Volume 16, Issue 1 (Jan & Feb 2026)
J Research Health 2026, 16(1): 5-18 |
Back to browse issues page
Ethics code: IR.MEDSAB.REC.1403.104
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Forouhar N, Shegarf Nakhaie M, Torkmannejad Sabzevari M, Rad M. Maternal’ Lived Experiences of Their Near-miss Events: A Metasynthesis of Qualitative Studies. J Research Health 2026; 16 (1) :5-18
URL: http://jrh.gmu.ac.ir/article-1-2684-en.html
URL: http://jrh.gmu.ac.ir/article-1-2684-en.html
1- Department of Obstetrics and Gynecology, Non-communicable disease research center, School of Medicine, Mobini Maternity Hospital, Sabzevar University of Medical Sciences, Sabzevar, Iran.
2- Iranian Research Center of Healthy Aging, School of Medicine, Vasei Hospital, Sabzevar University of Medical Sciences, Sabzevar, Iran.
3- Department of Midwifery, School of Nursing and Midwifery, Sabzevar University of Medical Sciences, Sabzevar, Iran.
4- Department of Nursing, Iranian Research Center of Healthy Aging, School of Nursing and Midwifery, Sabzevar University of Medical Sciences, Sabzevar, Iran. ,radmostafa633@gmail.com
2- Iranian Research Center of Healthy Aging, School of Medicine, Vasei Hospital, Sabzevar University of Medical Sciences, Sabzevar, Iran.
3- Department of Midwifery, School of Nursing and Midwifery, Sabzevar University of Medical Sciences, Sabzevar, Iran.
4- Department of Nursing, Iranian Research Center of Healthy Aging, School of Nursing and Midwifery, Sabzevar University of Medical Sciences, Sabzevar, Iran. ,
Full-Text [PDF 745 kb]
(59 Downloads)
| Abstract (HTML) (2102 Views)
Full-Text: (1 Views)
Introduction
Maternal mortality rate is a key indicator of the effectiveness of maternal and child healthcare [1]. Although maternal mortality is a critical concern, maternal morbidity occurs at a significantly higher rate. Consequently, maternal near-miss (MNM) has been proposed as a more effective indicator for evaluating and enhancing maternal health services [2]. Analyzing maternal mortality within health centers is crucial for identifying systemic weaknesses or failures and implementing necessary improvements in maternal care treatments [3]. Reducing maternal mortality is a key development goal of the third millennium. To achieve this objective, countries must establish accurate data on the causes and rates of maternal mortality [4].
During a MNM, a mother’s life can be at risk due to serious problems with her heart, lungs, kidneys, blood, liver, or brain. Heart problems may include severe shock or cardiac arrest. Breathing difficulties could involve needing help from a machine to breathe, or severe pneumonia. Kidney problems may lead to decreased urine output or kidney failure. Blood clotting problems, liver issues, such as jaundice, and neurological problems, such as seizures, coma, or stroke are also possible. In severe cases, surgery to remove the uterus may be required to stop life-threatening bleeding or infection [5].
In developing countries, the rate of mothers who give birth in hospitals and experience severe acute maternal complications has been 4-8% [6]. It has been found that performing too many cesarean sections is one of the causes of MNM [5]. The lack of facilities in people’s treatment systems significantly affects the occurrence of MNM [7]. In a study, postpartum hemorrhage is mentioned as the leading cause of maternal mortality worldwide, and the investigation and analysis of the cause of hemorrhage can increase women’s survival [3]. In a systematic study, the estimate of the MNM due to organ dysfunction was 0.42% based on mantel criteria (part of the broader framework for evaluating multiple organ dysfunction syndrome or multi-organ failure), and the rate of emergency hysterectomy was 0.039%. The meta-regression results showed that the rate of emergency hysterectomy increased by about 8% per year [8]. Anemia is a primary contributor to maternal death. Notably, a substantial proportion of MNM cases occur prior to hospital admission, leading to enduring psychological and emotional consequences for the affected women [2].
The examination of lived experiences among women surviving MNM with significant complications during pregnancy or childbirth is increasingly acknowledged as a critical tool for assessing the quality of maternity care [9]. By exploring MNM experiences, it is possible to formulate patient-centered clinical guidelines, which can optimize service delivery, promote standardization, mitigate unnecessary interventions and associated harm, reduce healthcare expenditures, and ultimately enhance the overall effectiveness of the health system [10]. The occurrence of an MNM event presents a profound stressor for mothers, who often juggle multiple responsibilities as mothers, wives, and family caregivers [11]. From a clinical perspective, MNM cases demand intensive physical care, with a primary emphasis on preserving maternal life. However, this acute focus on physiological stability can result in the inadvertent neglect of patients’ psychological and spiritual well-being [12]. Consequently, mothers may develop severe post-traumatic stress disorder, necessitating specialized mental and emotional support. Moreover, the communication of MNM-related information, which represents ‘bad news,’ can trigger significant distress in patients and their support networks [1]. As noted earlier, healthcare providers may focus on preserving the mother’s life, whereas mothers may experience profound discomfort from residual physical impairments or perceive deficiencies in their treatment. This divergence in perspectives during MNM events reveals a significant gap between mothers’ lived experiences and healthcare professionals. A comprehensive understanding of these experiences is essential to bridge this gap and enhance the quality of care. Since numerous qualitative studies have explored mothers’ experiences of near-death events, a qualitative review methodology is well-suited to integrate and synthesize these findings. Therefore, this study aimed to investigate the lived experiences of mothers with MNM events using a metasynthesis of qualitative studies.
Methods
Synthesis methodology
A systematic review of qualitative studies was conducted using the meta-synthesis method. In this study, thematic synthesis techniques were used to analyze the approach. Thematic synthesis is performed in three stages: line-by-line coding of the text, formation of descriptive themes, and production of analytical themes [13]. We included qualitative studies where the focus was on women who experienced a near-miss event. The key search term was “near miss” OR (experience AND (obstetric* OR matern* OR pregnant *OR woman OR women and “qualitative” (Table 1).
.PNG)
Inclusion and exclusion criteria
The inclusion criteria included mothers’ near-death experiences, which were mentioned in the title, abstract, or body of the article. Documents requiring full-text review were thoroughly studied. The exclusion criteria included studies on near-loss of an infant, non-Persian or non-English articles, conference abstracts, letters to the editor, case reports, and quantitative studies.
Data sources
Electronic search strategy
Studies were identified by searching electronic databases. Search were conducted to August 2024 in the MEDLINE database through PubMed, the Social Science Citation Index (SSCI) via Web of Science, the Cochrane Library, Scopus, and Magiran without date restrictions using the search strategy (Table 1).
Study screening methods
In conducting this review, we followed the guidelines reported in the enhancing transparency in reporting the synthesis of qualitative research (ENTREQ) statement to increase transparency in reporting the synthesis of qualitative evidence [14].
Study characteristics
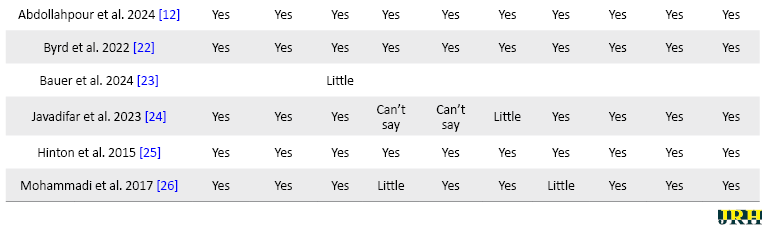
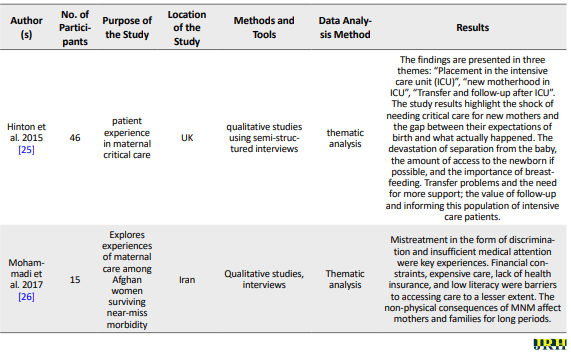
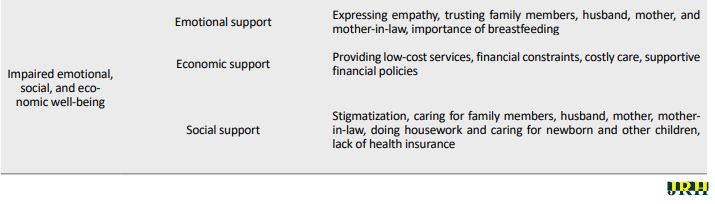
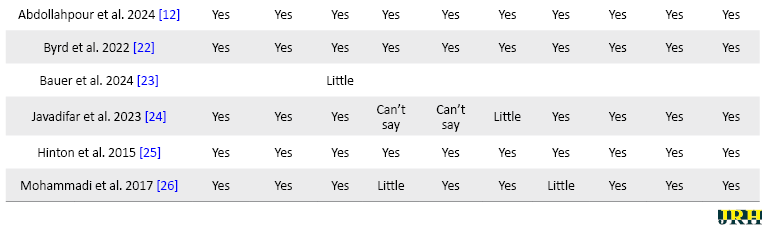
The quality of each qualitative study was independently evaluated by two authors using the critical appraisal skills program (CASP) tool [15]. The appraisal focused on several key criteria, including: The clarity of research aims, the appropriateness of the chosen qualitative methodology, the alignment of study design with research objectives, the suitability of the sampling strategy, the effectiveness of data collection in addressing research questions, the researchers’ attention to their relationship with participants, adherence to ethical standards, the rigor of data analysis, the clear presentation of findings, and the overall value of the research (Table 2).
.PNG)
Studies were selected for inclusion by two independent researchers. Out of 97938 studies identified, 16 met the inclusion criteria (Figure 1).
.PNG)
.PNG)
The full text of all eligible documents was reviewed in detail. Two researchers extracted data from the studies included in the analysis using a pre-prepared data extraction form. Any disagreement was resolved by referring to the third author and their consensus.
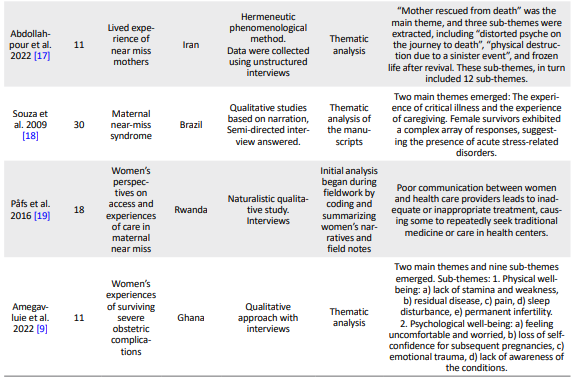
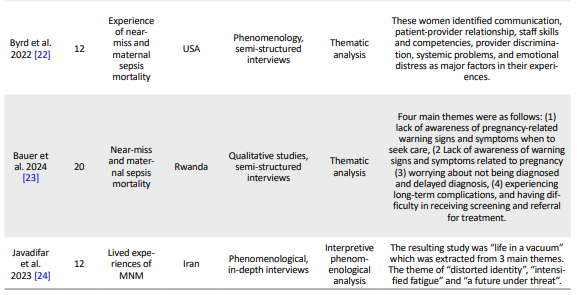
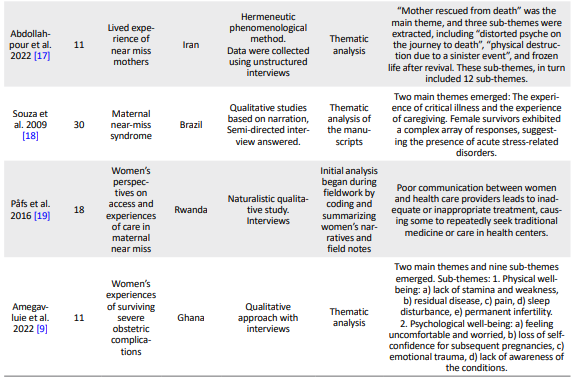
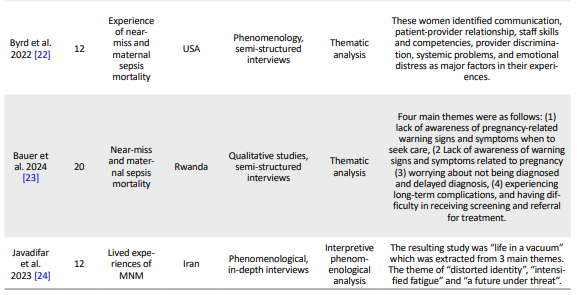
Two authors independently extracted data regarding study setting, sample, methods, data collection tools, analysis, and results (Table 3).
.PNG)
.PNG)
Separately, they created an Excel file to document reported experiences, applying the thematic analysis method [13].
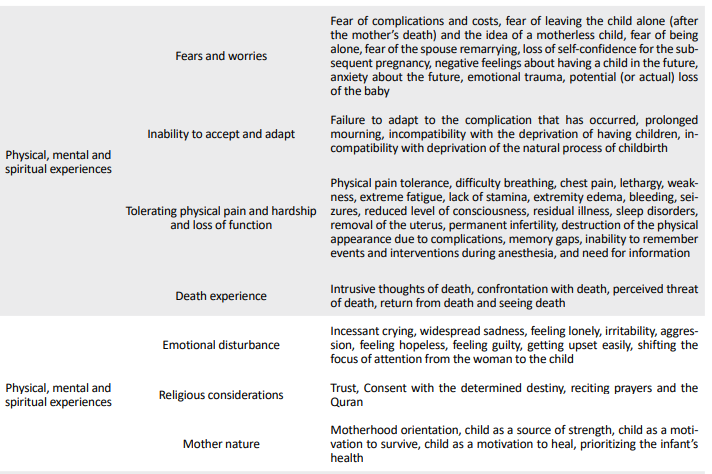
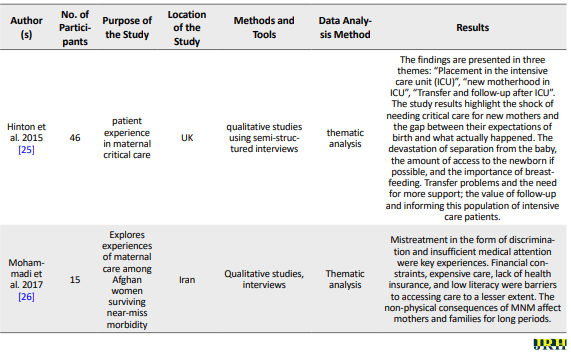
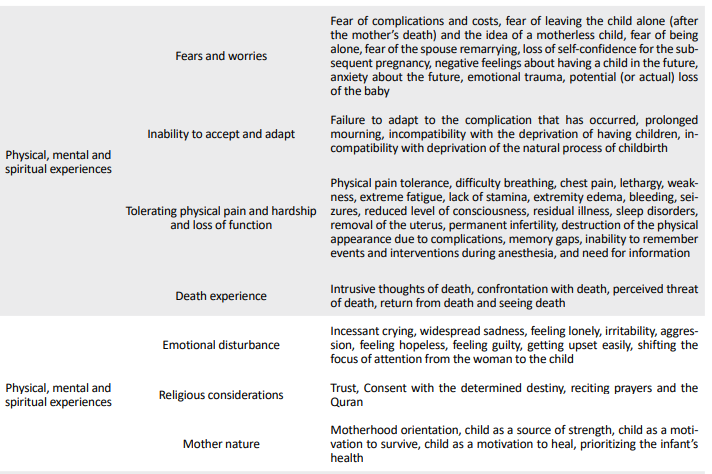
In the initial coding round, emerging themes were synthesized into descriptive themes. Descriptive themes are extracted from the initial codes that are close to the original concept in the studies. After obtaining the descriptive themes, they were interpreted, and the analytical themes were derived. Two researchers independently applied initial coding, manually sorting text units into codes and descriptive themes until analytical themes emerged. Discrepancies in thematic analysis were resolved through discussion and consensus, with input from a third author. MAXQDA software, version 24 and Word were used for data extraction (Table 4).
.PNG)
Two authors abstracted the MNM experiences reported in the included studies, illustrated by descriptive themes, and developed key recommendations for the appropriate treatment of patients with MNM experiences. This process was first performed independently by each author and then reviewed with a third author until consensus was reached.
Results
Of the 97938 studies identified, 16 were reviewed. By country, the papers were from the USA (n=1), Iran (n=5), Brazil (n=1), Rwanda (n=2), Malawi (n=1), Malaysia (n=1), Ghana (n=2), and the UK (n=1). The studies combined a variety of methodological approaches, such as grounded theory, phenomenological, and content analysis.
“Perception of the quality of care”, “physical, mental and spiritual experiences”, and “disturbance in emotional, social and economic well-being” were the three main categories in the recent metasynthesis, which sub-categories for the perception of the quality of care include mismanagement of the medical team, access to health care facilities, communication problems of the medical team with the patient and the patient’s awareness. The subcategories of physical, psychological, and spiritual experiences included fears, worries, inability to accept and adapt, endure physical pain and hardship, and loss of function, experience of death, emotional disturbance, religious concerns, and maternal nature. For the emotional, social, and economic well-being category, the subclasses included emotional, economic, and social support.
Perception of quality of care
The sub-categories of perception of the quality of care included mismanagement of the medical team, access to health care facilities, communication problems between the medical team and the patient, and patient awareness.
“The first doctor said she should have a cesarean section, but when the shift changed, the next doctor who came said she should have a natural birth [1]”.
Mismanagement of the medical team
According to the available documents, the experiences of MNM showed factors, such as delay in diagnosis and implementation of treatment, delay of healthcare providers in transferring the patient to a specialized center, delay in therapeutic intervention, errors and medical malpractice, lack of skill and competence of staff, misdiagnosis, inadequacy of guidelines based on the evidence and protocols, problem in the referral system, inadequacy or lack of emergency management, lack of support and carelessness of the treatment staff [5, 10, 18, 25], discrimination in the provision of services, and the mismanagement of the medical team [26].
Access to health care facilities
According to the experiences of MNM, the lack of human and physical resources in healthcare, distance, difficulty in transportation, high costs of medical care, lack of insurance, and delay in seeking care by women were considered the factors of insufficient access to healthcare facilities [1, 5, 10, 17, 19, 20, 22].
The communication problem of the medical team and informing the patient
Communication problems of the medical team observed in the experiences of MNM included ineffective interpersonal communication between the medical team and the patient [5, 18, 19], lack of information and awareness of the patient due to lack of timely notification, increasing family information to support the mother, the need for information about the patient’s current problem, to be informed of the process of care [9, 10, 12, 21], the mother’s desire to be involved in treatment and therapeutic interventions, being encouraged to do so [20], the mother’s unfamiliarity with treatment and therapeutic interventions, the fear of the mother asking questions from the doctors, [17, 18], and the mother’s desire to seek care [1, 5, 24].
Physical, mental, and spiritual experiences
The subcategories of physical, psychological, and spiritual experiences included fears and worries, inability to accept and adapt, endure physical pain and hardship, and loss of function, experience of death, emotional disturbance, religious concerns, and maternal nature.
"I thought I had died, obviously, when I was sleeping, I dreamed that I had gone, it was a desert, how can I say that world? Then a woman came with a black veil and took my hand to get up, but I couldn’t get up... [10]".
Fears and worries
Fear of complications and costs, fear of the child being left alone (after the mother’s death) and the thought of a motherless child, fear of being alone, fear of the spouse remarrying due to the loss of the uterus or the inability to conceive, loss of hope and anxiety about the subsequent pregnancy, negative feelings about future childbearing, anxiety about the future, emotional trauma, and possible (or actual) loss of the baby [1, 9, 17] were fears and concerns mentioned in the literature based on MNM experiences.
Inability to accept and adapt
Some of the experiences mentioned in the documents included not adapting to the complication, prolonged mourning, not adapting to being deprived of having children, and not adapting to being deprived of the natural process of childbirth [1, 5, 17, 20].
Tolerating physical pain, difficulty, and loss of function
The codes obtained from the documentation of mothers’ experiences regarding the tolerance of pain and physical difficulty and loss of function, pointed out to tolerated physical pain, difficult breathing, chest pain, lethargy, weakness, extreme fatigue, lack of energy, limb edema, bleeding, convulsions, reduced level of consciousness, residual disease, sleep disorder, removal of the uterus, permanent infertility, destruction of the physical body due to complications, memory gap, and failure to remember events and interventions during unconsciousness and the need for information [1, 5, 18].
Death experience
It seems that one of the experiences of the mothers was the experience of death, so that they had disturbing thoughts of death during the illness, and sometimes still have them. They experienced facing death, felt the perceived threat of death, and felt the return from death; in other words, they saw death with their own eyes [1, 5, 9, 17, 20].
Emotional turmoil
Experiences, such as incessant crying, widespread sadness, feeling lonely, irritability, aggression, feeling hopeless, feeling guilty, getting hurt early, and feeling shifting the center of attention from the woman to the child are signs of emotional disturbance [9, 20].
Religious considerations
During the illness and its complications, according to the literature, the mothers mentioned in their experiences religious attentions, including trust in God Almighty, satisfaction with the determined destiny, reading Zikr and the Qur’an, and calling on Imams [1, 5, 17].
Maternal nature
MNM experiences showed they had tendency to become a mother, and that during illness and painful events; the child was considered as a source of mother’s strength and the motivation to survive or continue treatment. Moreover, mothers pointed out that they prioritize their babies’ health [5, 17, 18].
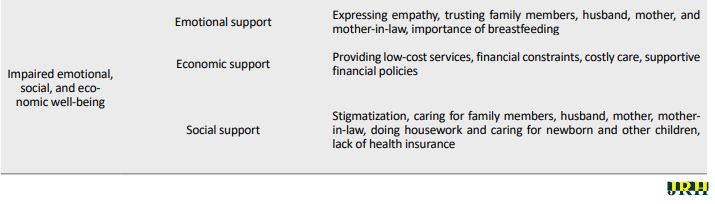
Disruption of emotional, social, and economic well-being
For the emotional, social and economic well-being disturbance category, the subcategories included emotional, economic and social support.
"... On the one hand, I feel sad about the limb defect; on the other hand, the high cost of frequent visits to the doctor has caused turmoil for our family [18]"
Emotional support
Mothers expressed the need for emotional support, including the need to express empathy, trust in family members (husband, mother, mother-in-law), and the importance of feeding their baby with breast milk [1, 5, 9, 12, 18].
Economic support
Due to the high cost of medical care, dying mothers had financial constraints and needed economic support. They also called for supportive financial policies and the provision of low-cost services [5, 12, 19, 20].
Social support
Mothers need family support included not stigmatizing, taking care of family members, husband, mother, mother-in-law in doing housework and taking care of baby and other children. Also, they need social and insurance support due to the lack of health insurance [1, 5, 18-20].
Discussion
The findings of the study showed that the quality of care is affected by factors, such as mismanagement of the medical team, difficulty in accessing healthcare facilities, communication problems between the medical team and the patient, and lack of awareness. In addition to these fears and worries, the inability to accept and adapt, endure pain and physical hardship and loss of function, experience of death, emotional turmoil, religious concerns, and maternal nature, among the physical, psychological, and spiritual experiences of mothers who have the experience of MNM. The need for emotional, social and economic support was indicative of the disturbance in the emotional, social and economic well-being of mothers who experienced MNM. Therefore, suggestions are made in the discussion to improve services to these mothers.
To improve the quality of care and prevent mismanagement by the medical team, evidence-based and updated standard guidelines should be used, available at medical and health centers [1, 5, 10]. Continuous and up-to-date training should performed for the medical personnel and team to improve their skills and competence; to reduce errors and medical malpractice, delay in diagnosis, prevent misdiagnosis and the delay of health care providers in transferring the patient to a specialized center, this work will also reduce the delay in therapeutic intervention and emergency management of the problem [5, 10, 18, 20]. The number of personnel should be sufficient to provide care, and experienced personnel must be present in different shifts. Sufficient and healthy hospital facilities and equipment are accessible to the personnel. On the other hand, the communication problems between the medical team and the patient should be resolved, and the awareness of the patients should be increased. Training of communication skills and management of the medical team, including doctors and nurses, should be done. To ensure effective leadership and coordination between the medical team, supervisors, and matrons play a key role in this regard [1, 5, 19, 20]. In the event of a medical error, it is necessary to analyze the root of the problem, learn from it, and inform all personnel to avoid the problem from occurring again. Support continuing medical education [12]. Considering the many problems that arise for patients in the physical, mental, and psychological dimensions, physical problems should be prioritized to prevent physical complications and alleviate pain and suffering. For mental and psychological problems, psychologists and spiritual experts should be consulted to provide the necessary care in this field. Necessary training and counseling should be provided to the husband and important family members who play a role in caring for the mother so that they can have the necessary emotional and social support from the mother [1, 5, 12]. In addition, policymakers in the field of medical sciences should address patients’ economic concerns by covering supplementary insurance [12, 19].
Emotional trauma emerged as a concept experienced by women in this study. Similarly, studies showed that women experience intense fear of death and anxiety about losing their babies [5, 20]. The loss of a baby significantly worsens psychological and emotional trauma, leading to more negative emotions. Women with severe complications experienced poorer mental health in the postpartum period. Similar to this study, where reliance and hope in God helped prevent emotional harm, in other studies, religious beliefs were a common coping mechanism [20, 21].
In this study, women’s experiences emphasized the importance of clear communication, information, and respectful staff attitudes. Similarly, another study showed that in interactions with patients, some healthcare providers had poor communication, displayed impolite behavior, and showed negative behavior when asked for help [21]. They mentioned feelings of neglect, discrimination, and verbal abuse during care, which aligns with the results of this study. Respectful staff behavior, including active listening, empathy, and attention to patients’ needs, is of great importance. Inappropriate, rude, or discriminatory behavior can significantly affect patients’ experiences. Training staff in communication and behavioral skills, including empathy, active listening, and conflict management, can help improve the quality of healthcare.
Conclusion
Mismanagement of the medical team, difficulty in accessing healthcare facilities, communication problems between the medical team and the patient, and lack of informing may affect the quality of care. In addition to these fears and worries, the inability to accept and adapt, endure pain and physical hardship, and loss of function, experience of death, emotional turmoil, religious concerns, and maternal nature were among the physical, psychological, and spiritual experiences of mothers with MNM. The need for emotional, social, and economic support was indicative of disturbances in the emotional, social, and economic well-being of mothers who experienced an MNM.
It is suggested that the medical team improve the communication among themselves and between the medical team and the patient to prevent and reduce complications, such as MNM. During hospitalization, psychological counseling should be provided to alleviate the psychological pain experienced by patients. After discharge from the hospital, insurance support should be provided to reduce economic costs. In addition, family counseling should be conducted to reduce the fear of the husband’s remarriage and re-pregnancy.
Limitations and recommendations
The strengths of this study were that a standard search strategy was used across several electronic databases. The main limitation of this study was that the search was restricted to only Persian and English languages. Despite the aforementioned limitation, this review identified a significant number of high-quality studies from Asian and African countries. Therefore, the findings of the review can be largely generalized to these contexts.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Sabzevar University of Medical Sciences, Sabzevar, Iran (Code: IR.MEDSAB.REC.1403.104).
Funding
This research did not receive grants from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and supervision: Mostafa Rad, Narjes Frohar; Methodology: Mostafa Rad, Marzieh Torkmannejad Sabzevari and Mohammadreza Shegarf Nakhaie; Data collection, investigation, and writing: All authors.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgments
The authors express their gratitude and appreciation to the Research Vice-Chancellor of Sabzevar University of Medical Sciences and the Clinical Research Center, who were responsible for financing this project.
Maternal mortality rate is a key indicator of the effectiveness of maternal and child healthcare [1]. Although maternal mortality is a critical concern, maternal morbidity occurs at a significantly higher rate. Consequently, maternal near-miss (MNM) has been proposed as a more effective indicator for evaluating and enhancing maternal health services [2]. Analyzing maternal mortality within health centers is crucial for identifying systemic weaknesses or failures and implementing necessary improvements in maternal care treatments [3]. Reducing maternal mortality is a key development goal of the third millennium. To achieve this objective, countries must establish accurate data on the causes and rates of maternal mortality [4].
During a MNM, a mother’s life can be at risk due to serious problems with her heart, lungs, kidneys, blood, liver, or brain. Heart problems may include severe shock or cardiac arrest. Breathing difficulties could involve needing help from a machine to breathe, or severe pneumonia. Kidney problems may lead to decreased urine output or kidney failure. Blood clotting problems, liver issues, such as jaundice, and neurological problems, such as seizures, coma, or stroke are also possible. In severe cases, surgery to remove the uterus may be required to stop life-threatening bleeding or infection [5].
In developing countries, the rate of mothers who give birth in hospitals and experience severe acute maternal complications has been 4-8% [6]. It has been found that performing too many cesarean sections is one of the causes of MNM [5]. The lack of facilities in people’s treatment systems significantly affects the occurrence of MNM [7]. In a study, postpartum hemorrhage is mentioned as the leading cause of maternal mortality worldwide, and the investigation and analysis of the cause of hemorrhage can increase women’s survival [3]. In a systematic study, the estimate of the MNM due to organ dysfunction was 0.42% based on mantel criteria (part of the broader framework for evaluating multiple organ dysfunction syndrome or multi-organ failure), and the rate of emergency hysterectomy was 0.039%. The meta-regression results showed that the rate of emergency hysterectomy increased by about 8% per year [8]. Anemia is a primary contributor to maternal death. Notably, a substantial proportion of MNM cases occur prior to hospital admission, leading to enduring psychological and emotional consequences for the affected women [2].
The examination of lived experiences among women surviving MNM with significant complications during pregnancy or childbirth is increasingly acknowledged as a critical tool for assessing the quality of maternity care [9]. By exploring MNM experiences, it is possible to formulate patient-centered clinical guidelines, which can optimize service delivery, promote standardization, mitigate unnecessary interventions and associated harm, reduce healthcare expenditures, and ultimately enhance the overall effectiveness of the health system [10]. The occurrence of an MNM event presents a profound stressor for mothers, who often juggle multiple responsibilities as mothers, wives, and family caregivers [11]. From a clinical perspective, MNM cases demand intensive physical care, with a primary emphasis on preserving maternal life. However, this acute focus on physiological stability can result in the inadvertent neglect of patients’ psychological and spiritual well-being [12]. Consequently, mothers may develop severe post-traumatic stress disorder, necessitating specialized mental and emotional support. Moreover, the communication of MNM-related information, which represents ‘bad news,’ can trigger significant distress in patients and their support networks [1]. As noted earlier, healthcare providers may focus on preserving the mother’s life, whereas mothers may experience profound discomfort from residual physical impairments or perceive deficiencies in their treatment. This divergence in perspectives during MNM events reveals a significant gap between mothers’ lived experiences and healthcare professionals. A comprehensive understanding of these experiences is essential to bridge this gap and enhance the quality of care. Since numerous qualitative studies have explored mothers’ experiences of near-death events, a qualitative review methodology is well-suited to integrate and synthesize these findings. Therefore, this study aimed to investigate the lived experiences of mothers with MNM events using a metasynthesis of qualitative studies.
Methods
Synthesis methodology
A systematic review of qualitative studies was conducted using the meta-synthesis method. In this study, thematic synthesis techniques were used to analyze the approach. Thematic synthesis is performed in three stages: line-by-line coding of the text, formation of descriptive themes, and production of analytical themes [13]. We included qualitative studies where the focus was on women who experienced a near-miss event. The key search term was “near miss” OR (experience AND (obstetric* OR matern* OR pregnant *OR woman OR women and “qualitative” (Table 1).
.PNG)
Inclusion and exclusion criteria
The inclusion criteria included mothers’ near-death experiences, which were mentioned in the title, abstract, or body of the article. Documents requiring full-text review were thoroughly studied. The exclusion criteria included studies on near-loss of an infant, non-Persian or non-English articles, conference abstracts, letters to the editor, case reports, and quantitative studies.
Data sources
Electronic search strategy
Studies were identified by searching electronic databases. Search were conducted to August 2024 in the MEDLINE database through PubMed, the Social Science Citation Index (SSCI) via Web of Science, the Cochrane Library, Scopus, and Magiran without date restrictions using the search strategy (Table 1).
Study screening methods
In conducting this review, we followed the guidelines reported in the enhancing transparency in reporting the synthesis of qualitative research (ENTREQ) statement to increase transparency in reporting the synthesis of qualitative evidence [14].
Study characteristics
The quality of each qualitative study was independently evaluated by two authors using the critical appraisal skills program (CASP) tool [15]. The appraisal focused on several key criteria, including: The clarity of research aims, the appropriateness of the chosen qualitative methodology, the alignment of study design with research objectives, the suitability of the sampling strategy, the effectiveness of data collection in addressing research questions, the researchers’ attention to their relationship with participants, adherence to ethical standards, the rigor of data analysis, the clear presentation of findings, and the overall value of the research (Table 2).
.PNG)
Studies were selected for inclusion by two independent researchers. Out of 97938 studies identified, 16 met the inclusion criteria (Figure 1).
.PNG)
.PNG)
The full text of all eligible documents was reviewed in detail. Two researchers extracted data from the studies included in the analysis using a pre-prepared data extraction form. Any disagreement was resolved by referring to the third author and their consensus.
Two authors independently extracted data regarding study setting, sample, methods, data collection tools, analysis, and results (Table 3).
.PNG)
.PNG)
Separately, they created an Excel file to document reported experiences, applying the thematic analysis method [13].
In the initial coding round, emerging themes were synthesized into descriptive themes. Descriptive themes are extracted from the initial codes that are close to the original concept in the studies. After obtaining the descriptive themes, they were interpreted, and the analytical themes were derived. Two researchers independently applied initial coding, manually sorting text units into codes and descriptive themes until analytical themes emerged. Discrepancies in thematic analysis were resolved through discussion and consensus, with input from a third author. MAXQDA software, version 24 and Word were used for data extraction (Table 4).
.PNG)
Two authors abstracted the MNM experiences reported in the included studies, illustrated by descriptive themes, and developed key recommendations for the appropriate treatment of patients with MNM experiences. This process was first performed independently by each author and then reviewed with a third author until consensus was reached.
Results
Of the 97938 studies identified, 16 were reviewed. By country, the papers were from the USA (n=1), Iran (n=5), Brazil (n=1), Rwanda (n=2), Malawi (n=1), Malaysia (n=1), Ghana (n=2), and the UK (n=1). The studies combined a variety of methodological approaches, such as grounded theory, phenomenological, and content analysis.
“Perception of the quality of care”, “physical, mental and spiritual experiences”, and “disturbance in emotional, social and economic well-being” were the three main categories in the recent metasynthesis, which sub-categories for the perception of the quality of care include mismanagement of the medical team, access to health care facilities, communication problems of the medical team with the patient and the patient’s awareness. The subcategories of physical, psychological, and spiritual experiences included fears, worries, inability to accept and adapt, endure physical pain and hardship, and loss of function, experience of death, emotional disturbance, religious concerns, and maternal nature. For the emotional, social, and economic well-being category, the subclasses included emotional, economic, and social support.
Perception of quality of care
The sub-categories of perception of the quality of care included mismanagement of the medical team, access to health care facilities, communication problems between the medical team and the patient, and patient awareness.
“The first doctor said she should have a cesarean section, but when the shift changed, the next doctor who came said she should have a natural birth [1]”.
Mismanagement of the medical team
According to the available documents, the experiences of MNM showed factors, such as delay in diagnosis and implementation of treatment, delay of healthcare providers in transferring the patient to a specialized center, delay in therapeutic intervention, errors and medical malpractice, lack of skill and competence of staff, misdiagnosis, inadequacy of guidelines based on the evidence and protocols, problem in the referral system, inadequacy or lack of emergency management, lack of support and carelessness of the treatment staff [5, 10, 18, 25], discrimination in the provision of services, and the mismanagement of the medical team [26].
Access to health care facilities
According to the experiences of MNM, the lack of human and physical resources in healthcare, distance, difficulty in transportation, high costs of medical care, lack of insurance, and delay in seeking care by women were considered the factors of insufficient access to healthcare facilities [1, 5, 10, 17, 19, 20, 22].
The communication problem of the medical team and informing the patient
Communication problems of the medical team observed in the experiences of MNM included ineffective interpersonal communication between the medical team and the patient [5, 18, 19], lack of information and awareness of the patient due to lack of timely notification, increasing family information to support the mother, the need for information about the patient’s current problem, to be informed of the process of care [9, 10, 12, 21], the mother’s desire to be involved in treatment and therapeutic interventions, being encouraged to do so [20], the mother’s unfamiliarity with treatment and therapeutic interventions, the fear of the mother asking questions from the doctors, [17, 18], and the mother’s desire to seek care [1, 5, 24].
Physical, mental, and spiritual experiences
The subcategories of physical, psychological, and spiritual experiences included fears and worries, inability to accept and adapt, endure physical pain and hardship, and loss of function, experience of death, emotional disturbance, religious concerns, and maternal nature.
"I thought I had died, obviously, when I was sleeping, I dreamed that I had gone, it was a desert, how can I say that world? Then a woman came with a black veil and took my hand to get up, but I couldn’t get up... [10]".
Fears and worries
Fear of complications and costs, fear of the child being left alone (after the mother’s death) and the thought of a motherless child, fear of being alone, fear of the spouse remarrying due to the loss of the uterus or the inability to conceive, loss of hope and anxiety about the subsequent pregnancy, negative feelings about future childbearing, anxiety about the future, emotional trauma, and possible (or actual) loss of the baby [1, 9, 17] were fears and concerns mentioned in the literature based on MNM experiences.
Inability to accept and adapt
Some of the experiences mentioned in the documents included not adapting to the complication, prolonged mourning, not adapting to being deprived of having children, and not adapting to being deprived of the natural process of childbirth [1, 5, 17, 20].
Tolerating physical pain, difficulty, and loss of function
The codes obtained from the documentation of mothers’ experiences regarding the tolerance of pain and physical difficulty and loss of function, pointed out to tolerated physical pain, difficult breathing, chest pain, lethargy, weakness, extreme fatigue, lack of energy, limb edema, bleeding, convulsions, reduced level of consciousness, residual disease, sleep disorder, removal of the uterus, permanent infertility, destruction of the physical body due to complications, memory gap, and failure to remember events and interventions during unconsciousness and the need for information [1, 5, 18].
Death experience
It seems that one of the experiences of the mothers was the experience of death, so that they had disturbing thoughts of death during the illness, and sometimes still have them. They experienced facing death, felt the perceived threat of death, and felt the return from death; in other words, they saw death with their own eyes [1, 5, 9, 17, 20].
Emotional turmoil
Experiences, such as incessant crying, widespread sadness, feeling lonely, irritability, aggression, feeling hopeless, feeling guilty, getting hurt early, and feeling shifting the center of attention from the woman to the child are signs of emotional disturbance [9, 20].
Religious considerations
During the illness and its complications, according to the literature, the mothers mentioned in their experiences religious attentions, including trust in God Almighty, satisfaction with the determined destiny, reading Zikr and the Qur’an, and calling on Imams [1, 5, 17].
Maternal nature
MNM experiences showed they had tendency to become a mother, and that during illness and painful events; the child was considered as a source of mother’s strength and the motivation to survive or continue treatment. Moreover, mothers pointed out that they prioritize their babies’ health [5, 17, 18].
Disruption of emotional, social, and economic well-being
For the emotional, social and economic well-being disturbance category, the subcategories included emotional, economic and social support.
"... On the one hand, I feel sad about the limb defect; on the other hand, the high cost of frequent visits to the doctor has caused turmoil for our family [18]"
Emotional support
Mothers expressed the need for emotional support, including the need to express empathy, trust in family members (husband, mother, mother-in-law), and the importance of feeding their baby with breast milk [1, 5, 9, 12, 18].
Economic support
Due to the high cost of medical care, dying mothers had financial constraints and needed economic support. They also called for supportive financial policies and the provision of low-cost services [5, 12, 19, 20].
Social support
Mothers need family support included not stigmatizing, taking care of family members, husband, mother, mother-in-law in doing housework and taking care of baby and other children. Also, they need social and insurance support due to the lack of health insurance [1, 5, 18-20].
Discussion
The findings of the study showed that the quality of care is affected by factors, such as mismanagement of the medical team, difficulty in accessing healthcare facilities, communication problems between the medical team and the patient, and lack of awareness. In addition to these fears and worries, the inability to accept and adapt, endure pain and physical hardship and loss of function, experience of death, emotional turmoil, religious concerns, and maternal nature, among the physical, psychological, and spiritual experiences of mothers who have the experience of MNM. The need for emotional, social and economic support was indicative of the disturbance in the emotional, social and economic well-being of mothers who experienced MNM. Therefore, suggestions are made in the discussion to improve services to these mothers.
To improve the quality of care and prevent mismanagement by the medical team, evidence-based and updated standard guidelines should be used, available at medical and health centers [1, 5, 10]. Continuous and up-to-date training should performed for the medical personnel and team to improve their skills and competence; to reduce errors and medical malpractice, delay in diagnosis, prevent misdiagnosis and the delay of health care providers in transferring the patient to a specialized center, this work will also reduce the delay in therapeutic intervention and emergency management of the problem [5, 10, 18, 20]. The number of personnel should be sufficient to provide care, and experienced personnel must be present in different shifts. Sufficient and healthy hospital facilities and equipment are accessible to the personnel. On the other hand, the communication problems between the medical team and the patient should be resolved, and the awareness of the patients should be increased. Training of communication skills and management of the medical team, including doctors and nurses, should be done. To ensure effective leadership and coordination between the medical team, supervisors, and matrons play a key role in this regard [1, 5, 19, 20]. In the event of a medical error, it is necessary to analyze the root of the problem, learn from it, and inform all personnel to avoid the problem from occurring again. Support continuing medical education [12]. Considering the many problems that arise for patients in the physical, mental, and psychological dimensions, physical problems should be prioritized to prevent physical complications and alleviate pain and suffering. For mental and psychological problems, psychologists and spiritual experts should be consulted to provide the necessary care in this field. Necessary training and counseling should be provided to the husband and important family members who play a role in caring for the mother so that they can have the necessary emotional and social support from the mother [1, 5, 12]. In addition, policymakers in the field of medical sciences should address patients’ economic concerns by covering supplementary insurance [12, 19].
Emotional trauma emerged as a concept experienced by women in this study. Similarly, studies showed that women experience intense fear of death and anxiety about losing their babies [5, 20]. The loss of a baby significantly worsens psychological and emotional trauma, leading to more negative emotions. Women with severe complications experienced poorer mental health in the postpartum period. Similar to this study, where reliance and hope in God helped prevent emotional harm, in other studies, religious beliefs were a common coping mechanism [20, 21].
In this study, women’s experiences emphasized the importance of clear communication, information, and respectful staff attitudes. Similarly, another study showed that in interactions with patients, some healthcare providers had poor communication, displayed impolite behavior, and showed negative behavior when asked for help [21]. They mentioned feelings of neglect, discrimination, and verbal abuse during care, which aligns with the results of this study. Respectful staff behavior, including active listening, empathy, and attention to patients’ needs, is of great importance. Inappropriate, rude, or discriminatory behavior can significantly affect patients’ experiences. Training staff in communication and behavioral skills, including empathy, active listening, and conflict management, can help improve the quality of healthcare.
Conclusion
Mismanagement of the medical team, difficulty in accessing healthcare facilities, communication problems between the medical team and the patient, and lack of informing may affect the quality of care. In addition to these fears and worries, the inability to accept and adapt, endure pain and physical hardship, and loss of function, experience of death, emotional turmoil, religious concerns, and maternal nature were among the physical, psychological, and spiritual experiences of mothers with MNM. The need for emotional, social, and economic support was indicative of disturbances in the emotional, social, and economic well-being of mothers who experienced an MNM.
It is suggested that the medical team improve the communication among themselves and between the medical team and the patient to prevent and reduce complications, such as MNM. During hospitalization, psychological counseling should be provided to alleviate the psychological pain experienced by patients. After discharge from the hospital, insurance support should be provided to reduce economic costs. In addition, family counseling should be conducted to reduce the fear of the husband’s remarriage and re-pregnancy.
Limitations and recommendations
The strengths of this study were that a standard search strategy was used across several electronic databases. The main limitation of this study was that the search was restricted to only Persian and English languages. Despite the aforementioned limitation, this review identified a significant number of high-quality studies from Asian and African countries. Therefore, the findings of the review can be largely generalized to these contexts.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Sabzevar University of Medical Sciences, Sabzevar, Iran (Code: IR.MEDSAB.REC.1403.104).
Funding
This research did not receive grants from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and supervision: Mostafa Rad, Narjes Frohar; Methodology: Mostafa Rad, Marzieh Torkmannejad Sabzevari and Mohammadreza Shegarf Nakhaie; Data collection, investigation, and writing: All authors.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgments
The authors express their gratitude and appreciation to the Research Vice-Chancellor of Sabzevar University of Medical Sciences and the Clinical Research Center, who were responsible for financing this project.
Type of Study: Review Article |
Subject:
● Service Quality
Received: 2024/11/23 | Accepted: 2025/04/30 | Published: 2026/01/1
Received: 2024/11/23 | Accepted: 2025/04/30 | Published: 2026/01/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |