Volume 15, Issue 4 (Jul & Aug 2025)
J Research Health 2025, 15(4): 383-392 |
Back to browse issues page
Ethics code: SH-IRB 2024-014
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Jeong D, Park S. Effects of a Stabilization Exercise Program Using Respiratory Resistance in Older Adults With Low Back Pain. J Research Health 2025; 15 (4) :383-392
URL: http://jrh.gmu.ac.ir/article-1-2710-en.html
URL: http://jrh.gmu.ac.ir/article-1-2710-en.html
1- Department of Physical Therapy, Sehan University, Yeongam, Republic of Korea.
2- Department of Physical Therapy, Kwangju Women’s University, Gwangju, Republic of Korea. ,samho15@kwu.ac.kr
2- Department of Physical Therapy, Kwangju Women’s University, Gwangju, Republic of Korea. ,
Full-Text [PDF 1007 kb]
(66 Downloads)
| Abstract (HTML) (593 Views)
Full-Text: (23 Views)
Introduction
Modern society has entered an aging era because of advances in medical technology and extending life expectancy, which brings various social and economic challenges [1]. As aging progresses, the body functions gradually decline across various systems, with musculoskeletal degeneration leading to reduced motor function and muscle mass loss. In addition, the prevalence of low back pain (LBP) tends to increase with aging, with studies reporting that approximately 50% of older adults experience LBP at some point in their lives [2, 3]. Previous research has highlighted various interventions, including exercise therapy and lifestyle modifications, to mitigate LBP in older people [4, 5].
Physical changes associated with aging lead to the degeneration of muscles and bones, reducing physical activity and setting a cycle of decline [6]. Physical changes associated with aging lead to the degeneration of muscles and bones, reducing physical activity and setting a cycle of decline [6]. In South Korea, the prevalence of LBP among the elderly population is reported to be approximately 40%–50%, with a higher incidence observed in women than in men [7]. Additionally, a national health survey indicates that musculoskeletal disorders, including LBP, are among the leading causes of outpatient visits among older adults, accounting for a significant proportion of medical consultations [8]. For older adults, reduced activity signifies weakened physical function, adversely affecting their social engagement, relationships, and quality of life. In older adults with chronic LBP, higher levels of pain are often associated with reduced physical activity, leading to psychological issues such as depression and anxiety [9].
Among the interventions to reduce pain, restore functional ability, improve balance, and support spinal alignment in patients with LBP, lumbar stabilization exercise is used widely in clinical settings [10]. This method enhances lumbar stability by strengthening deep muscles. These exercises improve segmental control, reduce functional disability and enhance coordination. Additionally, they raise intra-abdominal pressure, support spinal alignment and strengthen abdominal muscles, reducing lumbar pressure. Engaging both abdominal and pelvic muscles also improves balance [11].
The abdominal drawing-in maneuver (ADIM) induces contractions of the diaphragm and transversus abdominis through abdominal hollowing and diaphragmatic breathing, increasing intra-abdominal pressure and effectively supporting lumbar stabilization [12]. Deep muscle contraction is crucial for providing stability to the lumbar segments. Various breathing techniques that promote contractions of the transversus abdominis and diaphragm were applied to maximize the effects of lumbar stabilization exercises for patients with LBP [13, 14]. Among these, lumbar stabilization exercises using respiratory resistance enhance stability by harmonizing the diaphragmatic and transversus abdominis muscle activity, increasing intra-abdominal pressure, and inducing a contraction of the spinal surrounding muscles [13, 14].
Previous studies have shown that lumbar stabilization exercises with respiratory resistance training can reduce pain and improve function in patients with lumbar instability and middle-aged women with LBP. However, research specifically targeting older adults with LBP and the role of breathing in their rehabilitation remains limited. Therefore, this study examined the effects of a lumbar stabilization exercise program using respiratory resistance on pain, motor function, psychosocial factors, and respiratory function in patients with LBP aged 65 years and older. Unlike previous research that assessed these interventions separately, this study evaluates their combined impact, addressing a key gap in the literature.
Methods
Study participants
This study included 53 patients receiving inpatient or outpatient care for LBP at Seongsim Geriatric Hospital, Mokpo, Republic of Korea. The total intervention period was from September 2024 to February 2025. The inclusion criteria were as follows: Aged 65 and older, experience of LBP within the past six weeks, and a quadruple visual analog scale (QVAS) score of 3 or higher [15]. The exclusion criteria included LBP caused by fractures and respiratory conditions that would hinder participation in the intervention.
Study design
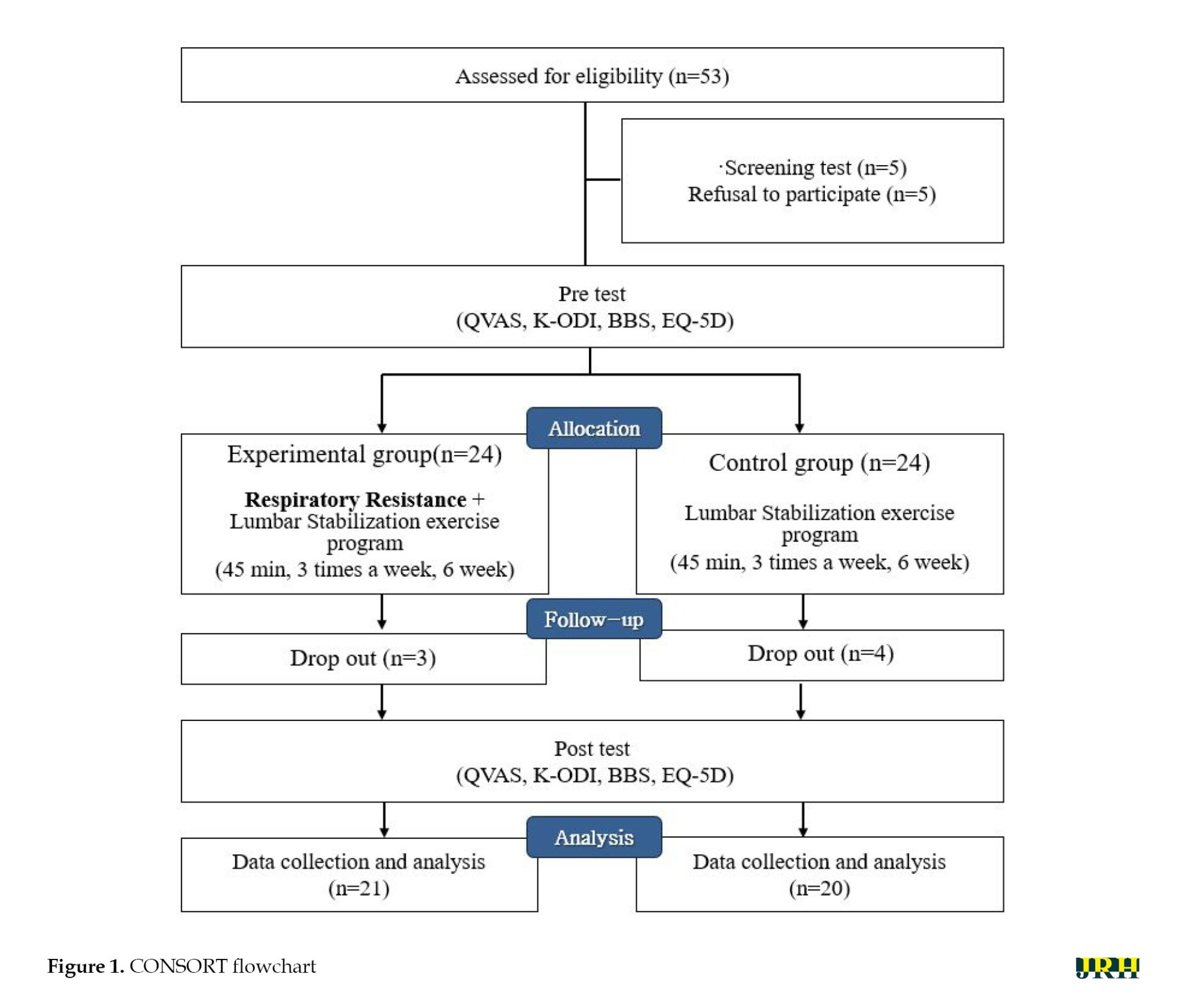
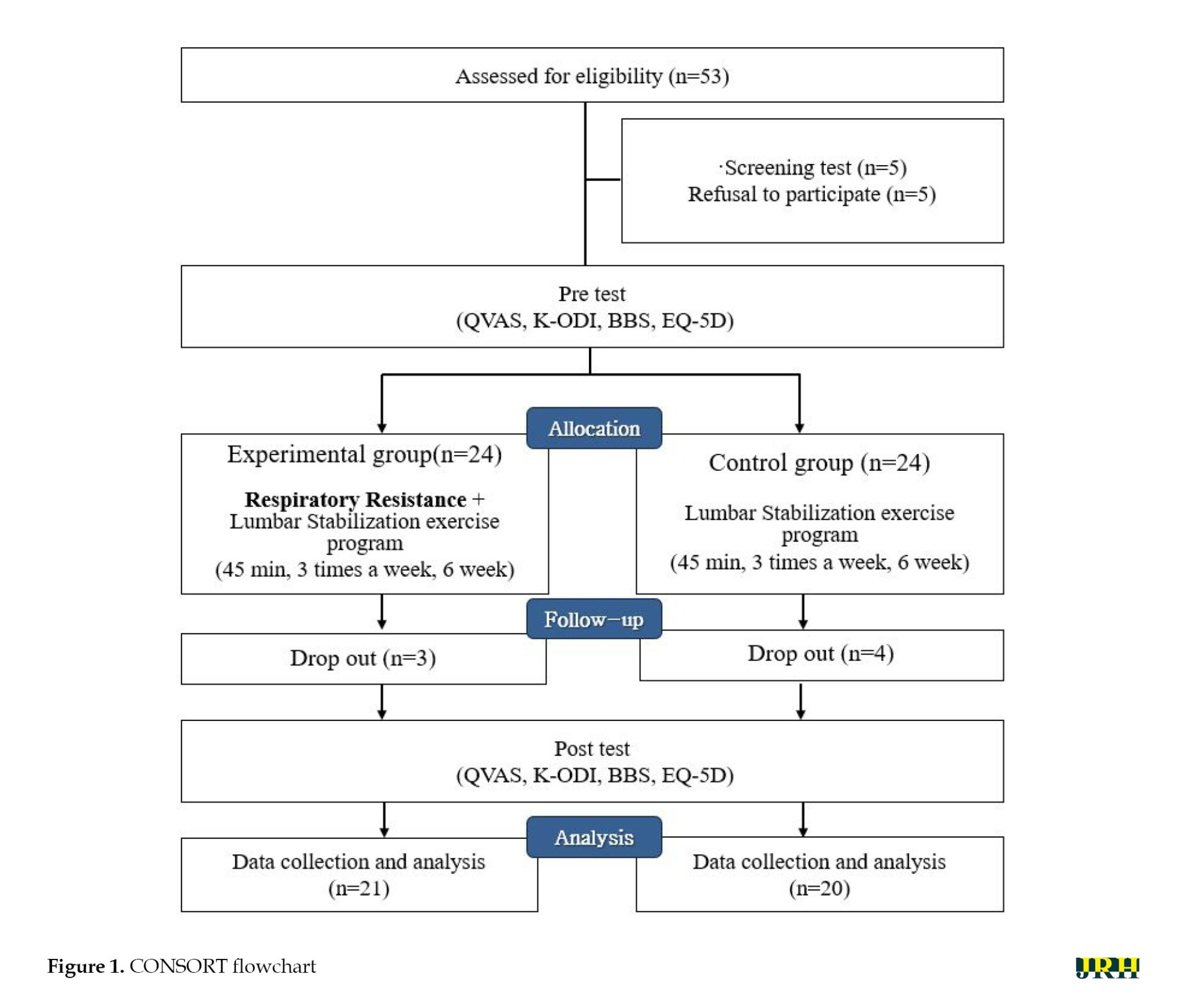
This study used a pre-test, post-test design with a control group with random assignment. The sample size was determined using G*Power software, version 3.1.9.7 (Heinrich Heine University, Düsseldorf, Germany). Based on the main effect size (d) of 0.88 from Park and Lee [13], a significance level (α) of 0.05 and a power (1-β) of 0.80, a minimum of 22 participants per group was required, with an additional 10% to account for potential dropouts, resulting in a target of 24 participants per group [16]. Of the 53 patients recruited, five declined to participate, leaving a final sample of 48 who completed a pre-test and were randomly assigned to either the experimental or control group. Randomization was conducted using an internet-based program (Research Randomizer) [17], assigning the participants to the experimental group (n=24) and control group (n=24).
The experimental group performed a lumbar stabilization exercise program combined with respiratory resistance training, whereas the control group performed only a lumbar stabilization exercise program. Each session included a 5-minute warm-up and cooldown stretch, with approximately 45 minutes per session, thrice a week over six weeks. The program effectiveness was evaluated by taking QVAS, the Korean version of the Oswestry disability index (K-ODI), balance ability, Euro quality of life 5 dimension (EQ-5D) and pulmonary function test (PFT) measurements before and after the intervention. The research flowchart is shown in Figure 1.
Study interventions
Lumbar stabilization exercise program
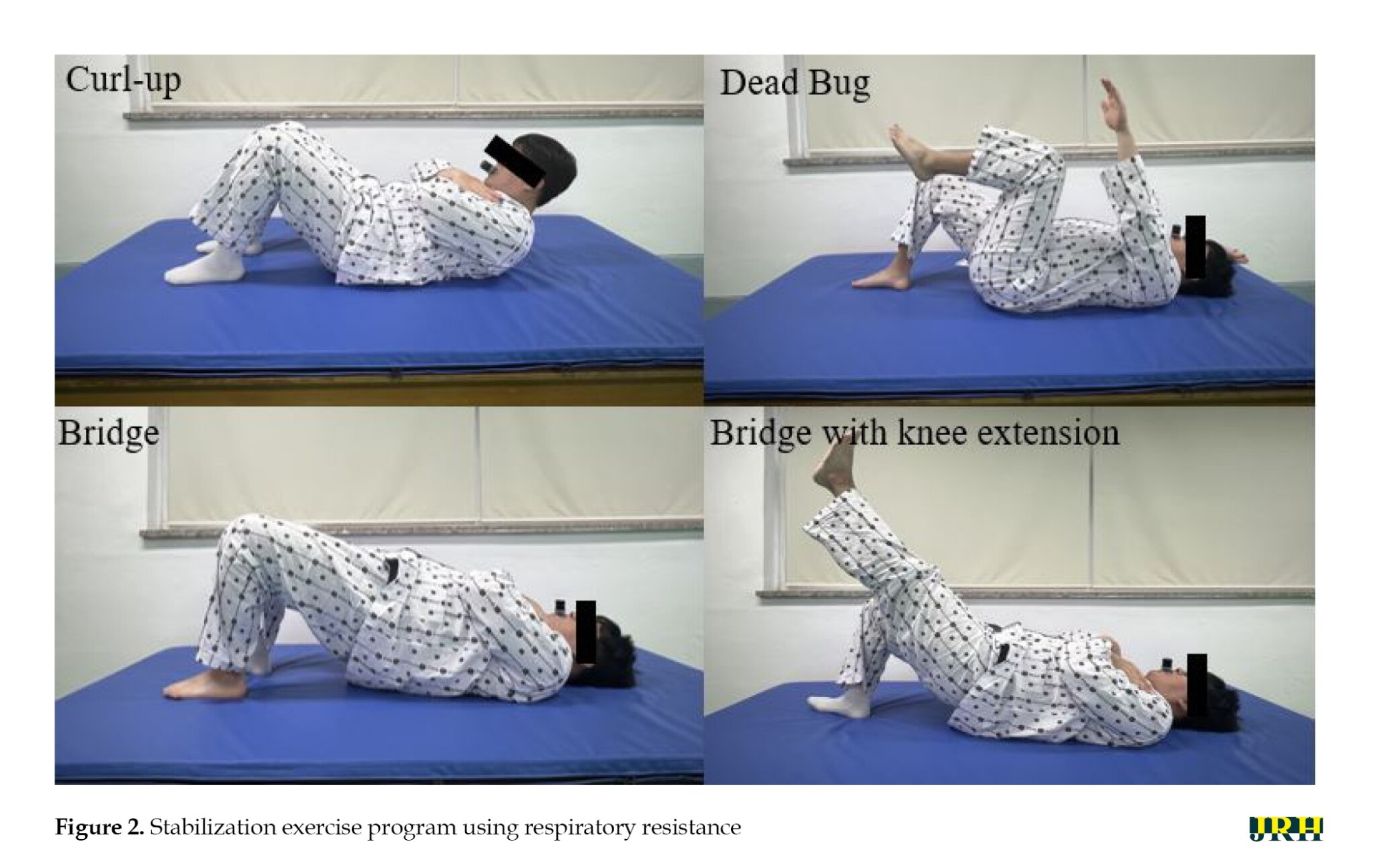
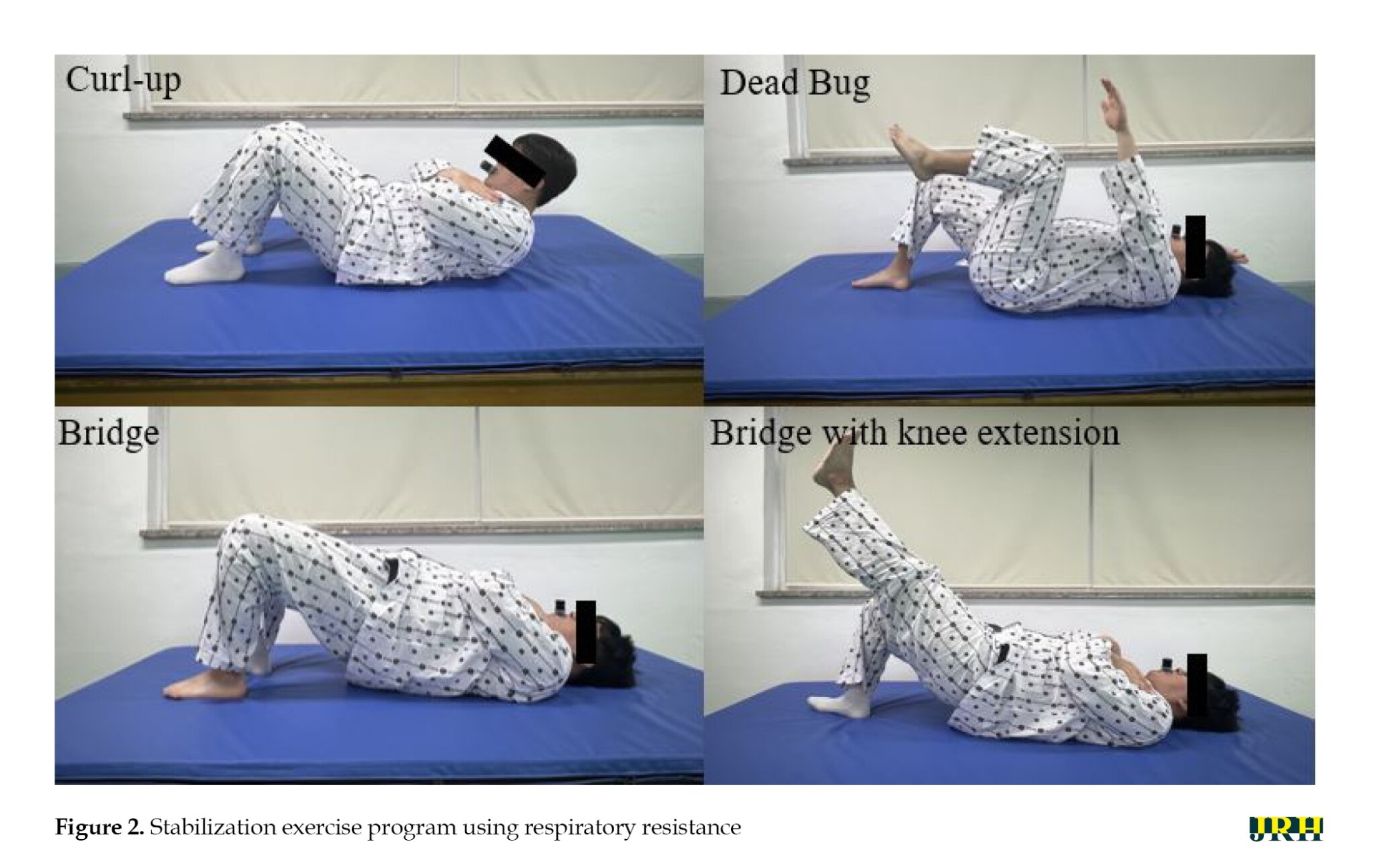
The lumbar stabilization exercise provided to both groups was a modified and supplemented version of the intervention method reported by Park and Lee [13]. The lumbar stabilization exercise program included movements designed to enhance deep muscle activation and promote balance and coordination of muscles surrounding the lumbar region: Curl-up, dead bug, bridge, and bridge with knee extension (Figure 2). Each movement was performed for 15 seconds, repeated 10 times per set, for three sets, with a 20 second rest between sets.
Lumbar stabilization exercise program using respiratory resistance
The experimental group performed breathing resistance training simultaneously with the lumbar stabilization exercise program. Before the intervention, the participants were provided with individualized respiratory resistance devices and were instructed on the operation and diaphragmatic breathing techniques. The respiratory resistance device (Expand-a-Lung, Miami, USA) consisted of a silicone mouthpiece and a main body that allowed airflow control, introducing resistance during inhalation and exhalation to strengthen the respiratory muscles.
During training, the resistance level was adjusted to maintain a rating of perceived exertion of 14 or lower, and participants were pre-informed about possible symptoms such as dizziness, nausea, vomiting, or difficulty breathing [18]. Medical equipment for monitoring body temperature, pulse, respiration, and blood pressure was prepared to cease intervention for adverse symptoms.
Assessment methods
Pain
The pain level of the participants before and after the intervention was assessed using the QVAS. This tool included four items: 1) Current pain, 2) Usual pain, 3) Least pain and 4) Worst pain. Each item was scored on a scale from 0 cm, indicating no pain, to 10 cm, indicating the most severe pain. The average score of the four items was calculated to quantify the pain levels. This tool had an intrarater reliability of r=0.76–0.84, indicating a high level of reliability [19].
Functional ability
The level of functional disability before and after the intervention was measured using the K-ODI. This questionnaire comprised 10 items, with higher scores indicating greater functional disability. The item on sexual activity was excluded, reflecting the cultural considerations in Korea, leaving nine items with a maximum score of 45. The K-ODI demonstrated high test, re-test reliability (r=0.92) [20]. Additionally, its content validity was confirmed through the content validity index (CVI) and content validity ratio (CVR), while internal consistency was assessed using the Cronbach α.
Balance ability
The participants’ balance ability was assessed using the Berg balance scale (BBS) before and after the intervention. The BBS measures static and dynamic balance, comprising 14 items across three domains: Sitting, standing, and posture changes. Each item was rated on a 5-point scale from 0 to 4, with a maximum total score of 56. The BBS demonstrated excellent reliability, with an intrarater reliability of r=0.99 and interrater reliability of r=0.98 [21]. Its validity was supported by the CVI and CVR, and internal consistency was confirmed with a high Cronbach α score.
Quality of life
The participants’ quality of life was evaluated before and after the intervention using the EQ-5D, a widely used tool in healthcare. This instrument assesses five domains: Self-care, mobility, usual activities, anxiety/depression, and pain/discomfort. Each domain is rated at three levels to reflect health status, with the EQ-5D demonstrating high reliability (r=0.87) [22]. The CVI and CVR have supported their validity, while internal consistency was confirmed with a high Cronbach’s α score.
Pulmonary function
The MicroQuark device (COSMED, Rome, Italy) assessed the pulmonary function after inputting each participant’s sex, age, and physical characteristics. The measurements were taken with the participants standing upright, their noses pinched, and biting down on the mouthpiece attached to the MicroQuark.
After maximal inhalation and forced exhalation, the total amount of emitted air is assigned as the forced vital capacity (FVC), and forced expiratory volume (FEV) for 1 s was set as FEV1. The two values were then used to derive the FEV1/FEV ratio (FEV1%) and the amount of ventilated air for 15 s at the fastest speed was converted to the amount in one minute to determine the maximal voluntary ventilation (MVV). A physical therapist with substantial experience in pulmonary function testing assessed three trials, and the values were used for analysis. A 10-minute break was allowed between each test.
Statistical analysis
Data were analyzed using SPSS software, version 21, IBM. The participants’ general characteristics are presented using descriptive statistics, including Mean±SD. The Shapiro-Wilk test was used to assess normality. A chi-square test was performed to analyze the participants’ gender, while a t-test was conducted to analyze the homogeneity of the other general characteristics and pre-test values. The independent samples t-test was used to compare the changes between the two groups before and after the intervention. The paired samples t-test was used to compare the changes in dependent variables before and after the intervention within groups. The statistical significance level (α) was set at 0.05.
Results
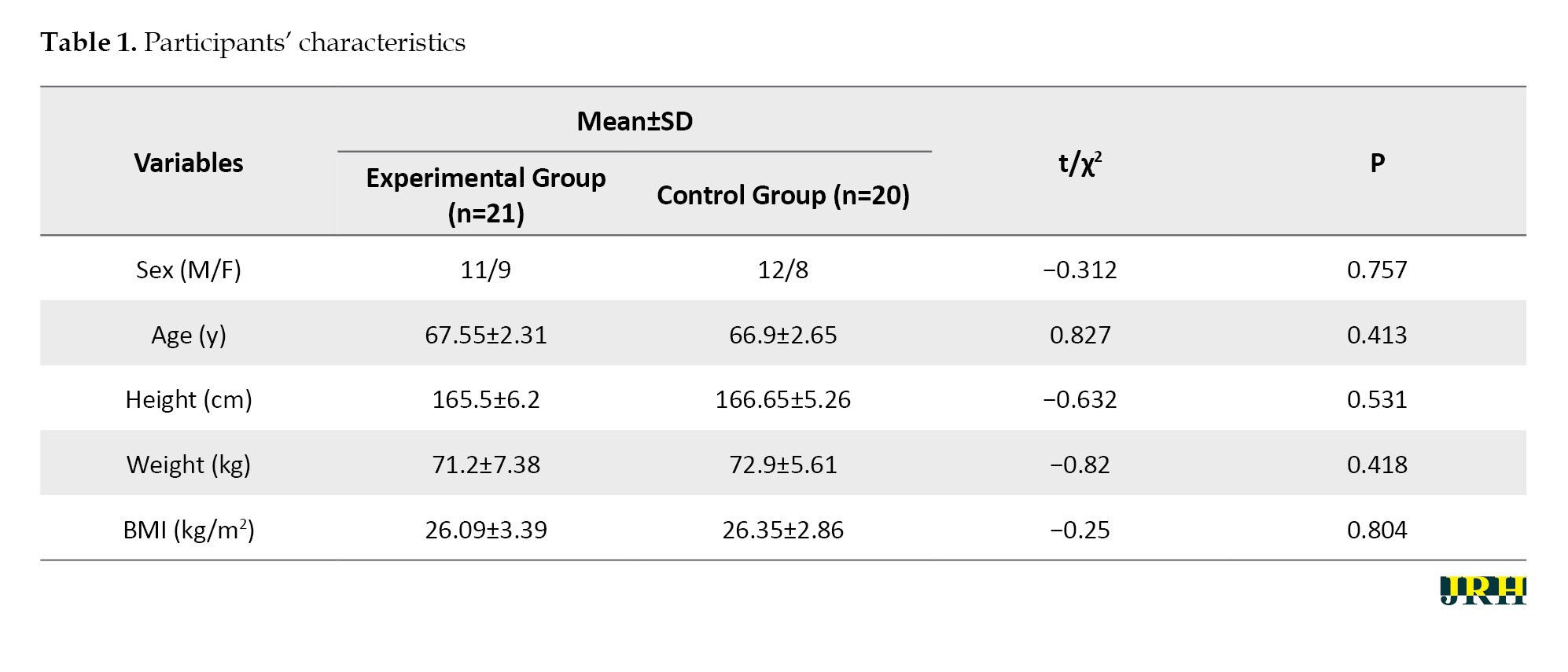
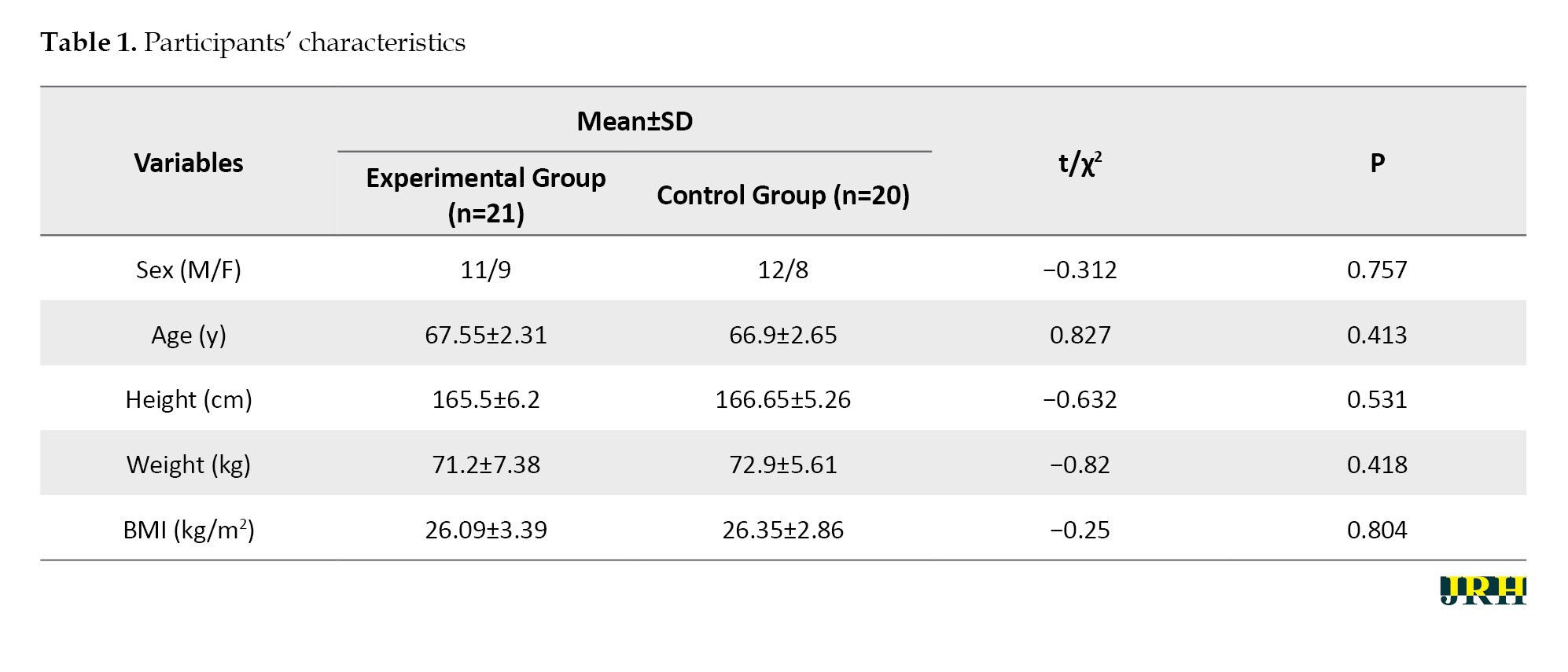
Seven patients were excluded from the experimental and control groups because they refused to participate, and the data from the experiment (n=21) and control (n=20) groups were collected. The general characteristics were similar in the two groups (Table 1).
QVAS, K-ODI, BBS and EQ-5D results showed no significant difference between the two groups before the intervention. However, both groups showed significant improvement after the intervention (P<0.05). Furthermore, the experimental group showed better results in QVAS, K-ODI, BBS and EQ-5D scores than the control group (P<0.05) (Table 2).
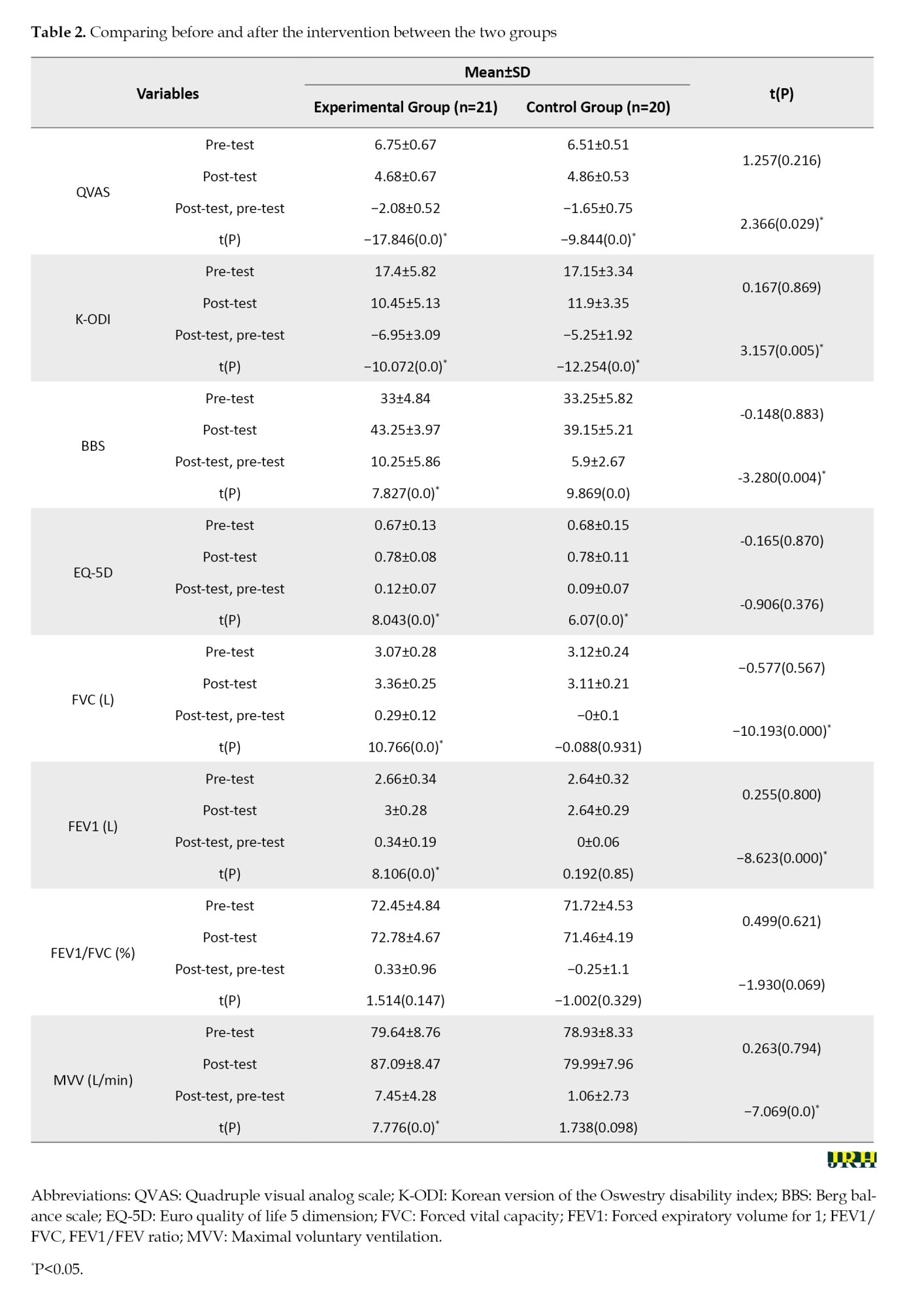
The FVC, FEV1 and MVV values were similar in the two groups before the intervention. A significant difference in the FVC, FEV1 and MVV was observed in the experimental group before and after the intervention (P<0.05). Also, a significant difference in the level of change was noted between the two groups (P<0.05) (Table 2).
Discussion
This study examined the effects of a lumbar stabilization exercise program using the respiratory resistance on pain, motor function, psychosocial factors, and respiratory function in patients aged 65 and older with LBP. The results revealed significant differences in the QVAS, K-ODI, BBS and EQ-5D scores among all study participants. In addition, the experimental group that underwent the lumbar stabilization exercise program using respiratory resistance exhibited significant differences in the changes observed in the QVAS, K-ODI, BBS, FVC, FEV1, and MVV.
Physical pain is one of the most commonly reported health issues among elderly individuals. Physical pain can lead to problems in motor function and physical, mental, and social issues [23]. Among these, LBP is a condition with a high prevalence, particularly requiring more management in the elderly population. Ge et al. [24] applied a core stability training program for four weeks to individuals aged 60 years and older with LBP, reporting significant improvement in pain levels (effect size: 1.72, P<0.05). Park et al. [10] examined women over 40 years with LBP, applying a stabilization exercise program using respiratory resistance for four weeks, also noting a significant improvement in the pain levels (effect size: 5.21, P<0.05). All participants showed significant improvement in the pain levels before and after the intervention (P<0.05). Furthermore, the experimental group that engaged in the lumbar stabilization exercise program using respiratory resistance showed differences from the control group (effect size: 0.84, P<0.05). Hence, breathing exercises, such as deep breathing, may activate the parasympathetic nervous system, helping to relieve tension and decrease pain sensitivity.
Older adults aged 65 years and above commonly experience musculoskeletal weakness and decline in motor function. Training combined with respiratory resistance offers a relatively low-intensity exercise approach that can safely and effectively aid in pain management. Ge et al. [24]. implemented a four-week core stability training program for individuals aged 60 years and older with LBP, reporting significant improvements in functional disability (effect size: 1.47) and dynamic balance ability (effect size: 2.07, P<0.05). Seo and Lee [25] applied a four-week stabilization exercise program with whole-body vibration in a population of individuals aged 75 and above, observing significant improvements in the static balance (effect size: −2.14) and dynamic balance (effect size: 1.27, P<0.05). Similarly, in this study, all participants showed significant improvement in the motor function levels before and after the intervention (P<0.05), and the experimental group who performed lumbar stabilization exercises using respiratory resistance exhibited significant differences compared to the control group (K-ODI effect size: 1.27, BBS effect size: −2.32). These findings suggest that respiratory resistance training activates the abdominal and thoracic muscles, contributing to the stabilization of spinal muscles by strengthening deep muscles. In particular, respiratory training may play a key role in enhancing motor function in older adults, where muscle weakness affects posture and body stability.
Respiratory resistance training activates the parasympathetic nervous system through deep breathing, reducing stress and tension [26]. This activation provides psychological stability and may help to alleviate anxiety related to pain in elderly individuals with LBP [27]. Park et al. [10] reported that a stabilization exercise program using respiratory resistance significantly improved the psychosocial aspects of physical activity (effect size: 3.02) and work (effect size: 2.87) in middle-aged women with LBP (P<0.05). Similarly, this study revealed significant improvement in the psychosocial levels before and after the intervention among all participants (P<0.05), even though no significant difference was found between the two groups (experimental group effect size: −0.45, control group effect size: −0.35). Although respiratory resistance training and lumbar stabilization exercises take different approaches, both exercise have a common positive impact on psychological states. For older adults, engaging in exercise promotes social interactions, improves confidence through participation in activities, reduces social isolation, and contributes to psychological stability.
Respiratory resistance training is essential for improving breathing efficiency and activating the muscles surrounding the spine. In older adults, decreased respiratory function, reduced muscle strength, and diminished flexibility can exacerbate LBP, highlighting a need for respiratory resistance training as part of a comprehensive management approach [10, 12-14]. Park and Lee [13] reported that a stabilization exercise program using respiratory resistance significantly improved the respiratory function in patients with lumbar instability (FVC effect size: −0.23, FEV1 effect size: −0.23, MVV effect size: −0.88). In addition, Oh et al. [12] reported significant improvements in the respiratory function in middle-aged women with LBP who performed ADIM lumbar stabilization exercises with respiratory resistance (FVC effect size: −0.52, FEV1 effect size: −0.35, MVV effect size: −1.14). Similarly, in this study, only the experimental group performing lumbar stabilization exercises using respiratory resistance showed significant improvements in the respiratory function (FVC effect size: −1.09, FEV1 effect size: −1.09, MVV effect size: −0.86). This finding suggests that training with respiratory resistance enhances the respiratory muscle strength, increases the oxygen supply capacity of the body and improves metabolic efficiency. Consequently, oxygen utilization during exercise becomes more efficient, enhancing respiratory endurance and control.
This study examined the qualitative effects of a lumbar stabilization exercise program using respiratory resistance on older adults with LBP aged 65 and above. The program provides multiple benefits, including pain management through muscle strengthening and relaxation, improved motor function through enhanced physical abilities, decreased stress and anxiety through psychosocial benefits and enhanced respiratory function. Nevertheless, some limitations should be considered. First, the participant characteristics require further consideration. As the average age of the participants was 67 years, variations in respiratory improvement may occur depending on age, gender, and the severity of LBP. This condition highlights the need for additional studies on a broader patient population. Second, the long-term effects of the program require further examination. Respiratory resistance training may temporarily improve respiratory function; additional research is needed to determine if these improvements are sustained over time. Future studies that address these limitations would provide more effective and individualized exercise methods for patients with diverse types of LBP. Hence, this could help patients achieve better treatment outcomes, ultimately contributing to an improved quality of life.
Conclusion
This study examined the effects of a lumbar stabilization exercise program using respiratory resistance on pain, motor function, psychosocial factors, and respiratory function in patients aged 65 and older with LBP. The findings suggest that the experimental group, who participated in lumbar stabilization exercises using respiratory resistance, showed significant improvements in their pain levels, motor, and respiratory functions. Based on these results, the lumbar stabilization exercise program incorporating respiratory resistance can effectively reduce pain, enhance motor function, and improve respiratory function in patients aged 65 and older with LBP.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Research Ethics Committee of Sehan University, Yeongam, Republic of Korea (Code: SH-IRB 2024-014). Informed written consent was obtained from all participants after explaining the research project’s purpose.
Funding
This study was financially supported by Sehan University, Yeongam, Republic of Korea.
Authors' contributions
Data collection, review and editing: Sam-Ho Park; Study design, statistical analysis, writing the original draft, conceptualization and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors acknowledge the Sehan University Research fund.
References
Modern society has entered an aging era because of advances in medical technology and extending life expectancy, which brings various social and economic challenges [1]. As aging progresses, the body functions gradually decline across various systems, with musculoskeletal degeneration leading to reduced motor function and muscle mass loss. In addition, the prevalence of low back pain (LBP) tends to increase with aging, with studies reporting that approximately 50% of older adults experience LBP at some point in their lives [2, 3]. Previous research has highlighted various interventions, including exercise therapy and lifestyle modifications, to mitigate LBP in older people [4, 5].
Physical changes associated with aging lead to the degeneration of muscles and bones, reducing physical activity and setting a cycle of decline [6]. Physical changes associated with aging lead to the degeneration of muscles and bones, reducing physical activity and setting a cycle of decline [6]. In South Korea, the prevalence of LBP among the elderly population is reported to be approximately 40%–50%, with a higher incidence observed in women than in men [7]. Additionally, a national health survey indicates that musculoskeletal disorders, including LBP, are among the leading causes of outpatient visits among older adults, accounting for a significant proportion of medical consultations [8]. For older adults, reduced activity signifies weakened physical function, adversely affecting their social engagement, relationships, and quality of life. In older adults with chronic LBP, higher levels of pain are often associated with reduced physical activity, leading to psychological issues such as depression and anxiety [9].
Among the interventions to reduce pain, restore functional ability, improve balance, and support spinal alignment in patients with LBP, lumbar stabilization exercise is used widely in clinical settings [10]. This method enhances lumbar stability by strengthening deep muscles. These exercises improve segmental control, reduce functional disability and enhance coordination. Additionally, they raise intra-abdominal pressure, support spinal alignment and strengthen abdominal muscles, reducing lumbar pressure. Engaging both abdominal and pelvic muscles also improves balance [11].
The abdominal drawing-in maneuver (ADIM) induces contractions of the diaphragm and transversus abdominis through abdominal hollowing and diaphragmatic breathing, increasing intra-abdominal pressure and effectively supporting lumbar stabilization [12]. Deep muscle contraction is crucial for providing stability to the lumbar segments. Various breathing techniques that promote contractions of the transversus abdominis and diaphragm were applied to maximize the effects of lumbar stabilization exercises for patients with LBP [13, 14]. Among these, lumbar stabilization exercises using respiratory resistance enhance stability by harmonizing the diaphragmatic and transversus abdominis muscle activity, increasing intra-abdominal pressure, and inducing a contraction of the spinal surrounding muscles [13, 14].
Previous studies have shown that lumbar stabilization exercises with respiratory resistance training can reduce pain and improve function in patients with lumbar instability and middle-aged women with LBP. However, research specifically targeting older adults with LBP and the role of breathing in their rehabilitation remains limited. Therefore, this study examined the effects of a lumbar stabilization exercise program using respiratory resistance on pain, motor function, psychosocial factors, and respiratory function in patients with LBP aged 65 years and older. Unlike previous research that assessed these interventions separately, this study evaluates their combined impact, addressing a key gap in the literature.
Methods
Study participants
This study included 53 patients receiving inpatient or outpatient care for LBP at Seongsim Geriatric Hospital, Mokpo, Republic of Korea. The total intervention period was from September 2024 to February 2025. The inclusion criteria were as follows: Aged 65 and older, experience of LBP within the past six weeks, and a quadruple visual analog scale (QVAS) score of 3 or higher [15]. The exclusion criteria included LBP caused by fractures and respiratory conditions that would hinder participation in the intervention.
Study design
This study used a pre-test, post-test design with a control group with random assignment. The sample size was determined using G*Power software, version 3.1.9.7 (Heinrich Heine University, Düsseldorf, Germany). Based on the main effect size (d) of 0.88 from Park and Lee [13], a significance level (α) of 0.05 and a power (1-β) of 0.80, a minimum of 22 participants per group was required, with an additional 10% to account for potential dropouts, resulting in a target of 24 participants per group [16]. Of the 53 patients recruited, five declined to participate, leaving a final sample of 48 who completed a pre-test and were randomly assigned to either the experimental or control group. Randomization was conducted using an internet-based program (Research Randomizer) [17], assigning the participants to the experimental group (n=24) and control group (n=24).
The experimental group performed a lumbar stabilization exercise program combined with respiratory resistance training, whereas the control group performed only a lumbar stabilization exercise program. Each session included a 5-minute warm-up and cooldown stretch, with approximately 45 minutes per session, thrice a week over six weeks. The program effectiveness was evaluated by taking QVAS, the Korean version of the Oswestry disability index (K-ODI), balance ability, Euro quality of life 5 dimension (EQ-5D) and pulmonary function test (PFT) measurements before and after the intervention. The research flowchart is shown in Figure 1.
Study interventions
Lumbar stabilization exercise program
The lumbar stabilization exercise provided to both groups was a modified and supplemented version of the intervention method reported by Park and Lee [13]. The lumbar stabilization exercise program included movements designed to enhance deep muscle activation and promote balance and coordination of muscles surrounding the lumbar region: Curl-up, dead bug, bridge, and bridge with knee extension (Figure 2). Each movement was performed for 15 seconds, repeated 10 times per set, for three sets, with a 20 second rest between sets.
Lumbar stabilization exercise program using respiratory resistance
The experimental group performed breathing resistance training simultaneously with the lumbar stabilization exercise program. Before the intervention, the participants were provided with individualized respiratory resistance devices and were instructed on the operation and diaphragmatic breathing techniques. The respiratory resistance device (Expand-a-Lung, Miami, USA) consisted of a silicone mouthpiece and a main body that allowed airflow control, introducing resistance during inhalation and exhalation to strengthen the respiratory muscles.
During training, the resistance level was adjusted to maintain a rating of perceived exertion of 14 or lower, and participants were pre-informed about possible symptoms such as dizziness, nausea, vomiting, or difficulty breathing [18]. Medical equipment for monitoring body temperature, pulse, respiration, and blood pressure was prepared to cease intervention for adverse symptoms.
Assessment methods
Pain
The pain level of the participants before and after the intervention was assessed using the QVAS. This tool included four items: 1) Current pain, 2) Usual pain, 3) Least pain and 4) Worst pain. Each item was scored on a scale from 0 cm, indicating no pain, to 10 cm, indicating the most severe pain. The average score of the four items was calculated to quantify the pain levels. This tool had an intrarater reliability of r=0.76–0.84, indicating a high level of reliability [19].
Functional ability
The level of functional disability before and after the intervention was measured using the K-ODI. This questionnaire comprised 10 items, with higher scores indicating greater functional disability. The item on sexual activity was excluded, reflecting the cultural considerations in Korea, leaving nine items with a maximum score of 45. The K-ODI demonstrated high test, re-test reliability (r=0.92) [20]. Additionally, its content validity was confirmed through the content validity index (CVI) and content validity ratio (CVR), while internal consistency was assessed using the Cronbach α.
Balance ability
The participants’ balance ability was assessed using the Berg balance scale (BBS) before and after the intervention. The BBS measures static and dynamic balance, comprising 14 items across three domains: Sitting, standing, and posture changes. Each item was rated on a 5-point scale from 0 to 4, with a maximum total score of 56. The BBS demonstrated excellent reliability, with an intrarater reliability of r=0.99 and interrater reliability of r=0.98 [21]. Its validity was supported by the CVI and CVR, and internal consistency was confirmed with a high Cronbach α score.
Quality of life
The participants’ quality of life was evaluated before and after the intervention using the EQ-5D, a widely used tool in healthcare. This instrument assesses five domains: Self-care, mobility, usual activities, anxiety/depression, and pain/discomfort. Each domain is rated at three levels to reflect health status, with the EQ-5D demonstrating high reliability (r=0.87) [22]. The CVI and CVR have supported their validity, while internal consistency was confirmed with a high Cronbach’s α score.
Pulmonary function
The MicroQuark device (COSMED, Rome, Italy) assessed the pulmonary function after inputting each participant’s sex, age, and physical characteristics. The measurements were taken with the participants standing upright, their noses pinched, and biting down on the mouthpiece attached to the MicroQuark.
After maximal inhalation and forced exhalation, the total amount of emitted air is assigned as the forced vital capacity (FVC), and forced expiratory volume (FEV) for 1 s was set as FEV1. The two values were then used to derive the FEV1/FEV ratio (FEV1%) and the amount of ventilated air for 15 s at the fastest speed was converted to the amount in one minute to determine the maximal voluntary ventilation (MVV). A physical therapist with substantial experience in pulmonary function testing assessed three trials, and the values were used for analysis. A 10-minute break was allowed between each test.
Statistical analysis
Data were analyzed using SPSS software, version 21, IBM. The participants’ general characteristics are presented using descriptive statistics, including Mean±SD. The Shapiro-Wilk test was used to assess normality. A chi-square test was performed to analyze the participants’ gender, while a t-test was conducted to analyze the homogeneity of the other general characteristics and pre-test values. The independent samples t-test was used to compare the changes between the two groups before and after the intervention. The paired samples t-test was used to compare the changes in dependent variables before and after the intervention within groups. The statistical significance level (α) was set at 0.05.
Results
Seven patients were excluded from the experimental and control groups because they refused to participate, and the data from the experiment (n=21) and control (n=20) groups were collected. The general characteristics were similar in the two groups (Table 1).
QVAS, K-ODI, BBS and EQ-5D results showed no significant difference between the two groups before the intervention. However, both groups showed significant improvement after the intervention (P<0.05). Furthermore, the experimental group showed better results in QVAS, K-ODI, BBS and EQ-5D scores than the control group (P<0.05) (Table 2).
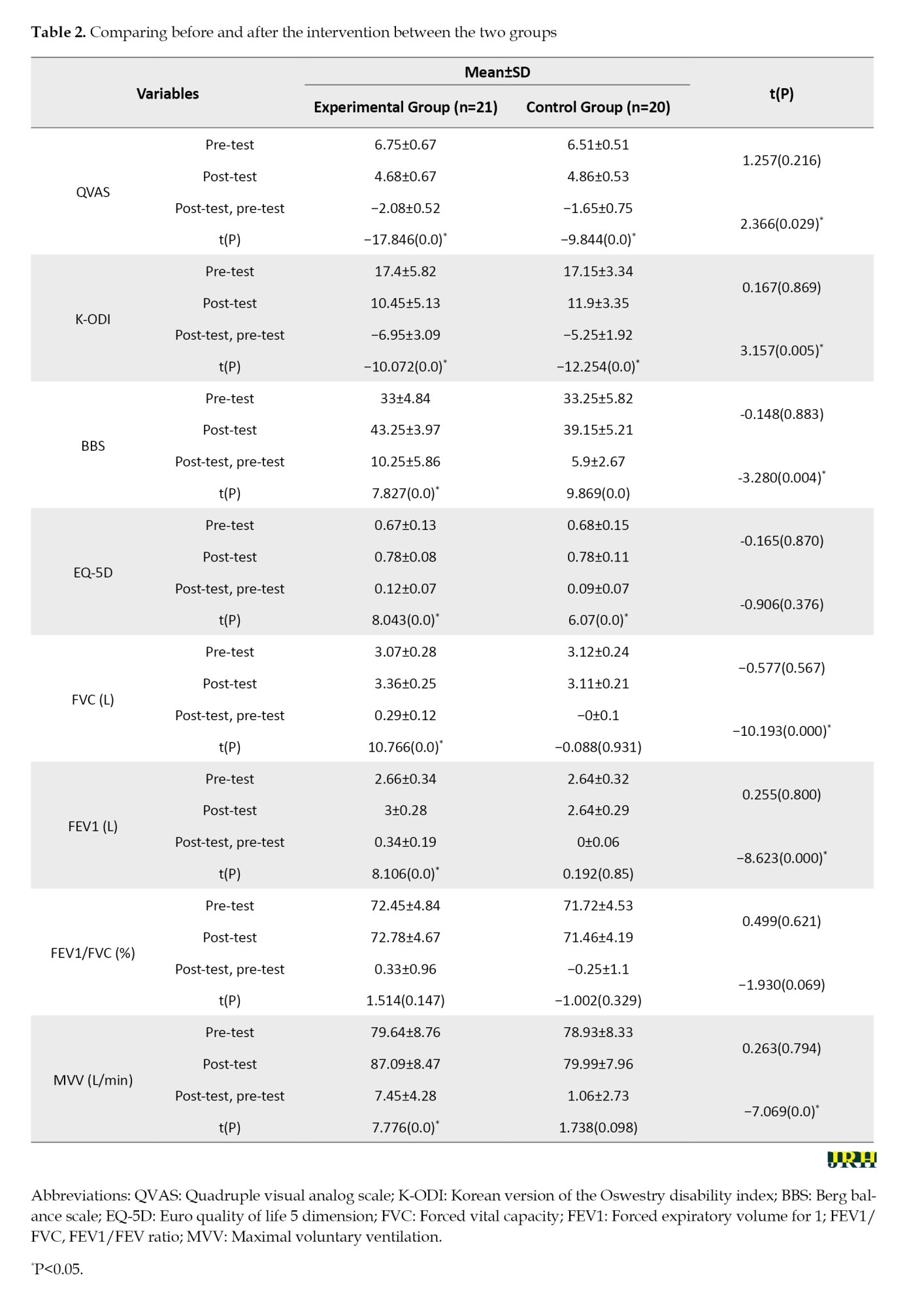
The FVC, FEV1 and MVV values were similar in the two groups before the intervention. A significant difference in the FVC, FEV1 and MVV was observed in the experimental group before and after the intervention (P<0.05). Also, a significant difference in the level of change was noted between the two groups (P<0.05) (Table 2).
Discussion
This study examined the effects of a lumbar stabilization exercise program using the respiratory resistance on pain, motor function, psychosocial factors, and respiratory function in patients aged 65 and older with LBP. The results revealed significant differences in the QVAS, K-ODI, BBS and EQ-5D scores among all study participants. In addition, the experimental group that underwent the lumbar stabilization exercise program using respiratory resistance exhibited significant differences in the changes observed in the QVAS, K-ODI, BBS, FVC, FEV1, and MVV.
Physical pain is one of the most commonly reported health issues among elderly individuals. Physical pain can lead to problems in motor function and physical, mental, and social issues [23]. Among these, LBP is a condition with a high prevalence, particularly requiring more management in the elderly population. Ge et al. [24] applied a core stability training program for four weeks to individuals aged 60 years and older with LBP, reporting significant improvement in pain levels (effect size: 1.72, P<0.05). Park et al. [10] examined women over 40 years with LBP, applying a stabilization exercise program using respiratory resistance for four weeks, also noting a significant improvement in the pain levels (effect size: 5.21, P<0.05). All participants showed significant improvement in the pain levels before and after the intervention (P<0.05). Furthermore, the experimental group that engaged in the lumbar stabilization exercise program using respiratory resistance showed differences from the control group (effect size: 0.84, P<0.05). Hence, breathing exercises, such as deep breathing, may activate the parasympathetic nervous system, helping to relieve tension and decrease pain sensitivity.
Older adults aged 65 years and above commonly experience musculoskeletal weakness and decline in motor function. Training combined with respiratory resistance offers a relatively low-intensity exercise approach that can safely and effectively aid in pain management. Ge et al. [24]. implemented a four-week core stability training program for individuals aged 60 years and older with LBP, reporting significant improvements in functional disability (effect size: 1.47) and dynamic balance ability (effect size: 2.07, P<0.05). Seo and Lee [25] applied a four-week stabilization exercise program with whole-body vibration in a population of individuals aged 75 and above, observing significant improvements in the static balance (effect size: −2.14) and dynamic balance (effect size: 1.27, P<0.05). Similarly, in this study, all participants showed significant improvement in the motor function levels before and after the intervention (P<0.05), and the experimental group who performed lumbar stabilization exercises using respiratory resistance exhibited significant differences compared to the control group (K-ODI effect size: 1.27, BBS effect size: −2.32). These findings suggest that respiratory resistance training activates the abdominal and thoracic muscles, contributing to the stabilization of spinal muscles by strengthening deep muscles. In particular, respiratory training may play a key role in enhancing motor function in older adults, where muscle weakness affects posture and body stability.
Respiratory resistance training activates the parasympathetic nervous system through deep breathing, reducing stress and tension [26]. This activation provides psychological stability and may help to alleviate anxiety related to pain in elderly individuals with LBP [27]. Park et al. [10] reported that a stabilization exercise program using respiratory resistance significantly improved the psychosocial aspects of physical activity (effect size: 3.02) and work (effect size: 2.87) in middle-aged women with LBP (P<0.05). Similarly, this study revealed significant improvement in the psychosocial levels before and after the intervention among all participants (P<0.05), even though no significant difference was found between the two groups (experimental group effect size: −0.45, control group effect size: −0.35). Although respiratory resistance training and lumbar stabilization exercises take different approaches, both exercise have a common positive impact on psychological states. For older adults, engaging in exercise promotes social interactions, improves confidence through participation in activities, reduces social isolation, and contributes to psychological stability.
Respiratory resistance training is essential for improving breathing efficiency and activating the muscles surrounding the spine. In older adults, decreased respiratory function, reduced muscle strength, and diminished flexibility can exacerbate LBP, highlighting a need for respiratory resistance training as part of a comprehensive management approach [10, 12-14]. Park and Lee [13] reported that a stabilization exercise program using respiratory resistance significantly improved the respiratory function in patients with lumbar instability (FVC effect size: −0.23, FEV1 effect size: −0.23, MVV effect size: −0.88). In addition, Oh et al. [12] reported significant improvements in the respiratory function in middle-aged women with LBP who performed ADIM lumbar stabilization exercises with respiratory resistance (FVC effect size: −0.52, FEV1 effect size: −0.35, MVV effect size: −1.14). Similarly, in this study, only the experimental group performing lumbar stabilization exercises using respiratory resistance showed significant improvements in the respiratory function (FVC effect size: −1.09, FEV1 effect size: −1.09, MVV effect size: −0.86). This finding suggests that training with respiratory resistance enhances the respiratory muscle strength, increases the oxygen supply capacity of the body and improves metabolic efficiency. Consequently, oxygen utilization during exercise becomes more efficient, enhancing respiratory endurance and control.
This study examined the qualitative effects of a lumbar stabilization exercise program using respiratory resistance on older adults with LBP aged 65 and above. The program provides multiple benefits, including pain management through muscle strengthening and relaxation, improved motor function through enhanced physical abilities, decreased stress and anxiety through psychosocial benefits and enhanced respiratory function. Nevertheless, some limitations should be considered. First, the participant characteristics require further consideration. As the average age of the participants was 67 years, variations in respiratory improvement may occur depending on age, gender, and the severity of LBP. This condition highlights the need for additional studies on a broader patient population. Second, the long-term effects of the program require further examination. Respiratory resistance training may temporarily improve respiratory function; additional research is needed to determine if these improvements are sustained over time. Future studies that address these limitations would provide more effective and individualized exercise methods for patients with diverse types of LBP. Hence, this could help patients achieve better treatment outcomes, ultimately contributing to an improved quality of life.
Conclusion
This study examined the effects of a lumbar stabilization exercise program using respiratory resistance on pain, motor function, psychosocial factors, and respiratory function in patients aged 65 and older with LBP. The findings suggest that the experimental group, who participated in lumbar stabilization exercises using respiratory resistance, showed significant improvements in their pain levels, motor, and respiratory functions. Based on these results, the lumbar stabilization exercise program incorporating respiratory resistance can effectively reduce pain, enhance motor function, and improve respiratory function in patients aged 65 and older with LBP.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Research Ethics Committee of Sehan University, Yeongam, Republic of Korea (Code: SH-IRB 2024-014). Informed written consent was obtained from all participants after explaining the research project’s purpose.
Funding
This study was financially supported by Sehan University, Yeongam, Republic of Korea.
Authors' contributions
Data collection, review and editing: Sam-Ho Park; Study design, statistical analysis, writing the original draft, conceptualization and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors acknowledge the Sehan University Research fund.
References
- Wettstein M, Wahl HW, Siebert J, Schröder J. Still more to learn about late-life cognitive development: How personality and health predict 20-year cognitive trajectories. Psychology and Aging. 2019; 34(5):714-28. [DOI:10.1037/pag0000374] [PMID]
- Frontera WR. Physiologic changes of the musculoskeletal system with aging: A brief review. Physical Medicine and Rehabilitation Clinics of North America. 2017; 28(4):705-11. [DOI:10.1016/j.pmr.2017.06.004] [PMID]
- Meucci RD, Fassa AG, Faria NM. Prevalence of chronic low back pain: Systematic review. Revista de Saude Publica. 2015; 49:1. [DOI:10.1590/S0034-8910.2015049005874] [PMID] [PMCID]
- Pennington E, Bell S, Hill JE. Should video laryngoscopy or direct laryngoscopy be used for adults undergoing endotracheal intubation in the pre-hospital setting? A critical appraisal of a systematic review. Journal of Paramedic Practice. 2023; 15(6):255-9. [DOI:10.1002/14651858] [PMID] [PMCID]
- Bekkering GE, Hendriks HJM, Koes BW, Oostendorp RAB, Ostelo RWJG, Thomassen JMC, et al. Dutch physiotherapy guidelines for low back pain. Physiotherapy. 2003; 82-96. [DOI:10.1016/S0031-9406(05)60579-2]
- Harridge SD, Lazarus NR. Physical activity, aging, and physiological function. Physiology. 32(2):152-61. [DOI:10.1152/physiol.00029.2016] [PMID]
- Cho JH, Lee KH, Lim ST. Aged lumbar extension strength of chronic low back pain in Korean population of 10-80 years. Iranian Journal of Public Health. 2020; 49(10):1894-901. [DOI:10.18502/ijph.v49i10.4692]
- Park SY, Jung YH, Park JS, Shin JY, Jang SI. Association between age and glycemic control of adult diabetics in Korea: A cross-sectional study based on KNHANES 2013-2021. 2024; [Unpublished]. [DOI:10.21203/rs.3.rs-4238160/v1]
- Hicks GE, Simonsick EM, Harris TB, Newman AB, Weiner DK, Nevitt MA, et al. Cross-sectional associations between trunk muscle composition, back pain, and physical function in the health, aging and body composition study. The Journals of Gerontology. Series A. 2005; 60(7):882-7. [DOI:10.1093/gerona/60.7.882] [PMID]
- Park SH, Oh YJ, Jung SH, Lee MM. The effects of lumbar stabilization exercise program using respiratory resistance on pain, dysfunction, psychosocial factor, respiratory pressure in female patients in’40s with low back pain: Randomized controlled trial. Annals of Applied Sport Science. 2021; 9(3):1-10. [DOI:10.52547/aassjournal.937]
- Coskun Benlidayi I, Basaran S. Comparative study of lumbosacral alignment in elderly versus young adults: Data on patients with low back pain. Aging Clinical and Experimental Research. 2015; 27(3):297-302. [DOI:10.1007/s40520-014-0274-3] [PMID]
- Oh YJ, Park SH, Lee MM. Comparison of effects of abdominal draw-in lumbar stabilization exercises with and without respiratory resistance on women with low back pain: A randomized controlled trial. Medical Science Monitor. 2020; 26:e921295. [DOI:10.12659/MSM.921295] [PMID] [PMCID]
- Park SH, Lee MM. Effects of a progressive stabilization exercise program using respiratory resistance for patients with lumbar instability: A randomized controlled trial. Medical Science Monitor. 2019; 25:1740-8. [DOI:10.12659/MSM.913036] [PMID] [PMCID]
- Park SH, Oh YJ, Seo JH, Lee MM. Effect of stabilization exercise combined with respiratory resistance and whole body vibration on patients with lumbar instability: A randomized controlled trial. Medicine. 2022; 101(46):e31843. [DOI:10.1097/MD.0000000000031843] [PMID] [PMCID]
- Mbada Ce, Akindele FF, Fatoye CT, Ademoyegun AB, Odole AC, Ogunlana MO, et al. Translation and psychometric evaluation of the yoruba version of quadruple visual analogue scale. Nigerian Journal of Health Science. 2018; 18(2):63. [DOI:10.4103/njhs.njhs_4_20]
- Faul F, Erdfelder E, Lang AG, Buchner A. G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007; 39(2):175-91. [DOI:10.3758/BF03193146] [PMID]
- Urbaniak GC, Plous S. Research randomizer, version 4.0 [Internet]. [Updated June 11]. Available from: [Link]
- Hollander DB, Durand RJ, Trynicki JL, Larock D, Castracane VD, Hebert EP, et al. RPE, pain, and physiological adjustment to concentric and eccentric contractions. Medicine and Science in Sports and Exercise. 2003; 35(6):1017-25. [DOI:10.1249/01.MSS.0000069749.13258.4E] [PMID]
- Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. International Journal of Rehabilitation Research. 2008; 31(2):165-9. [DOI:10.1097/MRR.0b013e3282fc0f93] [PMID]
- Kim DY, Lee SH, Lee HY, Lee HJ, Chung SK, Kim HJ. Validation of the Korean version of the oswestry disability index. Spine. 2005; 30(5):123-27. [DOI:10.1097/01.brs.0000157172.00635.3a]
- Bogle Thorbahn LD, Newton RA. Use of the berg balance test to predict falls in elderly persons. Physical Therapy. 1996; 76(6):576-83. [DOI:10.1093/ptj/76.6.576] [PMID]
- Devlin NJ, Brooks R. EQ-5D and the EuroQol Group: Past, present and future. Applied Health Economics and Health Policy. 2017; 15(2):127-37. [DOI:10.1007/s40258-017-0310-5] [PMID] [PMCID]
- Gregg EW, Engelgau MM, Narayan V. Complications of diabetes in elderly people. BMJ. 2002; 325(7370):916-7. [DOI:10.1136/bmj.325.7370.916] [PMID] [PMCID]
- Ge L, Huang H, Yu Q, Li Y, Li X, Li Z, et al. Effects of core stability training on older women with low back pain: A randomized controlled trial. European Review of Aging and Physical Activity. 2022; 19(1):10. [DOI:10.1186/s11556-022-00289-x] [PMID] [PMCID]
- Seo JH, Lee MM. Effects of whole body vibration exercise on the muscle strength, balance and falling efficacy of super-aged elderly: Randomized controlled trial study. Korean Society Physical Medicine. 2020; 15(1):33-42. [DOI:10.13066/kspm.2020.15.1.33]
- Kim BS, Park SH, Jung SS, Kim HJ, Woo SD, Lee MM. Validity study for clinical use of hand-held spirometer in patients with chronic obstructive pulmonary disease. Healthcare. 2024; 12(5):507. [DOI:10.3390/healthcare12050507] [PMID] [PMCID]
- Vaghela NP, Vaishnav BS, Ganjiwale JD. Effect of special breathing techniques on quality of life in elderly individuals. National Journal of Physiology Pharmacy and Pharmacology. 2019; 9(12):1185. [DOI:10.5455/njppp.2019.9.0931219092019]
Type of Study: Orginal Article |
Subject:
● Health Education
Received: 2024/12/24 | Accepted: 2025/03/5 | Published: 2025/07/1
Received: 2024/12/24 | Accepted: 2025/03/5 | Published: 2025/07/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









