Volume 14, Issue 1 (Jan & Feb 2024)
J Research Health 2024, 14(1): 71-82 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alirahmi M, Soleimannejad H, Kikhavani S. The Effectiveness of Behavioral Activation on Depression, Social Avoidance, and Mental Rumination of Mothers of Children With Cerebral Palsy in Ilam City, Iran. J Research Health 2024; 14 (1) :71-82
URL: http://jrh.gmu.ac.ir/article-1-2238-en.html
URL: http://jrh.gmu.ac.ir/article-1-2238-en.html
1- Department of Psychology, Faculty of Human Sciences, Ilam Branch, Islamic Azad University, Ilam, Iran. , mostafa5279@gmail.com
2- Department of Psychology, Faculty of Human Sciences, Ilam Branch, Islamic Azad University, Ilam, Iran.
3- Department of Clinical Psychology Psychosocial Injuries Research Center & School of Medicine, Ilam University of Medical Sciences, Ilam , Iran
2- Department of Psychology, Faculty of Human Sciences, Ilam Branch, Islamic Azad University, Ilam, Iran.
3- Department of Clinical Psychology Psychosocial Injuries Research Center & School of Medicine, Ilam University of Medical Sciences, Ilam , Iran
Full-Text [PDF 648 kb]
(581 Downloads)
| Abstract (HTML) (2357 Views)
Full-Text: (389 Views)
Introduction
Disabled children need more care and their parents bear the most stress to care for them [1]. Caring for a child with cerebral palsy requires intensive and long-term care activities [2] and these chronic conditions cause the parents of these children to experience more physical and mental health problems [3]. In most cultures of the world, mothers are more responsible for raising their children and are usually the main caregivers of disabled children [4]. Studies conducted in Iran also indicate that 91.4% of caregivers of children with cerebral palsy are mothers [5]. Although some mothers cope well with problems; mothers with disabled children have more physical disorders, depression, anxiety, tension, and nervous pressure, and less self-confidence than other mothers. These mothers also feel lonely and have problems in their communication with the people around them [6] because the presence of a child with cerebral palsy in the family causes intense feelings of stress, depression, and guilt to the extent that these families reduce their social activities due to these feelings [7].
Research results show that the prevalence of depression and rumination in mothers of children with developmental disorders is higher than in mothers of healthy children. Also, the unpredictable future in the case of a child with cerebral palsy leads to fatigue and tension in parents [8]. Since the mother is the first person who communicates directly with the child; feelings, such as guilt, fault, inadequacy, and deprivation caused by the child’s abnormality can cause isolation, lack of interest in establishing a relationship with the environment, and a decrease in self-esteem. Feelings of low self-esteem, worthlessness, and sadness in the mother, which results in depression, can jeopardize the mother’s mental health, and psychological helplessness [9].
Depression includes symptoms, such as apathy, sadness, and dysfunctional thoughts [10]. In recent years, examining maladaptive thinking patterns in emotional disorders and their role in the persistence of these disorders has been the focus of experts and clinical researchers. One of these maladaptive patterns in emotional disorders, such as depression is rumination [11]. Rumination is defined as the repeated and recurring thoughts about negative moods or life events [12]. According to Martin and Teiser, the concept of rumination refers to a thinking style that tends to repeat itself [13]. From their point of view, rumination introduces a set of conscious thoughts that revolve around a crucial issue and these thoughts appear even in the absence of immediate and necessary environmental demands. By providing signs, the external environment may lead to maintaining these thoughts, but at the same time, maintaining these thoughts and their continuation is not dependent on environmental signs. Also, rumination is defined as resistant and recurrent thoughts that go around a common topic, enter consciousness involuntarily, and divert attention from desired topics, and current goals [14]. The results of Siegel’s research showed multiple and separate constructs to measure the variable of rumination and each measure alone represents a specific aspect of rumination that is related to depression and mental health [15]. In the study conducted by Chu et al., it was found that behavioral activation therapy had better results in the treatment of severely depressed patients than drug therapy and cognitive therapy. Also, this treatment significantly reduced depression and rumination in the post-test and two-month follow-up stages. Conceptually, this treatment method is suitable as an inter-diagnostic intervention to deal with depression and rumination [16].
Social avoidance is the tendency to avoid social interactions and information, which has a high correlation with the fear of negative evaluation [16]. Social avoidance is the cognitive component of social phobia. According to the fifth edition of the diagnostic and statistical manual of the American Psychiatric Association (APA) (2013), social phobia is defined as an obvious fear of one or more social situations, such as talking to strangers, going to a party, or performing executive activities, such as giving a speech in which the person faces others and the possibility that it will be evaluated and verified by them [17].
According to the reported research, social avoidance has a significant contribution to the increase of social phobia because avoiding fearful and worrying situations causes the continuation of distance and maintaining the beliefs and cognitive distortions that cause this disorder. Also, social avoidance leads to the loss of people’s opportunities to develop and maintain social relationships, and, it seems that avoiding social situations creates a very serious interference with people’s personal and professional lives [18].
Today, many treatment methods exist to reduce the symptoms of depression, but few of them can be effective in randomized clinical trials, one of the effective treatment methods is behavioral activation therapy [19]. This therapeutic method is one of the third-wave psychotherapy methods based on the functional analysis of behavior [20]. Since avoidance in the short term causes quick comfort and relaxation of the patient, it deprives the person of reinforcement resources in the long term; therefore, in this treatment method, the patient is taught to use an alternative and adaptive coping pattern instead of avoidance. In other words, in this treatment, the patient is taught to react with an active behavior instead of avoiding the annoying and frustrating environmental conditions [21]. Behavioral activation therapy is a structured therapeutic process that increases behaviors that increase a person’s contact with reinforcing environmental connections [22]. This method of treatment looks for the cause of disorders (such as anxiety and depression) outside the person, not inside (in the person’s life), [23].
Research results indicate the effectiveness of behavioral activation therapy in reducing anxiety and depression. For example, Chu et al. in research reported that behavioral activation therapy reduced anxiety and depression in young people [19]. Polenick and Flora, while researching behavioral activation for depression, concluded that behavioral activation training significantly reduces depression [24]. Also, in research entitled the effectiveness of group behavioral activation therapy on the symptoms of depression, anxiety and rumination in patients suffering from depression and anxiety, Zemestani et al. concluded that behavioral activation therapy significantly reduced depression, anxiety, and rumination in post-test and two-month follow-up [25]. In another study, Taheri et al. reported that behavioral activation therapy is effective in reducing the symptoms of social anxiety disorder, and this method is significantly effective in reducing the severity of symptoms of social anxiety disorder [26].
The behavioral activation model also emphasizes the role of rumination in the development and persistence of depression. Behavioral activation therapy obviously focuses on reducing rumination [27]. Behavioral activation therapists target the process of rumination rather than its content. In the behavioral activation model, rumination is conceptualized as a form of avoidance that prevents clients from facing difficult situations. Behavioral activation therapists help clients learn several techniques to cope with their thoughts and engage in crucial life activities [28]. Since short-term group behavioral activation therapy may be a promising treatment for mothers with cerebral palsy children suffering from depression, rumination, and social avoidance, the present study was conducted to investigate the effectiveness of behavioral activation on depression, social avoidance, and mental rumination of mothers of children with cerebral palsy.
Methods
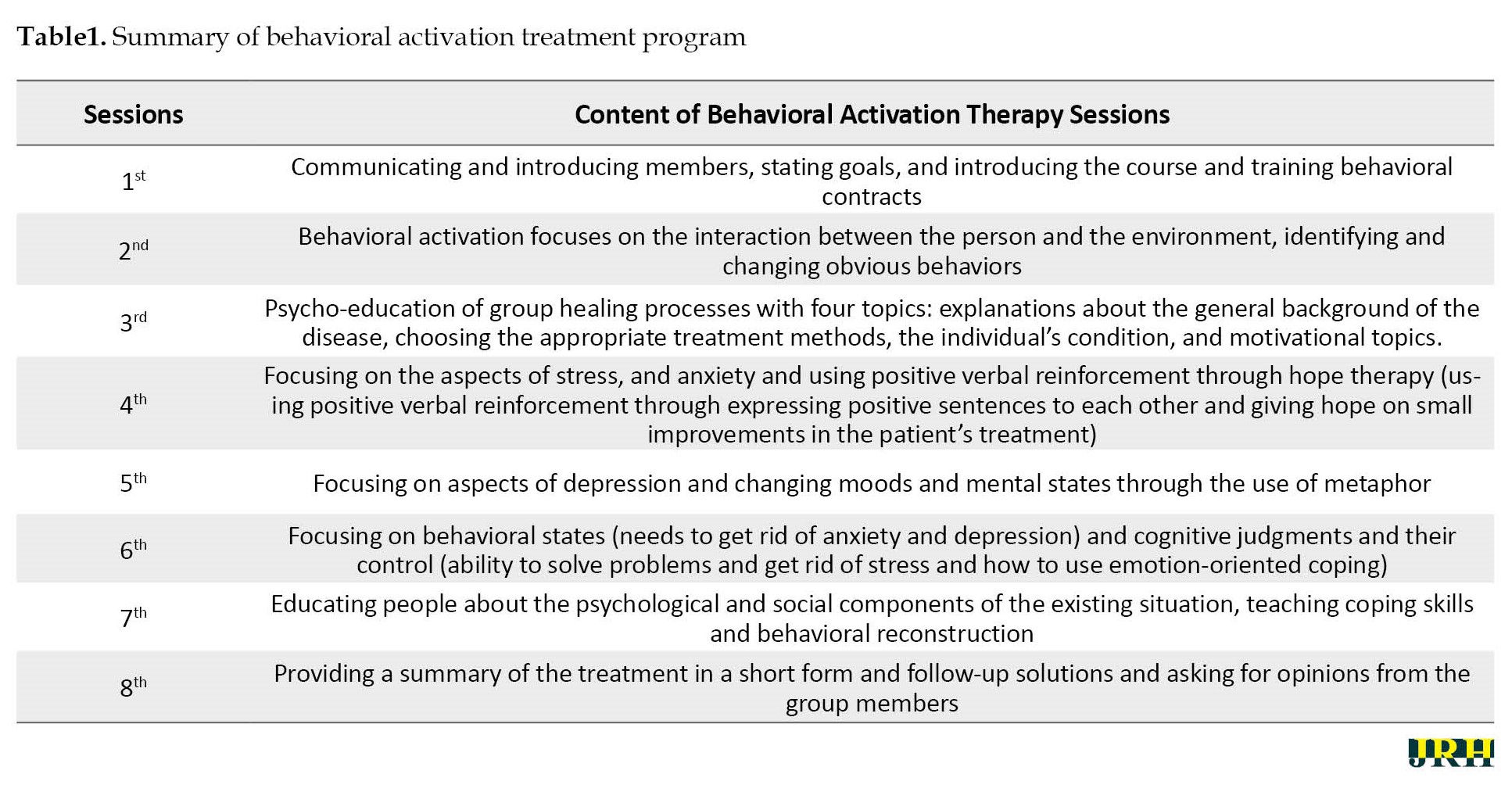
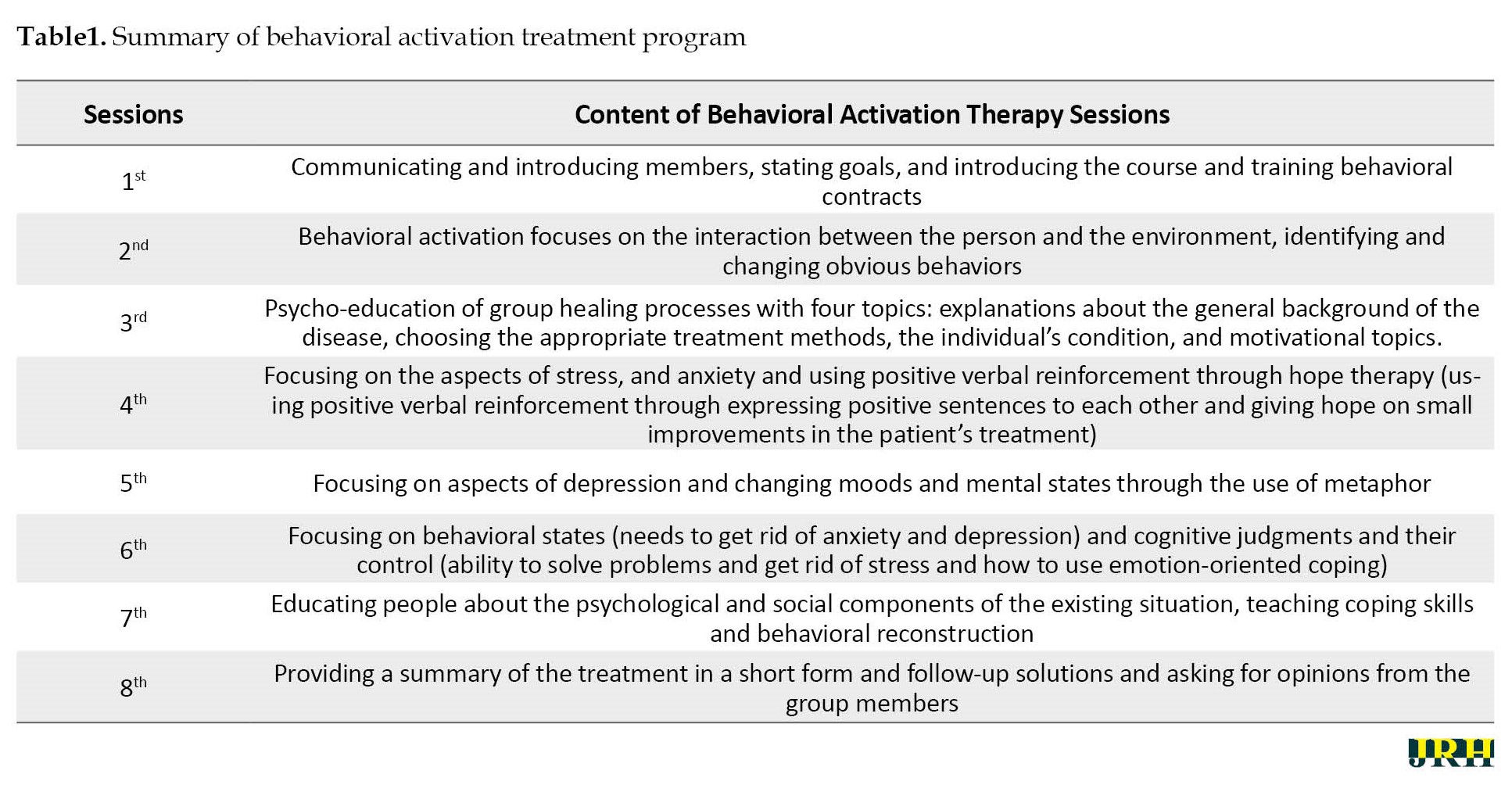
The present research design was a quasi-experimental pre-test-post-test study with an experimental group and a control group. The statistical population of the research includes 237 mothers with children with cerebral palsy who refer to the occupational therapy centers in Ilam City. First, a preliminary screening was conducted in terms of depression, mental rumination, and social avoidance among all mothers. By observing the ethical principles and receiving written consent from the subjects to participate in the research, among those who were screened, considering that in experimental studies, a minimum sample size of 15 people is recommended for each group. Forty people who had a high average score of depression, mental rumination, and social avoidance were included in the study. They were randomly selected into two groups of 20 people, an experimental group and a control group. On the entire sample, the Beck depression inventory-second edition (BDI-II), rumination, and social anxiety questionnaire were administered as a pre-test. Then the experimental group received behavioral activation group therapy based on the protocol provided by Kanter, Busch, and Rusch during 8 sessions of 90 minutes in the form of one session and group session per week. (Table 1 presents the description of the intervention sessions).
The control group did not receive any program during this period. Immediately after the treatment period, the Persian translated form of BDI-II, mental rumination questionnaire, and social anxiety questionnaire were administered individually for the group. Research data were analyzed using SPSS software, version 24 (IBM Corp., Armonk, NY, USA) and multivariate analysis of covariance (MANCOVA) statistical model. The inclusion criteria included obtaining a high score in the depression, rumination, and social anxiety questionnaire, not taking medication, not participating in any type of therapeutic intervention at the same time as participating in the research program, and expressing the desire to participate in the program in writing. The exclusion criteria included absence of more than one session in treatment sessions, diagnosis of personality disorders, presence of mood problems due to drug use or biological problems, and lack of consent to participate in research. Examining the scores of the experimental group in the research variables indicated a change in the scores of the subjects in the post-test compared to the pre-test stage. Therefore, MANCOVA was used to check the significance or non-significance of the changes made in the mentioned scores, considering the differences in the pretest. Before using this test, establish the assumptions of covariance analysis, including the normality of the distribution by the Kolmogorov-Smirnov and Shapiro-Wilk tests, the homogeneity of the regression slope, and the homogeneity of the variances, confidence was achieved at a significant level (α>0.05), (P<0.05).
Then covariance analysis was used to check the statistical significance of the experimental group scores in social avoidance components at a significant level (α<0.05). The following tools were used to collect data.
Beck depression inventory-second edition (BDI-II): The Beck depression inventory-second edition (BDI-II) is a revised form of the Beck depression inventory, which was developed to measure depression and has 21 items, the range of scores of which is from 0 to 63, the scoring method is on a continuum from 0 to 3 for each item. Scores between 0-13 indicate partial depression, 14-19 mild depression, 20-28 moderate depression, and 29-63 severe depression [29]. Beck et al. [30] reported the internal consistency of this tool to be 0.73 to 0.92 with an average of 0.86 and the α coefficient for the sick and healthy groups, respectively, 0.86 and 0.81. Dobson and Mohammad Khani [31] reported the reliability of the questionnaire using Cronbach’s α method as 0.92 for outpatients and 0.93 for students. Also, in their research, the validity of the questionnaire was reported to be 0.73 in a two-week interval. Kaviani [32] in her research reported the reliability coefficient of this questionnaire as 0.77, its validity as 0.70, and its internal consistency as 0.91. In the present study, the reliability coefficient of this questionnaire was obtained by Cronbach’s α method equal to 0.79.
Nalan Hooksema and Maro Ruminative response scale (RRS): Nalen-Hooksema and Maro (1991) developed a self-test questionnaire that assessed four different styles of reaction to negative mood. The response styles questionnaire consists of two scales of ruminating responses and a scale of distracting responses. The ruminative response scale (RRS) has 22 items and the scoring method of this questionnaire is based on the four-option Likert scale, whose options are scored from one (never) to four (always). The range of scores of this questionnaire is between 22 and 88, with a score of 33 as the cut-off point of the questionnaire, scores below 33 indicate low rumination and scores higher than that indicate high rumination, which predicts primary depression. Based on empirical evidence, the scale of rumination responses has high internal reliability. Cronbach’s α coefficient is in the range of 0.88 to 0.92. Various studies show that the test re-test correlation for rumination responses is 0.67 [33]. Among the Iranian sample in the study conducted by Mansoury et al. Cronbach’s α was 0.90. The predictive validity of the RRS has been tested in a large number of studies. The results of many studies show that the scale of rumination responses predicts the severity of depression in follow-up periods in clinical and non-clinical samples by controlling variables, such as the initial level of depression or stressful factors [34]. In the present study, the reliability coefficient of this questionnaire was obtained by Cronbach’s α method equal to 0.71.
Social anxiety questionnaire: The social anxiety questionnaire was developed by Connor et al. in 2000 to assess social phobia. It is a self-measurement scale that has 17 items. It has three subscales of fear (items 1, 3, 5, 10, 14, 15), avoidance (items 4, 6, 8, 9, 11, 12, 16) and physiological discomfort (items 2, 7, 13, 17). This questionnaire has high reliability and validity. Its validity, using the re-test method, is equal to 0.78 to 0.89 and its Cronbach’s α coefficient is reported as 0.94. Its construct validity has also been favorable [35], Amozadeh has investigated the validity and reliability of this scale among students in Iran. Its reliability was obtained at 0.97, 0.97, and 0.82, respectively, using Cronbach’s α coefficient, Spearman-Brown coefficient, and re-test. Its convergent validity with the revised 90-item phobic anxiety syndrome is equal to 0.83, and with the cognitive error scale equal to 0.47, its differential validity was reported with the self-esteem rating of 70. -0.44 and with a body image index of -0.44 [36]. In the present study, the reliability coefficient of this questionnaire was obtained by Cronbach’s α method equal to 0.74.
This treatment method was implemented in a group by a senior clinical psychology expert with an employment license from the organization of psychology and includes the following principles:
Results
The results of the present research are the results of the study of 40 mothers with cerebral palsy children with an average age of 34.13 years; an experimental group and a control group existed with the education level of diploma to master’s degree.
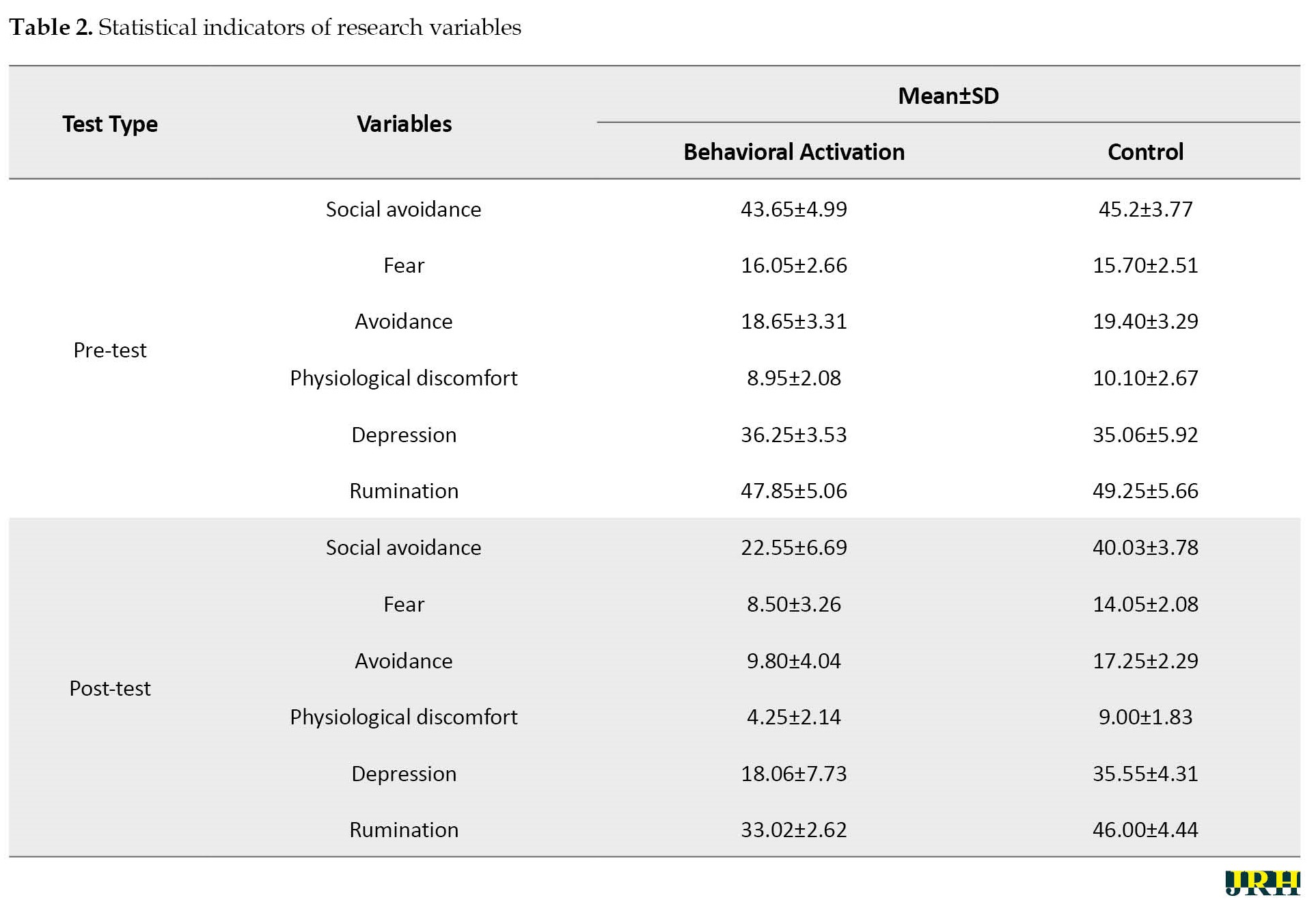
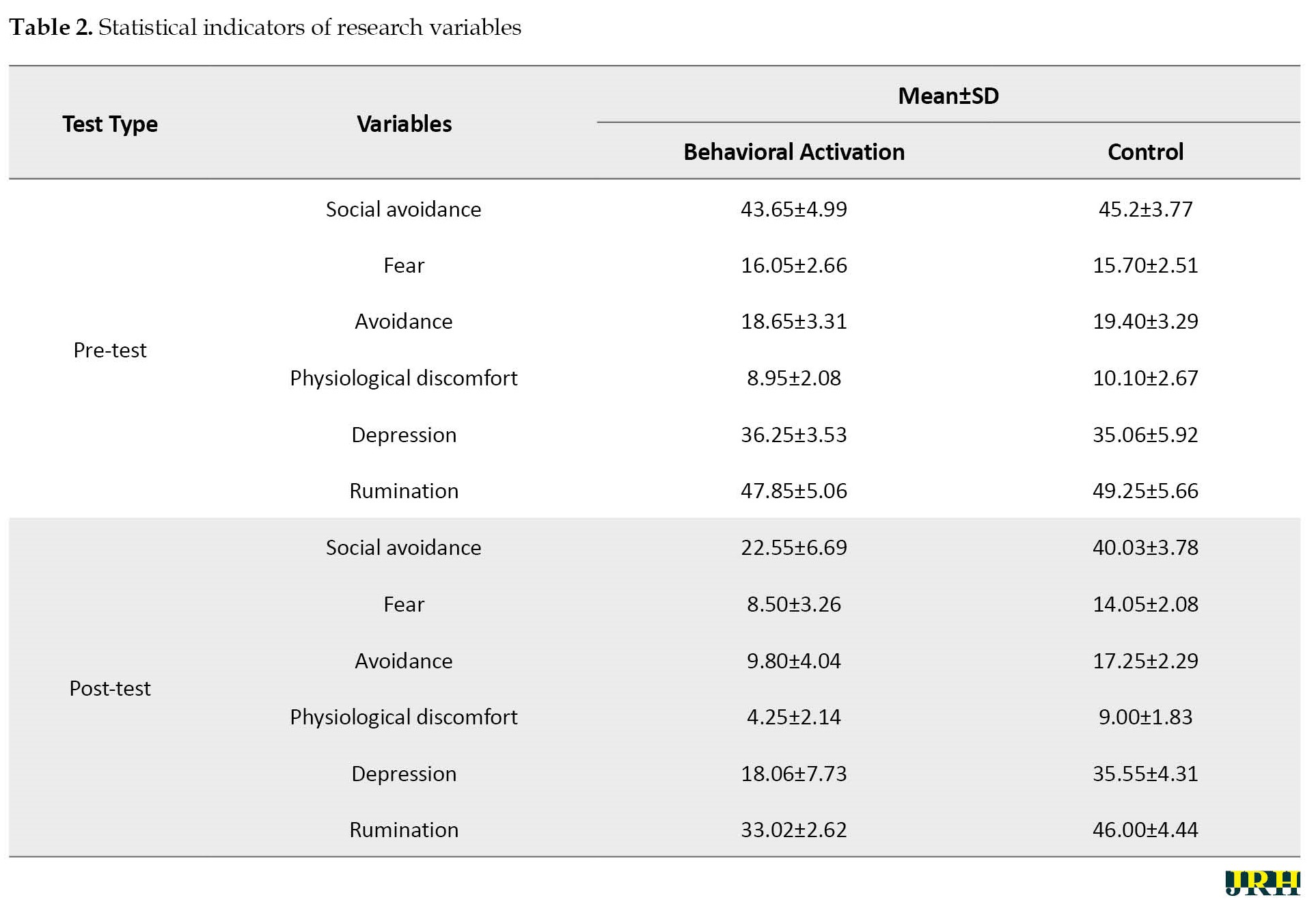
Table 2 presents the statistical indices of the two groups in the dependent variables of the research in the pre-test and post-test stages.
MANCOVA was used to analyze the data. To perform covariance analysis, its defaults were checked first.
As the data in Table 2 shows, a significant difference is observed between the mean of the experimental and control groups in the pre-test and post-test stages in the research variables. To check the difference of averages and test the hypotheses according to the presence of an extraneous source of diffraction with a minimum distance scale that cannot be directly experimentally controlled (pre-test) and also according to the presence of several dependent variables, MANCOVA was used, the results of which are shown in Table 3.
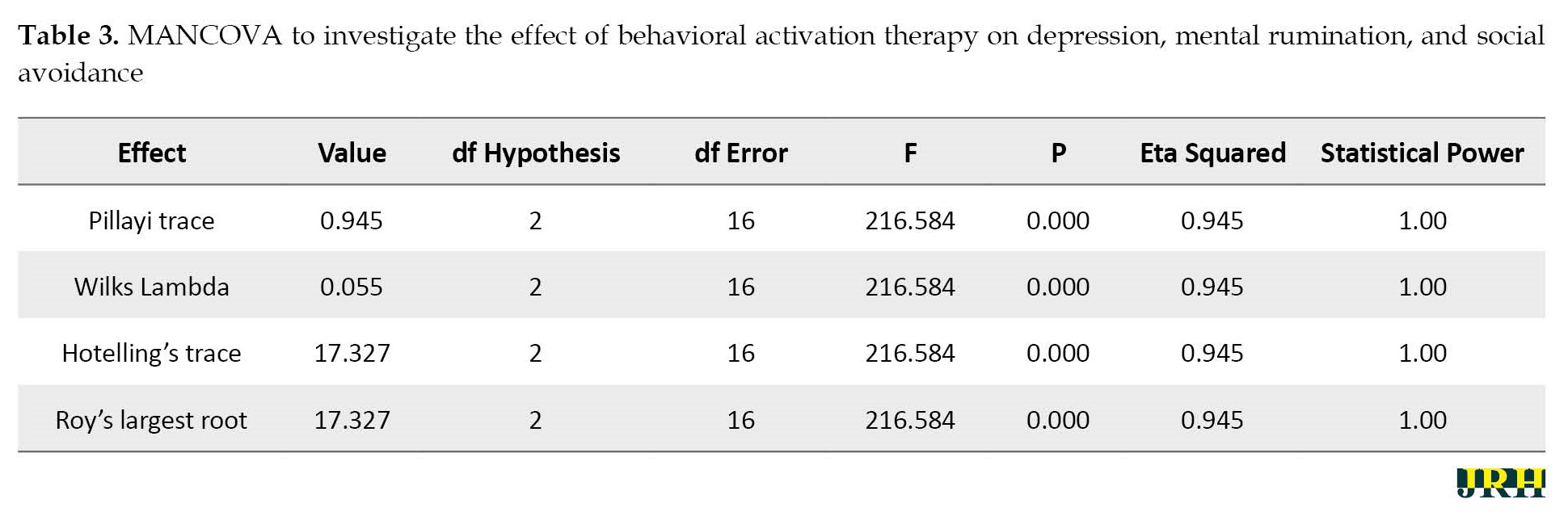
According to the results of Table 3, the value of the significance level of the F test in all four tests is less than 0.01, that is, the independent variable (behavioral activation therapy) has a significant effect on the dependent variables (depression, rumination, and social avoidance). The results of multivariate covariance analysis on the mean post-test scores of the dependent variables with the control of the pre-tests in the experimental and control groups showed that the F value of Wilks’s lambda was significant (F=216.58, P≤0.001). Based on this, a significant difference is observed between the two groups in at least one of the dependent variables. To check the point of difference, a one-way covariance analysis was performed with pre-test control. Table 4 presents the results of this analysis.
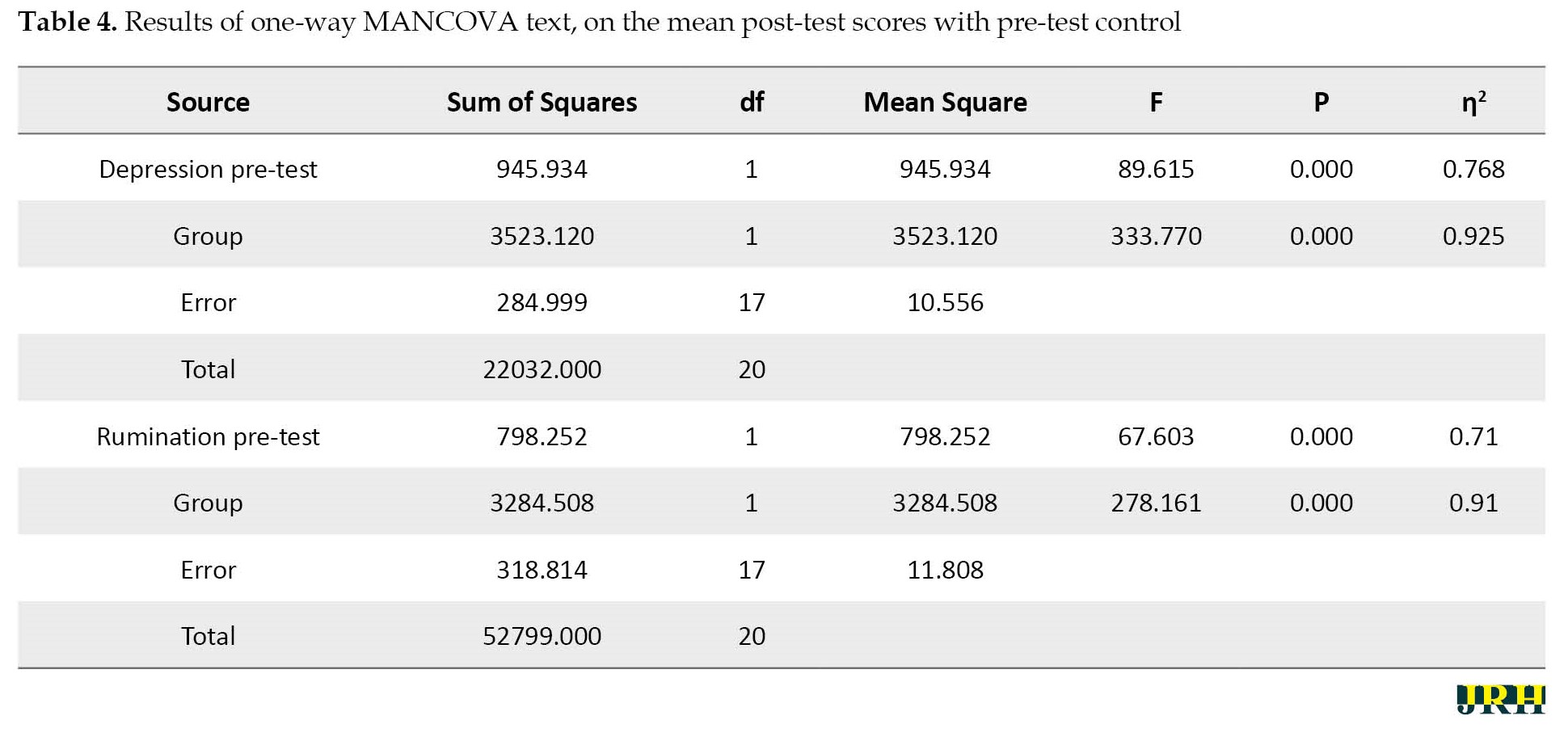
The results of Table 4 showed that the difference between the two groups in the variables of depression (F=89.615, P≤0.001) and rumination (F=67.60, P≤0.001) is significant in the post-test stage.
According to the results of Table 5, the results of the analysis of covariance indicated a significant difference between the mean scores of total social avoidance and physiological discomfort according to the group (experimental and control groups) in the post-test (P<0.05).
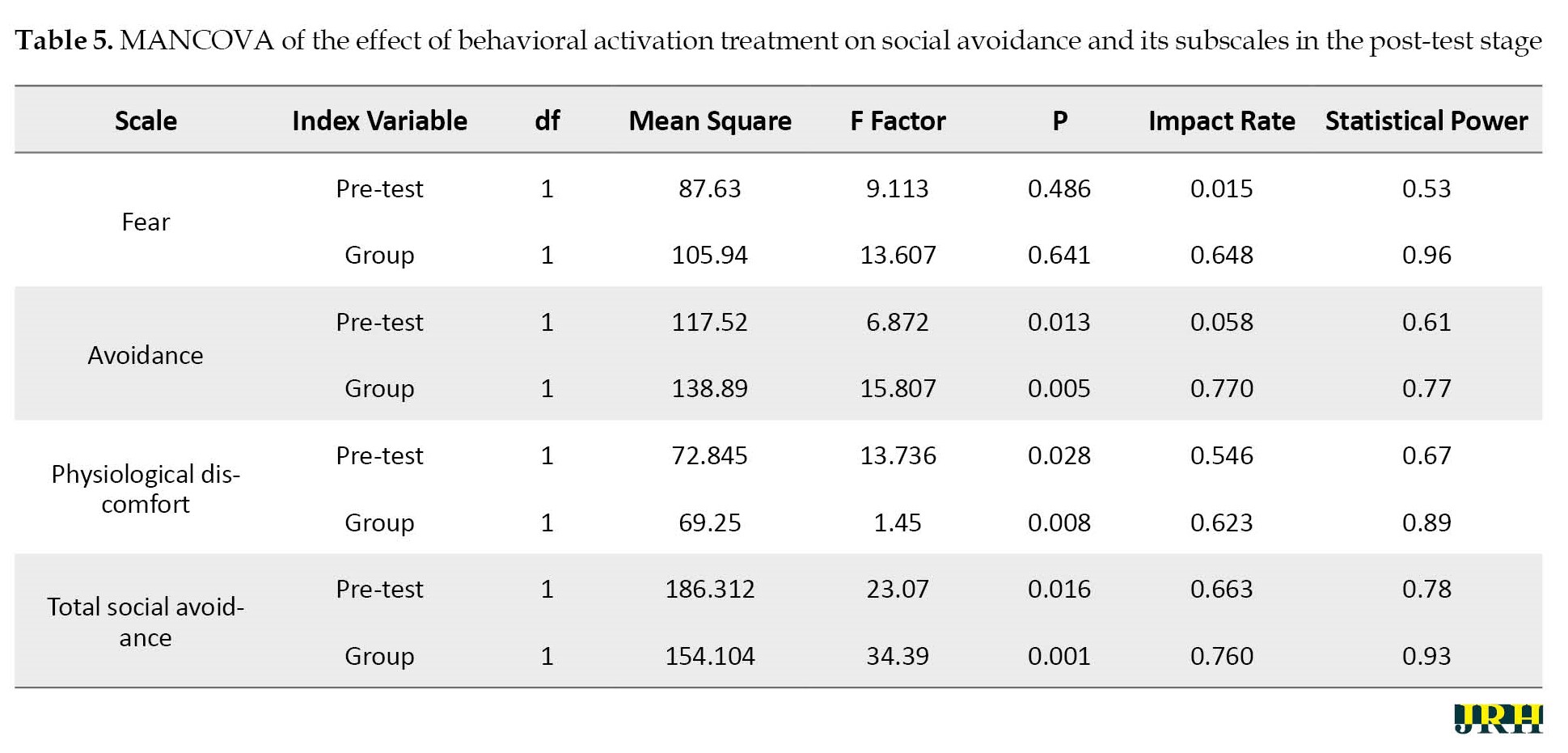
However, the effectiveness of this treatment has not been significant in the components of fear (P>0.05). Therefore, behavioral activation therapy had a positive and significant effect on social avoidance and each of its components except for fear in the post-test stage of the experimental group. The result showed that the mentioned therapy method is effective on the research variables.
Discussion
This study was conducted to investigate the effectiveness of behavioral activation group therapy on depression, mental rumination, and social avoidance in mothers with children with cerebral palsy. The present study is a promising development of the behavioral activation treatment guide in group form for mothers with children with cerebral palsy. This study found that the mean scores of depression, mental rumination, and social avoidance were high.
The clinical improvement observed in this study is consistent with the results of previous studies that have shown the effectiveness of behavioral activation therapy in depressed samples [37, 38, 39, 40]. Regarding the effectiveness of behavioral activation treatment on depression symptoms, as the interpretation of the results of the study, the behavioral theory of depression suggests that this treatment is effective because it leads to an increase in positive reinforcement. The goal of behavioral activation is to increase behaviors that are likely to lead to receiving rewards from the patient. Rewards may be intrinsic (such as pleasure or a sense of accomplishment) or extrinsic (such as social attention). These increased rewards help to improve the patient’s mood [41].
Behavioral activation therapy uses the strategy of breaking down difficult tasks into simple elements. Therefore, by implementing this strategy, depressed people can progressively achieve success, and this subsequently facilitates the achievement of positive reinforcement [42]. This therapeutic approach encourages depressed patients to become more active despite feeling tired and sad, or to try to perform behavioral tasks related to the treatment process, even if they have no motivation to do so. Over time, such a process leads to an increase in environmental reinforcement, followed by an improvement in mood [42]. Solomonov et al. [43] also suggested that the reason for the effectiveness of this treatment can be that during the treatment, people learn to change their lifestyle and follow a new rule in their lives; that is, instead of “turning off when they feel sad,” “turning on when they feel sad.” [43] Regarding the effectiveness of this treatment on rumination, it can be said that one of the goals of behavioral activation is to reduce depressing rumination through the patient’s focus on environmental activities [41].
According to the behavioral activation theory, rumination is a private behavior that prevents full involvement in life activities and therefore can act as a form of avoidance. According to this theory, rumination leads to two specific problems that are targeted at improving depression. First, rumination separates a person from her environment and focuses her on her inner thoughts instead of engaging in the activities of that moment. Second, rumination prevents fruitful problem-solving [44]. Behavioral activation therapy uses specific techniques, such as highlighting the consequences of rumination, problem-solving, paying close attention to sensory experience, refocusing on the task at hand, and redirecting one’s attention away from ruminative and problematic thoughts. These techniques provide a way to target the rumination process without interfering with the content of thoughts [44]. The present study is consistent with previous studies [42, 45], showing that behavioral activation therapy has a significant effect on reducing depressive rumination. This result implicitly has crucial implications, which can be considered as proof of the successful performance of behavioral activation in changing cognitions. The behavioral change created by behavioral activation therapy may lead to a change in beliefs and cognitions, which are essential components for long-lasting emotional and behavioral change. In addition, it has been suggested that behavioral modification (and therefore behavioral activation therapy) may represent an effective method of changing cognitions [44].
The effectiveness of group behavioral activation therapy in reducing the severity of social avoidance symptoms is by the results of new research that has investigated the effect of behavioral activation therapy on anxiety disorders [46]. In a study, 23 students with social anxiety disorder were treated with 8 sessions of cognitive-behavioral therapy and behavioral activation.
These results provide evidence that real-time increases in activity levels (activation) that are functionally related to anxious behaviors may be associated with decreased anxiety. The outcomes of the study have crucial implications for the practitioner seeking to provide cost-effective treatment for adult anxiety in typical outpatient settings. BA targets avoidance, withdrawal, isolation, and inactivity, it is hypothesized that BA will favorably affect social anxiety and depression symptoms [47]. However, avoidance behaviors will be targeted through examining the individual’s behavioral repertoire, rather than through exposure techniques, possibly making BA acceptable to clients. BA strategies (e.g. scheduling and participating in positively reinforcing and or valued activities) may enhance exposure therapy for social anxiety symptoms by directly targeting comorbid depression symptoms and areas of functional impairment. BA highlights the relationship between stressful life events and the development of psychopathology, both emphasize the concepts of avoidance and engagement. BA strategies may target a broader range of symptoms and psychosocial domains [48].
This is further supported by results from a study in which Martins Oud et al. [49] found that treatment was performed equally well and concluded that BA was one of the most cost-effective treatment methods for depression. If several treatments are equally effective for one specific disorder, the most cost-effective alternative should be chosen. BA requires fewer amounts of training and time and can be taught to therapists with less training and experience in the treatment of social anxiety symptoms. Behavioral strategies consist of restoring an adequate schedule of positive reinforcement in the person’s life, thereby reducing depression. Commonly, alterations are made in the frequency, quality, and range of the patient’s activities and social relationships. Targeting avoidance behaviors may be a crucial innovation. Addressing avoidance is standard in treatments for anxiety, and recent models propose that avoidance may be a fundamental element underlying multiple psychopathologies and that blocking avoidance may be a critical element of treatment [19].
Avoidance minimizes immediate distress at the cost of diminishing opportunities to reinforce and exacerbate ongoing stressors. BA explicitly targets the reduction of avoidance behaviors related to both intrapersonal and interpersonal difficulties. The BA model uses focused activation strategies to explicitly target avoidance patterns and associated functional consequences. In essence, in BA, patients learn to identify patterns of avoidance and to respond with activation; this basic principle is applied repeatedly across multiple situations in therapy. BA encourages attention to the consequences of ruminating (avoidance and withdrawal) and the use of activation strategies as alternatives [50].
In this regard, BA shares critical elements with other contemporary behavioral therapies that emphasize function rather than topography of behavior. Emphasis on the utility or function of thinking may have a particularly critical role in the treatment of depression. Patients are encouraged to notice when they are ruminating and to move their attention away from the content of ruminative thoughts toward direct and immediate experience; for instance, a patient may be asked to experiment with attending to the sights, smells, or sounds around her when she notices rumination [51].
Conclusion
As indicated, the results of the study showed that among the mothers with children with cerebral palsy, the mean scores of depression, mental rumination, and social avoidance were high, which potentially have crucial practical implications for improving people’s mental health and preventing the occurrence of depression, mental rumination and social avoidance in mothers with children with cerebral palsy. One of the implications of these results is that behavioral activation therapy is beneficial as a short-term group therapy and can be considered a cost-effective treatment. Therefore, short-term group behavioral activation therapy may be a promising treatment for mothers with cerebral palsy children suffering from depression, rumination, and social avoidance.
Limitation and recommendation
The present research had limitations, including low sample volume, using self-report questionnaires as a data collection tool, not having a follow-up stage, and not measuring the placebo effect of the treatment on the control group. Certainly, the generalizability of the results requires more research in this field. Therefore, it is suggested to conduct further studies with a larger sample and on clinical patients referring to psychology and psychiatry counseling centers. It is also suggested to consider the follow-up stage in future studies and to conduct longer follow-ups. Long-term follow-up evaluations can help understand the long-term effects of this treatment on depression, rumination, and social avoidance.
Ethical Considerations
Compliance with ethical guidelines
The current study was approved by the Ilam Branch, Islamic Azad Univerity (Code: IR.IAU.ILAM.REC.1401.045). The participants provided written informed consent to take part in this study and assured that their information would remain confidential.
Funding
The paper was extracted from the PhD dissertation of Mostafa Alirahmi, approved by Department of Psychology, Faculty of Human Sciences, Ilam Branch, Islamic Azad Univerity.
Authors' contributions
Study design and manuscript preparation: Mostafa Alirahmi, Sattar Kikhavani, Akbar Azizifar and Homeira Soleimannejad; Data collection: Mostafa Alirahmi and Sattar Kikhavani; Statistical analysis and intervention: Sehat Aibod; Review and editing: Akbar Azizifar; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors hereby express their gratitude and appreciation to all the dear ones who somehow played a role in the implementation of this research and facilitated its implementation process, especially the assistance of occupational therapy centers in Ilam City.
References
Disabled children need more care and their parents bear the most stress to care for them [1]. Caring for a child with cerebral palsy requires intensive and long-term care activities [2] and these chronic conditions cause the parents of these children to experience more physical and mental health problems [3]. In most cultures of the world, mothers are more responsible for raising their children and are usually the main caregivers of disabled children [4]. Studies conducted in Iran also indicate that 91.4% of caregivers of children with cerebral palsy are mothers [5]. Although some mothers cope well with problems; mothers with disabled children have more physical disorders, depression, anxiety, tension, and nervous pressure, and less self-confidence than other mothers. These mothers also feel lonely and have problems in their communication with the people around them [6] because the presence of a child with cerebral palsy in the family causes intense feelings of stress, depression, and guilt to the extent that these families reduce their social activities due to these feelings [7].
Research results show that the prevalence of depression and rumination in mothers of children with developmental disorders is higher than in mothers of healthy children. Also, the unpredictable future in the case of a child with cerebral palsy leads to fatigue and tension in parents [8]. Since the mother is the first person who communicates directly with the child; feelings, such as guilt, fault, inadequacy, and deprivation caused by the child’s abnormality can cause isolation, lack of interest in establishing a relationship with the environment, and a decrease in self-esteem. Feelings of low self-esteem, worthlessness, and sadness in the mother, which results in depression, can jeopardize the mother’s mental health, and psychological helplessness [9].
Depression includes symptoms, such as apathy, sadness, and dysfunctional thoughts [10]. In recent years, examining maladaptive thinking patterns in emotional disorders and their role in the persistence of these disorders has been the focus of experts and clinical researchers. One of these maladaptive patterns in emotional disorders, such as depression is rumination [11]. Rumination is defined as the repeated and recurring thoughts about negative moods or life events [12]. According to Martin and Teiser, the concept of rumination refers to a thinking style that tends to repeat itself [13]. From their point of view, rumination introduces a set of conscious thoughts that revolve around a crucial issue and these thoughts appear even in the absence of immediate and necessary environmental demands. By providing signs, the external environment may lead to maintaining these thoughts, but at the same time, maintaining these thoughts and their continuation is not dependent on environmental signs. Also, rumination is defined as resistant and recurrent thoughts that go around a common topic, enter consciousness involuntarily, and divert attention from desired topics, and current goals [14]. The results of Siegel’s research showed multiple and separate constructs to measure the variable of rumination and each measure alone represents a specific aspect of rumination that is related to depression and mental health [15]. In the study conducted by Chu et al., it was found that behavioral activation therapy had better results in the treatment of severely depressed patients than drug therapy and cognitive therapy. Also, this treatment significantly reduced depression and rumination in the post-test and two-month follow-up stages. Conceptually, this treatment method is suitable as an inter-diagnostic intervention to deal with depression and rumination [16].
Social avoidance is the tendency to avoid social interactions and information, which has a high correlation with the fear of negative evaluation [16]. Social avoidance is the cognitive component of social phobia. According to the fifth edition of the diagnostic and statistical manual of the American Psychiatric Association (APA) (2013), social phobia is defined as an obvious fear of one or more social situations, such as talking to strangers, going to a party, or performing executive activities, such as giving a speech in which the person faces others and the possibility that it will be evaluated and verified by them [17].
According to the reported research, social avoidance has a significant contribution to the increase of social phobia because avoiding fearful and worrying situations causes the continuation of distance and maintaining the beliefs and cognitive distortions that cause this disorder. Also, social avoidance leads to the loss of people’s opportunities to develop and maintain social relationships, and, it seems that avoiding social situations creates a very serious interference with people’s personal and professional lives [18].
Today, many treatment methods exist to reduce the symptoms of depression, but few of them can be effective in randomized clinical trials, one of the effective treatment methods is behavioral activation therapy [19]. This therapeutic method is one of the third-wave psychotherapy methods based on the functional analysis of behavior [20]. Since avoidance in the short term causes quick comfort and relaxation of the patient, it deprives the person of reinforcement resources in the long term; therefore, in this treatment method, the patient is taught to use an alternative and adaptive coping pattern instead of avoidance. In other words, in this treatment, the patient is taught to react with an active behavior instead of avoiding the annoying and frustrating environmental conditions [21]. Behavioral activation therapy is a structured therapeutic process that increases behaviors that increase a person’s contact with reinforcing environmental connections [22]. This method of treatment looks for the cause of disorders (such as anxiety and depression) outside the person, not inside (in the person’s life), [23].
Research results indicate the effectiveness of behavioral activation therapy in reducing anxiety and depression. For example, Chu et al. in research reported that behavioral activation therapy reduced anxiety and depression in young people [19]. Polenick and Flora, while researching behavioral activation for depression, concluded that behavioral activation training significantly reduces depression [24]. Also, in research entitled the effectiveness of group behavioral activation therapy on the symptoms of depression, anxiety and rumination in patients suffering from depression and anxiety, Zemestani et al. concluded that behavioral activation therapy significantly reduced depression, anxiety, and rumination in post-test and two-month follow-up [25]. In another study, Taheri et al. reported that behavioral activation therapy is effective in reducing the symptoms of social anxiety disorder, and this method is significantly effective in reducing the severity of symptoms of social anxiety disorder [26].
The behavioral activation model also emphasizes the role of rumination in the development and persistence of depression. Behavioral activation therapy obviously focuses on reducing rumination [27]. Behavioral activation therapists target the process of rumination rather than its content. In the behavioral activation model, rumination is conceptualized as a form of avoidance that prevents clients from facing difficult situations. Behavioral activation therapists help clients learn several techniques to cope with their thoughts and engage in crucial life activities [28]. Since short-term group behavioral activation therapy may be a promising treatment for mothers with cerebral palsy children suffering from depression, rumination, and social avoidance, the present study was conducted to investigate the effectiveness of behavioral activation on depression, social avoidance, and mental rumination of mothers of children with cerebral palsy.
Methods
The present research design was a quasi-experimental pre-test-post-test study with an experimental group and a control group. The statistical population of the research includes 237 mothers with children with cerebral palsy who refer to the occupational therapy centers in Ilam City. First, a preliminary screening was conducted in terms of depression, mental rumination, and social avoidance among all mothers. By observing the ethical principles and receiving written consent from the subjects to participate in the research, among those who were screened, considering that in experimental studies, a minimum sample size of 15 people is recommended for each group. Forty people who had a high average score of depression, mental rumination, and social avoidance were included in the study. They were randomly selected into two groups of 20 people, an experimental group and a control group. On the entire sample, the Beck depression inventory-second edition (BDI-II), rumination, and social anxiety questionnaire were administered as a pre-test. Then the experimental group received behavioral activation group therapy based on the protocol provided by Kanter, Busch, and Rusch during 8 sessions of 90 minutes in the form of one session and group session per week. (Table 1 presents the description of the intervention sessions).
The control group did not receive any program during this period. Immediately after the treatment period, the Persian translated form of BDI-II, mental rumination questionnaire, and social anxiety questionnaire were administered individually for the group. Research data were analyzed using SPSS software, version 24 (IBM Corp., Armonk, NY, USA) and multivariate analysis of covariance (MANCOVA) statistical model. The inclusion criteria included obtaining a high score in the depression, rumination, and social anxiety questionnaire, not taking medication, not participating in any type of therapeutic intervention at the same time as participating in the research program, and expressing the desire to participate in the program in writing. The exclusion criteria included absence of more than one session in treatment sessions, diagnosis of personality disorders, presence of mood problems due to drug use or biological problems, and lack of consent to participate in research. Examining the scores of the experimental group in the research variables indicated a change in the scores of the subjects in the post-test compared to the pre-test stage. Therefore, MANCOVA was used to check the significance or non-significance of the changes made in the mentioned scores, considering the differences in the pretest. Before using this test, establish the assumptions of covariance analysis, including the normality of the distribution by the Kolmogorov-Smirnov and Shapiro-Wilk tests, the homogeneity of the regression slope, and the homogeneity of the variances, confidence was achieved at a significant level (α>0.05), (P<0.05).
Then covariance analysis was used to check the statistical significance of the experimental group scores in social avoidance components at a significant level (α<0.05). The following tools were used to collect data.
Beck depression inventory-second edition (BDI-II): The Beck depression inventory-second edition (BDI-II) is a revised form of the Beck depression inventory, which was developed to measure depression and has 21 items, the range of scores of which is from 0 to 63, the scoring method is on a continuum from 0 to 3 for each item. Scores between 0-13 indicate partial depression, 14-19 mild depression, 20-28 moderate depression, and 29-63 severe depression [29]. Beck et al. [30] reported the internal consistency of this tool to be 0.73 to 0.92 with an average of 0.86 and the α coefficient for the sick and healthy groups, respectively, 0.86 and 0.81. Dobson and Mohammad Khani [31] reported the reliability of the questionnaire using Cronbach’s α method as 0.92 for outpatients and 0.93 for students. Also, in their research, the validity of the questionnaire was reported to be 0.73 in a two-week interval. Kaviani [32] in her research reported the reliability coefficient of this questionnaire as 0.77, its validity as 0.70, and its internal consistency as 0.91. In the present study, the reliability coefficient of this questionnaire was obtained by Cronbach’s α method equal to 0.79.
Nalan Hooksema and Maro Ruminative response scale (RRS): Nalen-Hooksema and Maro (1991) developed a self-test questionnaire that assessed four different styles of reaction to negative mood. The response styles questionnaire consists of two scales of ruminating responses and a scale of distracting responses. The ruminative response scale (RRS) has 22 items and the scoring method of this questionnaire is based on the four-option Likert scale, whose options are scored from one (never) to four (always). The range of scores of this questionnaire is between 22 and 88, with a score of 33 as the cut-off point of the questionnaire, scores below 33 indicate low rumination and scores higher than that indicate high rumination, which predicts primary depression. Based on empirical evidence, the scale of rumination responses has high internal reliability. Cronbach’s α coefficient is in the range of 0.88 to 0.92. Various studies show that the test re-test correlation for rumination responses is 0.67 [33]. Among the Iranian sample in the study conducted by Mansoury et al. Cronbach’s α was 0.90. The predictive validity of the RRS has been tested in a large number of studies. The results of many studies show that the scale of rumination responses predicts the severity of depression in follow-up periods in clinical and non-clinical samples by controlling variables, such as the initial level of depression or stressful factors [34]. In the present study, the reliability coefficient of this questionnaire was obtained by Cronbach’s α method equal to 0.71.
Social anxiety questionnaire: The social anxiety questionnaire was developed by Connor et al. in 2000 to assess social phobia. It is a self-measurement scale that has 17 items. It has three subscales of fear (items 1, 3, 5, 10, 14, 15), avoidance (items 4, 6, 8, 9, 11, 12, 16) and physiological discomfort (items 2, 7, 13, 17). This questionnaire has high reliability and validity. Its validity, using the re-test method, is equal to 0.78 to 0.89 and its Cronbach’s α coefficient is reported as 0.94. Its construct validity has also been favorable [35], Amozadeh has investigated the validity and reliability of this scale among students in Iran. Its reliability was obtained at 0.97, 0.97, and 0.82, respectively, using Cronbach’s α coefficient, Spearman-Brown coefficient, and re-test. Its convergent validity with the revised 90-item phobic anxiety syndrome is equal to 0.83, and with the cognitive error scale equal to 0.47, its differential validity was reported with the self-esteem rating of 70. -0.44 and with a body image index of -0.44 [36]. In the present study, the reliability coefficient of this questionnaire was obtained by Cronbach’s α method equal to 0.74.
This treatment method was implemented in a group by a senior clinical psychology expert with an employment license from the organization of psychology and includes the following principles:
Results
The results of the present research are the results of the study of 40 mothers with cerebral palsy children with an average age of 34.13 years; an experimental group and a control group existed with the education level of diploma to master’s degree.
Table 2 presents the statistical indices of the two groups in the dependent variables of the research in the pre-test and post-test stages.
MANCOVA was used to analyze the data. To perform covariance analysis, its defaults were checked first.
As the data in Table 2 shows, a significant difference is observed between the mean of the experimental and control groups in the pre-test and post-test stages in the research variables. To check the difference of averages and test the hypotheses according to the presence of an extraneous source of diffraction with a minimum distance scale that cannot be directly experimentally controlled (pre-test) and also according to the presence of several dependent variables, MANCOVA was used, the results of which are shown in Table 3.
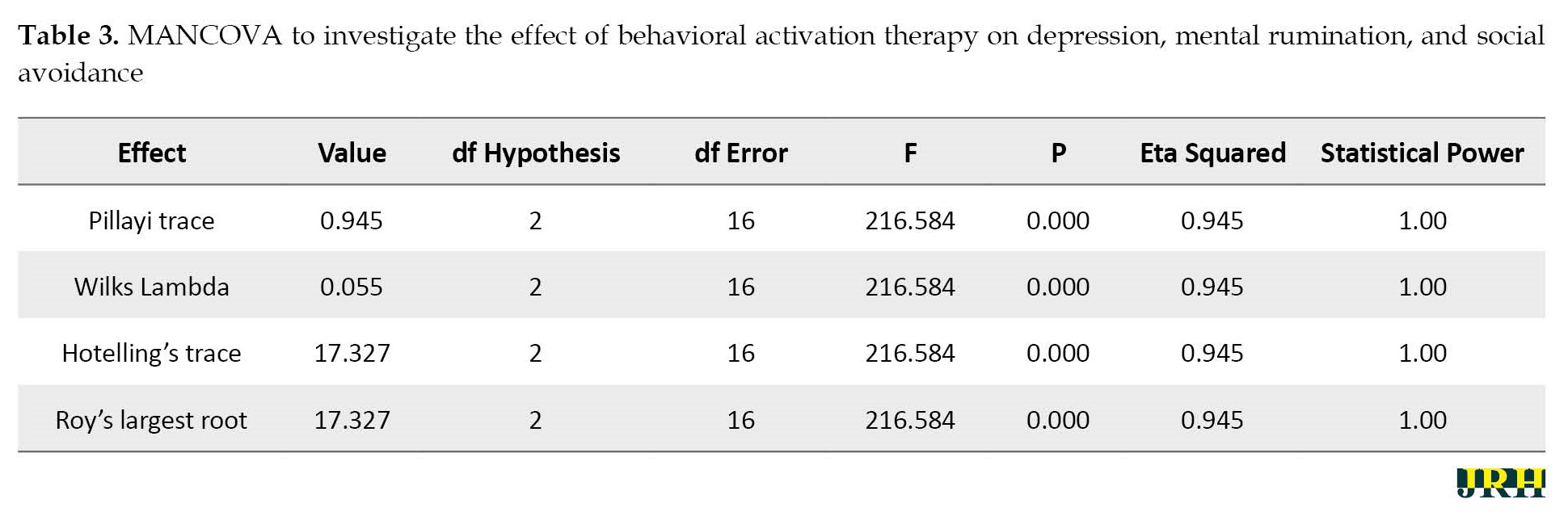
According to the results of Table 3, the value of the significance level of the F test in all four tests is less than 0.01, that is, the independent variable (behavioral activation therapy) has a significant effect on the dependent variables (depression, rumination, and social avoidance). The results of multivariate covariance analysis on the mean post-test scores of the dependent variables with the control of the pre-tests in the experimental and control groups showed that the F value of Wilks’s lambda was significant (F=216.58, P≤0.001). Based on this, a significant difference is observed between the two groups in at least one of the dependent variables. To check the point of difference, a one-way covariance analysis was performed with pre-test control. Table 4 presents the results of this analysis.
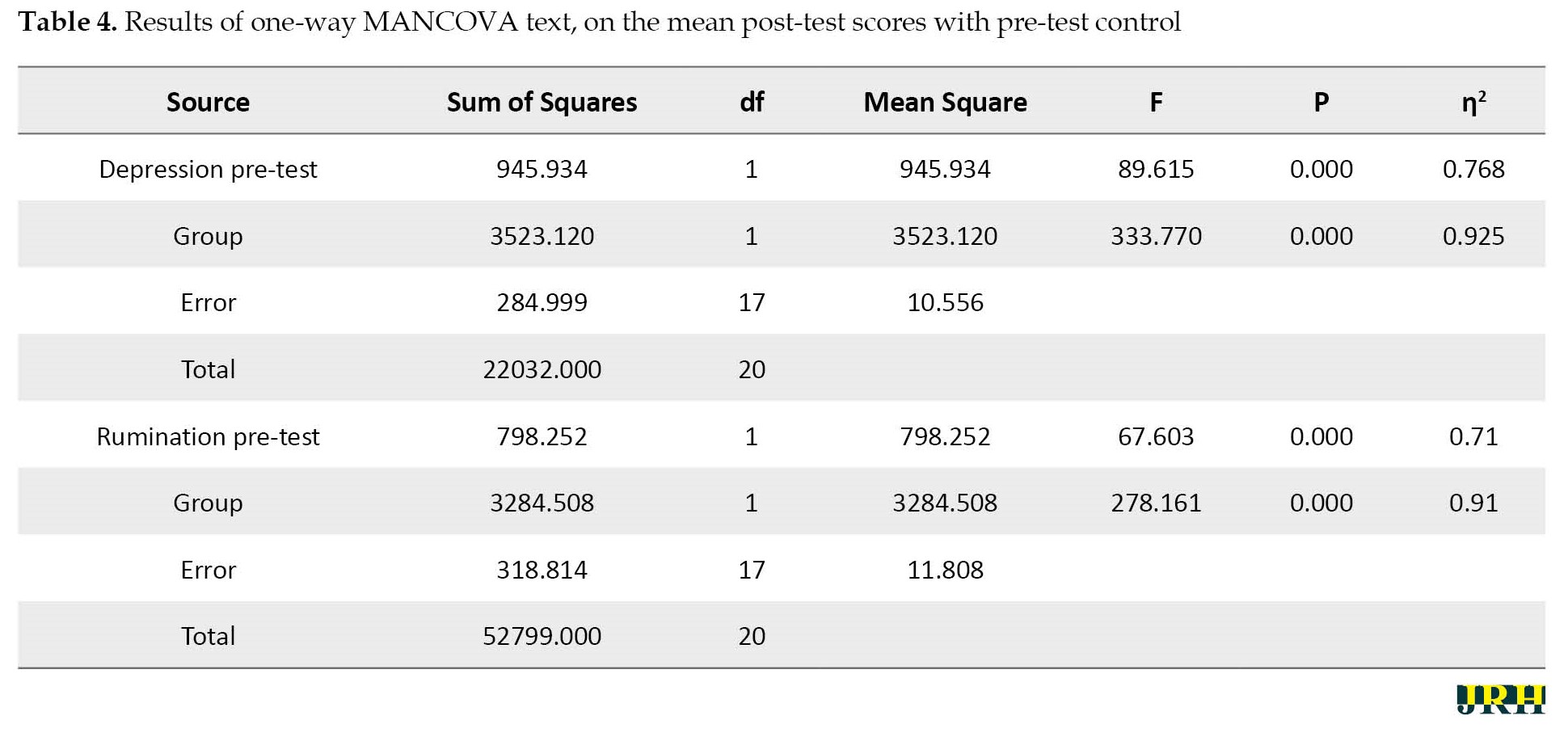
The results of Table 4 showed that the difference between the two groups in the variables of depression (F=89.615, P≤0.001) and rumination (F=67.60, P≤0.001) is significant in the post-test stage.
According to the results of Table 5, the results of the analysis of covariance indicated a significant difference between the mean scores of total social avoidance and physiological discomfort according to the group (experimental and control groups) in the post-test (P<0.05).
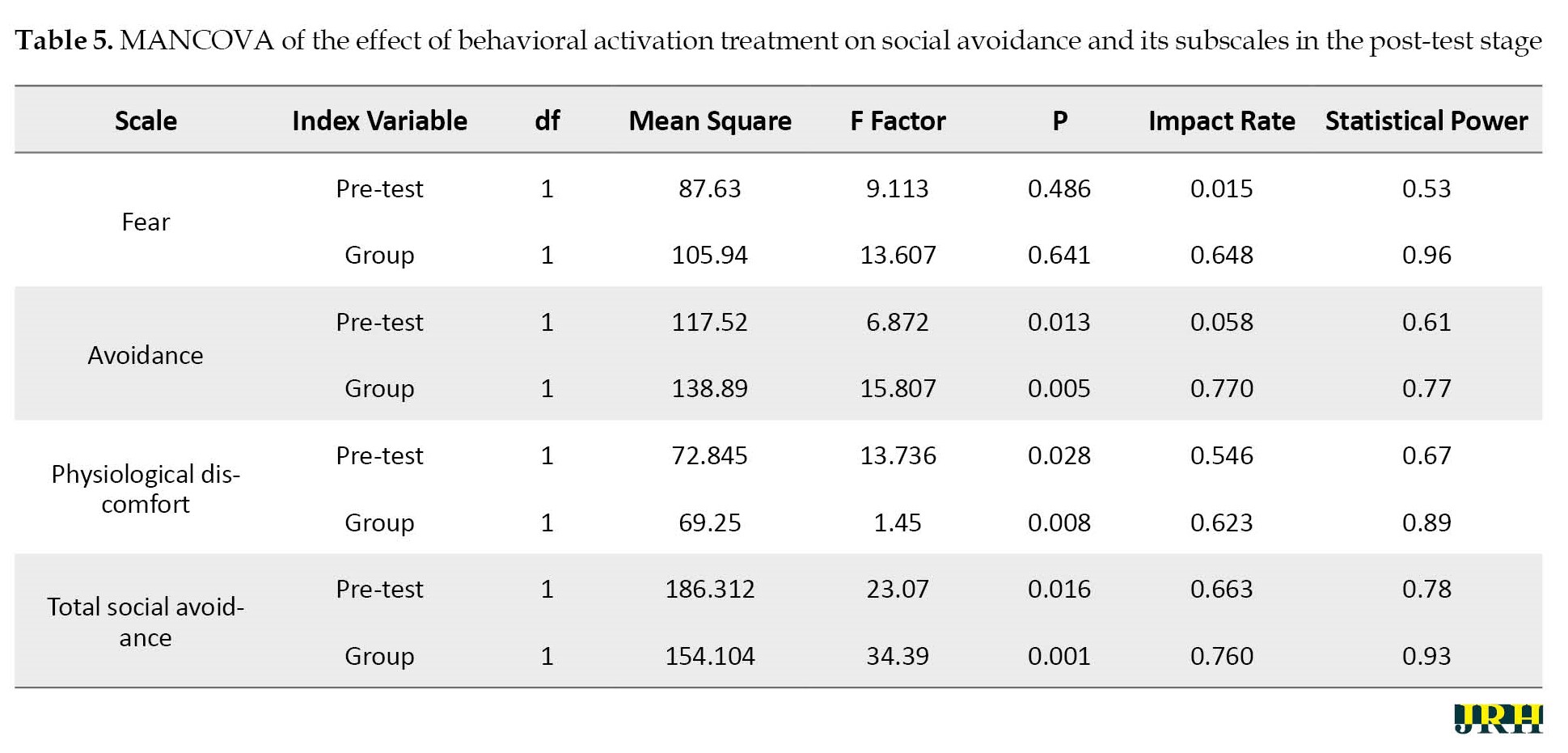
However, the effectiveness of this treatment has not been significant in the components of fear (P>0.05). Therefore, behavioral activation therapy had a positive and significant effect on social avoidance and each of its components except for fear in the post-test stage of the experimental group. The result showed that the mentioned therapy method is effective on the research variables.
Discussion
This study was conducted to investigate the effectiveness of behavioral activation group therapy on depression, mental rumination, and social avoidance in mothers with children with cerebral palsy. The present study is a promising development of the behavioral activation treatment guide in group form for mothers with children with cerebral palsy. This study found that the mean scores of depression, mental rumination, and social avoidance were high.
The clinical improvement observed in this study is consistent with the results of previous studies that have shown the effectiveness of behavioral activation therapy in depressed samples [37, 38, 39, 40]. Regarding the effectiveness of behavioral activation treatment on depression symptoms, as the interpretation of the results of the study, the behavioral theory of depression suggests that this treatment is effective because it leads to an increase in positive reinforcement. The goal of behavioral activation is to increase behaviors that are likely to lead to receiving rewards from the patient. Rewards may be intrinsic (such as pleasure or a sense of accomplishment) or extrinsic (such as social attention). These increased rewards help to improve the patient’s mood [41].
Behavioral activation therapy uses the strategy of breaking down difficult tasks into simple elements. Therefore, by implementing this strategy, depressed people can progressively achieve success, and this subsequently facilitates the achievement of positive reinforcement [42]. This therapeutic approach encourages depressed patients to become more active despite feeling tired and sad, or to try to perform behavioral tasks related to the treatment process, even if they have no motivation to do so. Over time, such a process leads to an increase in environmental reinforcement, followed by an improvement in mood [42]. Solomonov et al. [43] also suggested that the reason for the effectiveness of this treatment can be that during the treatment, people learn to change their lifestyle and follow a new rule in their lives; that is, instead of “turning off when they feel sad,” “turning on when they feel sad.” [43] Regarding the effectiveness of this treatment on rumination, it can be said that one of the goals of behavioral activation is to reduce depressing rumination through the patient’s focus on environmental activities [41].
According to the behavioral activation theory, rumination is a private behavior that prevents full involvement in life activities and therefore can act as a form of avoidance. According to this theory, rumination leads to two specific problems that are targeted at improving depression. First, rumination separates a person from her environment and focuses her on her inner thoughts instead of engaging in the activities of that moment. Second, rumination prevents fruitful problem-solving [44]. Behavioral activation therapy uses specific techniques, such as highlighting the consequences of rumination, problem-solving, paying close attention to sensory experience, refocusing on the task at hand, and redirecting one’s attention away from ruminative and problematic thoughts. These techniques provide a way to target the rumination process without interfering with the content of thoughts [44]. The present study is consistent with previous studies [42, 45], showing that behavioral activation therapy has a significant effect on reducing depressive rumination. This result implicitly has crucial implications, which can be considered as proof of the successful performance of behavioral activation in changing cognitions. The behavioral change created by behavioral activation therapy may lead to a change in beliefs and cognitions, which are essential components for long-lasting emotional and behavioral change. In addition, it has been suggested that behavioral modification (and therefore behavioral activation therapy) may represent an effective method of changing cognitions [44].
The effectiveness of group behavioral activation therapy in reducing the severity of social avoidance symptoms is by the results of new research that has investigated the effect of behavioral activation therapy on anxiety disorders [46]. In a study, 23 students with social anxiety disorder were treated with 8 sessions of cognitive-behavioral therapy and behavioral activation.
These results provide evidence that real-time increases in activity levels (activation) that are functionally related to anxious behaviors may be associated with decreased anxiety. The outcomes of the study have crucial implications for the practitioner seeking to provide cost-effective treatment for adult anxiety in typical outpatient settings. BA targets avoidance, withdrawal, isolation, and inactivity, it is hypothesized that BA will favorably affect social anxiety and depression symptoms [47]. However, avoidance behaviors will be targeted through examining the individual’s behavioral repertoire, rather than through exposure techniques, possibly making BA acceptable to clients. BA strategies (e.g. scheduling and participating in positively reinforcing and or valued activities) may enhance exposure therapy for social anxiety symptoms by directly targeting comorbid depression symptoms and areas of functional impairment. BA highlights the relationship between stressful life events and the development of psychopathology, both emphasize the concepts of avoidance and engagement. BA strategies may target a broader range of symptoms and psychosocial domains [48].
This is further supported by results from a study in which Martins Oud et al. [49] found that treatment was performed equally well and concluded that BA was one of the most cost-effective treatment methods for depression. If several treatments are equally effective for one specific disorder, the most cost-effective alternative should be chosen. BA requires fewer amounts of training and time and can be taught to therapists with less training and experience in the treatment of social anxiety symptoms. Behavioral strategies consist of restoring an adequate schedule of positive reinforcement in the person’s life, thereby reducing depression. Commonly, alterations are made in the frequency, quality, and range of the patient’s activities and social relationships. Targeting avoidance behaviors may be a crucial innovation. Addressing avoidance is standard in treatments for anxiety, and recent models propose that avoidance may be a fundamental element underlying multiple psychopathologies and that blocking avoidance may be a critical element of treatment [19].
Avoidance minimizes immediate distress at the cost of diminishing opportunities to reinforce and exacerbate ongoing stressors. BA explicitly targets the reduction of avoidance behaviors related to both intrapersonal and interpersonal difficulties. The BA model uses focused activation strategies to explicitly target avoidance patterns and associated functional consequences. In essence, in BA, patients learn to identify patterns of avoidance and to respond with activation; this basic principle is applied repeatedly across multiple situations in therapy. BA encourages attention to the consequences of ruminating (avoidance and withdrawal) and the use of activation strategies as alternatives [50].
In this regard, BA shares critical elements with other contemporary behavioral therapies that emphasize function rather than topography of behavior. Emphasis on the utility or function of thinking may have a particularly critical role in the treatment of depression. Patients are encouraged to notice when they are ruminating and to move their attention away from the content of ruminative thoughts toward direct and immediate experience; for instance, a patient may be asked to experiment with attending to the sights, smells, or sounds around her when she notices rumination [51].
Conclusion
As indicated, the results of the study showed that among the mothers with children with cerebral palsy, the mean scores of depression, mental rumination, and social avoidance were high, which potentially have crucial practical implications for improving people’s mental health and preventing the occurrence of depression, mental rumination and social avoidance in mothers with children with cerebral palsy. One of the implications of these results is that behavioral activation therapy is beneficial as a short-term group therapy and can be considered a cost-effective treatment. Therefore, short-term group behavioral activation therapy may be a promising treatment for mothers with cerebral palsy children suffering from depression, rumination, and social avoidance.
Limitation and recommendation
The present research had limitations, including low sample volume, using self-report questionnaires as a data collection tool, not having a follow-up stage, and not measuring the placebo effect of the treatment on the control group. Certainly, the generalizability of the results requires more research in this field. Therefore, it is suggested to conduct further studies with a larger sample and on clinical patients referring to psychology and psychiatry counseling centers. It is also suggested to consider the follow-up stage in future studies and to conduct longer follow-ups. Long-term follow-up evaluations can help understand the long-term effects of this treatment on depression, rumination, and social avoidance.
Ethical Considerations
Compliance with ethical guidelines
The current study was approved by the Ilam Branch, Islamic Azad Univerity (Code: IR.IAU.ILAM.REC.1401.045). The participants provided written informed consent to take part in this study and assured that their information would remain confidential.
Funding
The paper was extracted from the PhD dissertation of Mostafa Alirahmi, approved by Department of Psychology, Faculty of Human Sciences, Ilam Branch, Islamic Azad Univerity.
Authors' contributions
Study design and manuscript preparation: Mostafa Alirahmi, Sattar Kikhavani, Akbar Azizifar and Homeira Soleimannejad; Data collection: Mostafa Alirahmi and Sattar Kikhavani; Statistical analysis and intervention: Sehat Aibod; Review and editing: Akbar Azizifar; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors hereby express their gratitude and appreciation to all the dear ones who somehow played a role in the implementation of this research and facilitated its implementation process, especially the assistance of occupational therapy centers in Ilam City.
References
- Meral BF, Wehmeyer ML, Cinisli NA, Yilmaz E. The positive psychology constructs of parents of children with intellectual and developmental disabilities in Turkey. Journal of Intellectual Disability Research. 2021; 65(7):638-54. [DOI:10.1111/jir.12839] [PMID]
- Nobakht Z, Rassafiani M, Hosseini SA, Hosseinzadeh S. A web-based daily care training to improve the quality of life of mothers of children with cerebral palsy: A randomized controlled trial. Research in Developmental Disabilities. 2020; 105:103731. [DOI:10.1016/j.ridd.2020.103731] [PMID]
- Vadivelan K, Sekar P, Sruthi SS, Gopichandran V. Burden of caregivers of children with cerebral palsy: An intersectional analysis of gender, poverty, stigma, and public policy. BMC Public Health. 2020; 20(1):645. [DOI:10.1186/s12889-020-08808-0] [PMID]
- Lee MH, Matthews AK, Park C. Determinants of health-related quality of life among mothers of children with cerebral palsy. Journal of Pediatric Nursing. 2019; 44:1-8. [DOI:10.1016/j.pedn.2018.10.001] [PMID]
- Ahmadi Kahjoogh M, Kessler D, Hosseini SA, Rassafiani M, Akbarfahimi N, Khankeh HR, et al. Randomized controlled trial of occupational performance coachingfor mothers of children with cerebral palsy. British Journal of Occupational Therapy. 2019; 82(4):213-9. [DOI:10.1177/0308022618799944]
- Sharma R, Singh H, Murti M, Chatterjee K, Rakkar JS. Depression and anxiety in parents of children and adolescents with intellectual disability. Industrial Psychiatry Journal. 2021; 30(2):291-8. [DOI:10.4103/ipj.ipj_216_20] [PMID]
- Goheir A, Jadoon A, Fayyaz SS, Kiran N, Akhtar N, Qamar Z. Severity of depression in mothers of children suffering from cerebral palsy. Pakistan Journal of Medical & Health Sciences. 2022; 16(08):18. [DOI:10.53350/pjmhs2216818]
- Austin A, Lin JP, Selway R, Ashkan K, Owen T. What parents think and feel about deep brain stimulation in paediatric secondary dystonia including cerebral palsy: A qualitative study of parental decision-making. European Journal of Paediatric Neurology. 2017; 21(1):185-92. [DOI:10.1016/j.ejpn.2016.08.011] [PMID]
- Tabrizchi N, Vahidi Z. [Comparing emotional regulation, mindfulness and psychological well-being in mothers of students with and without learning disabilities (Persian)]. Journal of Learning Disabilities. 2015; 4(4):21-35. [Link]
- Schreiber KL, Zinboonyahgoon N, Xu X, Spivey T, King T, Dominici L, et al. Preoperative psychosocial and psychophysical phenotypes as predictors of acute pain outcomes after breast surgery. The Journal of Pain. 2019; 20(5):540-56. [DOI:10.1016/j.jpain.2018.11.004] [PMID]
- Ghorbani N, Watson PJ, Hargis MB. Integrative Self-Knowledge Scale: Correlations and incremental validity of a cross-cultural measure developed in Iran and the United States. The Journal of Psychology. 2008; 142(4):395-412. [DOI:10.3200/JRPL.142.4.395-412] [PMID]
- Robinson M, Alloy LB. Negative cognitive styles and stress-reactive rumination interact to predict depression: A prospective study. Cognitive Therapy and Research. 2003; 27(3):275-91. [Link]
- Wyer RS, SrullTK. Advances in social cognition. A dual process model of impression formation. New York: Psychology Press; 2014. [DOI: 10.4324/9781315801940]
- Joormann J. Differential effects of rumination and dysphoria on the inhibition of irrelevant emotional material: Evidence from a negative priming task. Cognitive Therapy and Research. 2006; 30(2):149-60. [DOI:10.1007/s10608-006-9035-8]
- Siegle G, Steinhauer S, Carter C, Thase M. Convergence and divergence in measures of rumination. Paper presented at: 34 th Annual Convention of the Association for Advancement of Behaviour Therapy, New Orleans; 2000. [Link]
- Wright DB, Busnello RH, Buratto LG, Stein LM. Are valence and social avoidance associated with the memory conformity effect? Acta Psychologica. 2012; 141(1):78-85. [DOI:10.1016/j.actpsy.2012.06.008] [PMID]
- Asher M, Asnaani A, Aderka IM. Gender differences in social anxiety disorder: A review. Clinical Psychology Review. 2017; 56:1-12. [DOI:10.1016/j.cpr.2017.05.004] [PMID]
- Miers AC, Blöte AW, Heyne DA, Westenberg PM. Developmental pathways of social avoidance across adolescence: The role of social anxiety and negative cognition. Journal of Anxiety Disorders. 2014; 28(8):787-94. [DOI:10.1016/j.janxdis.2014.09.008] [PMID]
- Chu BC, Crocco ST, Esseling P, Areizaga MJ, Lindner AM, Skriner LC. Transdiagnostic group behavioral activation and exposure therapy for youth anxiety and depression: Initial randomized controlled trial. Behaviour Research and Therapy. 2016; 76:65-75. [DOI:10.1016/j.brat.2015.11.005] [PMID]
- Moshier SJ, Otto MW. Behavioral activation treatment for major depression: A randomized trial of the efficacy of augmentation with cognitive control training. Journal of Affective Disorders. 2017; 210:265-8. [DOI:10.1016/j.jad.2017.01.003] [PMID]
- Richards DA, Ekers D, McMillan D, Taylor RS, Byford S, Warren FC, et al. Cost and outcome of behavioural activation versus cognitive behavioural therapy for depression (COBRA): A randomised, controlled, non-inferiority trial. The Lancet. 2016; 388(10047):871-80. [DOI:10.1016/S0140-6736(16)31140-0] [PMID]
- Stein AT, Carl E, Cuijpers P, Karyotaki E, Smits JAJ. Looking beyond depression: A meta-analysis of the effect of behavioral activation on depression, anxiety, and activation. Psychological Medicine. 2021; 51(9):1491-504. [DOI:10.1017/S0033291720000239] [PMID]
- Pan C, Tie B, Yuwen W, Su X, Deng Y, Ma X, et al. ‘Mindfulness Living with Insomnia’: An mHealth intervention for individuals with insomnia in China: A study protocol of a randomised controlled trial. BMJ Open. 2022; 12(2):e053501. [DOI:10.1136/bmjopen-2021-053501] [PMID]
- Polenick CA, Flora SR. Behavioral activation for depression in older adults: Theoretical and practical considerations. The Behavior Analyst. 2013; 36(1):35-55. [DOI:10.1007/BF03392291] [PMID]
- Zemestani M, Davoudi I, Mehrabizadeh HM, Zargar Y. [Effectiveness of group behavioral activation on depression, anxiety and rumination in patients with depression and anxiety (Persian)]. Journal of Clinical Psychology. 2014; 5(4):73-84. [Link]
- Taheri E, Amiri M, Birashk B, Gharrayi B. Cognitive therapy versus behavioral activation therapy in the treatment of social anxiety disorder. Journal of Fundamentals of Mental Health. 2016;18(5):294-9. [DOI:10.22038/JFMH.2016.7481]
- Watkins ER. Rumination-focused cognitive-behavioral therapy for depression. New York: Guilford Publications; 2018. [Link]
- Martell CR, Dimidjian S, Herman-Dunn R. Behavioral activation for depression: A clinician's guide. New York: Guilford Publications; 2021. [Link]
- Thombs BD, Ziegelstein RC, Beck CA, Pilote L. A general factor model for the Beck Depression Inventory-II: Validation in a sample of patients hospitalized with acute myocardial infarction. Journal of Psychosomatic Research. 2008; 65(2):115-21. [DOI:10.1016/j.jpsychores.2008.02.027] [PMID]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988; 56(6):893-7. [DOI:10.1037/0022-006X.56.6.893] [PMID]
- Stefan-Dabson K, Mohammadkhani P, Massah-Choulabi O. [Psychometrics characteristic of Beck Depression Inventory-II in patients with magor depressive disorder (Persian)]. Archives of Rehabilitation. 2007; 8:0-6. [Link]
- Kaviani H, Seiforian H, Sharifi V, Ebrahimkhani N. [Reliability and validity of Anxiety and Depression Hospital Scales (HADS): Iranian patients with anxiety and depression disorders (Persian)]. Tehran University of Medical Sciences Journal. 2009; 67(5):379-85. [Link]
- Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta Earthquake. Journal of Personality and Social Psychology. 1991; 61(1):115-21. [DOI:10.1037/0022-3514.61.1.115] [PMID]
- Mansoury A, Bashipour R, Mahmoud A, Farnam A, Fakhari A. [Comparison of worries, obsessive compulsive and ruminant in people with generalized anxiety disorder, obsessive-compulsive disorder, major depressive disorder, and normal people (Persian)]. Psychological Studies. 2011; 7(4):55-74. [Link]
- Connor KM, Davidson JR, Churchill LE, Sherwood A, Foa E, Weisler RH. Psychometric properties of the Social Phobia Inventory (SPIN): New self-rating scale. The British Journal of Psychiatry. 2000; 176(4):379-86. [DOI:10.1192/bjp.176.4.379] [PMID]
- Hassanvand Amouzadeh M. [Validity and reliability of social phobia inventory in students with social anxiety (Persian)]. Journal of Mazandaran University of Medical Sciences. 2016; 26(139):166-77. [Link]
- Fazzino TL, Lejuez CW, Yi R. A behavioral activation intervention administered in a 16-week freshman orientation course: Study protocol. Contemporary Clinical Trials. 2020; 90:105950. [DOI:10.1016/j.cct.2020.105950] [PMID]
- Sailer P, Wieber F, Pröpster K, Stoewer S, Nischk D, Volk F, et al. A brief intervention to improve exercising in patients with schizophrenia: a controlled pilot study with mental contrasting and implementation intentions (MCII). BMC psychiatry. 2015; 15:211. [DOI:10.1186/s12888-015-0513-y] [PMID]
- Houghton S, Curran J, Ekers D. Behavioural activation in the treatment of depression. Mental Health Practice. 2011; 14(7):18-23. [DOI:10.7748/mhp2011.04.14.7.18.c8407]
- Gawrysiak M, Nicholas C, Hopko DR. Behavioral activation for moderately depressed university students: Randomized controlled trial. Journal of Counseling Psychology. 2009; 56(3):468-75. [DOI:10.1037/a0016383]
- Menear M, Girard A, Dugas M, Gervais M, Gilbert M, Gagnon MP. Personalized care planning and shared decision making in collaborative care programs for depression and anxiety disorders: A systematic review. Plos One. 2022; 17(6):e0268649. [DOI:10.1371/journal.pone.0268649] [PMID]
- Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. Focus. 2018; 16(4):420-9. [DOI:10.1176/appi.focus.16407] [PMID]
- Solomonov N, Bress JN, Sirey JA, Gunning FM, Flückiger C, Raue PJ, et al. Engagement in socially and interpersonally rewarding activities as a predictor of outcome in “Engage” behavioral activation therapy for late-life depression. The American Journal of Geriatric Psychiatry. 2019; 27(6):571-8. [DOI:10.1016/j.jagp.2018.12.033] [PMID]
- Wang X, Zhou X, Yang H. Guided self-help behavioral activation intervention for geriatric depression: Protocol for pilot randomized controlled trial. JMIR Research Protocols. 2020; 9(9):e18259. [DOI:10.2196/18259] [PMID]
- Ledari RB, Masjedi A, Bakhtyari M, Zarghami M, Nouri R, Hosseini H. A comparison between the effectiveness of acceptance and commitment treatment and behavioral activation treatment for depression on symptoms severity and rumination among patients with treatment-resistant depression. Iranian Journal of Psychiatry and Behavioral Sciences. 2018; 12(3):e10742. [Link]
- Boswell JF, Iles BR, Gallagher MW, Farchione TJ. Behavioral activation strategies in cognitive-behavioral therapy for anxiety disorders. Psychotherapy. 2017; 54(3):231-6. [DOI:10.1037/pst0000119] [PMID]
- Walsh S, Moseley GL, Gray RJ, Gillam M, Gunn KM, Barker T, et al. Use of behavioural activation to manage pain: A systematic scoping review. BMJ Open. 2022; 12(6):e056404. [DOI:10.1136/bmjopen-2021-056404] [PMID]
- Martin F, Oliver T. Behavioral activation for children and adolescents: A systematic review of progress and promise. European Child & Adolescent Psychiatry. 2019; 28(4):427-41. [DOI:10.1007/s00787-018-1126-z] [PMID]
- Oud M, De Winter L, Vermeulen-Smit E, Bodden D, Nauta M, Stone L, et al. Effectiveness of CBT for children and adolescents with depression: A systematic review and meta-regression analysis. European Psychiatry. 2019; 57:33-45. [DOI:10.1016/j.eurpsy.2018.12.008] [PMID]
- Nagy GA, Cernasov P, Pisoni A, Walsh E, Dichter GS, Smoski MJ. Reward network modulation as a mechanism of change in behavioral activation. Behav Modif. 2020; 44(2):186-213. [DOI:10.1177/0145445518805682] [PMID]
- Soleimani M, Mohammadkhani P, Dolatshahi B, Alizadeh H, Overmann KA, Coolidge FL.A comparative study of group behavioral activation and cognitive therapy in reducing subsyndromal anxiety and depressive symptoms. Iranian Journal of Psychiatry. 2015; 10(2):71-8. [PMID]
Type of Study: Orginal Article |
Subject:
● Psychosocial Health
Received: 2023/06/16 | Accepted: 2023/06/20 | Published: 2024/02/1
Received: 2023/06/16 | Accepted: 2023/06/20 | Published: 2024/02/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









