Volume 13, Issue 6 (Nov & Dec 2023)
J Research Health 2023, 13(6): 457-466 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pranata S, Vivienne Wu S, Armiyati Y, Khoiriyah K, Shing L C, Liu J. Implementing Precision Health Care Program at Hospitals in Indonesia. J Research Health 2023; 13 (6) :457-466
URL: http://jrh.gmu.ac.ir/article-1-2318-en.html
URL: http://jrh.gmu.ac.ir/article-1-2318-en.html
Satriya Pranata1 

 , Shu-Fang Vivienne Wu2
, Shu-Fang Vivienne Wu2 

 , Yunie Armiyati3
, Yunie Armiyati3 

 , Khoiriyah Khoiriyah3
, Khoiriyah Khoiriyah3 

 , Lin Chun Shing4
, Lin Chun Shing4 

 , Ju-Han Liu2
, Ju-Han Liu2 




 , Shu-Fang Vivienne Wu2
, Shu-Fang Vivienne Wu2 

 , Yunie Armiyati3
, Yunie Armiyati3 

 , Khoiriyah Khoiriyah3
, Khoiriyah Khoiriyah3 

 , Lin Chun Shing4
, Lin Chun Shing4 

 , Ju-Han Liu2
, Ju-Han Liu2 


1- Department of Nursing, Faculty of Nursing and Health Sciences, Muhammadiyah University of Semarang, Central Java, Indonesia. , satriya.pranata@unimus.ac.id
2- School of Nursing, National Taipei, University of Nursing and Health Sciences, Taipei, Taiwan.
3- Department of Nursing, Faculty of Nursing and Health Sciences, Muhammadiyah University of Semarang, Central Java, Indonesia.
4- Veteran General Hospital, Taipei, Taiwan.
2- School of Nursing, National Taipei, University of Nursing and Health Sciences, Taipei, Taiwan.
3- Department of Nursing, Faculty of Nursing and Health Sciences, Muhammadiyah University of Semarang, Central Java, Indonesia.
4- Veteran General Hospital, Taipei, Taiwan.
Full-Text [PDF 643 kb]
(394 Downloads)
| Abstract (HTML) (2092 Views)
Data collection
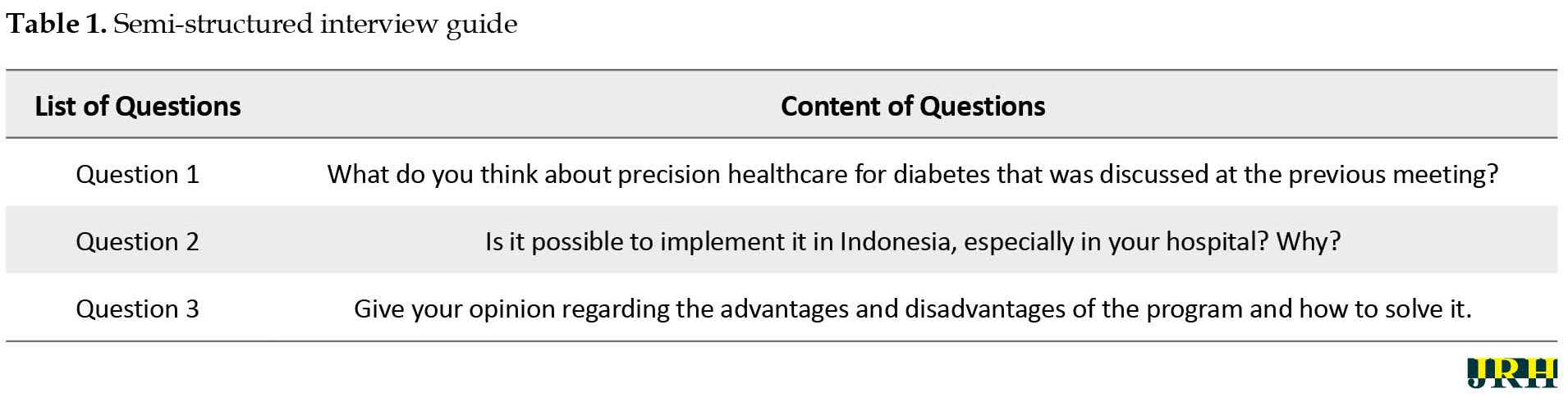
After receiving the consent form, the researcher asked the participants to describe their experiences related to health professionals’ and policymakers’ perceptions about the possibility of implementing a precision healthcare program in hospitals in Indonesia. The perceptions were explored by deep, semi-structured interviews with several broad questions presented in Table 1.
Probing questions were also prepared to encourage the participants to give more information about their experiences, such as “can you tell me more about that?” Interviews lasted 20 to 30 min and were digitally recorded and transcribed precisely.
Data analysis
The researcher analyzed the interview results according to the Colaizzi phenomenological analytic method. It consists of 7 steps, as follows: 1) Read all protocols to acquire a feeling for them; 2) Review each protocol and extract significant statements; 3) Spell out the meaning of each significant statement; 4) Organize the formulated meanings into clusters of themes; 5) Integrate results into an exhaustive description of the phenomenon under study; 6) Formulate an exhaustive description of the phenomenon under study in as unequivocal a statement of identification as possible; 7) Ask participants about the findings thus far as a final validating step [15].
The interviews were transcribed verbatim by the principal investigator. The researchers then read the results several times to find significant phrases and grouped them into themes. Subsequently, the findings were then incorporated into a comprehensive, in-depth account of the phenomena. Following the collection of descriptions and themes, some participants were approached for a second time by interview to confirm the findings. The additional information was then incorporated into the final description. The following four criteria were used to ensure the accuracy of the data: Credibility, dependency, conformability, and transferability. The principal investigator discussed the themes and subthemes, during which their opinions conflicted until they agreed.
3. Results
Three themes were identified to illustrate health professionals’ and policymakers’ perceptions about possibly implementing precision healthcare programs in Indonesia’s hospitals. These themes were: 1) Precision health care for diabetes related to genetics, big data, and patient preference; 2) Barriers to implementing precision health care in Indonesian hospitals; 3) The implementation of precision health care can be succeeded step by step.
Precision health care for diabetes-related with genetic, big data and patient preference
The precision healthcare concept is composed of essential elements. These elements are complementary to the concept. Established elements in precision health care are genetics, big data analysis, and patient preferences. These components are the primary basis for determining the best personalized intervention for each patient. Each person has a different analysis, and the elements will show it. The theme was divided into several sub-themes as follows: 1) Precision health care related to genetic information; 2) Precision health care related to big data information; 3) Precision health care related to patient preference.
Precision health care related with genetic information
“According to the discussion and presentation of the presenters, precision health care focuses on genetics to determine appropriate interventions for diabetic patients” (Respondent 8).
“I see that genetics will play an essential role in determining the best intervention for diabetic patients” (Respondent 2).
“Genetics is very expensive; we do not know when we can use genetic testing in clinical decisions” (Respondent 7).
“I am unsure and still doubt how we can make health professionals, especially nurses, understand genetic analysis. Of course, it needs to be strengthened at the university first to produce nurses who are experts in the field of genetics” (Respondent 1).
Precision health care related with big data information
“Big data allows us to leverage large sample sizes to generate statistically significant findings that may be clinically irrelevant. The National Institutes of Health’s big data to knowledge initiative acknowledges insufficient training in developing and using methods and tools needed to analyze big data as a major impediment to maximizing the value of the growing volume and complexity of data available” (Respondent 16).
“Big data is extraordinary. Imagine if we can collect so much data, then we determine the conclusions from each data to be clustered into a picture of the results. It will be interesting and very accurate” (Respondent 13).
I do not know when we will start big data analysis. I know that other countries have started, but as far as I know, we have not started clearly. Maybe the data on national insurance can be included in big data analysis in the future; I’m not sure about that” (Respondent 5).
Many tools use big data to determine a person’s health. Just look at a smartphone or smartwatch; these devices can interpret our condition by calculating the data they get, whether it be blood pressure, pulse, sleep cycle, etc.” (Respondent 16).
“How can we ensure the security of patient data if big data already exists? I am still worried because hackers can access a lot of data, but we haven’t been able to protect it. Imagine that people’s data can be accessed by hackers and how dangerous it is” (Respondent 10).
“Big data analytical applications have great potential to improve the quality of healthcare services” (Respondent 2).
Precision health care with patient preference
“Whatever the result, whatever we decide from data calculations through big data and genetic approaches, the decision is still in the hands of patients. We cannot force them to decide, give them the freedom” (Respondent 9).
“I believe we should respect the decisions of diabetic patients in determining the best intervention for them, but what if the patient does not have sufficient knowledge? They need basic information first, then they can make the best decision themselves” (Respondent 6).
“Data collection regarding genetics is also important, but of course, the decision is in the hands of the patient; we must respect every opinion of patients” (Respondent 4).
Barriers to implementing precision health care in Indonesian hospitals
In implementing precision health care, various obstacles are predicted to be found, especially in hospitals in Indonesia. Respondents analyzed this constraint due to various factors, namely the availability of facilities, the costs incurred, and the development of supporting human resources. The themes related to barriers to implementing this concept were divided into several sub-themes as follows: 1) Nurses did not have an active role in genetics; 2) The lack of knowledge on genetics and considerable data interpretation; 3) The lack of demand for nursing services in personalized care; 4) Restricted time; 5) Economic limitations.
Nurses and other health professionals with no active role in genetics
“There was no single health professional in our hospital who has the competence in genetic analysis, be it a doctor or a nurse” (Respondent 15).
“Is genetic analysis taught at university? Recently, I do not think nurses have the competence for genetic analysis” (Respondent 10).
“Until now, in colleges and nursing organizations, there has been no discussion regarding the role of nurses in genetic analysis competence” (Respondent 9).
“I am confused about what role we can take in applying patient genetic analysis” (Respondent 17).
“Nurses must be able to analyze a person’s genetics and further provide education based on patient data to make decisions about the best medication or therapy for the patient. But until now, nurses do not have the competence for this, and there is no significant role for nurses to charge in these competencies” (Respondent 8).
Lack of knowledge related with genetic and big data interpretation
“Even if you ask me about genetics, I will only be able to explain the basics, not fully understand the concept” (Respondent 5).
“I saw the interpretation of the data in overseas hospitals based on the standard equipment they had set and then trained the staff for interpretation. There is no training here regarding these competencies” (Respondent 1).
“So far, we have used family trees to detect a person’s potential for genetic disease, but I do not think that is useful. It requires deep understanding, and we have never studied in depth about it” (Respondent 6).
“How to interpret big data? I see health professionals get in-depth training, but we have not been programmed to do such training” (Respondent 13).
Lack of demand for nursing services in personalized care
“So far, we are still using the population approach, not focusing on the personal approach” (Respondent 12).
“Patients cannot determine the best treatment and management for their health, so personalized care cannot be fully implemented in our hospital” (Respondent 2).
“I think personalized care is necessary for patients because we respect their preferences, but can patients determine their preferences? I am not sure” (Respondent 14).
“Personalized care has not been regulated in a regulation so that remuneration in the form of awards and fees is not yet available. This may be an obstacle in implementing this approach in hospitals” (Respondent 5).
Restricted time
“In the past, health professionals, especially doctors, could provide services to patients briefly; in the future, services will focus more on individuals, so it may take longer to analyze each patient” (Respondent 3).
“We will need time to go through the details of each examination to make the right decision for each patient. Will all of them help big data analysis with artificial intelligence? I’m not sure” (Respondent 1).
“Perhaps artificial intelligence will make precision healthcare approaches faster and more accurate, but there are too many things that cannot be considered for artificial intelligence. We are dealing with humans, where a wiser decision is also needed. Artificial intelligence probably will not accommodate these situations” (Respondent 4).
Economic limitation
“How much money do we have to spend to start preparing systems and equipment to support big data analysis and genetic assessment? It will be huge” (Respondent 15).
“It will cost a lot of money to train health professionals and even send them to school or provide training for health professionals to become experts in precision medicine and precision health care” (Respondent 3).
“Will health insurance cover this service? Many important checks up to now are sometimes not covered by health insurance, let alone genetic tests?” (Respondent 7).
“Maybe only people with a good economy can cover this service in the future. I am not sure if this program will be able to run shortly. It took a lot of time to make this program successful” (Respondent 10).
The implementation of precision health care succeeded step by step
The new concept of precision health care among health professionals makes its application take time and process. The stages of applying the concept of precision health care were analyzed based on the experience and considerations of the respondents recruited in the study process. Precision healthcare was divided into several subthemes as follows: 1) Focus on educating nurses to be competent in genetic and considerable data interpretation; 2) Nurses need to understand patient needs and make decision-making based on patient preferences; 3) The service should be covered by national health insurance; 4) The existence of a precision health care approach must be included in hospital accreditation standards.
Focus on educating health professionals to be competent in genetic and big data interpretation
“Nurses and other health professionals will ultimately be liable for failing to incorporate genetic/genomic and big data discoveries into practice. There were no nurses who could do big data and genome analysis; there may be a need for special nurse specialties in informatics and big data analysis. That is why data analysis for genetic and big data is needed in hospitals to help health professionals make clinical decisions” (Respondent 16).
“What are the criteria for nurses who can develop genetic analysis and big data interpretation? Does he have to be an expert in internet technology or something? Of course, everything must be prepared carefully since they are studying at the university” (Respondent 5).
“If we are going to provide training, then who will provide training for nurses in Indonesia? Currently, the new experts may come from experts in the field of internet technology for big data, not nurses. This will also be a problem because experts in other fields do not necessarily understand how health professionals interpret health data in detail” (Respondent 7).
“Big data interpretation will be faster if using smart technology, such as artificial intelligence, but all of this has not been structured in the education of nurses or other health professionals. It is necessary to develop a new department for that. I believe it is necessary and important to do this now” (Respondent 4).
“Education on genetics has not been discussed in detail and clearly in universities. There is also no clear curriculum for genetic analysis, especially for nurses. We should think about curriculum preparation first so that the competencies of nurses and other health professionals we want are available for work in hospitals” (Respondent 17).
“It takes quite a long time to make nurses understand well the workings and interpretation of genetics and big data analysis in clinical practice” (Respondent 10).
Nurse needs to understand patient needs and make decision making based on patient preferences
“Patients and their families seem resigned to whatever choices and decisions are made by health professionals. There is still little decision-making done by patients and their families independently; it might be related to literacy and knowledge” (Respondent 6).
“The patient’s opinion must be prioritized; they have the independence to determine the best intervention. Ideally, it would be like that, but it cannot be done optimally in the hospital. Health professionals should think about the basic knowledge of patients and families first. Further, the independence of the patient and family will be improved” (Respondent 11).
“The needs of patients and families are basic knowledge about the disease and the various therapeutic options they will receive” (Respondent 16).
“Before the patient makes the best choice for himself, he should have been exposed to information about the choice of therapy” (Respondent 7).
Service should be covered by national health insurance
“Personalized care approach will certainly be expensive. In Indonesia, if health programs are not covered by health insurance, it will be difficult to run the program” (Respondent 10).
“Health insurance plays an essential role in Indonesian health services. Many hospitals have not cooperated with health insurance in the beginning, and as a result, people have not been interested in those hospital services. The patient did not come there. Likewise, the precision health care approach program, if we hope diabetic patients will use this program, it must be covered by health insurance first” (Respondent 17).
“I cannot imagine how much the cost for genetic testing and procurement of tools to support big data analysis. If everything is covered by health insurance, maybe it will be possible in the future” (Respondent 3).
“In-depth analysis of needs and a prior evaluation of the success of a personal approach are needed. We can learn from other countries. Suppose it is proven that this approach can reduce the number of complications of diabetes patients in the future. In that case, this should be interesting and maybe will be covered by the government through national health insurance” (Respondent 8).
Existence of a precision health care approach must be included in hospital accreditation standards
“In the past, before the implementation of educational standards for health professionals, nurses in hospitals were reluctant to take further studies. Now that education standards have been included in hospital accreditation standards, many health professionals want to improve their education level—likewise, precision healthcare programs it is included in hospital accreditation standards. Of course, the hospital will exert efforts to make the program successful in the future” (Respondent 5).
“If many countries have successfully implemented a precision health care approach program and succeeded significantly in reducing the risk of complications due to diabetes in the future. I am sure this new approach will be included in hospital accreditation standards” (Respondent 14).
“If it is already included in the accreditation, the hospital will inevitably adopt this approach. That could be one of the strategies that this program will be able to run in the future in the healthcare setting” (Respondent 15).
4. Discussion
The results of in-depth interviews with respondents demonstrated that precision health care focuses more on genetic elements, big data, and patient preference. Nurses must be competent to obtain comprehensive family histories, identify family members at risk of developing a genomic-influenced condition, and for genomic-influenced drug reactions, assist people in making informed decisions about and understanding the results of their genetic/genomic tests and therapies, and refer at-risk people to appropriate health care professionals and agencies for specialized care [17, 18, 19]. Moreover, understanding big data is a priority for nurse leaders as we aim to provide the best possible care to patients [20, 21]. The big data challenge is made more difficult by working with healthcare companies with complex information technology and networks with numerous clinical, financial, and claim systems that must be integrated [22, 23]. Integrating and analyzing disparate data to better understand outcomes is not straightforward [24]. Access to the correct information at the right time to support clinical decisions is essential in planning and providing patient care [20]. All clinicians require real-time information to make fast, crucial clinical choices [25, 26]. Big data technologies can assist nurses and other healthcare professionals in enhancing patient care, maximizing results, and lowering healthcare costs [20–23]. Additionally, by respecting patient preferences, we can improve outpatient care decisions through enhanced support systems that give care suggestions priority and better communication of information about treatments with diabetic patients [12, 27]. For instance, by considering the full person, including the complex interplay of comorbid conditions, psychosocial and functional status, and individual needs in clinical practice, patient conditions can be addressed [13].
The data show that various obstacles are predicted to be found, especially in hospitals in Indonesia, due to multiple factors, namely the availability of facilities, the costs incurred, and the development of supporting human resources [28]. It was related to a study that mentioned that when that data of details is adequately assembled, integrated, and analyzed, it will offer substantial new potential at two levels: The individual and the population as a whole [20, 24, 29]. We can identify trends and interactions once all relevant data has been tracked and analyzed, which no system or software could do individually [20]. However, to do so, we must also safeguard the data’s security and privacy, and we need analytic to gather useful information [30, 31]. Changes in healthcare stakeholders’ perspectives are also necessary to accommodate this iterative flow of personal data. For instance, patients, customers, and physicians must be willing to trust and learn from user-generated data. This requires personal and analytical evolution [21, 32]. Additionally, graduate-level nurses should be able to gather a precise family history, understand how to apply genetics to patient diagnosis, treatment, and care, and know the best ways to communicate this information to patients and families. These skills require additional work, time, and cost [20, 33]. Given the accessibility of direct-to-consumer genetic testing, nurses must develop their skills in reading, interpreting, and advising patients about their genetic profiles. As integral members of interdisciplinary teams, nurses working in clinical settings must be prepared to deal with these issues and support informed decision-making that may affect healthcare decisions [18, 34]. When delivering individualized care to patients from diverse origins and responding to genetic profiles and healthcare options inquiries, it is essential to consider cultural attitudes and views toward genomics [20, 35–37].
Health professionals in this study believe that the implementation of precision health care can succeed step by step. Those were analyzed based on their experience. Existing approaches to extensive data set analysis provide a necessary but insufficient foundation for nursing to participate in the precision healthcare revolution [20]. Through precision health care, the social policy statement of nursing guides a principled, ethical perspective on big data and data science [24, 30, 38]. There are implications for practicing basic and advanced practice clinical nurses, nurse scientists collaborating with data scientists, and nurse data scientists. Nursing’s inquiry traditions, which rely on electronic health records, claims data exploration, or public health data sets, provide a solid foundation for thinking about data science [23, 39]. Notably, nursing must use all familiar and emerging methods to generate nursing knowledge [23, 38, 40]. It is beneficial to connect what we must do in the future to what we have accomplished in the past. Nurse scientists are utilizing the opportunities provided by big data and data science in novel ways. For decades, nurse scientists have worked in interdisciplinary teams to apply some of the mining and modeling techniques now associated with big data and data science to phenomena central to nursing and health via precision health care [23, 40, 41]. Therefore, despite many obstacles and steps we must go through in this initial phase, a precision healthcare approach can provide greater richness in understanding patient phenomena and tailoring interventional strategies personalized to the patient [20].
5. Conclusion
More time is needed to implement the precision healthcare concept in Indonesia. Many things can be prepared in advance, especially in preparing human resources for health professionals through education at universities, strengthening national organizations’ regulation and the costs of procuring genetic tests and big data analysis. Necessarily, it takes time, but applying the concept has great potential to be developed in reducing the risk of complications caused by diabetes mellitus in the future.
Ethical Considerations
Compliance with ethical guidelines
The current study was approved by the Health Research Ethics Committee STIKES Bina Usada Bali (Code: 267/EA/KEPK-BUB-2022). The participants provided written informed consent to take part in this study.
Funding
This study was financially supported by the Universitas Muhammadiyah Semarang.
Authors' contributions
Conceptualization and supervision: Satriya Pranata and Shu-Fang Vivienne Wu; Methodology: Yunie Armiyati and Khoiriyah Khoiriyah; Investigation, writing original draft, review and editing: Satriya Pranata and Ju-Han Liu; Data analysis: Lin Chun Shing and Satriya Pranata; Data collection: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Universitas Muhammadiyah Semarang for funding support.
References
Full-Text: (376 Views)
1. Introduction
In 2019, diabetes in Indonesia reached 10.7 million cases. In Southeast Asia, Indonesia ranks third with the highest prevalence of diabetes, with a prevalence of 11.3%. By 2030, the number will reach 13.7 million and then to 16.9 million in 2045 [1]. Moreover, people with diabetes are 2 to 3 times more likely to have cardiovascular disease and up to 10 times more likely to have end-stage renal disease, amputation, cognitive impairments, and central nervous system macro and micro pathologies [2].
The increasing number of patients with diabetes and complications requires health professionals to continue to improve health service programs by taking promotive, preventive steps with meal planning, counseling, and health education [3, 4]. Those programs have been based on evidence-based practice and guidelines of diabetes care for a long time [5]; however, a personalized approach has not been applied.
The education must be tailor-made. It must be tuned into the individual patient’s needs (social–cognitive determinants, intention, and behavior) [6, 7]. In recent years, research efforts in this direction have been labeled “precision medicine,” becoming a new trend in clinical settings. Precision medicine is a new medical mode for deep understanding of the patient’s genetic and genomic information to realize disease prediction and make effective prevention, diagnosis, and treatment [8]. On the other hand, patient care and preference, patient-oriented, personalized approach, evidence-based care, and self-management refer to precision health care [9, 10, 11].
Several hospitals have successfully implemented precision healthcare programs that recognize various aspects, including patients’ preferences, evidence-based practices, big data, genome technology, and personal goals in the healthcare system over the past five years. A precision healthcare approach is needed in the context of the Indonesian healthcare system, especially as an effort to improve the self-management activities of diabetes patients. Moreover, health professionals, namely doctors, nurses, and nutritionists, believe that precision care will be the solution to reduce the risk of CVD complications in diabetic patients because precision health care can improve self-management among patients with diabetes through glycemic control [12, 13]. Accordingly, this study explores the perception of the possibility of implementing precision healthcare programs in hospitals in Indonesia through interviews with policymakers and health professionals in Indonesia.
2. Methods
Study design
Qualitative research explores unknown areas of knowledge, and phenomenology investigates the meaning of phenomena from the individual’s perspective [14]. The cases objectively described the phenomena and obtained the truth of matters in the broadest sense [15, 16]. The focus of this study was to understand the perception of health professionals and policymakers about the possibility of implementing precision healthcare programs in hospitals in Indonesia.
Settings and participants
The researcher recruited participants using a purposive sampling method in Indonesia. The data saturation was achieved after interviewing 17 policymakers and health professionals in the hospitals. Before conducting the interviews, the participants who wished to participate in the focus group discussed with experts from hospitals (Taipei veteran general hospitals) and universities (National Taipei University of Nursing and Health Sciences) who succeeded in implementing precision health care in their country. Experts from Taipei Veteran General Hospitals and the National Taipei University of Nursing and Health Sciences present all the programs from their hospitals and universities to health professionals in Indonesia. Further, policymakers and health professionals in Indonesia discussed the possibility of the program being implemented in Indonesia and the challenges to implementing the program and discovering solutions. Policymakers were recruited because they determined policies in hospitals, while health professionals are individuals who understand the basic needs of diabetic patients. These respondents were recruited to align the policies with the patient’s needs in the clinical service.
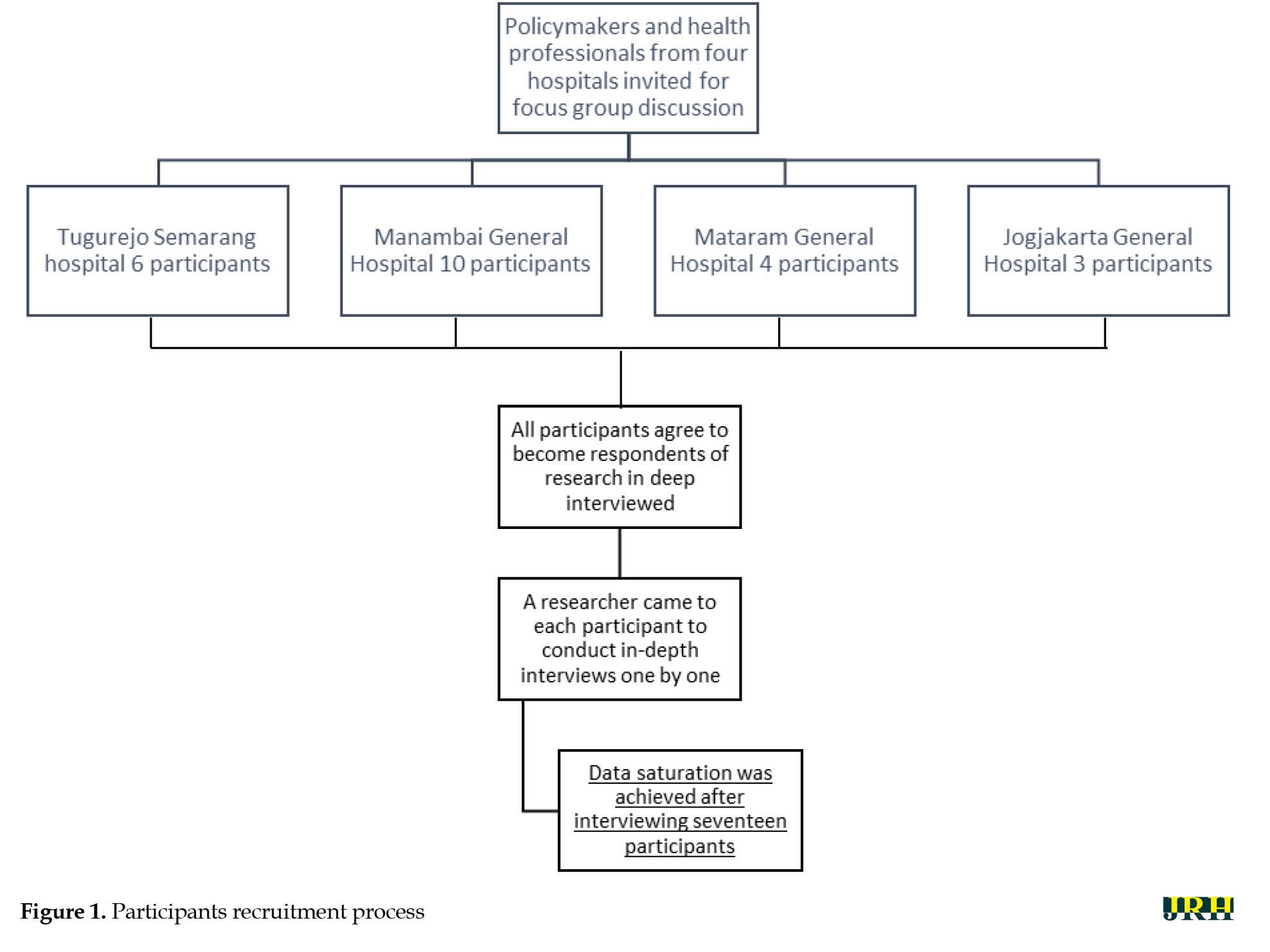
The eligibility criteria were set for selecting the participants, such as policymakers and health professionals from Tugurejo Semarang Hospital, Manambai General Hospital, Mataram General Hospital, and Jogjakarta General Hospital who were willing to participate in the focus group discussion and the research, provided signed the informed consent form, were willing to express their feelings and thoughts, and shared their experiences via an in-depth interview. On the other hand, respondents who refused to focus group discussions and interviews and were unwilling to participate in the study were excluded. The recruitment process is explained in Figure 1.
In 2019, diabetes in Indonesia reached 10.7 million cases. In Southeast Asia, Indonesia ranks third with the highest prevalence of diabetes, with a prevalence of 11.3%. By 2030, the number will reach 13.7 million and then to 16.9 million in 2045 [1]. Moreover, people with diabetes are 2 to 3 times more likely to have cardiovascular disease and up to 10 times more likely to have end-stage renal disease, amputation, cognitive impairments, and central nervous system macro and micro pathologies [2].
The increasing number of patients with diabetes and complications requires health professionals to continue to improve health service programs by taking promotive, preventive steps with meal planning, counseling, and health education [3, 4]. Those programs have been based on evidence-based practice and guidelines of diabetes care for a long time [5]; however, a personalized approach has not been applied.
The education must be tailor-made. It must be tuned into the individual patient’s needs (social–cognitive determinants, intention, and behavior) [6, 7]. In recent years, research efforts in this direction have been labeled “precision medicine,” becoming a new trend in clinical settings. Precision medicine is a new medical mode for deep understanding of the patient’s genetic and genomic information to realize disease prediction and make effective prevention, diagnosis, and treatment [8]. On the other hand, patient care and preference, patient-oriented, personalized approach, evidence-based care, and self-management refer to precision health care [9, 10, 11].
Several hospitals have successfully implemented precision healthcare programs that recognize various aspects, including patients’ preferences, evidence-based practices, big data, genome technology, and personal goals in the healthcare system over the past five years. A precision healthcare approach is needed in the context of the Indonesian healthcare system, especially as an effort to improve the self-management activities of diabetes patients. Moreover, health professionals, namely doctors, nurses, and nutritionists, believe that precision care will be the solution to reduce the risk of CVD complications in diabetic patients because precision health care can improve self-management among patients with diabetes through glycemic control [12, 13]. Accordingly, this study explores the perception of the possibility of implementing precision healthcare programs in hospitals in Indonesia through interviews with policymakers and health professionals in Indonesia.
2. Methods
Study design
Qualitative research explores unknown areas of knowledge, and phenomenology investigates the meaning of phenomena from the individual’s perspective [14]. The cases objectively described the phenomena and obtained the truth of matters in the broadest sense [15, 16]. The focus of this study was to understand the perception of health professionals and policymakers about the possibility of implementing precision healthcare programs in hospitals in Indonesia.
Settings and participants
The researcher recruited participants using a purposive sampling method in Indonesia. The data saturation was achieved after interviewing 17 policymakers and health professionals in the hospitals. Before conducting the interviews, the participants who wished to participate in the focus group discussed with experts from hospitals (Taipei veteran general hospitals) and universities (National Taipei University of Nursing and Health Sciences) who succeeded in implementing precision health care in their country. Experts from Taipei Veteran General Hospitals and the National Taipei University of Nursing and Health Sciences present all the programs from their hospitals and universities to health professionals in Indonesia. Further, policymakers and health professionals in Indonesia discussed the possibility of the program being implemented in Indonesia and the challenges to implementing the program and discovering solutions. Policymakers were recruited because they determined policies in hospitals, while health professionals are individuals who understand the basic needs of diabetic patients. These respondents were recruited to align the policies with the patient’s needs in the clinical service.
The eligibility criteria were set for selecting the participants, such as policymakers and health professionals from Tugurejo Semarang Hospital, Manambai General Hospital, Mataram General Hospital, and Jogjakarta General Hospital who were willing to participate in the focus group discussion and the research, provided signed the informed consent form, were willing to express their feelings and thoughts, and shared their experiences via an in-depth interview. On the other hand, respondents who refused to focus group discussions and interviews and were unwilling to participate in the study were excluded. The recruitment process is explained in Figure 1.
Data collection
After receiving the consent form, the researcher asked the participants to describe their experiences related to health professionals’ and policymakers’ perceptions about the possibility of implementing a precision healthcare program in hospitals in Indonesia. The perceptions were explored by deep, semi-structured interviews with several broad questions presented in Table 1.
Probing questions were also prepared to encourage the participants to give more information about their experiences, such as “can you tell me more about that?” Interviews lasted 20 to 30 min and were digitally recorded and transcribed precisely.
Data analysis
The researcher analyzed the interview results according to the Colaizzi phenomenological analytic method. It consists of 7 steps, as follows: 1) Read all protocols to acquire a feeling for them; 2) Review each protocol and extract significant statements; 3) Spell out the meaning of each significant statement; 4) Organize the formulated meanings into clusters of themes; 5) Integrate results into an exhaustive description of the phenomenon under study; 6) Formulate an exhaustive description of the phenomenon under study in as unequivocal a statement of identification as possible; 7) Ask participants about the findings thus far as a final validating step [15].
The interviews were transcribed verbatim by the principal investigator. The researchers then read the results several times to find significant phrases and grouped them into themes. Subsequently, the findings were then incorporated into a comprehensive, in-depth account of the phenomena. Following the collection of descriptions and themes, some participants were approached for a second time by interview to confirm the findings. The additional information was then incorporated into the final description. The following four criteria were used to ensure the accuracy of the data: Credibility, dependency, conformability, and transferability. The principal investigator discussed the themes and subthemes, during which their opinions conflicted until they agreed.
3. Results
Three themes were identified to illustrate health professionals’ and policymakers’ perceptions about possibly implementing precision healthcare programs in Indonesia’s hospitals. These themes were: 1) Precision health care for diabetes related to genetics, big data, and patient preference; 2) Barriers to implementing precision health care in Indonesian hospitals; 3) The implementation of precision health care can be succeeded step by step.
Precision health care for diabetes-related with genetic, big data and patient preference
The precision healthcare concept is composed of essential elements. These elements are complementary to the concept. Established elements in precision health care are genetics, big data analysis, and patient preferences. These components are the primary basis for determining the best personalized intervention for each patient. Each person has a different analysis, and the elements will show it. The theme was divided into several sub-themes as follows: 1) Precision health care related to genetic information; 2) Precision health care related to big data information; 3) Precision health care related to patient preference.
Precision health care related with genetic information
“According to the discussion and presentation of the presenters, precision health care focuses on genetics to determine appropriate interventions for diabetic patients” (Respondent 8).
“I see that genetics will play an essential role in determining the best intervention for diabetic patients” (Respondent 2).
“Genetics is very expensive; we do not know when we can use genetic testing in clinical decisions” (Respondent 7).
“I am unsure and still doubt how we can make health professionals, especially nurses, understand genetic analysis. Of course, it needs to be strengthened at the university first to produce nurses who are experts in the field of genetics” (Respondent 1).
Precision health care related with big data information
“Big data allows us to leverage large sample sizes to generate statistically significant findings that may be clinically irrelevant. The National Institutes of Health’s big data to knowledge initiative acknowledges insufficient training in developing and using methods and tools needed to analyze big data as a major impediment to maximizing the value of the growing volume and complexity of data available” (Respondent 16).
“Big data is extraordinary. Imagine if we can collect so much data, then we determine the conclusions from each data to be clustered into a picture of the results. It will be interesting and very accurate” (Respondent 13).
I do not know when we will start big data analysis. I know that other countries have started, but as far as I know, we have not started clearly. Maybe the data on national insurance can be included in big data analysis in the future; I’m not sure about that” (Respondent 5).
Many tools use big data to determine a person’s health. Just look at a smartphone or smartwatch; these devices can interpret our condition by calculating the data they get, whether it be blood pressure, pulse, sleep cycle, etc.” (Respondent 16).
“How can we ensure the security of patient data if big data already exists? I am still worried because hackers can access a lot of data, but we haven’t been able to protect it. Imagine that people’s data can be accessed by hackers and how dangerous it is” (Respondent 10).
“Big data analytical applications have great potential to improve the quality of healthcare services” (Respondent 2).
Precision health care with patient preference
“Whatever the result, whatever we decide from data calculations through big data and genetic approaches, the decision is still in the hands of patients. We cannot force them to decide, give them the freedom” (Respondent 9).
“I believe we should respect the decisions of diabetic patients in determining the best intervention for them, but what if the patient does not have sufficient knowledge? They need basic information first, then they can make the best decision themselves” (Respondent 6).
“Data collection regarding genetics is also important, but of course, the decision is in the hands of the patient; we must respect every opinion of patients” (Respondent 4).
Barriers to implementing precision health care in Indonesian hospitals
In implementing precision health care, various obstacles are predicted to be found, especially in hospitals in Indonesia. Respondents analyzed this constraint due to various factors, namely the availability of facilities, the costs incurred, and the development of supporting human resources. The themes related to barriers to implementing this concept were divided into several sub-themes as follows: 1) Nurses did not have an active role in genetics; 2) The lack of knowledge on genetics and considerable data interpretation; 3) The lack of demand for nursing services in personalized care; 4) Restricted time; 5) Economic limitations.
Nurses and other health professionals with no active role in genetics
“There was no single health professional in our hospital who has the competence in genetic analysis, be it a doctor or a nurse” (Respondent 15).
“Is genetic analysis taught at university? Recently, I do not think nurses have the competence for genetic analysis” (Respondent 10).
“Until now, in colleges and nursing organizations, there has been no discussion regarding the role of nurses in genetic analysis competence” (Respondent 9).
“I am confused about what role we can take in applying patient genetic analysis” (Respondent 17).
“Nurses must be able to analyze a person’s genetics and further provide education based on patient data to make decisions about the best medication or therapy for the patient. But until now, nurses do not have the competence for this, and there is no significant role for nurses to charge in these competencies” (Respondent 8).
Lack of knowledge related with genetic and big data interpretation
“Even if you ask me about genetics, I will only be able to explain the basics, not fully understand the concept” (Respondent 5).
“I saw the interpretation of the data in overseas hospitals based on the standard equipment they had set and then trained the staff for interpretation. There is no training here regarding these competencies” (Respondent 1).
“So far, we have used family trees to detect a person’s potential for genetic disease, but I do not think that is useful. It requires deep understanding, and we have never studied in depth about it” (Respondent 6).
“How to interpret big data? I see health professionals get in-depth training, but we have not been programmed to do such training” (Respondent 13).
Lack of demand for nursing services in personalized care
“So far, we are still using the population approach, not focusing on the personal approach” (Respondent 12).
“Patients cannot determine the best treatment and management for their health, so personalized care cannot be fully implemented in our hospital” (Respondent 2).
“I think personalized care is necessary for patients because we respect their preferences, but can patients determine their preferences? I am not sure” (Respondent 14).
“Personalized care has not been regulated in a regulation so that remuneration in the form of awards and fees is not yet available. This may be an obstacle in implementing this approach in hospitals” (Respondent 5).
Restricted time
“In the past, health professionals, especially doctors, could provide services to patients briefly; in the future, services will focus more on individuals, so it may take longer to analyze each patient” (Respondent 3).
“We will need time to go through the details of each examination to make the right decision for each patient. Will all of them help big data analysis with artificial intelligence? I’m not sure” (Respondent 1).
“Perhaps artificial intelligence will make precision healthcare approaches faster and more accurate, but there are too many things that cannot be considered for artificial intelligence. We are dealing with humans, where a wiser decision is also needed. Artificial intelligence probably will not accommodate these situations” (Respondent 4).
Economic limitation
“How much money do we have to spend to start preparing systems and equipment to support big data analysis and genetic assessment? It will be huge” (Respondent 15).
“It will cost a lot of money to train health professionals and even send them to school or provide training for health professionals to become experts in precision medicine and precision health care” (Respondent 3).
“Will health insurance cover this service? Many important checks up to now are sometimes not covered by health insurance, let alone genetic tests?” (Respondent 7).
“Maybe only people with a good economy can cover this service in the future. I am not sure if this program will be able to run shortly. It took a lot of time to make this program successful” (Respondent 10).
The implementation of precision health care succeeded step by step
The new concept of precision health care among health professionals makes its application take time and process. The stages of applying the concept of precision health care were analyzed based on the experience and considerations of the respondents recruited in the study process. Precision healthcare was divided into several subthemes as follows: 1) Focus on educating nurses to be competent in genetic and considerable data interpretation; 2) Nurses need to understand patient needs and make decision-making based on patient preferences; 3) The service should be covered by national health insurance; 4) The existence of a precision health care approach must be included in hospital accreditation standards.
Focus on educating health professionals to be competent in genetic and big data interpretation
“Nurses and other health professionals will ultimately be liable for failing to incorporate genetic/genomic and big data discoveries into practice. There were no nurses who could do big data and genome analysis; there may be a need for special nurse specialties in informatics and big data analysis. That is why data analysis for genetic and big data is needed in hospitals to help health professionals make clinical decisions” (Respondent 16).
“What are the criteria for nurses who can develop genetic analysis and big data interpretation? Does he have to be an expert in internet technology or something? Of course, everything must be prepared carefully since they are studying at the university” (Respondent 5).
“If we are going to provide training, then who will provide training for nurses in Indonesia? Currently, the new experts may come from experts in the field of internet technology for big data, not nurses. This will also be a problem because experts in other fields do not necessarily understand how health professionals interpret health data in detail” (Respondent 7).
“Big data interpretation will be faster if using smart technology, such as artificial intelligence, but all of this has not been structured in the education of nurses or other health professionals. It is necessary to develop a new department for that. I believe it is necessary and important to do this now” (Respondent 4).
“Education on genetics has not been discussed in detail and clearly in universities. There is also no clear curriculum for genetic analysis, especially for nurses. We should think about curriculum preparation first so that the competencies of nurses and other health professionals we want are available for work in hospitals” (Respondent 17).
“It takes quite a long time to make nurses understand well the workings and interpretation of genetics and big data analysis in clinical practice” (Respondent 10).
Nurse needs to understand patient needs and make decision making based on patient preferences
“Patients and their families seem resigned to whatever choices and decisions are made by health professionals. There is still little decision-making done by patients and their families independently; it might be related to literacy and knowledge” (Respondent 6).
“The patient’s opinion must be prioritized; they have the independence to determine the best intervention. Ideally, it would be like that, but it cannot be done optimally in the hospital. Health professionals should think about the basic knowledge of patients and families first. Further, the independence of the patient and family will be improved” (Respondent 11).
“The needs of patients and families are basic knowledge about the disease and the various therapeutic options they will receive” (Respondent 16).
“Before the patient makes the best choice for himself, he should have been exposed to information about the choice of therapy” (Respondent 7).
Service should be covered by national health insurance
“Personalized care approach will certainly be expensive. In Indonesia, if health programs are not covered by health insurance, it will be difficult to run the program” (Respondent 10).
“Health insurance plays an essential role in Indonesian health services. Many hospitals have not cooperated with health insurance in the beginning, and as a result, people have not been interested in those hospital services. The patient did not come there. Likewise, the precision health care approach program, if we hope diabetic patients will use this program, it must be covered by health insurance first” (Respondent 17).
“I cannot imagine how much the cost for genetic testing and procurement of tools to support big data analysis. If everything is covered by health insurance, maybe it will be possible in the future” (Respondent 3).
“In-depth analysis of needs and a prior evaluation of the success of a personal approach are needed. We can learn from other countries. Suppose it is proven that this approach can reduce the number of complications of diabetes patients in the future. In that case, this should be interesting and maybe will be covered by the government through national health insurance” (Respondent 8).
Existence of a precision health care approach must be included in hospital accreditation standards
“In the past, before the implementation of educational standards for health professionals, nurses in hospitals were reluctant to take further studies. Now that education standards have been included in hospital accreditation standards, many health professionals want to improve their education level—likewise, precision healthcare programs it is included in hospital accreditation standards. Of course, the hospital will exert efforts to make the program successful in the future” (Respondent 5).
“If many countries have successfully implemented a precision health care approach program and succeeded significantly in reducing the risk of complications due to diabetes in the future. I am sure this new approach will be included in hospital accreditation standards” (Respondent 14).
“If it is already included in the accreditation, the hospital will inevitably adopt this approach. That could be one of the strategies that this program will be able to run in the future in the healthcare setting” (Respondent 15).
4. Discussion
The results of in-depth interviews with respondents demonstrated that precision health care focuses more on genetic elements, big data, and patient preference. Nurses must be competent to obtain comprehensive family histories, identify family members at risk of developing a genomic-influenced condition, and for genomic-influenced drug reactions, assist people in making informed decisions about and understanding the results of their genetic/genomic tests and therapies, and refer at-risk people to appropriate health care professionals and agencies for specialized care [17, 18, 19]. Moreover, understanding big data is a priority for nurse leaders as we aim to provide the best possible care to patients [20, 21]. The big data challenge is made more difficult by working with healthcare companies with complex information technology and networks with numerous clinical, financial, and claim systems that must be integrated [22, 23]. Integrating and analyzing disparate data to better understand outcomes is not straightforward [24]. Access to the correct information at the right time to support clinical decisions is essential in planning and providing patient care [20]. All clinicians require real-time information to make fast, crucial clinical choices [25, 26]. Big data technologies can assist nurses and other healthcare professionals in enhancing patient care, maximizing results, and lowering healthcare costs [20–23]. Additionally, by respecting patient preferences, we can improve outpatient care decisions through enhanced support systems that give care suggestions priority and better communication of information about treatments with diabetic patients [12, 27]. For instance, by considering the full person, including the complex interplay of comorbid conditions, psychosocial and functional status, and individual needs in clinical practice, patient conditions can be addressed [13].
The data show that various obstacles are predicted to be found, especially in hospitals in Indonesia, due to multiple factors, namely the availability of facilities, the costs incurred, and the development of supporting human resources [28]. It was related to a study that mentioned that when that data of details is adequately assembled, integrated, and analyzed, it will offer substantial new potential at two levels: The individual and the population as a whole [20, 24, 29]. We can identify trends and interactions once all relevant data has been tracked and analyzed, which no system or software could do individually [20]. However, to do so, we must also safeguard the data’s security and privacy, and we need analytic to gather useful information [30, 31]. Changes in healthcare stakeholders’ perspectives are also necessary to accommodate this iterative flow of personal data. For instance, patients, customers, and physicians must be willing to trust and learn from user-generated data. This requires personal and analytical evolution [21, 32]. Additionally, graduate-level nurses should be able to gather a precise family history, understand how to apply genetics to patient diagnosis, treatment, and care, and know the best ways to communicate this information to patients and families. These skills require additional work, time, and cost [20, 33]. Given the accessibility of direct-to-consumer genetic testing, nurses must develop their skills in reading, interpreting, and advising patients about their genetic profiles. As integral members of interdisciplinary teams, nurses working in clinical settings must be prepared to deal with these issues and support informed decision-making that may affect healthcare decisions [18, 34]. When delivering individualized care to patients from diverse origins and responding to genetic profiles and healthcare options inquiries, it is essential to consider cultural attitudes and views toward genomics [20, 35–37].
Health professionals in this study believe that the implementation of precision health care can succeed step by step. Those were analyzed based on their experience. Existing approaches to extensive data set analysis provide a necessary but insufficient foundation for nursing to participate in the precision healthcare revolution [20]. Through precision health care, the social policy statement of nursing guides a principled, ethical perspective on big data and data science [24, 30, 38]. There are implications for practicing basic and advanced practice clinical nurses, nurse scientists collaborating with data scientists, and nurse data scientists. Nursing’s inquiry traditions, which rely on electronic health records, claims data exploration, or public health data sets, provide a solid foundation for thinking about data science [23, 39]. Notably, nursing must use all familiar and emerging methods to generate nursing knowledge [23, 38, 40]. It is beneficial to connect what we must do in the future to what we have accomplished in the past. Nurse scientists are utilizing the opportunities provided by big data and data science in novel ways. For decades, nurse scientists have worked in interdisciplinary teams to apply some of the mining and modeling techniques now associated with big data and data science to phenomena central to nursing and health via precision health care [23, 40, 41]. Therefore, despite many obstacles and steps we must go through in this initial phase, a precision healthcare approach can provide greater richness in understanding patient phenomena and tailoring interventional strategies personalized to the patient [20].
5. Conclusion
More time is needed to implement the precision healthcare concept in Indonesia. Many things can be prepared in advance, especially in preparing human resources for health professionals through education at universities, strengthening national organizations’ regulation and the costs of procuring genetic tests and big data analysis. Necessarily, it takes time, but applying the concept has great potential to be developed in reducing the risk of complications caused by diabetes mellitus in the future.
Ethical Considerations
Compliance with ethical guidelines
The current study was approved by the Health Research Ethics Committee STIKES Bina Usada Bali (Code: 267/EA/KEPK-BUB-2022). The participants provided written informed consent to take part in this study.
Funding
This study was financially supported by the Universitas Muhammadiyah Semarang.
Authors' contributions
Conceptualization and supervision: Satriya Pranata and Shu-Fang Vivienne Wu; Methodology: Yunie Armiyati and Khoiriyah Khoiriyah; Investigation, writing original draft, review and editing: Satriya Pranata and Ju-Han Liu; Data analysis: Lin Chun Shing and Satriya Pranata; Data collection: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Universitas Muhammadiyah Semarang for funding support.
References
- IDF Diabetes Atlas. Diabetes around the world in 2021 [Intenet]. 2021 [Updated 2023 October 10]. Available from: [Link]
- World Health Organization (WHO). Diabetes [Internet]. 2023 [Updated 2023 October 10]. Available from: [Link]
- Kementerian Kesehatan RI. [Riset Kesehatan Dasar: Riskesdas 2013 [Indonesian)]. Jakarta: Komite Nasional Pengendalian Tembakau. [Link]
- Kementrian Kesehatan RI. [Basic Health Research (RISKESDAS) (Indonesian). Jakarta: Balitbang Kemkes; 2018.
- Alikhani G, Balochian S, Khajavi A, Ziaee M. Intelligent blood glucose control in diabetic patients by designing and simulating an artificial pancreas with a predictive sliding mode control method. Journal of Research & Health. 2022; 12(6):435-42. [DOI:10.32598/JRH.12.6.2010.1]
- Sassen B. Nursing: Health education and improving patient self-management. Berlin: Springer; 2018. [DOI:10.1007/978-3-319-51769-8]
- World Self-medication Industry. The story of self- care and medication 40 years of progress, 1970-2010. Geneva: World Self-medication Industry; 2010. [Link]
- Wang ZG, Zhang L, Zhao WJ. Definition and application of precision medicine. Chinese Journal of Traumatology. 2016; 19(5):249-50. [DOI:10.1016/j.cjtee.2016.04.005] [PMID]
- Bierman AS, Tinetti ME. Precision medicine to precision care: Managing multimorbidity. Lancet. 2016; 388(10061):2721-3. [DOI:10.1016/S0140-6736(16)32232-2] [PMID]
- Corwin E, Redeker NS, Richmond TS, Docherty SL, Pickler RH. Ways of knowing in precision health. Nursing Outlook. 2019; 67(4):293-301. [DOI:10.1016/j.outlook.2019.05.011] [PMID]
- Davies AK, McGale N, Humphries SE, Hirani SP, Beaney KE, Bappa DA, et al. Effectiveness of a self-management intervention with personalised genetic and lifestyle-related risk information on coronary heart disease and diabetes-related risk in type 2 diabetes (CoRDia): Study protocol for a randomised controlled trial. Trials. 2015; 16:547. [DOI:10.1186/s13063-015-1073-7] [PMID]
- Pranata Satriya, Vivienne Wu SF, Chu CH, Nugroho KH. Precision health care strategies for older adults with diabetes in Indonesia: A delphi consensus study. Medical Journal of Indonesia. 2021; 30(3):221-7. [DOI:10.13181/mji.oa.215525]
- Pranata S, Wu SV, Alizargar J, Liu JH, Liang SY, Lu YY. Precision health care elements, definitions, and strategies for patients with diabetes: A literature review. International Journal of Environmental Research and Public Health. 2021; 18(12):6535. [DOI:10.3390/ijerph18126535] [PMID]
- Neubauer BE, Witkop CT, Varpio L. How phenomenology can help us learn from the experiences of others. Perspectives on Medical Education. 2019; 8(2):90-97. [DOI:10.1007/S40037-019-0509-2] [PMID]
- Morrow R, Rodriguez A, King N. Colaizzi’s descriptive phenomenological method. The Psychologist. 2015; 28(8):643-4. [Link]
- Gill MJ. The possibilities of phenomenology for organizational research. Organizational Research Methods. 2014; 17(2):118-37. [DOI:10.1177/1094428113518348]
- Terzioglu F, Dinç L. Nurses' views on their role in genetics. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2004; 33(6):756-64. [DOI:10.1177/0884217504270712] [PMID]
- Hickey KT, Taylor JY, Barr TL, Hauser NR, Jia H, Riga TC, et al. Nursing genetics and genomics: The international society of nurses in genetics (ISONG) survey. Nurse Education Today. 2018; 63:12-7. [DOI:10.1016/j.nedt.2018.01.002] [PMID]
- Spiegel AM, Hawkins M. 'Personalized medicine' to identify genetic risks for type 2 diabetes and focus prevention: Can it fulfill its promise? Health Affairs. 2012; 31(1):43-9. [DOI:10.1377/hlthaff.2011.1054] [PMID]
- Brennan PF, Bakken S. Nursing needs big data and big data needs nursing. Journal of Nursing Scholarship. 2015; 47(5):477-84. [DOI:10.1111/jnu.12159] [PMID]
- Topaz M, Pruinelli L. Big data and nursing: Implications for the future. Studies in Health Technology and Informatics. 2017; 232:165-71. [PMID]
- Gleason KT, Dennison Himmelfarb CR. Big Data: Contributions, Limitations, and Implications for Cardiovascular Nurses. The Journal of Cardiovascular Nursing. 2017; 32(1):4-6. [DOI:10.1097/JCN.0000000000000384] [PMID]
- Founds S. Systems biology for nursing in the era of big data and precision health. Nursing Outlook. 2018; 66(3):283-92. [DOI:10.1016/j.outlook.2017.11.006] [PMID]
- Sensmeier J. Understanding the impact of big data on nursing knowledge. Nursing Critical Care. 11(2):11-13. [DOI:10.1097/01.CCN.0000480755.60698.ff]
- Bagheri A, Nasiri S, Lame E, Mahdavipanah M, Darogheh L, Sadat Z. Health needs of adolescents in Aran va Bidgol City, Iran. Journal of Research & Health. 2023; 13(1):59-66. [DOI:10.32598/JRH.13.1.2005.1]
- Mutatina B, Kanyarutokye Basaza R, Kawulukusi Sewankambo N, Lavis J N. Identifying key steps in developing a one-stop shop for health policy and system information in a limited-resource setting: A case study. Journal of Research & Health. 2022; 12(6):363-76. [DOI:10.32598/JRH.12.6.1970.3]
- Hertroijs DFL, Brouwers MCGJ, Elissen AMJ, Hiligsmann M, Schaper NC, Ruwaard D. Patients’ preferences for diabetes care: A discrete choice experiment. International Journal of Integrated Care. 2018; 18:283. [DOI:10.5334/ijic.s2283]
- Sitoayu L, Purwara Dewanti L, Melani V, Azahra Sumitra P, Rulina Marpaung M. Differences in eating habits, stress, and weight changes among Indonesian generations Y and Z students during the COVID-19 pandemic. Journal of Research & Health. 2023; 13(2):79-86. [DOI:10.32598/JRH.13.2.2076.1]
- Zhu R, Han S, Su Y, Zhang C, Yu Q, Duan Z. The application of big data and the development of nursing science: A discussion paper. International Journal of Nursing Sciences. 2019; 6(2):229-34. [DOI:10.1016/j.ijnss.2019.03.001] [PMID] [PMCID]
- Glasgow RE, Kwan BM, Matlock DD. Realizing the full potential of precision health: The need to include patient-reported health behavior, mental health, social determinants, and patient preferences data. Journal of Clinical and Translational Science. 2018; 2(3):183-5. [DOI:10.1017/cts.2018.31] [PMID]
- Dash S, Shakyawar SK, Sharma M, Kaushik S. Big data in healthcare: Management, analysis and future prospects. Journal of Big Data. 2019; 6(54):1-25. [DOI:10.1186/s40537-019-0217-0]
- Mohan V, Radha V. Precision diabetes is slowly becoming a reality. Medical Principles and Practice. 2019; 28(1):1-9.[DOI:10.1159/000497241] [PMID]
- Vogel C, Zwolinsky S, Griffiths C, Hobbs M, Henderson E, Wilkins E. A delphi study to build consensus on the definition and use of big data in obesity research. International Journal of Obesity. 2019; 43(12):2573-86. [DOI:10.1038/s41366-018-0313-9] [PMID]
- AL-Dewik NI, Qoronfleh MW. Genomics and precision medicine: Molecular diagnostics innovations shaping the future of healthcare in Qatar. Advances in Public Health. 2019; 2019; 2019:1-11. [DOI:10.1155/2019/3807032]
- Hu J, Amirehsani KA, Wallace DC, McCoy TP, Silva Z. A family-based, culturally tailored diabetes intervention for hispanics and their family members. The Diabetes Educator. 2016; 42(3):299-314. [DOI:10.1177/0145721716636961] [PMID]
- Lutes LD, Cummings DM, Littlewood K, Solar C, Carraway M, Kirian K, et al. COMRADE: A randomized trial of an individually tailored integrated care intervention for uncontrolled type 2 diabetes with depression and/or distress in the rural southeastern US. Contemporary Clinical Trials. 2018; 70:8-14. [DOI:10.1016/j.cct.2018.04.007] [PMID]
- Pranata S, Shing LC, Vranada A, Chun LY, Armiyati Y, Khoiriyah K. The implementation of precision personalized care to improve diabetes patients ‘ self-management at taipei veteran general hospital : An observational study. 2021; 10(3):1304-7. [DOI:10.15562/bmj.v10i3.2902]
- Hickey KT, Bakken S, Byrne MW, Bailey DCE, Demiris G, Docherty SL, et al. Precision health: Advancing symptom and self-management science. Nursing Outlook. 2019; 67(4):462-75. [DOI:10.1016/j.outlook.2019.01.003] [PMID]
- Pastorino R, De Vito C, Migliara G, Glocker K, Binenbaum I, Ricciardi W, et al. Benefits and challenges of big data in healthcare: An overview of the European initiatives. European Journal of Public Health. 2019; 29(Supplement_3):23-27. [DOI:10.1093/eurpub/ckz168] [PMID]
- Fineout-Overholt E, Melnyk BM, Schultz A. Transforming health care from the inside out: Advancing evidence-based practice in the 21st century. Journal of Professional Nursing. 2005; 21(6):335-44. [DOI:10.1016/j.profnurs.2005.10.005] [PMID]
- Mahato K, Srivastava A, Chandra P. Paper based diagnostics for personalized health care: Emerging technologies and commercial aspects. Biosensors & Bioelectronics. 2017; 96:246-59.[DOI:10.1016/j.bios.2017.05.001] [PMID]
Type of Study: Orginal Article |
Subject:
● Health Education
Received: 2023/03/23 | Accepted: 2023/06/28 | Published: 2023/10/3
Received: 2023/03/23 | Accepted: 2023/06/28 | Published: 2023/10/3
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |