Volume 15, Issue 4 (Jul & Aug 2025)
J Research Health 2025, 15(4): 365-374 |
Back to browse issues page
Ethics code: 4454/TMS/2023
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Falah M, Sansuwito T B, Dioso R I, Sari N P, Lismayanti L, Pranata S et al . A Family’s Knowledge and Attitudes Toward the Prevention of Pulmonary Tuberculosis in Tasikmalaya City, Indonesia, in 2023: A Cross-sectional Study. J Research Health 2025; 15 (4) :365-374
URL: http://jrh.gmu.ac.ir/article-1-2597-en.html
URL: http://jrh.gmu.ac.ir/article-1-2597-en.html
Miftahul Falah1 

 , Tukimin Bin Sansuwito2
, Tukimin Bin Sansuwito2 

 , Regidor III Dioso2
, Regidor III Dioso2 

 , Nina Pamela Sari3
, Nina Pamela Sari3 

 , Lilis Lismayanti3
, Lilis Lismayanti3 

 , Satriya Pranata4
, Satriya Pranata4 

 , Sri Wahyuni5
, Sri Wahyuni5 




 , Tukimin Bin Sansuwito2
, Tukimin Bin Sansuwito2 

 , Regidor III Dioso2
, Regidor III Dioso2 

 , Nina Pamela Sari3
, Nina Pamela Sari3 

 , Lilis Lismayanti3
, Lilis Lismayanti3 

 , Satriya Pranata4
, Satriya Pranata4 

 , Sri Wahyuni5
, Sri Wahyuni5 


1- Department of Nursing, Faculty of Health Sciences, Universitas Muhammadiyah Tasikmalaya, Tasikmalaya, Indonesia. , miftahul@umtas.ac.id
2- Department of Nursing, Faculty of Nursing, Lincoln University College, Petaling Jaya, Malaysia.
3- Department of Nursing, Faculty of Health Sciences, Universitas Muhammadiyah Tasikmalaya, Tasikmalaya, Indonesia.
4- Department of Nursing, Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Indonesia.
5- Department of Nursing, Faculty of Health Science, Universitas YPIB Majalengka, Majalengka, Indonesia.
2- Department of Nursing, Faculty of Nursing, Lincoln University College, Petaling Jaya, Malaysia.
3- Department of Nursing, Faculty of Health Sciences, Universitas Muhammadiyah Tasikmalaya, Tasikmalaya, Indonesia.
4- Department of Nursing, Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Indonesia.
5- Department of Nursing, Faculty of Health Science, Universitas YPIB Majalengka, Majalengka, Indonesia.
Full-Text [PDF 753 kb]
(82 Downloads)
| Abstract (HTML) (672 Views)
Full-Text: (41 Views)
Introduction
Tuberculosis (TB) is an infectious disease caused by the bacteria Mycobacterium tuberculosis and remains a major health threat globally and in Indonesia. TB has become one of the oldest infectious diseases for humans and around one billion people have died [1]. The barrier that makes TB difficult to treat and eliminate is inextricably tied to Mycobacterium TB's intracellular lifestyle [2]. The immunological response to M. tuberculosis is multifaceted and complicated [3]. Cough is a central feature of pulmonary TB, as a symptom, a marker of disease activity, and a means of transmitting infection. Cough can be followed by other symptoms such as bloody sputum, bleeding cough, shortness of breath, drowsiness, loss of appetite, weight loss, anger, night sweats if not physically active, and constant shivering for over a month [4, 5]. The physical, psychological, social, and environmental aspects of TB patients are strongly connected, and these experiences greatly impact their quality of life.
TB is still a major global public health concern, accounting for a large portion of disease and mortality. Despite advancements in diagnosis and treatment, more than 10 million new cases of TB were recorded in 2020, with an anticipated 1.5 million TB-related deaths globally [6]. About 25% of people on the planet are carriers of latent TB infections, which increases their chance of ever experiencing active disease. The World Health Organization (WHO) projects that by 2021, there will be an estimated 10.6 million TB cases worldwide, an increase of almost 600000 cases [7].
The Ministry of Health in Indonesia reports the highest number of cases in West Java (105794 cases), East Java (71791 cases), Central Java (65014 cases), DKI Jakarta (41441 cases) and North Sumatra (35.035 cases). According to the Indonesian Ministry of Health, they are the five provinces with the highest number of cases. West Java is a densely populated, humid area conducive to the growth of pulmonary TB cases [8, 9]. One city in the province of West Java is Tasikmalaya, where 2837 cases of TB were reported in 2022, 1476 cases in 2021, 1041 cases in 2020 and 1435 cases in 2019. The number of TB patients appears small, yet they are quite numerous. Pulmonary TB is similar to the “ice mountain phenomenon” in that some individuals are terrified of becoming ill and getting sputum tested. Poor knowledge and negative attitudes contribute to an increase in TB patients in some areas. They remain quiet about the illness they have for a reason—a low sense of self-worth and a fear of rejection from their family and communities. The level of knowledge and negative attitudes toward TB will make it difficult to diagnose and cure the patients [10-12].
Poor knowledge about TB is a significant factor contributing to its high incidence and treatment challenges. Studies have shown that TB patients often have better knowledge than the general population. However, knowledge remains inadequate regarding transmission, symptoms and prevention. Factors associated with poor TB knowledge include older age, lower education, and lack of prior TB diagnosis. Limited knowledge can lead to delayed treatment, poor adherence, and increased risk of recurrence [13]. Misconceptions about TB transmission persist, and stigma remains a concern. Community interventions and health education programs can improve TB knowledge. Enhancing TB-related knowledge is crucial for better healthcare-seeking behavior, treatment adherence, and ultimately, TB control and eradication efforts [14].
Negative attitudes toward TB patients can significantly impact treatment adherence and outcomes. Studies have shown that health care workers, including resident doctors and nursing students, often display fear, a lack of compassion, and avoidance toward TB patients. These attitudes can reinforce societal stigma and affect patients’ treatment-seeking behavior [8]. However, positive attitudes and knowledge about TB among healthcare providers and patients are associated with better treatment adherence. Training programs for health care workers and structured patient education can improve knowledge, attitudes and treatment outcomes. Additionally, community-based directly observed treatment (CB-DOT) can be effective, but patients’ perceived attitudes toward treatment observers can influence adherence. Addressing knowledge gaps and positive attitudes is crucial for improving TB control efforts [14].
Several studies have assessed the knowledge, attitudes, and practices (KAP) of TB patients in various countries. These studies consistently found that many patients had some awareness of TB symptoms and transmission, but there were significant knowledge gaps and misconceptions. Factors associated with better TB knowledge included higher education levels, urban residence, and male gender [15]. Despite knowledge gaps, most patients demonstrated favourable attitudes towards TB treatment. However, stigma and negative community attitudes remained challenges. Educational interventions were effective in improving TB knowledge and attitudes among patients. The studies highlighted the need for enhanced TB awareness programs, particularly targeting less educated groups and addressing misconceptions, to support TB control efforts [8].
TB patients' family knowledge and positive attitudes affect TB transmission prevention efforts. Knowledge is essential to prevent the spread of TB [16]. It covers awareness of and precautions against TB transmission in households with close relatives. The patient's family is very significant to the patient. A thorough understanding of the family can stop the disease from spreading to other family members. Previous studies show that of 23 families with good knowledge, 17(73.9%) were involved in TB prevention. Also, of 21 families with positive attitudes toward TB, 16(76.2%) had good performance in preventing TB transmission. In another study, 17 families had good knowledge and effective disease prevention (85%) and of the 30 respondents with high knowledge, 70% had a role in preventing the spread of TB inside the family [17, 18]. Attitudes towards TB were generally positive, although some studies reported negative attitudes. Preventive practices were often found to be inadequate. Many studies emphasized the need for improved TB education and awareness programs to address misconceptions and enhance prevention efforts. This finding aligns with the research that found a relationship between knowledge and family attitudes with the prevention of TB transmission [18-20]. The better the knowledge and the family attitudes of TB patients, the better the efforts of TB prevention [21]. Knowledge and attitudes determine family behaviour. Therefore, regarding treatment and prevention, TB disease transmission within the family plays a major role in preventing the transmission to other family members. This study investigates the association between family attitudes and knowledge regarding preventing pulmonary TB.
Methods
Study design
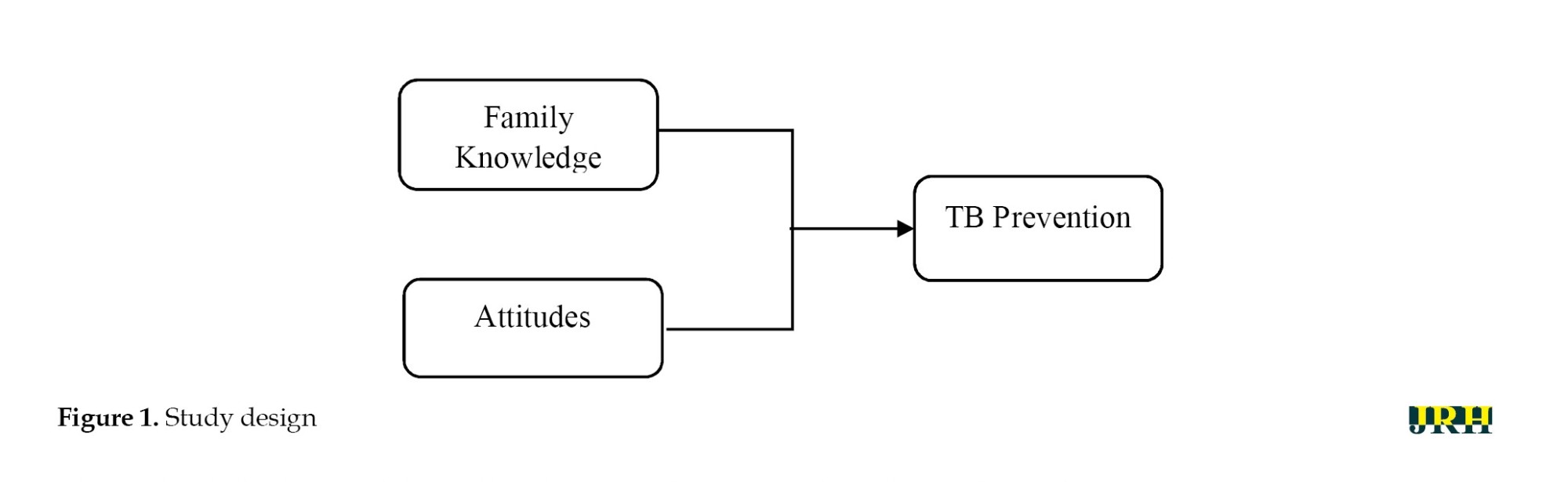
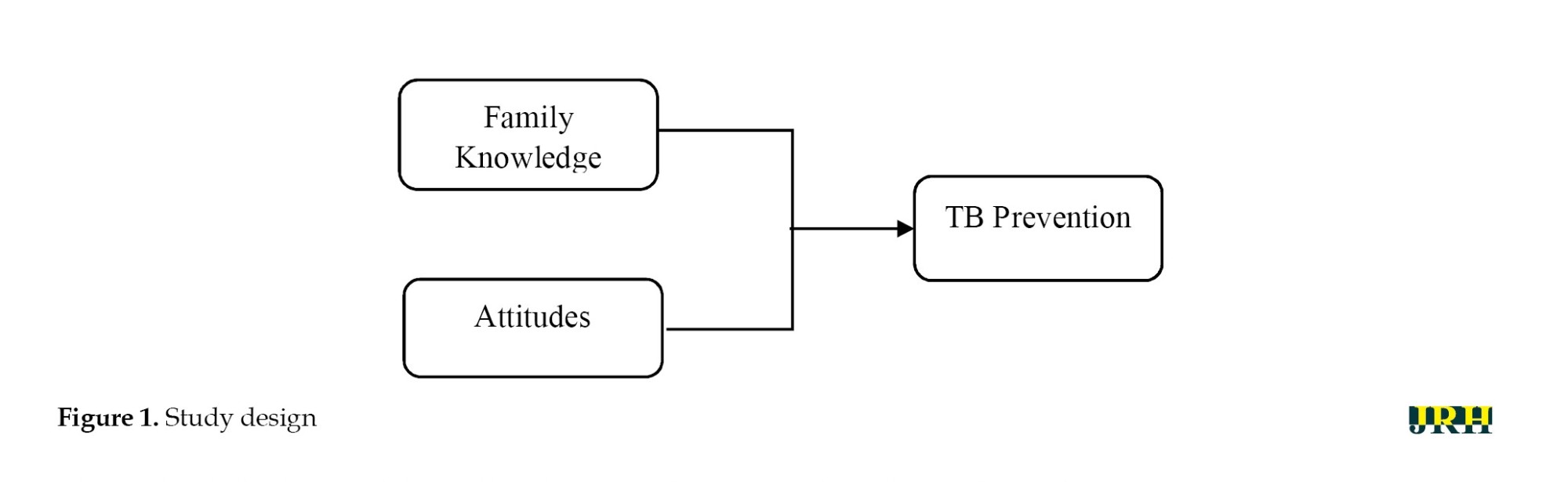
The study used a quantitative design and cross-sectional approach. The variables in the study were family knowledge, attitudes and TB prevention (Figure 1). This study found a relationship between the level of knowledge and family attitudes in preventing pulmonary TB.
Samples and locations
The sample in the study was a family with pulmonary TB patients referred to the Tamansari Public Health Center, Tasikmalaya, Indonesia in 2023 (total of pulmonary TB patients: 82 patients). All families with TB patients were identified and joined the WhatsApp group. This area focuses on handling the TB program and has become one of the highest cases in Tasikmalaya. The total sampling techniques used in this study included 82 respondents. All respondents were interviewed and filled out the questionnaire.
Data collection
Institutional review board permission was received from the health office of Tasikmalaya City (register: 128). Data collection was held from January to June 2023 with the cooperation of the Tamansari Public Health Center. Data collection in this study used a questionnaire (knowledge: 25 questions, attitudes: 25 questions, and TB prevention: 24 questions). Validity and reliability tests were conducted in the study. The reliability test found the acceptable values of Cronbach α for knowledge (0.961) and attitudes (0.976). The researcher meets with respondents and conducts informed consent before completing the survey. Ensure all questions are answered and saved into a box file—all data were entered into SPSS software, version 27 for data analysis.
Study instruments
The study used a questionnaire of knowledge (1: Right and 0: False), attitudes (4: Agree, 3: Agree, 2: Disagree and 1: Totally disagree) and TB prevention (3: Always, 2: Sometimes and 1: Never) developed from a previous study [7]. Skewness value with standard error for the knowledge subscale was -1.470; for the attitude subscale, -1.432; and for the prevention subscale, -1.342 (ranging between -2 and 2). Also, the cut-off point for the knowledge subscale was 18.45 (with a score ≥18.45 indicating good knowledge); for the attitude subscale, 68.99 (with a score ≥68.99 indicating positive attitude), and for the prevention subscale, 54.28 (with a score ≥54.28 indicating good performance). The instruments passed validity (conducted for 20 respondents at Purbaratu Public Health Centre) and reliability tests. The reliability test found the acceptable values of Cronbach α for knowledge (0.961) and attitudes (0.976).
Data analysis
Data analysis in the study used univariate, bivariate, and multivariate analyses. Univariate analysis was conducted to determine characteristic knowledge (good and poor), attitudes (positive and negative) and prevention practices among respondents (cut-off point). Bivariate analysis was conducted using a chi-square test to gain insight into relationships between variables, and multivariate analysis was used in logistic regression testing to find the dominant factor. The IBM SPSS software, version 27 application was used in the study. P<0.05 was Considered significantically.
Results
A total of 82 participants completed this study. Table 1 presents demographic characteristic as follows: Gender, 42 males (51.2%) and 40 females (48.7%); age, 11-20 years, 12(14.6%), 21-30 years, 20(24.3%), 31-40 years, 25(30.4%), >40 years, 25(30.4%); education, elementary school, 30(36.5%), Junior high school, 11(13.4%), senior high school, 20(24.3%), university, 21(25.6%); marital status, married, 60(73.1%), not married, 22(26.8%).
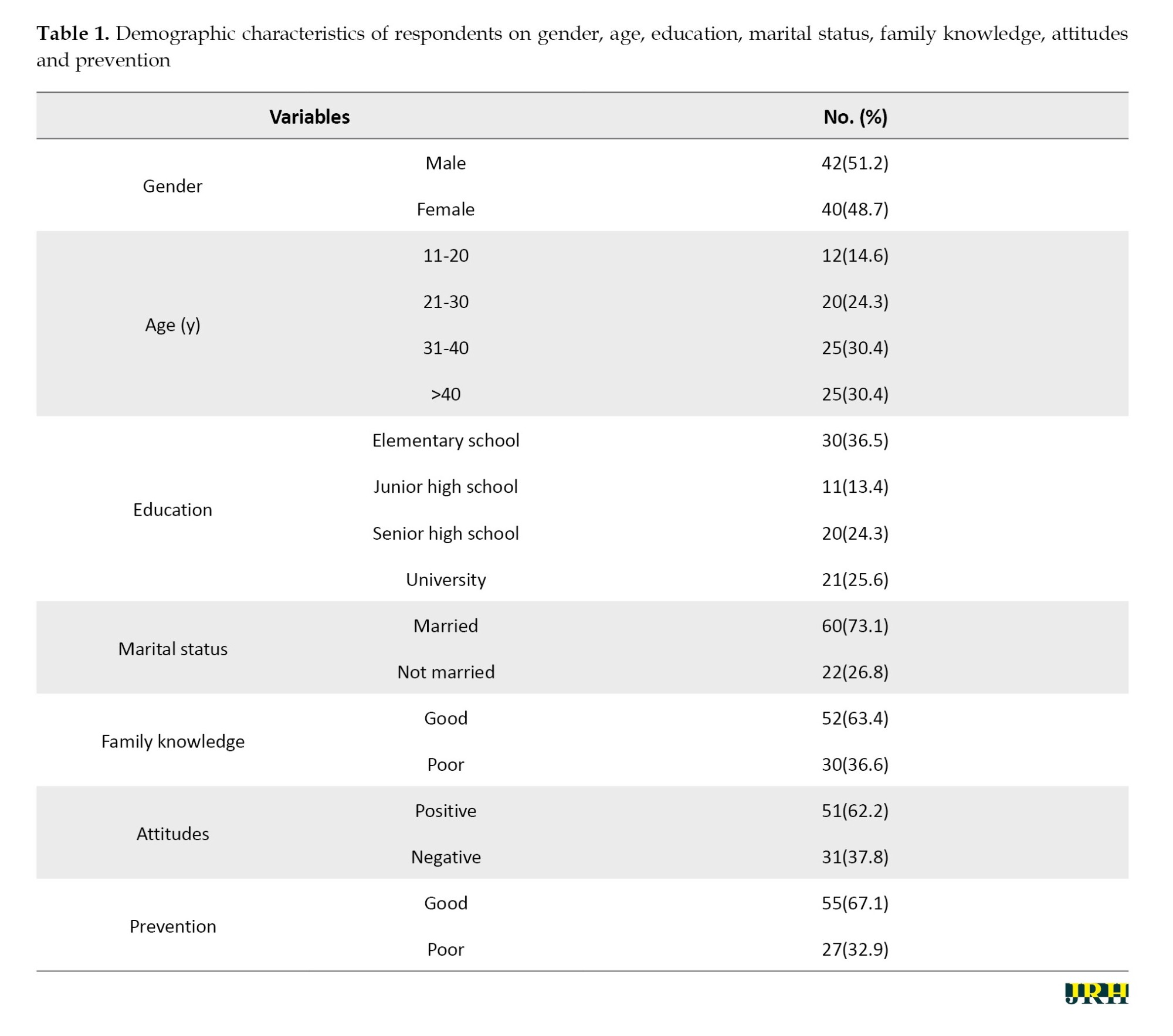
Frequency distribution of family knowledge about pulmonary TB disease shows that 52 people (63.4%) had good knowledge, and 30 people (36.6%) had poor knowledge. According to family attitudes, the data shows that 51 people (62.2%) had positive attitudes and 31 (37.8%) had negative attitudes. Based on data on TB prevention, the TB prevention of families with pulmonary TB patients was good in 55 people (67.1%) and poor in 27 people (32.9%) (Table 1).
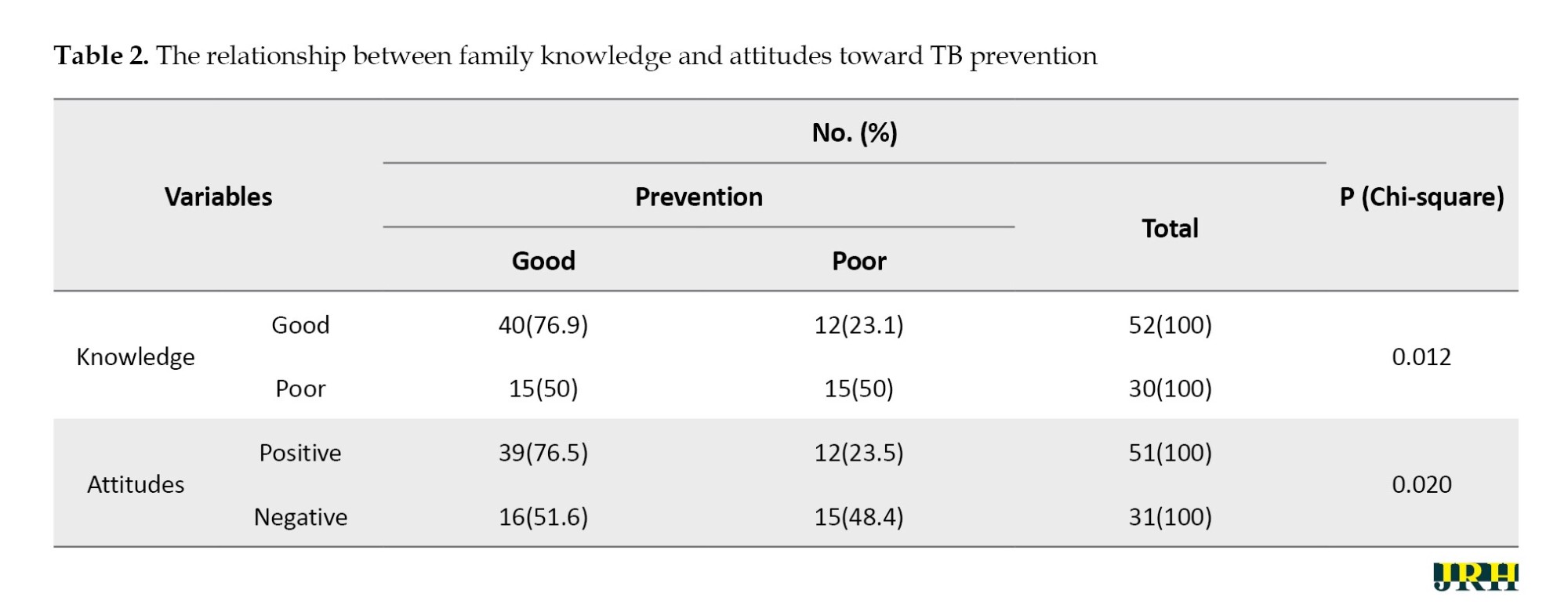
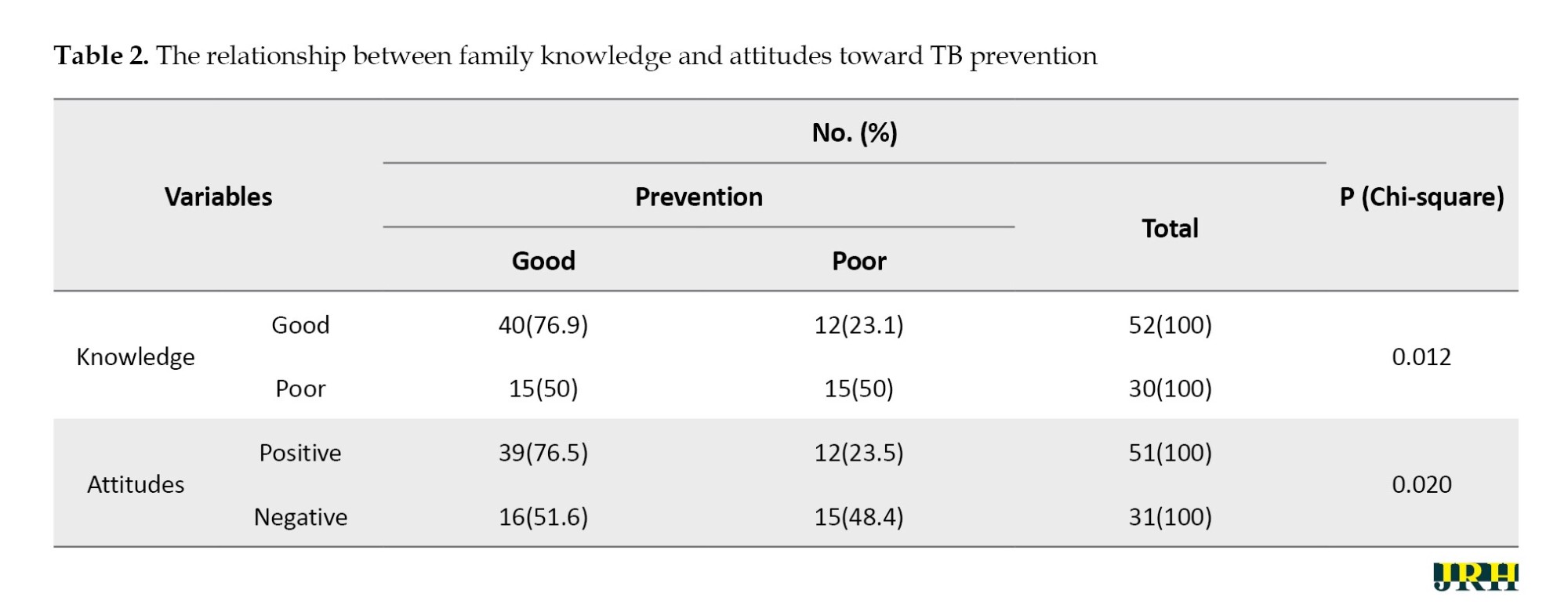
Family knowledge and attitudes are significantly associated with TB prevention, knowledge (P=0.012) and attitudes (P=0.020) (Table 2).
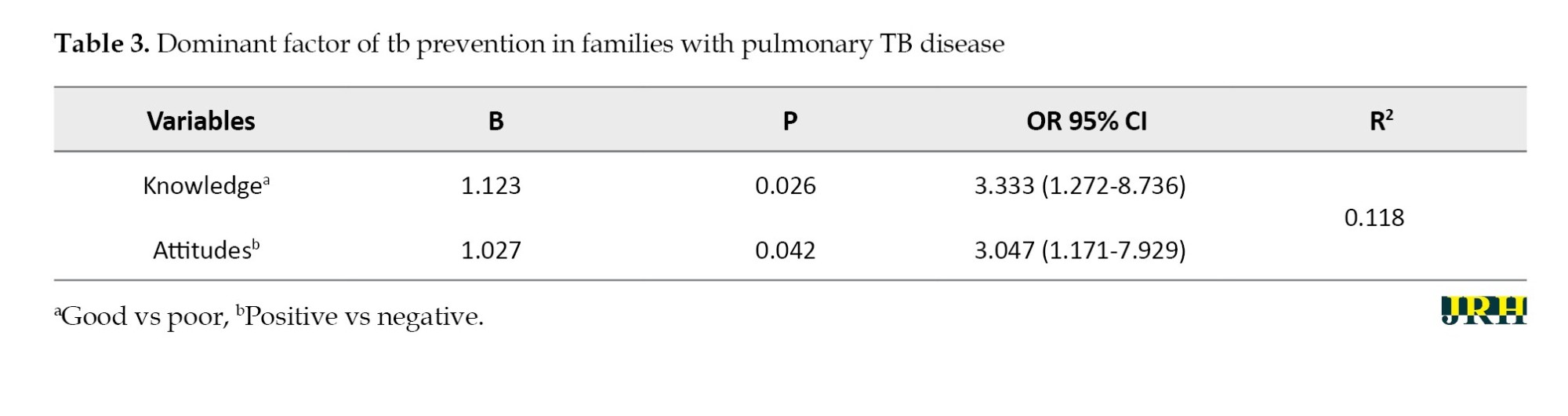
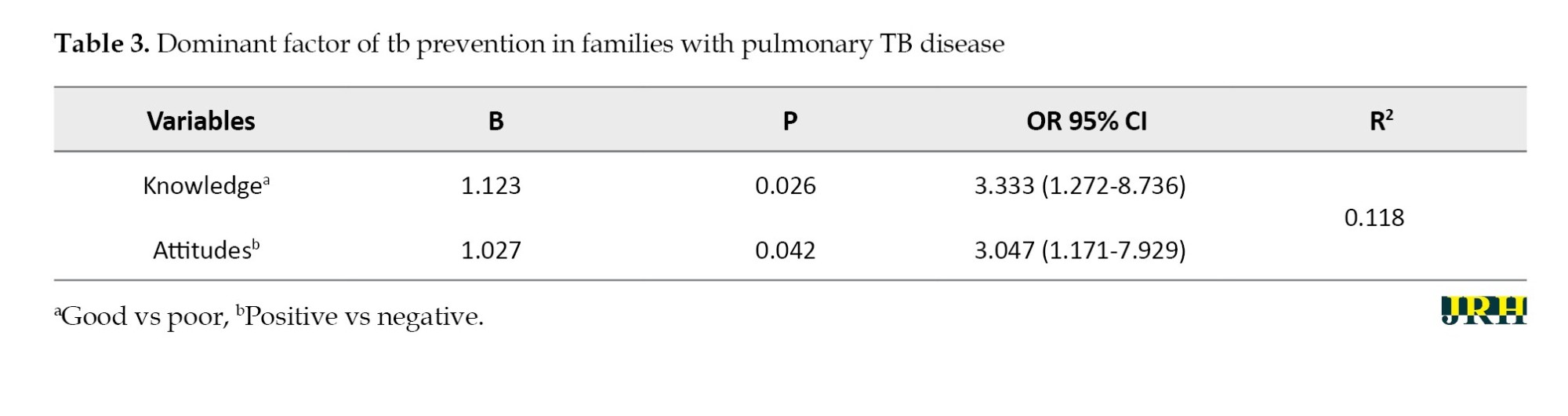
Family knowledge is a dominant factor in TB prevention compared to attitudes (OR=3.333), presented in Table 3.
Discussion
The study showed that most participants had a good level of knowledge. The study showed that families provide good information about preventing TB to patients. The same result showed that most respondents had good knowledge about preventing pulmonary TB [9, 21, 22]. Good knowledge is obtained through many factors, such as mass media, experience and environmental information from trusted people (family members, relatives, etc.) and health workers during respondents' visits to report TB [9]. There is a relationship between good family literacy and good prevention of TB in families [19, 23-25]. This research states that respondents have secondary school education or higher, so they also support preventing the transmission of this disease in the family or community. Several resource people actively asked for information from the community health center staff to learn more about preventing TB transmission. According to the study, patients can assist others to reinforce their beliefs, modify poor living habits, and acquire positive oral behaviours by discussing, preaching and learning from one another's experiences [26]. The crucial solution for TB management is providing education for patients and healthcare providers [27]. Previous studies found that knowledge can be improved by case management mode [28] and health education. Consequently, effective health education intervention for vulnerable diseases will positively impact the results [29]. Promoting knowledge will improve health quality [30]. Knowledge may be influenced by gender (males higher than females) and age group (30-39 years old) [31]. Increasing a person's age will also increase their knowledge to prevent transmission of pulmonary TB to other people [9].
Poor knowledge about TB is associated with a lower socioeconomic and educational level. Poor knowledge is also a communication challenge between patients and health workers, one of the factors of TB infection prevention and control during treatment [32]. This study revealed gaps in knowledge among TB patients [33]. On the other hand, in 2013, two hospitals were chosen for preliminary research on TB preventive knowledge, attitudes, and behaviours. A questionnaire assessing TB patients’ KAP among nurses was used to interview them. Only 20% of them were determined to be knowledgeable. Also, 80% of family members correctly replied that TB is typically connected with the lungs, and 80% claimed it is treatable and curable. However, 60% were still ignorant that the bacteria M. tuberculosis cause TB. Regarding TB treatment, 80% of family members correctly picked the completion of a 6-month course of anti-TB medicine [34].
TB patients’ attitudes significantly influence treatment adherence and outcomes. Positive attitudes towards treatment improve adherence, while negative attitudes can lead to non-adherence. Many patients trust their physicians and accept treatment, but some experience depression due to lengthy treatment durations. TB often worsens patients’ social relationships and living standards, leading to social phobia [8]. Knowledge about TB is generally good among patients, but there is a gap between knowledge and practice, particularly regarding safe sputum disposal. Health care providers should focus on enhancing patients’ understanding of TB and its treatment, addressing stigma, and creating a supportive environment to foster positive attitudes and improve adherence [20, 35]. Based on the research results, the respondents’ attitudes were positive. Judging from these data, most respondents seem to have a good view of TB prevention, and family attitudes play an important role in preventing TB transmission [36]. A positive attitude among respondents will enable them to carry out a supportive attitude in maintaining their health, including preventing TB. A similar study found that most respondents have a positive attitude towards preventing TB. In other studies, according to the findings, 40% of the five family members of TB patients have good views toward TB prevention. All of the family members felt empathy for TB patients and were eager to help and contact the patients; however, 60% of them were still concerned about the possibility of transmitting TB infection while dealing with TB patients. They also agreed that excellent communication with TB patients is essential as a family member. However, only 80% employed suitable terminology while speaking with TB patients [35]. Families already know that TB can spread through fluids from the mouth, whether coughing, sneezing, or saliva. In other words, the result is that some families have a positive attitude about preventing TB transmission and tend to accept and know about the disease [17, 37].
The research results showed that most respondents have made good efforts to prevent pulmonary TB disease. One of the preventive measures is that respondents always seek medical treatment if they have a cough for more than 2 weeks, do not spit phlegm anywhere, always wear masks when talking to TB sufferers and never isolate TB sufferers in social situations. The study found that respondents were aware that isolating people with illnesses would increase the burden on those people’s minds, apart from the fact that there was a strong brotherhood or kinship and a strong home environment. In addition, respondents can independently take precautions such as using masks and encouraging patients to wear masks [12, 38]. Human effort or behaviour is all human activities that can be directly observed (walking, singing, laughing, etc.) and those that cannot be observed by outsiders (thinking, acting, fantasizing, etc.). The ways to prevent TB include to cover their mouths for patients when coughing so that the germs that come out are not inhaled by healthy family members, not to throw phlegm anywhere, have other family members checked, eat nutritious food (enough carbohydrates, protein and vitamins), separate the patient’s use of eating and drinking utensils, pay attention to the condition of the house, good ventilation and lighting, give bacillus calmette-guérin (BCG) immunization to babies, open the windows of the house to kill TB bacteria and minimize transmission to the family, and dry the bed of the TB patient lungs [18, 37].
Based on the results, the variable with the highest odds ratio (OR) was knowledge, meaning that this variable had the greatest relationship to TB prevention efforts. This finding indicates that respondents with good family knowledge have a 3.07 times greater chance of making good prevention efforts than those with low-income family knowledge after controlling for attitude variables. Regarding these data, knowledge can directly influence prevention efforts after the family has a positive attitude [39]. It is reasonable because it will increase the family's knowledge of preventing pulmonary TB [40]. Based on this description, it can be stated that the better the knowledge of preventing pulmonary TB, the higher the respondent's attitude will have a positive influence on preventing pulmonary TB [41]. This finding aligns with the research that found a relationship between knowledge and family attitudes with the prevention of TB transmission [18-20]. The better the knowledge and the family attitudes of TB patients, the better the efforts of TB prevention [21]. Knowledge and attitudes determine family behaviour. Therefore, regarding treatment and prevention, TB disease transmission within the family plays a major role in preventing the transmission to other family members. In conclusion, TB prevention will be better if respondents have knowledge and a positive attitude from their family.
Conclusion
There was a significant association between family knowledge and attitudes in preventing pulmonary TB. Knowledge is a dominant factor compared to attitudes in TB patients.
Implications and limitations
Health care professionals must strengthen coordination and cooperation with patients’ families, especially in lessons for TB prevention. The family has strong rules to control their member from the disease. This study focused on family knowledge, attitude, and TB prevention and was conducted in only one public health centre in Indonesia. Further analysis can explore other variables that may influence TB patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Universitas Muhammadiyah Tasikmalaya, Tasikmalaya, Indonesia (Code: 4454/TMS/2023). The participants received the study’s explanation (goal and procedures) before responding to the questionnaires. They were also allowed to process and ask for clearer explanations for their doubts to facilitate informed consent. The participants were volunteers and granted the right to withdraw from the study.
Funding
This study was financially supported by Universitas Muhammadiyah Tasikmalaya, Tasikmalaya, Indonesia (Code: 271/UMTAS/2023).
Authors' contributions
Formal analysis and investigation: Miftahul Falah, Tukimin bin Sansuwito and Regidor III Dioso; Data curation, resources, visualization, validation, supervision, review, editing and project administration: Nina Pamela Sari, Lilis Lismayanti, Satriya Pranata, and Sri Wahyuni; Conceptualization, methodology and writing of the original draft: All authors.
Conflict of interest
The author declared no conflict of interest.
Acknowledgments
The authors thank Universitas Muhammadiyah Tasikmalaya, Tasikmalaya, Indonesia for supporting this study with funding.
References
Tuberculosis (TB) is an infectious disease caused by the bacteria Mycobacterium tuberculosis and remains a major health threat globally and in Indonesia. TB has become one of the oldest infectious diseases for humans and around one billion people have died [1]. The barrier that makes TB difficult to treat and eliminate is inextricably tied to Mycobacterium TB's intracellular lifestyle [2]. The immunological response to M. tuberculosis is multifaceted and complicated [3]. Cough is a central feature of pulmonary TB, as a symptom, a marker of disease activity, and a means of transmitting infection. Cough can be followed by other symptoms such as bloody sputum, bleeding cough, shortness of breath, drowsiness, loss of appetite, weight loss, anger, night sweats if not physically active, and constant shivering for over a month [4, 5]. The physical, psychological, social, and environmental aspects of TB patients are strongly connected, and these experiences greatly impact their quality of life.
TB is still a major global public health concern, accounting for a large portion of disease and mortality. Despite advancements in diagnosis and treatment, more than 10 million new cases of TB were recorded in 2020, with an anticipated 1.5 million TB-related deaths globally [6]. About 25% of people on the planet are carriers of latent TB infections, which increases their chance of ever experiencing active disease. The World Health Organization (WHO) projects that by 2021, there will be an estimated 10.6 million TB cases worldwide, an increase of almost 600000 cases [7].
The Ministry of Health in Indonesia reports the highest number of cases in West Java (105794 cases), East Java (71791 cases), Central Java (65014 cases), DKI Jakarta (41441 cases) and North Sumatra (35.035 cases). According to the Indonesian Ministry of Health, they are the five provinces with the highest number of cases. West Java is a densely populated, humid area conducive to the growth of pulmonary TB cases [8, 9]. One city in the province of West Java is Tasikmalaya, where 2837 cases of TB were reported in 2022, 1476 cases in 2021, 1041 cases in 2020 and 1435 cases in 2019. The number of TB patients appears small, yet they are quite numerous. Pulmonary TB is similar to the “ice mountain phenomenon” in that some individuals are terrified of becoming ill and getting sputum tested. Poor knowledge and negative attitudes contribute to an increase in TB patients in some areas. They remain quiet about the illness they have for a reason—a low sense of self-worth and a fear of rejection from their family and communities. The level of knowledge and negative attitudes toward TB will make it difficult to diagnose and cure the patients [10-12].
Poor knowledge about TB is a significant factor contributing to its high incidence and treatment challenges. Studies have shown that TB patients often have better knowledge than the general population. However, knowledge remains inadequate regarding transmission, symptoms and prevention. Factors associated with poor TB knowledge include older age, lower education, and lack of prior TB diagnosis. Limited knowledge can lead to delayed treatment, poor adherence, and increased risk of recurrence [13]. Misconceptions about TB transmission persist, and stigma remains a concern. Community interventions and health education programs can improve TB knowledge. Enhancing TB-related knowledge is crucial for better healthcare-seeking behavior, treatment adherence, and ultimately, TB control and eradication efforts [14].
Negative attitudes toward TB patients can significantly impact treatment adherence and outcomes. Studies have shown that health care workers, including resident doctors and nursing students, often display fear, a lack of compassion, and avoidance toward TB patients. These attitudes can reinforce societal stigma and affect patients’ treatment-seeking behavior [8]. However, positive attitudes and knowledge about TB among healthcare providers and patients are associated with better treatment adherence. Training programs for health care workers and structured patient education can improve knowledge, attitudes and treatment outcomes. Additionally, community-based directly observed treatment (CB-DOT) can be effective, but patients’ perceived attitudes toward treatment observers can influence adherence. Addressing knowledge gaps and positive attitudes is crucial for improving TB control efforts [14].
Several studies have assessed the knowledge, attitudes, and practices (KAP) of TB patients in various countries. These studies consistently found that many patients had some awareness of TB symptoms and transmission, but there were significant knowledge gaps and misconceptions. Factors associated with better TB knowledge included higher education levels, urban residence, and male gender [15]. Despite knowledge gaps, most patients demonstrated favourable attitudes towards TB treatment. However, stigma and negative community attitudes remained challenges. Educational interventions were effective in improving TB knowledge and attitudes among patients. The studies highlighted the need for enhanced TB awareness programs, particularly targeting less educated groups and addressing misconceptions, to support TB control efforts [8].
TB patients' family knowledge and positive attitudes affect TB transmission prevention efforts. Knowledge is essential to prevent the spread of TB [16]. It covers awareness of and precautions against TB transmission in households with close relatives. The patient's family is very significant to the patient. A thorough understanding of the family can stop the disease from spreading to other family members. Previous studies show that of 23 families with good knowledge, 17(73.9%) were involved in TB prevention. Also, of 21 families with positive attitudes toward TB, 16(76.2%) had good performance in preventing TB transmission. In another study, 17 families had good knowledge and effective disease prevention (85%) and of the 30 respondents with high knowledge, 70% had a role in preventing the spread of TB inside the family [17, 18]. Attitudes towards TB were generally positive, although some studies reported negative attitudes. Preventive practices were often found to be inadequate. Many studies emphasized the need for improved TB education and awareness programs to address misconceptions and enhance prevention efforts. This finding aligns with the research that found a relationship between knowledge and family attitudes with the prevention of TB transmission [18-20]. The better the knowledge and the family attitudes of TB patients, the better the efforts of TB prevention [21]. Knowledge and attitudes determine family behaviour. Therefore, regarding treatment and prevention, TB disease transmission within the family plays a major role in preventing the transmission to other family members. This study investigates the association between family attitudes and knowledge regarding preventing pulmonary TB.
Methods
Study design
The study used a quantitative design and cross-sectional approach. The variables in the study were family knowledge, attitudes and TB prevention (Figure 1). This study found a relationship between the level of knowledge and family attitudes in preventing pulmonary TB.
Samples and locations
The sample in the study was a family with pulmonary TB patients referred to the Tamansari Public Health Center, Tasikmalaya, Indonesia in 2023 (total of pulmonary TB patients: 82 patients). All families with TB patients were identified and joined the WhatsApp group. This area focuses on handling the TB program and has become one of the highest cases in Tasikmalaya. The total sampling techniques used in this study included 82 respondents. All respondents were interviewed and filled out the questionnaire.
Data collection
Institutional review board permission was received from the health office of Tasikmalaya City (register: 128). Data collection was held from January to June 2023 with the cooperation of the Tamansari Public Health Center. Data collection in this study used a questionnaire (knowledge: 25 questions, attitudes: 25 questions, and TB prevention: 24 questions). Validity and reliability tests were conducted in the study. The reliability test found the acceptable values of Cronbach α for knowledge (0.961) and attitudes (0.976). The researcher meets with respondents and conducts informed consent before completing the survey. Ensure all questions are answered and saved into a box file—all data were entered into SPSS software, version 27 for data analysis.
Study instruments
The study used a questionnaire of knowledge (1: Right and 0: False), attitudes (4: Agree, 3: Agree, 2: Disagree and 1: Totally disagree) and TB prevention (3: Always, 2: Sometimes and 1: Never) developed from a previous study [7]. Skewness value with standard error for the knowledge subscale was -1.470; for the attitude subscale, -1.432; and for the prevention subscale, -1.342 (ranging between -2 and 2). Also, the cut-off point for the knowledge subscale was 18.45 (with a score ≥18.45 indicating good knowledge); for the attitude subscale, 68.99 (with a score ≥68.99 indicating positive attitude), and for the prevention subscale, 54.28 (with a score ≥54.28 indicating good performance). The instruments passed validity (conducted for 20 respondents at Purbaratu Public Health Centre) and reliability tests. The reliability test found the acceptable values of Cronbach α for knowledge (0.961) and attitudes (0.976).
Data analysis
Data analysis in the study used univariate, bivariate, and multivariate analyses. Univariate analysis was conducted to determine characteristic knowledge (good and poor), attitudes (positive and negative) and prevention practices among respondents (cut-off point). Bivariate analysis was conducted using a chi-square test to gain insight into relationships between variables, and multivariate analysis was used in logistic regression testing to find the dominant factor. The IBM SPSS software, version 27 application was used in the study. P<0.05 was Considered significantically.
Results
A total of 82 participants completed this study. Table 1 presents demographic characteristic as follows: Gender, 42 males (51.2%) and 40 females (48.7%); age, 11-20 years, 12(14.6%), 21-30 years, 20(24.3%), 31-40 years, 25(30.4%), >40 years, 25(30.4%); education, elementary school, 30(36.5%), Junior high school, 11(13.4%), senior high school, 20(24.3%), university, 21(25.6%); marital status, married, 60(73.1%), not married, 22(26.8%).
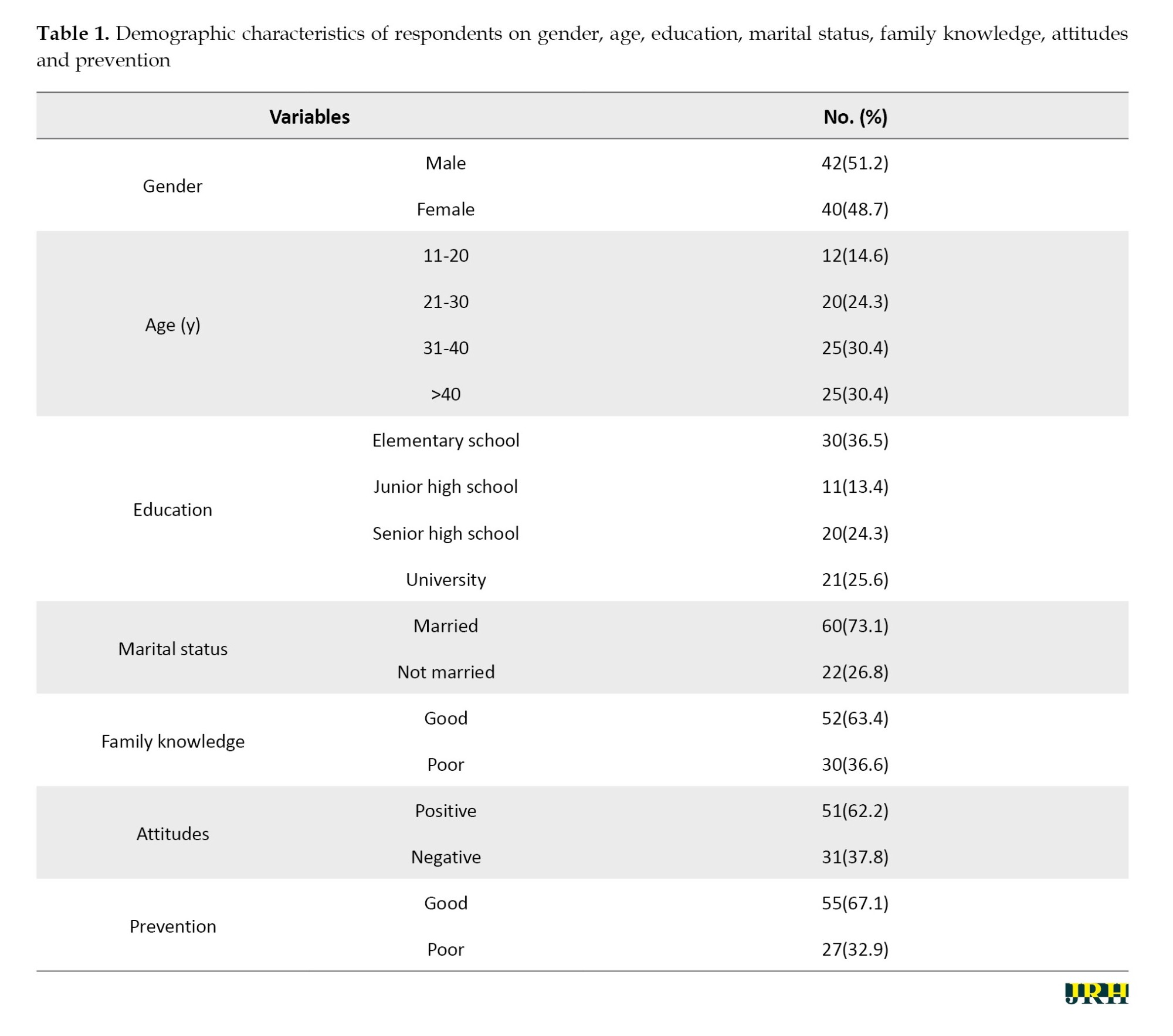
Frequency distribution of family knowledge about pulmonary TB disease shows that 52 people (63.4%) had good knowledge, and 30 people (36.6%) had poor knowledge. According to family attitudes, the data shows that 51 people (62.2%) had positive attitudes and 31 (37.8%) had negative attitudes. Based on data on TB prevention, the TB prevention of families with pulmonary TB patients was good in 55 people (67.1%) and poor in 27 people (32.9%) (Table 1).
Family knowledge and attitudes are significantly associated with TB prevention, knowledge (P=0.012) and attitudes (P=0.020) (Table 2).
Family knowledge is a dominant factor in TB prevention compared to attitudes (OR=3.333), presented in Table 3.
Discussion
The study showed that most participants had a good level of knowledge. The study showed that families provide good information about preventing TB to patients. The same result showed that most respondents had good knowledge about preventing pulmonary TB [9, 21, 22]. Good knowledge is obtained through many factors, such as mass media, experience and environmental information from trusted people (family members, relatives, etc.) and health workers during respondents' visits to report TB [9]. There is a relationship between good family literacy and good prevention of TB in families [19, 23-25]. This research states that respondents have secondary school education or higher, so they also support preventing the transmission of this disease in the family or community. Several resource people actively asked for information from the community health center staff to learn more about preventing TB transmission. According to the study, patients can assist others to reinforce their beliefs, modify poor living habits, and acquire positive oral behaviours by discussing, preaching and learning from one another's experiences [26]. The crucial solution for TB management is providing education for patients and healthcare providers [27]. Previous studies found that knowledge can be improved by case management mode [28] and health education. Consequently, effective health education intervention for vulnerable diseases will positively impact the results [29]. Promoting knowledge will improve health quality [30]. Knowledge may be influenced by gender (males higher than females) and age group (30-39 years old) [31]. Increasing a person's age will also increase their knowledge to prevent transmission of pulmonary TB to other people [9].
Poor knowledge about TB is associated with a lower socioeconomic and educational level. Poor knowledge is also a communication challenge between patients and health workers, one of the factors of TB infection prevention and control during treatment [32]. This study revealed gaps in knowledge among TB patients [33]. On the other hand, in 2013, two hospitals were chosen for preliminary research on TB preventive knowledge, attitudes, and behaviours. A questionnaire assessing TB patients’ KAP among nurses was used to interview them. Only 20% of them were determined to be knowledgeable. Also, 80% of family members correctly replied that TB is typically connected with the lungs, and 80% claimed it is treatable and curable. However, 60% were still ignorant that the bacteria M. tuberculosis cause TB. Regarding TB treatment, 80% of family members correctly picked the completion of a 6-month course of anti-TB medicine [34].
TB patients’ attitudes significantly influence treatment adherence and outcomes. Positive attitudes towards treatment improve adherence, while negative attitudes can lead to non-adherence. Many patients trust their physicians and accept treatment, but some experience depression due to lengthy treatment durations. TB often worsens patients’ social relationships and living standards, leading to social phobia [8]. Knowledge about TB is generally good among patients, but there is a gap between knowledge and practice, particularly regarding safe sputum disposal. Health care providers should focus on enhancing patients’ understanding of TB and its treatment, addressing stigma, and creating a supportive environment to foster positive attitudes and improve adherence [20, 35]. Based on the research results, the respondents’ attitudes were positive. Judging from these data, most respondents seem to have a good view of TB prevention, and family attitudes play an important role in preventing TB transmission [36]. A positive attitude among respondents will enable them to carry out a supportive attitude in maintaining their health, including preventing TB. A similar study found that most respondents have a positive attitude towards preventing TB. In other studies, according to the findings, 40% of the five family members of TB patients have good views toward TB prevention. All of the family members felt empathy for TB patients and were eager to help and contact the patients; however, 60% of them were still concerned about the possibility of transmitting TB infection while dealing with TB patients. They also agreed that excellent communication with TB patients is essential as a family member. However, only 80% employed suitable terminology while speaking with TB patients [35]. Families already know that TB can spread through fluids from the mouth, whether coughing, sneezing, or saliva. In other words, the result is that some families have a positive attitude about preventing TB transmission and tend to accept and know about the disease [17, 37].
The research results showed that most respondents have made good efforts to prevent pulmonary TB disease. One of the preventive measures is that respondents always seek medical treatment if they have a cough for more than 2 weeks, do not spit phlegm anywhere, always wear masks when talking to TB sufferers and never isolate TB sufferers in social situations. The study found that respondents were aware that isolating people with illnesses would increase the burden on those people’s minds, apart from the fact that there was a strong brotherhood or kinship and a strong home environment. In addition, respondents can independently take precautions such as using masks and encouraging patients to wear masks [12, 38]. Human effort or behaviour is all human activities that can be directly observed (walking, singing, laughing, etc.) and those that cannot be observed by outsiders (thinking, acting, fantasizing, etc.). The ways to prevent TB include to cover their mouths for patients when coughing so that the germs that come out are not inhaled by healthy family members, not to throw phlegm anywhere, have other family members checked, eat nutritious food (enough carbohydrates, protein and vitamins), separate the patient’s use of eating and drinking utensils, pay attention to the condition of the house, good ventilation and lighting, give bacillus calmette-guérin (BCG) immunization to babies, open the windows of the house to kill TB bacteria and minimize transmission to the family, and dry the bed of the TB patient lungs [18, 37].
Based on the results, the variable with the highest odds ratio (OR) was knowledge, meaning that this variable had the greatest relationship to TB prevention efforts. This finding indicates that respondents with good family knowledge have a 3.07 times greater chance of making good prevention efforts than those with low-income family knowledge after controlling for attitude variables. Regarding these data, knowledge can directly influence prevention efforts after the family has a positive attitude [39]. It is reasonable because it will increase the family's knowledge of preventing pulmonary TB [40]. Based on this description, it can be stated that the better the knowledge of preventing pulmonary TB, the higher the respondent's attitude will have a positive influence on preventing pulmonary TB [41]. This finding aligns with the research that found a relationship between knowledge and family attitudes with the prevention of TB transmission [18-20]. The better the knowledge and the family attitudes of TB patients, the better the efforts of TB prevention [21]. Knowledge and attitudes determine family behaviour. Therefore, regarding treatment and prevention, TB disease transmission within the family plays a major role in preventing the transmission to other family members. In conclusion, TB prevention will be better if respondents have knowledge and a positive attitude from their family.
Conclusion
There was a significant association between family knowledge and attitudes in preventing pulmonary TB. Knowledge is a dominant factor compared to attitudes in TB patients.
Implications and limitations
Health care professionals must strengthen coordination and cooperation with patients’ families, especially in lessons for TB prevention. The family has strong rules to control their member from the disease. This study focused on family knowledge, attitude, and TB prevention and was conducted in only one public health centre in Indonesia. Further analysis can explore other variables that may influence TB patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Universitas Muhammadiyah Tasikmalaya, Tasikmalaya, Indonesia (Code: 4454/TMS/2023). The participants received the study’s explanation (goal and procedures) before responding to the questionnaires. They were also allowed to process and ask for clearer explanations for their doubts to facilitate informed consent. The participants were volunteers and granted the right to withdraw from the study.
Funding
This study was financially supported by Universitas Muhammadiyah Tasikmalaya, Tasikmalaya, Indonesia (Code: 271/UMTAS/2023).
Authors' contributions
Formal analysis and investigation: Miftahul Falah, Tukimin bin Sansuwito and Regidor III Dioso; Data curation, resources, visualization, validation, supervision, review, editing and project administration: Nina Pamela Sari, Lilis Lismayanti, Satriya Pranata, and Sri Wahyuni; Conceptualization, methodology and writing of the original draft: All authors.
Conflict of interest
The author declared no conflict of interest.
Acknowledgments
The authors thank Universitas Muhammadiyah Tasikmalaya, Tasikmalaya, Indonesia for supporting this study with funding.
References
- Paulson T. Epidemiology: A mortal foe. Nature. 2013; 502(7470):S2-3. [DOI:10.1038/502S2a] [PMID]
- Bussi C, Gutierrez MG. Mycobacterium tuberculosis infection of host cells in space and time. FEMS Microbiology Reviews. 2019; 43(4):341-61. [DOI:10.1093/femsre/fuz006] [PMID] [PMCID]
- Flynn JL, Chan J. Immune cell interactions in tuberculosis. Cell. 2022; 185(25):4682-702. [DOI:10.1016/j.cell.2022.10.025] [PMID]
- Wu S, Litvinjenko S, Magwood O, Wei X. Defining tuberculosis vulnerability based on an adapted social determinants of health framework: A narrative review. Global Public Health. 2023; 18(1):2221729. [DOI:10.1080/17441692.2023.2221729] [PMID] [PMCID]
- Musaazi J, Sekaggya-Wiltshire C, Okoboi S, Zawedde-Muyanja S, Senkoro M, Kalema N, et al. Increased uptake of tuberculosis preventive therapy (TPT) among people living with HIV following the 100-days accelerated campaign: A retrospective review of routinely collected data at six urban public health facilities in Uganda. Plos One. 2023; 18(2):e0268935. [DOI:10.1371/journal.pone.0268935] [PMID] [PMCID]
- Goletti D, Pisapia R, Fusco FM, Aiello A, Van Crevel R. Epidemiology, pathogenesis, clinical presentation and management of TB in patients with HIV and diabetes. The International Journal of Tuberculosis and Lung Disease. 2023; 27(4):284-90. [DOI:10.5588/ijtld.22.0685] [PMID] [PMCID]
- Sibua S, Tumiwa FF, Pondaa A. Pemberian pendidikan kesehatan untuk meningkatkan pengetahuan penderita tuberkulosis. Watson Journal Of Nursing. 2023; 1(2):11-5. [Link]
- Aisah S, Al Jihad MN, Pebriani A, Pranata S, Soesanto E. Bibliometric analysis of nursing interventions to improve adherence to treatment among patients with tuberculosis. Africa Journal of Nursing and Midwifery. 2024; 26(1):19. [DOI:10.25159/2520-5293/14557]
- Andriani D, Sukardin S. Pengetahuan dan sikap keluarga dengan pencegahan penularan penyakit tuberculosis (TBC) di wilayah kerja puskesmas penana’e kota bima. Jurnal Ilmiah Ilmu Keperawatan Indonesia. 2020; 10(3):72-80. [DOI:10.33221/jiiki.v10i03.589]
- Goroh MMD, van den Boogaard CHA, Lukman KA, Lowbridge C, Juin WK, William T, et al. Factors affecting implementation of tuberculosis contact investigation and tuberculosis preventive therapy among children in Sabah, East Malaysia: A qualitative study. Plos One. 2023; 18(5):e0285534. [DOI:10.1371/journal.pone.0285534] [PMID] [PMCID]
- Bozzani FM, McCreesh N, Diaconu K, Govender I, White RG, Kielmann K, et al. Cost-effectiveness of tuberculosis infection prevention and control interventions in South African clinics: a model-based economic evaluation informed by complexity science methods. BMJ Global Health. 2023 Feb;8(2):e010306. [DOI:10.1136/bmjgh-2022-010306] [PMID] [PMCID]
- Shringarpure K, Gurumurthy M, Sagili KD, Taylor M, Garner P, Tonsing J, et al. Patient adherence to tuberculosis treatment in the Indian subcontinent: Systematic review and meta-synthesis of qualitative research. BMJ Open. 2023; 13(5):e063926. [DOI:10.1136/bmjopen-2022-063926] [PMID] [PMCID]
- Farrah Fahdhienie, Tiara Mairani, Phossy Vionica Ramadhana, et al. Analisis Spasial Kejadian Tuberkulosis di Kota Banda Aceh. Media Publikasi Promosi Kesehatan Indonesia. 2023; 6(8):1599-607. [DOI:10.56338/mppki.v6i8.3536]
- Dewi AAK, Irnawati. The relationship between pulmonary tuberculosis knowledge and anxiety among pulmonary tuberculosis patients at wiradesa community health center. Paper presented at: The 16th University Research Colloqium. 2022. 1 January 2022; Bandung, Indonesia. [Link]
- Patwal R, Sachdeva A, Bhaskarapillai B, Arasappa R, Muliyala KP, Desai G. Prevalence of suicidal ideations and suicide attempts in patients with tuberculosis: A systematic review and meta-analysis. Journal of Psychosomatic Research. 2023; 167:111171. [DOI:10.1016/j.jpsychores.2023.111171] [PMID]
- Sazali MF, Rahim SSSA, Mohammad AH, Kadir F, Payus AO, Avoi R, et al. Improving tuberculosis medication adherence: The potential of integrating digital technology and health belief model. Tuberculosis and Respiratory Diseases. 2023; 86(2):82-93. [DOI:10.4046/trd.2022.0148] [PMID] [PMCID]
- Salles I, Travassos P, Spener-Gomes R, Loch AP, Saraceni V, Lauria L, et al. Contextualizing and optimizing novel strategies to improve the latent TB continuum of care: Insights from people living with HIV and health care providers in Brazil. PLOS Global Public Health. 2023; 3(1):e0001251. [DOI:10.1371/journal.pgph.0001251] [PMID] [PMCID]
- Nagarajan K, Muniyandi M, Sellappan S, Karunanidhi S, Senthilkumar K, Palani B, et al. A study on tuberculosis disease disclosure patterns and its associated factors: Findings from a prospective observational study in Chennai. Plos One. 2023; 18(1):e0280812. [DOI:10.1371/journal.pone.0280812] [PMID] [PMCID]
- Harding R, Snyman L, Ostgathe C, Odell S, Gwyther L. The ethical imperative to relieve suffering for people with tuberculosis by ensuring access to palliative care. The international Journal of Tuberculosis and Lung Disease. 2020; 24(5):3-8. [DOI:10.5588/ijtld.18.0240] [PMID]
- Palacios CF, Hough MA, Shrestha R, Moll AP, Kompala T, Andrews L, et al. Perceived stigma related to TB preventive therapy. The International Journal of Tuberculosis and Lung Disease. 2023; 27(3):209-214. [DOI:10.5588/ijtld.22.0570] [PMID]
- Setiya Sulistiyana C, Susanti S. Hubungan pengetahuan dan sikap keluarga pasien tuberkulosis paru dengan upaya pencegahan penyakit tuberkulosis paru di wilayah kerja puskesmas kesunean dan pegambiran kota cirebon. Tunas Medika Jurnal Kedokteran & Kesehatan. 2015; 2(3):1-10. [Link]
- Gunawan E. Gambaran pengetahuan keluarga tentang cara pencegahan penularan penyakit tb paru di wilayah kerja puskesmas baregbeg kecamatan baregbeg Tahun 2018. Jurnal Keperawatan Galuh. 2020; 2(2):61. [DOI:10.25157/jkg.v2i2.4536]
- Lukitaningtyas D, Hidayah N, Mahendra R. Pengetahuan Keluarga Berhubungan Dengan Upaya Keluarga Dalam Pencegahan Penularan Tb Paru. Jurnal Penelitian Perawat Profesional. 2023; 5(1):423-6. [DOI:10.37287/jppp.v5i1.1453]
- Cenzi CM, Marziale MHP. Mobile application development structured in self-care for occupational post-exposure prophylaxis to biological material. Revista Brasileira de Enfermagem. 2020; 73(suppl 5):e20190721. [DOI:10.1590/0034-7167-2019-0721] [PMID]
- Wulandari DA. Hubungan pengetahuan pencegahan penyakit tbc dengan perilaku pencegahan tbc pada kepala keluarga di padukuhan nologaten, kecamatan Depok, Kabupaten Sleman, Yogyakarta. Jurnal Kesehatan Masyarakat. 2018; 11(1):973-81. [DOI:10.47317/jkm.v11i1.74]
- Nibali, L., Gkranias, N., Mainas, G., & Di Pino, A. Periodontitis and implant complications in diabetes. Periodontology 2000. 2022; 90(1): 88-105. [DOI: 10.1111/prd.12451] [PMID]
- Chang SH, Cataldo JK. A systematic review of global cultural variations in knowledge, attitudes and health responses to tuberculosis stigma. The International Journal of Tuberculosis and Lung Disease. 2014; 18(2):168-73. [DOI:10.5588/ijtld.13.0181] [PMID]
- Li Y, Wang Y, Wang G, Wang Y, Tian Y, Zhu S, et al. Effectiveness of a case management model in newly treated smear-positive pulmonary tuberculosis patients. The Journal of Infection in Developing Countries. 2021; 15(11):1670-6. [DOI:10.3855/jidc.14935]
- Bisallah CI, Rampal L, Lye MS, Mohd Sidik S, Ibrahim N, Iliyasu Z, et al. Effectiveness of health education intervention in improving knowledge, attitude, and practices regarding Tuberculosis among HIV patients in General Hospital Minna, Nigeria - A randomized control trial. Plos One. 2018; 13(2):e0192276. [DOI:10.1371/journal.pone.0192276] [PMID] [PMCID]
- Wang Y, Li DX, Wang YL, Tao W, Wang JT, Zhao YM, et al. Influence of small-group experiential learning of integrated traditional Chinese and Western medicine on the oral health knowledge, beliefs, and behaviors of elderly patients with diabetes. Revista da Associacao Medica Brasileira. 2022; 68(2):217-21. [DOI:10.1590/1806-9282.20210833] [PMID]
- Gautam N, Karki RR, Khanam R. Knowledge on tuberculosis and utilization of DOTS service by tuberculosis patients in Lalitpur District, Nepal. Plos One. 2021; 16(1):e0245686. [DOI:10.1371/journal.pone.0245686] [PMID] [PMCID]
- Zwama G, Diaconu K, Voce AS, O'May F, Grant AD, Kielmann K. Health system influences on the implementation of tuberculosis infection prevention and control at health facilities in low-income and middle-income countries: A scoping review. BMJ Global Health. 2021; 6(5):e004735. [DOI:10.1136/bmjgh-2020-004735] [PMID] [PMCID]
- Craciun OM, Torres MDR, Llanes AB, Romay-Barja M. Tuberculosis knowledge, attitudes, and practice in middle- and low-income countries: A systematic review. Journal of Tropical Medicine. 2023; 2023:1014666. [DOI:10.1155/2023/1014666] [PMID] [PMCID]
- Farhanah Abd Wahab FA, Sarimah Abdullah SA, Jafri Malin Abdullah JM, Hasnan Jaafar HJ, Siti Suraiya MN, Wan Mohd ZW, et al. Updates on knowledge, attitude and preventive practices on tuberculosis among healthcare workers. The Malaysian Journal of Medical Sciences. 2016; 23(6):25-34. [Link]
- Palomares Velosa JE, Figueroa Gómez JE, Rojas Zúñiga CN, Díaz G, Ferro BE, Davis JL, et al. Exploring stakeholders perspectives on TB contact investigation in Cali, Colombia: A qualitative study. Frontiers in Public Health. 2023; 11:1204862. [DOI:10.3389/fpubh.2023.1204862] [PMID] [PMCID]
- Ramadany S, Djaharuddin I, Zainuddin AA, Aras I, Madjid I, Delima AA. Knowledge and attitudes of patients’ family toward efforts in preventing tuberculosis in Tamalanrea Health Center. Enfermería Clínica. 2020; 30:36-9. [DOI: 10.1016/j.enfcli.2020.06.010]
- Seloma NM, Makgatho ME, Maimela E. Evaluation of drug-resistant tuberculosis treatment outcome in Limpopo province, South Africa. African Journal of Primary Health Care & Family Medicine. 2023; 15(1):e1-7. [DOI:10.4102/phcfm.v15i1.3764] [PMID] [PMCID]
- Sandoval M, Mtetwa G, Devezin T, Vambe D, Sibanda J, Dube GS, et al. Community-based tuberculosis contact management: Caregiver experience and factors promoting adherence to preventive therapy. PLOS Global Public Health. 2023; 3(7):e0001920. [DOI:10.1371/journal.pgph.0001920] [PMID] [PMCID]
- Weraman P, Ndoen HI. Relationship of knowledge and attitude to pulmonary tb prevention behavior in home contact in the working area of puskesmas batuputih in 2020. Journal of Health and Behavioral Science. 2021; 3(4):470-80. [DOI:10.35508/jhbs.v3i4.4363]
- Siregar RR, Sari E, Gultom DM, Ahmadi H. The relationship between knowledge and attitude of pulmonary TB patients on the prevention of pulmonary TB disease transmission at puskesmas padangmatinggi. Science Midwifery. 2022; 10(3):2110-4. [DOI:10.35335/midwifery.v10i3.621]
- Madebo M, Balta B, Daka D. Knowledge, attitude and practice on prevention and control of pulmonary tuberculosis index cases family in Shebedino District, Sidama Region, Ethiopia. Heliyon. 2023; 9(10):e20565. [DOI:10.1016/j.heliyon.2023.e20565] [PMID] [PMCID]
Type of Study: Orginal Article |
Subject:
● Disease Control
Received: 2024/08/1 | Accepted: 2025/01/29 | Published: 2025/07/1
Received: 2024/08/1 | Accepted: 2025/01/29 | Published: 2025/07/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






