Volume 15, Issue 4 (Jul & Aug 2025)
J Research Health 2025, 15(4): 403-410 |
Back to browse issues page
Ethics code: IR.IAU.B.REC.1402.063
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Dadvar H, Jafarinia G, Rahedzadeh A. Exploring the Social Health of Employees Working in the Persian Gulf Special Economic Zone. J Research Health 2025; 15 (4) :403-410
URL: http://jrh.gmu.ac.ir/article-1-2586-en.html
URL: http://jrh.gmu.ac.ir/article-1-2586-en.html
1- Department of Sociology, Faculty of Humanities, Bushehr Branch, Islamic Azad University, Bushehr, Iran.
2- Department of Sociology, Faculty of Humanities, Bushehr Branch, Islamic Azad University, Bushehr, Iran. ,Jafarinia_reza@iaubushehr.ac.ir
2- Department of Sociology, Faculty of Humanities, Bushehr Branch, Islamic Azad University, Bushehr, Iran. ,
Full-Text [PDF 564 kb]
(433 Downloads)
| Abstract (HTML) (2820 Views)
Full-Text: (381 Views)
Introduction
The workplace strongly influences employees’ social health. According to research, an organization’s workplace can significantly affect employee happiness and job satisfaction [1]. Higher job satisfaction and productivity levels can result from supportive work environments that prioritizing employee social health and better employee retention and organizational performance [2]. These work environments generate healthy interactions between colleagues, employee engagement, and a sense of purpose. In addition, they provide opportunities for professional development, recognition, and work-life balance, all of which can improve the overall social health of employees [3]. Fostering a sense of belonging within an organization is the strongest driver of employee engagement. When employees feel connected and included, overall job satisfaction and loyalty to the company rise. A workplace prioritizing social health fosters a supportive community, reduces feelings of isolation and burnout, and fosters a collaborative atmosphere [4].
As a prerequisite for active participation in social roles, health is intimately linked to the general well-being of a community. Social health is undoubtedly the most important aspect of social issues, individually and collectively. Throughout history, people have pursued social health, culminating in developing comprehensive medical and biological sciences dedicated to protecting individual and societal health [5]. Currently, any decline in societal health, whether physical or mental, inevitably hinders progress and development. Consequently, societies that strive for sustainable development prioritize the health of their members [6].
Social environments and socioeconomic conditions significantly determine each aspect of an individual’s health [7]. The concept of social health was first introduced by Belloc et al. [8] and a few years later by Ware et al. [9]. They believed that health was a broader concept than reporting symptoms of illness and a person’s functional abilities. They argued that individual well-being and comfort differ from physical and mental health [10]. The World Health Organization (WHO) has recognized social health as one of several aspects of an individual’s total health. Social health includes emotional, psychological, and social well-being and influences cognition, perception, and behavior. According to WHO, it is a “state of well-being in which individuals recognize their abilities, cope with the normal stresses of life, work productively and fruitfully, and contribute to the well-being of their community” [11]. Still, the concept of social health is frequently associated with social indicators operationalized through economic measures (e.g. gross domestic product and poverty rate) that reflect the “health” of narrow sectors of society. Keyes [12] was a leading sociologist in the micro-level conceptualization and measurement of social health. He believed that social health is a person’s assessment of his or her functioning in society.
Social health can be defined as an individual’s self-report of the quality of their relationships with other people, the neighborhood, and the community. Social health represents a fundamentally public (as opposed to private) phenomenon focusing on social obligations people face within social structures and communities. Keyes [12] defined social health as a person’s report of the quality of relationships with others (close people and social groups) to which they belong. He believed that the key to deciding whether a measure of social well-being is part of an individual’s health is whether the measure reflects internal responses to stimuli—feelings, thoughts, and behaviors that reflect satisfaction or dissatisfaction with the social environment. The WHO was the first to mention social health as a dimension of health. Numerous studies have shown that the quantity and quality of a person’s relationships with others affect their physical and mental health. Social health, as a dimension of health, is the ability to perform social roles effectively and efficiently without harming others, and is an evaluation of an individual’s conditions and achievements in society. Some social factors shape various dimensions of social health, including social integration, social acceptance, social participation, social flourishing and social cohesion [13]. Researchers in workplace activity have long developed theoretical models to explain the influence of the work environment on social health. These theoretical models were originally based on a “stimulus-response” principle and have been refined to incorporate various variables (individual or environmental) that moderate or exacerbate the effects of the work environment on social health [14].
Keyes (1998) proposed five dimensions of social well-being operationalized at the level of the individual: Social integration, social acceptance, social contribution, social coherence, and social actualization. Social integration is the degree to which people feel a sense of common identity and belonging to those who make up their social reality (the quality of relationships between individuals concerning society. Social acceptance is the interpretation of a society based on the character and qualities of other people as a generalized category. Social contribution refers to an individual assessing their social value. Individuals with an appropriate level of social contribution believe that what they do in society is valuable. Social coherence refers to an individual’s assessment of whether society is understandable, predictable, and tangible. Finally, social actualization refers to a person’s evaluation of a society’s potential and developmental trajectory and the belief that the society is experiencing gradual progress and has the potential for positive transformation [15].
Hosseinzadeh et al. [15] conducted a case study with young adults in Khorramabad City, Iran and found a significant association between social capital variables and social health. Furthermore, they observed a direct relationship between life satisfaction and social health in young adults, whereas social alienation had an inverse relationship with social health. The regression analysis revealed that 51% of the variance in social health was explained by five social capital variables: social trust, social networks, social participation, social norms, and social sanctions.
Ghorbani et al. [16] examined the relationship between psychological capital and social health, considering the mediating role of social support. Their results showed that university students with higher levels of psychological capital had better social health.
The Persian Gulf special economic zone (PGSEZ) is a major economic institution that plays a critical role in transforming global supply chains and development models. The PGSEZ is at the 13th km of the Shahid Rajaei Highway in Bandar Abbas, Iran. It was initially set up as a special economic zone for mining and metals on January 14, 1998. However, it later changed its name to PGSEZ. The PGSEZ is strategically located in the Persian Gulf region, known for its rich natural resources, particularly in the mining and metals industries [17].
This study offers several novel contributions to the literature on social health in industrial settings, with a particular focus on PGSEZ in Hormozgan Province, Iran. It addresses the unique sociocultural and organizational context of Iranian industrial settings, which has been largely overlooked in previous research. It extends the literature by focusing on high-risk industrial sectors where social health can play a critical role in alleviating work stress and improving safety. Given the lack of information on the social health and psychological well-being of industrial workers in Hormozgan Province, this study aimed to examine the following hypotheses:
Hypothesis 1: The social health status of employees working in PGSEZ is average. Hypothesis 2: There is a significant association of the level of “perceived social support,” “hope for the future,” “general social trust,” and “social vitality” with the level of “social health” of employees working in PGSEZ.
Methods
Study design and participants
This study aimed to examine the social health of employees working in PGSEZ. This study was conducted using a correlational design. A total of 237 participants were selected using cluster sampling. Data were collected using Keyes social well-being and perceived social support scales. Parametric and nonparametric statistical tests were used to analyze the data in SPSS software, version 26. The research population consisted of all employees working in PGSEZ in 2023. The sample size was 237 participants selected using a cluster sampling method. This study used the Cochran formula to determine the sample size. The final sample size accepted by the research team comprised 250 participants, but 237 participants answered the questionnaires. We collected the data after obtaining the participants’ consent to observe the ethical considerations in this research. Participants were assured of the confidentiality of their personal information, and the results were provided without specifying the names and details of the participants. Ethical considerations were also carefully considered throughout the research process, demonstrating the researcher’s commitment to respecting the participants’ involvement and confidentiality.
Study measures
Keyes social well-being scale
The Keyes social well-being scale is a 20-item questionnaire that measures various aspects of social health, including social integration, social acceptance, social contribution, social coherence, and social actualization. The questionnaire is scored on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (completely agree) [12]. In this scale, items 1, 6, 13, 14, 15, 17, 18, 19 and 20 are reverse scored (1=5, 2=4, 3=3, 4=2, 5=1). After adding the scores for all 20 items, the total score can range from 20 to 100.
In this study, the Cronbach α was used to estimate the scale’s internal consistency, which was 0.90, indicating an acceptable reliability. Also, the Cronbach α for all dimensions of this questionnaire were as follows: Social integration (α=0.84), social acceptance (α=0.91), social contribution (α=0.89), social coherence (α=0.84) and social actualization (α=0.91). Thus, the reliability of the questionnaire for all dimensions was confirmed.
The validity of the Keyes social well-being scale has been supported in various studies that confirmed its effectiveness in measuring social well-being across different populations [1, 18]. Keyes (1998) provided evidence of both convergent and discriminant validity, showing that the dimensions of social well-being correlate significantly with other established measures, such as anomie, generativity, perceived social constraints, community involvement and overall social health [12]. Content and construct validity were examined in this study to evaluate the scale’s validity. Content validity focuses on whether the scale fully represents the theoretical construct of social well-being. In this study, content validity was assessed using the theories of experienced professors and the approval of sociology and psychology experts. This approach ensured the content was theoretically sound and practically relevant, incorporating insights from established scholars in the respective fields. The involvement of experts helped enhance the credibility and reliability of the research findings. This study assessed construct validity through confirmatory factor analysis to ensure that the scale items loaded on the expected factors corresponding to the theoretical dimensions. The findings showed satisfactory fit indices with a comparative fit index of 0.94 and a root mean square error of approximation of 0.05. These results indicated strong construct validity and confirmed that the scale effectively measured the intended constructs as theoretically predicted.
Perceived social support scale
The multidimensional scale of perceived social support (MSPSS) developed by Canty-Mitchell and Zimet [19] was used to assess perceived social support. This scale consists of 12 items measuring three components: perceived support from family (4 items), perceived support from significant others (4 items) and perceived support from friends (4 items).
All items on the scale are rated on a 5-point Likert scale (strongly agree, agree, neither agree nor disagree, disagree, strongly disagree). The total score for the scale ranges from 12 to 60.
The Cronbach coefficient α, a measure of internal reliability, was obtained for the total scale and each subscale. For the “significant others,” “family,” and “friends” subscales, the values were 0.91, 0.87, and 0.85, respectively. The reliability of the total scale was 0.88. These values indicate good internal consistency for the scale as a whole and its three subscales [19]. In this study, the reliability of the total scale was 0.85.
Data analysis
Data collected using questionnaires were analyzed at descriptive and inferential statistics levels using SPSS software, version 26. The descriptive statistics section presented the frequency and percentage of the research variables in tables. The inferential statistics section used the Pearson correlation coefficient test, one-sample independent t-test, linear regression, analysis of variance (ANOVA) and multicollinearity test.
Results
Demographic findings revealed that 209 participants (80%) were male and 28(20%) were female. Regarding education, 22 participants (9.3%) had a high school degree, 49(20.67%) a diploma degree, 31(13.08%) a college or associate’s degree, 93(39.24%) a bachelor’s degree, and 42(17.72%) postgraduate (MS and PhD) degrees. Finally, 38 participants (16%) were permanent and formally employed and 199 (84%) were temporary and contract employees.
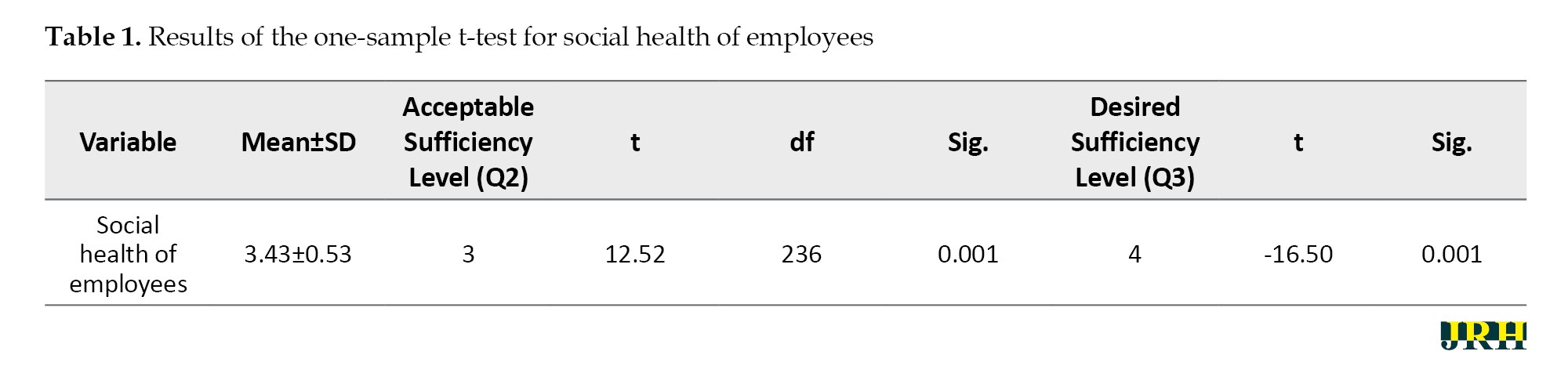
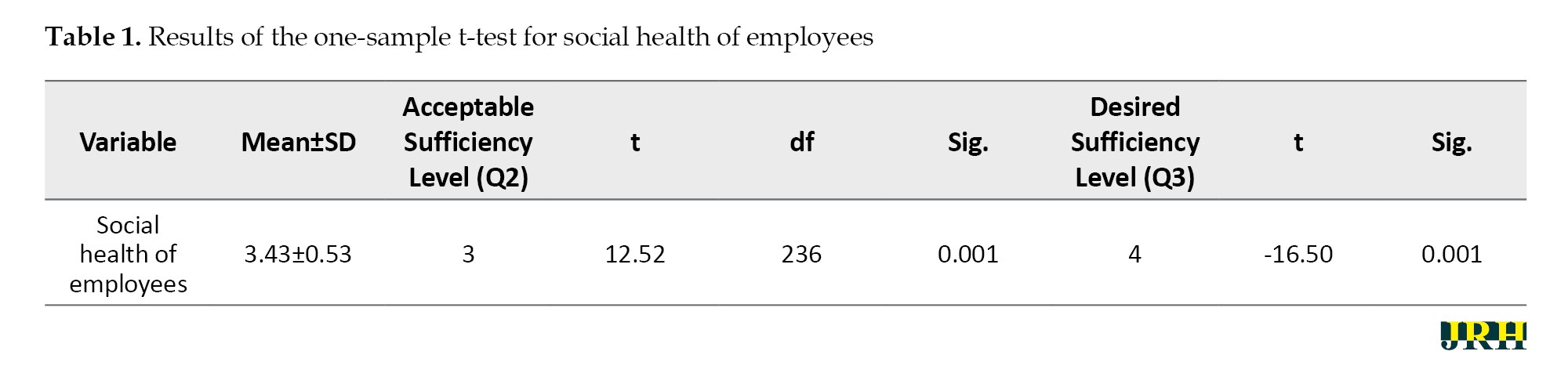
Hypothesis 1: The social health status of employees in the PGSEZ is average. According to Table 1, the sample mean is 3.43. Based on the obtained t value of 12.52 with 236 df, there is a significant difference between the obtained mean and the acceptable sufficiency level at a 95% confidence interval (CI) (P<0.05). Furthermore, the obtained mean value deviates significantly from the desired sufficiency level, as indicated by the t-value of -16.50 (P<0.05). Based on the above findings, social health among workers in the PGSEZ is well above the acceptable and desired sufficient level. Therefore, Hypothesis 1 is confirmed.
Hypothesis 2: There is a significant association of the level of “perceived social support,” “hope for the future,” “general social trust,” and “social vitality” with the level of “social health” of employees working in PGSEZ.
According to Table 2, the correlation coefficients between perceived social support and employee social health (r=0.397), hope for the future and employee social health (r=0.715), general social trust and the social health of employees (r=0.620) as well as social vitality and social health of employees (r=0.551) are all positive and significant (P<0.05). These findings suggest that as these variables’ values increase, employees’ social health level increases and vice versa. Therefore, the hypothesis is confirmed.
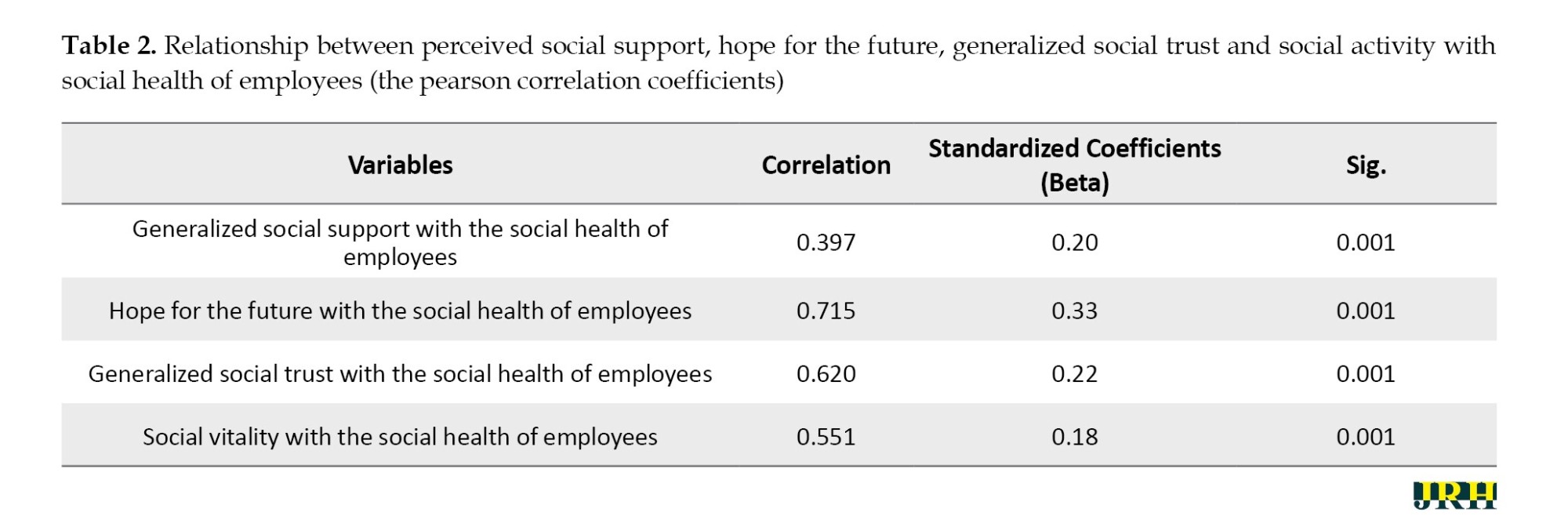
Among these variables, the “hope for the future” variable has the greatest impact on social health, with a beta value of 0.33. The direction of the effect of this variable is positive, indicating that as hope for the future increases, employees’ social health also improves. In other words, for every unit of standard deviation increase in future hope, there is a corresponding 0.33 standard deviation increase in employee social health. Perceived social support, generalized social trust, social vitality, and hope for the future are important predictors of social health.
According to Table 3, the tolerance index for all independent variables is greater than 0.4, and the variance inflation factor is <2.5. These results indicate no significant multicollinearity between the independent variables. The results of the multicollinearity test support using multiple regression to test the hypothesis. The absence of multicollinearity suggests that the independent variables are not redundant and that each variable uniquely contributes to predicting the dependent variable.
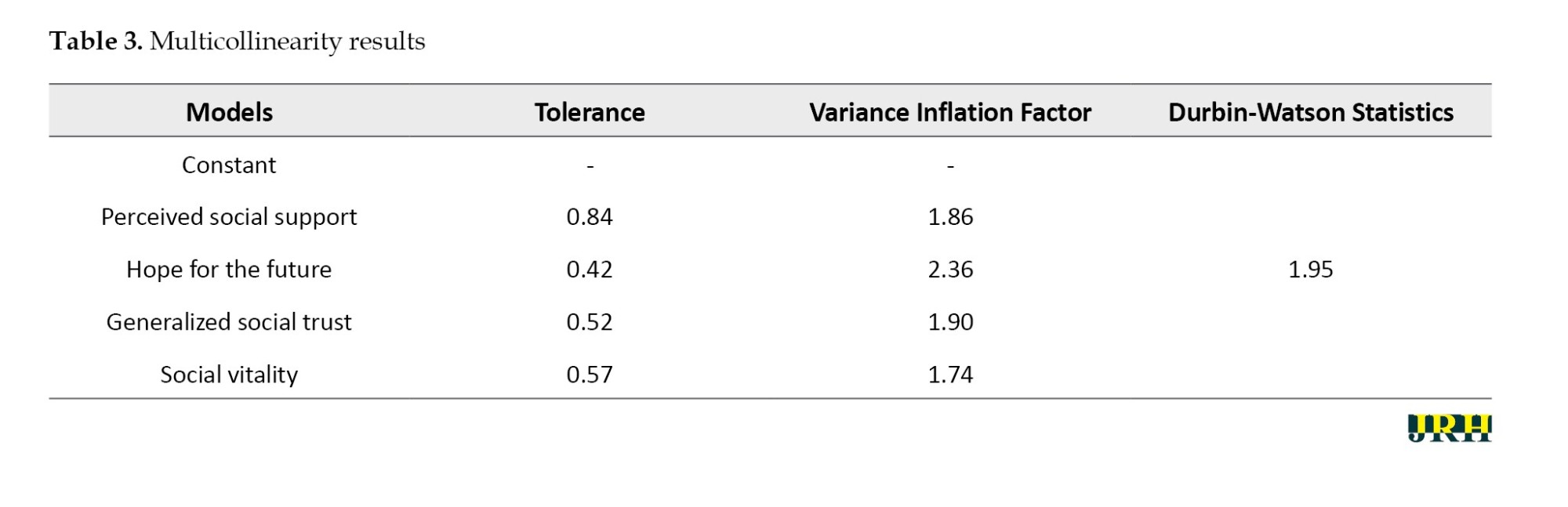
Another assumption of regression is that the errors (the differences between the actual values and the values predicted by the regression equation) are independent of each other. The Durbin-Watson test was used to check the independence of errors. According to Table 3, the Durbin-Watson statistics (d) of 1.95 is between 1.5 and 2.5, indicating that the assumption of no autocorrelation between the errors is met.
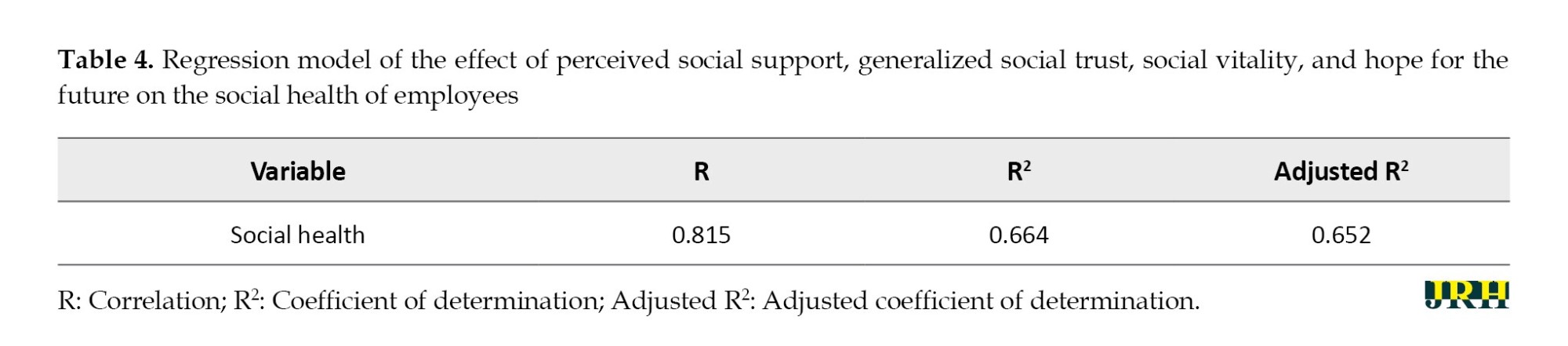
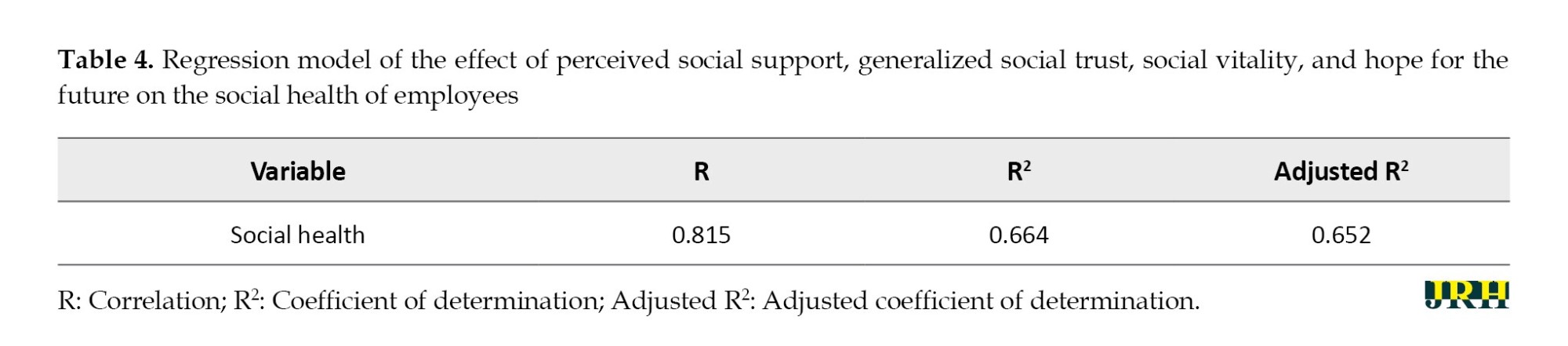
As shown in Table 4, the coefficient of determination (R2) is 0.664. This finding indicates that 66.4% of the variance in social health is explained by perceived social support, generalized social trust, social vitality, and hope for the future.
Discussion
This study examined the social health of employees working in the PGSEZ. The interpretation of hypothesis 1 results suggests that the “level of social health among employees” is significantly higher than the acceptable and desired sufficiency levels for both. Therefore, Hypothesis 1 was confirmed. While employees working in the PGSEZ do not enjoy the desired level of social health, they have a moderate level of social health. The findings of this study were consistent with those reported by Moradi et al. [7], Parvish et al. [5], Arabi [6], Goudarzi and Sabzevar [20], Hosseinzadeh et al. [15], Hajebi and Faridnia [21] and Keyes and Shapiro [22]. The results show that most employees working in the PGSEZ have an average level of social health. Many employees have poor social health, which can be described as social illness.
Social health is a social goal and a desired outcome of various societal development measures. Achieving this goal requires resource utilization mechanisms and coordinated programs at the social, economic, and political levels. Social health, like education, is considered one of the most important social and economic indicators, since ensuring health components among various groups in society increases the sense of security and sustainable economic growth and development in any country. Social health, an important dimension of health, is defined as an individual’s assessment of the quality of his or her relationships with family, others, and social groups. The Keyes social health scale indicates a person’s satisfaction or dissatisfaction with life and social environment [12]. According to Goudarzi and Sabzevar [20], a socially healthy individual functions well when perceiving society as a meaningful, understandable, and potentially growing and thriving. They feel like they belong to social groups and see themselves as partners in society and its progress [15].
Interpreting the results of hypothesis 2 suggests that social support, a fundamental aspect of social interactions, includes the perception, reception, and need for support and encouragement from one’s social network. The type and importance of social support vary significantly from one person to another and are influenced by age, gender, personality, and cultural background. Furthermore, the aspects of social support that matter most may fluctuate over the life course, with certain elements taking precedence over others at different stages. In this context, social relationships can be conceptualized as an intermediate variable that bridges the gap between social circumstances and individual well-being. The quality and quantity of social support play a critical role in determining how social conditions impact an individual’s health. The results of the current study are also consistent with the research of Hajebi and Faridnia [21] entitled “The relationship between mental health and social support in health staff of Bushehr oil industry.” Both studies demonstrate a significant association between mental health and social support, although this association varies depending on demographic factors. Furthermore, the present study shows that employees working in rotating shifts experience lower psychological well-being and social support levels than employees in other employment arrangements.
Hope for the future is a cornerstone of quality of life and social health. It serves as the origin of every dynamic and progressive aspect of human existence. Hope for the future is a basic human need because without it, individuals cannot follow their personal and social goals [23]. While individual circumstances significantly influence hope for the future, social factors are crucial in increasing or weakening its intensity. On the one hand, society can promote conditions that lead individuals to realize their personal goals and desires.
The connection between social vitality and employees’ social health can be characterized as a reciprocal and mutually reinforcing dynamic. Social health in employees increases the likelihood of increased social vitality, although with the caveat that broader external variables at the societal level also influence this phenomenon. Socially important employees demonstrate increased motivation, greater commitment to work, loyalty to the organization, and dedication to their employer [10]. These factors, in turn, have a positive impact on the productivity and profitability of the organization. However, it is important to recognize that job satisfaction represents only one dimension of social vitality. Promoting social vitality among employees and workers has much deeper and broader implications [13].
Based on the study findings, the following recommendations have been made. Companies should consider integrating social health metrics into their overall employee health assessment. This measure can help identify areas that need improvement and track progress over time. Training programs for managers on the importance of social health and fostering a supportive environment can be helpful. Managers play a critical role in shaping workplace culture and employee experiences. Continuous evaluation of workplace wellness initiatives is essential to ensure they meet the changing needs of employees. Feedback mechanisms should be considered to collect employee insights on social health initiatives.
This study has some limitations. It is limited to the industries and organizations in the PGSEZ and does not include other industry organizations in Iran. The study did not include a comparison group of employees working in different industries or regions of Iran. The study focuses exclusively on employees, so the generalizability of the results to this specific group is limited. The study used a cross-sectional design, meaning the data were collected simultaneously. This design limitation prevents researchers from establishing causal relationships between sociocultural workplace factors and social health and mental illness.
Conclusion
The study concluded that workers’ social health was not at the desired level, but at a moderate level in the PGSEZ. The study highlighted that social health is an important dimension of overall health, similar to physical and mental well-being. Social health encompasses a person’s perception of their relationships and social environment and significantly impacts their psychological and social functioning. The socially healthy employees are more likely to perceive their society as meaningful and feel a sense of belonging, promoting constructive engagement in personal and professional areas. Conversely, employees with poor social health are prone to despair, hopelessness, and reduced psychological well-being, which can negatively impact their work performance and personal life. The study results also confirmed a significant association between social health and factors such as perceived social support, hope for the future, general social trust, and social vitality. The results echo previous research and suggest that social support is critical to employees’ mental and social well-being. Employees who perceived greater social support from their colleagues and supervisors generally reported higher levels of social health.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Bushehr Branch, Islamic Azad University, Bushehr, Iran (Code: IR.IAU.B.REC.1402.063).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interpretation of the results, and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors want to thank everyone who helped them with the project.
References
The workplace strongly influences employees’ social health. According to research, an organization’s workplace can significantly affect employee happiness and job satisfaction [1]. Higher job satisfaction and productivity levels can result from supportive work environments that prioritizing employee social health and better employee retention and organizational performance [2]. These work environments generate healthy interactions between colleagues, employee engagement, and a sense of purpose. In addition, they provide opportunities for professional development, recognition, and work-life balance, all of which can improve the overall social health of employees [3]. Fostering a sense of belonging within an organization is the strongest driver of employee engagement. When employees feel connected and included, overall job satisfaction and loyalty to the company rise. A workplace prioritizing social health fosters a supportive community, reduces feelings of isolation and burnout, and fosters a collaborative atmosphere [4].
As a prerequisite for active participation in social roles, health is intimately linked to the general well-being of a community. Social health is undoubtedly the most important aspect of social issues, individually and collectively. Throughout history, people have pursued social health, culminating in developing comprehensive medical and biological sciences dedicated to protecting individual and societal health [5]. Currently, any decline in societal health, whether physical or mental, inevitably hinders progress and development. Consequently, societies that strive for sustainable development prioritize the health of their members [6].
Social environments and socioeconomic conditions significantly determine each aspect of an individual’s health [7]. The concept of social health was first introduced by Belloc et al. [8] and a few years later by Ware et al. [9]. They believed that health was a broader concept than reporting symptoms of illness and a person’s functional abilities. They argued that individual well-being and comfort differ from physical and mental health [10]. The World Health Organization (WHO) has recognized social health as one of several aspects of an individual’s total health. Social health includes emotional, psychological, and social well-being and influences cognition, perception, and behavior. According to WHO, it is a “state of well-being in which individuals recognize their abilities, cope with the normal stresses of life, work productively and fruitfully, and contribute to the well-being of their community” [11]. Still, the concept of social health is frequently associated with social indicators operationalized through economic measures (e.g. gross domestic product and poverty rate) that reflect the “health” of narrow sectors of society. Keyes [12] was a leading sociologist in the micro-level conceptualization and measurement of social health. He believed that social health is a person’s assessment of his or her functioning in society.
Social health can be defined as an individual’s self-report of the quality of their relationships with other people, the neighborhood, and the community. Social health represents a fundamentally public (as opposed to private) phenomenon focusing on social obligations people face within social structures and communities. Keyes [12] defined social health as a person’s report of the quality of relationships with others (close people and social groups) to which they belong. He believed that the key to deciding whether a measure of social well-being is part of an individual’s health is whether the measure reflects internal responses to stimuli—feelings, thoughts, and behaviors that reflect satisfaction or dissatisfaction with the social environment. The WHO was the first to mention social health as a dimension of health. Numerous studies have shown that the quantity and quality of a person’s relationships with others affect their physical and mental health. Social health, as a dimension of health, is the ability to perform social roles effectively and efficiently without harming others, and is an evaluation of an individual’s conditions and achievements in society. Some social factors shape various dimensions of social health, including social integration, social acceptance, social participation, social flourishing and social cohesion [13]. Researchers in workplace activity have long developed theoretical models to explain the influence of the work environment on social health. These theoretical models were originally based on a “stimulus-response” principle and have been refined to incorporate various variables (individual or environmental) that moderate or exacerbate the effects of the work environment on social health [14].
Keyes (1998) proposed five dimensions of social well-being operationalized at the level of the individual: Social integration, social acceptance, social contribution, social coherence, and social actualization. Social integration is the degree to which people feel a sense of common identity and belonging to those who make up their social reality (the quality of relationships between individuals concerning society. Social acceptance is the interpretation of a society based on the character and qualities of other people as a generalized category. Social contribution refers to an individual assessing their social value. Individuals with an appropriate level of social contribution believe that what they do in society is valuable. Social coherence refers to an individual’s assessment of whether society is understandable, predictable, and tangible. Finally, social actualization refers to a person’s evaluation of a society’s potential and developmental trajectory and the belief that the society is experiencing gradual progress and has the potential for positive transformation [15].
Hosseinzadeh et al. [15] conducted a case study with young adults in Khorramabad City, Iran and found a significant association between social capital variables and social health. Furthermore, they observed a direct relationship between life satisfaction and social health in young adults, whereas social alienation had an inverse relationship with social health. The regression analysis revealed that 51% of the variance in social health was explained by five social capital variables: social trust, social networks, social participation, social norms, and social sanctions.
Ghorbani et al. [16] examined the relationship between psychological capital and social health, considering the mediating role of social support. Their results showed that university students with higher levels of psychological capital had better social health.
The Persian Gulf special economic zone (PGSEZ) is a major economic institution that plays a critical role in transforming global supply chains and development models. The PGSEZ is at the 13th km of the Shahid Rajaei Highway in Bandar Abbas, Iran. It was initially set up as a special economic zone for mining and metals on January 14, 1998. However, it later changed its name to PGSEZ. The PGSEZ is strategically located in the Persian Gulf region, known for its rich natural resources, particularly in the mining and metals industries [17].
This study offers several novel contributions to the literature on social health in industrial settings, with a particular focus on PGSEZ in Hormozgan Province, Iran. It addresses the unique sociocultural and organizational context of Iranian industrial settings, which has been largely overlooked in previous research. It extends the literature by focusing on high-risk industrial sectors where social health can play a critical role in alleviating work stress and improving safety. Given the lack of information on the social health and psychological well-being of industrial workers in Hormozgan Province, this study aimed to examine the following hypotheses:
Hypothesis 1: The social health status of employees working in PGSEZ is average. Hypothesis 2: There is a significant association of the level of “perceived social support,” “hope for the future,” “general social trust,” and “social vitality” with the level of “social health” of employees working in PGSEZ.
Methods
Study design and participants
This study aimed to examine the social health of employees working in PGSEZ. This study was conducted using a correlational design. A total of 237 participants were selected using cluster sampling. Data were collected using Keyes social well-being and perceived social support scales. Parametric and nonparametric statistical tests were used to analyze the data in SPSS software, version 26. The research population consisted of all employees working in PGSEZ in 2023. The sample size was 237 participants selected using a cluster sampling method. This study used the Cochran formula to determine the sample size. The final sample size accepted by the research team comprised 250 participants, but 237 participants answered the questionnaires. We collected the data after obtaining the participants’ consent to observe the ethical considerations in this research. Participants were assured of the confidentiality of their personal information, and the results were provided without specifying the names and details of the participants. Ethical considerations were also carefully considered throughout the research process, demonstrating the researcher’s commitment to respecting the participants’ involvement and confidentiality.
Study measures
Keyes social well-being scale
The Keyes social well-being scale is a 20-item questionnaire that measures various aspects of social health, including social integration, social acceptance, social contribution, social coherence, and social actualization. The questionnaire is scored on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (completely agree) [12]. In this scale, items 1, 6, 13, 14, 15, 17, 18, 19 and 20 are reverse scored (1=5, 2=4, 3=3, 4=2, 5=1). After adding the scores for all 20 items, the total score can range from 20 to 100.
In this study, the Cronbach α was used to estimate the scale’s internal consistency, which was 0.90, indicating an acceptable reliability. Also, the Cronbach α for all dimensions of this questionnaire were as follows: Social integration (α=0.84), social acceptance (α=0.91), social contribution (α=0.89), social coherence (α=0.84) and social actualization (α=0.91). Thus, the reliability of the questionnaire for all dimensions was confirmed.
The validity of the Keyes social well-being scale has been supported in various studies that confirmed its effectiveness in measuring social well-being across different populations [1, 18]. Keyes (1998) provided evidence of both convergent and discriminant validity, showing that the dimensions of social well-being correlate significantly with other established measures, such as anomie, generativity, perceived social constraints, community involvement and overall social health [12]. Content and construct validity were examined in this study to evaluate the scale’s validity. Content validity focuses on whether the scale fully represents the theoretical construct of social well-being. In this study, content validity was assessed using the theories of experienced professors and the approval of sociology and psychology experts. This approach ensured the content was theoretically sound and practically relevant, incorporating insights from established scholars in the respective fields. The involvement of experts helped enhance the credibility and reliability of the research findings. This study assessed construct validity through confirmatory factor analysis to ensure that the scale items loaded on the expected factors corresponding to the theoretical dimensions. The findings showed satisfactory fit indices with a comparative fit index of 0.94 and a root mean square error of approximation of 0.05. These results indicated strong construct validity and confirmed that the scale effectively measured the intended constructs as theoretically predicted.
Perceived social support scale
The multidimensional scale of perceived social support (MSPSS) developed by Canty-Mitchell and Zimet [19] was used to assess perceived social support. This scale consists of 12 items measuring three components: perceived support from family (4 items), perceived support from significant others (4 items) and perceived support from friends (4 items).
All items on the scale are rated on a 5-point Likert scale (strongly agree, agree, neither agree nor disagree, disagree, strongly disagree). The total score for the scale ranges from 12 to 60.
The Cronbach coefficient α, a measure of internal reliability, was obtained for the total scale and each subscale. For the “significant others,” “family,” and “friends” subscales, the values were 0.91, 0.87, and 0.85, respectively. The reliability of the total scale was 0.88. These values indicate good internal consistency for the scale as a whole and its three subscales [19]. In this study, the reliability of the total scale was 0.85.
Data analysis
Data collected using questionnaires were analyzed at descriptive and inferential statistics levels using SPSS software, version 26. The descriptive statistics section presented the frequency and percentage of the research variables in tables. The inferential statistics section used the Pearson correlation coefficient test, one-sample independent t-test, linear regression, analysis of variance (ANOVA) and multicollinearity test.
Results
Demographic findings revealed that 209 participants (80%) were male and 28(20%) were female. Regarding education, 22 participants (9.3%) had a high school degree, 49(20.67%) a diploma degree, 31(13.08%) a college or associate’s degree, 93(39.24%) a bachelor’s degree, and 42(17.72%) postgraduate (MS and PhD) degrees. Finally, 38 participants (16%) were permanent and formally employed and 199 (84%) were temporary and contract employees.
Hypothesis 1: The social health status of employees in the PGSEZ is average. According to Table 1, the sample mean is 3.43. Based on the obtained t value of 12.52 with 236 df, there is a significant difference between the obtained mean and the acceptable sufficiency level at a 95% confidence interval (CI) (P<0.05). Furthermore, the obtained mean value deviates significantly from the desired sufficiency level, as indicated by the t-value of -16.50 (P<0.05). Based on the above findings, social health among workers in the PGSEZ is well above the acceptable and desired sufficient level. Therefore, Hypothesis 1 is confirmed.
Hypothesis 2: There is a significant association of the level of “perceived social support,” “hope for the future,” “general social trust,” and “social vitality” with the level of “social health” of employees working in PGSEZ.
According to Table 2, the correlation coefficients between perceived social support and employee social health (r=0.397), hope for the future and employee social health (r=0.715), general social trust and the social health of employees (r=0.620) as well as social vitality and social health of employees (r=0.551) are all positive and significant (P<0.05). These findings suggest that as these variables’ values increase, employees’ social health level increases and vice versa. Therefore, the hypothesis is confirmed.
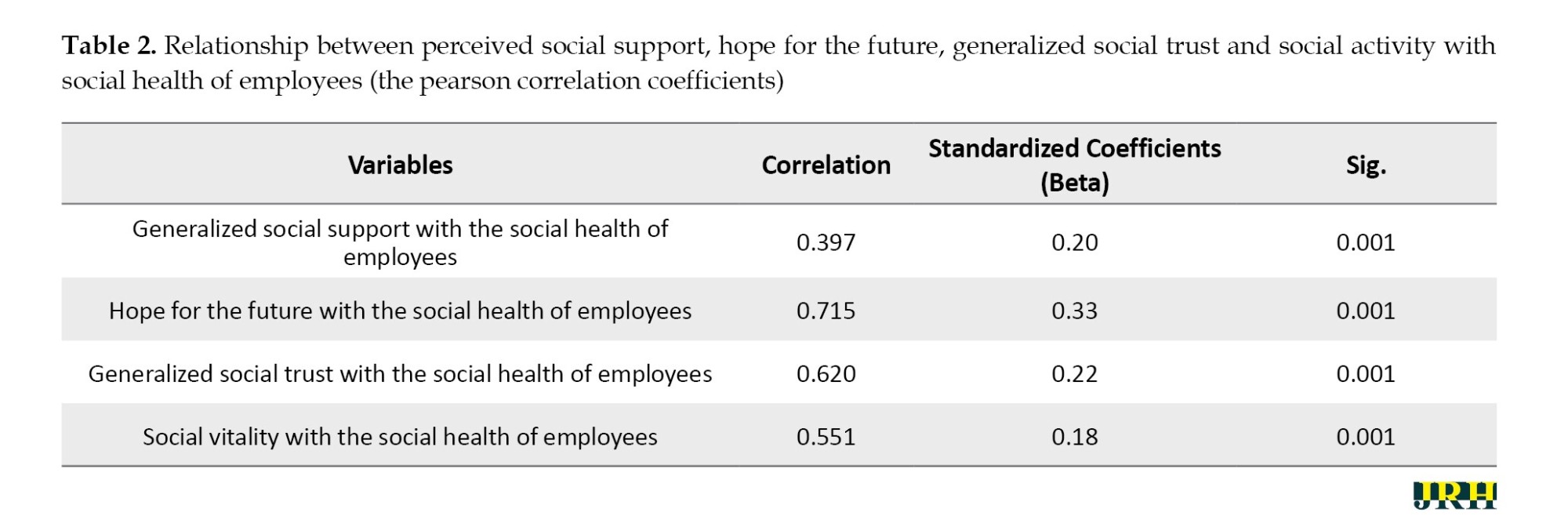
Among these variables, the “hope for the future” variable has the greatest impact on social health, with a beta value of 0.33. The direction of the effect of this variable is positive, indicating that as hope for the future increases, employees’ social health also improves. In other words, for every unit of standard deviation increase in future hope, there is a corresponding 0.33 standard deviation increase in employee social health. Perceived social support, generalized social trust, social vitality, and hope for the future are important predictors of social health.
According to Table 3, the tolerance index for all independent variables is greater than 0.4, and the variance inflation factor is <2.5. These results indicate no significant multicollinearity between the independent variables. The results of the multicollinearity test support using multiple regression to test the hypothesis. The absence of multicollinearity suggests that the independent variables are not redundant and that each variable uniquely contributes to predicting the dependent variable.
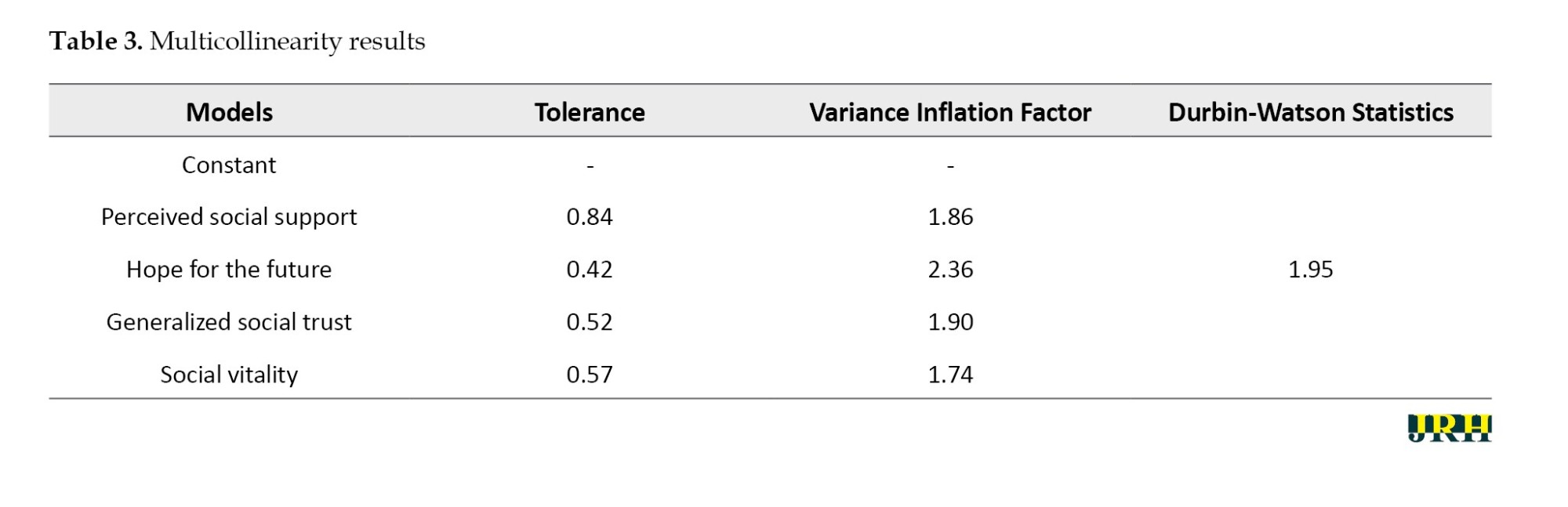
Another assumption of regression is that the errors (the differences between the actual values and the values predicted by the regression equation) are independent of each other. The Durbin-Watson test was used to check the independence of errors. According to Table 3, the Durbin-Watson statistics (d) of 1.95 is between 1.5 and 2.5, indicating that the assumption of no autocorrelation between the errors is met.
As shown in Table 4, the coefficient of determination (R2) is 0.664. This finding indicates that 66.4% of the variance in social health is explained by perceived social support, generalized social trust, social vitality, and hope for the future.
Discussion
This study examined the social health of employees working in the PGSEZ. The interpretation of hypothesis 1 results suggests that the “level of social health among employees” is significantly higher than the acceptable and desired sufficiency levels for both. Therefore, Hypothesis 1 was confirmed. While employees working in the PGSEZ do not enjoy the desired level of social health, they have a moderate level of social health. The findings of this study were consistent with those reported by Moradi et al. [7], Parvish et al. [5], Arabi [6], Goudarzi and Sabzevar [20], Hosseinzadeh et al. [15], Hajebi and Faridnia [21] and Keyes and Shapiro [22]. The results show that most employees working in the PGSEZ have an average level of social health. Many employees have poor social health, which can be described as social illness.
Social health is a social goal and a desired outcome of various societal development measures. Achieving this goal requires resource utilization mechanisms and coordinated programs at the social, economic, and political levels. Social health, like education, is considered one of the most important social and economic indicators, since ensuring health components among various groups in society increases the sense of security and sustainable economic growth and development in any country. Social health, an important dimension of health, is defined as an individual’s assessment of the quality of his or her relationships with family, others, and social groups. The Keyes social health scale indicates a person’s satisfaction or dissatisfaction with life and social environment [12]. According to Goudarzi and Sabzevar [20], a socially healthy individual functions well when perceiving society as a meaningful, understandable, and potentially growing and thriving. They feel like they belong to social groups and see themselves as partners in society and its progress [15].
Interpreting the results of hypothesis 2 suggests that social support, a fundamental aspect of social interactions, includes the perception, reception, and need for support and encouragement from one’s social network. The type and importance of social support vary significantly from one person to another and are influenced by age, gender, personality, and cultural background. Furthermore, the aspects of social support that matter most may fluctuate over the life course, with certain elements taking precedence over others at different stages. In this context, social relationships can be conceptualized as an intermediate variable that bridges the gap between social circumstances and individual well-being. The quality and quantity of social support play a critical role in determining how social conditions impact an individual’s health. The results of the current study are also consistent with the research of Hajebi and Faridnia [21] entitled “The relationship between mental health and social support in health staff of Bushehr oil industry.” Both studies demonstrate a significant association between mental health and social support, although this association varies depending on demographic factors. Furthermore, the present study shows that employees working in rotating shifts experience lower psychological well-being and social support levels than employees in other employment arrangements.
Hope for the future is a cornerstone of quality of life and social health. It serves as the origin of every dynamic and progressive aspect of human existence. Hope for the future is a basic human need because without it, individuals cannot follow their personal and social goals [23]. While individual circumstances significantly influence hope for the future, social factors are crucial in increasing or weakening its intensity. On the one hand, society can promote conditions that lead individuals to realize their personal goals and desires.
The connection between social vitality and employees’ social health can be characterized as a reciprocal and mutually reinforcing dynamic. Social health in employees increases the likelihood of increased social vitality, although with the caveat that broader external variables at the societal level also influence this phenomenon. Socially important employees demonstrate increased motivation, greater commitment to work, loyalty to the organization, and dedication to their employer [10]. These factors, in turn, have a positive impact on the productivity and profitability of the organization. However, it is important to recognize that job satisfaction represents only one dimension of social vitality. Promoting social vitality among employees and workers has much deeper and broader implications [13].
Based on the study findings, the following recommendations have been made. Companies should consider integrating social health metrics into their overall employee health assessment. This measure can help identify areas that need improvement and track progress over time. Training programs for managers on the importance of social health and fostering a supportive environment can be helpful. Managers play a critical role in shaping workplace culture and employee experiences. Continuous evaluation of workplace wellness initiatives is essential to ensure they meet the changing needs of employees. Feedback mechanisms should be considered to collect employee insights on social health initiatives.
This study has some limitations. It is limited to the industries and organizations in the PGSEZ and does not include other industry organizations in Iran. The study did not include a comparison group of employees working in different industries or regions of Iran. The study focuses exclusively on employees, so the generalizability of the results to this specific group is limited. The study used a cross-sectional design, meaning the data were collected simultaneously. This design limitation prevents researchers from establishing causal relationships between sociocultural workplace factors and social health and mental illness.
Conclusion
The study concluded that workers’ social health was not at the desired level, but at a moderate level in the PGSEZ. The study highlighted that social health is an important dimension of overall health, similar to physical and mental well-being. Social health encompasses a person’s perception of their relationships and social environment and significantly impacts their psychological and social functioning. The socially healthy employees are more likely to perceive their society as meaningful and feel a sense of belonging, promoting constructive engagement in personal and professional areas. Conversely, employees with poor social health are prone to despair, hopelessness, and reduced psychological well-being, which can negatively impact their work performance and personal life. The study results also confirmed a significant association between social health and factors such as perceived social support, hope for the future, general social trust, and social vitality. The results echo previous research and suggest that social support is critical to employees’ mental and social well-being. Employees who perceived greater social support from their colleagues and supervisors generally reported higher levels of social health.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Bushehr Branch, Islamic Azad University, Bushehr, Iran (Code: IR.IAU.B.REC.1402.063).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interpretation of the results, and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors want to thank everyone who helped them with the project.
References
- Morse G, Salyers MP, Rollins AL, Monroe-DeVita M, Pfahler C. Burnout in mental health services: A review of the problem and its remediation. Administration and Policy in Mental Health. 2012; 39(5):341-52. [DOI:10.1007/s10488-011-0352-1] [PMID] [PMCID]
- Sirgy MJ, Reilly NP, Wu J, Efraty D. Review of research related to quality of work life (QWL) programs. In: Land K, Michalos AC, Sirgy MJ, editors. Handbook of social indicators and quality of life research. London: Springer; 2012. [DOI:10.1007/978-94-007-2421-1_13]
- Atroszko PA, Atroszko B. The costs of work-addicted managers in organizations: Towards integrating clinical and organizational frameworks. Amfiteatru Economic. 2020; 22(14):1265-82. [DOI:10.24818/EA/2020/S14/1265]
- Radu C. Fostering a positive workplace culture: Impacts on performance and agility. Vilas Boas AA, editor. Human resource management-an update. London: IntechOpen; 2023. [DOI:10.5772/intechopen.1003259]
- Parvish T, Behravan H, Hasani Darmian G. Identification and prioritization of effective factors on the social health of the elderly using DEMATEL and ISM Methods. Journal of Research and Health. 2021; 11(3):165-74. [DOI:10.32598/jrh.11.3.1736.1]
- Arabi S. Sociological analysis of social harms and their influence on health. Journal of Research and Health. 2019; 9(1):1-2. [DOI:10.29252/jrh.9.1.1]
- Moradi G, Mohammadi A, Jahanbakhsh I. A comparison of social health components among the farmers in the villages of saffron and other plants in South Khorasan Province. Journal of Research and Health. 2021; 11(5):341-50. [DOI:10.32598/jrh.11.5.1723.1]
- Belloc NB, Breslow L, Hochstim JR. Measurement of physical health in a general population survey. American Journal of Epidemiology. 1971; 93(5):328-36. [DOI:10.1093/oxfordjournals.aje.a121265] [PMID]
- Ware JE, Eisen M, Brook RH, Donald CA. Conceptualization and measurement of health for children in the health insurance study. Santa Monica: RAND Corporation; 1980. [Link]
- Tavakol M, Mousavi SMA. Investigating the effects of industrialization on various aspects of societal health (proposing a theoretical model). Quarterly of Social Studies and Research in Iran. 2024; 12(4):608-28. [DOI:10.22059/jisr.2024.363426.1425]
- World Health Organization (WHO). Working for a brighter, healthier future: how WHO improves health and promotes well-being for the world’s adolescents. Geneva: World Health Organization; 2021. [Link]
- Keyes CLM. Social wll-being. Social Psycology Quarterly. 1998; 61(2):121-40. [DOI:10.2307/2787065]
- Soofizad G, Rakhshanderou S, Ramezankhani A, Ghaffari M. The concept of social health from an iranian perspective: A qualitative exploration. Frontiers in Public Health. 2022; 10:797777. [DOI:10.3389/fpubh.2022.797777] [PMID] [PMCID]
- Althaus V, Kop JL, Grosjean V. Critical review of theoretical models linking work environment, stress and health: Towards a meta-model. Le Travail Humain. 2013; 76(2):81-103. DOI: 10.2307/41969976 [DOI:10.3917/th.762.0081]
- Hosseinzadeh AH, Rashidi S, Rostami A. [A study on the relationship between social capital and social health (Case study: Youth in Khorramabad city) (Persian)]. Strategic Studies on Youth and Sports. 2021; 20(52):293-310. [Link]
- Ghorbani S, Jahanizadeh MR, Mirbod SM, Omidi L. [Investigation the relation of psychological and social capitals with social health, with regards to the, mediator variable of social support (Persian)]. Social Psychology Research. 2020; 10(38):83-100. [DOI:10.22034/spr.2020.114694]
- Noori S, Korevaar G, Ramirez AR. Assessing industrial symbiosis potential in emerging industrial clusters: The case of Persian Gulf mining and metal industries special economic zone. Journal of Cleaner Production. 2021; 280(1):124765. [DOI:10.1016/j.jclepro.2020.124765]
- Sham WWL, Yeung GTY, Mak WWS, Powell CLYM. Comprehensive well-being scale: Development and validation among Chinese in recovery of mental illness in Hong Kong. BMC Psychology. 2021; 9(1):179. [DOI:10.1186/s40359-021-00686-4] [PMID] [PMCID]
- Canty-Mitchell J, Zimet GD. Psychometric properties of the multidimensional scale of perceived social support in urban adolescents. American Journal of Community Psychology. 2000; 28(3):391-400. [DOI:DOI:10.1023/A:1005109522457] [PMID]
- Goudarzi S, Sabzevar A. [Sociological study of factors related to social health of working women in hospital (Persian)]. Journal of Woman and Family Studies. 2022; 10(2):108-32. [DOI:10.22051/jwfs.2022.32253.2479]
- Hajebi A, Faridnia P. [The relationship between mental health and social support in health staffs of Bushehr oil industry (Persian)]. Iranian South Medical Journal. 2009; 12(1):67-74. [Link]
- Keyes C, Shapiro A. Social well-being in the US: A descriptive epidemiology. In: Ryff CD, Gilbert Brim O, Kessler C. editor. How healthy are we? A national study of well-being of Midlife. Chicago: University of Chicago Press; 2004. [Link]
- Niazi M, Farhadian A, Irani F, Khoshbayani F. A meta-combination study of model design and dimensions affecting life expectancy in young people. Strategic Studies on Youth and Sports. 2023; 22(60) [Unpublished]. [DOI:10.22034/ssys.2023.2847.3074]
Type of Study: Orginal Article |
Subject:
● Psychosocial Health
Received: 2024/06/13 | Accepted: 2024/11/2 | Published: 2025/07/1
Received: 2024/06/13 | Accepted: 2024/11/2 | Published: 2025/07/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









