Volume 15, Issue 1 (Jan & Feb 2025)
J Research Health 2025, 15(1): 71-80 |
Back to browse issues page
Ethics code: KEC.2023.6A2
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bulut S, Saadati N, Al-Dossary S A, Coelho O, Rostami M, Parsakia K, et al . Introspective Awareness and Its Predictive Power on Health Anxiety: A Cross-sectional Study. J Research Health 2025; 15 (1) :71-80
URL: http://jrh.gmu.ac.ir/article-1-2529-en.html
URL: http://jrh.gmu.ac.ir/article-1-2529-en.html
Sefa Bulut1 

 , Nadereh Saadati2
, Nadereh Saadati2 

 , Saeed Abdullah Al-Dossary3
, Saeed Abdullah Al-Dossary3 

 , Olga Coelho4
, Olga Coelho4 

 , Mehdi Rostami5
, Mehdi Rostami5 

 , Kamdin Parsakia1
, Kamdin Parsakia1 

 , Zohreh Zadhasn1
, Zohreh Zadhasn1 

 , Seyed Hadi Seyed Ali Tabar1
, Seyed Hadi Seyed Ali Tabar1 

 , Parichehr Mehdi Abadi6
, Parichehr Mehdi Abadi6 




 , Nadereh Saadati2
, Nadereh Saadati2 

 , Saeed Abdullah Al-Dossary3
, Saeed Abdullah Al-Dossary3 

 , Olga Coelho4
, Olga Coelho4 

 , Mehdi Rostami5
, Mehdi Rostami5 

 , Kamdin Parsakia1
, Kamdin Parsakia1 

 , Zohreh Zadhasn1
, Zohreh Zadhasn1 

 , Seyed Hadi Seyed Ali Tabar1
, Seyed Hadi Seyed Ali Tabar1 

 , Parichehr Mehdi Abadi6
, Parichehr Mehdi Abadi6 


1- Department of Counseling Psychology, School of Education, Counseling Center, Ibn Haldun University, Istanbul, Turkey.
2- Department of Psychology and Counseling, KMAN Research Institute, Richmond Hill, Canada.
3- Department of Psychology, College of Education, University of Ha’il, Ha’il, Saudi Arabi.
4- Faculty of Psychology, Research Center for Psychological Science CICPSI), University of Lisbon, Lisbon, Portugal.
5- Department of Psychology and Counseling, KMAN Research Institute, Richmond Hill, Canada. ,mehdirostami@kmanresce.ca
6- Department of Psychology, School of Psychology, University of East London, London, UK.
2- Department of Psychology and Counseling, KMAN Research Institute, Richmond Hill, Canada.
3- Department of Psychology, College of Education, University of Ha’il, Ha’il, Saudi Arabi.
4- Faculty of Psychology, Research Center for Psychological Science CICPSI), University of Lisbon, Lisbon, Portugal.
5- Department of Psychology and Counseling, KMAN Research Institute, Richmond Hill, Canada. ,
6- Department of Psychology, School of Psychology, University of East London, London, UK.
Full-Text [PDF 762 kb]
(670 Downloads)
| Abstract (HTML) (2730 Views)
Full-Text: (572 Views)
Introduction
Health anxiety, characterized by excessive worry about having a serious illness, has a significant prevalence in the general population, affecting approximately 4-6% of individuals. During the COVID-19 pandemic, the prevalence of health anxiety increased markedly due to the pervasive fear of infection and uncertainty about the disease [1-3]. Health anxiety can lead to substantial mental health challenges, including increased levels of generalized anxiety, depression, and stress [4, 5]. It can also result in frequent medical consultations and unnecessary medical tests, increasing the burden on healthcare systems. Understanding the prevalence and impact of health anxiety underscores the importance of studying this condition, especially in the context of the COVID-19 pandemic and post-pandemic period [1, 6, 7].
The concepts of health anxiety and introspective awareness occupy a pivotal position in contemporary psychological research, especially in the context of their impact on mental health during the COVID-19 pandemic and post-pandemic period. Health anxiety, broadly defined as the misinterpretation of normal bodily sensations as dangerous [3, 8-10], has emerged prominently during the pandemic, with studies noting a significant increase in its prevalence across different populations [4, 7, 11, 12]. Introspective awareness, or the ability to notice and accurately interpret bodily signals [6, 13, 14], plays a crucial role in managing health anxiety, as it influences how individuals perceive and respond to their health-related fears.
Health anxiety can be understood through cognitive-behavioral frameworks that emphasize the role of misinterpretations of bodily sensations and the subsequent behavioral responses that maintain anxiety [8]. The COVID-19 pandemic has intensified these responses [15], giving rise to what Albery et al. described as a “COVID-19 anxiety syndrome”, characterized by an excessive focus on bodily sensations, avoidance behaviors, and reassurance seeking [11]. Such heightened health anxiety affects not only individuals with pre-existing anxiety and mood disorders [5, 8, 16] but also a broad range of demographic groups, influenced by factors like age, gender, and ethnicity [1].
On the other hand, introspective awareness encompasses several dimensions, including the ability to attend to, interpret, and regulate one’s internal bodily sensations. The construct of introspective awareness draws from interoception theories, which examine the perception of internal bodily states, and their impact on emotional and cognitive functioning [13]. Enhanced introspective awareness, facilitated through practices, such as mindfulness, has been shown to mitigate the effects of psychological distress, including health anxiety [17].
The COVID-19 pandemic has significantly escalated health-related anxieties, with studies reporting a widespread increase in health anxiety symptoms across different populations [8, 11]. This rise is attributed to the pervasive fear of infection and the profound uncertainty surrounding the disease. For instance, Nikčević et al. found that health anxiety during the COVID-19 pandemic contributed to generalized anxiety and depressive symptoms, highlighting the extensive impact of the pandemic on mental health [2]. Similarly, Jin et al. reported that death anxiety, amplified by the pandemic, further exacerbates mental health challenges, underlining the complex interplay between health anxiety and broader psychological distress during such crises [18]. The literature also addresses the disparities in health anxiety experienced by various demographic groups. Barbek et al. conducted a systematic review and meta-analysis and revealed significant ethnic and migration-related inequalities in health anxiety, suggesting that these disparities are critical factors that should be considered in understanding and addressing health anxiety [1].
The role of introspective awareness in psychological well-being has been a focal point of research, particularly in the context of managing stress and anxiety. Garfinkel et al. elucidated the interoceptive dimensions across cardiac and respiratory axes, underscoring the importance of understanding bodily signals in psychological health [13]. Mindfulness, a practice that enhances introspective awareness, has been shown to serve as a protective factor against psychological distress, with age and gender moderating its effects [17, 19]. Moreover, Matiz et al. highlighted the positive impact of mindfulness meditation on mental health among female teachers during the COVID-19 outbreak in Italy, illustrating the potential of mindfulness in mitigating pandemic-related stress. The interaction between health anxiety and introspective awareness is complex [20]. Health anxiety often involves maladaptive interpretations of bodily sensations. However, enhanced introspective awareness, particularly through mindfulness, can provide a mechanism for managing these interpretations more effectively [17]. Cummings et al. and Polloni and Muraro explored the psychosocial impact of conditions like food allergies, which inherently involve heightened health anxiety and demand acute introspective awareness. These conditions underscore the critical need to balance accurate interpretation of bodily signals with the mitigation of unwarranted health anxiety [21, 22]. Recent studies have further explored this relationship. Ruan et al. examined the role of emotion regulation in the context of anxiety and depression among adolescents. Their findings suggest that difficulties in emotion regulation, closely tied to introspective awareness, significantly contribute to anxiety and depression, thereby highlighting the potential of introspective awareness in psychological interventions [23].
In summary, the current literature underscores the significance of health anxiety and introspective awareness in the context of the post-pandemic era, revealing a potential relationship between these constructs. The pandemic has not only intensified health anxiety but also spotlighted the importance of introspective awareness as a crucial component in managing such anxiety. Despite the growing recognition of health anxiety as a significant mental health concern, especially during the COVID-19 pandemic, there is a notable lack of research exploring the specific role of introspective awareness in this context. Theoretical frameworks suggest that a heightened awareness of bodily sensations can both alleviate and exacerbate anxiety, depending on the individual’s ability to accurately interpret these signals. Practically, this study addresses a critical gap by examining how specific components of introspective awareness influence health anxiety. The findings have substantial implications for mental health interventions and policy development [24], suggesting that enhancing introspective awareness through mindfulness practices and cognitive-behavioral techniques could be pivotal in reducing health anxiety. Furthermore, policymakers can leverage these insights to design community-based programs that promote mental well-being and resilience, especially in post-pandemic recovery efforts. This study not only contributes to the theoretical understanding of health anxiety but also offers practical solutions for improving mental health outcomes.
This review lays the groundwork for the present study, which aimed to explore the predictive relationship between introspective awareness components and health anxiety among residents of Richmond Hill, Ontario, Canada during the COVID-19 post-pandemic period. By doing so, the study seeks to enhance the body of research on health anxiety and introspective awareness, contributing valuable insights to the field.
Methods
Study design and participants
This study utilized a cross-sectional design to investigate the relationship between health anxiety and introspective awareness among individuals in Richmond Hill, Ontario, Canada from April to August 2023. The sample size was determined to be 350 participants who were selected via a convenient sampling method, based on recommendations from Morgan and Krejcie’s table for population-based studies. The inclusion criteria were adults aged 18 years and above, residing in Richmond Hill, Ontario, Canada, who provided informed consent to participate in the study. Participants were recruited through various channels, including social media platforms, local community centers, and universities, to ensure a diverse representation of the population. The study adhered to ethical guidelines established by the KMAN Research Institute, ensuring the protection of participants’ rights and confidentiality.
Measures
Demographic questionnaire
Participants completed a demographic questionnaire to provide information on key characteristics such as age, gender, educational background, and employment status. Specifically, age was categorized into four groups: 18-29 years, 30-39 years, 40-49 years, and 50 years and above. Gender was recorded as either male or female. Educational background was classified into four levels: High school diploma, college diploma, bachelor’s degree, and graduate degree. Employment status was also documented, with categories, including employed, unemployed, student, and retired. These demographic characteristics were essential for describing the sample and controlling for potential confounding variables in the analysis.
Health anxiety inventory (HAI)
The HAI, developed by Salkovskis et al. in 2002 [25], is a prominent measure designed to assess the severity of health anxiety. The HAI consists of 18 items divided into four subscales: Illness likelihood, illness severity, body vigilance, and reassurance seeking. Respondents rate each item on a four-point scale, reflecting the frequency and severity of their health anxiety symptoms. The HAI’s scoring system provides a total health anxiety score, with higher scores indicating greater anxiety. The total score can range from 0 to 54, with higher scores indicating greater levels of health anxiety. It determines mild, moderate, and severe levels based on the scores. The HAI categorizes health anxiety levels as mild, moderate, or severe, with moderate anxiety indicated by scores between 18 and 48. It has demonstrated high validity and reliability in numerous studies. The construct validity of the HAI has been supported through correlations with other measures of health anxiety and general anxiety. The internal consistency reliability (Cronbach’s α) of the HAI typically ranges from 0.88 to 0.92, indicating excellent reliability. Test-retest reliability over a period of several weeks shows coefficients between 0.80 and 0.85, confirming its stability over time. These values are based on sample sizes ranging from 200 to 500 participants in various studies [5, 7, 10].
Multidimensional assessment of interoceptive awareness (MAIA)
The MAIA is a validated instrument created by Mehling et al. in 2012 [26]. It comprises 32 items across eight subscales: Noticing, not-distracting, not-worrying, attention regulation, emotional awareness, self-regulation, body listening, and trusting. These subscales collectively assess an individual’s awareness of bodily sensations and their ability to regulate distress without becoming overwhelmed. Each item is scored on a 6-point Likert scale, from 0 (never) to 5 (always), with total scores indicating the level of introspective awareness. It has been validated in diverse populations, showing strong psychometric properties. The MAIA’s construct validity is supported through its correlations with measures of mindfulness, emotional awareness, and anxiety. The internal consistency reliability (Cronbach’s α) for the MAIA subscales ranges from 0.66 to 0.82, indicating acceptable to good reliability. Test-retest reliability over several weeks ranges from 0.60 to 0.75 for the subscales, based on sample sizes of 300 to 600 participants [27].
Data analysis
Data were analyzed using SPSS software, version 27. Initially, descriptive statistics were computed to summarize the demographic characteristics of the study sample and the main variables of interest. To examine the relationship between health anxiety (dependent variable) and each component of introspective awareness (independent variables), Pearson correlation coefficients were calculated. These analyses allowed us to determine the strength and direction of the associations between health anxiety and the various dimensions of introspective awareness.
Subsequently, linear regression analysis was performed to explore the predictive value of introspective awareness components on health anxiety. Specifically, a model was constructed with health anxiety as the dependent variable and two independent variables representing key aspects of introspective awareness. The selection of these variables was informed by the correlation analysis to ensure relevance and potential predictive power. The regression model aimed to elucidate the extent to which introspective awareness components could predict levels of health anxiety, adjusting for potential confounders identified during the study.
All statistical tests were two-tailed, and P<0.05 was considered statistically significant. The analyses were meticulously carried out, ensuring adherence to the principles of ethical research and data integrity, under the approved ethics code from the KMAN Research Institute.
Results
The study’s participant pool comprised 350 individuals from Richmond Hill, Ontario, Canada. Of these, 187(53.43%) were female, and 163(46.57%) were male, highlighting a slight female predominance in our sample. The age distribution of participants was as follows: 18-29 years (112 individuals, 32.00%), 30-39 years (89 individuals, 25.43%), 40-49 years (78 individuals, 22.29%), and 50 years and above (71 individuals, 20.28%). Regarding educational background, the majority of participants had completed some form of post-secondary education, with 120 individuals (34.29%) holding a bachelor’s degree, 95(27.14%) possessing a college diploma, and 65(18.57%) having completed a graduate degree. The remaining 70 participants (20%) reported having a high school diploma as their highest level of education.
The descriptive statistics for our study variables, including health anxiety and the eight subscales of introspective awareness, are summarized in Table 1.
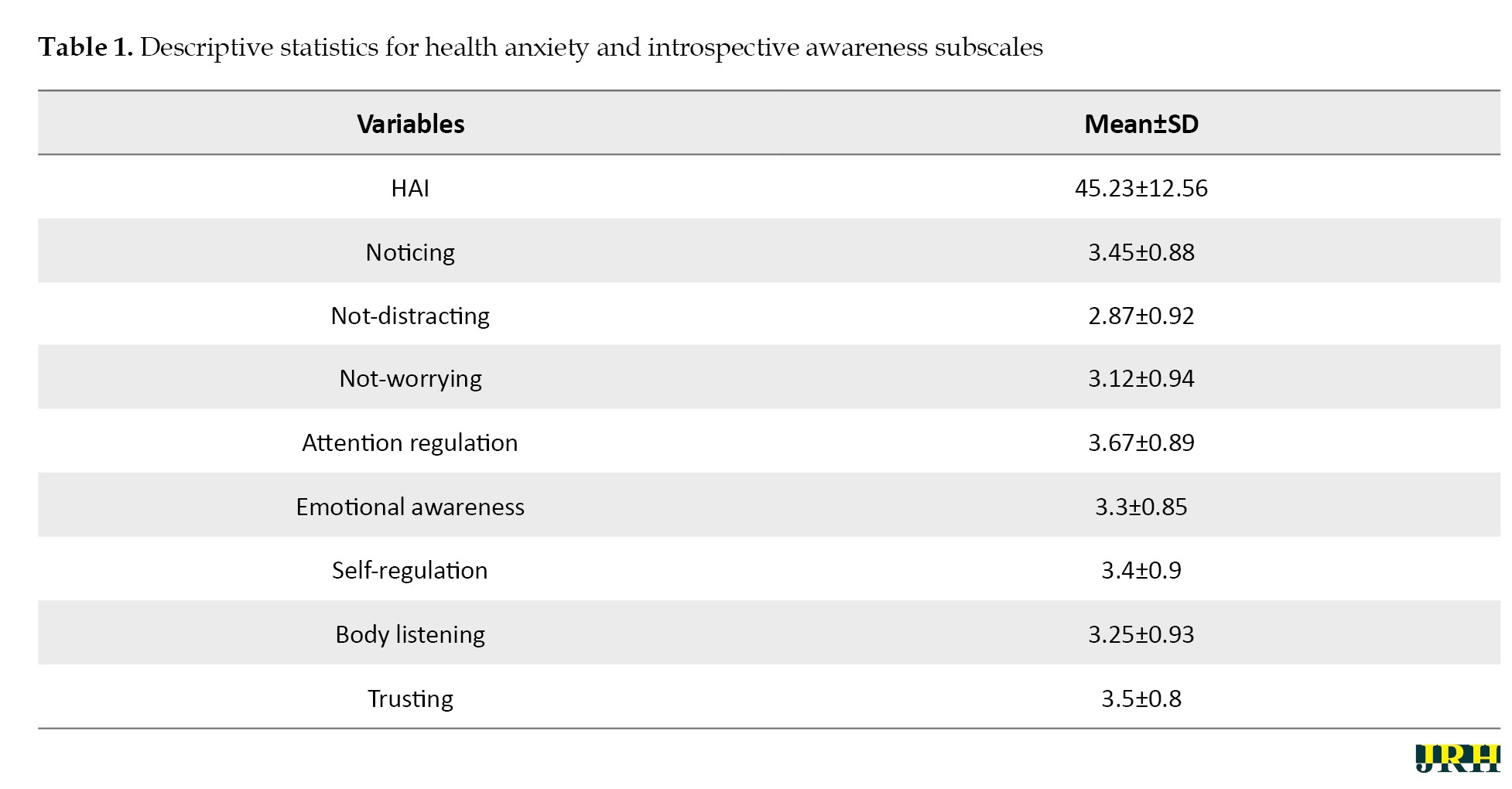
The HAI scores among participants averaged 45.23±12.56, indicating a moderate level of health anxiety within the sample. Among the introspective awareness components, attention regulation was reported highest with a mean score of 3.67±0.89, suggesting a relatively strong ability among participants to control attention in relation to bodily sensations. The lowest average score was observed for not-distracting, with a mean of 2.87±0.92, indicating a challenge in ignoring bodily sensations. These statistics provide a foundational understanding of the sample’s general health anxiety levels and their introspective awareness capacities.
Prior to conducting the primary analyses, we meticulously checked and confirmed the assumptions necessary for Pearson correlation and linear regression analyses. For the Pearson correlation, the normality of the variables was assessed, with skewness values ranging from -0.45 to 0.52 and kurtosis values from -0.60 to 0.55, all within acceptable ranges. These results indicated that the data distribution did not significantly deviate from normality. The linearity assumption was also satisfied, as evidenced by scatterplots showing linear relationships between health anxiety and each component of introspective awareness. For linear regression analysis, the assumption of multicollinearity was assessed using the variance inflation factor (VIF), with all values found to be below the threshold of five (ranging from 1.08 to 2.34), suggesting no concerning multicollinearity among the independent variables. Additionally, the Durbin-Watson statistic was 1.98, indicating no autocorrelation in the residuals. Homoscedasticity was confirmed through visual inspection of a plot of standardized residuals against predicted values, showing a random scatter of points. These checks ensured the robustness and reliability of the subsequent statistical analyses, confirming that the foundational assumptions of Pearson correlation and linear regression were adequately met in this study.
Table 2 presents the Pearson correlation coefficients between health anxiety and each independent variable, indicating diverse relationships.
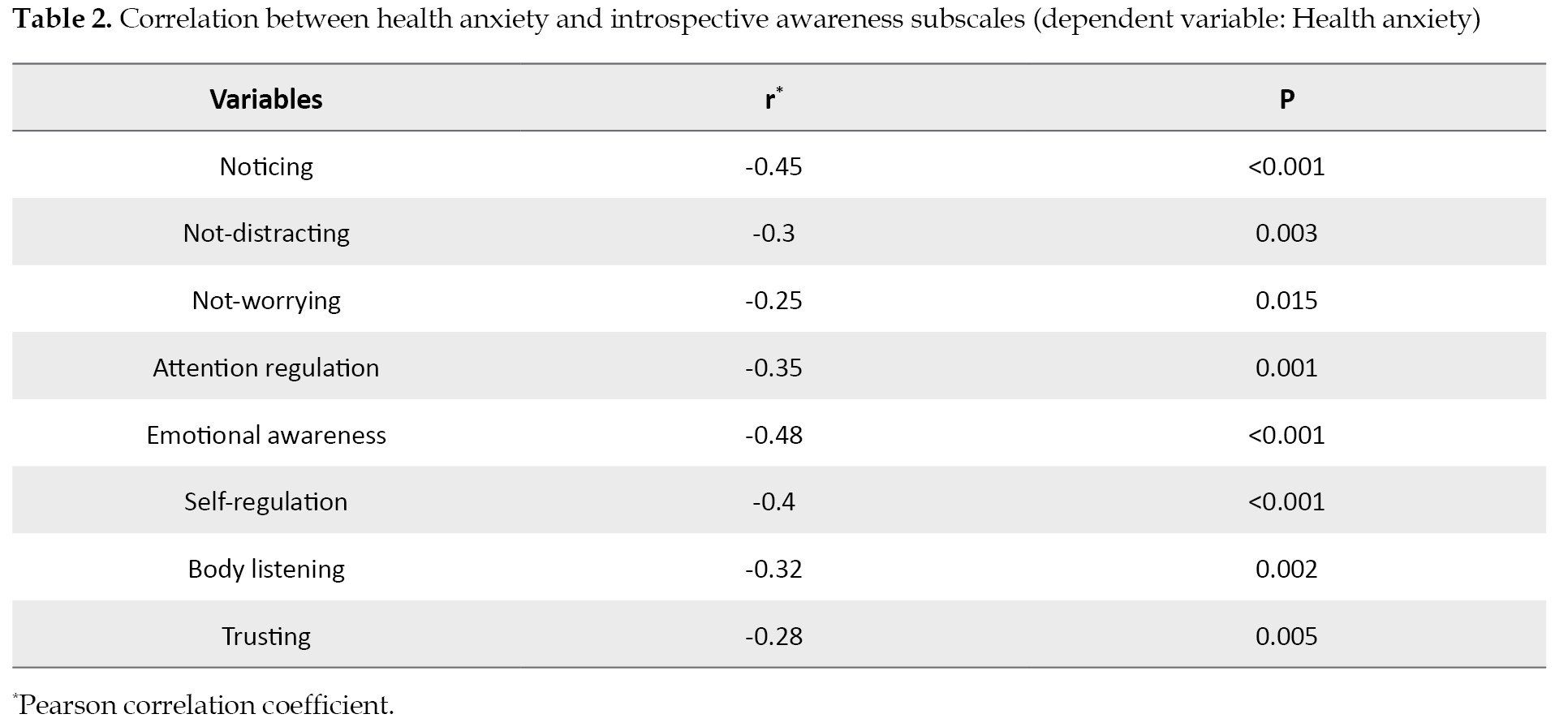
Notably, emotional awareness showed the strongest negative correlation with health anxiety (r=-0.48, P<0.001), suggesting that higher emotional awareness is associated with lower health anxiety levels. Conversely, noticing also demonstrated a significant negative correlation (r=-0.45, P<0.001), indicating that an increased awareness of internal bodily sensations correlated with reduced health anxiety. These findings highlight the intricate relationships between different facets of introspective awareness and health anxiety, suggesting potential areas for intervention.
The regression analysis summary, as detailed in Table 3, revealed that the model explained a substantial portion of the variance in health anxiety (R2=0.42, R2adj=0.41, F(2, 347)=48.35, P<0.001).
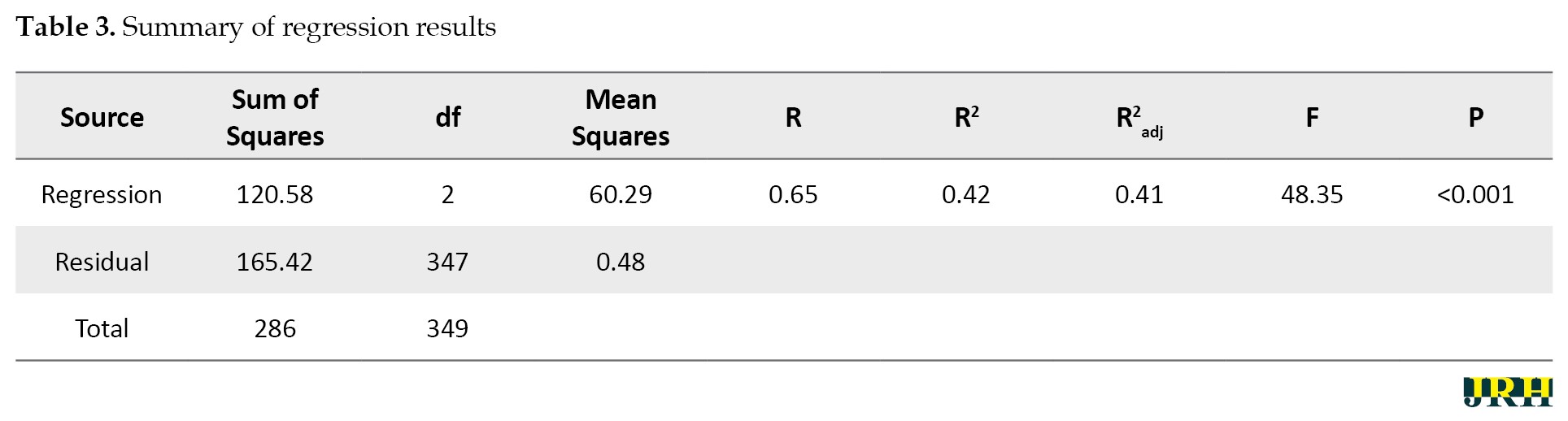
This indicates a strong model fit, with approximately 42% of the variance in health anxiety scores accounted for by the predictors. The significant F-statistic confirms the model’s overall statistical significance, suggesting that the included components of introspective awareness had a meaningful predictive relationship with health anxiety levels among the participants.
In the multivariate regression analysis detailed in Table 4, only noticing and emotional awareness were significant predictors of health anxiety.
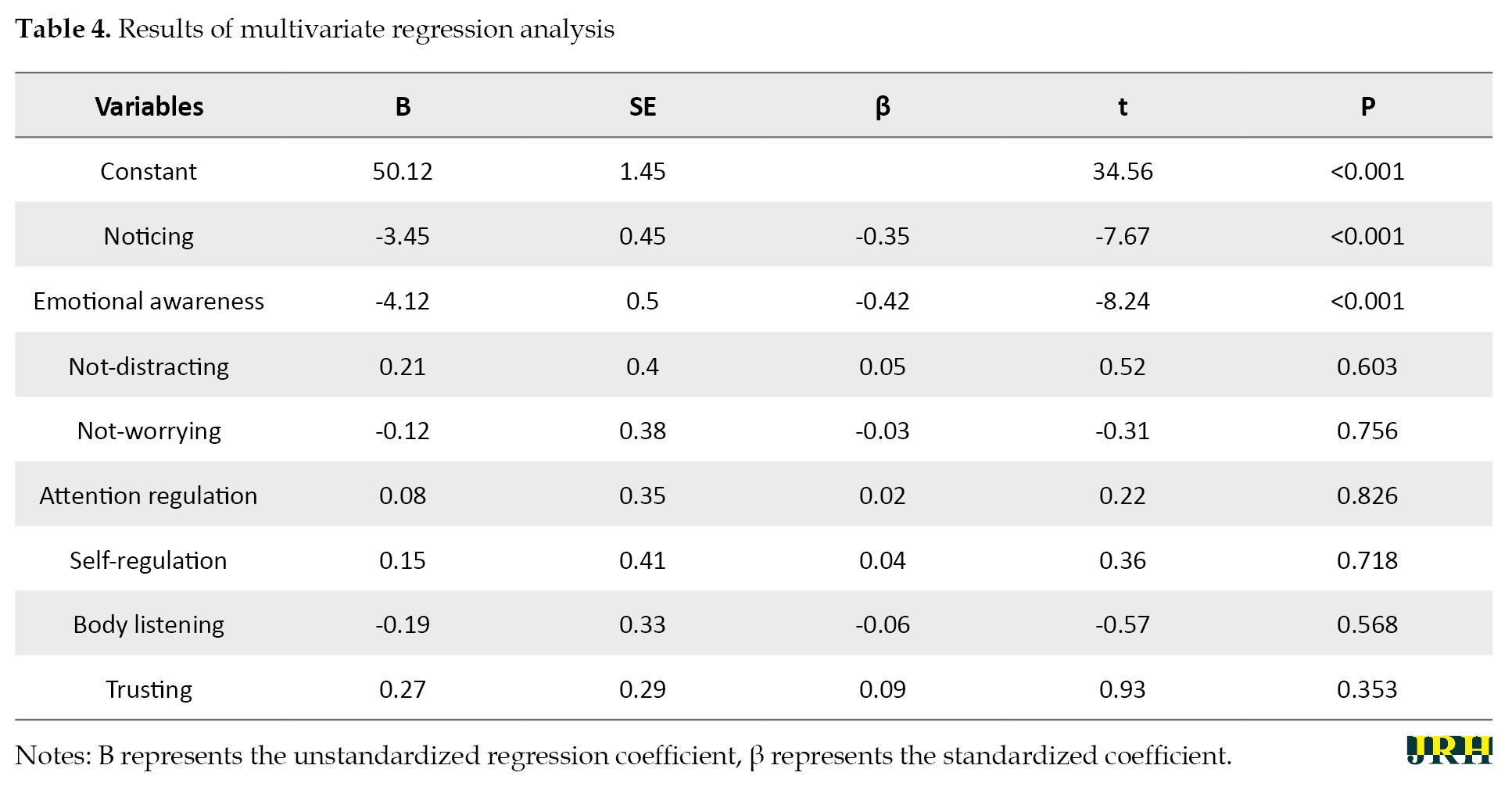
Specifically, for every unit increase in noticing, there was a significant decrease in health anxiety scores (B=-3.45, SE=0.45, β=-0.35, t=-7.67, P<0.001). Similarly, an increase in emotional awareness was associated with a significant reduction in health anxiety (B=-4.12, SE=0.50, β=-0.42, t=-8.24, P<0.001). These results underscore the protective role of noticing and emotional awareness against health anxiety, emphasizing their importance in psychological interventions aimed at managing health-related anxieties.
Conversely, the six other subscales—not-distracting, not-worrying, attention regulation, self-regulation, body listening, and trusting—did not present a significant predictive value for health anxiety, with p-values ranging from 0.353 to 0.826 (P>0.05). These results indicate that while certain aspects of introspective awareness are pivotal in the context of health anxiety, others may not directly influence its levels. Specifically, the ability to distract oneself from or refrain from worrying about bodily sensations, regulate attention or emotional responses, listen to bodily signals, or trust in those signals does not significantly predict health anxiety in this sample.
Discussion
The present study’s findings illuminate the intricate relationship between introspective awareness and health anxiety among residents of Richmond Hill, Ontario, Canada. Our results significantly underscore the predictive power of certain components of introspective awareness against health anxiety, resonating with and expanding upon the existing literature. Specifically, the dimensions of noticing and emotional awareness within introspective awareness emerged as significant predictors of health anxiety levels in our sample. These findings are discussed in the context of the theoretical frameworks and empirical evidence from previous studies, as outlined below.
The significant prediction of health anxiety by the introspective awareness components aligns with the conceptualizations of Garfinkel et al. [13], who highlighted the importance of interoceptive awareness in understanding and regulating emotional and physical states. Our study extends this notion by explicitly linking introspective awareness to health anxiety, suggesting that enhanced awareness and understanding of bodily sensations may serve as a protective factor against the exacerbation of health anxiety. This is particularly relevant in the context of a global health crisis, where fears related to health are heightened [8, 11].
The relationship between introspective awareness and health anxiety is influenced by various socio-cultural and environmental factors. Media exposure during the pandemic has amplified health anxiety by perpetuating fear and uncertainty. Social support networks, such as family and community connections, provide emotional and practical support, which can mitigate anxiety. Access to community resources, including mental health services and educational programs, can enhance introspective awareness and offer coping strategies [1]. These factors interact with individual differences to shape mental health outcomes, highlighting the importance of a comprehensive approach to addressing health anxiety in the post-pandemic period.
In our study, six subscales of introspective awareness—not-distracting, not-worrying, attention regulation, self-regulation, body listening, and trusting—did not significantly predict health anxiety among participants. This finding diverges from some expectations based on prior research and theoretical frameworks, suggesting a nuanced relationship between various facets of introspective awareness and health anxiety that may depend on specific contexts or individual differences. Not-distracting and not-worrying subscales, which pertain to the ability to divert attention away from distressing bodily sensations and worries about health, respectively, did not show a significant predictive relationship with health anxiety. This could suggest that during heightened states of global health crises, such as the COVID-19 pandemic, the general tendency to avoid or ignore health-related thoughts and sensations may not effectively mitigate health anxiety. This is consistent with the findings of Asmundson et al., who noted that avoidance behaviors could potentially exacerbate health anxiety in the context of a pandemic. Similarly, the lack of significant findings for attention regulation, self-regulation, and body listening can indicate that the capacity to regulate attention and respond to bodily signals does not directly impact health anxiety levels in the same context [8]. This could be due to the overwhelming nature of pandemic-related information and stressors, which may overshadow the benefits of these introspective abilities. Gulliver et al. highlighted the complexity of mental health help-seeking behaviors, suggesting that even well-developed self-regulation and attention to bodily cues might not suffice to alleviate health anxiety without targeted mental health support [28]. The trusting subscale, reflecting confidence in the body’s reliability and health, also did not significantly predict health anxiety. In the post-pandemic period, external factors such as pervasive health threats and uncertainty may undermine this trust, regardless of an individual’s baseline introspective awareness. This finding is consistent with that of Conversano et al. who emphasized that the unique stressors associated with the COVID-19 pandemic necessitate specific coping strategies beyond general trust in bodily signals [19].
In contrast, the noticing and emotional awareness subscales demonstrated a significant predictive role in health anxiety. Noticing, defined as the awareness of internal bodily sensations, was negatively associated with health anxiety. This suggests that a heightened awareness and accurate interpretation of bodily signals may serve as a buffer against the misinterpretation of such sensations as indicative of illness, a core feature of health anxiety as described by Cummings et al. [21]. This finding underscores the importance of mindfulness and bodily awareness practices in mitigating health anxiety, supporting Hofmann et al. ‘s assertion regarding the effectiveness of mindfulness-based therapy in reducing anxiety symptoms. Emotional awareness, or the ability to understand and differentiate emotional responses to bodily sensations, also significantly predicted lower health anxiety levels. This highlights the critical role of emotional processing in managing health anxiety, suggesting that individuals who can accurately identify and regulate their emotional responses to health-related information may be better equipped to manage health anxiety [17]. This is consistent with the protective role of emotional intelligence components against psychological distress, as reported by Taheri et al. [29].
Our findings also resonate with the research on mindfulness and its impact on psychological well-being [17]. Mindfulness practices, which enhance introspective awareness, have been shown to reduce symptoms of anxiety and depression, including those related to health concerns. The significant predictive relationship observed in our study suggests that mindfulness interventions could be particularly beneficial for individuals experiencing high levels of health anxiety. The implications of our findings extend to considerations of health disparities, as highlighted by Barbek et al. Given the varying levels of health anxiety reported among different demographic groups, interventions aimed at enhancing introspective awareness may need to be tailored to address the specific needs and contexts of these groups, thereby contributing to more equitable mental health outcomes [1].
Introspective awareness may influence health anxiety through several potential mediating mechanisms. Effective emotion regulation strategies are likely employed by individuals with high introspective awareness, reducing the intensity of health anxiety. Additionally, a strong sense of introspective awareness can enhance perceived control over health outcomes, serving as a buffer against the uncertainty associated with health concerns [30-32]. Cognitive appraisals of bodily sensations also play a significant role; individuals with high introspective awareness are more likely to interpret these sensations accurately and less catastrophically, thereby reducing anxiety. Understanding these mediating mechanisms can inform more targeted interventions [32-34].
Conclusion
The primary aim of this study was to investigate the predictive relationship between components of introspective awareness and levels of health anxiety among residents of Richmond Hill, Ontario, Canada, during the COVID-19 post-pandemic period. Our findings revealed that specific dimensions of introspective awareness, namely noticing and emotional awareness, significantly predict health anxiety, suggesting that heightened awareness and understanding of bodily sensations and emotional responses to these sensations can play a crucial role in managing health anxiety.
Future research should address these limitations by adopting longitudinal study designs to better understand the causal relationships between introspective awareness and health anxiety over time. Expanding the study to include diverse geographic locations and populations would enhance the generalizability of the findings. Additionally, incorporating objective measures of introspective awareness and health anxiety, alongside self-reported measures, could provide a more comprehensive understanding of these constructs. Investigating other potential mediators and moderators, such as social support and coping strategies, could also offer deeper insights into the mechanisms underlying the relationship between introspective awareness and health anxiety.
The findings of this study have several practical implications for psychological practice, especially in the context of a global health crisis. Healthcare professionals could consider integrating mindfulness-based interventions into their practice to enhance introspective awareness among individuals with high levels of health anxiety. Tailoring these interventions to meet the specific needs of diverse demographic groups could also help in addressing health disparities. Additionally, psychoeducation on recognizing and interpreting bodily sensations accurately could be beneficial in reducing health anxiety. Implementing these practices could contribute to improved mental health outcomes and resilience in facing ongoing and future health challenges. Individuals should be encouraged to adopt mindfulness practices, such as mindfulness meditation and body scanning, to enhance their introspective awareness and reduce health anxiety. Healthcare professionals should integrate cognitive-behavioral techniques into therapeutic interventions to help patients reframe their perceptions of bodily sensations and manage anxiety effectively. Policymakers should develop and implement community-based interventions to increase public awareness of mental health resources and ensure that mental health support is accessible and culturally sensitive, integrating these services into post-pandemic recovery plans. The implications of the findings should also be considered within a cross-cultural framework [35]. Cultural beliefs and values significantly shape how individuals experience and express health anxiety and introspective awareness. In cultures that emphasize community and collective well-being, social support networks may play a more pronounced role in mitigating health anxiety. When developing interventions, it is crucial to consider cultural differences in the conceptualization of health-related concerns and employ culturally sensitive approaches. Incorporating culturally relevant practices and addressing specific cultural stressors can enhance the effectiveness of interventions, ensuring they are respectful and effective across diverse cultural backgrounds [36, 37]. This approach is essential for developing equitable mental health strategies in the post-pandemic era.
This study, while informative, is subject to several limitations. The cross-sectional design restricts our ability to infer causality between introspective awareness and health anxiety. Additionally, the sample was drawn from a single geographic location, which may limit the generalizability of the findings to other populations or contexts. Another limitation is the reliance on self-reported measures, which are susceptible to biases, such as social desirability or recall bias.
Ethical Considerations
Compliance with ethical guidelines
The study's protocol adhered to the principles outlined in the Helsinki Declaration, which provides guidelines for ethical research involving human participants. The study was conducted according to the ethical guidelines set forth by the KMAN Research Institute, Richmond Hill, Canada (Code: KEC.2023.6A2), ensuring the protection of participants’ rights and confidentiality.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their gratitude to all individuals who helped us to do the project.
References
Health anxiety, characterized by excessive worry about having a serious illness, has a significant prevalence in the general population, affecting approximately 4-6% of individuals. During the COVID-19 pandemic, the prevalence of health anxiety increased markedly due to the pervasive fear of infection and uncertainty about the disease [1-3]. Health anxiety can lead to substantial mental health challenges, including increased levels of generalized anxiety, depression, and stress [4, 5]. It can also result in frequent medical consultations and unnecessary medical tests, increasing the burden on healthcare systems. Understanding the prevalence and impact of health anxiety underscores the importance of studying this condition, especially in the context of the COVID-19 pandemic and post-pandemic period [1, 6, 7].
The concepts of health anxiety and introspective awareness occupy a pivotal position in contemporary psychological research, especially in the context of their impact on mental health during the COVID-19 pandemic and post-pandemic period. Health anxiety, broadly defined as the misinterpretation of normal bodily sensations as dangerous [3, 8-10], has emerged prominently during the pandemic, with studies noting a significant increase in its prevalence across different populations [4, 7, 11, 12]. Introspective awareness, or the ability to notice and accurately interpret bodily signals [6, 13, 14], plays a crucial role in managing health anxiety, as it influences how individuals perceive and respond to their health-related fears.
Health anxiety can be understood through cognitive-behavioral frameworks that emphasize the role of misinterpretations of bodily sensations and the subsequent behavioral responses that maintain anxiety [8]. The COVID-19 pandemic has intensified these responses [15], giving rise to what Albery et al. described as a “COVID-19 anxiety syndrome”, characterized by an excessive focus on bodily sensations, avoidance behaviors, and reassurance seeking [11]. Such heightened health anxiety affects not only individuals with pre-existing anxiety and mood disorders [5, 8, 16] but also a broad range of demographic groups, influenced by factors like age, gender, and ethnicity [1].
On the other hand, introspective awareness encompasses several dimensions, including the ability to attend to, interpret, and regulate one’s internal bodily sensations. The construct of introspective awareness draws from interoception theories, which examine the perception of internal bodily states, and their impact on emotional and cognitive functioning [13]. Enhanced introspective awareness, facilitated through practices, such as mindfulness, has been shown to mitigate the effects of psychological distress, including health anxiety [17].
The COVID-19 pandemic has significantly escalated health-related anxieties, with studies reporting a widespread increase in health anxiety symptoms across different populations [8, 11]. This rise is attributed to the pervasive fear of infection and the profound uncertainty surrounding the disease. For instance, Nikčević et al. found that health anxiety during the COVID-19 pandemic contributed to generalized anxiety and depressive symptoms, highlighting the extensive impact of the pandemic on mental health [2]. Similarly, Jin et al. reported that death anxiety, amplified by the pandemic, further exacerbates mental health challenges, underlining the complex interplay between health anxiety and broader psychological distress during such crises [18]. The literature also addresses the disparities in health anxiety experienced by various demographic groups. Barbek et al. conducted a systematic review and meta-analysis and revealed significant ethnic and migration-related inequalities in health anxiety, suggesting that these disparities are critical factors that should be considered in understanding and addressing health anxiety [1].
The role of introspective awareness in psychological well-being has been a focal point of research, particularly in the context of managing stress and anxiety. Garfinkel et al. elucidated the interoceptive dimensions across cardiac and respiratory axes, underscoring the importance of understanding bodily signals in psychological health [13]. Mindfulness, a practice that enhances introspective awareness, has been shown to serve as a protective factor against psychological distress, with age and gender moderating its effects [17, 19]. Moreover, Matiz et al. highlighted the positive impact of mindfulness meditation on mental health among female teachers during the COVID-19 outbreak in Italy, illustrating the potential of mindfulness in mitigating pandemic-related stress. The interaction between health anxiety and introspective awareness is complex [20]. Health anxiety often involves maladaptive interpretations of bodily sensations. However, enhanced introspective awareness, particularly through mindfulness, can provide a mechanism for managing these interpretations more effectively [17]. Cummings et al. and Polloni and Muraro explored the psychosocial impact of conditions like food allergies, which inherently involve heightened health anxiety and demand acute introspective awareness. These conditions underscore the critical need to balance accurate interpretation of bodily signals with the mitigation of unwarranted health anxiety [21, 22]. Recent studies have further explored this relationship. Ruan et al. examined the role of emotion regulation in the context of anxiety and depression among adolescents. Their findings suggest that difficulties in emotion regulation, closely tied to introspective awareness, significantly contribute to anxiety and depression, thereby highlighting the potential of introspective awareness in psychological interventions [23].
In summary, the current literature underscores the significance of health anxiety and introspective awareness in the context of the post-pandemic era, revealing a potential relationship between these constructs. The pandemic has not only intensified health anxiety but also spotlighted the importance of introspective awareness as a crucial component in managing such anxiety. Despite the growing recognition of health anxiety as a significant mental health concern, especially during the COVID-19 pandemic, there is a notable lack of research exploring the specific role of introspective awareness in this context. Theoretical frameworks suggest that a heightened awareness of bodily sensations can both alleviate and exacerbate anxiety, depending on the individual’s ability to accurately interpret these signals. Practically, this study addresses a critical gap by examining how specific components of introspective awareness influence health anxiety. The findings have substantial implications for mental health interventions and policy development [24], suggesting that enhancing introspective awareness through mindfulness practices and cognitive-behavioral techniques could be pivotal in reducing health anxiety. Furthermore, policymakers can leverage these insights to design community-based programs that promote mental well-being and resilience, especially in post-pandemic recovery efforts. This study not only contributes to the theoretical understanding of health anxiety but also offers practical solutions for improving mental health outcomes.
This review lays the groundwork for the present study, which aimed to explore the predictive relationship between introspective awareness components and health anxiety among residents of Richmond Hill, Ontario, Canada during the COVID-19 post-pandemic period. By doing so, the study seeks to enhance the body of research on health anxiety and introspective awareness, contributing valuable insights to the field.
Methods
Study design and participants
This study utilized a cross-sectional design to investigate the relationship between health anxiety and introspective awareness among individuals in Richmond Hill, Ontario, Canada from April to August 2023. The sample size was determined to be 350 participants who were selected via a convenient sampling method, based on recommendations from Morgan and Krejcie’s table for population-based studies. The inclusion criteria were adults aged 18 years and above, residing in Richmond Hill, Ontario, Canada, who provided informed consent to participate in the study. Participants were recruited through various channels, including social media platforms, local community centers, and universities, to ensure a diverse representation of the population. The study adhered to ethical guidelines established by the KMAN Research Institute, ensuring the protection of participants’ rights and confidentiality.
Measures
Demographic questionnaire
Participants completed a demographic questionnaire to provide information on key characteristics such as age, gender, educational background, and employment status. Specifically, age was categorized into four groups: 18-29 years, 30-39 years, 40-49 years, and 50 years and above. Gender was recorded as either male or female. Educational background was classified into four levels: High school diploma, college diploma, bachelor’s degree, and graduate degree. Employment status was also documented, with categories, including employed, unemployed, student, and retired. These demographic characteristics were essential for describing the sample and controlling for potential confounding variables in the analysis.
Health anxiety inventory (HAI)
The HAI, developed by Salkovskis et al. in 2002 [25], is a prominent measure designed to assess the severity of health anxiety. The HAI consists of 18 items divided into four subscales: Illness likelihood, illness severity, body vigilance, and reassurance seeking. Respondents rate each item on a four-point scale, reflecting the frequency and severity of their health anxiety symptoms. The HAI’s scoring system provides a total health anxiety score, with higher scores indicating greater anxiety. The total score can range from 0 to 54, with higher scores indicating greater levels of health anxiety. It determines mild, moderate, and severe levels based on the scores. The HAI categorizes health anxiety levels as mild, moderate, or severe, with moderate anxiety indicated by scores between 18 and 48. It has demonstrated high validity and reliability in numerous studies. The construct validity of the HAI has been supported through correlations with other measures of health anxiety and general anxiety. The internal consistency reliability (Cronbach’s α) of the HAI typically ranges from 0.88 to 0.92, indicating excellent reliability. Test-retest reliability over a period of several weeks shows coefficients between 0.80 and 0.85, confirming its stability over time. These values are based on sample sizes ranging from 200 to 500 participants in various studies [5, 7, 10].
Multidimensional assessment of interoceptive awareness (MAIA)
The MAIA is a validated instrument created by Mehling et al. in 2012 [26]. It comprises 32 items across eight subscales: Noticing, not-distracting, not-worrying, attention regulation, emotional awareness, self-regulation, body listening, and trusting. These subscales collectively assess an individual’s awareness of bodily sensations and their ability to regulate distress without becoming overwhelmed. Each item is scored on a 6-point Likert scale, from 0 (never) to 5 (always), with total scores indicating the level of introspective awareness. It has been validated in diverse populations, showing strong psychometric properties. The MAIA’s construct validity is supported through its correlations with measures of mindfulness, emotional awareness, and anxiety. The internal consistency reliability (Cronbach’s α) for the MAIA subscales ranges from 0.66 to 0.82, indicating acceptable to good reliability. Test-retest reliability over several weeks ranges from 0.60 to 0.75 for the subscales, based on sample sizes of 300 to 600 participants [27].
Data analysis
Data were analyzed using SPSS software, version 27. Initially, descriptive statistics were computed to summarize the demographic characteristics of the study sample and the main variables of interest. To examine the relationship between health anxiety (dependent variable) and each component of introspective awareness (independent variables), Pearson correlation coefficients were calculated. These analyses allowed us to determine the strength and direction of the associations between health anxiety and the various dimensions of introspective awareness.
Subsequently, linear regression analysis was performed to explore the predictive value of introspective awareness components on health anxiety. Specifically, a model was constructed with health anxiety as the dependent variable and two independent variables representing key aspects of introspective awareness. The selection of these variables was informed by the correlation analysis to ensure relevance and potential predictive power. The regression model aimed to elucidate the extent to which introspective awareness components could predict levels of health anxiety, adjusting for potential confounders identified during the study.
All statistical tests were two-tailed, and P<0.05 was considered statistically significant. The analyses were meticulously carried out, ensuring adherence to the principles of ethical research and data integrity, under the approved ethics code from the KMAN Research Institute.
Results
The study’s participant pool comprised 350 individuals from Richmond Hill, Ontario, Canada. Of these, 187(53.43%) were female, and 163(46.57%) were male, highlighting a slight female predominance in our sample. The age distribution of participants was as follows: 18-29 years (112 individuals, 32.00%), 30-39 years (89 individuals, 25.43%), 40-49 years (78 individuals, 22.29%), and 50 years and above (71 individuals, 20.28%). Regarding educational background, the majority of participants had completed some form of post-secondary education, with 120 individuals (34.29%) holding a bachelor’s degree, 95(27.14%) possessing a college diploma, and 65(18.57%) having completed a graduate degree. The remaining 70 participants (20%) reported having a high school diploma as their highest level of education.
The descriptive statistics for our study variables, including health anxiety and the eight subscales of introspective awareness, are summarized in Table 1.
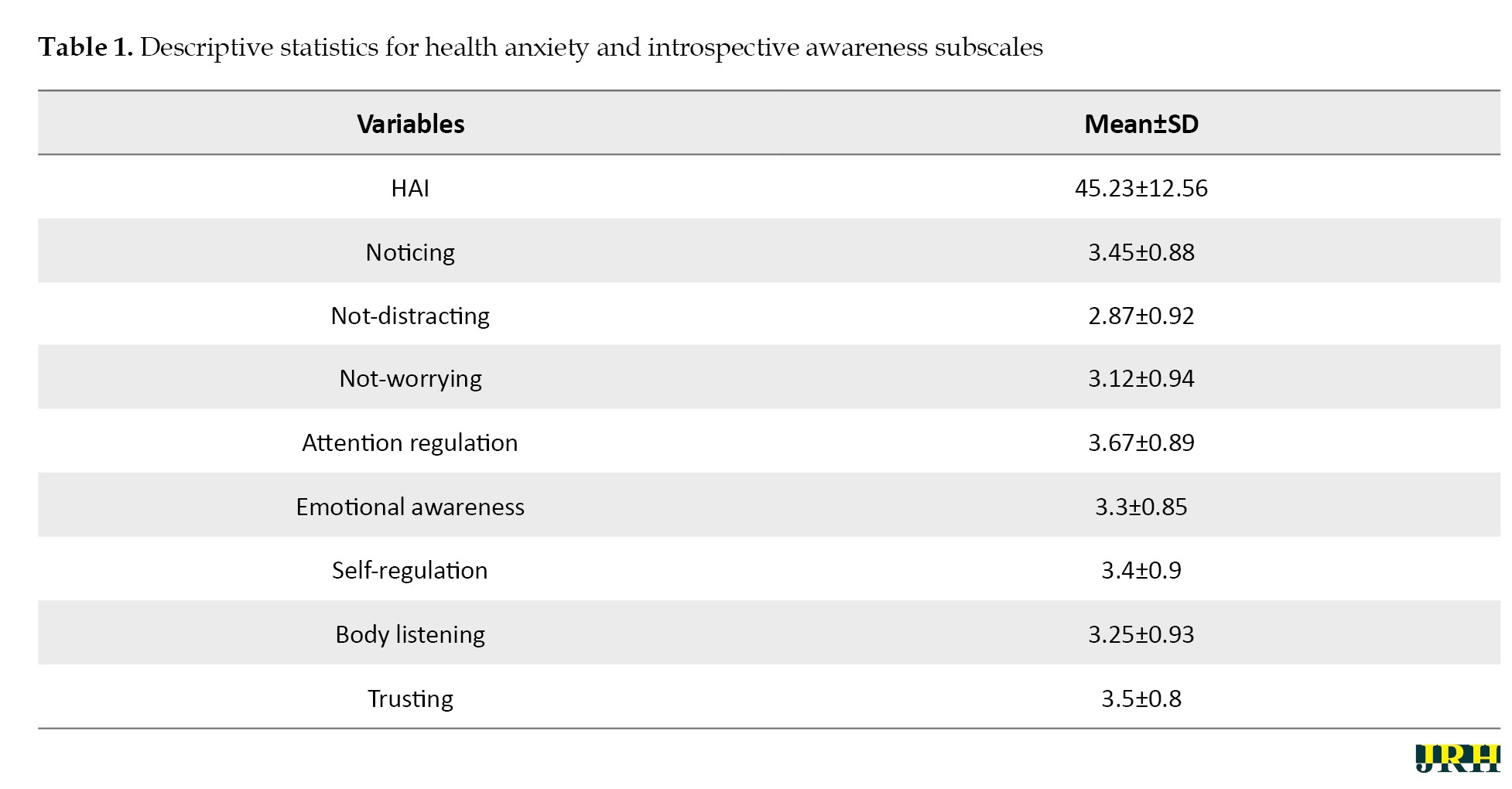
The HAI scores among participants averaged 45.23±12.56, indicating a moderate level of health anxiety within the sample. Among the introspective awareness components, attention regulation was reported highest with a mean score of 3.67±0.89, suggesting a relatively strong ability among participants to control attention in relation to bodily sensations. The lowest average score was observed for not-distracting, with a mean of 2.87±0.92, indicating a challenge in ignoring bodily sensations. These statistics provide a foundational understanding of the sample’s general health anxiety levels and their introspective awareness capacities.
Prior to conducting the primary analyses, we meticulously checked and confirmed the assumptions necessary for Pearson correlation and linear regression analyses. For the Pearson correlation, the normality of the variables was assessed, with skewness values ranging from -0.45 to 0.52 and kurtosis values from -0.60 to 0.55, all within acceptable ranges. These results indicated that the data distribution did not significantly deviate from normality. The linearity assumption was also satisfied, as evidenced by scatterplots showing linear relationships between health anxiety and each component of introspective awareness. For linear regression analysis, the assumption of multicollinearity was assessed using the variance inflation factor (VIF), with all values found to be below the threshold of five (ranging from 1.08 to 2.34), suggesting no concerning multicollinearity among the independent variables. Additionally, the Durbin-Watson statistic was 1.98, indicating no autocorrelation in the residuals. Homoscedasticity was confirmed through visual inspection of a plot of standardized residuals against predicted values, showing a random scatter of points. These checks ensured the robustness and reliability of the subsequent statistical analyses, confirming that the foundational assumptions of Pearson correlation and linear regression were adequately met in this study.
Table 2 presents the Pearson correlation coefficients between health anxiety and each independent variable, indicating diverse relationships.
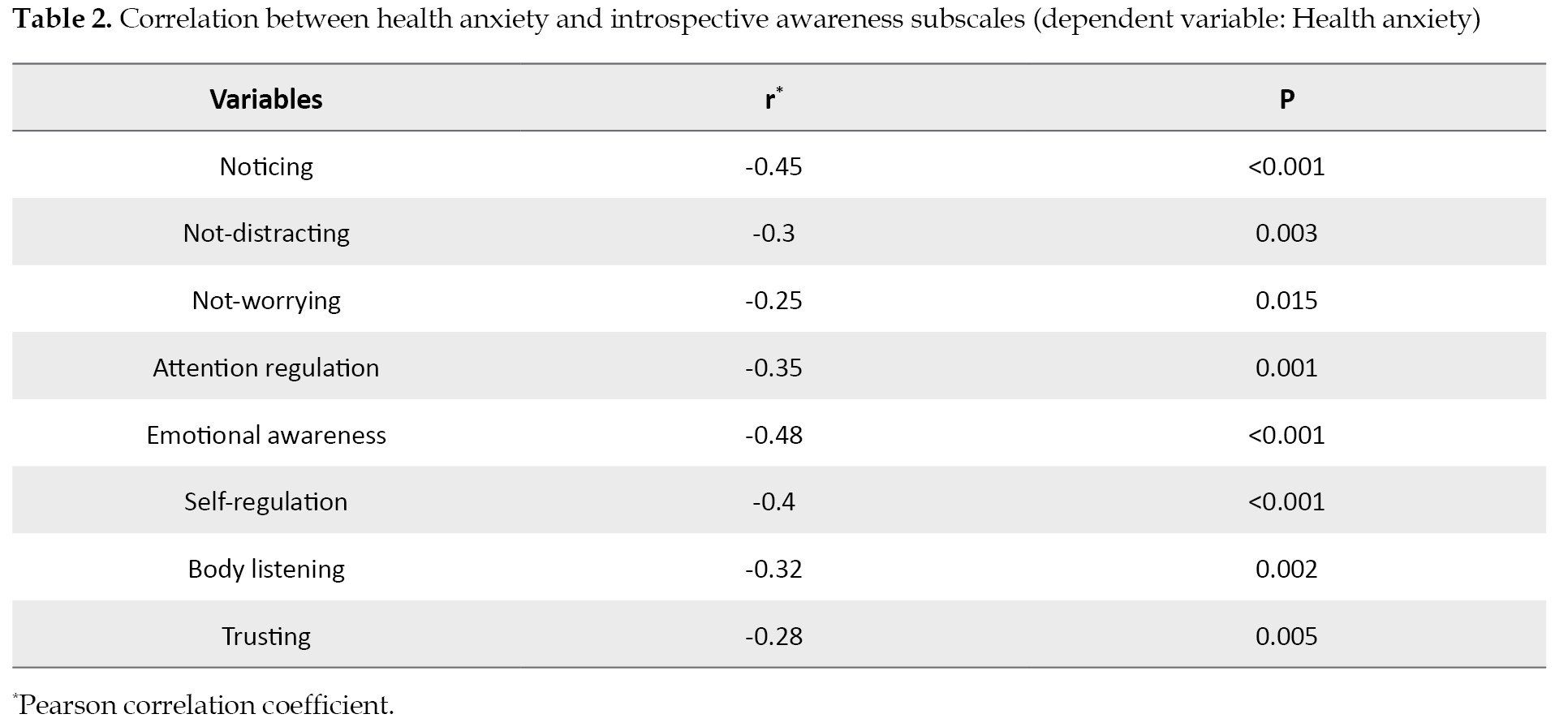
Notably, emotional awareness showed the strongest negative correlation with health anxiety (r=-0.48, P<0.001), suggesting that higher emotional awareness is associated with lower health anxiety levels. Conversely, noticing also demonstrated a significant negative correlation (r=-0.45, P<0.001), indicating that an increased awareness of internal bodily sensations correlated with reduced health anxiety. These findings highlight the intricate relationships between different facets of introspective awareness and health anxiety, suggesting potential areas for intervention.
The regression analysis summary, as detailed in Table 3, revealed that the model explained a substantial portion of the variance in health anxiety (R2=0.42, R2adj=0.41, F(2, 347)=48.35, P<0.001).
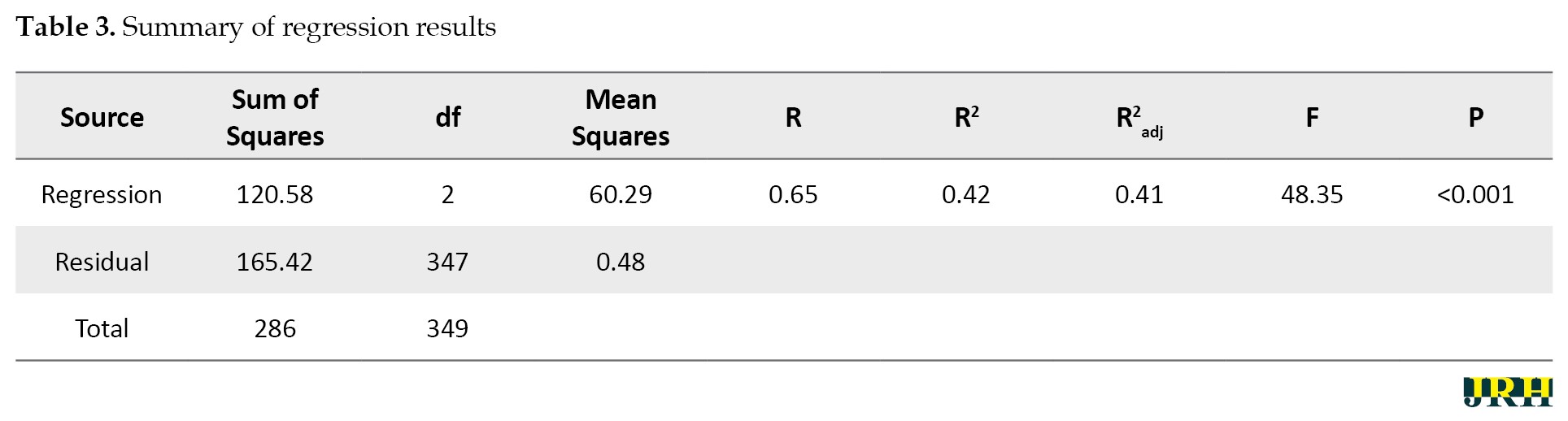
This indicates a strong model fit, with approximately 42% of the variance in health anxiety scores accounted for by the predictors. The significant F-statistic confirms the model’s overall statistical significance, suggesting that the included components of introspective awareness had a meaningful predictive relationship with health anxiety levels among the participants.
In the multivariate regression analysis detailed in Table 4, only noticing and emotional awareness were significant predictors of health anxiety.
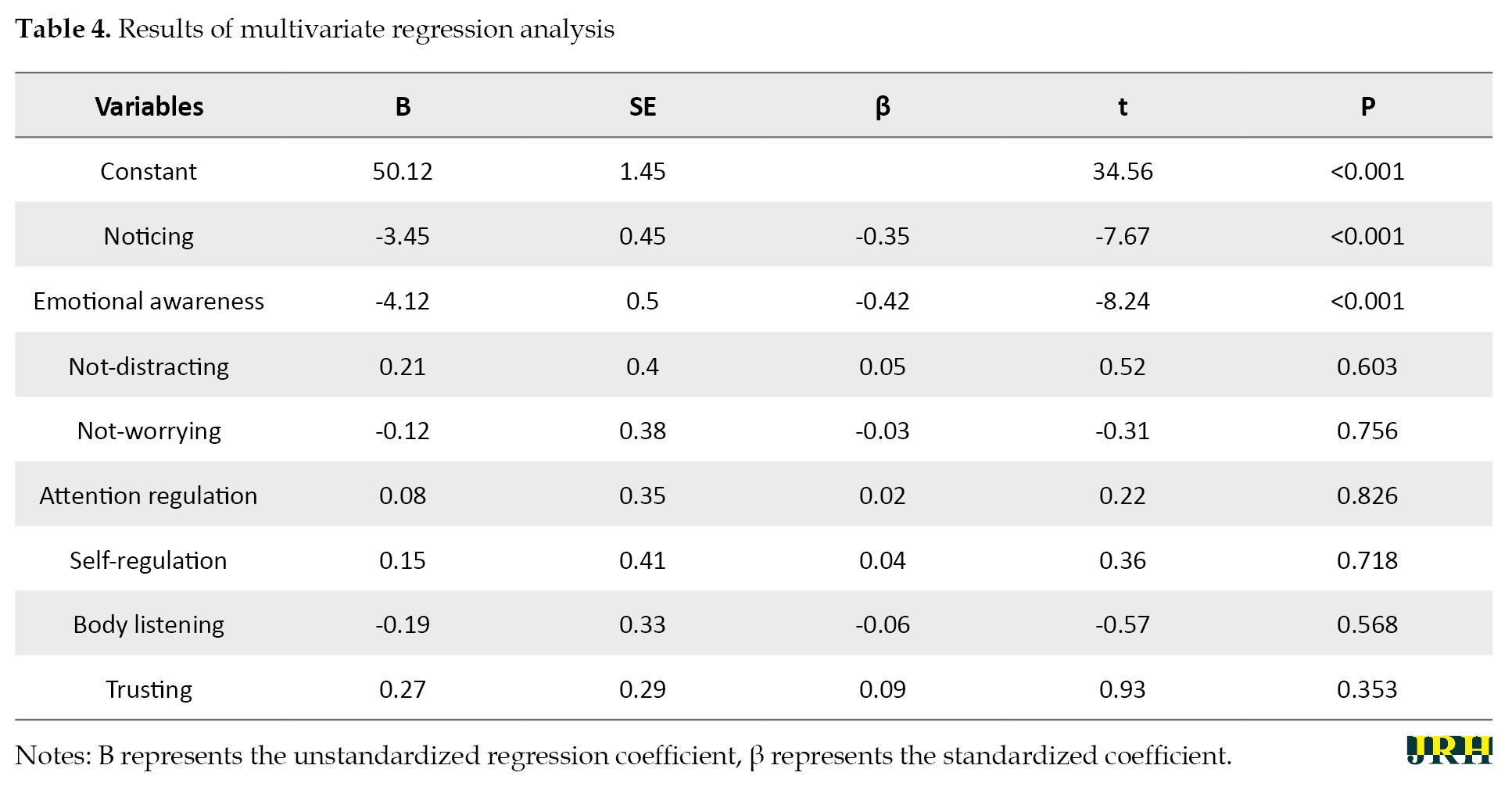
Specifically, for every unit increase in noticing, there was a significant decrease in health anxiety scores (B=-3.45, SE=0.45, β=-0.35, t=-7.67, P<0.001). Similarly, an increase in emotional awareness was associated with a significant reduction in health anxiety (B=-4.12, SE=0.50, β=-0.42, t=-8.24, P<0.001). These results underscore the protective role of noticing and emotional awareness against health anxiety, emphasizing their importance in psychological interventions aimed at managing health-related anxieties.
Conversely, the six other subscales—not-distracting, not-worrying, attention regulation, self-regulation, body listening, and trusting—did not present a significant predictive value for health anxiety, with p-values ranging from 0.353 to 0.826 (P>0.05). These results indicate that while certain aspects of introspective awareness are pivotal in the context of health anxiety, others may not directly influence its levels. Specifically, the ability to distract oneself from or refrain from worrying about bodily sensations, regulate attention or emotional responses, listen to bodily signals, or trust in those signals does not significantly predict health anxiety in this sample.
Discussion
The present study’s findings illuminate the intricate relationship between introspective awareness and health anxiety among residents of Richmond Hill, Ontario, Canada. Our results significantly underscore the predictive power of certain components of introspective awareness against health anxiety, resonating with and expanding upon the existing literature. Specifically, the dimensions of noticing and emotional awareness within introspective awareness emerged as significant predictors of health anxiety levels in our sample. These findings are discussed in the context of the theoretical frameworks and empirical evidence from previous studies, as outlined below.
The significant prediction of health anxiety by the introspective awareness components aligns with the conceptualizations of Garfinkel et al. [13], who highlighted the importance of interoceptive awareness in understanding and regulating emotional and physical states. Our study extends this notion by explicitly linking introspective awareness to health anxiety, suggesting that enhanced awareness and understanding of bodily sensations may serve as a protective factor against the exacerbation of health anxiety. This is particularly relevant in the context of a global health crisis, where fears related to health are heightened [8, 11].
The relationship between introspective awareness and health anxiety is influenced by various socio-cultural and environmental factors. Media exposure during the pandemic has amplified health anxiety by perpetuating fear and uncertainty. Social support networks, such as family and community connections, provide emotional and practical support, which can mitigate anxiety. Access to community resources, including mental health services and educational programs, can enhance introspective awareness and offer coping strategies [1]. These factors interact with individual differences to shape mental health outcomes, highlighting the importance of a comprehensive approach to addressing health anxiety in the post-pandemic period.
In our study, six subscales of introspective awareness—not-distracting, not-worrying, attention regulation, self-regulation, body listening, and trusting—did not significantly predict health anxiety among participants. This finding diverges from some expectations based on prior research and theoretical frameworks, suggesting a nuanced relationship between various facets of introspective awareness and health anxiety that may depend on specific contexts or individual differences. Not-distracting and not-worrying subscales, which pertain to the ability to divert attention away from distressing bodily sensations and worries about health, respectively, did not show a significant predictive relationship with health anxiety. This could suggest that during heightened states of global health crises, such as the COVID-19 pandemic, the general tendency to avoid or ignore health-related thoughts and sensations may not effectively mitigate health anxiety. This is consistent with the findings of Asmundson et al., who noted that avoidance behaviors could potentially exacerbate health anxiety in the context of a pandemic. Similarly, the lack of significant findings for attention regulation, self-regulation, and body listening can indicate that the capacity to regulate attention and respond to bodily signals does not directly impact health anxiety levels in the same context [8]. This could be due to the overwhelming nature of pandemic-related information and stressors, which may overshadow the benefits of these introspective abilities. Gulliver et al. highlighted the complexity of mental health help-seeking behaviors, suggesting that even well-developed self-regulation and attention to bodily cues might not suffice to alleviate health anxiety without targeted mental health support [28]. The trusting subscale, reflecting confidence in the body’s reliability and health, also did not significantly predict health anxiety. In the post-pandemic period, external factors such as pervasive health threats and uncertainty may undermine this trust, regardless of an individual’s baseline introspective awareness. This finding is consistent with that of Conversano et al. who emphasized that the unique stressors associated with the COVID-19 pandemic necessitate specific coping strategies beyond general trust in bodily signals [19].
In contrast, the noticing and emotional awareness subscales demonstrated a significant predictive role in health anxiety. Noticing, defined as the awareness of internal bodily sensations, was negatively associated with health anxiety. This suggests that a heightened awareness and accurate interpretation of bodily signals may serve as a buffer against the misinterpretation of such sensations as indicative of illness, a core feature of health anxiety as described by Cummings et al. [21]. This finding underscores the importance of mindfulness and bodily awareness practices in mitigating health anxiety, supporting Hofmann et al. ‘s assertion regarding the effectiveness of mindfulness-based therapy in reducing anxiety symptoms. Emotional awareness, or the ability to understand and differentiate emotional responses to bodily sensations, also significantly predicted lower health anxiety levels. This highlights the critical role of emotional processing in managing health anxiety, suggesting that individuals who can accurately identify and regulate their emotional responses to health-related information may be better equipped to manage health anxiety [17]. This is consistent with the protective role of emotional intelligence components against psychological distress, as reported by Taheri et al. [29].
Our findings also resonate with the research on mindfulness and its impact on psychological well-being [17]. Mindfulness practices, which enhance introspective awareness, have been shown to reduce symptoms of anxiety and depression, including those related to health concerns. The significant predictive relationship observed in our study suggests that mindfulness interventions could be particularly beneficial for individuals experiencing high levels of health anxiety. The implications of our findings extend to considerations of health disparities, as highlighted by Barbek et al. Given the varying levels of health anxiety reported among different demographic groups, interventions aimed at enhancing introspective awareness may need to be tailored to address the specific needs and contexts of these groups, thereby contributing to more equitable mental health outcomes [1].
Introspective awareness may influence health anxiety through several potential mediating mechanisms. Effective emotion regulation strategies are likely employed by individuals with high introspective awareness, reducing the intensity of health anxiety. Additionally, a strong sense of introspective awareness can enhance perceived control over health outcomes, serving as a buffer against the uncertainty associated with health concerns [30-32]. Cognitive appraisals of bodily sensations also play a significant role; individuals with high introspective awareness are more likely to interpret these sensations accurately and less catastrophically, thereby reducing anxiety. Understanding these mediating mechanisms can inform more targeted interventions [32-34].
Conclusion
The primary aim of this study was to investigate the predictive relationship between components of introspective awareness and levels of health anxiety among residents of Richmond Hill, Ontario, Canada, during the COVID-19 post-pandemic period. Our findings revealed that specific dimensions of introspective awareness, namely noticing and emotional awareness, significantly predict health anxiety, suggesting that heightened awareness and understanding of bodily sensations and emotional responses to these sensations can play a crucial role in managing health anxiety.
Future research should address these limitations by adopting longitudinal study designs to better understand the causal relationships between introspective awareness and health anxiety over time. Expanding the study to include diverse geographic locations and populations would enhance the generalizability of the findings. Additionally, incorporating objective measures of introspective awareness and health anxiety, alongside self-reported measures, could provide a more comprehensive understanding of these constructs. Investigating other potential mediators and moderators, such as social support and coping strategies, could also offer deeper insights into the mechanisms underlying the relationship between introspective awareness and health anxiety.
The findings of this study have several practical implications for psychological practice, especially in the context of a global health crisis. Healthcare professionals could consider integrating mindfulness-based interventions into their practice to enhance introspective awareness among individuals with high levels of health anxiety. Tailoring these interventions to meet the specific needs of diverse demographic groups could also help in addressing health disparities. Additionally, psychoeducation on recognizing and interpreting bodily sensations accurately could be beneficial in reducing health anxiety. Implementing these practices could contribute to improved mental health outcomes and resilience in facing ongoing and future health challenges. Individuals should be encouraged to adopt mindfulness practices, such as mindfulness meditation and body scanning, to enhance their introspective awareness and reduce health anxiety. Healthcare professionals should integrate cognitive-behavioral techniques into therapeutic interventions to help patients reframe their perceptions of bodily sensations and manage anxiety effectively. Policymakers should develop and implement community-based interventions to increase public awareness of mental health resources and ensure that mental health support is accessible and culturally sensitive, integrating these services into post-pandemic recovery plans. The implications of the findings should also be considered within a cross-cultural framework [35]. Cultural beliefs and values significantly shape how individuals experience and express health anxiety and introspective awareness. In cultures that emphasize community and collective well-being, social support networks may play a more pronounced role in mitigating health anxiety. When developing interventions, it is crucial to consider cultural differences in the conceptualization of health-related concerns and employ culturally sensitive approaches. Incorporating culturally relevant practices and addressing specific cultural stressors can enhance the effectiveness of interventions, ensuring they are respectful and effective across diverse cultural backgrounds [36, 37]. This approach is essential for developing equitable mental health strategies in the post-pandemic era.
This study, while informative, is subject to several limitations. The cross-sectional design restricts our ability to infer causality between introspective awareness and health anxiety. Additionally, the sample was drawn from a single geographic location, which may limit the generalizability of the findings to other populations or contexts. Another limitation is the reliance on self-reported measures, which are susceptible to biases, such as social desirability or recall bias.
Ethical Considerations
Compliance with ethical guidelines
The study's protocol adhered to the principles outlined in the Helsinki Declaration, which provides guidelines for ethical research involving human participants. The study was conducted according to the ethical guidelines set forth by the KMAN Research Institute, Richmond Hill, Canada (Code: KEC.2023.6A2), ensuring the protection of participants’ rights and confidentiality.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to express their gratitude to all individuals who helped us to do the project.
References
- Barbek R, Henning S, Ludwig J, von dem Knesebeck O. Ethnic and migration-related inequalities in health anxiety: A systematic review and meta-analysis. Frontiers in Psychology. 2022; 13:960256. [DOI:10.3389/fpsyg.2022.960256] [PMID] [PMCID]
- Nikčević AV, Marino C, Kolubinski DC, Leach D, Spada MM. Modelling the contribution of the Big Five personality traits, health anxiety, and COVID-19 psychological distress to generalised anxiety and depressive symptoms during the COVID-19 pandemic. Journal of Affective Disorders. 2021; 279:578-84. [DOI:10.1016/j.jad.2020.10.053] [PMID] [PMCID]
- Shahamatinejad S. The relationship between health anxiety and emotion regulation with rumors on social networks during the COVID-19 pandemic. Journal of Assessment and Research in Applied Counseling. 2021; 3(1):38-48. [DOI:10.52547/jarcp.3.1.38]
- Bazgouneh A, Zarbakhsh M. The relationship between sleeping disorders and posttraumatic stress disorder syndrome with corona anxiety: The intermediary role of health anxiety. Applied Family Therapy Journal. 2021; 2(5):287-308. [Link]
- Nakhaei Moghadam R, Bahrainian SA, Nasri M. The effectiveness of intensive and short-term dynamic psychotherapy on attachment styles, somatization and health anxiety in patients with chronic pain. Journal of Assessment and Research in Applied Counseling. 2024; 6(1):142-9. [DOI:10.61838/kman.jarac.6.1.16]
- Tayebmanesh L, Saadati N. Effectiveness of integrating quality of life-based therapy and phototherapy on emotion regulation, depression, and anxiety in psychosomatic patients. KMAN Counseling & Psychology Nexus. 2023; 1(2):37-43. [DOI:10.61838/kman.psychnexus.1.2.7]
- Asadi L, Seirafi M, Ahadi M. Evaluation of the effectiveness of painting therapy on health anxiety, loneliness and death anxiety in the elderly. Applied Family Therapy Journal. 2023; 4(2):395-413. [DOI:10.61838/kman.aftj.4.2.25]
- Asmundson GJG, Paluszek MM, Landry CA, Rachor GS, McKay D, Taylor S. Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? Journal of Anxiety Disorders. 2020; 74:102271. [DOI:10.1016/j.janxdis.2020.102271] [PMID] [PMCID]
- Partovi Pirooz L, Jomehori F, Seadatee Shamir A, Hasani J. Structural model of health anxiety based on intolerance of uncertainty and anxiety sensitivity with mediating the role of rumination in college students. Journal of Adolescent and Youth Psychological Studies. 2022; 3(2):278-90. [DOI:10.61838/kman.jayps.3.2.21]
- Navidi Poshtiri S, Hassanzadeh R, Olia Emadian S. The effectiveness of acceptance and commitment therapy on tolerance failure and health anxiety in nursing and midwifery students with health anxiety. Journal of Adolescent and Youth Psychological Studies. 2022; 3(1):222-31. [DOI:10.61838/kman.jayps.3.1.18]
- Albery IP, Spada MM, Nikčević AV. The COVID-19 anxiety syndrome and selective attentional bias towards COVID-19-related stimuli in UK residents during the 2020-2021 pandemic. Clinical Psychology & Psychotherapy. 2021; 28(6):1367-78. [DOI:10.1002/cpp.2639] [PMID] [PMCID]
- Angazi F, Hosseini S, Arefi M, Kakabraei K. Structural model of anxiety disorders based on corona anxiety, mental health and the level of health concern with the mediating role of coping strategies in pregnant women. Applied Family Therapy Journal. 2023; 4(5):161-72. [DOI:10.6180938/kman.aftj.4.5.9]
- Garfinkel SN, Manassei MF, Hamilton-Fletcher G, In den Bosch Y, Critchley HD, Engels M. Interoceptive dimensions across cardiac and respiratory axes. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 2016; 371(1708):20160014. [DOI:10.1098/rstb.2016.0014] [PMID] [PMCID]
- Li J, Zhou L. Efficacy of mindfulness-based stress reduction on reducing somatization and attachment anxiety: A randomized controlled trial. Journal of Personality and Psychosomatic Research. 2023; 1(4):14-22. [DOI:10.61838/kman.jppr.1.4.3]
- Darbani S, Mirzaei A. Consequences of the COVID-19 pandemic on mental health: A review study. Journal of Assessment and Research in Applied Counseling. 2022; 4(1):48-63. [DOI:10.52547/jarac.4.2.48]
- Navidi Poshtiri S, Hasanzadeh R, Emadian SO. The effectiveness of mindfulness-based schema therapy on cognitive distortions and causal attributions in nursing and midwifery students with health anxiety. Applied Family Therapy Journal. 2023; 4(4):581-93. [DOI:10.61838/kman.aftj.4.4.35]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010; 78(2):169-83. [DOI:10.1037/a0018555] [PMID] [PMCID]
- Jin Y, Zhang Q, Cong X, An J, Zheng P. Impact of death anxiety on mental health during COVID-19: The mediating role of the meaning in life. Journal of Pacific Rim Psychology. 2023; 11(3):65-87. [DOI:10.1177/18344909231165187]
- Conversano C, Di Giuseppe M, Miccoli M, Ciacchini R, Gemignani A, Orrù G. Mindfulness, age and gender as protective factors against psychological distress during COVID-19 pandemic. Frontiers in Psychology. 2020; 11:1900. [DOI:10.3389/fpsyg.2020.01900] [PMID] [PMCID]
- Matiz A, Fabbro F, Paschetto A, Cantone D, Paolone AR, Crescentini C. Positive impact of mindfulness meditation on mental health of female teachers during the COVID-19 outbreak in Italy. International Journal of Environmental Research and Public Health. 2020; 17(18):6450. [DOI:10.3390/ijerph17186450] [PMID] [PMCID]
- Cummings AJ, Knibb RC, King RM, Lucas JS. The psychosocial impact of food allergy and food hypersensitivity in children, adolescents and their families: A review. Allergy. 2010; 65(8):933-45. [DOI:10.1111/j.1398-9995.2010.02342.x] [PMID]
- Polloni L, Muraro A. Anxiety and food allergy: A review of the last two decades. Clinical and Experimental Allergy. 2020; 50(4):420-41. [DOI:10.1111/cea.13548] [PMID]
- Ruan QN, Chen YH, Yan WJ. A network analysis of difficulties in emotion regulation, anxiety, and depression for adolescents in clinical settings. Child and Adolescent Psychiatry And Mental Health. 2023; 17(1):29. [DOI:10.1186/s13034-023-00574-2] [PMID] [PMCID]
- Kotwal S. Addressing the gap: The importance of mental health legislation and policy. Interdisciplinary Studies in Society, Law, and Politics. 2022; 1(2):1-3. [DOI:10.61838/kman.isslp.1.2.1]
- Salkovskis PM, Rimes KA, Warwick HM, Clark DM. The Health Anxiety Inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol Med. 2002; 32(5):843-53. [DOI: 10.1017/s0033291702005822] [PMID]
- Mehling WE, Price C, Daubenmier JJ, Acree M, Bartmess E, Stewart A. The Multidimensional Assessment of Interoceptive Awareness (MAIA). PLoS One. 2012; 7(11):e48230. [DOI: 10.1371/journal.pone.0048230] [PMID]
- Willem C, Gandolphe MC, Roussel M, Verkindt H, Pattou F, Nandrino JL. Difficulties in emotion regulation and deficits in interoceptive awareness in moderate and severe obesity. Eating and Weight Disorders. 2019; 24(4):633-44. [DOI:10.1007/s40519-019-00738-0] [PMID]
- Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry. 2010; 10:113. [DOI:10.1186/1471-244X-10-113] [PMID] [PMCID]
- Taheri M, Hasani J, Jamalooei HR, Mohebbi A. Attachment Styles and Emotional Intelligence Components: The Predictors of Health Dimensions. Journal of Research and Health. 2019; 9(1):82-95. [DOI:10.29252/jrh.9.1.82]
- Lu JI. Educational models of spiritual formation in theological education: Introspection-based spiritual formation. Teaching Theology & Religion. 2021; 24(1):28-41. [DOI:10.1111/teth.12560]
- Sapeta P, Centeno C, Belar A, Arantzamendi M. Adaptation and continuous learning: Integrative review of coping strategies of palliative care professionals. Palliative Medicine. 2022; 36(1):15-29. [DOI:10.1177/02692163211047149] [PMID] [PMCID]
- Majlessi Koupaei H, Farista R. Psychological pathways to immunity: The role of emotions and stress in health and disease. Journal of Personality and Psychosomatic Research (JPPR). 2024; 2(1):1-3. [DOI:10.61838/kman.jppr.2.1.1]
- Hooshmandi R, Aljaberi MA, Hammadi F, Ma J. The impact of interoceptive awareness on pain catastrophizing and illness perception. Journal of Personality and Psychosomatic Research. 2024; 2(2):4-10. [DOI:10.61838/kman.jppr.2.2.2]
- Sayed Alitabar SH, Goli F. The interplay of neuroticism and self-efficacy in pain catastrophizing: A quantitative analysis. Journal of Personality and Psychosomatic Research. 2023; 1(2):19-24. [DOI:10.61838/kman.jppr.1.2.4]
- Çevik M, Toker H. Social determinants of health: legal frameworks for addressing inequities. Interdisciplinary Studies in Society, Law, and Politics. 2022; 1(1):14-22. [DOI:10.61838/kman.isslp.1.1.3]
- Boltivets S. Cultural beliefs and mental health. Journal of Psychosociological Research in Family and Culture. 2023; 1(4):1-3. [DOI:10.61838/kman.jprfc.1.4.1]
- Bilač S, Öztop F, Kutuk Y, Karadag M. Cultural narratives and their impact on family mental health. Journal of Psychosociological Research in Family and Culture. 2024; 2(2):18-24. [DOI:10.61838/kman.jprfc.2.2.4]
Type of Study: Orginal Article |
Subject:
● International Health
Received: 2024/04/7 | Accepted: 2024/06/19 | Published: 2025/01/1
Received: 2024/04/7 | Accepted: 2024/06/19 | Published: 2025/01/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






