Volume 13, Issue 6 (Nov & Dec 2023)
J Research Health 2023, 13(6): 447-456 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Momayyezi M, Peigan P, Fallahzadeh H, Sefidkar R. Poisonings During the COVID-19 Pandemic: Attention to Children and Adolescents Admitted to the Referral Teaching Hospitals of Yazd and Taft Cities, Iran. J Research Health 2023; 13 (6) :447-456
URL: http://jrh.gmu.ac.ir/article-1-2160-en.html
URL: http://jrh.gmu.ac.ir/article-1-2160-en.html
1- Departments of Biostatistics and Epidemiology, Center for Healthcare Data Modeling, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
2- Departments of Biostatistics and Epidemiology, Center for Healthcare Data Modeling, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,Hofaab@yahoo.com
2- Departments of Biostatistics and Epidemiology, Center for Healthcare Data Modeling, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,
Full-Text [PDF 618 kb]
(356 Downloads)
| Abstract (HTML) (1257 Views)
Full-Text: (323 Views)
1. Introduction
The new coronavirus 2019 (COVID-19) was recorded for the first time on December 26, 2019, in Wuhan City, China [1]. The virus gradually expanded to other countries until the World Health Organization (WHO) declared COVID-19 a pandemic on March 11, 2020 [2]. The first COVID-19 case in Iran was reported on February 19, 2020, in Qom City, Iran [3]. WHO suggested preventive measures and healthy lifestyles to protect individuals against the infection. One of the best WHO advice was to disinfect hands with soap or ethanol-based (>60% ethanol) hand sanitizers [4]. A study in China demonstrated that the best way to reduce the transmission of COVID-19 among people in the community is to carry out health measures, impose quarantine, avoid gatherings, timely diagnosis, and patient care in hospitals [5]. Alimohamadi et al. reported that the spread of COVID-19 in Iran can be reduced by various interventions, such as health education, preventing the formation of human gatherings, quarantine, and separation of patients during the period of the disease from the rest of the community [6].
With the increase in COVID-19 patients in Iran, several approaches were considered to prevent the disease, including using alcohol-based disinfection solutions commonly available to the general public [7]. By shutting down schools, children who had to stay at home were in contact with hazardous products, such as medications, alcohol, and disinfectants [8]. On the other hand, misconceptions about the use of alcoholic beverages to disinfect the mouth and throat (for instance, gargling alcohol) may increase poisoning in adolescents [9, 10]. Fear of COVID-19 changed people’s health behaviors. Excessive cleaning and disinfection of the house and improper use of bleaches and disinfectants became more common [11]. Also, the increasing demand for hand sanitizers led to the production of hand sanitizers with inappropriate proportions of ethanol (<60%) or hand sanitizers containing methanol [12]. Alcohol-based disinfectants affect human health through ingestion, inhalation, or skin contact [13]. After the onset of the COVID-19 pandemic in Iran, alcohol poisoning increased in some areas, leading to deaths. All provinces reported cases of methanol poisoning [14]. The lack of public awareness about the prevention and treatment of COVID-19, subjects’ lack of awareness about different types of alcohol, the sale of illegal and non-standard alcohol, and the spread of rumors and disinformation through social media about COVID-19 and its prevention methods were among the reasons for the increase of alcohol poisoning during the pandemic in Iran [15].
A study examining alcohol poisoning in Iranian children and adolescents demonstrated that the prevalence of alcohol poisoning during the COVID-19 pandemic was associated with increased hospitalization rates among children and adolescents [16]. Given that the prevalence of poisoning and its causes in children and adolescents during the COVID-19 pandemic in Iran remains unknown, the researchers decided to compare the poisoning on children under the age of 15 years who were admitted to the referral teaching hospitals of Yazd and Taft cities, Iran, during the first wave of COVID-19 versus its previous year (pre-COVID-19 period in 2019).
2. Methods
Study design
This analytic, cross-sectional study was conducted based on the administrative data obtained from the referral teaching hospital in Yazd and Taft cities, Iran. In this study, the data were collected by census. The information of all children under the age of 15 years admitted to the referral teaching hospital in the selected two cities (Shahid Sadoughi Hospital in Yazd City, Iran, and Shahid Beheshti Hospital in Taft City, Iran) due to poisoning was examined. Accordingly, 312 cases in pre-COVID-19 and 205 cases during the COVID-19 pandemic were examined. The study period was from February 19, 2020, to February 18, 2021 (12 months of the COVID-19 pandemic) compared to 2019 as the reference period (pre-COVID). The inclusion criteria were being under the age of 18 years, being a native of Yazd Province, Iran, and being hospitalized with a diagnosis of poisoning in the hospital record. Outpatients with alcohol exposure and incomplete records (such as not mentioning the cause of poisoning) were excluded from the study.
Data collection
The data collection method in this study included a checklist comprised of age, gender, duration of hospitalization, location (urban, rural), the season of occurrence of poisoning, cause of poisoning (medications, alcohol, oil and its derivatives, food, drugs-opioids, detergents, pesticides, CO gas, plants, chemical materials, and bites), route of exposure (swallowing, breathing, injection, skin, and eyes), death due to poisoning, type of poisoning (accidental, suicide), and clinical symptoms (gastrointestinal symptoms, headache, dizziness, delirium and hallucinations, seizures, respiratory problems, ocular symptoms, a lack of consciousness, cyanosis, fever and chills, urinary symptoms, restlessness and lethargy, gait disturbance, drowsiness). The data were extracted from the medical files. Patient records in Shahid Sadoughi Hospital were paper medical files, while they were electronic files in Shahid Beheshti Hospital.
Data analysis
The SPSS software, version 20 was used for data analysis. The descriptive statistics, chi-square test, independent t-test, and binary logistic regression were used. A P<0.05 was considered significant. An independent t-test was used to compare the age of the patients and the length of hospitalization between the two periods. The chi-square was used to compare the frequency of poisoning between two periods based on qualitative variables (gender, living area, season, and type of poisoning). The logistic regression model was used to investigate the effect of the period on the cause of poisoning. For this purpose, the univariate analysis was performed first, and the variables with a significance level above 0.3 were included in the final model.
3. Results
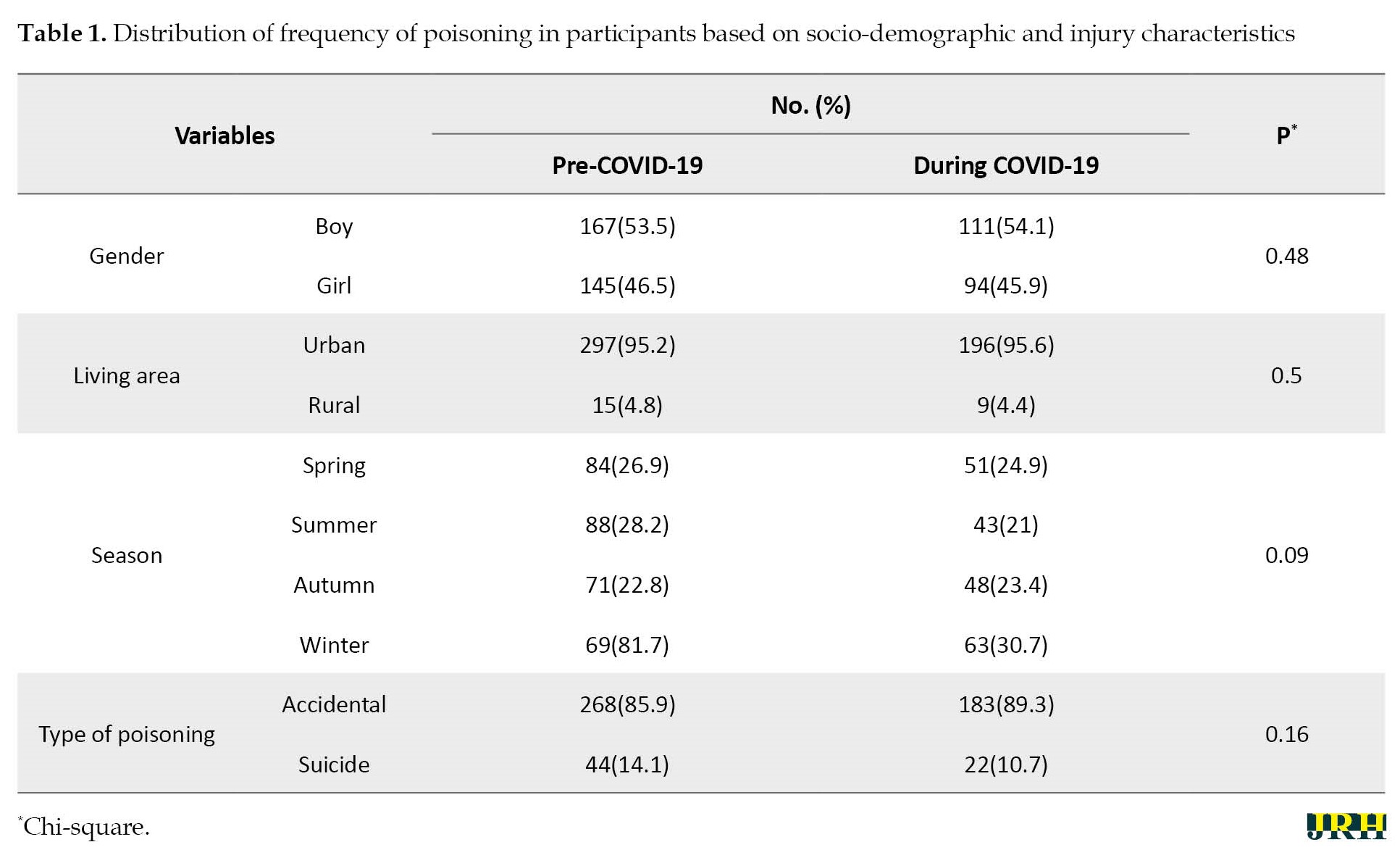
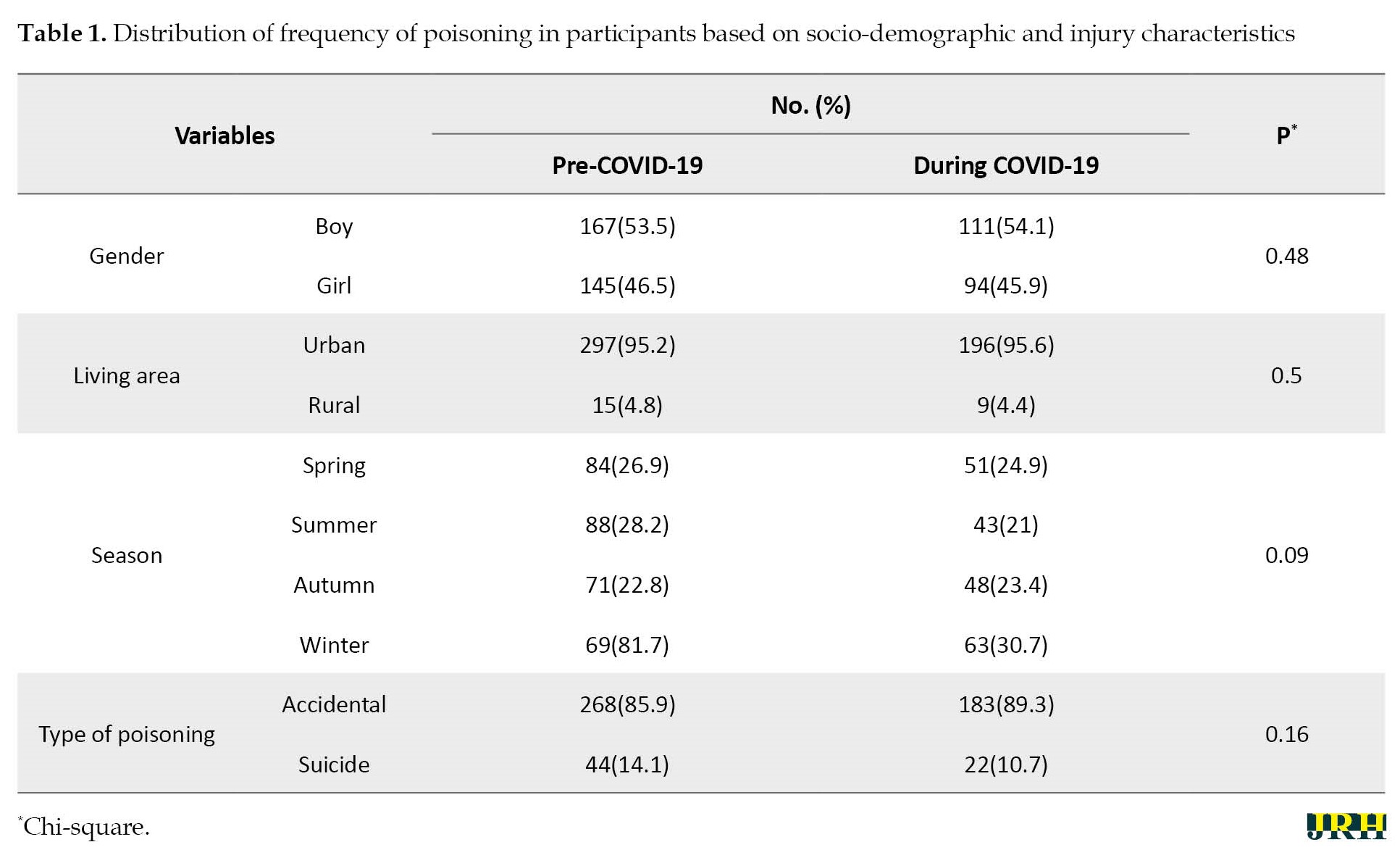
The results of this study showed that the prevalence of hospitalization because of poisoning in children under the age of 15 years during the COVID-19 pandemic and pre-COVID-19 was 2.39% and 2.6%, respectively. The Mean±SD age of poisoned children during the COVID-19 pandemic and pre-COVID-19 was 5.8±1.5 and 6.5±1.9 years (P=0.01), respectively, and the Mean±SD duration of hospitalization was 38.08±8.2 and 29.01±7.3 hours, respectively (P=0.008). According to Table 1, no statistical difference was observed between the poisonings of the two time periods regarding gender, location, and poisoning season.
In terms of clinical symptoms, gastrointestinal symptoms, drowsiness, a lack of consciousness, restlessness, and lethargy were the most common in both studied periods; however, no statistically significant difference was observed between the two periods. Regarding the route of exposure to poisonous agents, the result indicated that most people were poisoned by swallowing in both periods (97.4% in pre-COVID-19 and 95.6% in the COVID-19 pandemic).
Table 2 shows the causes of poisoning in the two periods.

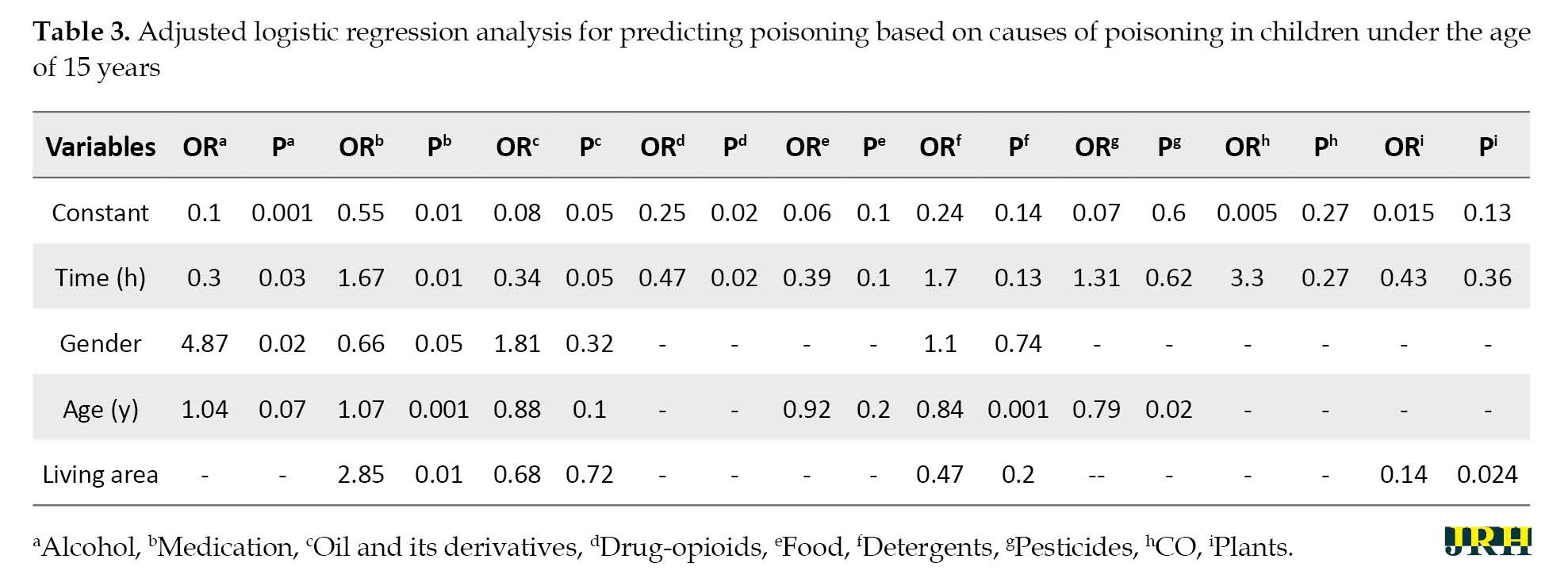
According to the results, drugs, opioids, and detergents had the highest frequency of causes of poisoning in both periods. The result showed increased hospitalization of children and adolescents due to alcohol poisoning during the outbreak of COVID-19. According to the results, the prevalence of alcohol poisoning in children under 15 years during the COVID-19 pandemic and pre-COVID-19 was 5.4% and 1.6%, respectively. The multivariate regression analysis showed that by adjusting the effects of age and sex, the chance of alcohol poisoning in the period before the outbreak of COVID-19 was 70% lower than during the outbreak of COVID-19 (odd ratio [OR]=0.3, P=0.03) (Table 3).
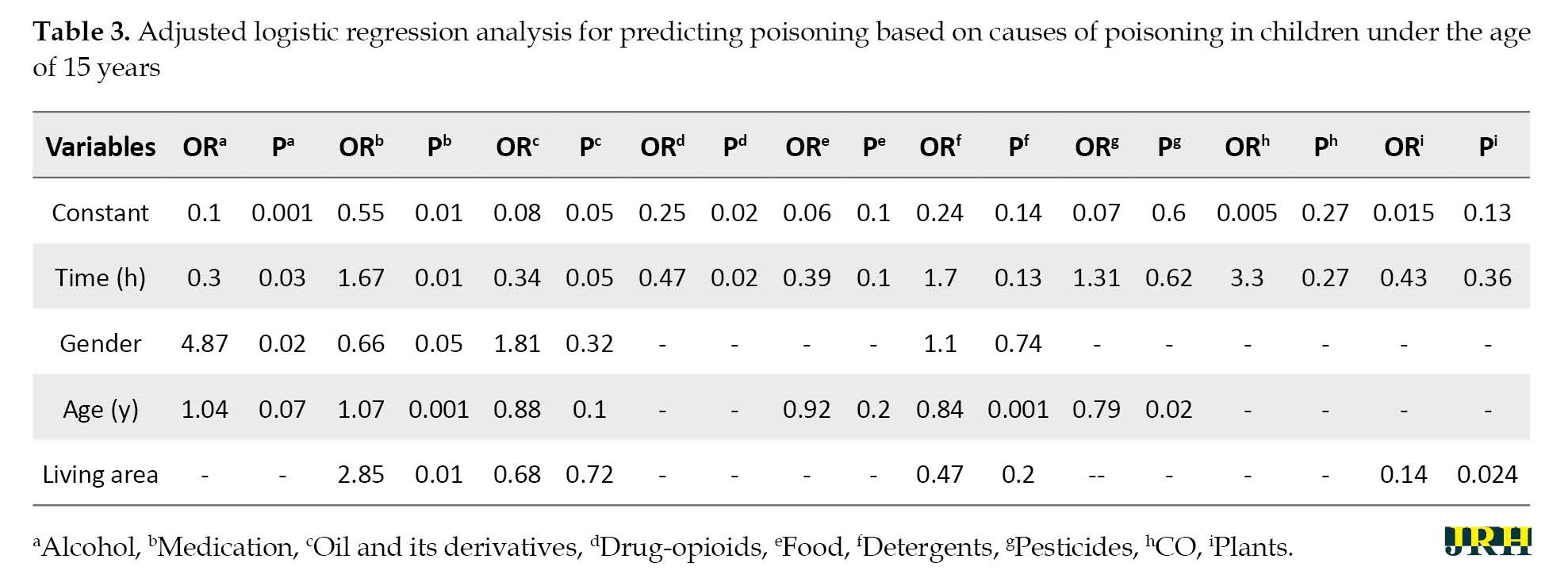
Further analysis showed that the mean age of alcohol poisoning during the COVID-19 pandemic and pre-COVID-19 was 6.8±1.2 and 12.2±3.2, respectively (P=0.07). This result indicates a decrease in the age of alcohol poisoning during the COVID-19 pandemic. Additionally, alcohol poisoning in the pre-COVID-19 period occurred only in boys and, in all cases, was accidental; however, during the COVID-19 pandemic, 27.3% of alcohol poisoning occurred in girls. According to Table 3, a case of alcohol suicide was also observed during 12 months of the COVID-19 pandemic. The results showed that most alcohol poisoning during the COVID-19 pandemic was related to the age group under three years; In boys, it was related to the age group above 10 years. Also, all cases of alcohol poisoning in both periods were swallowing in urban areas, and a doctor prescribed the discharge method.
The results also showed that the frequency of poisoning with oil, its derivatives, and drug opioids increased during the COVID-19 pandemic. Multivariate regression analysis showed that by adjusting the effects of age and sex, the chance of poisoning with oil and its derivatives in the period before the outbreak of COVID-19 was 67% lower than during the outbreak of COVID-19. (OR=0.33, P=0.05). Also, the chance of drug-opioid poisoning in the period before the outbreak of COVID-19 was 53% lower than during the outbreak of COVID-19 (OR=0.47, P=0.02) (Table 3).
The results showed that poisoning with oil and its derivatives was higher in boys than girls in both periods. The results also demonstrated that most cases of oil poisoning in both periods were related to children under 5 years old. According to the results, most cases of drug-opioid poisoning were in urban areas and by swallowing in the two periods. Meanwhile, most cases of drug-opioids poisoning in both periods were related to children less than one year of age; however, this prevalence was significantly different between the two time periods (P=0.06) (35.3% in pre-COVID-19 and 72.7% in the COVID-19 pandemic).
The results indicated that poisoning due to medication was reduced during the COVID-19 pandemic. Multivariate regression analysis showed that by adjusting the effects of age, sex, and place of residence, the chance of drug poisoning in the period before the outbreak of COVID-19 was 67% higher than during the outbreak of COVID-19 (OR=1.67, P=0.01) (Table 3).
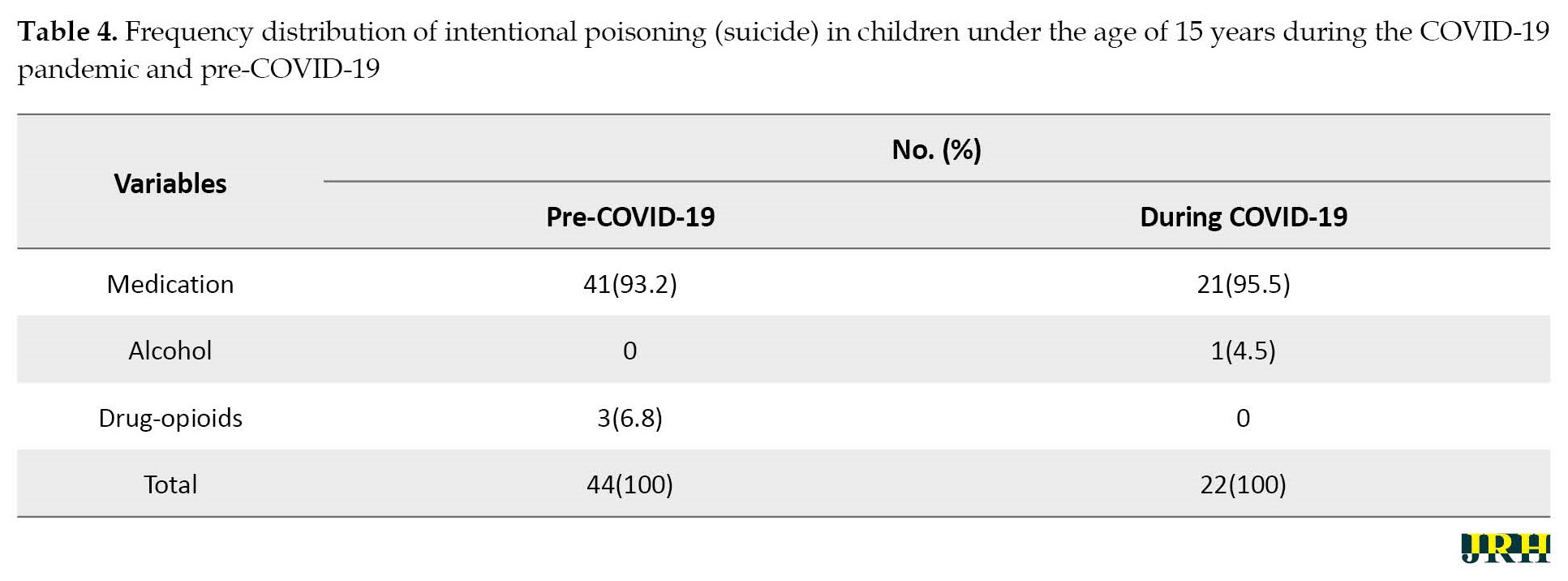
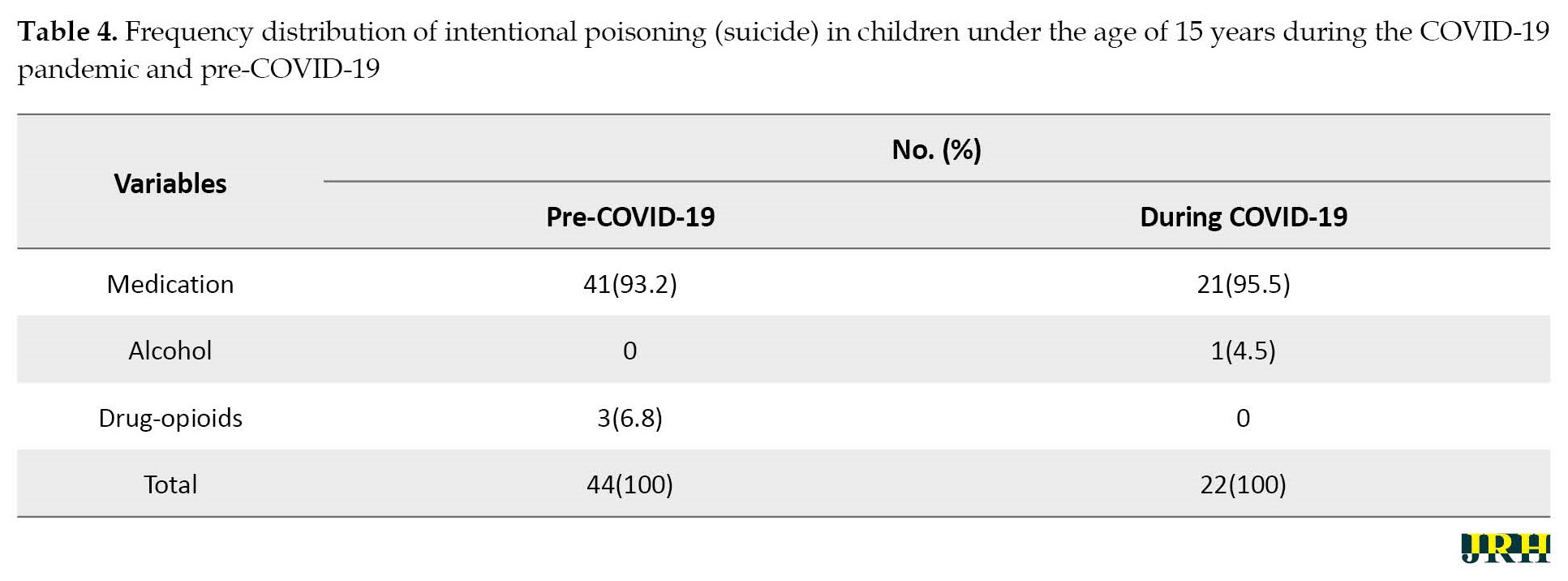
Further analyses showed that the age and gender distribution of drug poisoning in the two periods were almost the same; however, no statistically significant difference was detected. According to the results, drug poisoning in 22 people during the COVID-19 pandemic and 44 people during pre-COVID-19 was due to suicide, but this difference was not statistically significant (Table 4).
Also, 6 deaths occurred due to poisoning in pre-COVID-19, and 2 deaths occurred during the COVID-19 pandemic (P=0.48).
4. Discussion
The present study showed that hospitalization rates due to poisoning in children under 15 years were significantly higher during the COVID-19 pandemic compared to the 2019 reference period. Similar research in Morocco examined the characteristics of poisoning in children during the COVID-19 pandemic. Their study showed that the frequency of hospitalizations due to poisoning in children during the 12 months of the COVID-19 pandemic increased by 28 people compared to last year [3]. These results are consistent with a study conducted in Padova, Italy [17]. Research conducted by Cella et al. showed a decrease in emergency department visits due to poisoning in 2020 compared to 2019 and an increase in hospitalization cases due to poisoning in 2020 compared to 2019 [18].
Consistent with this results some other studies showed that outpatient visits to the emergency department due to poisoning were reduced during the COVID-19 pandemic [19-21]. The COVID-19 pandemic has considerably affected children’s social environments and access to healthcare and services. Fear of getting COVID-19 in a hospital emergency department will likely reduce emergency room visits, exacerbating the child’s condition and ultimately increasing cases of poisoning, leading to hospitalization.
Grasso et al. believe that most cases of poisoning in children during the COVID-19 pandemic are managed at home and as self-medication, and if symptoms worsen, lead to hospitalization [22]. On the other hand, due to the lower weight of children, if poisoning is not treated timely and properly, hypoglycemia occurs sooner, and the symptoms of poisoning intensify, leading to hospitalization [10]. Sabti et al. indicated that the reduction of emergency department visits during the COVID-19 pandemic was a factor in accepting patients with more severe conditions and reducing the financial workload of the emergency department [23]. However, the consequences of increasing self-medication and its impact on children’s health should be considered. Medication poisoning is one of the significant causes of poisoning in children. It may occur due to over-the-counter medication, giving medicine at the wrong time, or in higher doses [24].
After the prevalence of COVID-19, various strategies were made to prevent its expansion. One of these strategies was the use of alcoholic disinfectants [25]. Some of them did not have solid scientific documentation [10]. At the same time as increasing alcoholic disinfectants, some studies reported changes in the number of cases of poisoning, including a significant increase in methanol poisoning due to improper use of disinfectants and health products [26, 27]. A survey at the Center for Control and Prevention of American Diseases showed that nearly half of adults did not know that hand disinfectant should be kept out of the reach of children [28].
The results showed that the rate of hospitalization due to poisoning with alcohol, drugs-opioids, oil, and its derivatives was significantly increased in children under the age of 15 years during the COVID-19 pandemic compared to the same period in 2019. Also, the chance of poisoning with alcohol, which leads to hospitalization during the COVID-19 pandemic, was higher than in the same period in 2019. Mahdavi et al. examined the hospitalization rate due to poisoning in children in 9 hospitals in 5 provinces of Iran. Their study showed that hospitalization rates due to ethanol and methanol exposure in people aged 0 to 18 years increased significantly in 2020 compared to 2019 (375 vs 202 cases) [16]. McCulley et al. found that the increase in alcohol poisoning was in line with the growing demand for alcoholic disinfectants [29]. A study conducted in Morocco showed that poisoning with methanol and alcohol, caustics, and drug opioids increased among children during the COVID-19 pandemic. Also, the highest increase was in oil products and caustics. According to the authors, Moroccans widely used caustics to disinfect the air and surfaces to reduce the virus’s diffusion [3].
Coinciding with the spread of COVID-19, governments adopted a policy of closing schools and universities and nationwide quarantine. By shutting down schools, children who had to stay at home were in contact with hazardous products, such as medications, alcohol, and disinfectants [19, 30]. On the other hand, misconceptions about the use of alcoholic beverages to disinfect the mouth and throat (such as gargling alcohol) may increase poisoning in adolescents [31, 32]. People initially thought that COVID-19 was likely to be transmitted from surfaces. This perception led to the storage of disinfectants and alcohols in the home, often impregnated with a fragrant scent, and attracted children [24]. Parental teleworking at home also reduced child care and increased the risk of children being exposed to disinfectants and alcohol [33]. The combination of these factors is likely to increase alcohol poisoning in children and adolescents during the COVID-19 period.
In the present study, the prevalence of hospitalization of children due to drug-opioid poisoning during COVID-19 was significantly increased compared to the same period in 2019. The chance of drug-opioid poisoning in children during the COVID-19 period was higher than in the same period in 2019. Quarantine and staying at home may lead to increased drug use by parents and improve children’s access to drugs.
A similar study in Turkey found that drug-opioid poisoning in children during the outbreak of COVID-19 was 3.5 times higher than in the same period in 2019 [9]. Social isolation is a factor in reducing mental health and increasing depression and anxiety during COVID-19, which increases drug use in adults [34]. Some also believe that financial problems and unemployment caused by the COVID-19 outbreak increase depression, followed by increased drug-opioid use in adults [35]. With growing drug use in adults, children’s access to drugs will increase, and due to the curiosity of toddlers and their desire to put objects in their mouths, the rate of drug poisoning in children increased during the outbreak of COVID-19.
The results of the present study showed that hospitalization due to medication poisoning in both periods was the most common cause of poisoning, consistent with studies conducted in Brazil and Kuwait [23, 36]. The main culprits of medication poisoning in children are parents because their children do not have access to the medication, and the leading cause of medication poisoning is self-medication, giving medicine at the wrong time, or in higher doses [37]. On the other hand, the attractive form, pleasant taste of some medicines, colored pills, syrups with beautiful labels, and attractive packaging are the factors that attract children to medicines [24].
The results also indicated that the chances of medication poisoning in children under the age of 15 during the COVID-19 pandemic were significantly lower than in 2019, which is consistent with the results of a similar study conducted in Morocco [3]. Fear of COVID-19 infection increases health and self-care behaviors in individuals. This reduces viral diseases, such as colds or influenza, and self-medications (painkillers and antipyretics), thereby reducing medication poisoning.
The results also showed that the frequency of intentional poisoning (suicide) during COVID-19 compared to the same period in 2019 decreased, and the frequency of accidental poisoning increased, consistent with a similar study in Morocco. Amrani Hanchi et al. believed that because most suicides are medication-related, reducing medication poisoning reduces suicides in children [3]. However, Akcaboy et al., who examined changes in child hospitalization in Turkey after the outbreak of COVID-19, found that the rate of intentional poisoning in children during COVID-19 was 2.25 times the same time in 2019. They believe that school closure, quarantine, and travel restrictions are factors in reducing mental health and increasing the frequency of intentional poisonings [9].
In terms of route of exposure to poisonous agents, the result indicated that most people were poisoned by swallowing in both periods, which is consistent with similar studies [3, 33]. The findings also showed that the mean age of poisoned children and adolescents hospitalized during the COVID-19 pandemic slightly increased (P=0.01). Amrani Hanchi et al. reported that the mean age of children and adolescents was almost similar before and after the COVID-19 outbreak [3]. The present study showed that the mean age of alcohol poisoning decreased during the COVID-19 pandemic, which is likely due to more children’s access to disinfectants and alcohol.
The results also showed that the mean duration of hospitalization in poisoned children during the COVID-19 pandemic decreased by about 9 h compared to the same period in 2019 (P=0.008). One of the limitations of the present study is that it did not examine poisoned children who were treated as outpatients in the emergency room.
5. Conclusion
The results indicated that the frequency of poisoning with alcohol, drugs-opioids, oil, and its derivatives in children and adolescents in Yazd City, Iran, during the 12 months of the COVID-19 pandemic increased significantly compared to the same period last year. This finding highlights the need to increase knowledge about common poisoning during the COVID-19 pandemic and the dangers of using alcoholic disinfectants. Given that the prevalence of hospitalization of children and adolescents due to poisoning has increased during the COVID-19 pandemic, this is an alarm to prevent delayed referral of poisoned children to medical centers for treatment. There is a need to establish a poison control center in Yazd Province, Iran, that provides specialized medical care to poisoned patients, provides services such as face-to-face and telephone counseling to patients, poison management, and research activities on poisoning.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences (Code: IR.SSU.SPH.REC.1400.077).
Funding
This study was financially supported by the Shahid Sadoughi University of Medical Sciences (Grant No.: 10389).
Authors' contributions
The authors contributed equally to the preparation of this article.
Conflict of interest
The authors declared no conflict of interest
Acknowledgments
The authors would like to thank the Center for Healthcare Data Modeling and the participants for their cooperation in this research project.
References
The new coronavirus 2019 (COVID-19) was recorded for the first time on December 26, 2019, in Wuhan City, China [1]. The virus gradually expanded to other countries until the World Health Organization (WHO) declared COVID-19 a pandemic on March 11, 2020 [2]. The first COVID-19 case in Iran was reported on February 19, 2020, in Qom City, Iran [3]. WHO suggested preventive measures and healthy lifestyles to protect individuals against the infection. One of the best WHO advice was to disinfect hands with soap or ethanol-based (>60% ethanol) hand sanitizers [4]. A study in China demonstrated that the best way to reduce the transmission of COVID-19 among people in the community is to carry out health measures, impose quarantine, avoid gatherings, timely diagnosis, and patient care in hospitals [5]. Alimohamadi et al. reported that the spread of COVID-19 in Iran can be reduced by various interventions, such as health education, preventing the formation of human gatherings, quarantine, and separation of patients during the period of the disease from the rest of the community [6].
With the increase in COVID-19 patients in Iran, several approaches were considered to prevent the disease, including using alcohol-based disinfection solutions commonly available to the general public [7]. By shutting down schools, children who had to stay at home were in contact with hazardous products, such as medications, alcohol, and disinfectants [8]. On the other hand, misconceptions about the use of alcoholic beverages to disinfect the mouth and throat (for instance, gargling alcohol) may increase poisoning in adolescents [9, 10]. Fear of COVID-19 changed people’s health behaviors. Excessive cleaning and disinfection of the house and improper use of bleaches and disinfectants became more common [11]. Also, the increasing demand for hand sanitizers led to the production of hand sanitizers with inappropriate proportions of ethanol (<60%) or hand sanitizers containing methanol [12]. Alcohol-based disinfectants affect human health through ingestion, inhalation, or skin contact [13]. After the onset of the COVID-19 pandemic in Iran, alcohol poisoning increased in some areas, leading to deaths. All provinces reported cases of methanol poisoning [14]. The lack of public awareness about the prevention and treatment of COVID-19, subjects’ lack of awareness about different types of alcohol, the sale of illegal and non-standard alcohol, and the spread of rumors and disinformation through social media about COVID-19 and its prevention methods were among the reasons for the increase of alcohol poisoning during the pandemic in Iran [15].
A study examining alcohol poisoning in Iranian children and adolescents demonstrated that the prevalence of alcohol poisoning during the COVID-19 pandemic was associated with increased hospitalization rates among children and adolescents [16]. Given that the prevalence of poisoning and its causes in children and adolescents during the COVID-19 pandemic in Iran remains unknown, the researchers decided to compare the poisoning on children under the age of 15 years who were admitted to the referral teaching hospitals of Yazd and Taft cities, Iran, during the first wave of COVID-19 versus its previous year (pre-COVID-19 period in 2019).
2. Methods
Study design
This analytic, cross-sectional study was conducted based on the administrative data obtained from the referral teaching hospital in Yazd and Taft cities, Iran. In this study, the data were collected by census. The information of all children under the age of 15 years admitted to the referral teaching hospital in the selected two cities (Shahid Sadoughi Hospital in Yazd City, Iran, and Shahid Beheshti Hospital in Taft City, Iran) due to poisoning was examined. Accordingly, 312 cases in pre-COVID-19 and 205 cases during the COVID-19 pandemic were examined. The study period was from February 19, 2020, to February 18, 2021 (12 months of the COVID-19 pandemic) compared to 2019 as the reference period (pre-COVID). The inclusion criteria were being under the age of 18 years, being a native of Yazd Province, Iran, and being hospitalized with a diagnosis of poisoning in the hospital record. Outpatients with alcohol exposure and incomplete records (such as not mentioning the cause of poisoning) were excluded from the study.
Data collection
The data collection method in this study included a checklist comprised of age, gender, duration of hospitalization, location (urban, rural), the season of occurrence of poisoning, cause of poisoning (medications, alcohol, oil and its derivatives, food, drugs-opioids, detergents, pesticides, CO gas, plants, chemical materials, and bites), route of exposure (swallowing, breathing, injection, skin, and eyes), death due to poisoning, type of poisoning (accidental, suicide), and clinical symptoms (gastrointestinal symptoms, headache, dizziness, delirium and hallucinations, seizures, respiratory problems, ocular symptoms, a lack of consciousness, cyanosis, fever and chills, urinary symptoms, restlessness and lethargy, gait disturbance, drowsiness). The data were extracted from the medical files. Patient records in Shahid Sadoughi Hospital were paper medical files, while they were electronic files in Shahid Beheshti Hospital.
Data analysis
The SPSS software, version 20 was used for data analysis. The descriptive statistics, chi-square test, independent t-test, and binary logistic regression were used. A P<0.05 was considered significant. An independent t-test was used to compare the age of the patients and the length of hospitalization between the two periods. The chi-square was used to compare the frequency of poisoning between two periods based on qualitative variables (gender, living area, season, and type of poisoning). The logistic regression model was used to investigate the effect of the period on the cause of poisoning. For this purpose, the univariate analysis was performed first, and the variables with a significance level above 0.3 were included in the final model.
3. Results
The results of this study showed that the prevalence of hospitalization because of poisoning in children under the age of 15 years during the COVID-19 pandemic and pre-COVID-19 was 2.39% and 2.6%, respectively. The Mean±SD age of poisoned children during the COVID-19 pandemic and pre-COVID-19 was 5.8±1.5 and 6.5±1.9 years (P=0.01), respectively, and the Mean±SD duration of hospitalization was 38.08±8.2 and 29.01±7.3 hours, respectively (P=0.008). According to Table 1, no statistical difference was observed between the poisonings of the two time periods regarding gender, location, and poisoning season.
In terms of clinical symptoms, gastrointestinal symptoms, drowsiness, a lack of consciousness, restlessness, and lethargy were the most common in both studied periods; however, no statistically significant difference was observed between the two periods. Regarding the route of exposure to poisonous agents, the result indicated that most people were poisoned by swallowing in both periods (97.4% in pre-COVID-19 and 95.6% in the COVID-19 pandemic).
Table 2 shows the causes of poisoning in the two periods.

According to the results, drugs, opioids, and detergents had the highest frequency of causes of poisoning in both periods. The result showed increased hospitalization of children and adolescents due to alcohol poisoning during the outbreak of COVID-19. According to the results, the prevalence of alcohol poisoning in children under 15 years during the COVID-19 pandemic and pre-COVID-19 was 5.4% and 1.6%, respectively. The multivariate regression analysis showed that by adjusting the effects of age and sex, the chance of alcohol poisoning in the period before the outbreak of COVID-19 was 70% lower than during the outbreak of COVID-19 (odd ratio [OR]=0.3, P=0.03) (Table 3).
Further analysis showed that the mean age of alcohol poisoning during the COVID-19 pandemic and pre-COVID-19 was 6.8±1.2 and 12.2±3.2, respectively (P=0.07). This result indicates a decrease in the age of alcohol poisoning during the COVID-19 pandemic. Additionally, alcohol poisoning in the pre-COVID-19 period occurred only in boys and, in all cases, was accidental; however, during the COVID-19 pandemic, 27.3% of alcohol poisoning occurred in girls. According to Table 3, a case of alcohol suicide was also observed during 12 months of the COVID-19 pandemic. The results showed that most alcohol poisoning during the COVID-19 pandemic was related to the age group under three years; In boys, it was related to the age group above 10 years. Also, all cases of alcohol poisoning in both periods were swallowing in urban areas, and a doctor prescribed the discharge method.
The results also showed that the frequency of poisoning with oil, its derivatives, and drug opioids increased during the COVID-19 pandemic. Multivariate regression analysis showed that by adjusting the effects of age and sex, the chance of poisoning with oil and its derivatives in the period before the outbreak of COVID-19 was 67% lower than during the outbreak of COVID-19. (OR=0.33, P=0.05). Also, the chance of drug-opioid poisoning in the period before the outbreak of COVID-19 was 53% lower than during the outbreak of COVID-19 (OR=0.47, P=0.02) (Table 3).
The results showed that poisoning with oil and its derivatives was higher in boys than girls in both periods. The results also demonstrated that most cases of oil poisoning in both periods were related to children under 5 years old. According to the results, most cases of drug-opioid poisoning were in urban areas and by swallowing in the two periods. Meanwhile, most cases of drug-opioids poisoning in both periods were related to children less than one year of age; however, this prevalence was significantly different between the two time periods (P=0.06) (35.3% in pre-COVID-19 and 72.7% in the COVID-19 pandemic).
The results indicated that poisoning due to medication was reduced during the COVID-19 pandemic. Multivariate regression analysis showed that by adjusting the effects of age, sex, and place of residence, the chance of drug poisoning in the period before the outbreak of COVID-19 was 67% higher than during the outbreak of COVID-19 (OR=1.67, P=0.01) (Table 3).
Further analyses showed that the age and gender distribution of drug poisoning in the two periods were almost the same; however, no statistically significant difference was detected. According to the results, drug poisoning in 22 people during the COVID-19 pandemic and 44 people during pre-COVID-19 was due to suicide, but this difference was not statistically significant (Table 4).
Also, 6 deaths occurred due to poisoning in pre-COVID-19, and 2 deaths occurred during the COVID-19 pandemic (P=0.48).
4. Discussion
The present study showed that hospitalization rates due to poisoning in children under 15 years were significantly higher during the COVID-19 pandemic compared to the 2019 reference period. Similar research in Morocco examined the characteristics of poisoning in children during the COVID-19 pandemic. Their study showed that the frequency of hospitalizations due to poisoning in children during the 12 months of the COVID-19 pandemic increased by 28 people compared to last year [3]. These results are consistent with a study conducted in Padova, Italy [17]. Research conducted by Cella et al. showed a decrease in emergency department visits due to poisoning in 2020 compared to 2019 and an increase in hospitalization cases due to poisoning in 2020 compared to 2019 [18].
Consistent with this results some other studies showed that outpatient visits to the emergency department due to poisoning were reduced during the COVID-19 pandemic [19-21]. The COVID-19 pandemic has considerably affected children’s social environments and access to healthcare and services. Fear of getting COVID-19 in a hospital emergency department will likely reduce emergency room visits, exacerbating the child’s condition and ultimately increasing cases of poisoning, leading to hospitalization.
Grasso et al. believe that most cases of poisoning in children during the COVID-19 pandemic are managed at home and as self-medication, and if symptoms worsen, lead to hospitalization [22]. On the other hand, due to the lower weight of children, if poisoning is not treated timely and properly, hypoglycemia occurs sooner, and the symptoms of poisoning intensify, leading to hospitalization [10]. Sabti et al. indicated that the reduction of emergency department visits during the COVID-19 pandemic was a factor in accepting patients with more severe conditions and reducing the financial workload of the emergency department [23]. However, the consequences of increasing self-medication and its impact on children’s health should be considered. Medication poisoning is one of the significant causes of poisoning in children. It may occur due to over-the-counter medication, giving medicine at the wrong time, or in higher doses [24].
After the prevalence of COVID-19, various strategies were made to prevent its expansion. One of these strategies was the use of alcoholic disinfectants [25]. Some of them did not have solid scientific documentation [10]. At the same time as increasing alcoholic disinfectants, some studies reported changes in the number of cases of poisoning, including a significant increase in methanol poisoning due to improper use of disinfectants and health products [26, 27]. A survey at the Center for Control and Prevention of American Diseases showed that nearly half of adults did not know that hand disinfectant should be kept out of the reach of children [28].
The results showed that the rate of hospitalization due to poisoning with alcohol, drugs-opioids, oil, and its derivatives was significantly increased in children under the age of 15 years during the COVID-19 pandemic compared to the same period in 2019. Also, the chance of poisoning with alcohol, which leads to hospitalization during the COVID-19 pandemic, was higher than in the same period in 2019. Mahdavi et al. examined the hospitalization rate due to poisoning in children in 9 hospitals in 5 provinces of Iran. Their study showed that hospitalization rates due to ethanol and methanol exposure in people aged 0 to 18 years increased significantly in 2020 compared to 2019 (375 vs 202 cases) [16]. McCulley et al. found that the increase in alcohol poisoning was in line with the growing demand for alcoholic disinfectants [29]. A study conducted in Morocco showed that poisoning with methanol and alcohol, caustics, and drug opioids increased among children during the COVID-19 pandemic. Also, the highest increase was in oil products and caustics. According to the authors, Moroccans widely used caustics to disinfect the air and surfaces to reduce the virus’s diffusion [3].
Coinciding with the spread of COVID-19, governments adopted a policy of closing schools and universities and nationwide quarantine. By shutting down schools, children who had to stay at home were in contact with hazardous products, such as medications, alcohol, and disinfectants [19, 30]. On the other hand, misconceptions about the use of alcoholic beverages to disinfect the mouth and throat (such as gargling alcohol) may increase poisoning in adolescents [31, 32]. People initially thought that COVID-19 was likely to be transmitted from surfaces. This perception led to the storage of disinfectants and alcohols in the home, often impregnated with a fragrant scent, and attracted children [24]. Parental teleworking at home also reduced child care and increased the risk of children being exposed to disinfectants and alcohol [33]. The combination of these factors is likely to increase alcohol poisoning in children and adolescents during the COVID-19 period.
In the present study, the prevalence of hospitalization of children due to drug-opioid poisoning during COVID-19 was significantly increased compared to the same period in 2019. The chance of drug-opioid poisoning in children during the COVID-19 period was higher than in the same period in 2019. Quarantine and staying at home may lead to increased drug use by parents and improve children’s access to drugs.
A similar study in Turkey found that drug-opioid poisoning in children during the outbreak of COVID-19 was 3.5 times higher than in the same period in 2019 [9]. Social isolation is a factor in reducing mental health and increasing depression and anxiety during COVID-19, which increases drug use in adults [34]. Some also believe that financial problems and unemployment caused by the COVID-19 outbreak increase depression, followed by increased drug-opioid use in adults [35]. With growing drug use in adults, children’s access to drugs will increase, and due to the curiosity of toddlers and their desire to put objects in their mouths, the rate of drug poisoning in children increased during the outbreak of COVID-19.
The results of the present study showed that hospitalization due to medication poisoning in both periods was the most common cause of poisoning, consistent with studies conducted in Brazil and Kuwait [23, 36]. The main culprits of medication poisoning in children are parents because their children do not have access to the medication, and the leading cause of medication poisoning is self-medication, giving medicine at the wrong time, or in higher doses [37]. On the other hand, the attractive form, pleasant taste of some medicines, colored pills, syrups with beautiful labels, and attractive packaging are the factors that attract children to medicines [24].
The results also indicated that the chances of medication poisoning in children under the age of 15 during the COVID-19 pandemic were significantly lower than in 2019, which is consistent with the results of a similar study conducted in Morocco [3]. Fear of COVID-19 infection increases health and self-care behaviors in individuals. This reduces viral diseases, such as colds or influenza, and self-medications (painkillers and antipyretics), thereby reducing medication poisoning.
The results also showed that the frequency of intentional poisoning (suicide) during COVID-19 compared to the same period in 2019 decreased, and the frequency of accidental poisoning increased, consistent with a similar study in Morocco. Amrani Hanchi et al. believed that because most suicides are medication-related, reducing medication poisoning reduces suicides in children [3]. However, Akcaboy et al., who examined changes in child hospitalization in Turkey after the outbreak of COVID-19, found that the rate of intentional poisoning in children during COVID-19 was 2.25 times the same time in 2019. They believe that school closure, quarantine, and travel restrictions are factors in reducing mental health and increasing the frequency of intentional poisonings [9].
In terms of route of exposure to poisonous agents, the result indicated that most people were poisoned by swallowing in both periods, which is consistent with similar studies [3, 33]. The findings also showed that the mean age of poisoned children and adolescents hospitalized during the COVID-19 pandemic slightly increased (P=0.01). Amrani Hanchi et al. reported that the mean age of children and adolescents was almost similar before and after the COVID-19 outbreak [3]. The present study showed that the mean age of alcohol poisoning decreased during the COVID-19 pandemic, which is likely due to more children’s access to disinfectants and alcohol.
The results also showed that the mean duration of hospitalization in poisoned children during the COVID-19 pandemic decreased by about 9 h compared to the same period in 2019 (P=0.008). One of the limitations of the present study is that it did not examine poisoned children who were treated as outpatients in the emergency room.
5. Conclusion
The results indicated that the frequency of poisoning with alcohol, drugs-opioids, oil, and its derivatives in children and adolescents in Yazd City, Iran, during the 12 months of the COVID-19 pandemic increased significantly compared to the same period last year. This finding highlights the need to increase knowledge about common poisoning during the COVID-19 pandemic and the dangers of using alcoholic disinfectants. Given that the prevalence of hospitalization of children and adolescents due to poisoning has increased during the COVID-19 pandemic, this is an alarm to prevent delayed referral of poisoned children to medical centers for treatment. There is a need to establish a poison control center in Yazd Province, Iran, that provides specialized medical care to poisoned patients, provides services such as face-to-face and telephone counseling to patients, poison management, and research activities on poisoning.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences (Code: IR.SSU.SPH.REC.1400.077).
Funding
This study was financially supported by the Shahid Sadoughi University of Medical Sciences (Grant No.: 10389).
Authors' contributions
The authors contributed equally to the preparation of this article.
Conflict of interest
The authors declared no conflict of interest
Acknowledgments
The authors would like to thank the Center for Healthcare Data Modeling and the participants for their cooperation in this research project.
References
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. The New England Journal of Medicine. 2020; 382(8):727-733. [DOI:10.1056/NEJMoa2001017] [PMID]
- World Health Organization (WHO). Naming the coronavirus disease (COVID-19) and the virus that causes it [Internet]. 2020 [Updated 2023 October 6]. Available from: [Link]
- Amrani Hanchi S, Hoummani H, Mourabiti H, Chebaibi M, Chaouki S, Achour S, et al. Children’s poisoning profile during the Covid-19 pandemic-experience of Hassan II University Hospital in Fez, Morocco. Paper presented at: International Congress on Health Vigilance (VIGISAN 2021. 9 November 2021; Kenitra, Morocco. [DOI:10.1051/e3sconf/202131901077]
- World Health Organization (WHO). WHO guidelines on hand hygiene in health care: First global patient safety challenge clean care is safer care. Geneva: World Health Organization Copyright; 2009. [PMID]
- Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet. 2020; 395(10223):514-23. [DOI:10.1016/S0140-6736(20)30154-9] [PMID]
- Alimohamadi Y, Sepandi M. [Basic reproduction number: An important indicator for the future of the COVID-19 epidemic in Iran (Persian)]. Journal of Military Medicine. 2020; 22(1):96-7. [Link]
- Heidari M, Sayfouri N. COVID-19 and alcohol poisoning: A fatal competition. Disaster Medicine and Public Health Preparedness. 2022; 16(5):2179-2181. [DOI:10.1017/dmp.2021.89] [PMID]
- Le Roux G, Sinno-Tellier S; French Poison Control Centre members; Descatha A. COVID-19: Home poisoning throughout the containment period. Lancet Public Health. 2020; 5(6):e314. [DOI:10.1016/S2468-2667(20)30095-5] [PMID]
- Akcaboy M, Terin H, Senel S. Changes in hospitalization in children during COVID-19 pandemic quarantine in a single center in Turkey. The Journal of Pediatrics. 2021; 231:296-7. [DOI:10.1016/j.jpeds.2020.12.014] [PMID]
- Yip L, Bixler D, Brooks DE, Clarke KR, Datta SD, Dudley S, Jr., et al. Serious Adverse Health Events, Including Death, Associated with Ingesting Alcohol-Based Hand Sanitizers Containing Methanol - Arizona and New Mexico, May-June 2020. MMWR Morbidity and mortality weekly report. 2020;69(32):1070-3. [DOI:10.15585/mmwr.mm6932e1] [PMID]
- Mahdavi SA, Zamani N, McDonald R, Akhgari M, Kolahi AA, Gheshlaghi F, et al. A cross-sectional multicenter linkage study of hospital admissions and mortality due to methanol poisoning in Iranian adults during the COVID-19 pandemic. Scientific Reports. 2022; 12(1):9741. [DOI:10.1038/s41598-022-14007-1] [PMID]
- Jairoun AA, Al-Hemyari SS, Shahwan M. The pandemic of COVID-19 and its implications for the purity and authenticity of alcohol-based hand sanitizers: The health risks associated with falsified sanitizers and recommendations for regulatory and public health bodies. Research in Social & Administrative Pharmacy. 2021; 17(1):2050-1. [DOI:10.1016/j.sapharm.2020.04.014] [PMID]
- Mahmood A, Eqan M, Pervez S, Alghamdi HA, Tabinda AB, Yasar A, et al. COVID-19 and frequent use of hand sanitizers; human health and environmental hazards by exposure pathways. The Science of the Total Environment. 2020; 742:140561. [DOI:10.1016/j.scitotenv.2020.140561] [PMID]
- Iranian Legal Medicine Organization. Referral of more than 700 deaths due to alcohol poisoning from the beginning of March until now (Persian) [Internet]. 2020 [Updated 2020 April 8]. Available from: [Link]
- Aghababaeian H, Hamdanieh L, Ostadtaghizadeh A. Alcohol intake in an attempt to fight COVID-19: A medical myth in Iran. Alcohol. 2020; 88:29-32. [DOI:10.1016/j.alcohol.2020.07.006] [PMID]
- Mahdavi SA, Kolahi AA, Akhgari M, Gheshlaghi F, Gholami N, Moshiri M, et al. COVID-19 pandemic and methanol poisoning outbreak in Iranian children and adolescents: A data linkage study. Alcoholism, Clinical and Experimental Research. 2021; 45(9):1853-63. [DOI:10.1111/acer.14680] [PMID]
- Bressan S, Gallo E, Tirelli F, Gregori D, Da Dalt L. Lockdown: More domestic accidents than COVID-19 in children. Archives of Disease in Childhood. 2021; 106(2):e3.[DOI:10.1136/archdischild-2020-319547] [PMID]
- Cella A, Marchetti F, Iughetti L, Di Biase AR, Graziani G, De Fanti A, et al. Italian COVID-19 epidemic: Effects on paediatric emergency attendance-a survey in the Emilia Romagna region. BMJ Paediatrics Open. 2020; 4(1):e000742. [DOI:10.1136/bmjpo-2020-000742] [PMID]
- Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. The Lancet. Child & Adolescent Health. 2020; 4(5):e10-e11. [DOI:10.1016/S2352-4642(20)30108-5] [PMID]
- Pines JM, Zocchi MS, Black BS, Carlson JN, Celedon P, Moghtaderi A, et al. Characterizing pediatric emergency department visits during the COVID-19 pandemic. The American Journal of Emergency Medicine. 2021; 41:201-4. [DOI:10.1016/j.ajem.2020.11.037] [PMID]
- Williams TC, MacRae C, Swann OV, Haseeb H, Cunningham S, Davies P, et al. Indirect effects of the COVID-19 pandemic on paediatric healthcare use and severe disease: A retrospective national cohort study. Arch Dis Child. 2021; 106(9):911-7. [DOI:10.1136/archdischild-2020-321008] [PMID]
- Grasso A, Resnati C, Lanza A, Berrino L, Villani R. Toxicovigilance during COVID-19: Attention to poisoning related to disinfection. Minerva Anestesiologica. 2021; 87(2):251-2. [DOI:10.23736/S0375-9393.20.15010-7] [PMID]
- Sabti MA, Al-Ajmi S, Shamsaldeen YA. Paediatric poisoning in Kuwait-Al Adan joint hospital: The need for functional poisoning control centre in Kuwait. Saudi Pharmaceutical Journal. 2021; 29(11):1267-71. [DOI:10.1016/j.jsps.2021.10.001] [PMID]
- Momayyezi M, Peigan P, Fallahzadeh H. Epidemiological pattern of poisoning in children under the age of 15 admitted to the referral teaching hospitals of Yazd and Taft cities (2014-2019). Journal of Environmental Health and Sustainable Development. 2021; 6(3):1357-66. [DOI:10.18502/jehsd.v6i3.7243]
- Park SH, Hong SH, Kim K, Lee SW, Yon DK, Jung SJ, et al. Nonpharmaceutical interventions reduce the incidence and mortality of COVID-19: A study based on the survey from the international COVID-19 research network (ICRN). Journal of Medical Virology. 2023; 95(2):e28354. [DOI:10.1002/jmv.28354] [PMID]
- Chang A, Schnall AH, Law R, Bronstein AC, Marraffa JM, Spiller HA, et al. Cleaning and disinfectant chemical exposures and temporal associations with COVID-19 - national poison data system, United States, January 1, 2020-March 31, 2020. MMWR. Morbidity and Mortality Weekly Report. 2020; 69(16):496-8. [DOI:10.15585/mmwr.mm6916e1] [PMID]
- Sefidbakht S, Lotfi M, Jalli R, Moghadami M, Sabetian G, Iranpour P. Methanol toxicity outbreak: When fear of COVID-19 goes viral. Emergency Medicine Journal. 2020; 37(7):416. [DOI:10.1136/emermed-2020-209886] [PMID]
- Gharpure R, Hunter CM, Schnall AH, Barrett CE, Kirby AE, Kunz J, et al. Knowledge and practices regarding safe household cleaning and disinfection for COVID-19 prevention - United States, May 2020. MMWR. Morbidity and Mortality Weekly Report. 2020; 69(23):705-9. [DOI:10.15585/mmwr.mm6923e2] [PMID]
- McCulley L, Cheng C, Mentari E, Diak IL, Michele T. Alcohol-based hand sanitizer exposures and effects on young children in the U.S. during the COVID-19 pandemic. Clinical Toxicology. 2021; 59(4):355-6. [DOI:10.1080/15563650.2020.1811298] [PMID]
- Viner RM, Russell SJ, Croker H, Packer J, Ward J, Stansfield C, et al. School closure and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. The Lancet. Child & Adolescent Health. 2020; 4(5):397-404. [DOI:10.1016/S2352-4642(20)30095-X] [PMID]
- Delirrad M, Mohammadi AB. New methanol poisoning outbreaks in iran following COVID-19 pandemic. Alcohol and Alcoholism. 2020; 55(4):347-8. [DOI:10.1093/alcalc/agaa036] [PMID]
- Soltaninejad K. Methanol mass poisoning outbreak: A consequence of COVID-19 pandemic and misleading messages on social media. The International Journal of Occupational and Environmental Medicine. 2020; 11(3):148-50. [DOI:10.34172/ijoem.2020.1983] [PMID]
- Crescentini C, Feruglio S, Matiz A, Paschetto A, Vidal E, Cogo P, et al. Stuck outside and inside: An exploratory study on the effects of the COVID-19 Outbreak on Italian parents and children's internalizing symptoms. Frontiers in Psychology. 2020; 11:586074. [DOI:10.3389/fpsyg.2020.586074] [PMID]
- de Figueiredo CS, Sandre PC, Portugal LCL, Mázala-de-Oliveira T, da Silva Chagas L, Raony Í, Ferreira ES, et al. COVID-19 pandemic impact on children and adolescents' mental health: Biological, environmental, and social factors. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2021; 106:110171. [DOI:10.1016/j.pnpbp.2020.110171] [PMID]
- Tan ST, Chen TH, Yang HW, Su YJ. Changes in poisoning during the COVID-19 pandemic worldwide. The American Journal of Emergency Medicine. 2022; 56:291-293. [DOI:10.1016/j.ajem.2021.07.027] [PMID]
- Ferrer IL, Baptistella MKCS, de Oliveira FNM, de Souza AG, da Cunha LC, Magalhães AFA. Poisoning in children and adolescents assisted during the COVID-19 pandemic at the toxicological information and assistance center in federal district, Brazil (CIATOX-DF): Descriptive, cross-sectional, and analytical study with 1.037 patients. Research, Society and Development. 2021; 10(15):e25101521960. [DOI:10.33448/rsd-v10i15.21960]
- de Carvalho Fukuda R, Grispan e Silva LD, Tacla MTGM. [Intoxicações exógenas em pediatria (Portuguese)]. Varia Scientia-Ciências da Saúde. 2015;1(1):26-34. [DOI:10.48075/vscs.v1i1.11932]
Type of Study: Orginal Article |
Subject:
● Disease Control
Received: 2022/11/21 | Accepted: 2023/05/31 | Published: 2023/10/3
Received: 2022/11/21 | Accepted: 2023/05/31 | Published: 2023/10/3
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









