Volume 13, Issue 6 (Nov & Dec 2023)
J Research Health 2023, 13(6): 427-436 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Falah Neudehi M, Rezaei F, Bozorgi Kazerooni A, Ebadi Z. Emotion Regulation Training on Irritability, Alexithymia, and Interpersonal Problems of Adolescents With Disruptive Mood Dysregulation Disorder. J Research Health 2023; 13 (6) :427-436
URL: http://jrh.gmu.ac.ir/article-1-2245-en.html
URL: http://jrh.gmu.ac.ir/article-1-2245-en.html
1- Department of Educational Sciences and Psychology, Payame Noor University, Tehran, Iran.
2- Department of Clinical Psychology, Faculty of Literature Humanities and Social Sciences, Science and Research Branch, Islamic Azad University, Tehran, Iran. ,farnazrezaei.91@yahoo.com
3- Department of General Psychology, Faculty of Psychology and Educational Sciences, Marvdasht Branch, Islamic Azad University, Marvdasht, Iran.
4- Department of Psychology, Payame Noor University, Tehran, Iran.
2- Department of Clinical Psychology, Faculty of Literature Humanities and Social Sciences, Science and Research Branch, Islamic Azad University, Tehran, Iran. ,
3- Department of General Psychology, Faculty of Psychology and Educational Sciences, Marvdasht Branch, Islamic Azad University, Marvdasht, Iran.
4- Department of Psychology, Payame Noor University, Tehran, Iran.
Keywords: Emotion regulation, Irritability, Alexithymia, Interpersonal problems, Adolescents, Mood disorder
Full-Text [PDF 733 kb]
(1190 Downloads)
| Abstract (HTML) (3324 Views)
Full-Text: (1066 Views)
1. Introduction
Chronic, severe irritability is a common problem in children and adolescents [1]. Reflecting this pressing public health need, such a diagnostic and statistical manual of mental disorders, 5th edition (DSM-5) as disruptive mood dysregulation disorder (DMDD) [1, 2]. The prevalence estimates for severe irritability in school-age children and adolescents range from 0.12% to 5%, with 3% being the most common estimate for DMDD [1]. Irritable people are likely to suffer from poor functional outcomes throughout their lives, including concurrent and longitudinal emotional disorders, suicidality, poor school performance, and difficulties in their social and professional lives. Children with high irritability also have distinct physiological profiles, including hyper-reactivity to stress and perception of threats. The central diagnostic feature of DMDD is chronic and severe irritability, leading to functional impairment. DMDD has been operationalized for research as severe irritability related to hyper-arousal symptoms (agitation and distractibility) [3]. As relevant to emotion regulation, the pathophysiology of severe irritability has been associated with reduced context-dependent regulation, dysregulated attention-emotion interactions, and the misinterpretation of social cues, such as a preferential threat bias [4]. It is common for adolescents to develop behavioral problems because of emotional dysregulation during adolescence. Dysregulation of emotion refers to the inability to control one’s affective expression in different circumstances. As a result, it has little flexibility and spontaneity, a lack of control, and demonstration of disruptive behaviors [5]. Alexithymia and low emotion differentiation restrict access to emotional information and increase the propensity toward dysregulated and deviant behaviors, such as impulsive aggression [6].
In the study by Edwards & Wupperman (2017), alexithymic features and emotion differentiation explained nearly 43% of the variance in impulsive aggression. These relationships were fully mediated by emotion-regulation difficulty [6]. Moreover, the difficulty identifying feelings subscale of the Toronto alexithymia scale (TAS-20) was positively associated with alcohol problems through emotional dysregulation and psychological distress [7]. Inflexible emotion regulation increases allostatic load from frequent stress, inadequate reactivity, failed shutdown, and habituation. They may result in physical and mental illness. Alexithymia exemplifies inflexible emotion regulation with dysfunctions potentially across all stages of emotion processing, both psychologically and physiologically [8]. The findings suggested that the interpersonal style of alexithymic individuals is characterized by cold and socially avoidant behavior, corresponding to the predominantly insecure attachment pattern found in alexithymia [9].
A previous study showed that the TAS-20 scores correlate with numerous psychiatric concerns, mainly in the internalizing spectrum, thought difficulties, and self-reported aggression [10]. Furthermore, results revealed institutionalized girls to be more alexithymic, showing more difficulty identifying and describing feelings than boys, similar to community groups. Higher alexithymia was related to more total, internalizing, and externalizing problems through similar mechanisms of risk in community groups [11]. Concerning mood regulation, Besharat and Shahidi showed adolescent addicts with statistically significant differences compared to the control group. They showed lower attention to their feelings and lower repair of mood. Patients had low clarity of feelings and low mood repair significantly related to the first substance abuse (cannabinoids), and a significant relation between low attention to feelings and the cause of drug abuse was peer pressure and novelty-seeking [12]. Interpersonal difficulties are experienced with others and cause mental distress or are associated with mental disturbances. They include difficulties in assertiveness, sociability, submissiveness, intimacy, responsibility, and control. People with alexithymia cannot correctly identify emotions from other individuals’ faces. They cannot always show sympathy toward other individuals [13]. Analysis shows a direct relationship between alexithymia and social, familial, and romantic loneliness. Moreover, interpersonal distrust partly mediates this relationship, and alexithymia and interpersonal distrust interact to predict social and family loneliness. These findings suggest that links between the facets of alexithymia, interpersonal distrust, and loneliness are complex and multifaceted and discussed concerning interventions for young adolescents [14].
Considering therapeutic techniques currently available to clinicians may help target pathophysiological processes in severe mood dysregulation, and DMDD is useful. Comprehensive treatments for these patients will likely integrate well-conceptualized tools from extant interventions with novel advances tailored to the mechanisms of chronic irritability. Currently, DMDD is a severe and impairing psychiatric disorder without any validated psychotherapeutic or psycho-pharmacological interventions [4]. Currently, no gold standard, evidence-based treatments exist exclusively for DMDD or severe mood dysregulation; however, interventions designed for related clinical disorders have demonstrated promising findings, including parent management training, cognitive-behavioral therapy, and psychopharmacological interventions [4]. Non-pharmacological therapies throughout the treatment course included cognitive behavioral therapy, dialectical behavior therapy, 12-step facilitation, contingency management, family systems therapy, motivational enhancement therapy, psychodynamic psychotherapy, and motivational interviewing [15]. Since DMDD has recently been added as an efficacious treatment that specifically targets severe irritability, its presence in DMDD is still being developed [16]. The therapeutic emotion regulation process for children diagnosed with DMDD is a primary target, aiming to promote the child’s emotional development [17]. From a clinical perspective, emotion regulation is of utmost importance in interventions for childhood emotional and behavioral disorders, which are often aimed at promoting child self-regulation, approved in numerous studies [4, 17-21]. This study aims to implement self-regulation training techniques for adolescents with a disruptive mood disorder, emphasizing irritability, alexithymia, and interpersonal problems in adolescents with DMDD.
2. Methods
To evaluate the effectiveness of group training, we used the quasi-experimental method with a pre-test/post-test design and a control group. The study population comprised all 13 to 16 year-old girls in Tehran City, Iran, from 2022 to 2023 who had DMDD. A total of 30 girls were selected based on the multi-stage cluster random sampling method. The adequacy of the sample size was confirmed by the G*Power software, version 3.1.9.7 (α=0.05 and test power=0.80). Four junior high schools were randomly selected from the education districts of Tehran. Next, 6 classes from each school (seventh, eighth, and ninth grade) were chosen. Based on the questionnaire, 30 adolescents with a history of DMDD were selected as the sample and randomly assigned to two groups of experimental (n=15) and control (n=15). Thus, the inclusion criteria were female adolescents aged 13 to 16 years and at least one experience of DMDD. Before group training, members of both groups were assessed during the pre-test. Emotion regulation group training was applied to the experimental group, while the control group did not receive any training (Figure 1). Then, the participants in both groups were evaluated in the post-test to measure the effect of the independent variable (training) on the dependent variables (irritability, alexithymia, and interpersonal problems). This method is usually done when it is impossible to control all relevant variables in the research; therefore, relative control is possible by accurately identifying the factors that affect the external and internal validity. To apply maximum control, the groups were selected from a homogeneous community, and the subjects were randomly assigned to the experimental and control groups. The inclusion criteria were being female, having DMDD, and having 13 to 16 years of age. The exclusion criteria were having any psychological disorder, simultaneous participation in other training and counseling courses, and having more than 3 absent sessions during the training. Then, the pre-tests were received from all three groups, and the intervention group received self-regulation training over 2 months through eight 90-min based on the Gross protocol [22]. The summary of the sessions is reported in Table 1.

The control group received no treatment. A clinical psychologist performed eight sessions of intervention in a group twice weekly in one of the counseling and psychological service centers and clinics of the fifth district in Tehran City, Iran. The researcher reaffirms the participants’ understanding of their right to withdraw from the study for any reason. In addition, signed informed consent forms were obtained from the participants. Research objectives, procedures, benefits, voluntary participation, and confidentiality were explained to the participants. A post-test was received from all three groups, and the data were analyzed using the SPSS software, version 25, along with the multivariate analysis of covariance (MANCOVA). This research tested the linearity of the relationship between each dependent variable and its covariate. The linear significance level of the relationship between pre-test and post-test irritability, alexithymia, and interpersonal problems was obtained at r=0.82, r=0.80, and r=0.80, respectively (P<0.05). According to the received data, the assumption of linearity was established. The results of the homogeneity variance assumption according to the Levene test were insignificant in the variable of irritability (F(1, 28)=0.81, P=0.24), alexithymia (F(1, 28)=0.81, P=0.24), and interpersonal problems (F(1, 28)=0.26, P=0.65), respectively. Accordingly, the assumption of homogeneity of variances was confirmed (P>0.05). In addition, the significance level of the Kolmogorov-Smirnov test was more significant than 0.05; therefore, the assumption of normal distribution of the variables was established.
The Barratt impulsiveness scale (BIS-11)
BIS-11 has 30 items in self-report format on a 5-point scale (never, rarely, sometimes, often, and always). These items are scored to result in 6 first-order factors (attention, motor, self-control, cognitive complexity, perseverance, and cognitive instability impulsiveness) and three second-order factors (attentional, motor, and non-planning impulsiveness). Then, 11 out of 30 items on this scale are reversed (the highest and the lowest). The score of the non-psychiatric control group is usually between 50 and 60 [21]. This scale measures three factors of impulsivity: 2 cognitive/attentional impulsivities (quick cognitive decisions), 3 motor impulsivity (acting without thinking), and 4 impulsivities (a lack of foresight or sudden direction finding). In Iran, the validity and reliability of the mentioned research were 0.75 and 83.0, respectively, which shows that the validity and reliability of the Persian translation are desirable [22]. The Cronbach α in this study was 0.58.
Toronto alexithymia scale (TAS-20)
TAS-20 was developed in 1985 by Bagby et al. [23]. This scale is a self-report measure of deficiency in understanding, processing, or describing emotions. The current version comprises 20 items rated on a 5-point Likert scale (1=strongly disagree and 5=strongly agree). TAS-20 measures the following three factors: Factor I, difficulty in identifying feelings (1, 3, 6, 7, 9, 13, 14); factor II, difficulty in describing feelings (2, 4, 11, 12, 17); factor III, externally-oriented thinking (5, 8, 10, 15, 16, 18, 19, 20). Five items are scored inversely (4, 5, 10, 18, and 19). The total score can range from 0 to 100 (higher scores indicate more significant impairment/challenges). The total alexithymia score is the sum of responses to all 20 items, while the score for each subscale factor is the sum of the responses to that subscale. The TAS-20 uses the following cut-offs: Scores equal to or <51 indicate non-alexithymia, scores of 52 to 60 indicate possible alexithymia, and scores >61 suggest alexithymia. Iranian studies supported the three-factor structure, internal consistency, test re-test reliability, and predictive validity of the Persian TAS-20 in both clinical and non-clinical samples [24]. In this study, the Cronbach α was 0.78.
The inventory of interpersonal problems-short version (IIP-32)
IIP-32 was developed by Barkham et al. and is scored according to a 5-point Likert scale, ranging from 0 (not at all) to 5 (strongly) [25]. This scale is a self-report inventory, and its questions concern the problems people usually experience in interpersonal relations. High scores on IIP-32 are indicators of poorer interpersonal functioning [25]. The 8 factors are assertiveness and sociability, openness, caring, aggression, supportiveness and involvement, and dependency. The IIP-32 subscales’ internal consistency was calculated using the Cronbach α coefficient, ranging from 0.60 to 0.83. For the total consistency, a score of 0.81 and 0.86 was obtained [23]. The reliability of the Persian version of IIP-32 was calculated using internal consistency and half-split coefficients, namely 0.82 and 0.83, respectively [26]. According to the current research, the Cronbach α was 0.73.
3. Results
The analysis of adolescents showed that the mean age in the two groups was 15.11+2.33 years. Also, the chi-square test results showed no significant differences between groups regarding age and education grade (P>0.05) (Table 2).

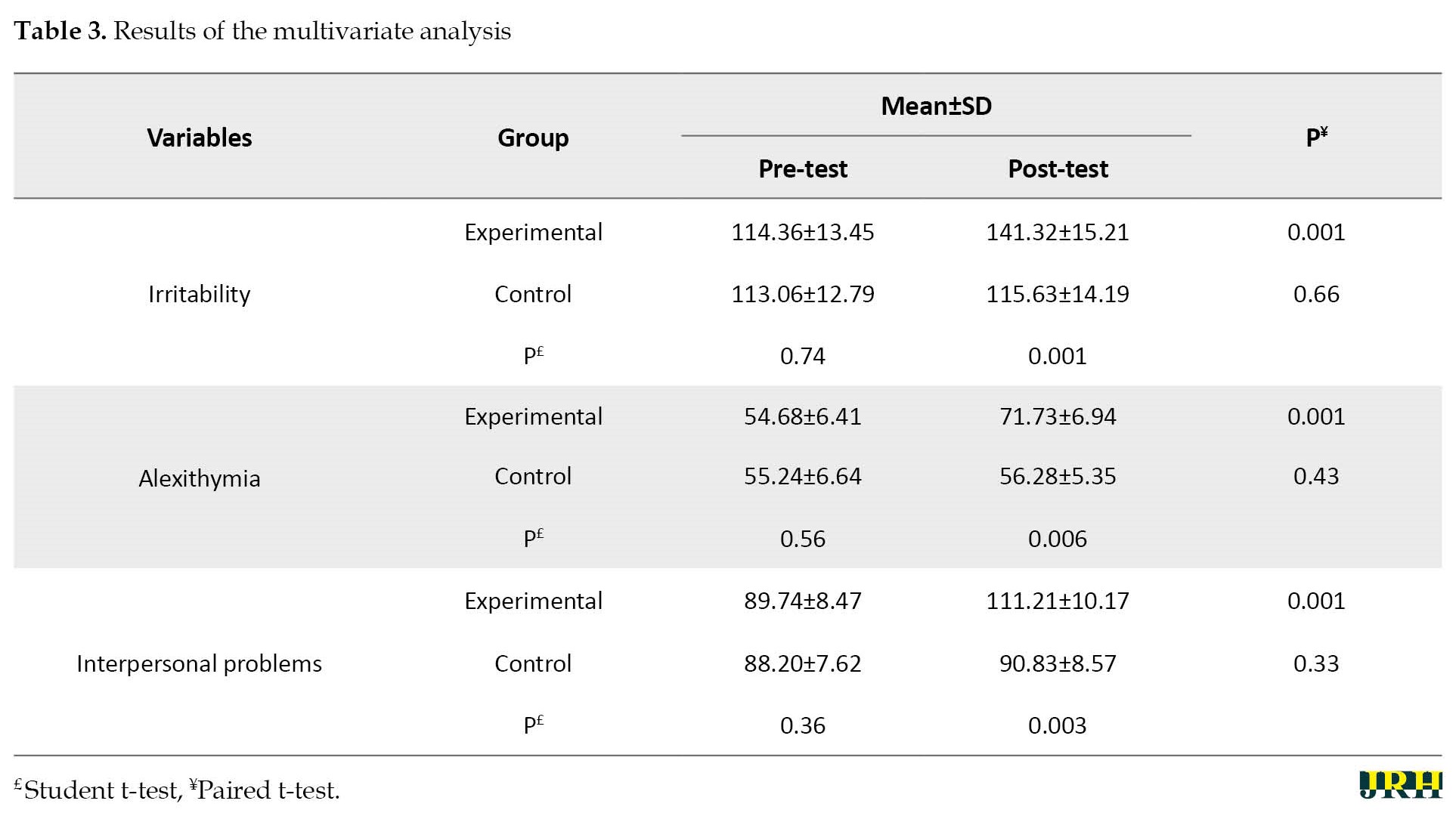
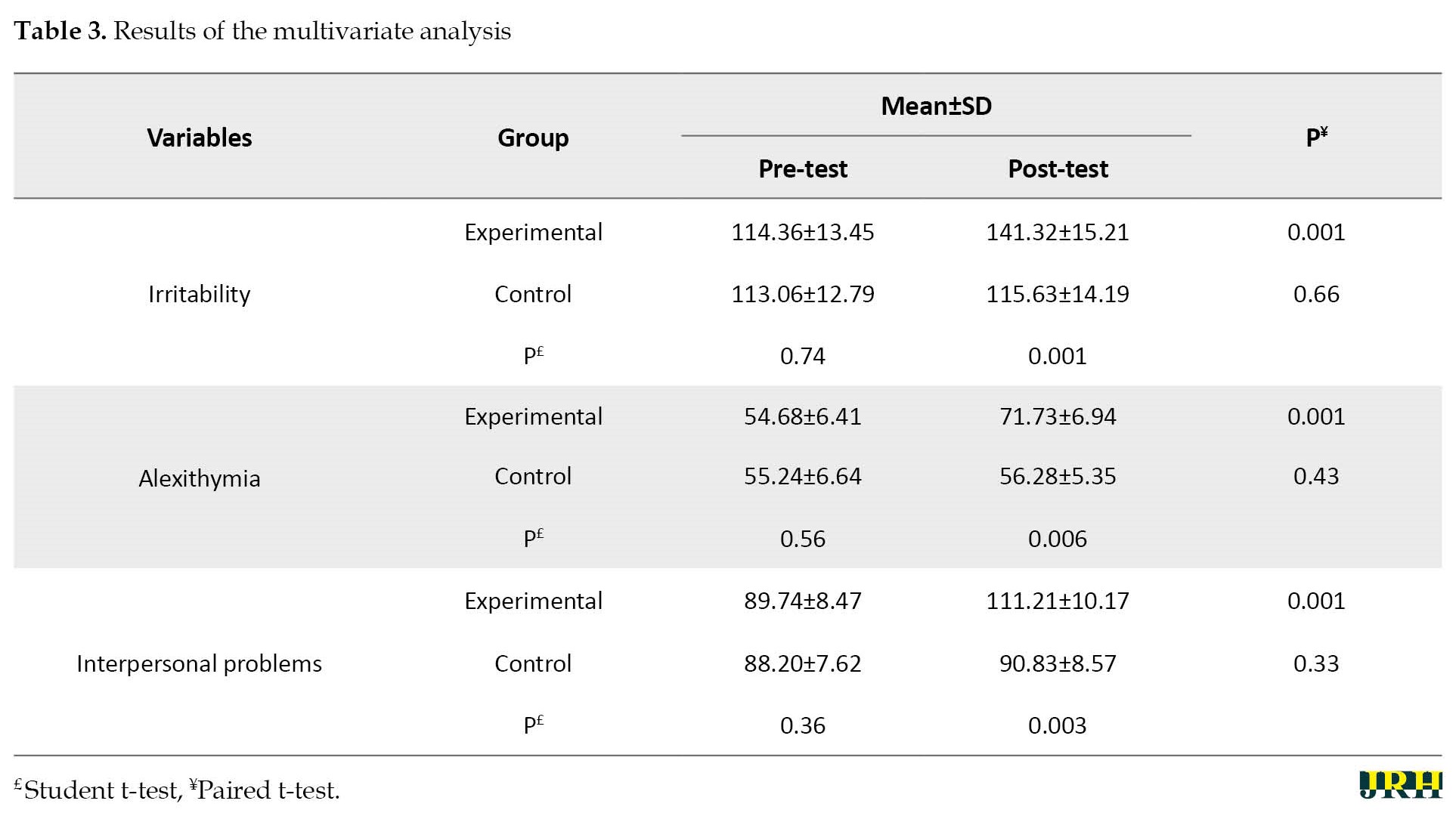
Table 3 shows that the Mean+SD of irritability, alexithymia, and interpersonal problems modified significantly compared to their post-test scores.
After evaluating the MANCOVA data, the test results showed a significant difference between variables in experimental and control groups (lambda=0.432, F=68.34, P<0.01). According to MANCOVA, two covariance analyses were conducted to determine this difference. In the experimental and control groups, 61% of the variances were explained by the independent variable based on the calculated effect size.
As indicated by the univariate results in Table 4, there is a significant difference between the groups in terms of irritability (F=26.45, P=0.001, η=0.695), alexithymia (F=38.91, P=0.001, η=0.781), and interpersonal problems (F=31.27, P=0.001, η=0.734).

Moreover, according to the alexithymia’s largest effect size (η=0.781), emotion regulation training had more effect on alexithymia.
4. Discussion
This article emphasizes self-regulation training techniques for adolescents with DMDD irritability, alexithymia, and interpersonal problems. The intervention significantly alleviated irritability, alexithymia, and interpersonal problems among adolescent girls with a disruptive mood disorder. This result is consistent with the previous studies on the effectiveness of group emotional regulation therapy [5, 17-20].
Vafaei et al. showed that emotion-regulation group training reduced self-injury behavior and the rate of depression and anger in adolescents [19]. As a result, Sheybani et al. demonstrated that cognitive-behavioral therapy and emotion regulation did not significantly differ in reducing anxiety, stress, and excitability in people with DMDD; however, both affected positive and negative emotions equally. There was a more significant reduction in depression symptoms with emotional regulation [20]. A study of adolescent girls with DMDD showed that this intervention could effectively improve emotional processing. Regulating emotions requires emotional awareness, acceptance, and control of impulsive behavior. The authors found the tendency to act impulsively in people who lack an understanding of their feelings and cannot control their violent tendencies with conscious effort. As a result, poor communication often occurs. This study showed that adolescent girls with DMDD are more attentive to their feelings and how to identify emotions in others [27, 28].
Hsu et al. results indicated a significant trend toward reducing impulsivity, anger with resentment, physical aggression, suspicion, and hostility. The intervention significantly alleviated the intensity of cognitive failure, improved the management of alexithymia features and attribution styles and errors, and fostered adequate decision-making styles and emotion regulation capacity [18]. This intervention provided patients with a more active role in managing their violent behavior with the involvement of alexithymia. Improvements in specific social cognitive functions, such as alexithymia features, attributional style, decision-making style, and preferences, can also be related to reductions in violent actions [18]. Similarly, alexithymia is associated with aggressive behavior because of emotional avoidance and emotional inexpressiveness [10-12], which is negatively correlated with the ability to cope with stress [8]. Although alexithymia is not a personality disorder, alexithymia may be associated with personality dysfunction [9].
The skills taught to the subjects during the program (especially emotion regulation skills) can reduce self-injury behavior in individuals. Accordingly, at the end of the sessions, individuals become more successful in regulating emotions by acquiring emotional regulation skills, including emotion recognition, perception, vulnerability, and suffering. Consequently, their dysfunctional behaviors are reduced. Emotional-regulation training by informing people about positive emotions, their acceptance, and timely expression is essential in reducing physical and mental symptoms and improving social functioning and levels of mental health. Thus, emotion regulation involves numerous regulatory processes and strategies, including cognitive, physical, social, and behavioral dimensions. Emotion-regulation strategies are used to increase adjustment and adaptation to manage emotions and are part of adaptation strategies related to the experience and treatment of emotional and physical disorders. Therefore, emotional regulation reduces negative emotions, such as depression, and increases positive emotions and adaptive behavior [19]. Irritable people perceive even the smallest provocation as a mistake and are more likely to become angry. As a result, maladaptive patients with destructive moods can avoid blaming themselves, blaming others, and having mental negativity through emotional regulation. Furthermore, emotional regulation significantly affects emotionally vulnerable people to allow themselves to be in their current time and place. As a result, they are more objective about the extent to which the situation is getting threatened instead of reacting with anger and confusion [20].
In generalizing the findings of this study to people in other cities and regions, caution should be observed due to some limitations of this study. For instance, the sample size of people for each group was small. Since the control group did not receive any intervention, the placebo effect of training is not apparent. The design does not have a follow-up stage, and considering the educational intervention, the impact continuity is unclear, which is one limitation of this study. To better understand how effective emotion regulation training is according to the Iranian cultural context, future research should be conducted by comparing it with other new therapeutic approaches, including third-wave therapies. Doing a test after the treatment period is suggested to see if it worked for a long time and to ensure everything is stable. One of the most important questions that may be applicable and useful in the way of science is doing the same variables on the parents of these children and using the same approach and variables in adolescents with self-harm and comparing it with children with DMDD. It is also suggested that the lack of purposefulness and executive functions such as metacognition and cognitive flexibility in these people should be investigated in future studies and compared with a healthy group.
5. Conclusion
Based on the present research results, emotion regulation training effectively reduces irritability, alexithymia, and DMDD in children and adolescents. It also causes a significant increase in interpersonal problems; therefore, this is considered an effective and practical method. It can be implemented effectively in clinics and psychological treatment centers. Also, as a result of using emotion regulation training, it is possible to improve these people’s psychological characteristics and social relations. It is also suggested that relevant organizations train specialists and school counselors this way.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by Tehran Mediacal Sciences, Islamic Azad University (Code: IR.AUMS.REC.1400.210).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and supervision: Masoumeh Falah Neudehi and Farnaz Rezaei; Methodology: Ameneh Bozorgi Kazerooni and Zahra Ebadi; Data collection: Farnaz Rezaei; Investigation, data analysis, writing original draft, review and editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors wish to thank the cooperation of students.
References
Chronic, severe irritability is a common problem in children and adolescents [1]. Reflecting this pressing public health need, such a diagnostic and statistical manual of mental disorders, 5th edition (DSM-5) as disruptive mood dysregulation disorder (DMDD) [1, 2]. The prevalence estimates for severe irritability in school-age children and adolescents range from 0.12% to 5%, with 3% being the most common estimate for DMDD [1]. Irritable people are likely to suffer from poor functional outcomes throughout their lives, including concurrent and longitudinal emotional disorders, suicidality, poor school performance, and difficulties in their social and professional lives. Children with high irritability also have distinct physiological profiles, including hyper-reactivity to stress and perception of threats. The central diagnostic feature of DMDD is chronic and severe irritability, leading to functional impairment. DMDD has been operationalized for research as severe irritability related to hyper-arousal symptoms (agitation and distractibility) [3]. As relevant to emotion regulation, the pathophysiology of severe irritability has been associated with reduced context-dependent regulation, dysregulated attention-emotion interactions, and the misinterpretation of social cues, such as a preferential threat bias [4]. It is common for adolescents to develop behavioral problems because of emotional dysregulation during adolescence. Dysregulation of emotion refers to the inability to control one’s affective expression in different circumstances. As a result, it has little flexibility and spontaneity, a lack of control, and demonstration of disruptive behaviors [5]. Alexithymia and low emotion differentiation restrict access to emotional information and increase the propensity toward dysregulated and deviant behaviors, such as impulsive aggression [6].
In the study by Edwards & Wupperman (2017), alexithymic features and emotion differentiation explained nearly 43% of the variance in impulsive aggression. These relationships were fully mediated by emotion-regulation difficulty [6]. Moreover, the difficulty identifying feelings subscale of the Toronto alexithymia scale (TAS-20) was positively associated with alcohol problems through emotional dysregulation and psychological distress [7]. Inflexible emotion regulation increases allostatic load from frequent stress, inadequate reactivity, failed shutdown, and habituation. They may result in physical and mental illness. Alexithymia exemplifies inflexible emotion regulation with dysfunctions potentially across all stages of emotion processing, both psychologically and physiologically [8]. The findings suggested that the interpersonal style of alexithymic individuals is characterized by cold and socially avoidant behavior, corresponding to the predominantly insecure attachment pattern found in alexithymia [9].
A previous study showed that the TAS-20 scores correlate with numerous psychiatric concerns, mainly in the internalizing spectrum, thought difficulties, and self-reported aggression [10]. Furthermore, results revealed institutionalized girls to be more alexithymic, showing more difficulty identifying and describing feelings than boys, similar to community groups. Higher alexithymia was related to more total, internalizing, and externalizing problems through similar mechanisms of risk in community groups [11]. Concerning mood regulation, Besharat and Shahidi showed adolescent addicts with statistically significant differences compared to the control group. They showed lower attention to their feelings and lower repair of mood. Patients had low clarity of feelings and low mood repair significantly related to the first substance abuse (cannabinoids), and a significant relation between low attention to feelings and the cause of drug abuse was peer pressure and novelty-seeking [12]. Interpersonal difficulties are experienced with others and cause mental distress or are associated with mental disturbances. They include difficulties in assertiveness, sociability, submissiveness, intimacy, responsibility, and control. People with alexithymia cannot correctly identify emotions from other individuals’ faces. They cannot always show sympathy toward other individuals [13]. Analysis shows a direct relationship between alexithymia and social, familial, and romantic loneliness. Moreover, interpersonal distrust partly mediates this relationship, and alexithymia and interpersonal distrust interact to predict social and family loneliness. These findings suggest that links between the facets of alexithymia, interpersonal distrust, and loneliness are complex and multifaceted and discussed concerning interventions for young adolescents [14].
Considering therapeutic techniques currently available to clinicians may help target pathophysiological processes in severe mood dysregulation, and DMDD is useful. Comprehensive treatments for these patients will likely integrate well-conceptualized tools from extant interventions with novel advances tailored to the mechanisms of chronic irritability. Currently, DMDD is a severe and impairing psychiatric disorder without any validated psychotherapeutic or psycho-pharmacological interventions [4]. Currently, no gold standard, evidence-based treatments exist exclusively for DMDD or severe mood dysregulation; however, interventions designed for related clinical disorders have demonstrated promising findings, including parent management training, cognitive-behavioral therapy, and psychopharmacological interventions [4]. Non-pharmacological therapies throughout the treatment course included cognitive behavioral therapy, dialectical behavior therapy, 12-step facilitation, contingency management, family systems therapy, motivational enhancement therapy, psychodynamic psychotherapy, and motivational interviewing [15]. Since DMDD has recently been added as an efficacious treatment that specifically targets severe irritability, its presence in DMDD is still being developed [16]. The therapeutic emotion regulation process for children diagnosed with DMDD is a primary target, aiming to promote the child’s emotional development [17]. From a clinical perspective, emotion regulation is of utmost importance in interventions for childhood emotional and behavioral disorders, which are often aimed at promoting child self-regulation, approved in numerous studies [4, 17-21]. This study aims to implement self-regulation training techniques for adolescents with a disruptive mood disorder, emphasizing irritability, alexithymia, and interpersonal problems in adolescents with DMDD.
2. Methods
To evaluate the effectiveness of group training, we used the quasi-experimental method with a pre-test/post-test design and a control group. The study population comprised all 13 to 16 year-old girls in Tehran City, Iran, from 2022 to 2023 who had DMDD. A total of 30 girls were selected based on the multi-stage cluster random sampling method. The adequacy of the sample size was confirmed by the G*Power software, version 3.1.9.7 (α=0.05 and test power=0.80). Four junior high schools were randomly selected from the education districts of Tehran. Next, 6 classes from each school (seventh, eighth, and ninth grade) were chosen. Based on the questionnaire, 30 adolescents with a history of DMDD were selected as the sample and randomly assigned to two groups of experimental (n=15) and control (n=15). Thus, the inclusion criteria were female adolescents aged 13 to 16 years and at least one experience of DMDD. Before group training, members of both groups were assessed during the pre-test. Emotion regulation group training was applied to the experimental group, while the control group did not receive any training (Figure 1). Then, the participants in both groups were evaluated in the post-test to measure the effect of the independent variable (training) on the dependent variables (irritability, alexithymia, and interpersonal problems). This method is usually done when it is impossible to control all relevant variables in the research; therefore, relative control is possible by accurately identifying the factors that affect the external and internal validity. To apply maximum control, the groups were selected from a homogeneous community, and the subjects were randomly assigned to the experimental and control groups. The inclusion criteria were being female, having DMDD, and having 13 to 16 years of age. The exclusion criteria were having any psychological disorder, simultaneous participation in other training and counseling courses, and having more than 3 absent sessions during the training. Then, the pre-tests were received from all three groups, and the intervention group received self-regulation training over 2 months through eight 90-min based on the Gross protocol [22]. The summary of the sessions is reported in Table 1.

The control group received no treatment. A clinical psychologist performed eight sessions of intervention in a group twice weekly in one of the counseling and psychological service centers and clinics of the fifth district in Tehran City, Iran. The researcher reaffirms the participants’ understanding of their right to withdraw from the study for any reason. In addition, signed informed consent forms were obtained from the participants. Research objectives, procedures, benefits, voluntary participation, and confidentiality were explained to the participants. A post-test was received from all three groups, and the data were analyzed using the SPSS software, version 25, along with the multivariate analysis of covariance (MANCOVA). This research tested the linearity of the relationship between each dependent variable and its covariate. The linear significance level of the relationship between pre-test and post-test irritability, alexithymia, and interpersonal problems was obtained at r=0.82, r=0.80, and r=0.80, respectively (P<0.05). According to the received data, the assumption of linearity was established. The results of the homogeneity variance assumption according to the Levene test were insignificant in the variable of irritability (F(1, 28)=0.81, P=0.24), alexithymia (F(1, 28)=0.81, P=0.24), and interpersonal problems (F(1, 28)=0.26, P=0.65), respectively. Accordingly, the assumption of homogeneity of variances was confirmed (P>0.05). In addition, the significance level of the Kolmogorov-Smirnov test was more significant than 0.05; therefore, the assumption of normal distribution of the variables was established.
The Barratt impulsiveness scale (BIS-11)
BIS-11 has 30 items in self-report format on a 5-point scale (never, rarely, sometimes, often, and always). These items are scored to result in 6 first-order factors (attention, motor, self-control, cognitive complexity, perseverance, and cognitive instability impulsiveness) and three second-order factors (attentional, motor, and non-planning impulsiveness). Then, 11 out of 30 items on this scale are reversed (the highest and the lowest). The score of the non-psychiatric control group is usually between 50 and 60 [21]. This scale measures three factors of impulsivity: 2 cognitive/attentional impulsivities (quick cognitive decisions), 3 motor impulsivity (acting without thinking), and 4 impulsivities (a lack of foresight or sudden direction finding). In Iran, the validity and reliability of the mentioned research were 0.75 and 83.0, respectively, which shows that the validity and reliability of the Persian translation are desirable [22]. The Cronbach α in this study was 0.58.
Toronto alexithymia scale (TAS-20)
TAS-20 was developed in 1985 by Bagby et al. [23]. This scale is a self-report measure of deficiency in understanding, processing, or describing emotions. The current version comprises 20 items rated on a 5-point Likert scale (1=strongly disagree and 5=strongly agree). TAS-20 measures the following three factors: Factor I, difficulty in identifying feelings (1, 3, 6, 7, 9, 13, 14); factor II, difficulty in describing feelings (2, 4, 11, 12, 17); factor III, externally-oriented thinking (5, 8, 10, 15, 16, 18, 19, 20). Five items are scored inversely (4, 5, 10, 18, and 19). The total score can range from 0 to 100 (higher scores indicate more significant impairment/challenges). The total alexithymia score is the sum of responses to all 20 items, while the score for each subscale factor is the sum of the responses to that subscale. The TAS-20 uses the following cut-offs: Scores equal to or <51 indicate non-alexithymia, scores of 52 to 60 indicate possible alexithymia, and scores >61 suggest alexithymia. Iranian studies supported the three-factor structure, internal consistency, test re-test reliability, and predictive validity of the Persian TAS-20 in both clinical and non-clinical samples [24]. In this study, the Cronbach α was 0.78.
The inventory of interpersonal problems-short version (IIP-32)
IIP-32 was developed by Barkham et al. and is scored according to a 5-point Likert scale, ranging from 0 (not at all) to 5 (strongly) [25]. This scale is a self-report inventory, and its questions concern the problems people usually experience in interpersonal relations. High scores on IIP-32 are indicators of poorer interpersonal functioning [25]. The 8 factors are assertiveness and sociability, openness, caring, aggression, supportiveness and involvement, and dependency. The IIP-32 subscales’ internal consistency was calculated using the Cronbach α coefficient, ranging from 0.60 to 0.83. For the total consistency, a score of 0.81 and 0.86 was obtained [23]. The reliability of the Persian version of IIP-32 was calculated using internal consistency and half-split coefficients, namely 0.82 and 0.83, respectively [26]. According to the current research, the Cronbach α was 0.73.
3. Results
The analysis of adolescents showed that the mean age in the two groups was 15.11+2.33 years. Also, the chi-square test results showed no significant differences between groups regarding age and education grade (P>0.05) (Table 2).

Table 3 shows that the Mean+SD of irritability, alexithymia, and interpersonal problems modified significantly compared to their post-test scores.
After evaluating the MANCOVA data, the test results showed a significant difference between variables in experimental and control groups (lambda=0.432, F=68.34, P<0.01). According to MANCOVA, two covariance analyses were conducted to determine this difference. In the experimental and control groups, 61% of the variances were explained by the independent variable based on the calculated effect size.
As indicated by the univariate results in Table 4, there is a significant difference between the groups in terms of irritability (F=26.45, P=0.001, η=0.695), alexithymia (F=38.91, P=0.001, η=0.781), and interpersonal problems (F=31.27, P=0.001, η=0.734).

Moreover, according to the alexithymia’s largest effect size (η=0.781), emotion regulation training had more effect on alexithymia.
4. Discussion
This article emphasizes self-regulation training techniques for adolescents with DMDD irritability, alexithymia, and interpersonal problems. The intervention significantly alleviated irritability, alexithymia, and interpersonal problems among adolescent girls with a disruptive mood disorder. This result is consistent with the previous studies on the effectiveness of group emotional regulation therapy [5, 17-20].
Vafaei et al. showed that emotion-regulation group training reduced self-injury behavior and the rate of depression and anger in adolescents [19]. As a result, Sheybani et al. demonstrated that cognitive-behavioral therapy and emotion regulation did not significantly differ in reducing anxiety, stress, and excitability in people with DMDD; however, both affected positive and negative emotions equally. There was a more significant reduction in depression symptoms with emotional regulation [20]. A study of adolescent girls with DMDD showed that this intervention could effectively improve emotional processing. Regulating emotions requires emotional awareness, acceptance, and control of impulsive behavior. The authors found the tendency to act impulsively in people who lack an understanding of their feelings and cannot control their violent tendencies with conscious effort. As a result, poor communication often occurs. This study showed that adolescent girls with DMDD are more attentive to their feelings and how to identify emotions in others [27, 28].
Hsu et al. results indicated a significant trend toward reducing impulsivity, anger with resentment, physical aggression, suspicion, and hostility. The intervention significantly alleviated the intensity of cognitive failure, improved the management of alexithymia features and attribution styles and errors, and fostered adequate decision-making styles and emotion regulation capacity [18]. This intervention provided patients with a more active role in managing their violent behavior with the involvement of alexithymia. Improvements in specific social cognitive functions, such as alexithymia features, attributional style, decision-making style, and preferences, can also be related to reductions in violent actions [18]. Similarly, alexithymia is associated with aggressive behavior because of emotional avoidance and emotional inexpressiveness [10-12], which is negatively correlated with the ability to cope with stress [8]. Although alexithymia is not a personality disorder, alexithymia may be associated with personality dysfunction [9].
The skills taught to the subjects during the program (especially emotion regulation skills) can reduce self-injury behavior in individuals. Accordingly, at the end of the sessions, individuals become more successful in regulating emotions by acquiring emotional regulation skills, including emotion recognition, perception, vulnerability, and suffering. Consequently, their dysfunctional behaviors are reduced. Emotional-regulation training by informing people about positive emotions, their acceptance, and timely expression is essential in reducing physical and mental symptoms and improving social functioning and levels of mental health. Thus, emotion regulation involves numerous regulatory processes and strategies, including cognitive, physical, social, and behavioral dimensions. Emotion-regulation strategies are used to increase adjustment and adaptation to manage emotions and are part of adaptation strategies related to the experience and treatment of emotional and physical disorders. Therefore, emotional regulation reduces negative emotions, such as depression, and increases positive emotions and adaptive behavior [19]. Irritable people perceive even the smallest provocation as a mistake and are more likely to become angry. As a result, maladaptive patients with destructive moods can avoid blaming themselves, blaming others, and having mental negativity through emotional regulation. Furthermore, emotional regulation significantly affects emotionally vulnerable people to allow themselves to be in their current time and place. As a result, they are more objective about the extent to which the situation is getting threatened instead of reacting with anger and confusion [20].
In generalizing the findings of this study to people in other cities and regions, caution should be observed due to some limitations of this study. For instance, the sample size of people for each group was small. Since the control group did not receive any intervention, the placebo effect of training is not apparent. The design does not have a follow-up stage, and considering the educational intervention, the impact continuity is unclear, which is one limitation of this study. To better understand how effective emotion regulation training is according to the Iranian cultural context, future research should be conducted by comparing it with other new therapeutic approaches, including third-wave therapies. Doing a test after the treatment period is suggested to see if it worked for a long time and to ensure everything is stable. One of the most important questions that may be applicable and useful in the way of science is doing the same variables on the parents of these children and using the same approach and variables in adolescents with self-harm and comparing it with children with DMDD. It is also suggested that the lack of purposefulness and executive functions such as metacognition and cognitive flexibility in these people should be investigated in future studies and compared with a healthy group.
5. Conclusion
Based on the present research results, emotion regulation training effectively reduces irritability, alexithymia, and DMDD in children and adolescents. It also causes a significant increase in interpersonal problems; therefore, this is considered an effective and practical method. It can be implemented effectively in clinics and psychological treatment centers. Also, as a result of using emotion regulation training, it is possible to improve these people’s psychological characteristics and social relations. It is also suggested that relevant organizations train specialists and school counselors this way.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by Tehran Mediacal Sciences, Islamic Azad University (Code: IR.AUMS.REC.1400.210).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and supervision: Masoumeh Falah Neudehi and Farnaz Rezaei; Methodology: Ameneh Bozorgi Kazerooni and Zahra Ebadi; Data collection: Farnaz Rezaei; Investigation, data analysis, writing original draft, review and editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors wish to thank the cooperation of students.
References
- Tamanaeifar S, Pirkashani NG, Nooripour R. How Mindfulness and Acceptance Could Help Psychiatrists Predict Alexithymia Among Students. The Journal of Nervous and Mental Disease. 2021; 209(4):297-301. [DOI:10.1097/NMD.0000000000001295] [PMID]
- Linke J, Kircanski K, Brooks J, Perhamus G, Gold AL, Brotman MA. Exposure-based cognitive-behavioral therapy for disruptive mood dysregulation disorder: An evidence-based case study. Behavior Therapy. 2020; 51(2):320-33.[DOI:10.1016/j.beth.2019.05.007] [PMID] [PMCID]
- Fongaro E, Picot MC, Stringaris A, Belloc C, Verissimo AS, Franc N, et al. Parent training for the treatment of irritability in children and adolescents: A multisite randomized controlled, 3-parallel-group, evaluator-blinded, superiority trial. BMC Psychology. 2022; 10(1):273. [DOI:10.1186/s40359-022-00984-5] [PMID] [PMCID]
- Kircanski K, Leibenluft E, Brotman MA. Emotion regulation in severe irritability and disruptive mood dysregulation disorder. In: Essau CA, LeBlanc SS, Ollendick TH, editors. Emotion regulation in severe irritability and disruptive mood dysregulation disorder. Oxford: Oxford Academic; 2017. [DOI:10.1093/med:psych/9780198765844.003.0014]
- Paulus FW, Ohmann S, Möhler E, Plener P, Popow C. Emotional dysregulation in children and adolescents with psychiatric disorders. A Narrative Review. Frontiers in Psychiatry. 2021; 12:628252. [DOI:10.3389/fpsyt.2021.628252] [PMID] [PMCID]
- Edwards ER, Wupperman P. Emotion regulation mediates effects of alexithymia and emotion differentiation on impulsive aggressive behavior. Deviant Behavior. 2017; 38(10):1160-71. [DOI:10.1080/01639625.2016.1241066]
- Linn BK, Zhao J, Bradizza CM, Lucke JF, Ruszczyk MU, Stasiewicz PR. Alexithymia disrupts emotion regulation processes and is associated with greater negative affect and alcohol problems. Journal of Clinical Psychology. 2021; 77(12):2915-28. [DOI:10.1002/jclp.23279] [PMID] [PMCID]
- Panayiotou G, Panteli M, Vlemincx E. Adaptive and maladaptive emotion processing and regulation, and the case of alexithymia. Cognition & Emotion. 2021; 35(3):488-499. [DOI:10.1080/02699931.2019.1671322] [PMID]
- Vanheule S, Desmet M, Meganck R, Bogaerts S. Alexithymia and interpersonal problems. Journal of Clinical Psychology. 2007; 63(1):109-17. [DOI:10.1002/jclp.20324] [PMID]
- Manninen M, Therman S, Suvisaari J, Ebeling H, Moilanen I, Huttunen M, et al. Alexithymia is common among adolescents with severe disruptive behavior. The Journal of Nervous and Mental Disease. 2011; 199(7):506-9. [DOI:10.1097/NMD.0b013e3182214281] [PMID]
- Muzi S. A narrative review on alexithymia in adolescents with previous adverse experiences placed for adoption, in foster care, or institutions. Prevalence, gender differences, and relations with internalizing and externalizing symptoms. Mediterranean Journal of Clinical Psychology. 2020; 8(2):1-25. [DOI:10.6092/2282-1619/mjcp-2449]
- Besharat MA, Shahidi V. The moderating role of attachment styles on the relationship between Alexithymia and interpersonal problems in an Iranian population. International Journal of Psychological Studies. 2013; 5(4):60-8. [DOI:10.5539/ijps.v5n4p60]
- El-Rasheed AH, ElAttar KS, Elrassas HH, Mahmoud DA, Mohamed SY. Mood regulation, alexithymia, and personality disorders in adolescent male addicts. Addictive Disorders & Their Treatment. 2017; 16(2):49-58. [DOI:10.1097/ADT.0000000000000098]
- Qualter P, Quinton SJ, Wagner H, Brown S. Loneliness, interpersonal distrust, and alexithymia in university students. Journal of Applied Social Psychology. 2009; 39(6):1461-79. [DOI:10.1111/j.1559-1816.2009.00491.x]
- Wei A, Navarro M, Yeager V, Goubran B, Moran RA. Naltrexone as an adjunctive treatment for adolescents with deliberate self-harm behavior and cannabis use: A case series. Consultant. 2023; 63(2):e1. [DOI:10.25270/con.2022.11.000006]
- Linke J, Kircanski K, Brooks J, Perhamus G, Gold AL, Brotman MA. Exposure-based cognitive-behavioral therapy for disruptive mood dysregulation disorder: An evidence-based case study. Behavior Therapy. 2020; 51(2):320-33.[DOI:10.1016/j.beth.2019.05.007] [PMID] [PMCID]
- Hajal NJ, Paley B. Parental emotion and emotion regulation: A critical target of study for research and intervention to promote child emotion socialization. Dev Psychol. 2020; 56(3):403-17. [DOI:10.1037/dev0000864] [PMID]
- Hsu MC, Ouyang WC. Effects of integrated violence intervention on alexithymia, cognitive, and neurocognitive features of violence in schizophrenia: A randomized controlled trial. Brain Sciences. 2021; 11(7):837. [DOI:10.3390/brainsci11070837] [PMID] [PMCID]
- Vafaei T, Samavi SA, Whisenhunt JL, Najarpourian S. The effectiveness of group training of emotional regulation on adolescent’s self-injury, depression, and anger. Journal of Research & Health. 2021; 11(6):383-92. [DOI:10.32598/JRH.11.6.1602.4]
- Sheybani H, Mikaeili N, Narimani M. [The efficacy of cognitive behavior therapy on emotion regulation and irritability of the students suffered from disruptive mood dysregulation disorder (Persian)]. Journal of School Psychology. 2022; 11(1):56-67. [DOI:10.22098/jsp.2022.1569]
- Barratt ES, Stanford MS, Kent TA, Felthous A. Neuropsychological and cognitive psychophysiological substrates of impulsive aggression. Biological Psychiatry. 1997; 41(10):1045-61. [DOI:10.1016/S0006-3223(96)00175-8] [PMID]
- Ekhtiari H, Safaei H, Esmaeeli Javid G, Atefvahid MK, Edalati H, Mokri A. [Reliability and validity of Persian versions of Eysenck, Barratt, Dickman and Zuckerman Questionnaires in assessing risky and impulsive behaviors (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology. 2008; 14(3):326-36. [Link]
- Bagby RM, Taylor GJ, Ryan D. Toronto alexithymia scale: relationship with personality and psychopathology measures. Psychotherapy and Psychosomatics. 1986; 45(4):207-15.[DOI:10.1159/000287950] [PMID]
- Besharat M. Psychometric characteristics of Persian version of the Toronto alexithymia scale-20 in clinical and non-clinical samples. Iranian Journal of Medical Sciences, 2008; 33(1):1-6. [Link]
- Barkham M, Hardy GE, Startup M. The IIP-32: A short version of the Inventory of Interpersonal Problems. The British Journal of Clinical Psychology. 1996; 35(1):21-35. [DOI:10.1111/j.2044-8260.1996.tb01159.x] [PMID]
- Fath N, Azad Fallah P, Rasool-zadeh Tabatabaei SK, Rahimi C. [Validity and reliability of the inventory of interpersonal problems (IIP-32) (Persian)]. Journal of Clinical Psycology. 2013; 5(3):69 -80. [DOI:10.22075/JCP.2017.2137]
- Garofalo C, Gillespie SM, Velotti P. Emotion regulation mediates relationships between mindfulness facets and aggression dimensions. Aggressive Behavior. 2020; 46(1):60-71. [DOI:10.1002/ab.21868] [PMID] [PMCID]
- Jenkins LN, Demaray MK, Tennant J. Social, emotional, and cognitive factors associated with bullying. School Psychology Review. 2017; 46(1):42-64. [DOI:10.17105/SPR46-1.42-64]
Type of Study: Orginal Article |
Subject:
● Health Education
Received: 2023/01/21 | Accepted: 2023/05/13 | Published: 2023/10/3
Received: 2023/01/21 | Accepted: 2023/05/13 | Published: 2023/10/3
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |










