Volume 14, Issue 1 (Jan & Feb 2024)
J Research Health 2024, 14(1): 7-18 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bazyar J, Karamelahi Z, Daliri S, Chehreh R. COVID-19 and Its Relationship to Breastfeeding Patterns: A Systematic Review Study. J Research Health 2024; 14 (1) :7-18
URL: http://jrh.gmu.ac.ir/article-1-2263-en.html
URL: http://jrh.gmu.ac.ir/article-1-2263-en.html
1- Department of Nursing, Faculty of Nursing and Midwifery, Prehospital Medical Emergency Organization, Ilam University of Medical Sciences, Ilam, Iran.
2- Clinical Research Development Unit (CRDU), 5azar Hospital, Golestan University of Medical Sciences, Gorgan, Iran.
3- Prehospital Medical Emergency Organization, Clinical Research Development Unit, Imam Hossein Hospital, Shahroud University of Medical Sciences, Shahroud, Iran.
4- Department of Midwifery, School of Midwifery and Nursing, Clinical Research Development Unit of Ayatollah Taleghani Hospital, Ilam University of Medical Sciences, Ilam, Iran. ,hashemieh_chehreh@yahoo.com
2- Clinical Research Development Unit (CRDU), 5azar Hospital, Golestan University of Medical Sciences, Gorgan, Iran.
3- Prehospital Medical Emergency Organization, Clinical Research Development Unit, Imam Hossein Hospital, Shahroud University of Medical Sciences, Shahroud, Iran.
4- Department of Midwifery, School of Midwifery and Nursing, Clinical Research Development Unit of Ayatollah Taleghani Hospital, Ilam University of Medical Sciences, Ilam, Iran. ,
Full-Text [PDF 706 kb]
(400 Downloads)
| Abstract (HTML) (1287 Views)
Results
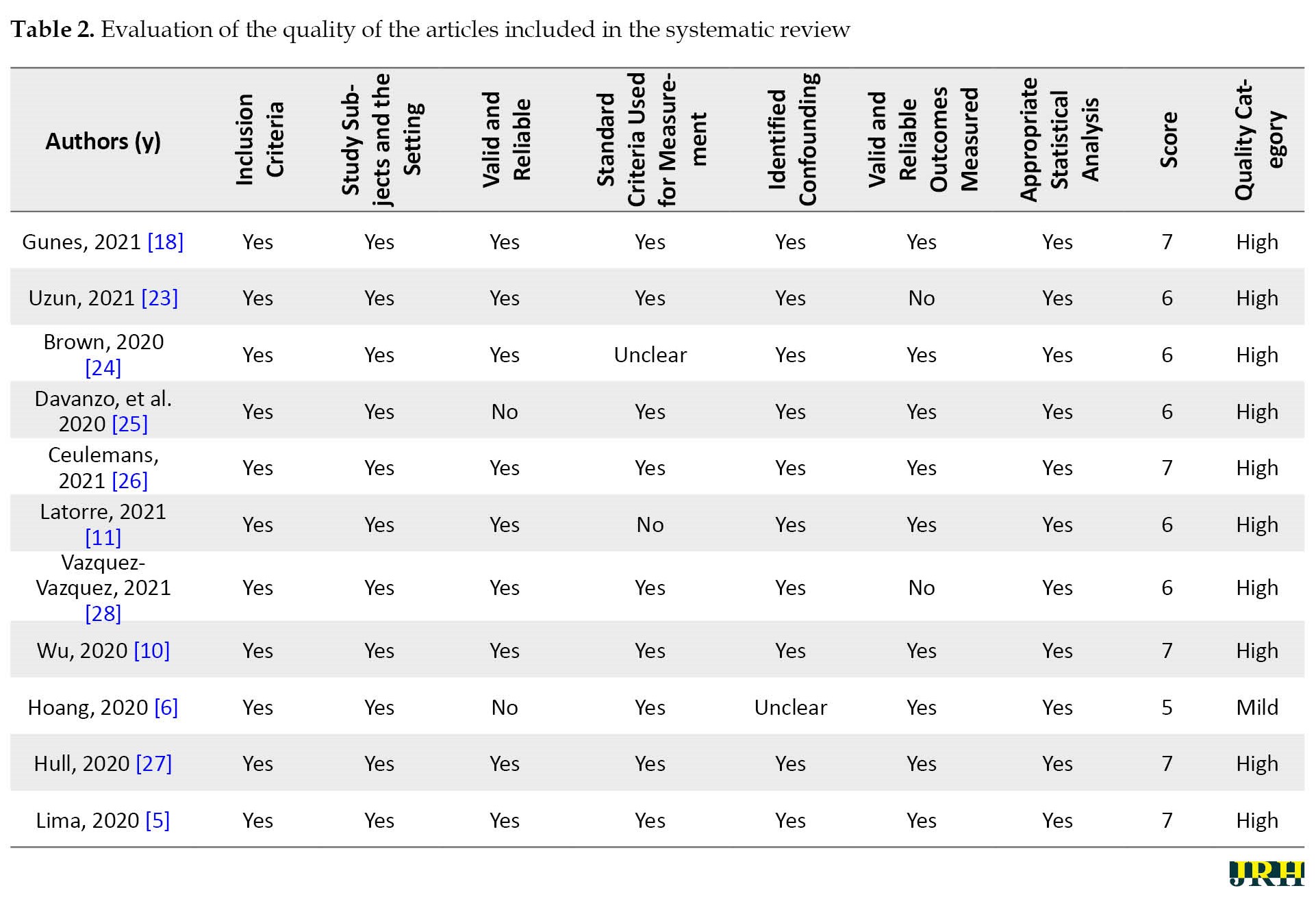
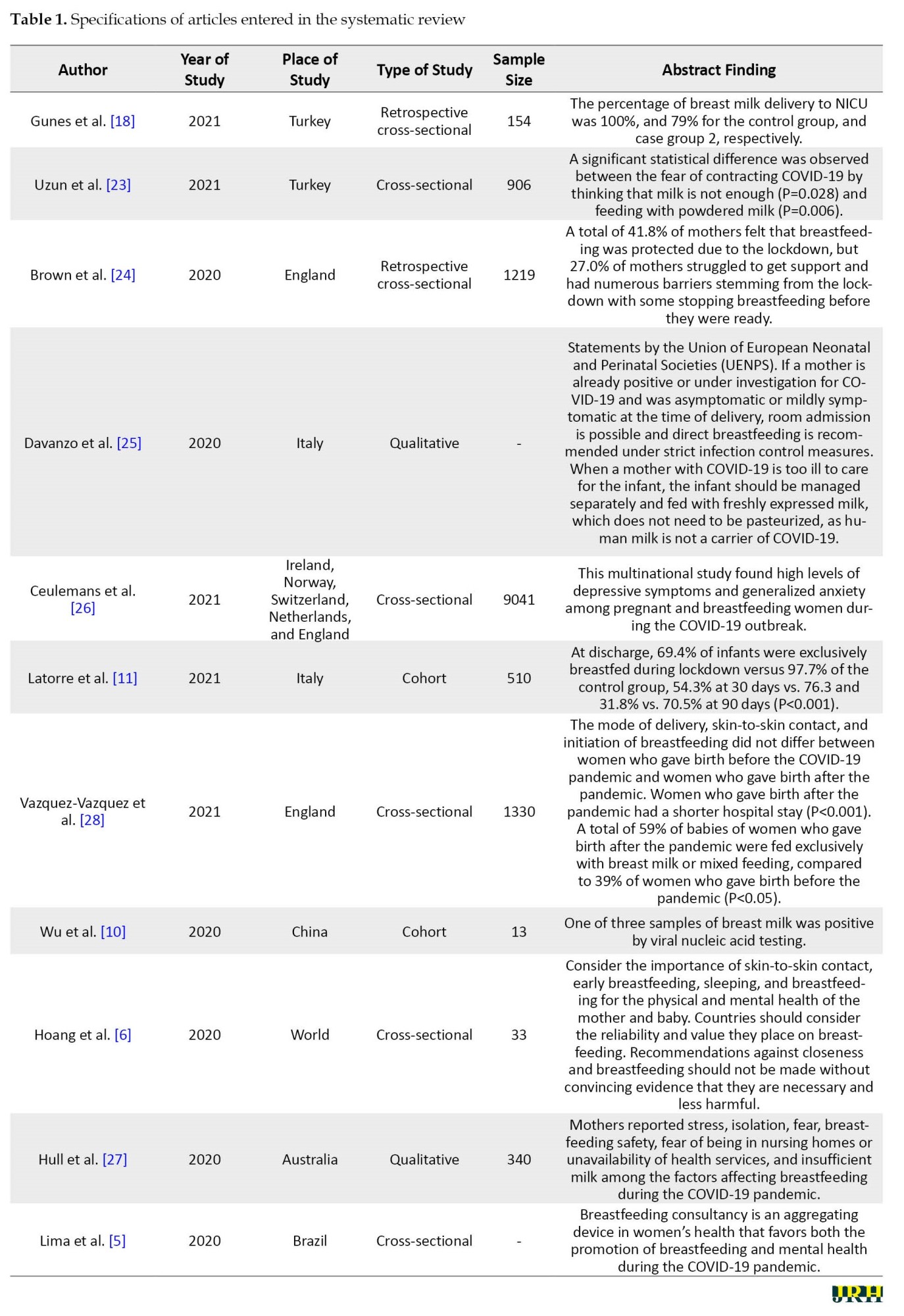
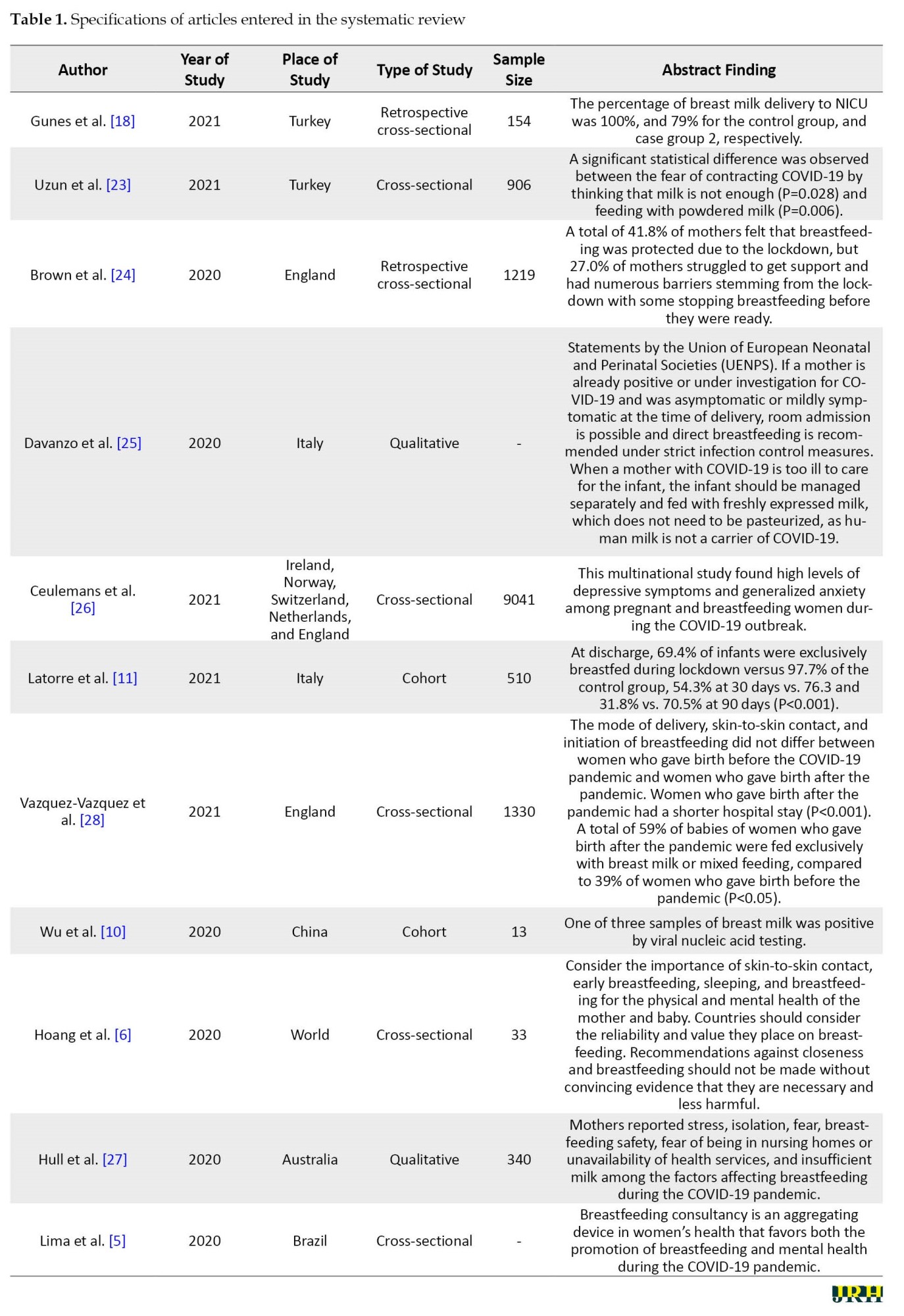
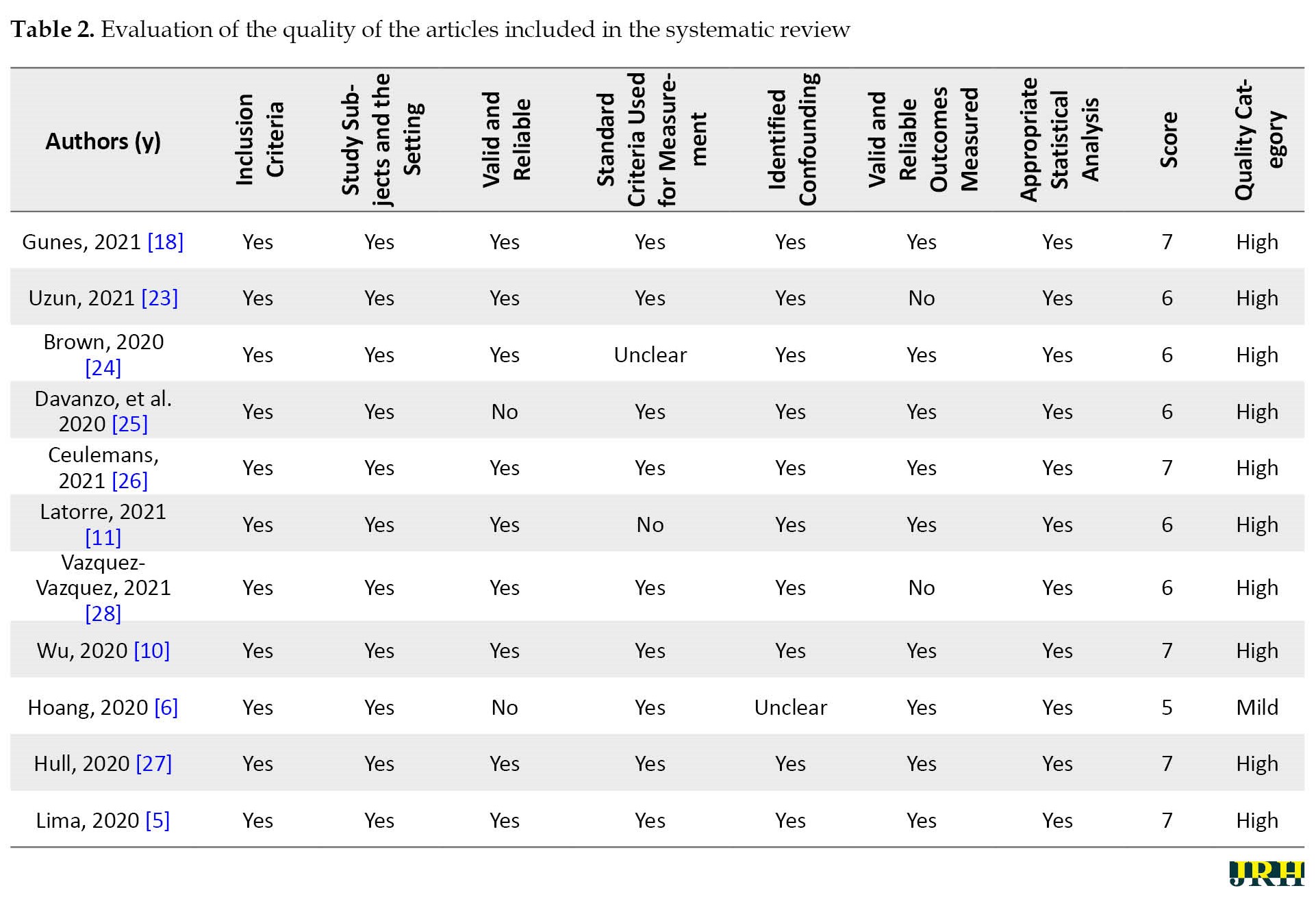
The COVID-19 pandemic has had adverse effects on the physical, mental, and social health of all members of society worldwide, including pregnant women. Pregnant women are considered one of the high-risk groups due to special conditions during pregnancy and postpartum, and their health is affected by this disease. The presence of unfavorable physical conditions of the mother can affect the health of the baby and cause adverse consequences in infants. One of the issues that have been considered is the effect of the COVID-19 pandemic on the way the baby is breastfed because due to the mother’s illness and the presence of psychological disorders caused by pandemics and other underlying factors, can interfere with breastfeeding [7, 22] Accordingly, 11 studies [5, 6, 10, 11, 18, 23-27] on the impact of the COVID-19 pandemic on breastfeeding in 2020 and 2021 were included in the systematic review (Table 1 and Table 2).
The effect of COVID-19 disease and quarantine on lactation
Due to the unknown aspects and effects of COVID-19 disease on maternal and infant health, adverse effects were observed on maternal performance in neonatal care, therefore the definite or suspected infection of the mother with COVID-19 led to a change in the hospitalization procedure for delivery, no skin-to-skin contact between mother and baby at birth, hospitalization of the baby in a separate room and no recommendation for breastfeeding. But then studies reported different approaches to breastfeeding and contact with the mother to maintain the baby health. Brown et al. [24] in the United Kingdom surveyed breastfeeding during the COVID-19 pandemic compared to 1 219 pregnant mothers before the pandemic. Of the pregnant mothers, 495 gave birth before the pandemic and 724 during the pandemic. According to the results, of all women, 18.9% stopped breastfeeding, of which 91.3% gave birth during the COVID-19 period. Moreover, 14.3% of the cases mentioned that they decided to breastfeed before the pandemic, which was 13.4% after the pandemic. A total of 12.5% of mothers who stopped breastfeeding during the COVID-19 pandemic stated that they had suspicious symptoms of COVID-19. In the field of breastfeeding after birth in the hospital at the beginning of the pandemic, 7.8% mentioned that they were not supported for skin contact with the baby at birth, 4.6% were not encouraged to breastfeed at birth, 24.6% were not instructed about breastfeeding in the hospital, and 21.2% mentioned that they were not supported to breastfeed their infants in the hospital. A total of 19.4% of women whose infants were transferred to the neonatal intensive care unit (NICU) could not see their infants and 16% reported that they could not breastfeed due to suspected symptoms of COVID-19 [24]. In the study conducted by Gunes et al., breastfeeding was compared in infants who needed to be admitted to the NICU in the pre-pandemic period to the pandemic period. The results showed that before the COVID-19 pandemic, 100% of mothers breastfed their infants, but during the COVID-19 period, 79% of the mothers breastfed their infants, indicating a 21% drop in breastfeeding ratesv [18]. Also, after discharge of infants up to 1 month of age, before the pandemic, 90% of mothers continued to breastfeed, but during the pandemic, 75.9% continued to breastfeed, which also shows a difference of 14% [18]. Latorre et al. compared the proportion of breastfeeding in women before and during the pandemic in Italy. According to the results, after discharge from the hospital, 97.7% of women before the coronavirus pandemic and 69.4% of the women during the COVID-19 pandemic continued to breastfeed their infants. In addition, this ratio was 76.3% vs. 54.3% 30 days after delivery before the pandemic and during the pandemic, and 70.5% vs. 31.8% 90 days after delivery, respectively, which shows that breastfeeding during the pandemic period is much lower than before the pandemic period [11]. Vazquez et al. in their study examined the ratio of breastfeeding during the COVID-19 pandemic compared to before. Based on the results, no significant difference was observed in skin-to-skin contact at birth before and after the pandemic (87% vs. 89%), contact duration, and the onset of lactation in the two groups. The exclusive breastfeeding ratio before and after the pandemic was 31% and 40%, and the ratio of feeding the baby with complementary milk before and after the pandemic was 12% and 14%, respectively. In both groups, with the onset of the pandemic and quarantine, they reported 30% change in infant feeding patterns. Among breastfeeding mothers, 60% reported no change in breastfeeding, 30% reported an increase in breastfeeding, and 10% reported a decrease in breastfeeding; 68% did not change the duration of breastfeeding, 17% increased its duration and 15% reduced its duration; 4% eventually stopped breastfeeding. In terms of professional breastfeeding support, at the time of the pandemic, 59% of women reported being supported by professional postpartum staff and 40% by their husbands and families. However, 45% stated that they did not receive sufficient support for breastfeeding [28]. Davanzo et al. [25] examined the views of various organizations on breastfeeding. According to the WHO, probable, suspected, and confirmed pregnant women with COVID-19 should make skin-to-skin contact in the delivery room, breastfeed the baby, and follow hygienic principles to prevent the horizontal transmission of the disease and disinfect the surrounding area. The United Nations International Children’s Emergency Fund (UNICEF) has not recommended the separation of mothers, and infants and has emphasized breastfeeding. The Centers for Disease Control and Prevention emphasizes the separation of a suspected mother with COVID-19 from the baby, but at the same time, it emphasizes the continuation of breastfeeding. The Royal College of Obstetricians and Gynecologists has not recommended the separation of the mother from the infant except in severe cases of COVID-19 but has emphasized the need to continue breastfeeding. The Italian National Institute of Health emphasizes breastfeeding and recommends the use of masks and hand washing to prevent transmission. According to the Italian Society on Neonatology, breastfeeding during the COVID-19 pandemic is not a problem even if the mother is infected with the disease and it is not required to pasteurize the milk and if the mother is infected, the baby should be separated [25]. Hoang et al. examined and compiled global guidance for breastfeeding and newborn care in several regions of the world, including Asia [6], Oceania [1], North America [4], South America [1], Europe [8] and Africa [6], it is shown that in mothers with COVID-19 in 27% of cases of skin contact with the mother after birth, 21% of breastfeeding immediately after birth, and 48% of breastfeeding up to the end, breastfeeding was recommended. Also, in the mothers with suspected COVID-19, the aforementioned rates were 24%, 18%, and 42%, respectively [6]. In a study conducted by Wu et al., 13 pregnant women with COVID-19 were studied. The results showed that vertical transmission of the disease from mother to infant and transmission of the disease through breast milk to infant did not occur in any of the cases. However, only one sample of women tested positive for viral nucleic acid testing in breast milk [10]. According to published studies and reports, the proportion of breastfeeding during the COVID-19 pandemic has decreased compared to before the pandemic. This reduction is due to the mother’s illness, the change in hospital function, and the existence of recommendations in contradictory instructions. According to the results of published studies, breastfeeding does not lead to the transmission of the disease from mother to baby and can increase the safety and health of the baby as well as resistance to COVID-19 disease. However, it is necessary to follow the health instructions to prevent the transmission of the disease from the mother with COVID-19 to the baby through inhalation or skin contact.
The effect of psychological disorders on breastfeeding during the COVID-19 pandemic
Due to the physiological changes during pregnancy and childbirth and the mother’s sensitivity to the care of the baby, women’s vulnerability to neuropsychiatric disorders and the need for psychological and social support from the husband and family increases. One of the factors that are affected by these protections is breastfeeding. During the COVID-19 pandemic, psychosocial support was suspended due to economic problems, social distance, lack of contact with other family members, and fear of illness that affects the mother’s mental health and can affect the mother’s performance in the field of breastfeeding [29, 30, 31]. In the study conducted by Uzun et al. in Turkey, which examined breastfeeding in 906 mothers during the COVID-19 pandemic, 94.2% of mothers breastfed, and among mothers who did not breastfeed, 70% said that they did not have enough milk, and 34.3% used formula. In this study, a fear of COVID-19 cale (FCV-19s) questionnaire was used to assess the fear of COVID-19 disease. The results showed a statistically significant difference in the mean score of fear in mothers who did not breastfeed compared to breastfeeding mothers, which showed that increased fear led to decreased breastfeeding [23]. In a study conducted by Brown et al. in the United Kingdom, among mothers who attempted to discontinue breastfeeding during the COVID-19 pandemic, 72.6% reported a lack of face-to-face support and 22% reported concerns about the safety of breast milk [24]. Regarding psychological factors, 16.4% of the cases mentioned that they did not want to contact health professionals due to anxiety caused by the pandemic and 30.5% had avoided making contact. Moreover, 58.8% mentioned that if they needed face-to-face contact with health professionals in the field of breastfeeding, they would be anxious. Other factors affecting breastfeeding in this study were quarantine, emotional support, meeting close relatives, having another child, having green space at home, and walking outdoors [24]. A study conducted by Ceulemans et al. in European countries, including Ireland, Norway, Switzerland, the Netherlands, and the UK, which examined psychiatric disorders in 3907 pregnant women and 5 134 lactating women during the COVID-19 pandemic, found that 15% of pregnant women and 13% of lactating women had severe depression, 11% of pregnant women and 10% of lactating women had severe anxiety, of which 7% of pregnant women and 6% of lactating women had a positive SARS-CoV-2 test. A total of 15.8% of women breastfed less than 6 weeks, 48.2% breastfed between 6 weeks and 6 months and only 36% continued breastfeeding for more than 6 months [26].
In a study conducted by Hull et al. in Australia, 18.8% of women continued breastfeeding during the COVID-19 pandemic, 11.5% did not use nutritional supplements in infants and increased breastfeeding, and 9.7% of cases had resumed breastfeeding. A total of 64% of women mentioned that they needed support to continue breastfeeding; 10% were concerned about milk safety during the pandemic; 61% were not willing to face health personnel due to fear of disease [27]. In a study conducted by Lima et al. in Brazil, breastfeeding counseling sessions increased the mothers’ desire to breastfeed. Due to fear and anxiety in mothers, personal hygiene is strengthened through counseling and team support. In addition, in the field of clinical problems after childbirth, therapeutic and preventive interventions are performed, and finally, the mother’s satisfaction with her condition and health leads to increased breastfeeding [5].
Breastfeeding is vital for the growth and development of infants. Based on the results of studies, due to psychological disorders, loss of support resources, fear of transmitting the disease to the infant, and lack of proper instructions due to unknown aspects of the disease and COVID-19 virus mutations on nutrition, the COVID-19 pandemic has indirectly affected breastfeeding and has reduced the ratio of breastfeeding compared to before. Finally, these cases require clarification and the development of guidelines for breastfeeding during the COVID-19 pandemic, so that breastfeeding mothers can proceed with confidence in feeding their babies. It is also recommended to provide support programs, such as breastfeeding counseling to enhance breastfeeding in the hospital and after the mother is discharged.
Discussion
It is well established that breast milk protects the baby by providing antibodies during the first few months of life while the baby’s immune system is still developing. But whether this is indirectly true for the COVID-19 pandemic indirectly is not entirely clear [32, 33]. The results of the present study showed that the proportion of breastfeeding during the COVID-19 pandemic has decreased compared to before the pandemic, which is due to the mother’s illness, changes in hospital function, and the existence of recommendations in conflicting guidelines. Moreover, although breastfeeding does not transmit the disease from mother to infant, breastfeeding instructions are still emphasized to prevent the transmission of the COVID-19 pandemic through inhalation and close contact. Cohen et al. in their meta-analysis study entitled ‘breastfeeding initiation and continuation: A meta-analysis’ showed that one of the factors that affect the onset and continuation of breastfeeding is the separation of the mother from the child for any reason [34]. In one study, they found that the roommate of the infant and mother is one of the vital and effective factors in the time of onset and exclusive breastfeeding [35]. Additionally, the results of some coherent studies show that the policies governing the systems and the support of health workers (information about breastfeeding) are among the critical barriers affecting the start of breastfeeding and the decision to continue it [36, 37]. The results of this study also show that social and family support, especially in the first 40 days after delivery, is a crucial facilitator for mothers to continue breastfeeding [37]. These results may be due to differences in social awareness and different guidelines regarding the COVID-19 situation in each country. More serious mortality and morbidity due to the emergence of new strains of the virus may lead to greater fears of people, especially pregnant and lactating mothers, of getting the COVID-19 virus, thus changing lifestyle and deciding to breastfeed become the priority for these people. Many recommendations suggest that mothers suspected or infected with COVID-19 should continue to breastfeed with adequate health and respiratory precautions during lactation [38, 39]. This leads to the isolation of the affected mother and the reduction of family support and leads to impaired breastfeeding [27].
Although there does not appear to be vertical transmission between mother and child, after birth in contact with their mother, the baby is susceptible to developing COVID-19 through person-to-person contact. For this reason, at the beginning of the epidemic, no contact was allowed between the infant and the mother, and breastfeeding was recommended subject to a negative maternal test, this factor led to a change in the breastfeeding rate and mothers’ decision to continue breastfeeding [40]. However, after confirmation of the international recommendations, it was shown that the benefits of breastfeeding and the mother-child relationship outweigh the risk of transmission of COVID-19 disease [38, 41].
The results of the present study also showed that due to psychological disorders, loss of support resources, fear of transmitting the disease to the infant, lack of proper instructions due to unknown aspects of the disease, and COVID-19 virus mutations on nutrition, the COVID-19 pandemic has indirectly affected breastfeeding and has reduced the ratio of breastfeeding compared to pre-pandemic times. The results of concomitant studies in this field showed that the greatest concern of mothers in feeding babies is the fear of virus transmission during breastfeeding [42-44]. Moreover, in mothers with COVID-19, despite the confirmations and recommendations to continue breastfeeding, the main reasons leading to a negative impact on breastfeeding can be due to increased responsibilities for child care at home and lack of family and emotional support due to avoidance of family members that can lead to increased anxiety and stress [28].
Family and paternal support are physically and psychologically crucial and potentially influence the decision to breastfeed. Studies have shown that family support is associated with the duration of exclusive breastfeeding for at least 12 months [27, 45, 46]. The support system of the health care provider team also provides positive counseling and breastfeeding and influences the decision to breastfeed [47]. In terms of emotional well-being, avoiding the separation of mother and baby after childbirth also increases the process of mother-infant bonding. Breastfeeding and early mother-infant contact may also facilitate mother-infant bonding. The risk of postpartum depression also decreases with breastfeeding and early mother-infant communication [48].
In particular, international centers support the cohabitation of mothers and infants and direct breastfeeding of asymptomatic mothers by adhering to respiratory and hand hygiene protocols to prevent horizontal transmission to infants. Many authorities also suggest that the baby be kept 2 meters away from the mother or placed in isolation with a barrier and cared for by a healthy person. On the other hand, the WHO emphasizes kangaroo and skin care for mothers and babies. The centers for disease control and prevention also defines its position as making joint decisions between mother and family and consulting with healthcare providers about the risks and benefits of close contact of mother-infant [49, 50]. One of the issues that should be addressed is that in hospital centers and in the postpartum wards that exist as a ward for patients with COVID-19, many patients may be hospitalized with a range of different symptoms and conditions and the mother and baby cannot be roommates, because in this case, the baby who is not infected will be exposed and in contact with different people. Beyond this, a companion or a sponsor cannot enter these wards to prevent the spread of the disease, and as a result, no positive consequences are observed due to the presence of a sponsor next to the infected mother.
Conclusion
The separation between mother and baby hurts the mother-child relationship and can disrupt breastfeeding. Although the new guidelines support the mother-infant close contact for a mother with COVID-19, a few things exist to keep in mind. First, breastfeeding in drug-treated COVID-19 patients is acceptable only if parents are aware of the potential risks. Although most medications used to treat COVID-19 are safe and compatible with breastfeeding, it is recommended that parents be aware of the potential side effects of these medications. Second, in patients with severe symptoms and need of intensive care and oxygen therapy, separation of mother and baby is inevitable, and the use of formula milk or donated milk and the use of breast milk is one of the options for feeding the baby because the mother is not in a good position to breastfeed her baby. Therefore, more studies should be conducted in this area to examine the possibility of vertical transmission of coronavirus through breast milk with more determination and to take effective steps to improve the health of mothers and children.
Limitations
The limitations of the study included the existence of heterogeneity between studies due to the use of different implementation methods, uncertainty of mother’s infection and non-infection with COVID-19 in some studies and its effect on breastfeeding, conducting studies in different countries that had different guidelines in the field of breastfeeding, failure to consider background factors, such as mother’s age, mother’s occupation, number of children, etc. in the participants in some studies and their effect on breastfeeding.
Ethical Considerations
Compliance with ethical guidelines
No ethical considerations were considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
Full-Text: (261 Views)
Introduction
Undoubtedly, breastfeeding has beneficial health consequences for infants and their mothers as well as many benefits for families because it has positive social and economic effects [1]. The World Health Organization (WHO) recommends that breastfeeding begin early within 1 hour of birth and be accompanied by exclusive breastfeeding in the first 6 months of life [2]. Breastfeeding prevents complications and death in the postpartum, infant, and childhood periods. Maternal mental status is also closely related to early breastfeeding because early weaning is a crucial factor for postpartum psychological symptoms [3]. Chang et al. showed that the separation of the mother from the infant for any reason can be one of the causes of early cessation of exclusive breastfeeding [4].
At the end of 2019, an acute respiratory syndrome caused by the coronavirus was reported, which rapidly affected all aspects of life worldwide. Because the virus is transmitted through respiratory droplets, mostly in close contact, the WHO has proposed measures to reduce its prevalence, including restrictions, quarantine, and social distancing [5]. Such actions have led to the separation of mothers and babies after birth, especially in cases of suspected or confirmed COVID-19 infection, and due to the unknown nature of the virus, close contact between mother and baby for breastfeeding was limited [6].
Fear of vertical transmission through breastfeeding quickly became a major concern for mothers, and feelings of self-efficacy and self-confidence in breastfeeding decisions ceased [7]. This was while the available evidence was still contradictory [5]. In a study including a sample of six women infected with COVID-19, no evidence of the virus existed in breast milk samples [8]. While two other studies reported severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the milk of the women studied [9, 10]. Also, in the study conducted by Latorre et al., which was performed on non-infected mothers, the results showed that restrictions and home quarantine in the samples studied reduced the amount of exclusive breastfeeding [11].
Among clinical and public health issues, the main concern with COVID-19 was mother-to-child transmission during pregnancy. In particular, the management of positive and suspected COVID-19 mothers and their offspring after birth and breastfeeding safety is still in question [12-14]. Although different recommendations were stated worldwide, Chinese experts believed that infants should not be fed by suspected or confirmed COVID-19 mothers until their mothers’ tests were negative [13]. Also, in a review study, vertical transmission of the disease from the infected mother to the fetus and neonates was reported in a few cases [15]. This led to the separation of mothers from infants and delayed breastfeeding.
Although it is reported that the presence of SARS-CoV-2 in positive mothers indicates the risk of transmission of the virus through breast milk, breast milk has not yet been established as a transmitter of the virus [16, 17]. On the other hand, according to current scientific knowledge, recommendations for breastfeeding during an epidemic vary from country to country. Gunes et al. in their study, which examined the breastfeeding rate in positive mothers in the neonatal intensive care unit, showed that from the time of discharge to 30 days of age, the rate of exclusive breastfeeding did not change in the study groups [18]. Supporting women to continue breastfeeding during the COVID-19 epidemic is a public health priority. Research to date has shown that acute respiratory syndrome caused by SARS-Cov-2 is not transmitted in breast milk [19].
Neonate breastfeeding is influenced by various factors, including the physical and mental health of the mother and neonate, and the economic and social conditions of the family. The COVID-19 pandemic affected all aspects of human life, which affected the mother’s breastfeeding. It is necessary to be aware of factors affecting breastfeeding, instructions, and approaches to strengthen breastfeeding. Because not feeding the neonate with breast milk can affect the health of the neonate and the mother. Based on this, the present study was conducted to investigate breastfeeding obstacles and guidelines and strategies for increasing breastfeeding during the COVID-19 pandemic.
Methods
This systematic review was conducted to investigate the effect of the COVID-19 pandemic on breastfeeding. The preferred reporting items for systematic reviews and meta-analyses (PRISMA) standard guideline was used to follow up the review process and report results [20].
Search strategy and information sources
This review focused on studies about breastfeeding and COVID-19 published in English language journals from the beginning of December 2019 up to 30 January 2023. The CINAHL, EMBASE, Medline, Cochrane CENTRAL, Science Direct, Google Scholar, and PubMed databases were searched for medical subject headings and relevant keywords, ‘breastfeeding’, ‘breastfeeding duration’, ‘breastfeeding continuation’, ‘breastfeeding decision-making’, AND ‘COVID-19’, ‘COVID-19 virus’, ‘coronavirus disease 2019’, ‘SARS-CoV-2’, ‘pandemic’, ‘outbreak’. They were used in isolation or combination through the Boolean method.
Syntax search in PubMed database
(Breastfeeding) OR (breastfed) OR (exclusive breastfeeding) OR (breast milk expression) OR (breast milk) OR (human milk) AND (COVID-19) OR (SARS-CoV-2 infection) OR (2019 novel coronavirus disease) OR (COVID-19 virus infection) OR (coronavirus disease 2019) OR (COVID-19 virus disease) OR (COVID-19 pandemic)
Eligibility criteria
The inclusion criteria included all English-language articles on breastfeeding and COVID-19 and of high quality. The exclusion criteria included articles of low quality and published in non-English language, review studies, meta-analyses, case reports, or series of cases.
Risk bias assessment
Risk bias assessment of articles was performed using the Joanna Briggs Institute critical appraisal checklist. This tool has these sections, inclusion criteria, study subjects and the setting, valid and reliable exposure measured, standard criteria used for measurement, identified confounding, valid and reliable outcomes measured, and appropriate statistical analysis, in each section the answers yes, no or unclear can be selected [21].
Sensitivity analysis was performed to investigate the influence of each study or a group of studies on the overall risk estimate; for instance, studies with small sample sizes or low-quality scores were deleted.
Screening and data extraction
The search results were imported into the Mendeley software, version 2.107.0 and duplicate titles were deleted. Selected studies were entered into abstract reading and were checked based on the inclusion criteria. Of which, the most relevant studies were selected for independent full-text reading by two researchers (Salman Daliri, Jafar Bazyar), and a third person as the expert epidemiologist checked the result. The reasons for the rejection of studies were mentioned, and in case of disagreement between the researchers, the perspective of a third researcher was sought. A checklist was used to extract data from the selected studies in terms of the sample size, study location, study years, study type, COVID-19 pandemic, and breastfeeding (Table 1).
Selection of articles
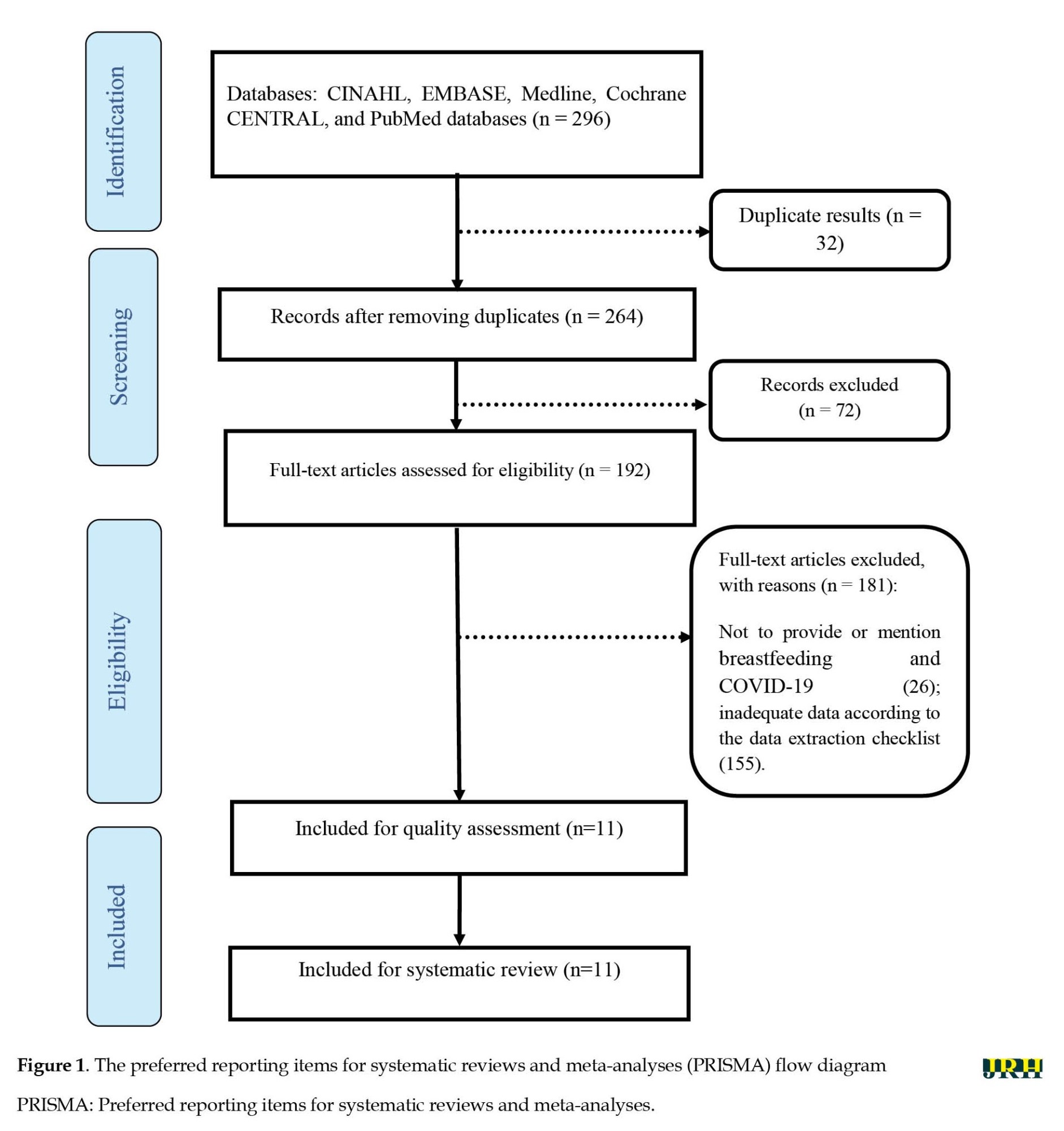
By searching databases, 296 studies were extracted. Initially, the articles were entered into Mendeley software and after an initial review, 32 articles were removed from the study due to duplication. Then, by reviewing the titles and abstracts of articles, 72 articles were removed due to irrelevance and after reviewing the full text of articles, 181 articles were excluded for other reasons. Finally, 11 articles met the inclusion criteria and entered the systematic review process (Figure 1).
Undoubtedly, breastfeeding has beneficial health consequences for infants and their mothers as well as many benefits for families because it has positive social and economic effects [1]. The World Health Organization (WHO) recommends that breastfeeding begin early within 1 hour of birth and be accompanied by exclusive breastfeeding in the first 6 months of life [2]. Breastfeeding prevents complications and death in the postpartum, infant, and childhood periods. Maternal mental status is also closely related to early breastfeeding because early weaning is a crucial factor for postpartum psychological symptoms [3]. Chang et al. showed that the separation of the mother from the infant for any reason can be one of the causes of early cessation of exclusive breastfeeding [4].
At the end of 2019, an acute respiratory syndrome caused by the coronavirus was reported, which rapidly affected all aspects of life worldwide. Because the virus is transmitted through respiratory droplets, mostly in close contact, the WHO has proposed measures to reduce its prevalence, including restrictions, quarantine, and social distancing [5]. Such actions have led to the separation of mothers and babies after birth, especially in cases of suspected or confirmed COVID-19 infection, and due to the unknown nature of the virus, close contact between mother and baby for breastfeeding was limited [6].
Fear of vertical transmission through breastfeeding quickly became a major concern for mothers, and feelings of self-efficacy and self-confidence in breastfeeding decisions ceased [7]. This was while the available evidence was still contradictory [5]. In a study including a sample of six women infected with COVID-19, no evidence of the virus existed in breast milk samples [8]. While two other studies reported severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the milk of the women studied [9, 10]. Also, in the study conducted by Latorre et al., which was performed on non-infected mothers, the results showed that restrictions and home quarantine in the samples studied reduced the amount of exclusive breastfeeding [11].
Among clinical and public health issues, the main concern with COVID-19 was mother-to-child transmission during pregnancy. In particular, the management of positive and suspected COVID-19 mothers and their offspring after birth and breastfeeding safety is still in question [12-14]. Although different recommendations were stated worldwide, Chinese experts believed that infants should not be fed by suspected or confirmed COVID-19 mothers until their mothers’ tests were negative [13]. Also, in a review study, vertical transmission of the disease from the infected mother to the fetus and neonates was reported in a few cases [15]. This led to the separation of mothers from infants and delayed breastfeeding.
Although it is reported that the presence of SARS-CoV-2 in positive mothers indicates the risk of transmission of the virus through breast milk, breast milk has not yet been established as a transmitter of the virus [16, 17]. On the other hand, according to current scientific knowledge, recommendations for breastfeeding during an epidemic vary from country to country. Gunes et al. in their study, which examined the breastfeeding rate in positive mothers in the neonatal intensive care unit, showed that from the time of discharge to 30 days of age, the rate of exclusive breastfeeding did not change in the study groups [18]. Supporting women to continue breastfeeding during the COVID-19 epidemic is a public health priority. Research to date has shown that acute respiratory syndrome caused by SARS-Cov-2 is not transmitted in breast milk [19].
Neonate breastfeeding is influenced by various factors, including the physical and mental health of the mother and neonate, and the economic and social conditions of the family. The COVID-19 pandemic affected all aspects of human life, which affected the mother’s breastfeeding. It is necessary to be aware of factors affecting breastfeeding, instructions, and approaches to strengthen breastfeeding. Because not feeding the neonate with breast milk can affect the health of the neonate and the mother. Based on this, the present study was conducted to investigate breastfeeding obstacles and guidelines and strategies for increasing breastfeeding during the COVID-19 pandemic.
Methods
This systematic review was conducted to investigate the effect of the COVID-19 pandemic on breastfeeding. The preferred reporting items for systematic reviews and meta-analyses (PRISMA) standard guideline was used to follow up the review process and report results [20].
Search strategy and information sources
This review focused on studies about breastfeeding and COVID-19 published in English language journals from the beginning of December 2019 up to 30 January 2023. The CINAHL, EMBASE, Medline, Cochrane CENTRAL, Science Direct, Google Scholar, and PubMed databases were searched for medical subject headings and relevant keywords, ‘breastfeeding’, ‘breastfeeding duration’, ‘breastfeeding continuation’, ‘breastfeeding decision-making’, AND ‘COVID-19’, ‘COVID-19 virus’, ‘coronavirus disease 2019’, ‘SARS-CoV-2’, ‘pandemic’, ‘outbreak’. They were used in isolation or combination through the Boolean method.
Syntax search in PubMed database
(Breastfeeding) OR (breastfed) OR (exclusive breastfeeding) OR (breast milk expression) OR (breast milk) OR (human milk) AND (COVID-19) OR (SARS-CoV-2 infection) OR (2019 novel coronavirus disease) OR (COVID-19 virus infection) OR (coronavirus disease 2019) OR (COVID-19 virus disease) OR (COVID-19 pandemic)
Eligibility criteria
The inclusion criteria included all English-language articles on breastfeeding and COVID-19 and of high quality. The exclusion criteria included articles of low quality and published in non-English language, review studies, meta-analyses, case reports, or series of cases.
Risk bias assessment
Risk bias assessment of articles was performed using the Joanna Briggs Institute critical appraisal checklist. This tool has these sections, inclusion criteria, study subjects and the setting, valid and reliable exposure measured, standard criteria used for measurement, identified confounding, valid and reliable outcomes measured, and appropriate statistical analysis, in each section the answers yes, no or unclear can be selected [21].
Sensitivity analysis was performed to investigate the influence of each study or a group of studies on the overall risk estimate; for instance, studies with small sample sizes or low-quality scores were deleted.
Screening and data extraction
The search results were imported into the Mendeley software, version 2.107.0 and duplicate titles were deleted. Selected studies were entered into abstract reading and were checked based on the inclusion criteria. Of which, the most relevant studies were selected for independent full-text reading by two researchers (Salman Daliri, Jafar Bazyar), and a third person as the expert epidemiologist checked the result. The reasons for the rejection of studies were mentioned, and in case of disagreement between the researchers, the perspective of a third researcher was sought. A checklist was used to extract data from the selected studies in terms of the sample size, study location, study years, study type, COVID-19 pandemic, and breastfeeding (Table 1).
Selection of articles
By searching databases, 296 studies were extracted. Initially, the articles were entered into Mendeley software and after an initial review, 32 articles were removed from the study due to duplication. Then, by reviewing the titles and abstracts of articles, 72 articles were removed due to irrelevance and after reviewing the full text of articles, 181 articles were excluded for other reasons. Finally, 11 articles met the inclusion criteria and entered the systematic review process (Figure 1).
Results
The COVID-19 pandemic has had adverse effects on the physical, mental, and social health of all members of society worldwide, including pregnant women. Pregnant women are considered one of the high-risk groups due to special conditions during pregnancy and postpartum, and their health is affected by this disease. The presence of unfavorable physical conditions of the mother can affect the health of the baby and cause adverse consequences in infants. One of the issues that have been considered is the effect of the COVID-19 pandemic on the way the baby is breastfed because due to the mother’s illness and the presence of psychological disorders caused by pandemics and other underlying factors, can interfere with breastfeeding [7, 22] Accordingly, 11 studies [5, 6, 10, 11, 18, 23-27] on the impact of the COVID-19 pandemic on breastfeeding in 2020 and 2021 were included in the systematic review (Table 1 and Table 2).
The effect of COVID-19 disease and quarantine on lactation
Due to the unknown aspects and effects of COVID-19 disease on maternal and infant health, adverse effects were observed on maternal performance in neonatal care, therefore the definite or suspected infection of the mother with COVID-19 led to a change in the hospitalization procedure for delivery, no skin-to-skin contact between mother and baby at birth, hospitalization of the baby in a separate room and no recommendation for breastfeeding. But then studies reported different approaches to breastfeeding and contact with the mother to maintain the baby health. Brown et al. [24] in the United Kingdom surveyed breastfeeding during the COVID-19 pandemic compared to 1 219 pregnant mothers before the pandemic. Of the pregnant mothers, 495 gave birth before the pandemic and 724 during the pandemic. According to the results, of all women, 18.9% stopped breastfeeding, of which 91.3% gave birth during the COVID-19 period. Moreover, 14.3% of the cases mentioned that they decided to breastfeed before the pandemic, which was 13.4% after the pandemic. A total of 12.5% of mothers who stopped breastfeeding during the COVID-19 pandemic stated that they had suspicious symptoms of COVID-19. In the field of breastfeeding after birth in the hospital at the beginning of the pandemic, 7.8% mentioned that they were not supported for skin contact with the baby at birth, 4.6% were not encouraged to breastfeed at birth, 24.6% were not instructed about breastfeeding in the hospital, and 21.2% mentioned that they were not supported to breastfeed their infants in the hospital. A total of 19.4% of women whose infants were transferred to the neonatal intensive care unit (NICU) could not see their infants and 16% reported that they could not breastfeed due to suspected symptoms of COVID-19 [24]. In the study conducted by Gunes et al., breastfeeding was compared in infants who needed to be admitted to the NICU in the pre-pandemic period to the pandemic period. The results showed that before the COVID-19 pandemic, 100% of mothers breastfed their infants, but during the COVID-19 period, 79% of the mothers breastfed their infants, indicating a 21% drop in breastfeeding ratesv [18]. Also, after discharge of infants up to 1 month of age, before the pandemic, 90% of mothers continued to breastfeed, but during the pandemic, 75.9% continued to breastfeed, which also shows a difference of 14% [18]. Latorre et al. compared the proportion of breastfeeding in women before and during the pandemic in Italy. According to the results, after discharge from the hospital, 97.7% of women before the coronavirus pandemic and 69.4% of the women during the COVID-19 pandemic continued to breastfeed their infants. In addition, this ratio was 76.3% vs. 54.3% 30 days after delivery before the pandemic and during the pandemic, and 70.5% vs. 31.8% 90 days after delivery, respectively, which shows that breastfeeding during the pandemic period is much lower than before the pandemic period [11]. Vazquez et al. in their study examined the ratio of breastfeeding during the COVID-19 pandemic compared to before. Based on the results, no significant difference was observed in skin-to-skin contact at birth before and after the pandemic (87% vs. 89%), contact duration, and the onset of lactation in the two groups. The exclusive breastfeeding ratio before and after the pandemic was 31% and 40%, and the ratio of feeding the baby with complementary milk before and after the pandemic was 12% and 14%, respectively. In both groups, with the onset of the pandemic and quarantine, they reported 30% change in infant feeding patterns. Among breastfeeding mothers, 60% reported no change in breastfeeding, 30% reported an increase in breastfeeding, and 10% reported a decrease in breastfeeding; 68% did not change the duration of breastfeeding, 17% increased its duration and 15% reduced its duration; 4% eventually stopped breastfeeding. In terms of professional breastfeeding support, at the time of the pandemic, 59% of women reported being supported by professional postpartum staff and 40% by their husbands and families. However, 45% stated that they did not receive sufficient support for breastfeeding [28]. Davanzo et al. [25] examined the views of various organizations on breastfeeding. According to the WHO, probable, suspected, and confirmed pregnant women with COVID-19 should make skin-to-skin contact in the delivery room, breastfeed the baby, and follow hygienic principles to prevent the horizontal transmission of the disease and disinfect the surrounding area. The United Nations International Children’s Emergency Fund (UNICEF) has not recommended the separation of mothers, and infants and has emphasized breastfeeding. The Centers for Disease Control and Prevention emphasizes the separation of a suspected mother with COVID-19 from the baby, but at the same time, it emphasizes the continuation of breastfeeding. The Royal College of Obstetricians and Gynecologists has not recommended the separation of the mother from the infant except in severe cases of COVID-19 but has emphasized the need to continue breastfeeding. The Italian National Institute of Health emphasizes breastfeeding and recommends the use of masks and hand washing to prevent transmission. According to the Italian Society on Neonatology, breastfeeding during the COVID-19 pandemic is not a problem even if the mother is infected with the disease and it is not required to pasteurize the milk and if the mother is infected, the baby should be separated [25]. Hoang et al. examined and compiled global guidance for breastfeeding and newborn care in several regions of the world, including Asia [6], Oceania [1], North America [4], South America [1], Europe [8] and Africa [6], it is shown that in mothers with COVID-19 in 27% of cases of skin contact with the mother after birth, 21% of breastfeeding immediately after birth, and 48% of breastfeeding up to the end, breastfeeding was recommended. Also, in the mothers with suspected COVID-19, the aforementioned rates were 24%, 18%, and 42%, respectively [6]. In a study conducted by Wu et al., 13 pregnant women with COVID-19 were studied. The results showed that vertical transmission of the disease from mother to infant and transmission of the disease through breast milk to infant did not occur in any of the cases. However, only one sample of women tested positive for viral nucleic acid testing in breast milk [10]. According to published studies and reports, the proportion of breastfeeding during the COVID-19 pandemic has decreased compared to before the pandemic. This reduction is due to the mother’s illness, the change in hospital function, and the existence of recommendations in contradictory instructions. According to the results of published studies, breastfeeding does not lead to the transmission of the disease from mother to baby and can increase the safety and health of the baby as well as resistance to COVID-19 disease. However, it is necessary to follow the health instructions to prevent the transmission of the disease from the mother with COVID-19 to the baby through inhalation or skin contact.
The effect of psychological disorders on breastfeeding during the COVID-19 pandemic
Due to the physiological changes during pregnancy and childbirth and the mother’s sensitivity to the care of the baby, women’s vulnerability to neuropsychiatric disorders and the need for psychological and social support from the husband and family increases. One of the factors that are affected by these protections is breastfeeding. During the COVID-19 pandemic, psychosocial support was suspended due to economic problems, social distance, lack of contact with other family members, and fear of illness that affects the mother’s mental health and can affect the mother’s performance in the field of breastfeeding [29, 30, 31]. In the study conducted by Uzun et al. in Turkey, which examined breastfeeding in 906 mothers during the COVID-19 pandemic, 94.2% of mothers breastfed, and among mothers who did not breastfeed, 70% said that they did not have enough milk, and 34.3% used formula. In this study, a fear of COVID-19 cale (FCV-19s) questionnaire was used to assess the fear of COVID-19 disease. The results showed a statistically significant difference in the mean score of fear in mothers who did not breastfeed compared to breastfeeding mothers, which showed that increased fear led to decreased breastfeeding [23]. In a study conducted by Brown et al. in the United Kingdom, among mothers who attempted to discontinue breastfeeding during the COVID-19 pandemic, 72.6% reported a lack of face-to-face support and 22% reported concerns about the safety of breast milk [24]. Regarding psychological factors, 16.4% of the cases mentioned that they did not want to contact health professionals due to anxiety caused by the pandemic and 30.5% had avoided making contact. Moreover, 58.8% mentioned that if they needed face-to-face contact with health professionals in the field of breastfeeding, they would be anxious. Other factors affecting breastfeeding in this study were quarantine, emotional support, meeting close relatives, having another child, having green space at home, and walking outdoors [24]. A study conducted by Ceulemans et al. in European countries, including Ireland, Norway, Switzerland, the Netherlands, and the UK, which examined psychiatric disorders in 3907 pregnant women and 5 134 lactating women during the COVID-19 pandemic, found that 15% of pregnant women and 13% of lactating women had severe depression, 11% of pregnant women and 10% of lactating women had severe anxiety, of which 7% of pregnant women and 6% of lactating women had a positive SARS-CoV-2 test. A total of 15.8% of women breastfed less than 6 weeks, 48.2% breastfed between 6 weeks and 6 months and only 36% continued breastfeeding for more than 6 months [26].
In a study conducted by Hull et al. in Australia, 18.8% of women continued breastfeeding during the COVID-19 pandemic, 11.5% did not use nutritional supplements in infants and increased breastfeeding, and 9.7% of cases had resumed breastfeeding. A total of 64% of women mentioned that they needed support to continue breastfeeding; 10% were concerned about milk safety during the pandemic; 61% were not willing to face health personnel due to fear of disease [27]. In a study conducted by Lima et al. in Brazil, breastfeeding counseling sessions increased the mothers’ desire to breastfeed. Due to fear and anxiety in mothers, personal hygiene is strengthened through counseling and team support. In addition, in the field of clinical problems after childbirth, therapeutic and preventive interventions are performed, and finally, the mother’s satisfaction with her condition and health leads to increased breastfeeding [5].
Breastfeeding is vital for the growth and development of infants. Based on the results of studies, due to psychological disorders, loss of support resources, fear of transmitting the disease to the infant, and lack of proper instructions due to unknown aspects of the disease and COVID-19 virus mutations on nutrition, the COVID-19 pandemic has indirectly affected breastfeeding and has reduced the ratio of breastfeeding compared to before. Finally, these cases require clarification and the development of guidelines for breastfeeding during the COVID-19 pandemic, so that breastfeeding mothers can proceed with confidence in feeding their babies. It is also recommended to provide support programs, such as breastfeeding counseling to enhance breastfeeding in the hospital and after the mother is discharged.
Discussion
It is well established that breast milk protects the baby by providing antibodies during the first few months of life while the baby’s immune system is still developing. But whether this is indirectly true for the COVID-19 pandemic indirectly is not entirely clear [32, 33]. The results of the present study showed that the proportion of breastfeeding during the COVID-19 pandemic has decreased compared to before the pandemic, which is due to the mother’s illness, changes in hospital function, and the existence of recommendations in conflicting guidelines. Moreover, although breastfeeding does not transmit the disease from mother to infant, breastfeeding instructions are still emphasized to prevent the transmission of the COVID-19 pandemic through inhalation and close contact. Cohen et al. in their meta-analysis study entitled ‘breastfeeding initiation and continuation: A meta-analysis’ showed that one of the factors that affect the onset and continuation of breastfeeding is the separation of the mother from the child for any reason [34]. In one study, they found that the roommate of the infant and mother is one of the vital and effective factors in the time of onset and exclusive breastfeeding [35]. Additionally, the results of some coherent studies show that the policies governing the systems and the support of health workers (information about breastfeeding) are among the critical barriers affecting the start of breastfeeding and the decision to continue it [36, 37]. The results of this study also show that social and family support, especially in the first 40 days after delivery, is a crucial facilitator for mothers to continue breastfeeding [37]. These results may be due to differences in social awareness and different guidelines regarding the COVID-19 situation in each country. More serious mortality and morbidity due to the emergence of new strains of the virus may lead to greater fears of people, especially pregnant and lactating mothers, of getting the COVID-19 virus, thus changing lifestyle and deciding to breastfeed become the priority for these people. Many recommendations suggest that mothers suspected or infected with COVID-19 should continue to breastfeed with adequate health and respiratory precautions during lactation [38, 39]. This leads to the isolation of the affected mother and the reduction of family support and leads to impaired breastfeeding [27].
Although there does not appear to be vertical transmission between mother and child, after birth in contact with their mother, the baby is susceptible to developing COVID-19 through person-to-person contact. For this reason, at the beginning of the epidemic, no contact was allowed between the infant and the mother, and breastfeeding was recommended subject to a negative maternal test, this factor led to a change in the breastfeeding rate and mothers’ decision to continue breastfeeding [40]. However, after confirmation of the international recommendations, it was shown that the benefits of breastfeeding and the mother-child relationship outweigh the risk of transmission of COVID-19 disease [38, 41].
The results of the present study also showed that due to psychological disorders, loss of support resources, fear of transmitting the disease to the infant, lack of proper instructions due to unknown aspects of the disease, and COVID-19 virus mutations on nutrition, the COVID-19 pandemic has indirectly affected breastfeeding and has reduced the ratio of breastfeeding compared to pre-pandemic times. The results of concomitant studies in this field showed that the greatest concern of mothers in feeding babies is the fear of virus transmission during breastfeeding [42-44]. Moreover, in mothers with COVID-19, despite the confirmations and recommendations to continue breastfeeding, the main reasons leading to a negative impact on breastfeeding can be due to increased responsibilities for child care at home and lack of family and emotional support due to avoidance of family members that can lead to increased anxiety and stress [28].
Family and paternal support are physically and psychologically crucial and potentially influence the decision to breastfeed. Studies have shown that family support is associated with the duration of exclusive breastfeeding for at least 12 months [27, 45, 46]. The support system of the health care provider team also provides positive counseling and breastfeeding and influences the decision to breastfeed [47]. In terms of emotional well-being, avoiding the separation of mother and baby after childbirth also increases the process of mother-infant bonding. Breastfeeding and early mother-infant contact may also facilitate mother-infant bonding. The risk of postpartum depression also decreases with breastfeeding and early mother-infant communication [48].
In particular, international centers support the cohabitation of mothers and infants and direct breastfeeding of asymptomatic mothers by adhering to respiratory and hand hygiene protocols to prevent horizontal transmission to infants. Many authorities also suggest that the baby be kept 2 meters away from the mother or placed in isolation with a barrier and cared for by a healthy person. On the other hand, the WHO emphasizes kangaroo and skin care for mothers and babies. The centers for disease control and prevention also defines its position as making joint decisions between mother and family and consulting with healthcare providers about the risks and benefits of close contact of mother-infant [49, 50]. One of the issues that should be addressed is that in hospital centers and in the postpartum wards that exist as a ward for patients with COVID-19, many patients may be hospitalized with a range of different symptoms and conditions and the mother and baby cannot be roommates, because in this case, the baby who is not infected will be exposed and in contact with different people. Beyond this, a companion or a sponsor cannot enter these wards to prevent the spread of the disease, and as a result, no positive consequences are observed due to the presence of a sponsor next to the infected mother.
Conclusion
The separation between mother and baby hurts the mother-child relationship and can disrupt breastfeeding. Although the new guidelines support the mother-infant close contact for a mother with COVID-19, a few things exist to keep in mind. First, breastfeeding in drug-treated COVID-19 patients is acceptable only if parents are aware of the potential risks. Although most medications used to treat COVID-19 are safe and compatible with breastfeeding, it is recommended that parents be aware of the potential side effects of these medications. Second, in patients with severe symptoms and need of intensive care and oxygen therapy, separation of mother and baby is inevitable, and the use of formula milk or donated milk and the use of breast milk is one of the options for feeding the baby because the mother is not in a good position to breastfeed her baby. Therefore, more studies should be conducted in this area to examine the possibility of vertical transmission of coronavirus through breast milk with more determination and to take effective steps to improve the health of mothers and children.
Limitations
The limitations of the study included the existence of heterogeneity between studies due to the use of different implementation methods, uncertainty of mother’s infection and non-infection with COVID-19 in some studies and its effect on breastfeeding, conducting studies in different countries that had different guidelines in the field of breastfeeding, failure to consider background factors, such as mother’s age, mother’s occupation, number of children, etc. in the participants in some studies and their effect on breastfeeding.
Ethical Considerations
Compliance with ethical guidelines
No ethical considerations were considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Dumitriu D, Emeruwa UN, Hanft E, Liao GV, Ludwig E, Walzer L, et al. Outcomes of neonates born to mothers with severe acute respiratory syndrome coronavirus 2 infection at a large medical center in New York City. JAMA Pediatrics. 2021; 175(2):157-67. [DOI:10.1001/jamapediatrics.2020.4298]
- Williams J, Namazova-Baranova L, Weber M, Vural M, Mestrovic J, Carrasco-Sanz A, et al. The importance of continuing breastfeeding during coronavirus disease-2019: In support of the World Health Organization statement on breastfeeding during the pandemic. The Journal of Pediatrics. 2020; 223:234-6. [DOI:10.1016/j.jpeds.2020.05.009]
- Woolhouse H, James J, Gartland D, McDonald E, Brown SJ. Maternal depressive symptoms at three months postpartum and breastfeeding rates at six months postpartum: Implications for primary care in a prospective cohort study of primiparous women in Australia. Women and Birth. 2016; 29(4):381-7. [DOI:10.1016/j.wombi.2016.05.008]
- Chang PC, Li SF, Yang HY, Wang LC, Weng CY, Chen KF, et al. Factors associated with cessation of exclusive breastfeeding at 1 and 2 months postpartum in Taiwan. International Breastfeeding Journal. 2019; 14(1):1-7. [DOI:10.1186/s13006-019-0213-1]
- Lima AC, Chaves AF, Oliveira MG, Lima SA, Machado MM, Oriá MO. Breastfeeding consultancy during the COVID-19 pandemic: Experience report. Escola Anna Nery. 2020; 24(spe):e20200350. [Link]
- Hoang DV, Cashin J, Gribble K, Marinelli K, Mathisen R. Misalignment of global COVID-19 breastfeeding and newborn care guidelines with World Health Organization recommendations. BMJ Nutrition, Prevention & Health. 2020; 3(2):339. [DOI:10.1136/bmjnph-2020-000184]
- Pacheco F, Sobral M, Guiomar R, de la Torre-Luque A, Caparros-Gonzalez RA, Ganho-Ávila A. Breastfeeding during COVID-19: A narrative review of the psychological impact on mothers. Behavioral Sciences. 2021; 11(3):34. [DOI:10.3390/bs11030034]
- Li P, Xie M, Zhang W. Clinical characteristics and intrauterine vertical transmission potential of coronavirus disease 2019 infection in 9 pregnant women: A retrospective review of medical records. American Journal of Obstetrics & Gynecology. 2020; 223(6):955-6. [DOI:10.1016/j.ajog.2020.08.059]
- Groß R, Conzelmann C, Müller JA, Stenger S, Steinhart K, Kirchhoff F, et al. Detection of SARS-CoV-2 in human breastmilk. The Lancet. 2020; 395(10239):1757-8. [DOI:10.1016/s0140-6736(20)31181-8]
- Wu Y, Liu C, Dong L, Zhang C, Chen Y, Liu J, et al. Coronavirus disease 2019 among pregnant Chinese women: Case series data on the safety of vaginal birth and breastfeeding. BJOG: An International Journal of Obstetrics & Gynaecology. 2020; 127(9):1109-15. [DOI:10.1111/1471-0528.16276]
- Latorre G, Martinelli D, Guida P, Masi E, Benedictis R, Maggio L. Impact of COVID-19 pandemic lockdown on exclusive breastfeeding in non-infected mothers. International Breastfeeding Journal. 2021; 16(1):36. [DOI:10.1186/s13006-021-00382-4]
- Pereira A, Cruz-Melguizo S, Adrien M, Fuentes L, Marin E, Forti A, et al. Breastfeeding mothers with COVID-19 infection: A case series. International Breastfeeding Journal. 2020; 15(1):1-8. [DOI:10.1186/s13006-020-00314-8]
- Wang L, Shi Y, Xiao T, Fu J, Feng X, Mu D, et al. Chinese expert consensus on the perinatal and neonatal management for the prevention and control of the 2019 novel coronavirus infection. Annals of Translational Medicine. 2020; 8(3):47. [DOI:10.21037/atm.2020.02.20]
- Chandrasekharan P, Vento M, Trevisanuto D, Partridge E, Underwood MA, Wiedeman J, et al. Neonatal resuscitation and postresuscitation care of infants born to mothers with suspected or confirmed SARS-CoV-2 infection. American Journal of Perinatology, 2020. 37(08):813-24. [DOI:10.1055/s-0040-1709688]
- Najafi, TF, Dashti S, Bahri N. Vertical transmission of covid-19: A systematic review. Archives of Pediatric Infectious Diseases. 2021. 9(2):e108769. [DOI:10.5812/pedinfect.108769]
- Zhu C, Liu W, Su H, Li S, Shereen MA, Lv Z, et al. Breastfeeding risk from detectable severe acute respiratory syndrome coronavirus 2 in breastmilk. Journal of Infection, 2020; 81(3):452-82. [DOI:10.1016/j.jinf.2020.06.001]
- Tam PC, Ly KM, Kernich ML, Spurrier N, Lawrence D, Gordon DL, et al. Detectable severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in human breast milk of a mildly symptomatic patient with coronavirus disease 2019 (COVID-19). Clinical Infectious Diseases. 2021; 72(1):128-30. [DOI:10.1093/cid/ciaa673]
- Gunes AO, Dincer E, Karadag N, Topcuoglu S, Karatekin G. Effects of COVID-19 pandemic on breastfeeding rates in a neonatal intensive care unit. Journal of Perinatal Medicine. 2021; 49(4):500-5. [DOI:10.1515/jpm-2020-0462]
- Chambers C, Krogstad P, Bertrand K, Contreras D, Tobin NH, Bode L, et al. Evaluation for SARS-CoV-2 in breast milk from 18 infected women. JAMA. 2020; 324(13):1347-8. [DOI:10.1001/jama.2020.15580]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015; 4(1):1-9. [DOI:10.1186/2046-4053-4-1]
- Buccheri RK, Sharifi C. Critical appraisal tools and reporting guidelines for evidence‐based practice. Worldviews on Evidence‐Based Nursing. 2017; 14(6):463-72. [DOI:10.1111/wvn.12258]
- Lubbe W, Botha E, Niela-Vilen H, Reimers P. Breastfeeding during the COVID-19 pandemic-a literature review for clinical practice. International Breastfeeding Journal. 2020; 15(1):1-9. [DOI:10.1186/s13006-020-00319-3]
- Uzun A, Öztürk GZ, Bozkurt Z, Çavuşoğlu M. Investigating of fear of COVID-19 after pregnancy and association with breastfeeding. Journal of Ideas in Health. 2021; 4(1):327-33. [DOI:10.47108/jidhealth.vol4.iss1.98]
- Brown A, Shenker N. Experiences of breastfeeding during COVID‐19: Lessons for future practical and emotional support. Maternal & Child Nutrition. 2021; 17(1):e13088. [DOI:10.1111/mcn.13088]
- Davanzo R, Moro G, Sandri F, Agosti M, Moretti C, Mosca F. Breastfeeding and coronavirus disease‐2019: Ad interim indications of the Italian Society of Neonatology endorsed by the Unio of European Neonatal & Perinatal Societies. Maternal & Child Nutrition. 2020. 16(3):e13010. [DOI:10.1111/mcn.13010]
- Ceulemans M, Foulon V, Ngo E, Panchaud A, Winterfeld U, Pomar L, et al. Mental health status of pregnant and breastfeeding women during the COVID‐19 pandemic-A multinational cross‐sectional study. Acta Obstetricia et Gynecologica Scandinavica. 2021; 100(7):1219-29. [DOI:10.1111/aogs.14092]
- Hull N, Kam RL, Gribble KD. Gribble, Providing breastfeeding support during the COVID-19 pandemic: Concerns of mothers who contacted the Australian Breastfeeding Association. Breastfeeding Review. 2020; 28(3):25-35. [DOI:10.1101/2020.07.18.20152256]
- Vazquez-Vazquez A, Dib S, Rougeaux E, Wells JC, Fewtrell MS. The impact of the Covid-19 lockdown on the experiences and feeding practices of new mothers in the UK: Preliminary data from the COVID-19 New Mum Study. Appetite. 2021; 156:104985. [DOI:10.1016/j.appet.2020.104985]
- Radzyminski S, Callister LC. Mother’s beliefs, attitudes, and decision making related to infant feeding choices. The Journal of Perinatal Education. 2016; 25(1):18 [DOI:10.1891/1058-1243.25.1.18]
- Deems NP, Leuner B. Pregnancy, postpartum and parity: Resilience and vulnerability in brain health and disease. Frontiers in Neuroendocrinology. 2020; 57:100820. [DOI: 10.1016/j.yfrne.2020.100820]
- Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: A systematic review. Bulletin of The World Health Organization. 2012; 90(2):139G-49G. [DOI:10.2471/blt.11.091850]
- Dong Y, Chi X, Hai H, Sun L, Zhang M, Xie WF, et al. Antibodies in the breast milk of a maternal woman with COVID-19. Emerging Microbes & Infections. 2020; 9(1):1467-9. [DOI:10.1080/22221751.2020.1780952]
- Mocelin HJ, Primo CC, Laignier MR. Overview on the recommendations for breastfeeding and COVID-19. Journal of Human Growth and Development. 2020; 30(3):335-43. [Link]
- Cohen SS, Alexander DD, Krebs NF, Young BE, Cabana MD, Erdmann P, et al. Factors associated with breastfeeding initiation and continuation: A meta-analysis. The Journal of Pediatrics. 2018; 203:190-6. [DOI:10.1016/j.jpeds.2018.08.008]
- Alzaheb RA. A review of the factors associated with the timely initiation of breastfeeding and exclusive breastfeeding in the Middle East. Clinical Medicine Insights: Pediatrics. 2017; 11. [DOI:10.1177/1179556517748912]
- Piankusol C, Sirikul W, Ongprasert K, Siviroj P. Factors affecting breastfeeding practices under lockdown during the COVID-19 pandemic in Thailand: A cross-sectional survey. International Journal of Environmental Research and Public Health. 2021; 18(16):8729. [DOI:10.3390/ijerph18168729]
- Murad A, Renfrew MJ, Symon A, Whitford H. Understanding factors affecting breastfeeding practices in one city in the Kingdom of Saudi Arabia: An interpretative phenomenological study. International Breastfeeding Journal. 2021; 16(1):1-9. [DOI:10.1186/s13006-020-00350-4]
- World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: Interim guidance.Geneva: World Health Organization; 2020. [DOI:10.15557/pimr.2020.0003]
- Patterson B, Marks M, Martinez-Garcia G, Bidwell G, Luintel A, Ludwig D, et al. A novel cohorting and isolation strategy for suspected COVID-19 cases during a pandemic. Journal of Hospital Infection. 2020; 105(4):632-7. [DOI:10.1016/j.jhin.2020.05.035]
- Giuliani C, Volsi PL, Brun E, Chiambretti A, Giandalia A, Tonutti L, et al. Breastfeeding during the COVID-19 pandemic: Suggestions on behalf of woman study group of AMD. Diabetes Research and Clinical Practice. 2020; 165:108239. [DOI:10.1016/j.diabres.2020.108239]
- Kucirka LM, Norton A, Sheffield JS. Severity of COVID‐19 in pregnancy: A review of current evidence. American Journal of Reproductive Immunology. 2020; 84(5):e13332. [DOI:10.1111/aji.13332]
- Liu W, Wang J, Li W, Zhou Z, Liu S, Rong Z. Clinical characteristics of 19 neonates born to mothers with COVID-19. Frontiers of Medicine. 2020; 14(2):193-8. [DOI:10.1007/s11684-020-0772-y]
- Salvatori G, De Rose DU, Concato C, Alario D, Olivini N, Dotta A, et al. Managing COVID-19-positive maternal-infant dyads: an Italian experience. Breastfeeding Medicine. 2020; 15(5):347-8. [DOI:10.1089/bfm.2020.0095]
- Bhatt H. Should COVID-19 mother breastfeed her newborn child? A literature review on the safety of breastfeeding for pregnant women with COVID-19. Current Nutrition Reports, 2021. 10(1):71-5. [DOI:10.1007/s13668-020-00343-z]
- Kumar S, Rathore P, Shweta, Krishnapriya V, Haokip N, Thankachan A, et al. Why I can’t breastfeed my new-born baby? Psychosocial dilemma of a COVID-positive post-LSCS mother. Indian Journal of Palliative Care. 2020; 26(Suppl 1):S150-2. [DOI:10.4103/ijpc.ijpc_157_2]
- Oncel MY, Akın IM, Kanburoglu MK, Tayman C, Coskun S, Narter F, et al. A multicenter study on epidemiological and clinical characteristics of 125 newborns born to women infected with COVID-19 by Turkish Neonatal Society. European Journal of Pediatrics. 2021; 180(3):733-42. [DOI:10.1007/s00431-020-03767-5]
- Del Ciampo LA, Del Ciampo IRL. Breastfeeding and the benefits of lactation for women’s health. Revista Brasileira de Ginecologia e Obstetrícia. 2018; 40(6):354-9.[DOI:10.1055/s-0038-1657766]
- Olza I, Uvnas-Moberg K, Ekström-Bergström A, Leahy-Warren P, Karlsdottir SI, Nieuwenhuijze M, et al. Birth as a neuro-psycho-social event: An integrative model of maternal experiences and their relation to neurohormonal events during childbirth. Plos One. 2020; 15(7):e0230992. [DOI:10.1371/journal.pone.0230992]
- Zhang P, Salafia C, Heyman T, Salafia C, Lederman S, Dygulska B. Detection of severe acute respiratory syndrome coronavirus 2 in placentas with pathology and vertical transmission. American Journal of Obstetrics & Gynecology MFM. 2020; 2(4):100197. [DOI:10.1016/j.ajogmf.2020.100197]
- Dimopoulou D, Triantafyllidou P, Daskalaki A, Syridou G, Papaevangelou V. Breastfeeding during the novel coronavirus (COVID-19) pandemic: Guidelines and challenges. The Journal of Maternal-Fetal & Neonatal Medicine. 2022; 35(19):3776-82. [DOI:10.1080/14767058.2020.1838481]
Type of Study: Review Article |
Subject:
● Disease Control
Received: 2023/02/1 | Accepted: 2023/07/4 | Published: 2024/02/1
Received: 2023/02/1 | Accepted: 2023/07/4 | Published: 2024/02/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |