Volume 15, Issue 2 (March & April 2025)
J Research Health 2025, 15(2): 135-144 |
Back to browse issues page
Ethics code: 118-IRB/PN-FoN-UPH/XI/2021
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Theresia T, Togatorop L B, Panjaitan T, Pranata S. Cadres’ Experience Regarding Tuberculosis Implementation During COVID-19: Differences and Challenges: A Qualitative Study. J Research Health 2025; 15 (2) :135-144
URL: http://jrh.gmu.ac.ir/article-1-2598-en.html
URL: http://jrh.gmu.ac.ir/article-1-2598-en.html
1- Department of Nursing, Faculty of Medicine, Universitas Pendidikan Ganesha, Bali, Indonesia. , theresia.theresia@undiksha.ac.id
2- Department of Nursing, Faculty of Health Sciences, Universitas Pembangunan Nasional Veteran Jakarta, Indonesia.
3- Department of Nursing, Faculty of Nursing, Universitas Pelita Harapan, Banten, Indonesia.
4- Department of Nursing, Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Indonesia.
2- Department of Nursing, Faculty of Health Sciences, Universitas Pembangunan Nasional Veteran Jakarta, Indonesia.
3- Department of Nursing, Faculty of Nursing, Universitas Pelita Harapan, Banten, Indonesia.
4- Department of Nursing, Faculty of Nursing and Health Sciences, Universitas Muhammadiyah Semarang, Semarang, Indonesia.
Full-Text [PDF 886 kb]
(228 Downloads)
| Abstract (HTML) (939 Views)
Full-Text: (215 Views)
Introduction
Tuberculosis (TB) is an infectious disease caused by bacterial contamination that is a global concern and a global emergency because of the high infection and death rates [1, 2]. The prevalence of TB cases continues to increase globally, with countries that had a high burden of TB in 2017 accounting for 87% of all cases reported worldwide. The countries contributing two-thirds of the global total are India (27%), China (9%), Indonesia (8%), Philippines (6%), Pakistan (5%), Nigeria (4%), Bangladesh (4%) and South Africa (3%).2 TB as an “old” invented infection is still a communicable disease in Indonesia [3-5].
The 2014 national tuberculosis control guidelines state that the government’s efforts to achieve success rates include health promotion about TB for families and communities. In addition, efforts to control risk factors b involve administering BCG injections as part of the strategy (find and get cured completely/temukan obati sampai sembuh) and providing logistics of Anti-TB drugs (obat anti TB). Successful TB treatment can be achieved by implementing the national tuberculosis control strategy [6, 7].
The rules that strengthen national strategies and guidelines for eradicating TB are outlined in presidential decree No. 67 of 2021, which emphasizes the role of cadres and the community in the national tuberculosis control program [3, 8]. Efforts to increase the role of these cadres will increase the effectiveness of the program implementation based on the district area (district-based public-private mix), such as improving patient independence in carrying out TB treatment and strengthening TB program management [9].
The COVID-19 pandemic substantially hindered the implementation of many communicable disease programs in the community [10-12]. Existing research regarding TB program implementation in Indonesia is quite limited. A previous qualitative study in Indonesia found that health cadres play a substantial role in supporting TB patients and their families, but it did not specifically address whether the COVID-19 pandemic affected this support. Another Indonesian quantitative study examined healthcare professionals in the context of private healthcare facilities regarding TB diagnosis during the COVID-19 pandemic [9, 13]. To our knowledge, there are few studies focused on exploring the experiences of health cadres during the implementation of TB programs in the COVID-19 era. As the participants were primarily members of the community, in which they live, this study approached their experiences through a qualitative design. This method was chosen due to the limited previous studies that could provide a baseline for this issue [14] Therefore, this study aimed to gain an understanding of the experience of community health cadres while implementing TB programs during COVID-19 and to comprehend what they perceived as differences between the period before COVID-19 and during COVID-19.
Methods
Samples and locations
This study was conducted in one sub-recipient community in Lampung, Indonesia, which focuses on managing the TB program. Inisiatif Lampung Sehat (ILS) has a well-equipped organization and is one of the community sub-recipients providing support for the TB program for the Province of Lampung. Coordination is managed through the Provincial Coordinator, while project officers oversee each district/city, where all cadres work within the sub-district health centers. Case managers coordinate patient support for multi-drug resistant TB (MDR TB) patients. The total number of participants was 26, including case managers, project officers, patient supporters, and cadres.
Design
This study used an interpretive phenomenological approach to understand the experiences of health cadres, specifically regarding TB program implementation (case detection and medication support). This approach allowed us to capture both positive and negative perceived experiences. This study’s objectives were to explore the experience of community health cadres while implementing the TB program during COVID-19 and to comprehend what they perceived as differences between the periods before and during COVID-19.
Data collection
Data collection was done in May 2021 in collaboration with a non-government organization, the sub-recipient community, which focuses on TB management. Data were collected using a recorder and field notes as resources. Each in-depth interview lasted between 45 and 60 minutes.
Instruments
The instrument used consisted of five semi-structured interview guidelines, with five questions serving as the foundational inquiries. 1) What differences were felt in mentoring patients before and during COVID-19 (this included case finding and the investigation of contacts: Household contacts and non-household contacts, as well as community and surrounding environments); 2), What actions were taken that differed before and during COVID-19 ? 3) How does it feel to supervise or assist TB treatment patients during the COVID-19 pandemic? 4) What obstacles/difficulties/challenges did you face in providing support to TB patients? 5) What are the hopes of cadres in facilitating patient support?
Data analysis
The audio recordings were transcribed verbatim by all researchers who conducted each in-depth interview using Microsoft Word. Participants were not identified and were coded in the transcripts to ensure anonymity. The transcripts were subsequently checked by two other researchers to enhance accuracy. We used thematic analysis with the following steps: Transcription, familiarization with the data, selection of quotations, selection of keywords, coding and theme development [15]. Data were analyzed in the form of themes by identifying similarities and differences in data in the interview data, which were then grouped into broader categories of meaning that were more abstract and comprehensive.
Results
All participants were from one sub-recipient community that was established for the TB implementation program. The sociodemographic findings are summarized in Table 1.
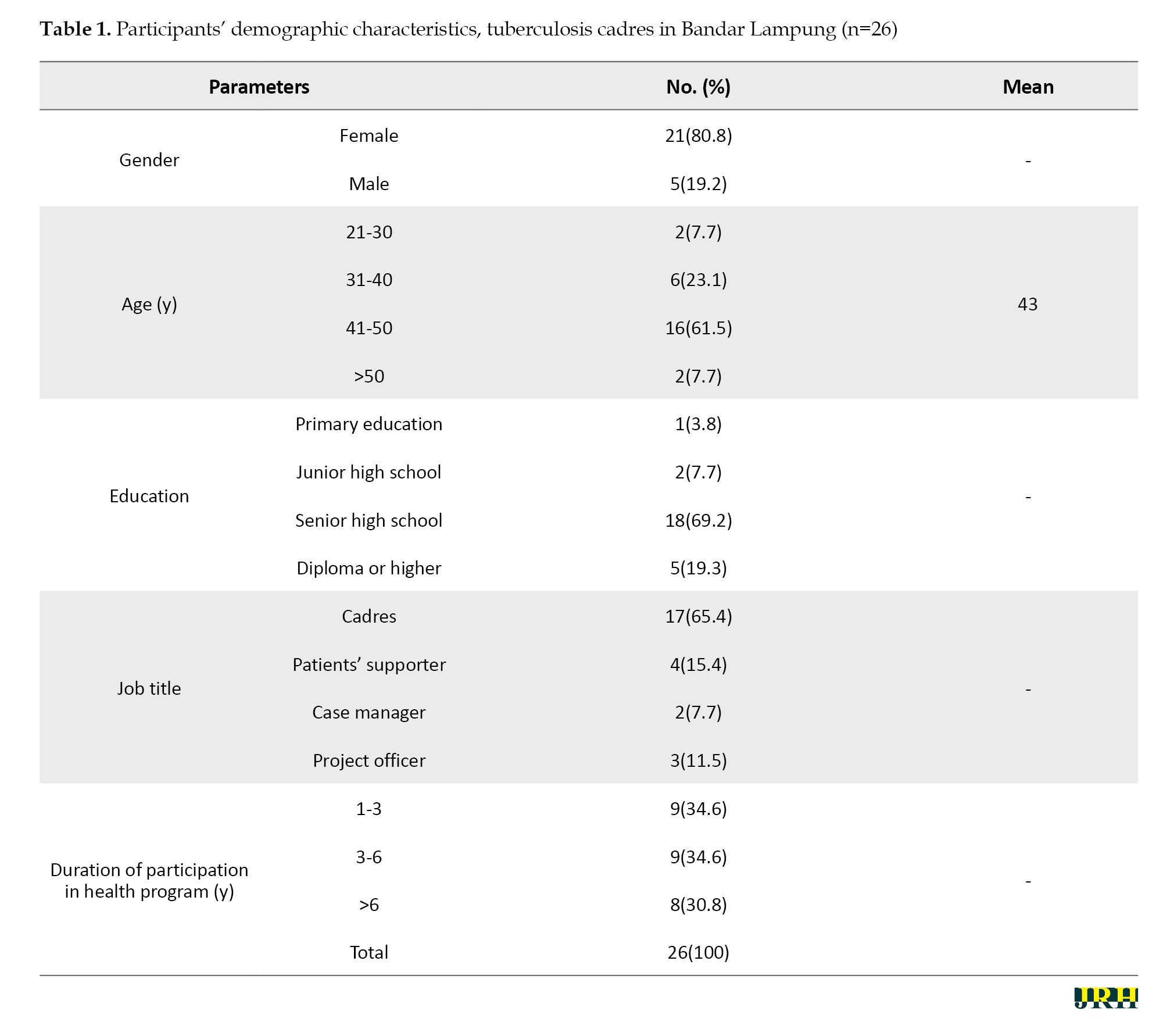
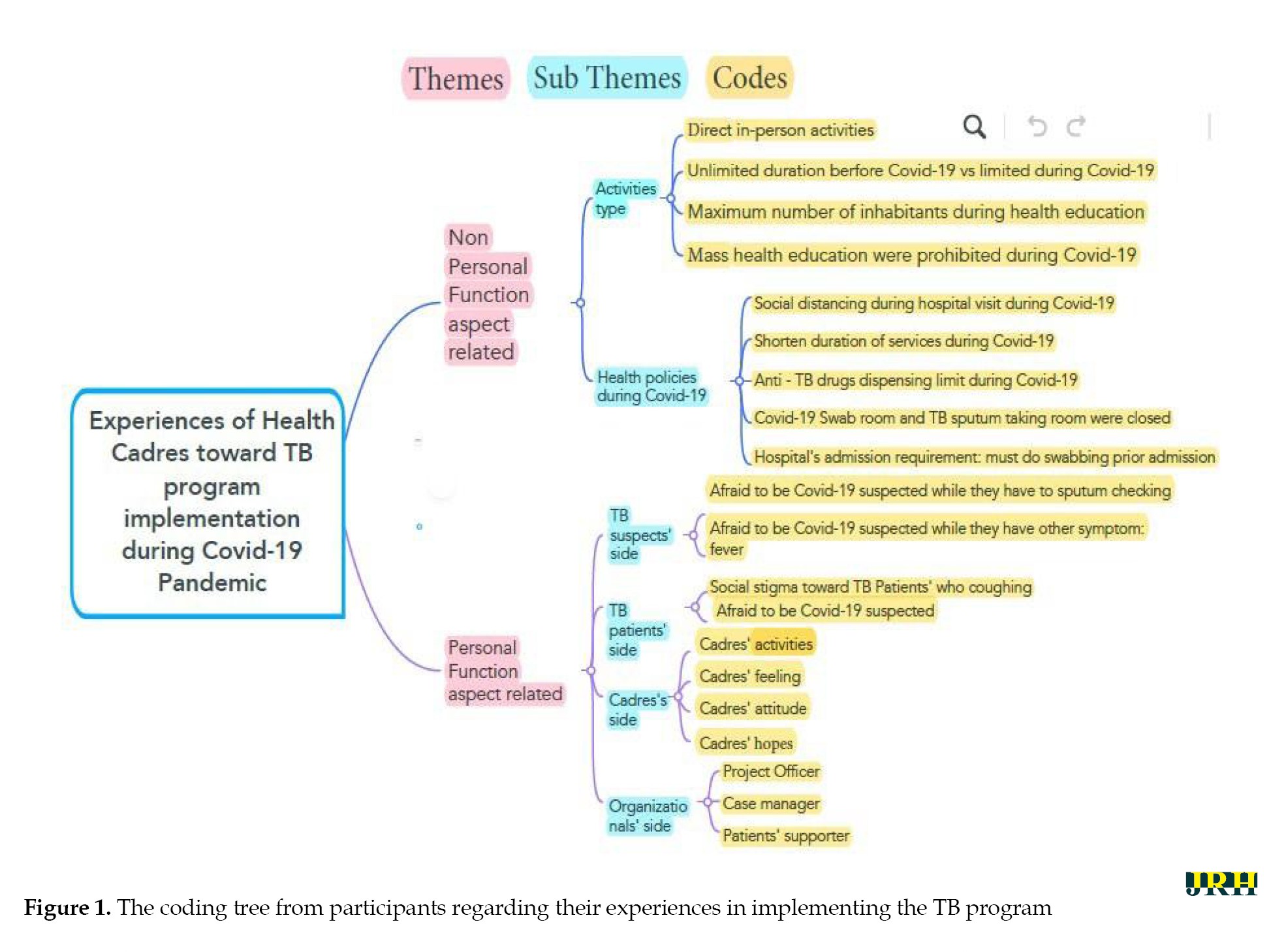
The themes found were described in Figure 1. A total of 26 informants contributed to this study. Most of the participants were cadres (65.4%). The majority of participants were female and aged 41 to 50 years. Moreover, most participants were senior high school graduates, with an average age of 43 years. All participants were from three districts: Pesawaran, Pringsewu, and South Lampung, as well as one city, Bandar Lampung.
Participants’ experiences regarding TB implementation varied before and during the COVID-19 pandemic era. This study highlights the COVID-19 period from its onset in 2020 until the end of 2021 when COVID-19 cases increased and social distancing measures were implemented in Indonesia.
Two themes emerged from the participant’s narratives: The non-personal function aspects, which classified experiences based on the types of activities and health policies implemented and the personal functional aspects, which were derived from the individuals involved in the participants’ experiences, such as TB suspects, TB patients, the cadres themselves and the organizations.
Non-personal function aspect
Participants described their experiences as being mostly stressful due to their activities and the health policies that were implemented during COVID-19.
1) The types of activities emphasized the differences between before and during COVID-19, highlighting the contrast between the two eras. Participants’ experiences regarding the types of activities include:
a. Indirect vs phone communication
“This pandemic has been very, very different, very far away. We can’t meet face to face, we can only communicate by phone” (P9-cadre). “Also, sometimes patients and companions only hear voices... We used to meet in person” (P6- patients supporter). “...it was mostly virtual assistance” (P2_case manager).
b. Unlimited vs limited
“Before COVID-19, we used to visit without being restricted. For example, during contact investigations, we were free. But after COVID-19, our access was limited” (P 12-cadre). “So that’s it, we still go to the field. COVID-19 restricts us from going out, right? So, if every medicine is taken, the cadre takes it from the health center and delivers it to patients” (P11-cadre).
c. Maximum number of participants in health education
“Before COVID-19, they would come in droves. We had up to 40 people” (P10-cadre). “During COVID-19, the sessions were not held as frequently, so there were fewer attendees. We also counseled only a few suspects. Additionally, some mosques were closed” (P13- cadre).
d. Prohibition of mass health education
“But during COVID-19, indeed we as cadres are not allowed to go out. We are not allowed to go out even for counseling or to visit patients” (P11-cadre). “Before COVID-19, we could gather people for a contact investigation. During COVID-19, we want to gather people, it’s difficult, we can’t (P8-cadre).
2) Health policies during COVID-19
a. Social distancing during hospital visits during COVID-1. “As much as possible, there should be no accumulation in the hospital” (P6-project officer).
b. Shortening the duration of services
“During COVID, health center services were limited, operating from 9 AM to 12 PM and then it was closed. The examination times were constrained; for TB, it was only on Tuesdays and Thursdays” (P8-cadre).
c. Restrictions on the distribution of anti-TB drugs
“During COVID-19, it was allowed to dispense anti-TB drugs for one-month supplies” (P12-cadre).
d. The COVID-19 Swab room and TB sputum collection room were closed. “The TB outpatient room is the same as the one for checking people who have COVID-19, it’s closed” (P12-cadre).
e. Hospital’s admission requirement: Swabbing before admission
“Since COVID, the hospital has been very strict when we must visit our patients. We have to be careful” (P5-Patients’ supporter). “When the patient condition worsens, they must go to the emergency room and undergo a PCR swab, which causes patients to choose not to go to the hospital because of the complicated admission procedure” (P15- Patients’ supporter).
Personal function aspects
This study gathered experiences from the whole sub-recipient community organization. Therefore, their experiences could be classified based on both the participants’ experiences and their perceptions of TB suspects and TB patients with whom they interacted.
1. TB suspects’ perspective
a. Afraid of being suspected of having COVID-19 while needing to undergo sputum testing. “Many inhabitants were afraid of being suspected of having COVID-19 during those times. They rarely intended to undergo swab testing. ‘Ah, I’m afraid; I’m afraid of being suspected of having COVID-19,’” (cadre imitating how the inhabitants spoke)” (P8-cadre). “During the COVID-19 pandemic, many people were afraid. So, I’m afraid (cadre imitating the way inhabitants spoke). I’m going to think it’s COVID-19 ; I don’t want them to pierce my nose, I hate it” (P13-cadre).
b. Afraid of being suspected of having COVID-19 while experiencing other symptoms, such as fever
“They did not want to get checked; they were afraid. They didn’t want to check their sputum; they felt feverish and didn’t want to go to the health center either.” (P9- cadre)
2. TB patients’ perspective
a. Social stigma toward TB patients who cough
“Society’s stigma towards patients who have a slight cough is getting worse because our patients are considered to have COVID-19, because the symptoms of TB and COVID are the same, such as coughing” (P3-project officer). “Especially when they were admitted to the hospital, they were afraid, and the stigma from other people was negative” (P3-project officer).
b. Afraid of being doubly diagnosed with COVID-19
“Our patients, if they have TB, are afraid that they will also be considered to have COVID-19 ” (P3-project officer).
3. Cadres’ perspective
a. Cadres’ feelings
“In the past, before the pandemic, we just relaxed and enjoyed ourselves. Now, there are many obstacles because, for example, when we visit a patient, we have to be extremely cautious” (P14-cadre). “There is still fear inside. But Alhamdulillah, we have been safe” (P12-cadre). Because we are the ones who visit the patient’s home, sometimes we feel… not welcomed—like we are being rejected” (P14-cadre).
b. Cadres’ attitude
“Doing health education was prohibited during the pandemic. But because we have a cadre identity, we continue to push forward” (P11-cadre). “We are already wearing standard masks, so sometimes what we are afraid of is our family, especially when we are not affected and not feeling well” (P8-cadre). I think I have a moral responsibility. The first time I became a cadre, I met a patient who had TB, and that’s why he left his wife. I got the news that the person was treated and died” (P12-cadre).
c. Cadres’ hopes
“Those who are infected with TB are not just from the upper-class economic group. I hope for continuous collaboration between our sub-recipient community and global financial supporters” (P14-cadre). “The hope is that, as cadres, especially in this sub-district, our society gets more knowledge and becomes more aware that being healthy is very important. So, hopefully, in this area, TB patients who are still on treatment could finish their medication and be free of TB” (P9-cadre). “The hope is that we, as cadres, will also receive concern and care. So, when we want to go to the field, we feel afraid; for example, regarding masks, yes, we need facilities” (P7-cadre).
2. Organizational officers’ perspectives
a. Project officer
“I feel afraid when carrying out assistance because of the issues and dangers associated with COVID-19 itself” (P4-project officer). “We hope that financial support in mentoring will be increased” (P3-project officer).
b. Case manager
“It’s the same but that, it’s just our hard work if our role is heavier. Our role is heavier in being aware of TB and being aware of the COVID-19 ” (P2-case manager). “It’s the same, but it’s just our hard work; our role is heavier. Our responsibility is to raise awareness about TB and COVID-19 ” (P2-case manager).
“I still hope we could go back to recovery situation like before COVID-19. MDR TB patients can sit together, and they commit to taking the medicine at the hospital in front of us” (P1-case manager).
a. “We hope that if this could be published, our statement and our stories would be beneficial for the society and improve the quality of the TB implementation program” (P1-case manager).
b. Patients’ supporter
“But alhamdulillah, I’m happy to fulfill my role as a patients’ supporter” (P6-patients’ supporter). “I feel proud. I am doing this not merely for money or material gain. I purely want to help others” (P5-patients’ supporter). “Yes, I hope my patient recovers; that’s all, I hope the treatment is finished” (P6-patients’ supporter).
Discussion
This study showed the crucial role of sub-province community organizations that coordinate implementation efforts alongside referral hospitals and health centers in combating TB during the COVID-19 pandemic. This context of this study is in line with an integrative review from several countries (India, Bangladesh, Pakistan, Sierra Leone, Kenya and Ethiopia) that emphasized the importance of community workers in areas, such as surveillance, and community education [12, 16, 17].
This study revealed that the connection of cadres to the communities they belong to was the primary rationale for the emergence of activity types related to non-personal functions and close relationships with community members. A previous Nigerian study showed that health extension workers, referred to as cadres in this study, are often undervalued in society and play a vital role in bridging the gap between the community and the healthcare systems [18]. This study, along with previous research, agrees that cadres played a significant role during the pandemic in assisting healthcare facilities with managing pandemics and other communicable disease burdens, such as TB [19, 20].
This study found that some cadres were eager to visit TB patients’ homes during the COVID-19 pandemic, even though the locations were quite distant. Previous quantitative studies conducted in East Nusa Tenggara Province, Indonesia, reported different results regarding geographical coverage [3, 21, 22]. These studies showed that Indonesia is an archipelago with many islands, each having varying levels of infrastructure and healthcare facilities. This study was done in a district near the city. Another difference is that the previous studies were conducted before the COVID-19 pandemic (January 2019), while this study was conducted during COVID-19 (May 2022) [23–26].
This study found that health cadres’ feelings, attitudes, and commitment to implementing TB initiatives during the COVID-19 pandemic were very robust, despite all the difficulties during the pandemic. Yet, a previous study before the COVID-19 pandemic in Palu City found that there is a positive correlation between cadres’ motivation and active case-finding activities [22]. Although both studies were set in a city near a coastal area, they utilized different quantitative and qualitative approaches. Some studies revealed that incentives and training can increase the motivation of health cadres [27, 28]. This study found that sub-recipient community organizations provided supportive coordination for the health cadres. Their involvement in TB implementation and motivation to ensure patients complete their medications were evident [29–31].
Stigma toward TB patients during the COVID-19 pandemic was also an important finding in this study. This issue is quite complex, as TB and COVID-19 are respiratory illnesses, with similar symptoms, such as coughing and fever. Cadres reported that it was challenging to persuade suspected TB patients to undergo sputum examinations during the COVID-19 pandemic [1, 32, 33]. Overcoming the stigma associated with TB, especially lessons learned during the COVID-19 pandemic, requires a multi-level approach that includes education, increasing awareness, patient-centered care, and community involvement [27].
This study revealed that cadres are striving to do their role in the TB implementation program because they recognize their importance to the community they serve [34, 35]. This finding affirms a previous study that indicated cadres maintain close relationships with the community and assist in bridging the gap between the community and healthcare systems [36, 37]. Cadres expressed the need for facilitation during the pandemic, such as personal protective equipment (PPE), which aligns with other previous studies [38, 39].
This study gathered data from participants who have worked for years in TB programs within the community, allowing for a detailed and in-depth examination of their experiences. The study observed participants doing some coordination meetings; however, the data collected may present a limitation that could affect the participants’ responses [40].
Conclusion
Sub-recipient community organizations that coordinate implementation along with referral hospitals and health centers play a vital role in dealing with TB during the COVID-19 pandemic. Health cadres were significant contributors during the pandemic, assisting healthcare facilities in managing the pandemic and other communicable disease burdens, such as TB. Healthcare professionals must strengthen coordination and cooperation with health cadres, especially considering the lessons learned during COVID-19. Health cadres are passionate and make every effort to serve the communities from which they originate. This qualitative study revealed that health cadres need support, including protective equipment, during outbreaks of communicable diseases. This study was conducted in only one city in Indonesia using simple interview guidelines. It would be beneficial to conduct a quantitative study to measure the health cadre’s abilities based on their experiences during COVID-19.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the research and community services, Universitas Pelita Harapan, Banten, Indonesia (Code: 118-IRB/PN-FoN-UPH/XI/2021). Each participant received the study’s explanation (study’s goal and procedures) before in-depth interviews began. Participants were also given the opportunity to ask for clearer explanations of their doubts to facilitate informed consent. Participation was voluntary, and participants had the right to withdraw from the study at any time. They were reassured that all statements shared were not considered right or wrong but were purely reflections of their personal experiences.
Funding
This study was financially supported by the Research and Community Service at Universitas Pelita Harapan, Banten, Indonesia.
Authors' contributions
Investigation: Theresia Theresia; Project administration, data collection, resources, visualization, and writing: Tirolyn Panjaitan; Validation, supervision and funding: Theresia Theresia, Lina Berliana Togatorop and Satriya Pranata; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Universitas Pelita Harapan, Banten, Indonesia for its funding support and Inisiatif Lampung Sehat for serving as our study partner.
References
Tuberculosis (TB) is an infectious disease caused by bacterial contamination that is a global concern and a global emergency because of the high infection and death rates [1, 2]. The prevalence of TB cases continues to increase globally, with countries that had a high burden of TB in 2017 accounting for 87% of all cases reported worldwide. The countries contributing two-thirds of the global total are India (27%), China (9%), Indonesia (8%), Philippines (6%), Pakistan (5%), Nigeria (4%), Bangladesh (4%) and South Africa (3%).2 TB as an “old” invented infection is still a communicable disease in Indonesia [3-5].
The 2014 national tuberculosis control guidelines state that the government’s efforts to achieve success rates include health promotion about TB for families and communities. In addition, efforts to control risk factors b involve administering BCG injections as part of the strategy (find and get cured completely/temukan obati sampai sembuh) and providing logistics of Anti-TB drugs (obat anti TB). Successful TB treatment can be achieved by implementing the national tuberculosis control strategy [6, 7].
The rules that strengthen national strategies and guidelines for eradicating TB are outlined in presidential decree No. 67 of 2021, which emphasizes the role of cadres and the community in the national tuberculosis control program [3, 8]. Efforts to increase the role of these cadres will increase the effectiveness of the program implementation based on the district area (district-based public-private mix), such as improving patient independence in carrying out TB treatment and strengthening TB program management [9].
The COVID-19 pandemic substantially hindered the implementation of many communicable disease programs in the community [10-12]. Existing research regarding TB program implementation in Indonesia is quite limited. A previous qualitative study in Indonesia found that health cadres play a substantial role in supporting TB patients and their families, but it did not specifically address whether the COVID-19 pandemic affected this support. Another Indonesian quantitative study examined healthcare professionals in the context of private healthcare facilities regarding TB diagnosis during the COVID-19 pandemic [9, 13]. To our knowledge, there are few studies focused on exploring the experiences of health cadres during the implementation of TB programs in the COVID-19 era. As the participants were primarily members of the community, in which they live, this study approached their experiences through a qualitative design. This method was chosen due to the limited previous studies that could provide a baseline for this issue [14] Therefore, this study aimed to gain an understanding of the experience of community health cadres while implementing TB programs during COVID-19 and to comprehend what they perceived as differences between the period before COVID-19 and during COVID-19.
Methods
Samples and locations
This study was conducted in one sub-recipient community in Lampung, Indonesia, which focuses on managing the TB program. Inisiatif Lampung Sehat (ILS) has a well-equipped organization and is one of the community sub-recipients providing support for the TB program for the Province of Lampung. Coordination is managed through the Provincial Coordinator, while project officers oversee each district/city, where all cadres work within the sub-district health centers. Case managers coordinate patient support for multi-drug resistant TB (MDR TB) patients. The total number of participants was 26, including case managers, project officers, patient supporters, and cadres.
Design
This study used an interpretive phenomenological approach to understand the experiences of health cadres, specifically regarding TB program implementation (case detection and medication support). This approach allowed us to capture both positive and negative perceived experiences. This study’s objectives were to explore the experience of community health cadres while implementing the TB program during COVID-19 and to comprehend what they perceived as differences between the periods before and during COVID-19.
Data collection
Data collection was done in May 2021 in collaboration with a non-government organization, the sub-recipient community, which focuses on TB management. Data were collected using a recorder and field notes as resources. Each in-depth interview lasted between 45 and 60 minutes.
Instruments
The instrument used consisted of five semi-structured interview guidelines, with five questions serving as the foundational inquiries. 1) What differences were felt in mentoring patients before and during COVID-19 (this included case finding and the investigation of contacts: Household contacts and non-household contacts, as well as community and surrounding environments); 2), What actions were taken that differed before and during COVID-19 ? 3) How does it feel to supervise or assist TB treatment patients during the COVID-19 pandemic? 4) What obstacles/difficulties/challenges did you face in providing support to TB patients? 5) What are the hopes of cadres in facilitating patient support?
Data analysis
The audio recordings were transcribed verbatim by all researchers who conducted each in-depth interview using Microsoft Word. Participants were not identified and were coded in the transcripts to ensure anonymity. The transcripts were subsequently checked by two other researchers to enhance accuracy. We used thematic analysis with the following steps: Transcription, familiarization with the data, selection of quotations, selection of keywords, coding and theme development [15]. Data were analyzed in the form of themes by identifying similarities and differences in data in the interview data, which were then grouped into broader categories of meaning that were more abstract and comprehensive.
Results
All participants were from one sub-recipient community that was established for the TB implementation program. The sociodemographic findings are summarized in Table 1.
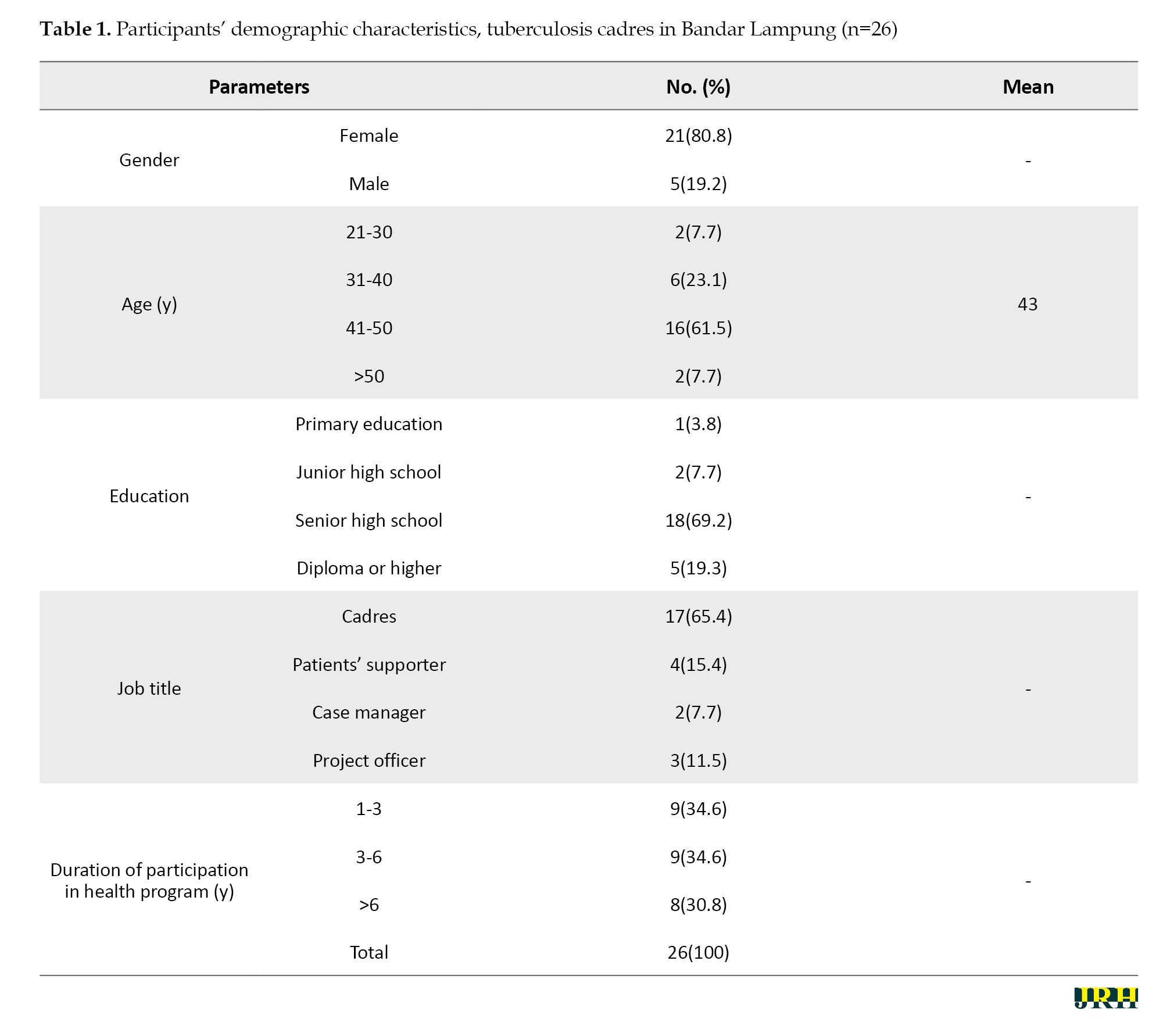
The themes found were described in Figure 1. A total of 26 informants contributed to this study. Most of the participants were cadres (65.4%). The majority of participants were female and aged 41 to 50 years. Moreover, most participants were senior high school graduates, with an average age of 43 years. All participants were from three districts: Pesawaran, Pringsewu, and South Lampung, as well as one city, Bandar Lampung.
Participants’ experiences regarding TB implementation varied before and during the COVID-19 pandemic era. This study highlights the COVID-19 period from its onset in 2020 until the end of 2021 when COVID-19 cases increased and social distancing measures were implemented in Indonesia.
Two themes emerged from the participant’s narratives: The non-personal function aspects, which classified experiences based on the types of activities and health policies implemented and the personal functional aspects, which were derived from the individuals involved in the participants’ experiences, such as TB suspects, TB patients, the cadres themselves and the organizations.
Non-personal function aspect
Participants described their experiences as being mostly stressful due to their activities and the health policies that were implemented during COVID-19.
1) The types of activities emphasized the differences between before and during COVID-19, highlighting the contrast between the two eras. Participants’ experiences regarding the types of activities include:
a. Indirect vs phone communication
“This pandemic has been very, very different, very far away. We can’t meet face to face, we can only communicate by phone” (P9-cadre). “Also, sometimes patients and companions only hear voices... We used to meet in person” (P6- patients supporter). “...it was mostly virtual assistance” (P2_case manager).
b. Unlimited vs limited
“Before COVID-19, we used to visit without being restricted. For example, during contact investigations, we were free. But after COVID-19, our access was limited” (P 12-cadre). “So that’s it, we still go to the field. COVID-19 restricts us from going out, right? So, if every medicine is taken, the cadre takes it from the health center and delivers it to patients” (P11-cadre).
c. Maximum number of participants in health education
“Before COVID-19, they would come in droves. We had up to 40 people” (P10-cadre). “During COVID-19, the sessions were not held as frequently, so there were fewer attendees. We also counseled only a few suspects. Additionally, some mosques were closed” (P13- cadre).
d. Prohibition of mass health education
“But during COVID-19, indeed we as cadres are not allowed to go out. We are not allowed to go out even for counseling or to visit patients” (P11-cadre). “Before COVID-19, we could gather people for a contact investigation. During COVID-19, we want to gather people, it’s difficult, we can’t (P8-cadre).
2) Health policies during COVID-19
a. Social distancing during hospital visits during COVID-1. “As much as possible, there should be no accumulation in the hospital” (P6-project officer).
b. Shortening the duration of services
“During COVID, health center services were limited, operating from 9 AM to 12 PM and then it was closed. The examination times were constrained; for TB, it was only on Tuesdays and Thursdays” (P8-cadre).
c. Restrictions on the distribution of anti-TB drugs
“During COVID-19, it was allowed to dispense anti-TB drugs for one-month supplies” (P12-cadre).
d. The COVID-19 Swab room and TB sputum collection room were closed. “The TB outpatient room is the same as the one for checking people who have COVID-19, it’s closed” (P12-cadre).
e. Hospital’s admission requirement: Swabbing before admission
“Since COVID, the hospital has been very strict when we must visit our patients. We have to be careful” (P5-Patients’ supporter). “When the patient condition worsens, they must go to the emergency room and undergo a PCR swab, which causes patients to choose not to go to the hospital because of the complicated admission procedure” (P15- Patients’ supporter).
Personal function aspects
This study gathered experiences from the whole sub-recipient community organization. Therefore, their experiences could be classified based on both the participants’ experiences and their perceptions of TB suspects and TB patients with whom they interacted.
1. TB suspects’ perspective
a. Afraid of being suspected of having COVID-19 while needing to undergo sputum testing. “Many inhabitants were afraid of being suspected of having COVID-19 during those times. They rarely intended to undergo swab testing. ‘Ah, I’m afraid; I’m afraid of being suspected of having COVID-19,’” (cadre imitating how the inhabitants spoke)” (P8-cadre). “During the COVID-19 pandemic, many people were afraid. So, I’m afraid (cadre imitating the way inhabitants spoke). I’m going to think it’s COVID-19 ; I don’t want them to pierce my nose, I hate it” (P13-cadre).
b. Afraid of being suspected of having COVID-19 while experiencing other symptoms, such as fever
“They did not want to get checked; they were afraid. They didn’t want to check their sputum; they felt feverish and didn’t want to go to the health center either.” (P9- cadre)
2. TB patients’ perspective
a. Social stigma toward TB patients who cough
“Society’s stigma towards patients who have a slight cough is getting worse because our patients are considered to have COVID-19, because the symptoms of TB and COVID are the same, such as coughing” (P3-project officer). “Especially when they were admitted to the hospital, they were afraid, and the stigma from other people was negative” (P3-project officer).
b. Afraid of being doubly diagnosed with COVID-19
“Our patients, if they have TB, are afraid that they will also be considered to have COVID-19 ” (P3-project officer).
3. Cadres’ perspective
a. Cadres’ feelings
“In the past, before the pandemic, we just relaxed and enjoyed ourselves. Now, there are many obstacles because, for example, when we visit a patient, we have to be extremely cautious” (P14-cadre). “There is still fear inside. But Alhamdulillah, we have been safe” (P12-cadre). Because we are the ones who visit the patient’s home, sometimes we feel… not welcomed—like we are being rejected” (P14-cadre).
b. Cadres’ attitude
“Doing health education was prohibited during the pandemic. But because we have a cadre identity, we continue to push forward” (P11-cadre). “We are already wearing standard masks, so sometimes what we are afraid of is our family, especially when we are not affected and not feeling well” (P8-cadre). I think I have a moral responsibility. The first time I became a cadre, I met a patient who had TB, and that’s why he left his wife. I got the news that the person was treated and died” (P12-cadre).
c. Cadres’ hopes
“Those who are infected with TB are not just from the upper-class economic group. I hope for continuous collaboration between our sub-recipient community and global financial supporters” (P14-cadre). “The hope is that, as cadres, especially in this sub-district, our society gets more knowledge and becomes more aware that being healthy is very important. So, hopefully, in this area, TB patients who are still on treatment could finish their medication and be free of TB” (P9-cadre). “The hope is that we, as cadres, will also receive concern and care. So, when we want to go to the field, we feel afraid; for example, regarding masks, yes, we need facilities” (P7-cadre).
2. Organizational officers’ perspectives
a. Project officer
“I feel afraid when carrying out assistance because of the issues and dangers associated with COVID-19 itself” (P4-project officer). “We hope that financial support in mentoring will be increased” (P3-project officer).
b. Case manager
“It’s the same but that, it’s just our hard work if our role is heavier. Our role is heavier in being aware of TB and being aware of the COVID-19 ” (P2-case manager). “It’s the same, but it’s just our hard work; our role is heavier. Our responsibility is to raise awareness about TB and COVID-19 ” (P2-case manager).
“I still hope we could go back to recovery situation like before COVID-19. MDR TB patients can sit together, and they commit to taking the medicine at the hospital in front of us” (P1-case manager).
a. “We hope that if this could be published, our statement and our stories would be beneficial for the society and improve the quality of the TB implementation program” (P1-case manager).
b. Patients’ supporter
“But alhamdulillah, I’m happy to fulfill my role as a patients’ supporter” (P6-patients’ supporter). “I feel proud. I am doing this not merely for money or material gain. I purely want to help others” (P5-patients’ supporter). “Yes, I hope my patient recovers; that’s all, I hope the treatment is finished” (P6-patients’ supporter).
Discussion
This study showed the crucial role of sub-province community organizations that coordinate implementation efforts alongside referral hospitals and health centers in combating TB during the COVID-19 pandemic. This context of this study is in line with an integrative review from several countries (India, Bangladesh, Pakistan, Sierra Leone, Kenya and Ethiopia) that emphasized the importance of community workers in areas, such as surveillance, and community education [12, 16, 17].
This study revealed that the connection of cadres to the communities they belong to was the primary rationale for the emergence of activity types related to non-personal functions and close relationships with community members. A previous Nigerian study showed that health extension workers, referred to as cadres in this study, are often undervalued in society and play a vital role in bridging the gap between the community and the healthcare systems [18]. This study, along with previous research, agrees that cadres played a significant role during the pandemic in assisting healthcare facilities with managing pandemics and other communicable disease burdens, such as TB [19, 20].
This study found that some cadres were eager to visit TB patients’ homes during the COVID-19 pandemic, even though the locations were quite distant. Previous quantitative studies conducted in East Nusa Tenggara Province, Indonesia, reported different results regarding geographical coverage [3, 21, 22]. These studies showed that Indonesia is an archipelago with many islands, each having varying levels of infrastructure and healthcare facilities. This study was done in a district near the city. Another difference is that the previous studies were conducted before the COVID-19 pandemic (January 2019), while this study was conducted during COVID-19 (May 2022) [23–26].
This study found that health cadres’ feelings, attitudes, and commitment to implementing TB initiatives during the COVID-19 pandemic were very robust, despite all the difficulties during the pandemic. Yet, a previous study before the COVID-19 pandemic in Palu City found that there is a positive correlation between cadres’ motivation and active case-finding activities [22]. Although both studies were set in a city near a coastal area, they utilized different quantitative and qualitative approaches. Some studies revealed that incentives and training can increase the motivation of health cadres [27, 28]. This study found that sub-recipient community organizations provided supportive coordination for the health cadres. Their involvement in TB implementation and motivation to ensure patients complete their medications were evident [29–31].
Stigma toward TB patients during the COVID-19 pandemic was also an important finding in this study. This issue is quite complex, as TB and COVID-19 are respiratory illnesses, with similar symptoms, such as coughing and fever. Cadres reported that it was challenging to persuade suspected TB patients to undergo sputum examinations during the COVID-19 pandemic [1, 32, 33]. Overcoming the stigma associated with TB, especially lessons learned during the COVID-19 pandemic, requires a multi-level approach that includes education, increasing awareness, patient-centered care, and community involvement [27].
This study revealed that cadres are striving to do their role in the TB implementation program because they recognize their importance to the community they serve [34, 35]. This finding affirms a previous study that indicated cadres maintain close relationships with the community and assist in bridging the gap between the community and healthcare systems [36, 37]. Cadres expressed the need for facilitation during the pandemic, such as personal protective equipment (PPE), which aligns with other previous studies [38, 39].
This study gathered data from participants who have worked for years in TB programs within the community, allowing for a detailed and in-depth examination of their experiences. The study observed participants doing some coordination meetings; however, the data collected may present a limitation that could affect the participants’ responses [40].
Conclusion
Sub-recipient community organizations that coordinate implementation along with referral hospitals and health centers play a vital role in dealing with TB during the COVID-19 pandemic. Health cadres were significant contributors during the pandemic, assisting healthcare facilities in managing the pandemic and other communicable disease burdens, such as TB. Healthcare professionals must strengthen coordination and cooperation with health cadres, especially considering the lessons learned during COVID-19. Health cadres are passionate and make every effort to serve the communities from which they originate. This qualitative study revealed that health cadres need support, including protective equipment, during outbreaks of communicable diseases. This study was conducted in only one city in Indonesia using simple interview guidelines. It would be beneficial to conduct a quantitative study to measure the health cadre’s abilities based on their experiences during COVID-19.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the research and community services, Universitas Pelita Harapan, Banten, Indonesia (Code: 118-IRB/PN-FoN-UPH/XI/2021). Each participant received the study’s explanation (study’s goal and procedures) before in-depth interviews began. Participants were also given the opportunity to ask for clearer explanations of their doubts to facilitate informed consent. Participation was voluntary, and participants had the right to withdraw from the study at any time. They were reassured that all statements shared were not considered right or wrong but were purely reflections of their personal experiences.
Funding
This study was financially supported by the Research and Community Service at Universitas Pelita Harapan, Banten, Indonesia.
Authors' contributions
Investigation: Theresia Theresia; Project administration, data collection, resources, visualization, and writing: Tirolyn Panjaitan; Validation, supervision and funding: Theresia Theresia, Lina Berliana Togatorop and Satriya Pranata; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Universitas Pelita Harapan, Banten, Indonesia for its funding support and Inisiatif Lampung Sehat for serving as our study partner.
References
- Salles I, Travassos P, Spener-Gomes R, Loch AP, Saraceni V, Lauria L, et al. Contextualizing and optimizing novel strategies to improve the latent TB continuum of care: Insights from people living with HIV and health care providers in Brazil. PLOS Global Public Health. 2023; 3(1):e0001251. [DOI:10.1371/journal.pgph.0001251] [PMID]
- Persaud N, Sabir A, Woods H, Sayani A, Agarwal A, Chowdhury M, et al. Preventive care recommendations to promote health equity. CMAJ. 2023; 195(37):E125073. [DOI:10.1503/cmaj.230237] [PMID]
- Amalia I, Farhany FF, Rachmawati MB, et al. Combating Infectious Diseases Threat among Students in Islamic Boarding School (Pondok Pesantren): A Pilot Assessment. Journal of Community Empowerment for Health. 2023; 6(1):7. [DOI:10.22146/jcoemph.77426]
- Kaaffah S, Kusuma IY, Renaldi FS, Lestari YE, Pratiwi ADE, Bahar MA. Knowledge, attitudes, and perceptions of tuberculosis in Indonesia: A multi-center cross-sectional study. Infection and Drug Resistance. 2023; 16:1787-800. [DOI:10.2147/IDR.S404171] [PMID]
- Chandru BA, Varma RP. Factors affecting ability of TB patients to follow treatment guidelines-Applying a capability approach. International Journal for Equity in Health. 2023; 22(1):176. [DOI:10.1186/s12939-023-01991-7] [PMID]
- Oduor C, Omwenga I, Ouma A, Mutinda R, Kiplangat S, Mogeni OD, et al. Mortality patterns over a 10-year period in Kibera, an urban informal settlement in Nairobi, Kenya, 2009-2018. Global Health Action. 2023; 16(1):2238428. [DOI:10.1080/16549716.2023.2238428] [PMID]
- Zhu X, Wang J, Zhang Z, Yan L, Liu H, Chen Y, et al. A participatory approach to understand the attitudes and perceptions towards priority endemic cattle diseases among dairy farmers and animal health experts in Henan province, China. Preventive Veterinary Medicine. 2023; 218:105994. [DOI:10.1016/j.prevetmed.2023.105994] [PMID]
- Andriani D, Sukardin S. [Pengetahuan dan sikap keluarga dengan pencegahan penularan penyakit tuberculosis (TBC) di wilayah kerja puskesmas penana’e kota bima (Indonesian)].Jurnal Ilmiah Ilmu Keperawatan Indonesia. 2020; 10:72-80. [DOI:10.33221/jiiki.v10i03.589]
- Aisah S, Al Jihad MN, Pebriani A, Pranata S, Soesanto E. Bibliometric analysis of nursing interventions to improve adherence to treatment among patients with tuberculosis. Africa Journal of Nursing and Midwifery. 2024; 26(1):1-19.[DOI:10.25159/2520-5293/14557]
- Alemu T, Bezabih B, Amsalu A, Hassen E, Haile M, Abite M. Health and nutrition emergency response among internally displaced persons at Ranch collective site, Chagni, Ethiopia: The role of emergency operation center, lessons from the field, and way forwards. Frontiers in Public Health. 2022; 10:926551. [DOI:10.3389/fpubh.2022.926551] [PMID]
- Jeong Y, Min J. Impact of COVID-19 pandemic on tuberculosis preventive services and their post-pandemic recovery strategies: A rapid review of literature. Journal of Korean Medical Science. 2023; 38(5):e43. [DOI:10.3346/jkms.2023.38.e43] [PMID]
- Alfaiate A, Rodrigues R, Aguiar A, Duarte R. Tuberculosis and COVID-19 related stigma: Portuguese patients experiences. Tuberculosis and Respiratory Diseases. 2023; 86(3):216-25. [DOI:10.4046/trd.2022.0062] [PMID]
- Widayanti AW. Understanding health-seeking behaviours of people in Indonesia; and developing, piloting, and evaluating a culturally appropriate intervention for people with diabetes [doctoral thesis]. Dunedin: University of Otago; 2018. [Link]
- Teherani A, Martimianakis T, Stenfors-Hayes T, Wadhwa A, Varpio L. Choosing a qualitative research approach. Journal of Graduate Medical Education. 2015; 7(4):669–70. [PMID]
- Naeem M, Ozuem W, Howell K, Ranfagni S. A step-by-step process of thematic analysis to develop a conceptual model in qualitative research. International Journal of Qualitative Methods. 2023; 22. [DOI:10.1177/16094069231205789]
- Bekele D, Aragie S, Alene KA, Dejene T, Warkaye S, Mezemir M, et al. Spatiotemporal distribution of tuberculosis in the oromia region of Ethiopia: A hotspot analysis. Tropical Medicine and Infectious Disease. 2023; 8(9):437. [DOI:10.3390/tropicalmed8090437] [PMID]
- Varshney K, Patel H, Kamal S. Trends in tuberculosis mortality across India: Improvements despite the COVID-19 pandemic. Cureus. 2023; 15:e38313. [DOI:10.7759/cureus.38313]
- Adepoju VA, Oladimeji KE, Adejumo OA, Adepoju OE, Adelekan A, Oladimeji O. Knowledge of international standards for tuberculosis care among private non-NTP providers in Lagos, Nigeria: A cross-sectional study. Tropical Medicine and Infectious Disease. 2022; 7(8):192. [DOI:10.3390/tropicalmed7080192] [PMID]
- Zaildo T, Santino TA, Chaves G, da Silva BAK, Alchieri JC, Patino CM, et al. Barriers to and facilitators of populational adherence to prevention and control measures of COVID-19 and other respiratory infectious diseases: A qualitative evidence synthesis. European Respiratory Review. 2023; 32(168):220238. [DOI:10.1183/16000617.0238-2022] [PMID]
- Kumwichar P, Chongsuvivatwong V. COVID-19 pneumonia and the subsequent risk of getting active pulmonary tuberculosis: A population-based dynamic cohort study using national insurance claims databases. EClinicalMedicine. 2023; 56:101825. [DOI:10.1016/j.eclinm.2023.101825] [PMID]
- Herdiana D. Social distancing: Indonesian policy response to the corona virus.Jurnal Ilmu Administrasi. 2020; 17:93-110. [DOI:10.31113/jia.v17i1.555]
- Lauren C, Iskandar A, Argie D, Malelak EB, Sebayang SE, Mawardy R, et al. Strategy within limitations during COVID-19 pandemic in Indonesia: Shortage of PPE, prevention and neurosurgery practice. Bali Medical Journal. 2020; 9(3):682-4. [DOI:10.15562/bmj.v9i3.1825]
- Hertinjung WS, Laksmadita CT, Ruhaena L, Sulandari S, Kusumawati DA. Reducing parenting stress among Muslim mothers during the COVID-19 pandemic through spiritual mindfulness training. Humanitas. 2023; 20(2):102-16. [DOI:10.26555/humanitas.v20i2.288]
- Khozanatuha F, Setiyani R, Kusumawardani LH. Predictors of COVID-19 related health literacy among older people living in rural areas of Indonesia. Investigacion y Educacion en Enfermeria. 2023; 41(2)e13. [DOI:10.17533/udea.iee.v41n2e13] [PMID]
- Hizbaron DR, Ruslanjari D, Mardiatno D. Amidst COVID-19 pandemic: An adaptive disaster governance in Yogyakarta, Indonesia. Social Sciences. 2021; 10(3):92. [DOI:10.3390/socsci10030092]
- Kementrian K. [Dashboard Case of COVID-19 in Indonesia (Indonesian)]. 2022.
- Pranata S, Vivienne Wu SF, Armiyati Y, Khoiriyah K, Shing LC, Liu JH. Implementing precision health care program at hospitals in Indonesia. Journal of Research and Health. 2023; 13(6):457-66. [DOI:10.32598/JRH.13.6.2183.3]
- Pranata S, Vranada A, Armiyati Y, Samiasih A, Aisah S, Kurnia A, et al. Inflammatory markers for predicting severity, mortality, and need for intensive care treatments of a patient infected with COVID-19: A scoping review. Bali Medical Journal. 2023; 12(1):324-30. [DOI:10.15562/bmj.v12i1.3751]
- Palupi S, Pambudi I, Surya A, Bramanthi R, Arfi M, Suyanto S, et al. Sequence of COVID-19 vaccination and COVID-19 infection and their association with the development of active tuberculosis: A case-control study. Cureus. 2023; 15(10):e46353. [DOI:10.7759/cureus.46353] [PMID]
- Madebo M, Balta B, Daka D. Knowledge, attitude and practice on prevention and control of pulmonary tuberculosis index cases family in Shebedino District, Sidama Region, Ethiopia. Heliyon. 2023; 9(10):e20565. [DOI:10.1016/j.heliyon.2023.e20565] [PMID]
- Wu S, Litvinjenko S, Magwood O, Wei X. Defining tuberculosis vulnerability based on an adapted social determinants of health framework: A narrative review. Global Public Health. 2023; 18(1):2221729. [DOI:10.1080/17441692.2023.2221729] [PMID]
- Hidayat J, Huang XY, Lin HR, Wei SJ, Chen MY, Pranata S. Exploring the experience of stigma among people living with HIV in Bali, Indonesia: Qualitative phenomenological study. Makara Journal of Health Research. 2022; 26:44-50. [DOI:10.7454/msk.v26i1.1331]
- Meskell P, Biesty LM, Dowling M, Roche K, Meehan E, Glenton C, et al. Factors that impact on recruitment to vaccine trials in the context of a pandemic or epidemic: A qualitative evidence synthesis. The Cochrane Database of Systematic Reviews. 2023; 9(9):MR000065. [DOI:10.1002/14651858.MR000065.pub2] [PMID]
- Sazali MF, Rahim SSSA, Mohammad AH, Kadir F, Payus AO, Avoi R, et al. Improving tuberculosis medication adherence: The potential of integrating digital technology and health belief model. Tuberculosis and Respiratory Diseases. 2023; 86(2):82-93. [DOI:10.4046/trd.2022.0148] [PMID]
- Klever AM, Alexander KA, Almeida D, Anderson MZ, Ball RL, Beamer G, et al. The many hosts of mycobacteria 9 (MHM9): A conference report. Tuberculosis. 2023; 142:102377. [DOI:10.1016/j.tube.2023.102377] [PMID]
- Harding R, Snyman L, Ostgathe C, Odell S, Gwyther L. The ethical imperative to relieve suffering for people with tuberculosis by ensuring access to palliative care. The International Journal of Tuberculosis and Lung Disease. 2020; 24(5):3-8. [DOI:10.5588/ijtld.18.0240]
- Craciun OM, Torres MDR, Llanes AB, Romay-Barja M. Tuberculosis knowledge, attitudes, and practice in middle- and low-income countries: A systematic review. Journal of Tropical Medicine. 2023; 2023:1014666. [DOI:10.1155/2023/1014666] [PMID]
- Srivastava S, Dey S, Mukhopadhyay S. Vaccines against Tuberculosis: Where are we now? Vaccines. 2023; 11(5):1013. [DOI:10.3390/vaccines11051013] [PMID]
- Palacios CF, Hough MA, Shrestha R, Moll AP, Kompala T, Andrews L, et al. Perceived stigma related to TB preventive therapy.The International Journal of Tuberculosis and Lung Disease. 2023; 27(3):209-14. [DOI:10.5588/ijtld.22.0570] [PMID]
- Anderson C. Presenting and evaluating qualitative research. American Journal of Pharmaceutical Education. 2010; 74(8):141. [DOI:10.5688/aj7408141]
Type of Study: Orginal Article |
Subject:
● Disease Control
Received: 2024/08/2 | Accepted: 2024/10/16 | Published: 2025/03/2
Received: 2024/08/2 | Accepted: 2024/10/16 | Published: 2025/03/2
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |