Volume 14, Issue 4 (Jul & Aug 2024)
J Research Health 2024, 14(4): 341-356 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Muwema M, Nankabirwa J I, Kaye D K, Nalwadda G, Nangendo J, Obeng-Amoako G O, et al . Structures and Available Processes to Support Perinatal Care in District Hospitals of Western Uganda. J Research Health 2024; 14 (4) :341-356
URL: http://jrh.gmu.ac.ir/article-1-2445-en.html
URL: http://jrh.gmu.ac.ir/article-1-2445-en.html
Structures and Available Processes to Support Perinatal Care in District Hospitals of Western Uganda
Mercy Muwema1 

 , Joaniter I Nankabirwa2
, Joaniter I Nankabirwa2 

 , Dan K. Kaye3
, Dan K. Kaye3 

 , Gorrette Nalwadda4
, Gorrette Nalwadda4 

 , Joanita Nangendo2
, Joanita Nangendo2 

 , Gloria Odei Obeng-Amoako5
, Gloria Odei Obeng-Amoako5 

 , Jean Claude Nkurunziza2
, Jean Claude Nkurunziza2 

 , Wilson Mwanja6
, Wilson Mwanja6 

 , Elizabeth N. Ekong7
, Elizabeth N. Ekong7 

 , Robert Basaza8
, Robert Basaza8 

 , Joan N. Kalyango2
, Joan N. Kalyango2 

 , Grace Edwards9
, Grace Edwards9 




 , Joaniter I Nankabirwa2
, Joaniter I Nankabirwa2 

 , Dan K. Kaye3
, Dan K. Kaye3 

 , Gorrette Nalwadda4
, Gorrette Nalwadda4 

 , Joanita Nangendo2
, Joanita Nangendo2 

 , Gloria Odei Obeng-Amoako5
, Gloria Odei Obeng-Amoako5 

 , Jean Claude Nkurunziza2
, Jean Claude Nkurunziza2 

 , Wilson Mwanja6
, Wilson Mwanja6 

 , Elizabeth N. Ekong7
, Elizabeth N. Ekong7 

 , Robert Basaza8
, Robert Basaza8 

 , Joan N. Kalyango2
, Joan N. Kalyango2 

 , Grace Edwards9
, Grace Edwards9 


1- Clinical Epidemiology Unit, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda. , muwecy@gmail.com
2- Clinical Epidemiology Unit, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda.
3- Department of Obstetrics and Gynecology, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda.
4- Department of Nursing, School of Health Sciences, College of Health Sciences, Makerere University, Kampala, Uganda.
5- Department of Nutrition and Food Science, School of Biological Sciences, College of Basic and Applied Sciences, University of Ghana, Legon, Ghana.
6- Whale Consult Limited, Kampala, Uganda.
7- Department of Nursing and Midwifery, Faculty of Public Health, Nursing and Midwifery, Uganda Christian University, Mukono, Uganda.
8- Department of Public Health, Faculty of Public Health, Nursing and Midwifery, Uganda Christian University, Mukono, Uganda.
9- Department of Midwifery, School of Nursing and Midwifery, Aga Khan University, Kampala, Uganda.
2- Clinical Epidemiology Unit, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda.
3- Department of Obstetrics and Gynecology, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda.
4- Department of Nursing, School of Health Sciences, College of Health Sciences, Makerere University, Kampala, Uganda.
5- Department of Nutrition and Food Science, School of Biological Sciences, College of Basic and Applied Sciences, University of Ghana, Legon, Ghana.
6- Whale Consult Limited, Kampala, Uganda.
7- Department of Nursing and Midwifery, Faculty of Public Health, Nursing and Midwifery, Uganda Christian University, Mukono, Uganda.
8- Department of Public Health, Faculty of Public Health, Nursing and Midwifery, Uganda Christian University, Mukono, Uganda.
9- Department of Midwifery, School of Nursing and Midwifery, Aga Khan University, Kampala, Uganda.
Keywords: Physical infrastructure, Staffing, Transition in care, Coordination of care, Continuity of care, Maternal health care
Full-Text [PDF 711 kb]
(486 Downloads)
| Abstract (HTML) (2660 Views)
Full-Text: (898 Views)
Introduction
igh-quality care is essential in reducing maternal and neonatal mortality and morbidity [1]. To ensure that every pregnant woman received high-quality care through pregnancy, childbirth, and postnatal period, the World Health Organization (WHO) developed a framework that defined the key components of quality maternal and newborn care as follows: 1) Provision of care which included evidence-based practices, efficient information, and referral systems domains; 2) Experience of care which included effective communication, respect and dignity, and emotional support domains; 3) Competent motivated human resource; and 4) Essential physical resources [2]. To operationalize this framework, WHO further released standards that informed healthcare planners, managers, and providers on what should be put in place to improve maternal and newborn care in health facilities [2].
According to the standard, the availability of competent and motivated human resources in sufficient numbers to meet the anticipated workload with regular supportive supervision and mentoring, opportunity for continuing professional development and skills development through in-service training and regular refresher sessions, and inter-professional collaborative practice are prerequisites for good quality care in health facilities. Additionally, good quality of care requires the availability of basic essential equipment and supplies, laboratory supplies and tests, and functional ultrasound machine, essential physical resources like reliable safe water, energy infrastructure, functional blood transfusion service, equipped operating theatre close to the childbirth area, and functioning ambulance, reliable communication methods, standardized referral processes, and a conducive environment that allows privacy and provision of respectful confidential care [3]. Furthermore, the need for all these resources in the provision of quality care was earlier emphasized by Avedis Donabedian in his framework for quality. The framework denotes that good structures/resources increase the likelihood of good processes which increase the likelihood of a good outcome [4].
Despite the requirements for good quality care, poor infrastructural developments, inadequate qualified staffing, and stock out of essential supplies and medicines have been cited as the main contributors to poor quality care. Studies done in Africa have revealed low doctor and midwife-to-patient ratios, low maternity and delivery beds per 10000 population, a lack of clean water and electricity in most of the health facilities, no emergency transport, and inadequate basic drugs, supplies, equipment, and infrastructure in the provision of maternal health care [5-8]. Uganda is not an exception, studies in Eastern, Central, and Western Uganda showed a persistent lack of medicines, equipment, inadequate space, inadequate staffing, and non-functional operating theatres for maternal and newborn care [9-11].
Regarding processes, a study in Uganda noted that there was no communication between the referral and receiving unit before the referral. Referrals were not escorted by a healthcare provider (HCP) and often referral notes lacked the important information to inform health interventions [11]. Within the maternity units, formal protocols for the handover of patient care, critical information transmission, and patient involvement in handover were found lacking [12]. Similar findings were found in Gambia where in addition to the lack of multi-disciplinary team handovers there were delays, and in some instances, patient care was not handed over [13]. These gaps may explain the maternal mortality of 336 deaths per 100000 live births and neonatal mortality of 27 deaths per 1000 live births in Uganda at the time of the study [14].
Although previous studies have documented gaps in existing structures and processes for maternal and newborn care, these gaps are often not reported together to offer an understanding of how the structures available could affect processes of care as indicated in the Donabedian quality framework. Accordingly, this study describes health facility structures and processes that were available to support perinatal care in three district hospitals of western Uganda that were previously reported in our earlier publication [15]. Specifically, this study describes the following items: 1) Staffing, basic equipment, essential medicines and supplies, diagnostic tests, and amenities, and 2) The nature of supervision and in-service training for HCPs in perinatal care, and transition in care, coordination of care and continuity of care processes that were available to support perinatal care. Findings from this study intend to inform on the bottlenecks that impede the provision of quality care to pregnant women.
Methods
Study design and setting
A facility-based cross-sectional study was conducted using structured interviews and observation between March and June 2020 in three public district hospitals of Bunyoro region, Uganda. The characteristics of the study site have been previously described [15], but briefly, the region is comprised of eight districts that include Kakumiro, Kibaale, Kagadi, Kikuube, Hoima, Masindi, Buliisa, and Kiryandongo [16]. The region has three district hospitals (Kagadi, Kiryandongo, and Masindi). The district hospitals offer preventive, promotive, and both in- and out-patient curative services in all areas of child and adult medicine [17]. An average of 860 antenatal contacts and 300 births are registered at these hospitals in any given month in the year before the study.
Study participants
HCPs and facility managers working in the three participating district hospitals were screened for eligibility to join the study. An HCP was eligible for inclusion if they passed the following criteria: 1) Worked in one of the perinatal units (antenatal, labor suite, postnatal); 2) Was a nurse, a midwife, a clinical officer, or a doctor; 3) Had worked with the participating hospital for a minimum of 6 months; and 4) Provided written informed consent to participate in the study. Additionally, any HCP performing the role of facility in-charge (medical superintendent) or worked as a perinatal unit in-charge, and provided written informed consent was eligible to participate in the study as a facility manager. HCPs and facility managers on leave at the time of data collection were excluded from the study.
Sample size and sampling procedure
The study involved all eligible doctors, midwives, nurses, and clinical officers who were working in the antenatal, labor suite, and postnatal units as well as facility in-charges and perinatal unit in-charges of the three participating hospitals at the time of data collection. A small proportion of the 305 HCPs available in these hospitals were expected to work in the perinatal units. Accordingly, this study recruited participants using the census sampling method to maximize participation.
Data collection
The data was collected using structured questionnaires and an observation checklist that had been developed with guidance from the WHO standards for improving maternal and neonatal care in health facilities [3]. Structured interviews using the questionnaires were conducted in English language to the facility managers and HCPs by the principal investigator and a trained research assistant with a bachelor’s degree in social sciences. Perinatal unit in-charges were identified through the facility in-charge while the HCPs were identified using the staff lists provided by the unit in-charges. The HCPs were screened for eligibility to join the study. Following consent, separate pre-tested structured questionnaires designed and uploaded on a tablet using the Open Data Kit software, version 1.28.1 were administered to the facility managers and the HCPs. Additionally, a pre-tested structured observation checklist also designed using the Open Data Kit software was used to collect data on perinatal units’ physical infrastructure and amenities.
Data collection instruments
The required data was collected using two pre-tested structured questionnaires and one pre-tested observation checklist. The tools were pre-tested in a similar district hospital of another region among facility managers and HCPs. The first questionnaire was administered to the facility managers and it consisted of two sections: Demographic characteristics and the various health facility structures. The first section on demographics contained information on age, gender, marital status, professional qualification, workstation, work experience, and management role and position. The second section on health facility structures had two parts, in which, part one was answered by the facility in-charges and part two answered by the perinatal unit in-charges. Part one by facility in-charges measured HCPs in the facility, funding and support streams for the perinatal services, leadership structure for perinatal units, and facility biographic data. Part two measured the HCPs and the equipment, supplies, and diagnostic tests available in the perinatal units.
The second questionnaire was administered to the HCPs and it contained two sections: Demographic characteristics and health facility processes. The demographic characteristics included age, gender, marital status, professional qualification, workstation, work experience, and management position. The health facility processes section contained in-service training/mentorship, supervision, transition in care, coordination of care, and continuity of care. Finally, the observation checklist measured the key amenities in the perinatal units and in the hospital that are expected to support perinatal services and the condition of the perinatal units’ buildings.
Data management and statistical analysis
The data collected was exported to the STATA software, version 13 for cleaning and analysis. The study variables considered for analysis were health facility structures and health facility processes. Health facility structures were defined as the physical infrastructure and amenities, equipment, supplies, tests, funding, support streams, leadership structure for the perinatal units, management guidelines, and staffing used in the provision of perinatal services. Health facility processes refer to transition in care, coordination of care, continuity of care, in-service training/mentorship for HCPs, and supervision of HCPs in the perinatal units. Particularly, transition in care referred to the presence of patient flow procedures and support, and patient referral processes. Coordination of care referred to the presence of joint ward rounds and joint meetings, HCPs peer consultations and support, patient involvement in care, and care handover procedures. Continuity of care refers to documentation of patient care practices (informational continuity), provision of patient HCPs contact on each visit (relational continuity), and use of patient records during management and patient follow-up (management continuity).
For health facility structures, a score of 1 was used to describe that the structure was available on the day of the survey while a score of 0 showed that it was unavailable. To assess the staffing levels, we compared the actual numbers with the available positions in the structure for each hospital. For the staff-to-patient ratio, the actual number of each category of staff was divided by the average monthly antenatal care (ANC) attendance in each hospital for ANC staff-to-patient ratios and divided by the average monthly births in each hospital for the maternity staff-to-patient ratios. These were summarized and presented as frequencies and ratios. For basic equipment, supplies, tests, and amenities availability, the number of available equipment, tests, supplies, and amenities was divided by the total number of expected equipment, supplies, tests, and amenities. These were summarized and presented as proportions and means. To calculate the bed density per 1000 pregnant women, the number of inpatient beds was divided by the total average annual ANC attendance for each hospital for the previous year. The resultant ratio was then adjusted to per 1000 population by multiplying it by 1000 [18].
Regarding facility processes, supervision, in-service training, transition in care, and continuity of care, each parameter regarded by the care provider as available was coded “yes” and given a score of 1 while a code of “no” with a score of 0 was given if it was unavailable. These were summarized and presented as proportions. Lastly, coordination in care was analyzed using means where a score of 1.0 – 2.5 was coded as disagree, a score of 2.6 – 3.5 as neutral, and 3.6 to 5.0 as agree.
Results
Description of the study population
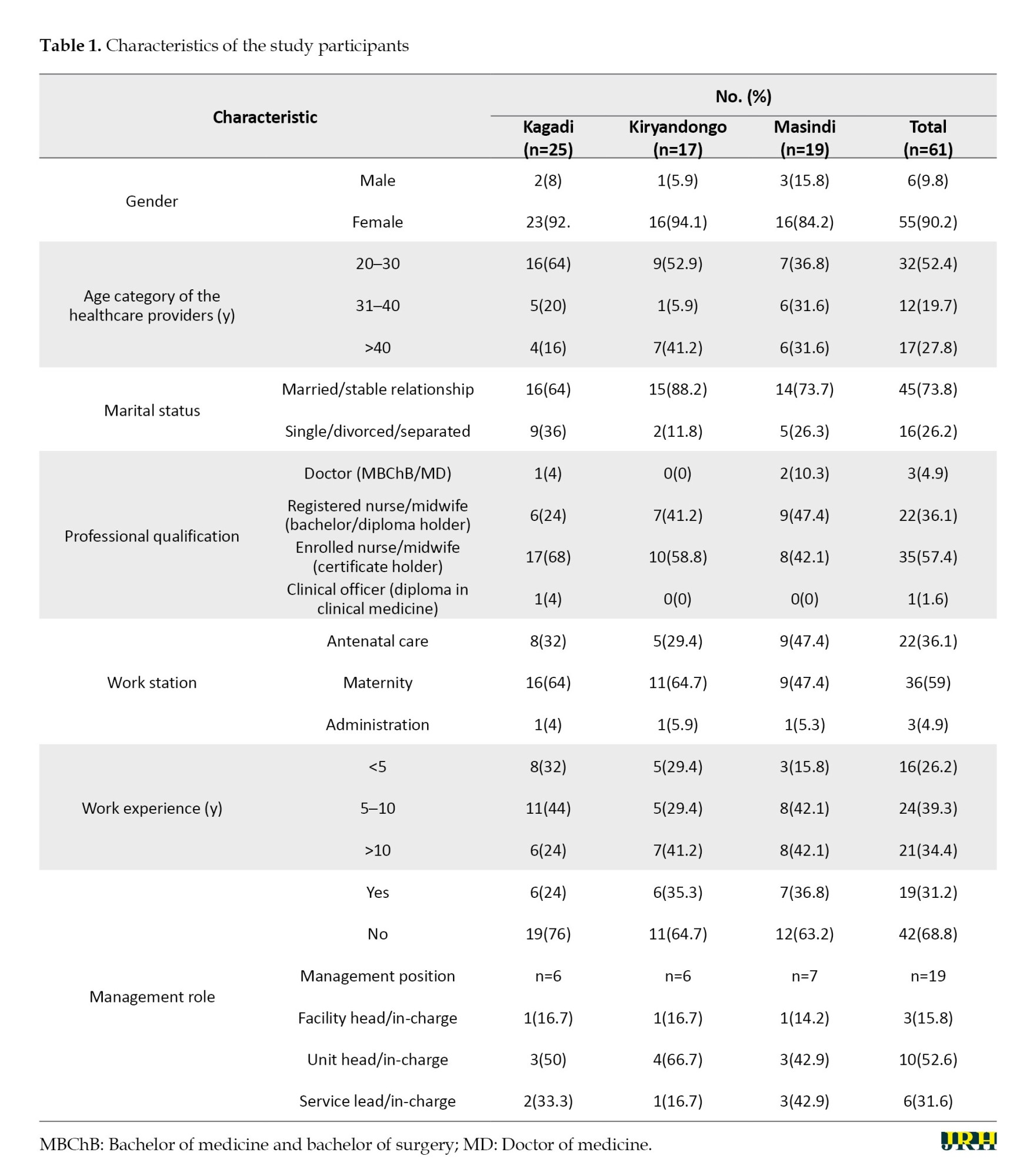
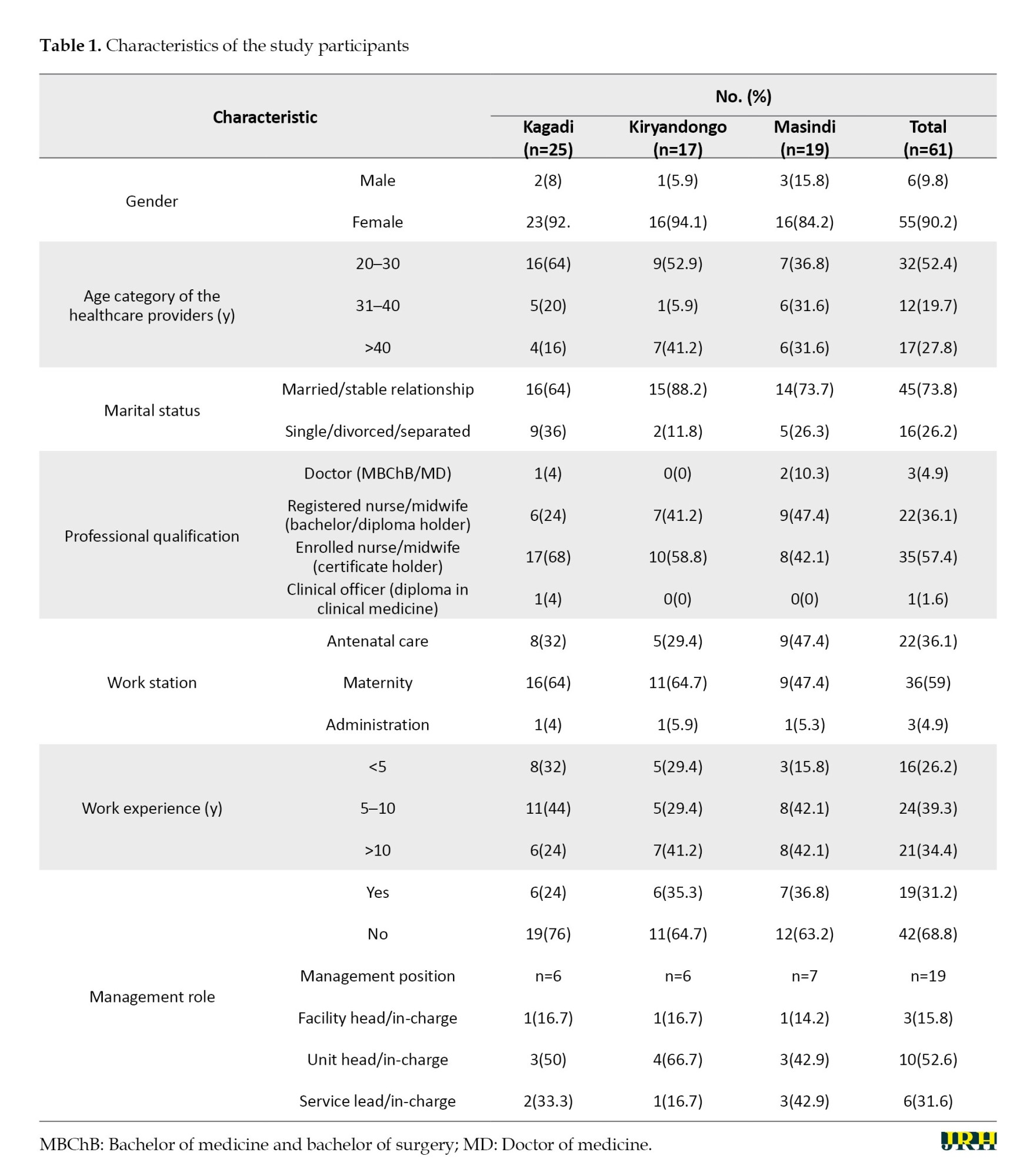
A total of 61 HCPs participated in the study, with the majority being female (n=55 [90.2%]), married or in a stable relationship (n=45 [73.8%]), and with no management role (n=42 [68.8%]). The Mean±SD age of the participants was 34.5±10.3 years. Only three (4.9%) participants worked in administration as described in Table 1.
Health facility structures to support perinatal care
Core staffing levels and leadership of perinatal units
A total of 18 doctors (62%) were found in the three hospitals out of the 29 total available positions in the structure. Masindi Hospital had the lowest proportion of filled positions for doctors (6[55%]) while Kiryandongo Hospital had the highest (7[70%]). Of the 18 doctors, only 5(27.8%) were placed in the perinatal units with Kagadi Hospital having the highest number of doctors in these units (3[60%]). Meanwhile, 93 midwives (93 [111%]) were found in the facilities out of the 84 total available positions in the structure. An excess number of midwives was found in Kagadi Hospital (41 [146%]) while a deficit of midwives was observed in Masindi Hospital (24[86%]). Of the 93 midwives, 74(79.6%) were placed in the perinatal units with Kagadi Hospital having the highest number (30 [40.5%]). Lastly, each hospital had one anesthetist out of the two available positions.
The mean ratio of doctors to women was 1:72 in antenatal and 1:60 in maternity. Masindi Hospital had the worst doctor-to-women ratio in both antenatal and maternity (1:1039 and 1:342, respectively). The average midwife-to-women ratio was 1:29 in antenatal and 1:7 in maternity. Kiryandongo Hospital had the lowest midwife-to-women ratio in antenatal (1:120) while Masindi Hospital had the highest midwife-to-women ratio in maternity (1:34). Concerning leadership of perinatal services, two of the facilities (Kagadi and Masindi) lacked a designated obstetrics and gynecology department head though all had in-charges for each perinatal unit.
Basic equipment, supplies, tests, and amenities for perinatal services at the study facilities
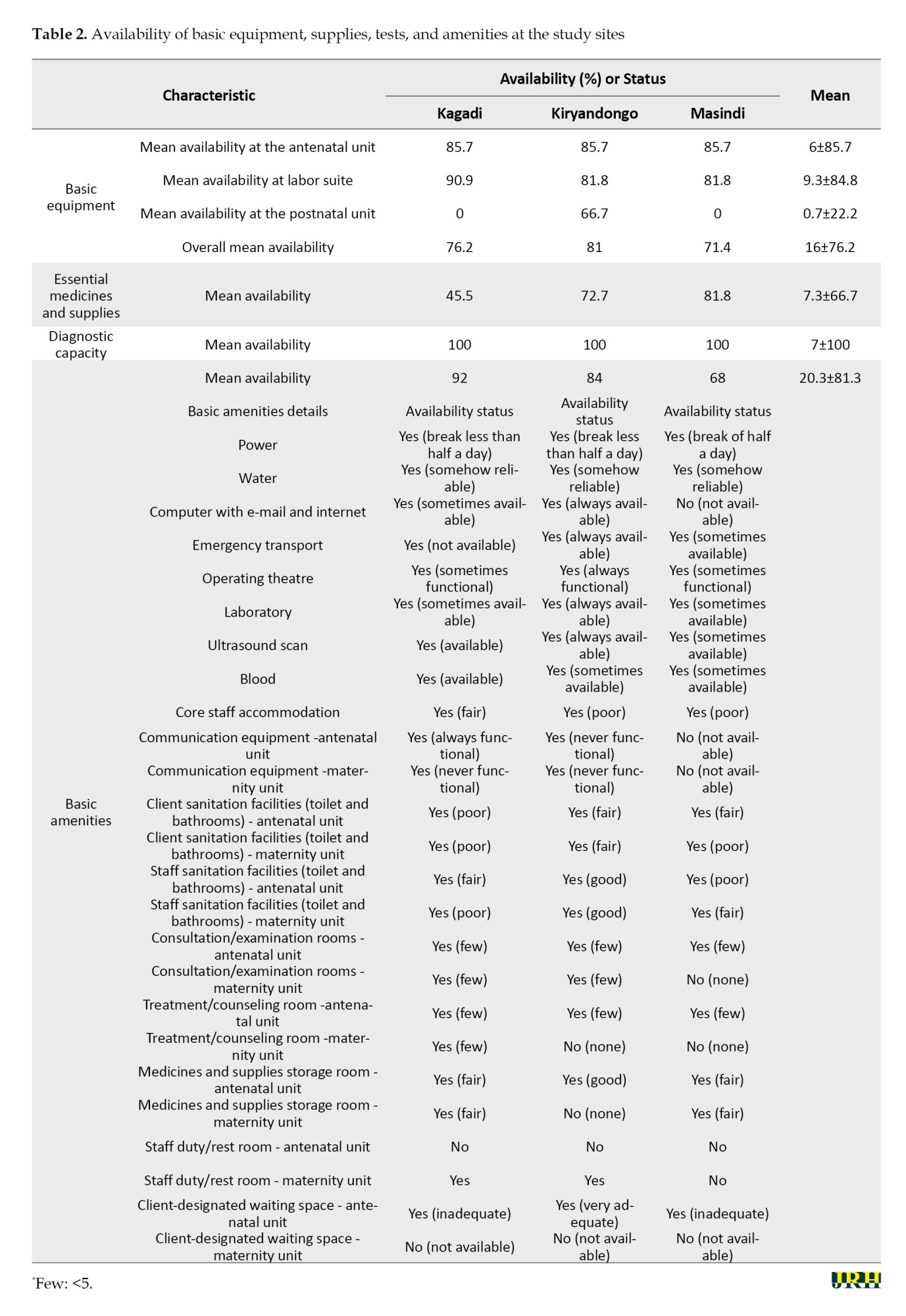
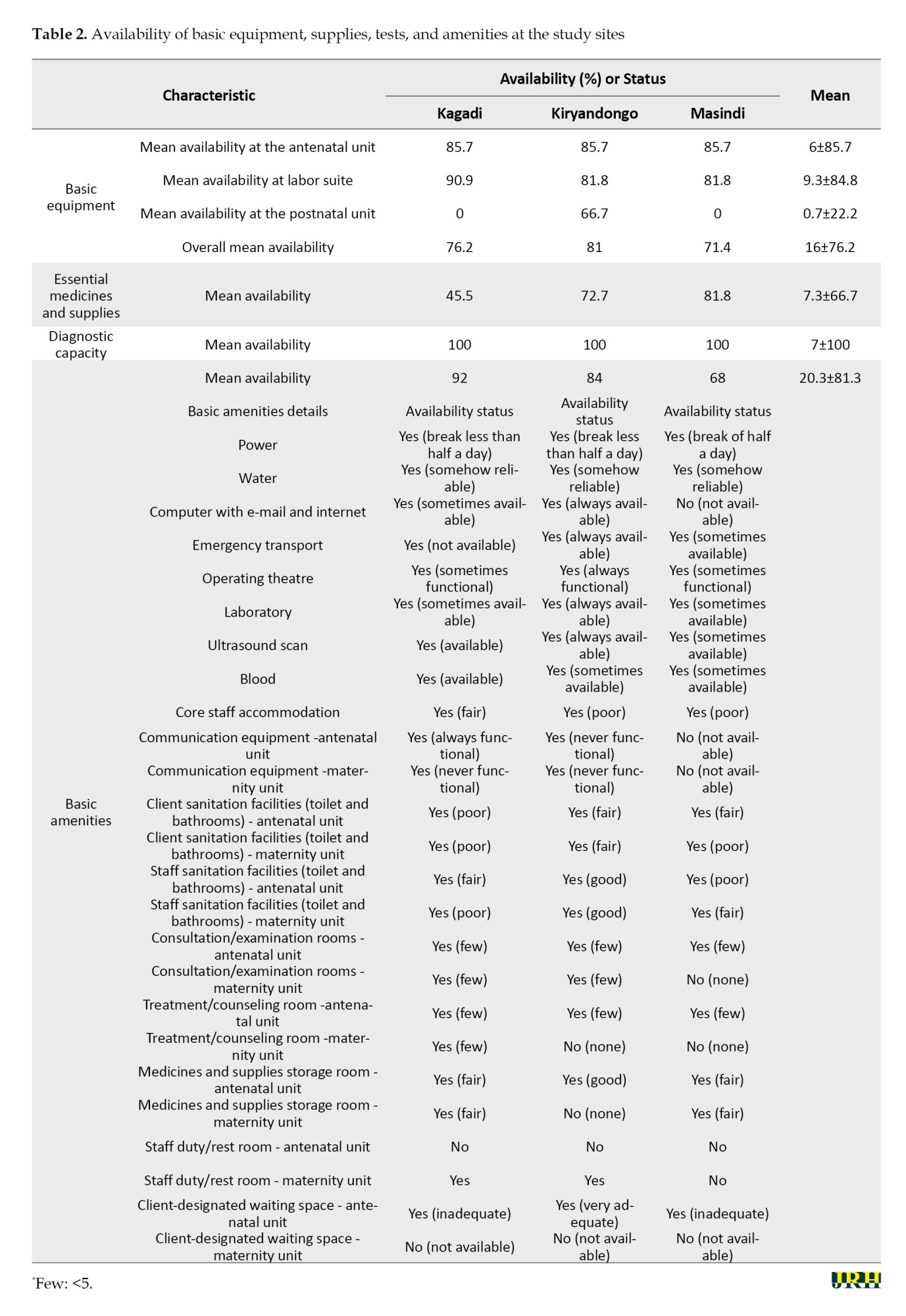
The mean availability of basic equipment for all hospitals in the antenatal, labor and delivery, and postnatal units was 6(85.7%), 9.3(84.8%), and 0.7(22.2%), respectively. Overall, the mean availability of basic equipment across all units in all facilities was 76.2%. Medicines and supplies availability was at 66.7% on mean while amenities were available at a level of 81.3% across all facilities. All facilities had all the required laboratory tests for perinatal care. Two of the hospitals did not have any vital equipment in their postnatal units (Kagadi Hospital and Masindi Hospital), communication equipment in their perinatal units (Kiryandongo Hospital and Masindi Hospital), and always available emergency transport, laboratory services, operating theatre (Kagadi Hospital and Masindi Hospital), and blood (Kiryandongo Hospital and Masindi Hospital) for their perinatal clients. No maternity unit had a designated waiting space for women in labor and yet the consultation rooms for women were less than five in both antenatal and maternity units (Table 2).
Delivery and maternity beds
The mean bed capacity for all hospitals in the labor suite and the postnatal was 6 and 35, respectively. The bed density per 1000 pregnant women in Masindi Hospital was 1.2, 6.6 in Kiryandongo Hospital, and 6.4 in Kagadi Hospital. Masindi Hospital had only three beds in the labor suite and 11 beds in the postnatal wards.
Funding and support streams
All facilities had annual budgets though specific data on the funds spent on perinatal services could not be obtained. Kiryandongo and Kagadi hospitals had to implement partner support in areas of capacity building, equipment, and supplies.
Health facility processes to support perinatal care
Supervision, in-service training, and transition in care
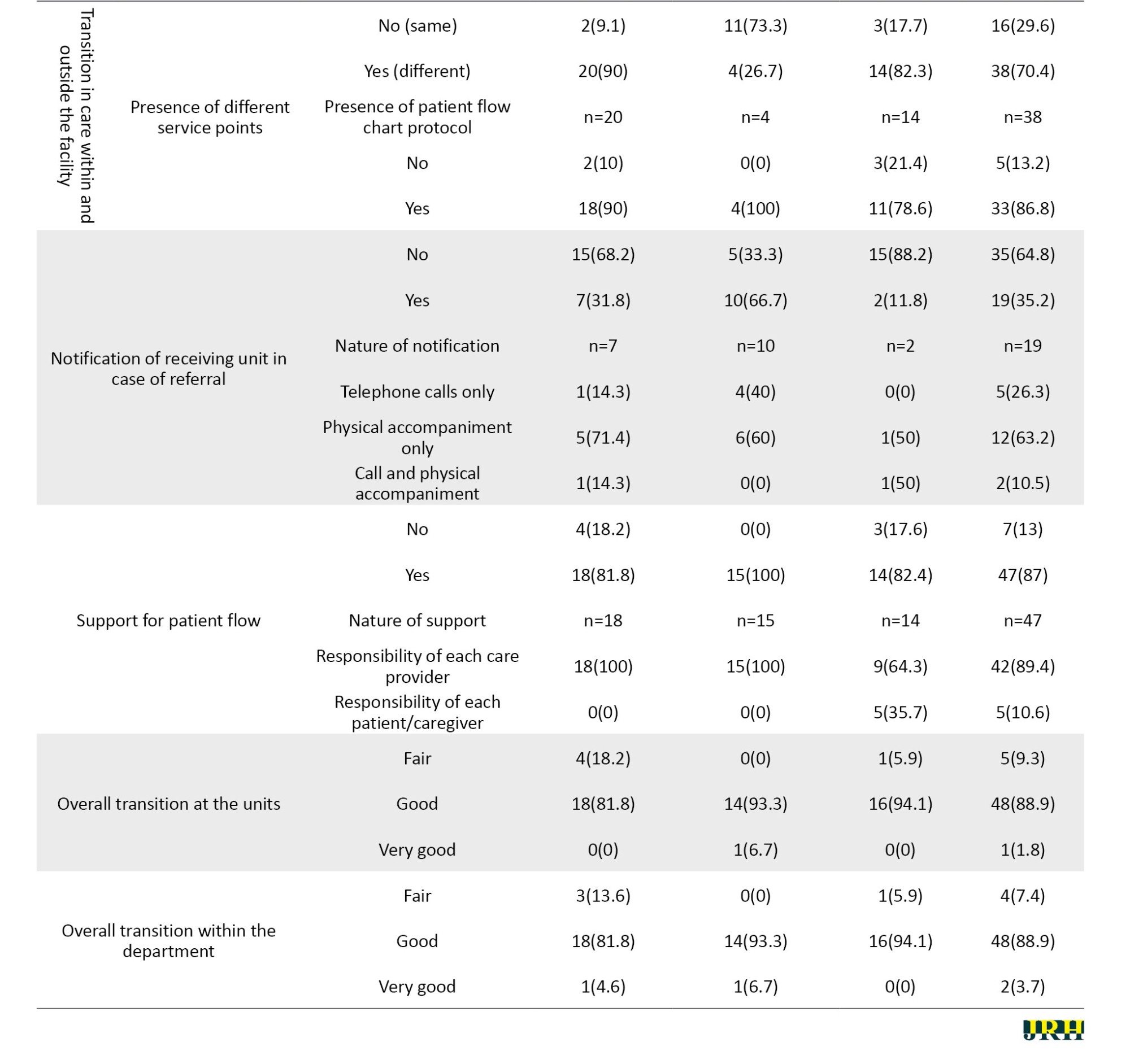
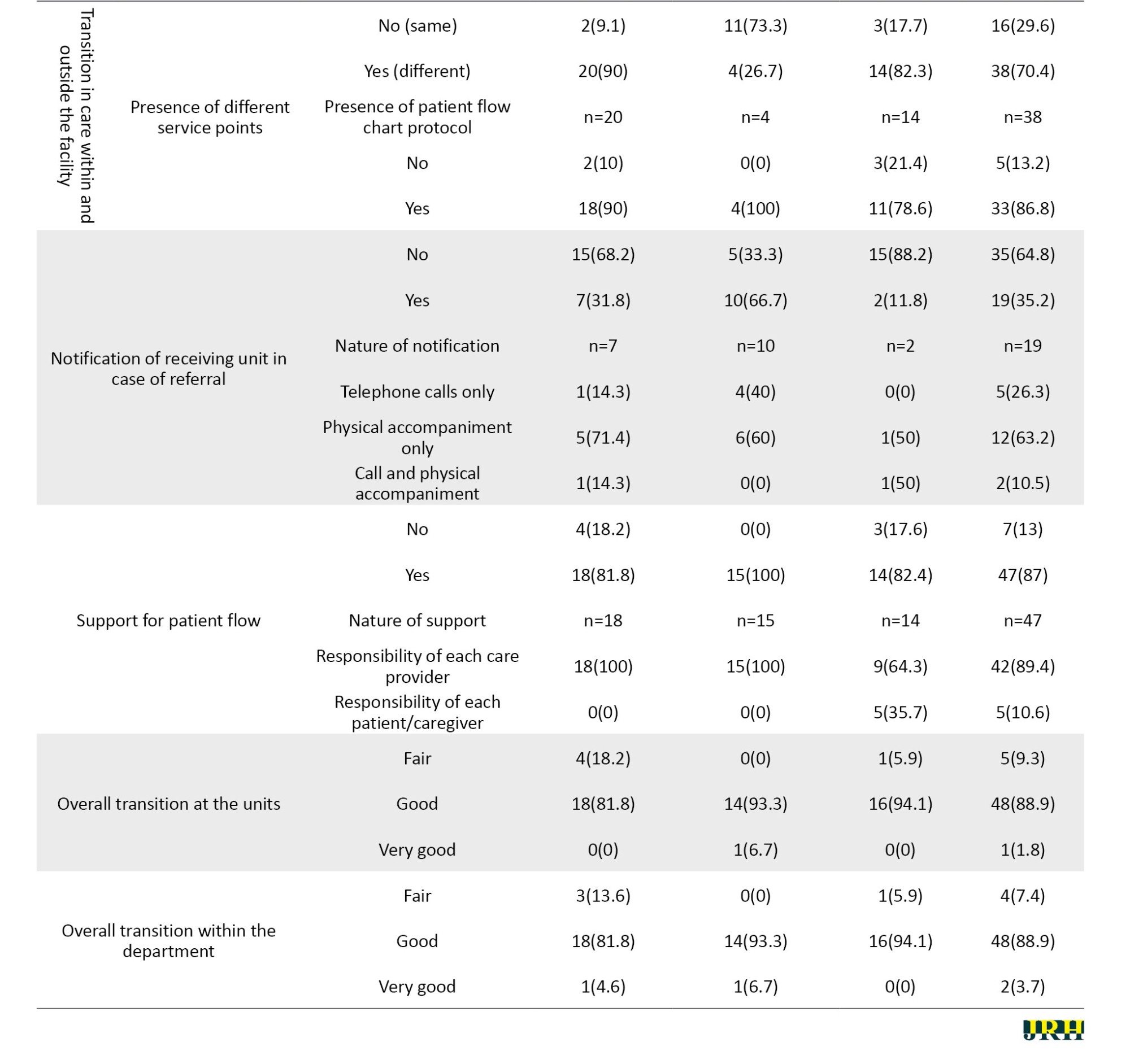
Regarding supervision, almost all (n=53 [98.2%]) HCPs felt supervised during their provision of perinatal care to women by both internal and external supervisors (n=45 [84.9%]), weekly by internal supervisors (n=24 [47.1%]) and quarterly by external supervisors (n=27 [57.4%]). For in-service training, continuing medical education was the most common form of in-service training (n=27 [50%]) and was held on a weekly basis (n=19 [54.3%]). Refresher training, despite being indicated as present in these facilities, was available only once a year (n=9 [69.2%]), with only Kagadi Hospital having the opportunity of holding them at least three times a year (n=3 [60%]). Meanwhile, almost half of Masindi Hospital participants denied having any form of in-service training (n=8 [47.1%]) Additionally, regarding transition in care, the majority of the HCPs indicated that perinatal care services were provided at different points with a clear patient flow protocol and patient support (n=38 [0.4%]; n=33 [86.8%]; and n=47 [87.0%], respectively). In case of any referral, receiving units were not notified (n=35 [64.8%]), mainly due to the lack of a standard notification method (n=34 [97.1%]). Despite this, the majority of the HCPs noted the transition in the care process to be good both at the units and within the department (n=48 [88.9%] for both) (Table 3). Even when the transition was rated as good by the participants, some of them (n=8 [14.8%]) expressed some difficulties in facilitating patient transition in care. The difficulties documented were mainly a result of patient or caretaker resistance to transit and a high number of patients at the receiving unit in case of a referral.

Coordination of care
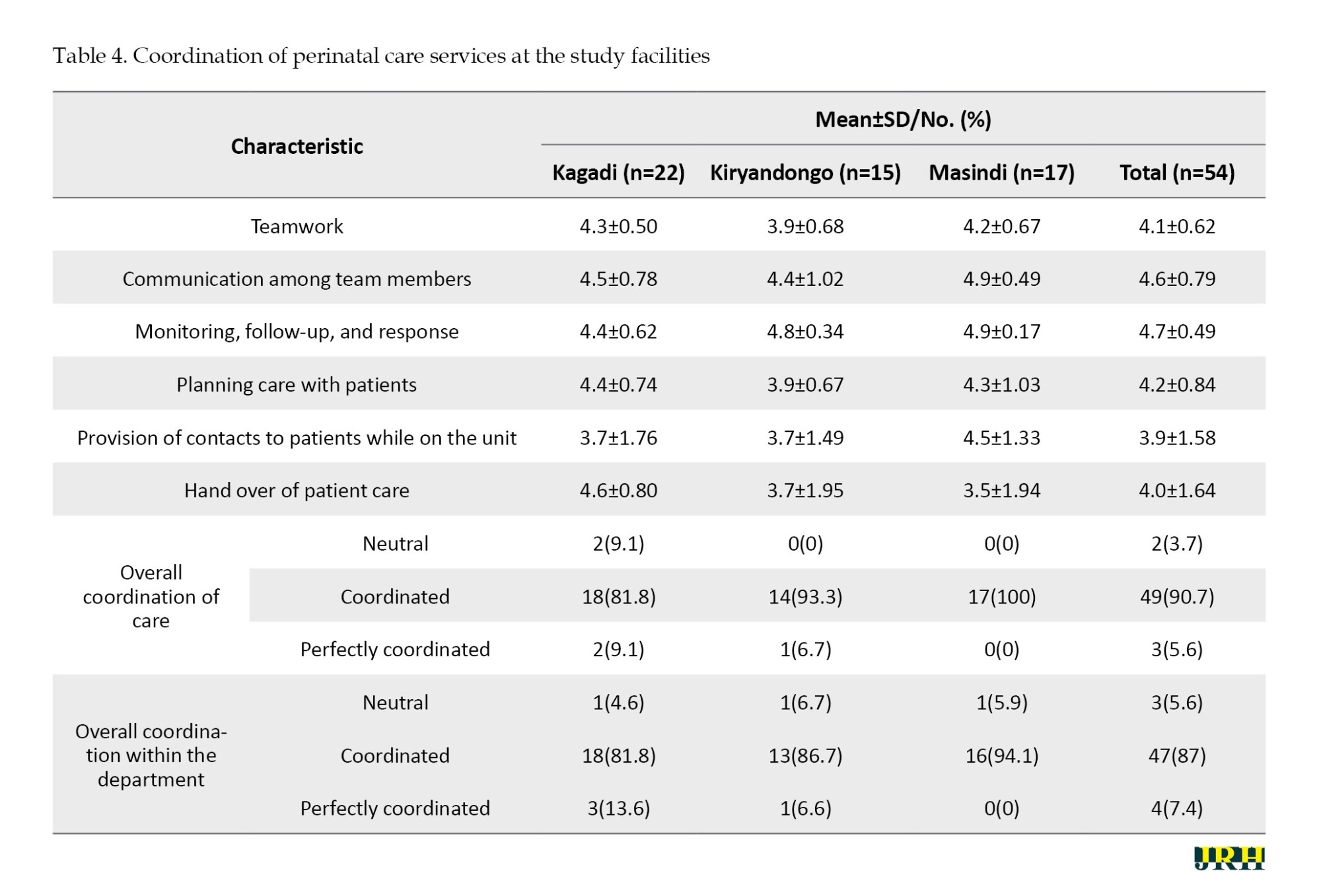
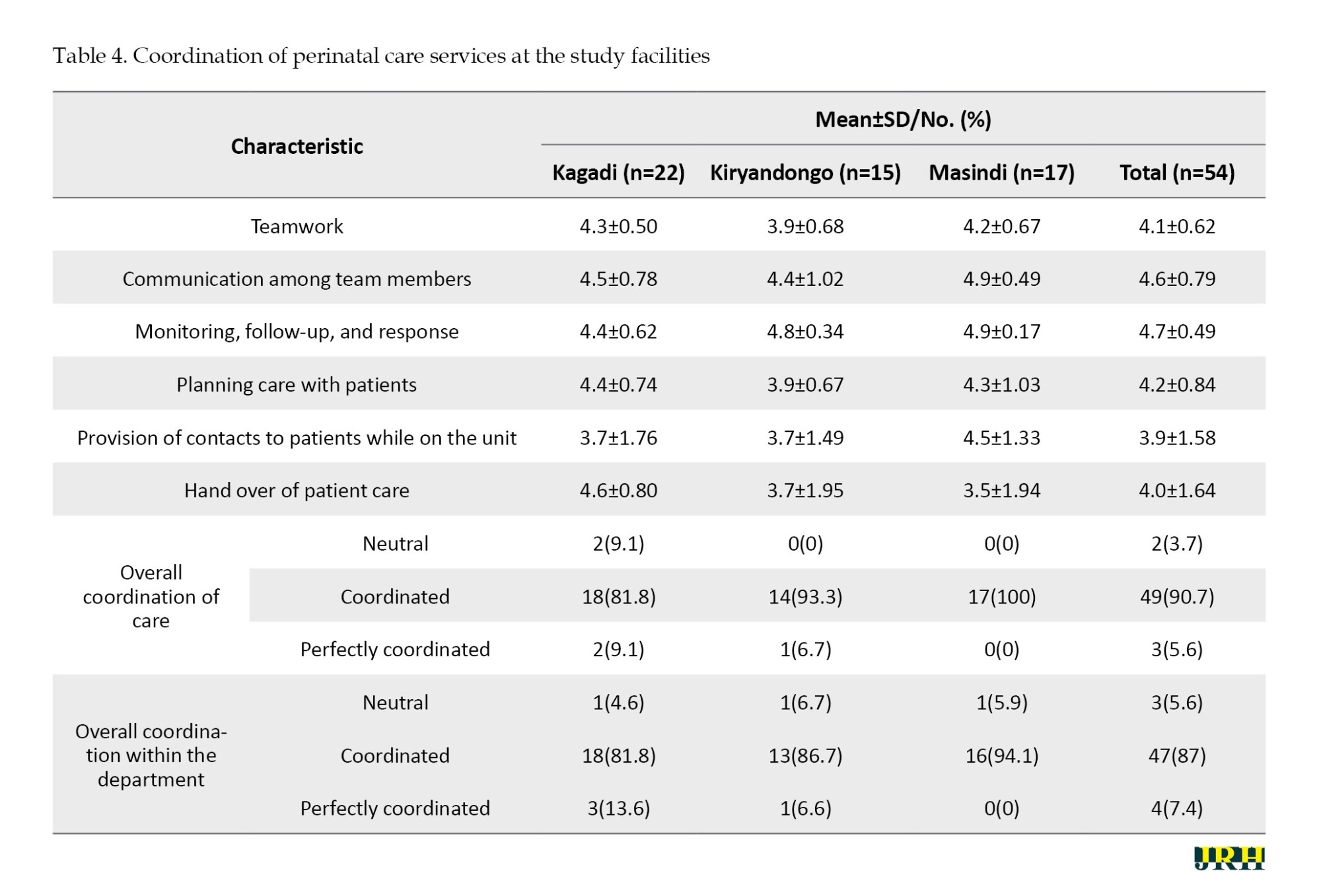
Regarding the coordination of care, HCPs agreed to have teamwork (Mean±SD 4.1±0.62), communication among the team members (Mean±SD 4.6±0.79), monitoring, follow-up, and response (Mean±SD 4.7±0.49), care planning with patients (Mean±SD 4.2±0.84), a contact provided to patients while on the unit (Mean±SD 3.9±1.58), and patient care handed over whenever shifts changed (Mean±SD 4.0±1.64). Overall, the majority of the care providers rated the care at the units and within the department to be coordinated (n=49 [90.7%] and n=47 [87.0%], respectively) (Table 4).
Continuity of care
Regarding informational continuity of care, all hospitals documented patient care manually with the commonest information documented being present history and care provided to the women (n=44 [81.5%] and n=41 [75.9%] respectively). Drugs or medications given to women during the perinatal period were the least documented information (n=25 [46.3%]). The documentation was done mainly using standardized tools (n=53 [98.2%]), which were both stored at the facility and kept by the patient (n=31 [57.4%]). Despite the use of standardized documentation tools, alternative records like papers or exercise books were also used in all the facilities (n=22 [40.7%]). Additionally, in case of a referral to another unit or facility, all hospitals offered a referral record in the form of a referral note (n=39, 73.6%). When documentation practices were assessed per unit, it was observed that documentation of drugs or medications was poor at both the antenatal and maternity units (n=9 [42.9%] for antenatal and n=16 [48.5%] for maternity). In addition, recording of assessment findings was also poor at the maternity units (n=16 [48.5%]) while recording of laboratory or diagnostic findings was also poor at the antenatal units (n=10 [47.6%]).
Regarding relational continuity, almost all the women saw different HCPs on each visit (n=51 [94.4%]). Lastly, for management continuity, the majority of the HCPs indicated referring to the women’s medical records during management on each visit (n=39 [72.2%]). In case a woman’s medical record was not referred to, care providers expressed inaccessibility to the record as the main reason for non-reference. Additionally, the hospitals did not follow up on their clients once they left the facility on each visit (n=40 [74.1%]) (Table 5).

Discussion
This study found a low HCPs to women ratio with no designated department leadership in two of the study hospitals. There were few vital pieces of equipment available for assessment of women in the postnatal units despite their availability in the antenatal and labor units. Medicines and supplies were sometimes available, with all facilities having the capacity to make diagnoses for women during pregnancy, labor and delivery, and postpartum. A maximum of six beds existed for 1000 pregnant women in these facilities. Staff felt adequately supervised during their provision of perinatal care though refresher training was rarely available to them. Even with clear patient flow protocols and support for patient transition in care, receiving units were not notified whenever women were referred to them. Patient care was manually documented, on paper or in exercise books at times, with drugs or medications being the least documented. In addition, assessment findings and diagnostic results were also least documented in the maternity and antenatal unit. Women were always attended to by different HCPs on each visit with no follow-up once they left the facility. We explore further the elements of quality of care as well.
Human resources
These hospitals had a shortage of critical human resources, equipment in the postnatal units, and medicines and supplies to adequately take care of pregnant women during antenatal, labor and childbirth, and postpartum periods. Similar findings have been found in other low-income countries and regions of Uganda [9, 19-22]. Doctors and anesthetic officers were the least available in these hospitals, a finding also revealed by other studies [23, 24]. The presence of these cadres is likely to affect emergency obstetric surgical services accessed by pregnant women [11, 20]. These shortages could explain the provision of inappropriate perinatal care in these facilities which was found in our earlier publication [15]. These findings could also explain the premise described by Donabedian’s quality of care model that structures are likely to affect processes which in turn affect the outcomes of care [4]. Lack of adequate staff, equipment, medicines, and supplies makes it difficult for pregnant women to receive the quality care as proposed by WHO in its recommendations during antenatal, intra-natal, and postnatal periods, as well as document the same as evidence [1].
Hospital beds
Fewer beds were found in the labor and postnatal units compared to the number of pregnant women who attended antenatal care in these hospitals. Accordingly, not all pregnant women accessing care in these hospitals would be guaranteed a bed during lab our or in the postnatal period. This is in line with findings of other studies elsewhere where fewer beds were found and women complained of the unfavorable birth environments in hospitals. Women complained of giving birth and sleeping on the floor after delivery [22, 25]. The absence of delivery and maternity beds is likely to undermine facility-based deliveries and the provision of immediate postpartum care to women after delivery [25].
Supervision
This study shows that staff were adequately supervised by both internal and external supervisors during their provision of perinatal care to pregnant women. Supervision of perinatal care especially by internal and external supervisors helps to enforce adherence to care standards, identify, and address maternal service delivery gaps [10, 26, 27]. This could explain the presence of diagnostic tests and equipment in the antenatal and lab units of these hospitals. Other studies associated good supervision with improved quality of care [10, 26]. However, in these hospitals, the quality of perinatal care was observed to be inappropriate [15]. The lack of a designated leader at the department level seen in two of these facilities could have affected the influence of supervision on the quality of care. There may be a need to explore the relationship between supervision and quality of perinatal care in these hospitals, and the nature of supervision provided through research. In addition, HCPs in these hospitals had a limited opportunity to attend refresher training and thus could have experienced difficulty in retaining and adhering to previous training as well as getting updates in perinatal care [28]. This again could have affected the quality of care provided to pregnant women in these hospitals.
Continuity of care
This study also showed that women who were referred to other units for care did not have the receiving units notified of their referral. This was mainly because these hospitals had no formalized way of notifying the receiving units and lacked communication equipment. This is in line with findings of a study conducted in South Western Uganda where all pregnant women referred had no prior communication to the receiving facility [11] and similar studies in Tanzania and Ghana [29, 30]. The lack of prior communication may hinder the receiving team from adequately preparing for the referral, enhance the quality of care, as well as ease patient transition in care.
Effective written communication is related to continuity and high quality of care while poor documentation is associated with poor quality of care [31]. In this study, care was manually documented, on paper or in exercise books at times, with drugs or medications being the least documented. In addition, assessment findings and diagnostic results were also least documented in the maternity and antenatal units. Manual documentation allows detailed information to be written which improves accuracy [31]. However, this system of documentation is influenced by workload and time, creating differences in the kind of information written [32]. The low HCPs to women ratio in this study could have adversely affected the documentation of information on medications received, assessments done, and diagnostic tests undertaken. This may require standardization of documentation to allow more accurate information in the time available. Conversely, documentation of care on unstandardized tools could undermine the storage, retrieval, and usage of information thus breaking continuity in care. The poor documentation practices may explain the inappropriate care that was reported to have been provided to pregnant women in these study sites [15].
Lastly, this study noted that women were attended to by different HCPs on each visit. This is a common practice in resource-constrained countries in what is referred to as a shared model of care [33]. Much as care by the same HCPs on each visit referred to as personal continuity is known to yield positive childbirth experiences and consistency in care for pregnant women [34, 35], this practice is far from being practiced in least-developed countries due to constraints in human resources [33]. Context-specific strategies for promoting relational continuity of care among pregnant women will be explored through research, mostly for such countries.
Conclusion
The study shows a shortage of critical human resources, equipment, and beds to support the provision of perinatal care to pregnant women. Pregnant women were not adequately supported to transit in care and have their care continued. The gaps in structures and processes could have resulted in the inappropriate perinatal care received by pregnant women documented in our earlier paper. Therefore, the provision of required equipment, infrastructure, and institution of clear systems for referral and documentation of care could enhance HCPs’ ability to provide quality care to pregnant women. There is also a need to structure supervision of perinatal care for positive outcomes. Further research could also be undertaken to explain the relationship between structures, processes, and outcomes of care; supervision and quality of care; and relational continuity of care practices and quality of care.
Study limitations and strengths
This study faced some limitations which we wish to acknowledge. First, this was a cross-sectional study where we collected data at one-time point. Perhaps, a follow-up study assessing the structures and processes available alongside the care processes over a certain period could have been more insightful. To mitigate this, interviews were held with facility managers to validate the structures available and processes reported, although this was limited, not documented, and included in the study findings. Secondly, the processes documented in this study were self-reported. It is possible that the information reported did not exactly reflect what was being done during the care of pregnant women. Direct observation would have given a better picture of how pregnant women are supported during care. Thirdly, the study reports the structures and processes of three referral hospitals in the region. It does not capture the capacity of lower-level facilities that could have cared for these pregnant women before they transitioned into these hospitals. The care provided at the lower units could have influenced the outcome seen in our earlier study. This study has some strengths. It is the first of its kind to the best of our knowledge in the Western region of Uganda, particularly Bunyoro where maternal and perinatal mortalities are high. This study further depicted the gaps in structures and processes that could affect the care provided to pregnant women in this region, which provides a basis for further analytical studies. It further contributes to the region case study that may help in understanding the quality of perinatal care provided to pregnant women across resource-constrained settings, and thus lays the ground for the development of quality-of-care standards in such settings.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was granted by the Makerere University School of Medicine Research and Ethics Committee (Code: 2019-137) and the Uganda National Council for Science and Technology (Code: HS483ES). All participants signed a written informed consent form before participating in the study. The data were collected following relevant guidelines and regulations.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and methodology: Mercy Muwema, Joaniter I. Nankabirwa, Dan K. Kaye, Grace Edwards, Gorrette Nalwadda, Joan N. Kalyango, Wilson Mwanja, Joanita Nangendo and Gloria Odei Obeng-Amoako; Supervision: Joaniter I. Nankabirwa, Dan K. Kaye, Grace Edwards, Gorrette Nalwadda and Joan N. Kalyango; Data collection, analysis, investigation and funding administration: Mercy Muwema and Wilson Mwanja; Writing the original draft: Mercy Muwema, Wilson Mwanja, Joanita Nangendo, Gloria Odei Obeng-Amoako, Elizabeth N. Ekong, Jean Claude Nkurunziza and Robert Basaza; Review, editing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are very thankful to all the women who agreed to participate in the study, the health facility managers who made access to women and their records possible, and the research assistants who ensured that quality data was obtained. Special appreciation is given to the study site supervisors: Rosemary Katusiime, Immaculate Ainembabazi, and Harriet Awaazi who ensured that data is timely accessed and collected. Lastly, the authors appreciate the district health officers for allowing this study to be conducted in their districts.
References
igh-quality care is essential in reducing maternal and neonatal mortality and morbidity [1]. To ensure that every pregnant woman received high-quality care through pregnancy, childbirth, and postnatal period, the World Health Organization (WHO) developed a framework that defined the key components of quality maternal and newborn care as follows: 1) Provision of care which included evidence-based practices, efficient information, and referral systems domains; 2) Experience of care which included effective communication, respect and dignity, and emotional support domains; 3) Competent motivated human resource; and 4) Essential physical resources [2]. To operationalize this framework, WHO further released standards that informed healthcare planners, managers, and providers on what should be put in place to improve maternal and newborn care in health facilities [2].
According to the standard, the availability of competent and motivated human resources in sufficient numbers to meet the anticipated workload with regular supportive supervision and mentoring, opportunity for continuing professional development and skills development through in-service training and regular refresher sessions, and inter-professional collaborative practice are prerequisites for good quality care in health facilities. Additionally, good quality of care requires the availability of basic essential equipment and supplies, laboratory supplies and tests, and functional ultrasound machine, essential physical resources like reliable safe water, energy infrastructure, functional blood transfusion service, equipped operating theatre close to the childbirth area, and functioning ambulance, reliable communication methods, standardized referral processes, and a conducive environment that allows privacy and provision of respectful confidential care [3]. Furthermore, the need for all these resources in the provision of quality care was earlier emphasized by Avedis Donabedian in his framework for quality. The framework denotes that good structures/resources increase the likelihood of good processes which increase the likelihood of a good outcome [4].
Despite the requirements for good quality care, poor infrastructural developments, inadequate qualified staffing, and stock out of essential supplies and medicines have been cited as the main contributors to poor quality care. Studies done in Africa have revealed low doctor and midwife-to-patient ratios, low maternity and delivery beds per 10000 population, a lack of clean water and electricity in most of the health facilities, no emergency transport, and inadequate basic drugs, supplies, equipment, and infrastructure in the provision of maternal health care [5-8]. Uganda is not an exception, studies in Eastern, Central, and Western Uganda showed a persistent lack of medicines, equipment, inadequate space, inadequate staffing, and non-functional operating theatres for maternal and newborn care [9-11].
Regarding processes, a study in Uganda noted that there was no communication between the referral and receiving unit before the referral. Referrals were not escorted by a healthcare provider (HCP) and often referral notes lacked the important information to inform health interventions [11]. Within the maternity units, formal protocols for the handover of patient care, critical information transmission, and patient involvement in handover were found lacking [12]. Similar findings were found in Gambia where in addition to the lack of multi-disciplinary team handovers there were delays, and in some instances, patient care was not handed over [13]. These gaps may explain the maternal mortality of 336 deaths per 100000 live births and neonatal mortality of 27 deaths per 1000 live births in Uganda at the time of the study [14].
Although previous studies have documented gaps in existing structures and processes for maternal and newborn care, these gaps are often not reported together to offer an understanding of how the structures available could affect processes of care as indicated in the Donabedian quality framework. Accordingly, this study describes health facility structures and processes that were available to support perinatal care in three district hospitals of western Uganda that were previously reported in our earlier publication [15]. Specifically, this study describes the following items: 1) Staffing, basic equipment, essential medicines and supplies, diagnostic tests, and amenities, and 2) The nature of supervision and in-service training for HCPs in perinatal care, and transition in care, coordination of care and continuity of care processes that were available to support perinatal care. Findings from this study intend to inform on the bottlenecks that impede the provision of quality care to pregnant women.
Methods
Study design and setting
A facility-based cross-sectional study was conducted using structured interviews and observation between March and June 2020 in three public district hospitals of Bunyoro region, Uganda. The characteristics of the study site have been previously described [15], but briefly, the region is comprised of eight districts that include Kakumiro, Kibaale, Kagadi, Kikuube, Hoima, Masindi, Buliisa, and Kiryandongo [16]. The region has three district hospitals (Kagadi, Kiryandongo, and Masindi). The district hospitals offer preventive, promotive, and both in- and out-patient curative services in all areas of child and adult medicine [17]. An average of 860 antenatal contacts and 300 births are registered at these hospitals in any given month in the year before the study.
Study participants
HCPs and facility managers working in the three participating district hospitals were screened for eligibility to join the study. An HCP was eligible for inclusion if they passed the following criteria: 1) Worked in one of the perinatal units (antenatal, labor suite, postnatal); 2) Was a nurse, a midwife, a clinical officer, or a doctor; 3) Had worked with the participating hospital for a minimum of 6 months; and 4) Provided written informed consent to participate in the study. Additionally, any HCP performing the role of facility in-charge (medical superintendent) or worked as a perinatal unit in-charge, and provided written informed consent was eligible to participate in the study as a facility manager. HCPs and facility managers on leave at the time of data collection were excluded from the study.
Sample size and sampling procedure
The study involved all eligible doctors, midwives, nurses, and clinical officers who were working in the antenatal, labor suite, and postnatal units as well as facility in-charges and perinatal unit in-charges of the three participating hospitals at the time of data collection. A small proportion of the 305 HCPs available in these hospitals were expected to work in the perinatal units. Accordingly, this study recruited participants using the census sampling method to maximize participation.
Data collection
The data was collected using structured questionnaires and an observation checklist that had been developed with guidance from the WHO standards for improving maternal and neonatal care in health facilities [3]. Structured interviews using the questionnaires were conducted in English language to the facility managers and HCPs by the principal investigator and a trained research assistant with a bachelor’s degree in social sciences. Perinatal unit in-charges were identified through the facility in-charge while the HCPs were identified using the staff lists provided by the unit in-charges. The HCPs were screened for eligibility to join the study. Following consent, separate pre-tested structured questionnaires designed and uploaded on a tablet using the Open Data Kit software, version 1.28.1 were administered to the facility managers and the HCPs. Additionally, a pre-tested structured observation checklist also designed using the Open Data Kit software was used to collect data on perinatal units’ physical infrastructure and amenities.
Data collection instruments
The required data was collected using two pre-tested structured questionnaires and one pre-tested observation checklist. The tools were pre-tested in a similar district hospital of another region among facility managers and HCPs. The first questionnaire was administered to the facility managers and it consisted of two sections: Demographic characteristics and the various health facility structures. The first section on demographics contained information on age, gender, marital status, professional qualification, workstation, work experience, and management role and position. The second section on health facility structures had two parts, in which, part one was answered by the facility in-charges and part two answered by the perinatal unit in-charges. Part one by facility in-charges measured HCPs in the facility, funding and support streams for the perinatal services, leadership structure for perinatal units, and facility biographic data. Part two measured the HCPs and the equipment, supplies, and diagnostic tests available in the perinatal units.
The second questionnaire was administered to the HCPs and it contained two sections: Demographic characteristics and health facility processes. The demographic characteristics included age, gender, marital status, professional qualification, workstation, work experience, and management position. The health facility processes section contained in-service training/mentorship, supervision, transition in care, coordination of care, and continuity of care. Finally, the observation checklist measured the key amenities in the perinatal units and in the hospital that are expected to support perinatal services and the condition of the perinatal units’ buildings.
Data management and statistical analysis
The data collected was exported to the STATA software, version 13 for cleaning and analysis. The study variables considered for analysis were health facility structures and health facility processes. Health facility structures were defined as the physical infrastructure and amenities, equipment, supplies, tests, funding, support streams, leadership structure for the perinatal units, management guidelines, and staffing used in the provision of perinatal services. Health facility processes refer to transition in care, coordination of care, continuity of care, in-service training/mentorship for HCPs, and supervision of HCPs in the perinatal units. Particularly, transition in care referred to the presence of patient flow procedures and support, and patient referral processes. Coordination of care referred to the presence of joint ward rounds and joint meetings, HCPs peer consultations and support, patient involvement in care, and care handover procedures. Continuity of care refers to documentation of patient care practices (informational continuity), provision of patient HCPs contact on each visit (relational continuity), and use of patient records during management and patient follow-up (management continuity).
For health facility structures, a score of 1 was used to describe that the structure was available on the day of the survey while a score of 0 showed that it was unavailable. To assess the staffing levels, we compared the actual numbers with the available positions in the structure for each hospital. For the staff-to-patient ratio, the actual number of each category of staff was divided by the average monthly antenatal care (ANC) attendance in each hospital for ANC staff-to-patient ratios and divided by the average monthly births in each hospital for the maternity staff-to-patient ratios. These were summarized and presented as frequencies and ratios. For basic equipment, supplies, tests, and amenities availability, the number of available equipment, tests, supplies, and amenities was divided by the total number of expected equipment, supplies, tests, and amenities. These were summarized and presented as proportions and means. To calculate the bed density per 1000 pregnant women, the number of inpatient beds was divided by the total average annual ANC attendance for each hospital for the previous year. The resultant ratio was then adjusted to per 1000 population by multiplying it by 1000 [18].
Regarding facility processes, supervision, in-service training, transition in care, and continuity of care, each parameter regarded by the care provider as available was coded “yes” and given a score of 1 while a code of “no” with a score of 0 was given if it was unavailable. These were summarized and presented as proportions. Lastly, coordination in care was analyzed using means where a score of 1.0 – 2.5 was coded as disagree, a score of 2.6 – 3.5 as neutral, and 3.6 to 5.0 as agree.
Results
Description of the study population
A total of 61 HCPs participated in the study, with the majority being female (n=55 [90.2%]), married or in a stable relationship (n=45 [73.8%]), and with no management role (n=42 [68.8%]). The Mean±SD age of the participants was 34.5±10.3 years. Only three (4.9%) participants worked in administration as described in Table 1.
Health facility structures to support perinatal care
Core staffing levels and leadership of perinatal units
A total of 18 doctors (62%) were found in the three hospitals out of the 29 total available positions in the structure. Masindi Hospital had the lowest proportion of filled positions for doctors (6[55%]) while Kiryandongo Hospital had the highest (7[70%]). Of the 18 doctors, only 5(27.8%) were placed in the perinatal units with Kagadi Hospital having the highest number of doctors in these units (3[60%]). Meanwhile, 93 midwives (93 [111%]) were found in the facilities out of the 84 total available positions in the structure. An excess number of midwives was found in Kagadi Hospital (41 [146%]) while a deficit of midwives was observed in Masindi Hospital (24[86%]). Of the 93 midwives, 74(79.6%) were placed in the perinatal units with Kagadi Hospital having the highest number (30 [40.5%]). Lastly, each hospital had one anesthetist out of the two available positions.
The mean ratio of doctors to women was 1:72 in antenatal and 1:60 in maternity. Masindi Hospital had the worst doctor-to-women ratio in both antenatal and maternity (1:1039 and 1:342, respectively). The average midwife-to-women ratio was 1:29 in antenatal and 1:7 in maternity. Kiryandongo Hospital had the lowest midwife-to-women ratio in antenatal (1:120) while Masindi Hospital had the highest midwife-to-women ratio in maternity (1:34). Concerning leadership of perinatal services, two of the facilities (Kagadi and Masindi) lacked a designated obstetrics and gynecology department head though all had in-charges for each perinatal unit.
Basic equipment, supplies, tests, and amenities for perinatal services at the study facilities
The mean availability of basic equipment for all hospitals in the antenatal, labor and delivery, and postnatal units was 6(85.7%), 9.3(84.8%), and 0.7(22.2%), respectively. Overall, the mean availability of basic equipment across all units in all facilities was 76.2%. Medicines and supplies availability was at 66.7% on mean while amenities were available at a level of 81.3% across all facilities. All facilities had all the required laboratory tests for perinatal care. Two of the hospitals did not have any vital equipment in their postnatal units (Kagadi Hospital and Masindi Hospital), communication equipment in their perinatal units (Kiryandongo Hospital and Masindi Hospital), and always available emergency transport, laboratory services, operating theatre (Kagadi Hospital and Masindi Hospital), and blood (Kiryandongo Hospital and Masindi Hospital) for their perinatal clients. No maternity unit had a designated waiting space for women in labor and yet the consultation rooms for women were less than five in both antenatal and maternity units (Table 2).
Delivery and maternity beds
The mean bed capacity for all hospitals in the labor suite and the postnatal was 6 and 35, respectively. The bed density per 1000 pregnant women in Masindi Hospital was 1.2, 6.6 in Kiryandongo Hospital, and 6.4 in Kagadi Hospital. Masindi Hospital had only three beds in the labor suite and 11 beds in the postnatal wards.
Funding and support streams
All facilities had annual budgets though specific data on the funds spent on perinatal services could not be obtained. Kiryandongo and Kagadi hospitals had to implement partner support in areas of capacity building, equipment, and supplies.
Health facility processes to support perinatal care
Supervision, in-service training, and transition in care
Regarding supervision, almost all (n=53 [98.2%]) HCPs felt supervised during their provision of perinatal care to women by both internal and external supervisors (n=45 [84.9%]), weekly by internal supervisors (n=24 [47.1%]) and quarterly by external supervisors (n=27 [57.4%]). For in-service training, continuing medical education was the most common form of in-service training (n=27 [50%]) and was held on a weekly basis (n=19 [54.3%]). Refresher training, despite being indicated as present in these facilities, was available only once a year (n=9 [69.2%]), with only Kagadi Hospital having the opportunity of holding them at least three times a year (n=3 [60%]). Meanwhile, almost half of Masindi Hospital participants denied having any form of in-service training (n=8 [47.1%]) Additionally, regarding transition in care, the majority of the HCPs indicated that perinatal care services were provided at different points with a clear patient flow protocol and patient support (n=38 [0.4%]; n=33 [86.8%]; and n=47 [87.0%], respectively). In case of any referral, receiving units were not notified (n=35 [64.8%]), mainly due to the lack of a standard notification method (n=34 [97.1%]). Despite this, the majority of the HCPs noted the transition in the care process to be good both at the units and within the department (n=48 [88.9%] for both) (Table 3). Even when the transition was rated as good by the participants, some of them (n=8 [14.8%]) expressed some difficulties in facilitating patient transition in care. The difficulties documented were mainly a result of patient or caretaker resistance to transit and a high number of patients at the receiving unit in case of a referral.

Coordination of care
Regarding the coordination of care, HCPs agreed to have teamwork (Mean±SD 4.1±0.62), communication among the team members (Mean±SD 4.6±0.79), monitoring, follow-up, and response (Mean±SD 4.7±0.49), care planning with patients (Mean±SD 4.2±0.84), a contact provided to patients while on the unit (Mean±SD 3.9±1.58), and patient care handed over whenever shifts changed (Mean±SD 4.0±1.64). Overall, the majority of the care providers rated the care at the units and within the department to be coordinated (n=49 [90.7%] and n=47 [87.0%], respectively) (Table 4).
Continuity of care
Regarding informational continuity of care, all hospitals documented patient care manually with the commonest information documented being present history and care provided to the women (n=44 [81.5%] and n=41 [75.9%] respectively). Drugs or medications given to women during the perinatal period were the least documented information (n=25 [46.3%]). The documentation was done mainly using standardized tools (n=53 [98.2%]), which were both stored at the facility and kept by the patient (n=31 [57.4%]). Despite the use of standardized documentation tools, alternative records like papers or exercise books were also used in all the facilities (n=22 [40.7%]). Additionally, in case of a referral to another unit or facility, all hospitals offered a referral record in the form of a referral note (n=39, 73.6%). When documentation practices were assessed per unit, it was observed that documentation of drugs or medications was poor at both the antenatal and maternity units (n=9 [42.9%] for antenatal and n=16 [48.5%] for maternity). In addition, recording of assessment findings was also poor at the maternity units (n=16 [48.5%]) while recording of laboratory or diagnostic findings was also poor at the antenatal units (n=10 [47.6%]).
Regarding relational continuity, almost all the women saw different HCPs on each visit (n=51 [94.4%]). Lastly, for management continuity, the majority of the HCPs indicated referring to the women’s medical records during management on each visit (n=39 [72.2%]). In case a woman’s medical record was not referred to, care providers expressed inaccessibility to the record as the main reason for non-reference. Additionally, the hospitals did not follow up on their clients once they left the facility on each visit (n=40 [74.1%]) (Table 5).

Discussion
This study found a low HCPs to women ratio with no designated department leadership in two of the study hospitals. There were few vital pieces of equipment available for assessment of women in the postnatal units despite their availability in the antenatal and labor units. Medicines and supplies were sometimes available, with all facilities having the capacity to make diagnoses for women during pregnancy, labor and delivery, and postpartum. A maximum of six beds existed for 1000 pregnant women in these facilities. Staff felt adequately supervised during their provision of perinatal care though refresher training was rarely available to them. Even with clear patient flow protocols and support for patient transition in care, receiving units were not notified whenever women were referred to them. Patient care was manually documented, on paper or in exercise books at times, with drugs or medications being the least documented. In addition, assessment findings and diagnostic results were also least documented in the maternity and antenatal unit. Women were always attended to by different HCPs on each visit with no follow-up once they left the facility. We explore further the elements of quality of care as well.
Human resources
These hospitals had a shortage of critical human resources, equipment in the postnatal units, and medicines and supplies to adequately take care of pregnant women during antenatal, labor and childbirth, and postpartum periods. Similar findings have been found in other low-income countries and regions of Uganda [9, 19-22]. Doctors and anesthetic officers were the least available in these hospitals, a finding also revealed by other studies [23, 24]. The presence of these cadres is likely to affect emergency obstetric surgical services accessed by pregnant women [11, 20]. These shortages could explain the provision of inappropriate perinatal care in these facilities which was found in our earlier publication [15]. These findings could also explain the premise described by Donabedian’s quality of care model that structures are likely to affect processes which in turn affect the outcomes of care [4]. Lack of adequate staff, equipment, medicines, and supplies makes it difficult for pregnant women to receive the quality care as proposed by WHO in its recommendations during antenatal, intra-natal, and postnatal periods, as well as document the same as evidence [1].
Hospital beds
Fewer beds were found in the labor and postnatal units compared to the number of pregnant women who attended antenatal care in these hospitals. Accordingly, not all pregnant women accessing care in these hospitals would be guaranteed a bed during lab our or in the postnatal period. This is in line with findings of other studies elsewhere where fewer beds were found and women complained of the unfavorable birth environments in hospitals. Women complained of giving birth and sleeping on the floor after delivery [22, 25]. The absence of delivery and maternity beds is likely to undermine facility-based deliveries and the provision of immediate postpartum care to women after delivery [25].
Supervision
This study shows that staff were adequately supervised by both internal and external supervisors during their provision of perinatal care to pregnant women. Supervision of perinatal care especially by internal and external supervisors helps to enforce adherence to care standards, identify, and address maternal service delivery gaps [10, 26, 27]. This could explain the presence of diagnostic tests and equipment in the antenatal and lab units of these hospitals. Other studies associated good supervision with improved quality of care [10, 26]. However, in these hospitals, the quality of perinatal care was observed to be inappropriate [15]. The lack of a designated leader at the department level seen in two of these facilities could have affected the influence of supervision on the quality of care. There may be a need to explore the relationship between supervision and quality of perinatal care in these hospitals, and the nature of supervision provided through research. In addition, HCPs in these hospitals had a limited opportunity to attend refresher training and thus could have experienced difficulty in retaining and adhering to previous training as well as getting updates in perinatal care [28]. This again could have affected the quality of care provided to pregnant women in these hospitals.
Continuity of care
This study also showed that women who were referred to other units for care did not have the receiving units notified of their referral. This was mainly because these hospitals had no formalized way of notifying the receiving units and lacked communication equipment. This is in line with findings of a study conducted in South Western Uganda where all pregnant women referred had no prior communication to the receiving facility [11] and similar studies in Tanzania and Ghana [29, 30]. The lack of prior communication may hinder the receiving team from adequately preparing for the referral, enhance the quality of care, as well as ease patient transition in care.
Effective written communication is related to continuity and high quality of care while poor documentation is associated with poor quality of care [31]. In this study, care was manually documented, on paper or in exercise books at times, with drugs or medications being the least documented. In addition, assessment findings and diagnostic results were also least documented in the maternity and antenatal units. Manual documentation allows detailed information to be written which improves accuracy [31]. However, this system of documentation is influenced by workload and time, creating differences in the kind of information written [32]. The low HCPs to women ratio in this study could have adversely affected the documentation of information on medications received, assessments done, and diagnostic tests undertaken. This may require standardization of documentation to allow more accurate information in the time available. Conversely, documentation of care on unstandardized tools could undermine the storage, retrieval, and usage of information thus breaking continuity in care. The poor documentation practices may explain the inappropriate care that was reported to have been provided to pregnant women in these study sites [15].
Lastly, this study noted that women were attended to by different HCPs on each visit. This is a common practice in resource-constrained countries in what is referred to as a shared model of care [33]. Much as care by the same HCPs on each visit referred to as personal continuity is known to yield positive childbirth experiences and consistency in care for pregnant women [34, 35], this practice is far from being practiced in least-developed countries due to constraints in human resources [33]. Context-specific strategies for promoting relational continuity of care among pregnant women will be explored through research, mostly for such countries.
Conclusion
The study shows a shortage of critical human resources, equipment, and beds to support the provision of perinatal care to pregnant women. Pregnant women were not adequately supported to transit in care and have their care continued. The gaps in structures and processes could have resulted in the inappropriate perinatal care received by pregnant women documented in our earlier paper. Therefore, the provision of required equipment, infrastructure, and institution of clear systems for referral and documentation of care could enhance HCPs’ ability to provide quality care to pregnant women. There is also a need to structure supervision of perinatal care for positive outcomes. Further research could also be undertaken to explain the relationship between structures, processes, and outcomes of care; supervision and quality of care; and relational continuity of care practices and quality of care.
Study limitations and strengths
This study faced some limitations which we wish to acknowledge. First, this was a cross-sectional study where we collected data at one-time point. Perhaps, a follow-up study assessing the structures and processes available alongside the care processes over a certain period could have been more insightful. To mitigate this, interviews were held with facility managers to validate the structures available and processes reported, although this was limited, not documented, and included in the study findings. Secondly, the processes documented in this study were self-reported. It is possible that the information reported did not exactly reflect what was being done during the care of pregnant women. Direct observation would have given a better picture of how pregnant women are supported during care. Thirdly, the study reports the structures and processes of three referral hospitals in the region. It does not capture the capacity of lower-level facilities that could have cared for these pregnant women before they transitioned into these hospitals. The care provided at the lower units could have influenced the outcome seen in our earlier study. This study has some strengths. It is the first of its kind to the best of our knowledge in the Western region of Uganda, particularly Bunyoro where maternal and perinatal mortalities are high. This study further depicted the gaps in structures and processes that could affect the care provided to pregnant women in this region, which provides a basis for further analytical studies. It further contributes to the region case study that may help in understanding the quality of perinatal care provided to pregnant women across resource-constrained settings, and thus lays the ground for the development of quality-of-care standards in such settings.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was granted by the Makerere University School of Medicine Research and Ethics Committee (Code: 2019-137) and the Uganda National Council for Science and Technology (Code: HS483ES). All participants signed a written informed consent form before participating in the study. The data were collected following relevant guidelines and regulations.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and methodology: Mercy Muwema, Joaniter I. Nankabirwa, Dan K. Kaye, Grace Edwards, Gorrette Nalwadda, Joan N. Kalyango, Wilson Mwanja, Joanita Nangendo and Gloria Odei Obeng-Amoako; Supervision: Joaniter I. Nankabirwa, Dan K. Kaye, Grace Edwards, Gorrette Nalwadda and Joan N. Kalyango; Data collection, analysis, investigation and funding administration: Mercy Muwema and Wilson Mwanja; Writing the original draft: Mercy Muwema, Wilson Mwanja, Joanita Nangendo, Gloria Odei Obeng-Amoako, Elizabeth N. Ekong, Jean Claude Nkurunziza and Robert Basaza; Review, editing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are very thankful to all the women who agreed to participate in the study, the health facility managers who made access to women and their records possible, and the research assistants who ensured that quality data was obtained. Special appreciation is given to the study site supervisors: Rosemary Katusiime, Immaculate Ainembabazi, and Harriet Awaazi who ensured that data is timely accessed and collected. Lastly, the authors appreciate the district health officers for allowing this study to be conducted in their districts.
References
- Sharma G, Mathai M, Dickson KE, Weeks A, Hofmeyr G, Lavender T, et al. Quality care during labour and birth: A multi-country analysis of health system bottlenecks and potential solutions. BMC Pregnancy & Childbirth. 2015; 15 Suppl 2(Suppl 2):S2. [DOI:10.1186/1471-2393-15-S2-S2] [PMID]
- Tunçalp O, Were WM, MacLennan C, Oladapo OT, Gülmezoglu AM, Bahl R, et al. Quality of care for pregnant women and newborns - the WHO Vision. BJOG: An International Journal of Obstetrics and Gynaecology. 2015; 122(8):1045-9.[DOI:10.1111/1471-0528.13451] [PMID]
- World Health Organization (WHO). Standards for improving quality of maternal and newborn care in health facilities. Geneva: World Health Organization; 2016. [Link]
- Donabedian A. The quality of care. How can it be assessed? Archives of Pathology and Laboratory Medicine. 1997; 121(11):1145-50. [PMID]
- Essendi H, Johnson FA, Madise N, Matthews Z, Falkingham J, Bahaj AS, et al. Infrastructural challenges to better health in maternity facilities in rural Kenya: Community and healthworker perceptions. Reproductive Health. 2015; 12:103. [DOI:10.1186/s12978-015-0078-8] [PMID]
- Dalinjong PA, Wang AY, Homer CSE. Are health facilities well equipped to provide basic quality childbirth services under the free maternal health policy? Findings from rural Northern Ghana. BMC Health Services Research. 2018; 18(1):959. [DOI:10.1186/s12913-018-3787-1] [PMID]
- Ameyaw EK, Amoah RM, Njue C, Tran NT, Dawson A. An assessment of hospital maternal health services in northern Ghana: A cross-sectional survey. BMC Health Services Research. 2020; 20(1):1088. [DOI:10.1186/s12913-020-05937-5] [PMID]
- Van Pelta S, Massarb K, Eem L, Shields-Zeemanc L, de Witd BFJ, Ruiterb ACR. “If you don’t have enough equipment, you’re not going to provide quality services”: Healthcare workers’ perceptions on improving the quality of antenatal care in rural Tanzania. International Journal of Africa Nursing Sciences. 2020; 13:100232. [DOI:10.1016/j.ijans.2020.100232]
- Kananura RM, Kiwanuka SN, Ekirapa-Kiracho E, Waiswa P. Persisting demand and supply gap for maternal and newborn care in eastern Uganda: A mixed-method cross-sectional study. Reproductive Health. 2017; 14(1):136. [DOI:10.1186/s12978-017-0402-6] [PMID]
- Munabi-Babigumira S, Glenton C, Willcox M, Nabudere H. Ugandan health workers’ and mothers’ views and experiences of the quality of maternity care and the use of informal solutions: A qualitative study. Plos One. 2019; 14(3):e0213511.[DOI:10.1371/journal.pone.0213511] [PMID]
- Kanyesigye H, Ngonzi J, Mulogo E, Fajardo Y, Kabakyenga J. Health care workers’ experiences, challenges of obstetric referral processes and self-reported solutions in South Western Uganda: Mixed methods study. Risk Management and Healthcare Policy. 2022; 15:1869-86. [DOI:10.2147/RMHP.S377304] [PMID]
- Kaye DK, Nakimuli A, Kakaire O, Osinde MO, Mbalinda SN, Kakande N. Gaps in continuity of care: patients’ perceptions of the quality of care during labor ward handover in Mulago hospital, Uganda. BMC Health Services Research. 2015; 15:190. [DOI:10.1186/s12913-015-0850-z] [PMID]
- Rickard F, Lu F, Gustafsson L, MacArthur C, Cummins C, Coker I, et al. Clinical handover communication at maternity shift changes and women’s safety in Banjul, the Gambia: A mixed-methods study. BMC Pregnancy & Childbirth. 2022; 22(1):784. [DOI:10.1186/s12884-022-05052-9] [PMID]
- Uganda Bureau of Statistics (UBOS). 2016 Uganda demographic and health survey key findings. Kampala: Uganda Bureau of Statistics; 2017. [Link]
- Muwema M, Kaye DK, Edwards G, Nalwadda G, Nangendo J, Okiring J, et al. Perinatal care in Western Uganda: Prevalence and factors associated with appropriate care among women attending three district hospitals. Plos One. 2022; 17(5):e0267015. [DOI:10.1371/journal.pone.0267015] [PMID]
- Uganda Bureau of Statistics (UBOS). 2020 statistical abstract. Kampala: Uganda Bureau of Statistics; 2020. [Link]
- The Health lnfrastructure Working Group. Guidelines for designation, establishment, and upgrading of health units: Criteria for designation of levels of services delivery of health units. Kampala: Ministry of Health; 2011. [Link]
- World Health Organization (WHO). Monitoring the building blocks of health systems: A handbook of indicators and their measurement strategies. Geneva, Switzerland: World Health Organization; 2010. [Link]
- Bradley S, Kamwendo F, Chipeta E, Chimwaza W, de Pinho H, McAuliffe E. Too few staff, too many patients: A qualitative study of the impact on obstetric care providers and on quality of care in Malawi. BMC Pregnancy & Childbirth. 2015; 15:65. [DOI:10.1186/s12884-015-0492-5] [PMID]
- Wilunda C, Oyerinde K, Putoto G, Lochoro P, Dall'Oglio G, Manenti F, et al. Availability, utilisation and quality of maternal and neonatal health care services in Karamoja region, Uganda: A health facility-based survey. Reproductive Health. 2015; 12:30. [DOI:10.1186/s12978-015-0018-7] [PMID]
- Odira C, Chiejina EN, Ezenduka PO. Capacity of health facilities to support skilled maternal health services in South-East Nigeria. International Journal of Studies in Midwifery Women’s Health. 2020; 1(1):6-15. [Link]
- Namutebi M, Nalwadda GK, Kasasa S, Muwanguzi PA, Ndikuno CK, Kaye DK. Readiness of rural health facilities to provide immediate postpartum care in Ugand. BMC Health Services Research. 2023; 23(1):22. [DOI:10.1186/s12913-023-09031-4] [PMID]
- Epiu I, Tindimwebwa JV, Mijumbi C, Chokwe TM, Lugazia E, Ndarugirire F, et al. Challenges of anesthesia in low- and middle-income countries: A cross-sectional survey of access to safe obstetric anesthesia in East Africa. Anesthesia & Analgesia 2017; 124(1):290-9. [DOI:10.1213/ANE.0000000000001690] [PMID]
- Geleto A, Chojenta C, Musa A, Loxton D. Barriers to access and utilization of emergency obstetric care at health facilities in sub-Saharan Africa: A systematic review of literature. Systematic Reviews. 2018; 7(1):183. [DOI:10.1186/s13643-018-0842-2] [PMID]
- Balde MD, Diallo BA, Bangoura A, Sall O, Soumah AM, Vogel JP, et al. Perceptions and experiences of the mistreatment of women during childbirth in health facilities in Guinea: A qualitative study with women and service providers. Reproductive Health. 2017; 14(1):3. [DOI:10.1186/s12978-016-0266-1] [PMID]
- Kisakye AN, Muhumuza Kananura R, Ekirapa-Kiracho E, Bua J, Akulume M, Namazzi G, et al. Effect of support supervision on maternal and newborn health services and practices in Rural Eastern Uganda. Global Health Action. 2017; 10(sup4):1345496. [DOI:10.1080/16549716.2017.1345496] [PMID]
- Snowdon DA, Leggat SG, Taylor NF. Does clinical supervision of healthcare professionals improve effectiveness of care and patient experience? A systematic review. BMC Health Services Research. 2017; 17(1):786. [DOI:10.1186/s12913-017-2739-5] [PMID]
- Health Communication Capacity Collaborative (HC3). Factors impacting the effectiveness of health care worker behavior change: A literature review. Baltimore: Johns Hopkins Center for Communication Programs; 2016. [Link]
- Mselle L, Sirili N, Anaeli A, Massawe S. Understanding barriers to implementing referral procedures in the rural and semiurban district hospitals in Tanzania: Experiences of healthcare providers working in maternity units. Plos One. 2021; 16(8):e0255475. [DOI:10.1371/journal.pone.0255475] [PMID]
- Daniels AA, Abuosi A. Improving emergency obstetric referral systems in low and middle income countries: A qualitative study in a tertiary health facility in Ghana. BMC Health Services Research. 2020; 20(1):32. [DOI:10.1186/s12913-020-4886-3] [PMID]
- Slyngstad L, Helgheim BI. How do different health record systems affect home health care? A cross-sectional study of electronic- versus manual documentation system. International Journal of General Medicine. 2022; 15:1945-1956.[DOI:10.2147/IJGM.S346366] [PMID]
- Shihundla RC, Lebese RT, Maputle MS. Effects of increased nurses’ workload on quality documentation of patient information at selected Primary Health Care facilities in Vhembe District, Limpopo Province. Curationis. 2016; 39(1):1545. [DOI:10.4102/curationis.v39i1.1545] [PMID]
- Michel-Schuldt M, McFadden A, Renfrew M, Homer C. The provision of midwife-led care in low-and middle-income countries: An integrative review. Midwifery. 2020; 84:102659.[DOI:10.1016/j.midw.2020.102659] [PMID]
- Dahlberg U, Aune I. The woman’s birth experience-The effect of interpersonal relationships and continuity of care. Midwifery. 2013; 29(4):407-15. [DOI:10.1016/j.midw.2012.09.006] [PMID]
- Perdok H, Verhoeven JC, van Dillen J, Schuitmaker JT, Hoogendoorn K, Colli J, et al. Continuity of care is an important and distinct aspect of childbirth experience: Findings of a survey evaluating experienced continuity of care, experienced quality of care and women’s perception of labor. BMC Pregnancy & Childbirth. 2018; 18(1):13. [DOI:10.1186/s12884-017-1615-y] [PMID]
Type of Study: Orginal Article |
Subject:
● Service Quality
Received: 2023/10/14 | Accepted: 2024/01/8 | Published: 2024/07/1
Received: 2023/10/14 | Accepted: 2024/01/8 | Published: 2024/07/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






