Volume 13, Issue 6 (Nov & Dec 2023)
J Research Health 2023, 13(6): 391-406 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghardashi F, Akbarzadeh R, Zardosht R, Zadeh Hesari M H. Evaluation of Non-pharmacological Interventions in the Control and Treatment of Type 2 Diabetes: A Systematic Review. J Research Health 2023; 13 (6) :391-406
URL: http://jrh.gmu.ac.ir/article-1-2262-en.html
URL: http://jrh.gmu.ac.ir/article-1-2262-en.html
1- Non-communicable Diseases Research Center, School of Paramedical, Sabzevar University of Medical Sciences, Sabzevar, Iran.
2- Department of Anesthesiology, School of Allied Medical Sciences, Sabzevar University of Medical Sciences, Sabzevar, Iran.
3- Department of operative room and anesthetics, Iranian Research Center on Healthy Aging, School of paramedical, Sabzevar University of Medical Sciences, Sabzevar, Iran ,Rozardosht@yahoo.com
4- School of Allied Medical Sciences, Sabzevar University of Medical Sciences, Sabzevar, Iran.
2- Department of Anesthesiology, School of Allied Medical Sciences, Sabzevar University of Medical Sciences, Sabzevar, Iran.
3- Department of operative room and anesthetics, Iranian Research Center on Healthy Aging, School of paramedical, Sabzevar University of Medical Sciences, Sabzevar, Iran ,
4- School of Allied Medical Sciences, Sabzevar University of Medical Sciences, Sabzevar, Iran.
Full-Text [PDF 779 kb]
(1205 Downloads)
| Abstract (HTML) (3071 Views)
Full-Text: (1482 Views)
1. Introduction
Diabetes is one of the most critical health challenges worldwide. During the past three decades, the number of diabetic cases has increased more than twofold [1, 2]. The prevalence of vulnerability to diabetes is growing rapidly and will reach approximately 625 million people in all quarters of the globe by 2045 [3]. According to the estimations by the international diabetes federation in the year 2015, about 75% of adult diabetics are living in low-income countries [4]. Some risk factors of vulnerability to type 2 diabetes are unchanging, such as age and family background; however, other risk factors, such as weight gain, blood sugar, and triglyceride, change dramatically with lifestyle correction [5]. Monitoring the metabolic indicators, such as blood pressure, body weight, blood sugar, HbA1c, and lipid, is imperative for managing diabetics [6]. Studies have shown that pharmaceutical interventions and lifestyle modification can effectively control Hyperglycemia [7]. Correcting the lifestyle and mood factors, self-confidence, and social support can save pre-diabetics from the risk of vulnerability to this illness [8, 9]. About 50% to 80% of the people with diabetes have no adequate skills and knowledge of self-care and illness management [10]. Numerous studies have demonstrated that healthcare strategies engaging the diabetics' family members cause higher awareness and self-efficacy concerning self-care in patients with diabetes [11]. In recent years, the US and UK diabetes associations have confirmed the effect of a low carbohydrate diet in lowering weight and improving blood glucose and lipid regulation in mellitus diabetics [12, 13]. Combinatorial diet programs and physical activity promotion plans may hinder and delay the progress of type 2 diabetes [14-17]. Disease management programs have introduced particular instructions as the best strategy for diabetes prevention in which the increase in physical activity [18, 19], decrease of consumable calories, and training of patients together with the support by peer groups are among the most crucial disease management programs [20-26]. Despite the variety and frequency of the interventions to control and treat type 2 diabetes in different countries, the knowledge and awareness of the methods and the relevant consequences are crucial for the science community. They can be counted as a decisive step toward promoting this science. A systematic review is a comprehensive study based on a predetermined and accurate protocol. Many studies do not have good interpretive power for various reasons; however, the systematic review and meta-analysis that often follows will combine studies to reach a larger sample size; therefore, they can be examined with greater power and ultimately provide better conclusions. Accordingly, this study aims to determine effective non-pharmacological interventions in controlling and treating type 2 diabetes by systematic review method. This study has been conducted to find answers to the following questions:
1) What are the types of non-pharmacological interventions used in intervention studies to control or treat type 2 diabetes?
2) Which non-pharmacological intervention is primarily recommended in controlling or treating type 2 diabetes in intervention studies?
3) What have been the outcomes of non-pharmacological interventions in controlling or treating type 2 diabetes?
2. Methods
This study is a systematic review of the papers published on the non-pharmaceutical intervention arrangements in controlling and treating patients with type 2 diabetes. The authors have used the standard systematic review guideline (PRISMA), including 27 items [27].
The search included the electronic data banks, including Medline, Science Direct, Embase, Scopus, Cochrane Library, and the Google Scholar search engine. The main selected keywords were as follows: “Clinical trial,” “treatment,” “type-2 diabetes,” and “control.” Their equivalents were also searched in MeSH: “NIDDM” and “diabetes mellitus.” The words “AND” and “OR” were used to combine the keywords. Searching was restricted to all relevant English papers published and indexed from June 2014 to the end of 2020.
Inclusion criteria
The inclusion criteria of selected papers were from scientific research journals, the language of the paper was in English, and the documents were full-text papers. The criteria for selecting articles were as follows: Type of participants=type 2 diabetes, type of interventions=non-pharmaceutical interventions, type of comparator=intervention performed, type of outcome=control or treatment, study type=clinical trial or empirical.
Exclusion criteria
The exclusion criteria of papers were inaccessibility to the full text, letters to the editors, and exclusively descriptive and review papers.
Data extraction, variables, and data analysis
A researcher-made data extraction form based on the study objective was used to analyze the papers. This form included parts of the article details, including the authors’ names, publication year, paper’s objective, study design, study methodology, information relevant to type 2 diabetes, and final results and outputs. Two researchers were involved in the selection work and data extraction activities. The main features of the studies and their results have been summarized considering the following variables:
Type of study: The papers from clinical trials or empirical studies were selected.
Target population: The patients with type 2 diabetes and gestational diabetes (GDM).
Types of interventions
Types of interventions in this study were classified into four categories, namely “lifestyle,” “education,” “traditional treatment,” and “Treatment devices,” based on the World Health Organization (WHO) interventions category guidelines [28], and the study objectives that embraced only the non-pharmaceutical interventions.
Two reviewers worked independently to determine whether a study met the inclusion criteria. They collected information to assess each study's methodological validity (degree of protection against confounding and bias). They also extracted data from the included studies using structured and standardized data extraction forms. The reviewers resolved discrepancies by jointly reviewing any study in question. A third reviewer would enter as an external peer reviewer if no consensus were reached. The third author was unaware of the other reviewers’ determinations and functioned as an arbitrator.
3. Results
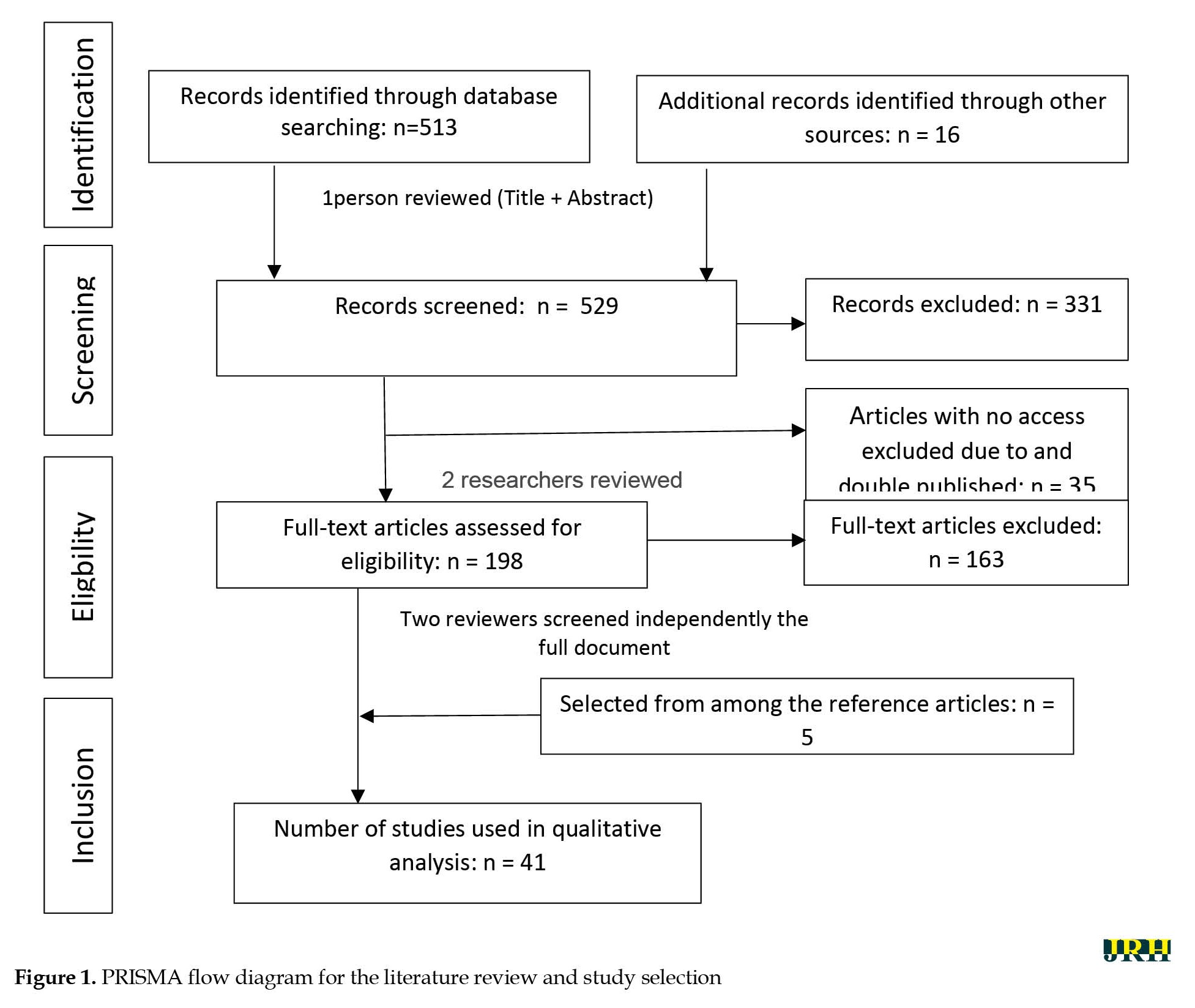
Searching of the data sources was performed for two months based on the keywords and searching strategies, and a total of 41 papers were selected from 529 articles after three selection steps. The authors systematically considered the title and abstract of all papers in the indices in the first step based on the relevancy to the study subject in addition to the inclusion and exclusion criteria. Accordingly, a total of 198 articles were entered into the study. Meanwhile, 35 articles were excluded from the study due to inaccessibility to the full text or duplication (indexed in different sites). An expert panel thoroughly analyzed the remaining articles (n=163) with two expert reviewers (after a full-text reading of the articles). Eventually, 68 articles with more comprehensive and relevant information were selected. The full text of the above 68 papers was then handed to two independent expert authors, and finally, 36 articles were selected. Then, 5 articles were added from among the articles’ references, and 41 papers were selected. The flow chart of article selection is presented in Figure 1. Table 1 represents the main features of the selected articles in addition to their aims and results.
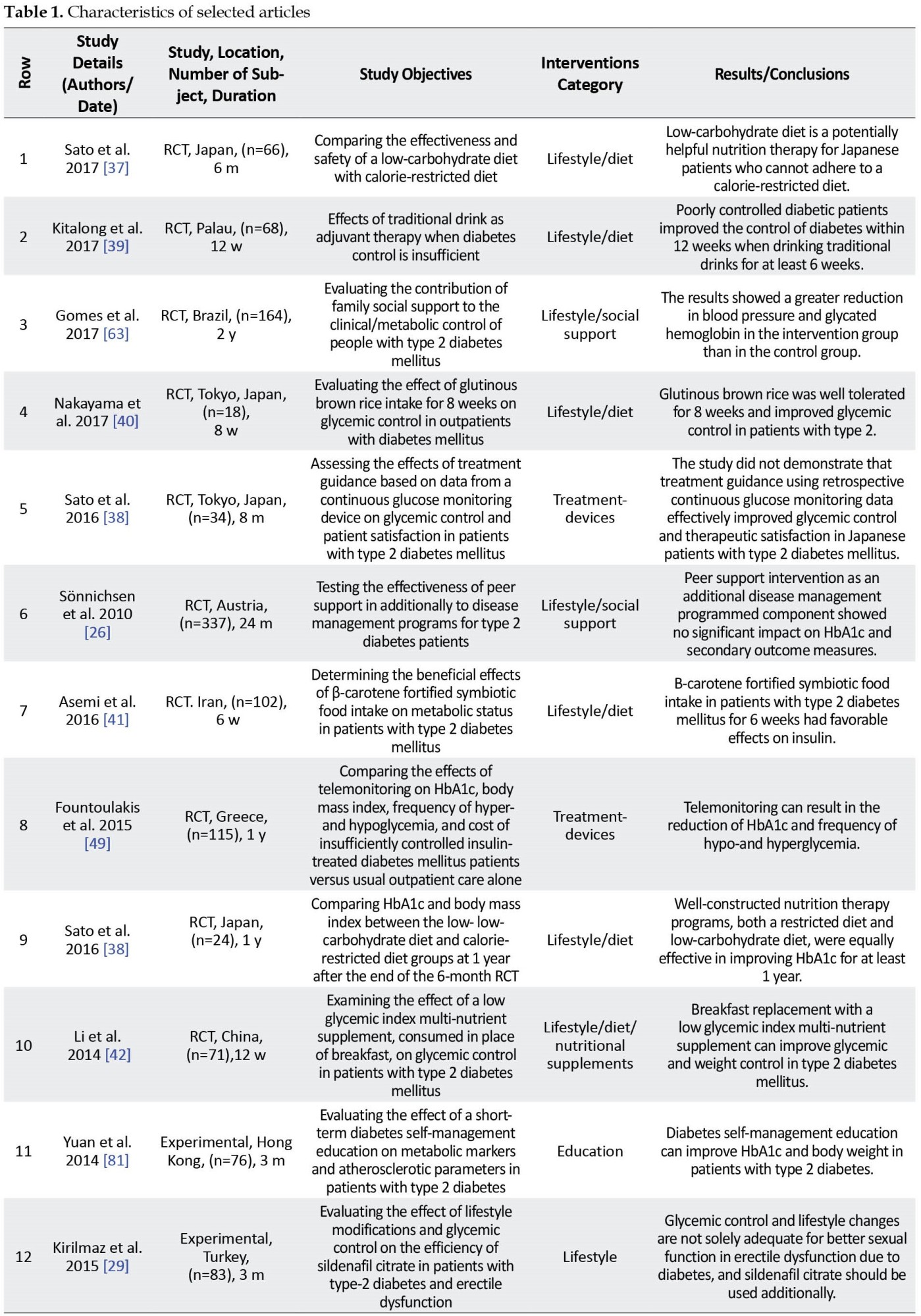
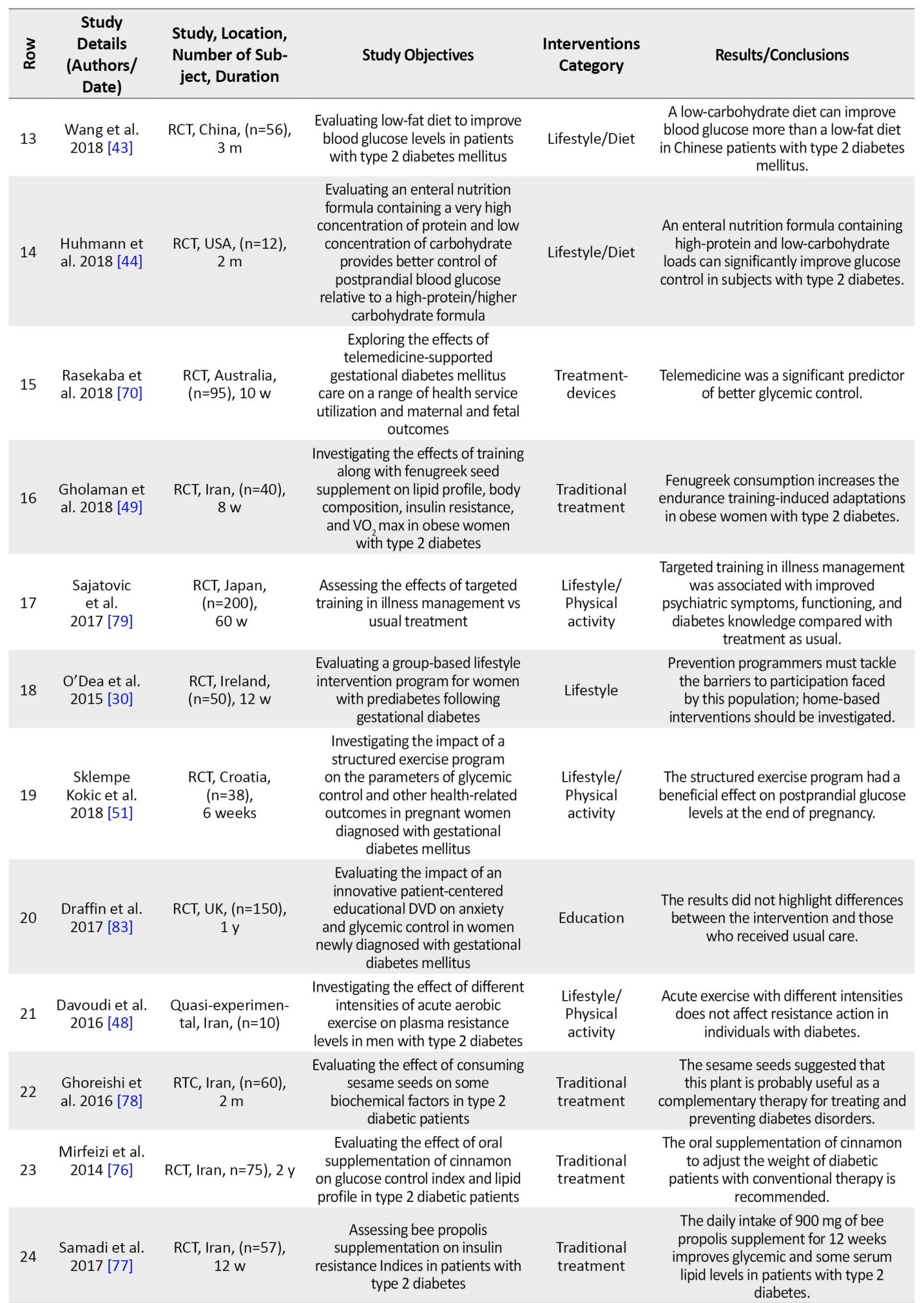
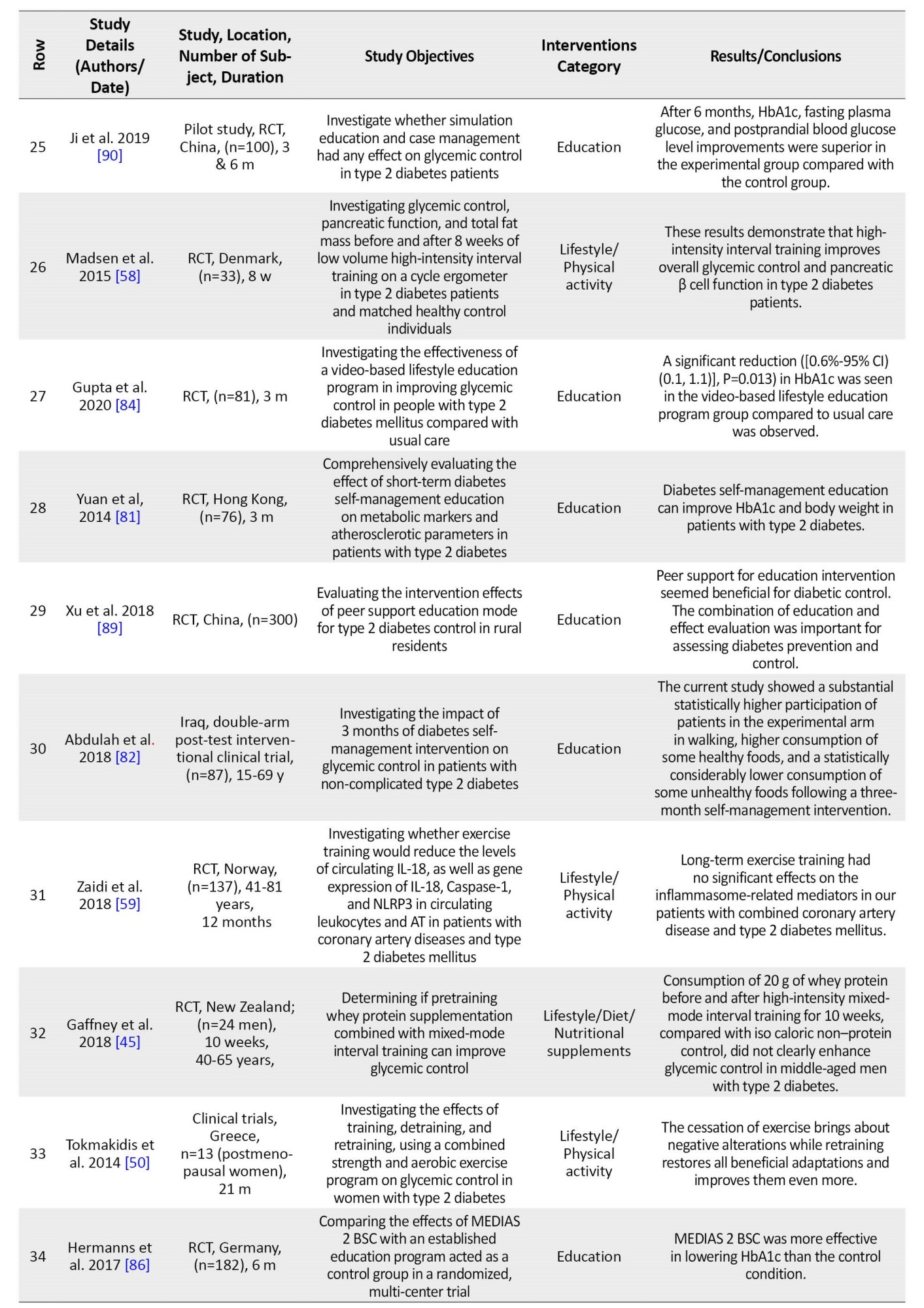
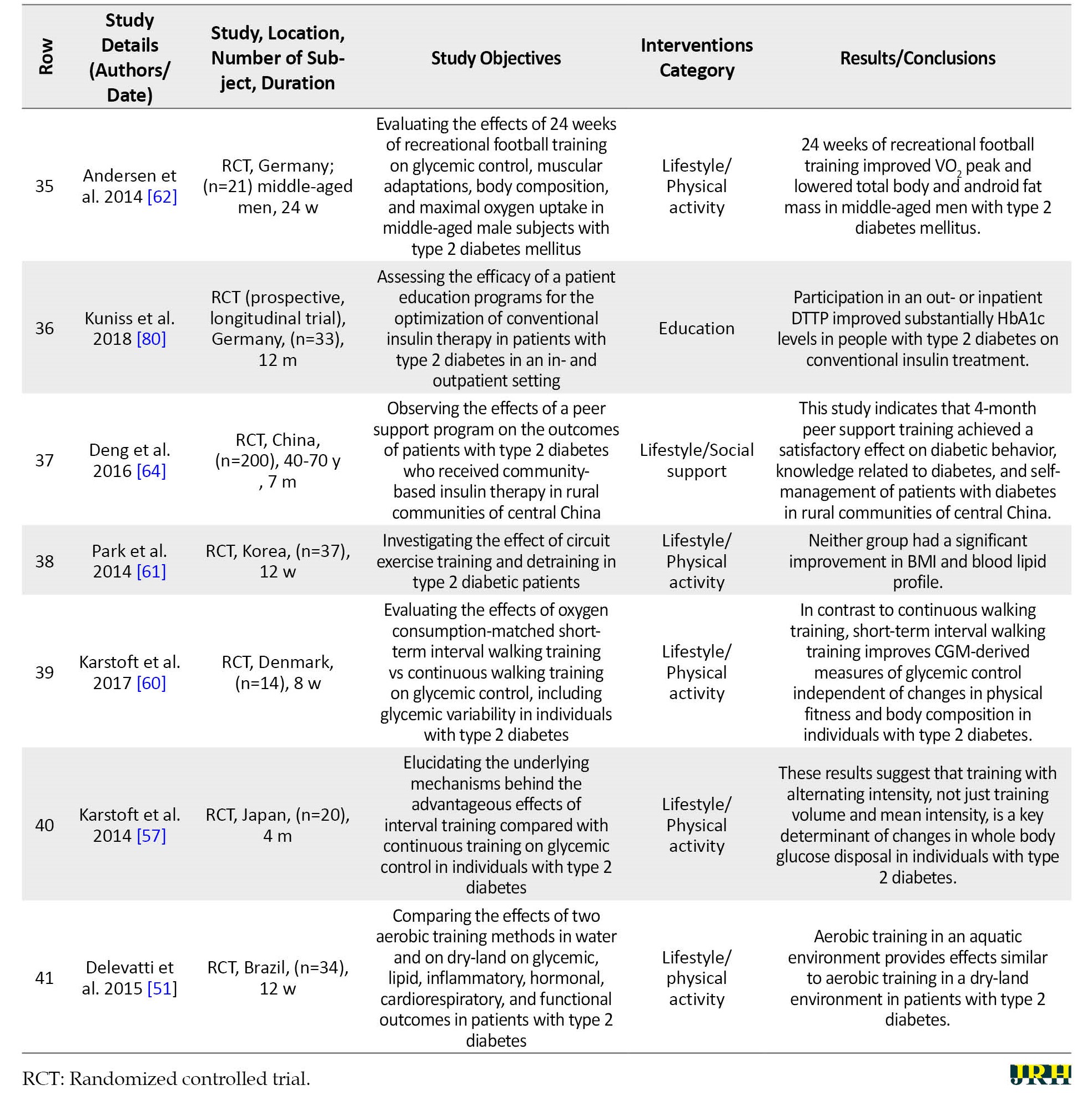
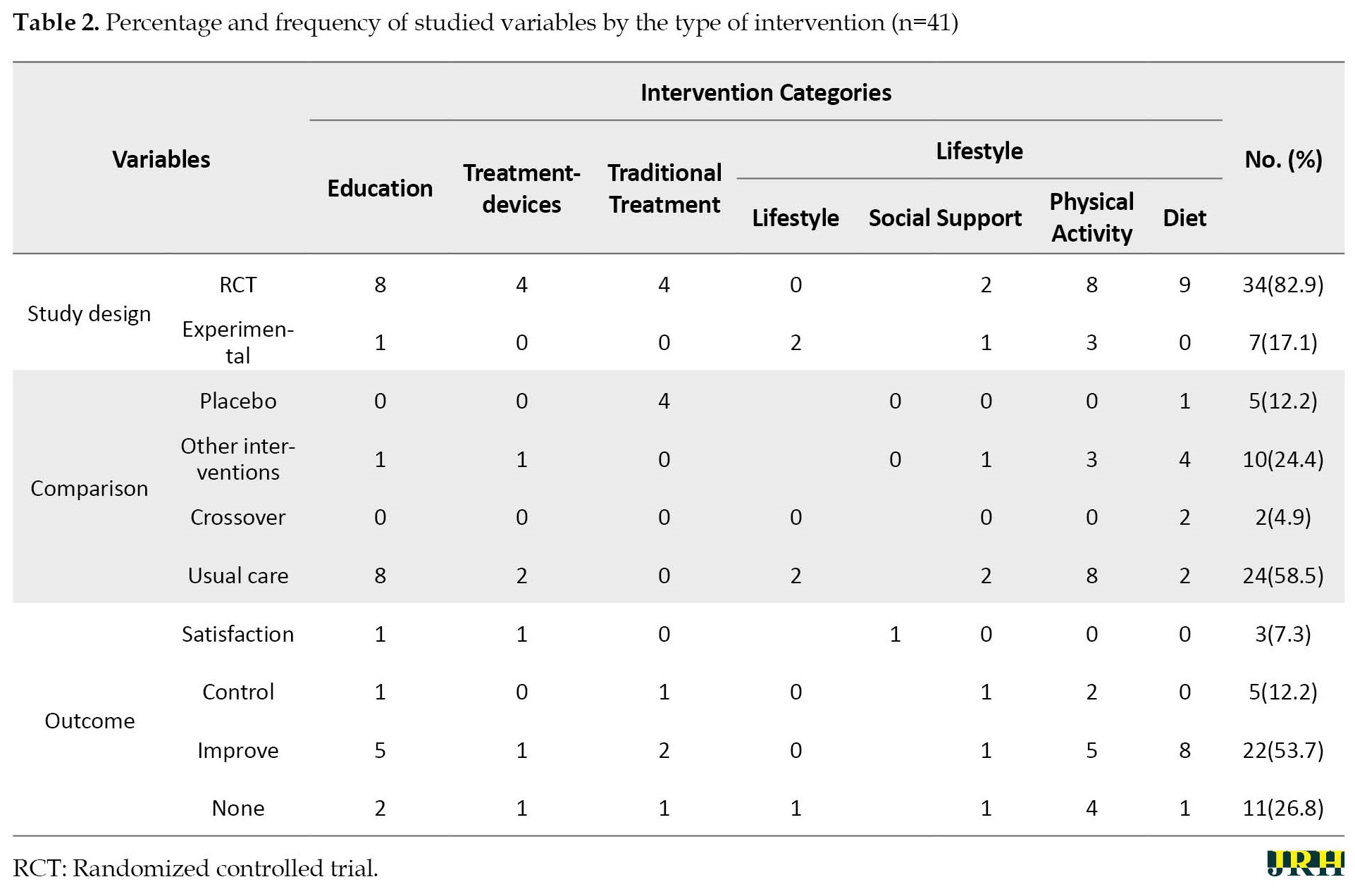
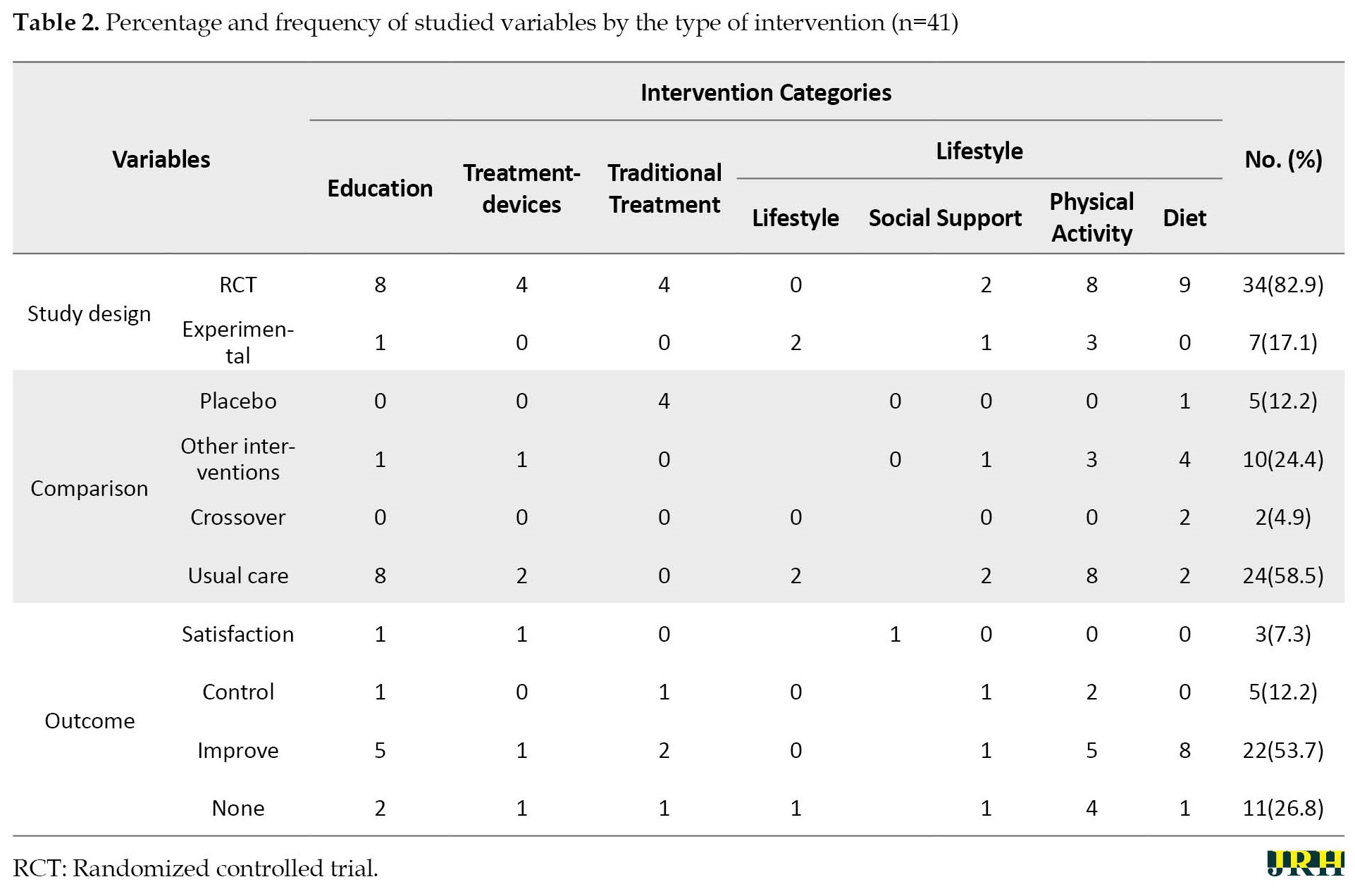
The result indicated that the above 41 selected articles were from the outcome of studies performed in 21 different countries. Most of the randomized controlled trial (RCT) studies (82.9%) and interventions were related to lifestyle (61%). Meanwhile, most studies (53.7%) represented an improvement in the patient’s status and a decrease in HbA1c, while the reduction of HbA1c accompanied the outcome of most diet intervention studies (88.9%). The percentage and frequency of the under-study variables in terms of the type of study, type of intervention, the comparison group, and the interventions’ outcomes are shown in Table 2.
In response to the first question of the study:
1) What are the types of non-pharmacological interventions used in intervention studies to control or treat type 2 diabetes?
In the present study, it was determined that the researchers had used the interventions, such as “changing the lifestyle (diet, physical activity, and social support),” “treatment devices,” “treatment-other,” “traditional treatment,” and other interventions (education).
In response to the second and third questions of the study:
2) In intervention studies, which non-pharmacological intervention is most recommended in controlling or treating type 2 diabetes?
3) What have been the outcomes of non-pharmacological interventions in controlling or treating type 2 diabetes?
Most non-pharmacological intervention to control and improve type 2 diabetes was related to lifestyle (60.9%), although only 4.9% of the studies had investigated all lifestyle elements. Among the lifestyle variables, the highest frequency was diet and nutritional supplements (19.5%). Subsequently, physical activity (26.8%) and social support (7.3%) had the highest frequencies, respectively.
About 65.9% of interventions resulted in controlling and improving blood sugar and decreasing HbA1c. Meanwhile, 7.3% of the studies represented satisfaction and increased patients’ quality of life; only 26.8% showed no significant statistical result. The study's results also demonstrated that all diet-related interventions produced the outcome of better control and improvement of blood sugar and decreased HbA1c, which indicates the importance of diet as an essential factor in controlling and preventing type 2 diabetes.
4. Discussion
Articles related to diabetes have dramatically increased worldwide in recent years. The Medline website contains more than 60 thousand papers published in the past seven years on this subject, hence confirming the importance of the issue and the concerns felt by all countries regarding the prevalence of diabetes and their serious attempt to find ways to prevent and control this disease. Using non-pharmaceutical interventions to treat and control diabetes while avoiding expenses for the patient and society prevents drug side effects. Hence, the use of non-pharmaceutical interventions is preferable to pharmaceutical ones.
WHO has classified the intervention types into 12 classes as follows: Behavior, diagnosis, early detection, lifestyle, placebo, prevention, rehabilitation, treatment devices, treatment-drugs, treatment-surgery, and treatment-other and other. The results of this study were classified into four categories: 1) Lifestyle, 2) Treatment-devices, 3) Treatment-other (traditional treatment), and 4) Other (education).
Lifestyle
US Diabetes Association considers lifestyle management a principal aspect of preventing and controlling type 2 diabetes [29]. Although lifestyle interventions are the major element of care in type 2 diabetes cases [30] and lifestyle can prevent the micro- and macro-vascular complications accompanied by type 2 diabetes [31], due to the complexity and time-consuming nature of complete intervention in lifestyle, a minimal number of studies are often conducted. Most studies consider only one of the elements involved in the lifestyle as an individual variable. This is while numerous factors, including smoking, alcohol consumption, physical activities, diet, social support and spiritual dimensions, and stress in lifestyle are also involved [32-34]. Based on the findings of this study, among the lifestyle components, most of the components, including physical activity, nutrition, and social support, have been studied.
Diet
Most of the articles reviewed in this study have investigated the diet component as an essential factor in lifestyle. Low carbohydrates, low-calorie diet [35-36], traditional beverages [37], brown rice [38], β carotene-enriched foods [39], nutritional supplements containing several low-glucose nutrients with breakfast [40], low-fat diet [41], and prepared food with high protein and low glucose concentration in enteral nutrition [42] have been effective in better blood sugar control and reduction of HbA1c level in type 2 diabetes patients. However, whey protein supplementation was not effective [43]. Vitamin D supplementation did not affect type 2 diabetes incidence or insulin resistance [44].
Accordingly, the results of this study are indicative of the essential role of diet in controlling the blood sugar of people with type 2 diabetes; therefore, it is recommended that considering the native and local nutritional cultures of each country and ease of access to foodstuffs, the necessary education is given to this type of diabetics. The latest guidelines for type 2 diabetes in China also introduce medical nutrition therapy as an essential component of the control and treatment of these patients [45].
Physical activity
In this study, it was confirmed that acute exercise with various intensities is ineffective in controlling the blood sugar of type 2 diabetes patients [46]; however, the use of vegetable supplements, such as fenugreek seed with physical activity, in addition to the reduction of blood sugar, would significantly decrease the body fat percentage [47]. The results of studies also indicate the effect of following a regular and uninterrupted exercise program throughout life on controlling glucose metabolism [48] and programmed structured exercise on the blood sugar level after delivery in the GDM [49].
Physical activity affects lipids, blood sugar, cardiovascular incidents, and life quality and is additionally considered an essential element in predicting and controlling type 2 diabetes. Physical activity with moderate weight loss can decrease the vulnerability risk of type 2 diabetes by up to 58% in high-risk populations [50]. Aerobic exercise, on land and in water, may improve blood sugar and nerve function in type 2 diabetes [51, 52]. Ghanbarzadeh (2017) also demonstrated that a balanced and low-fat diet maintained with (aerobic or anaerobic) exercise can be effective in decreasing the blood sugar of diabetics [53]. In some studies, the intensity of physical exercise is known as the main determinant of metabolic improvement and is also effective on blood sugar [54, 55].
According to the contradictory results of studies [56-60], the effective role of physical activity in decreasing weight and physical health is not unknown. Still, due to a lack of knowledge on the type of activity, intensity, and frequency of exercises that could be effective on the blood sugar of type 2 diabetes patients, the whole issue needs further investigation.
Social support
This study determined that the family's social support, especially with their participation in the health care program of type 2 diabetes patients, results in blood sugar control [61]. Peer social support had a satisfactory effect on diabetic behavior, diabetes-related knowledge, and self-management of diabetic patients in rural China [ ]; however, peer-supportive interventions were ineffective in controlling blood sugar and side effects [56].
The results of other studies are in line with the results of this study that community-based social support will be associated with better health [63] and is effective on the HbA1c level and lifestyle as well as self-efficacy [64-66].
Lifestyle
The study results indicate the effects of the lifestyle interventions on better sexual performance of the patients and their satisfaction [67]. Also, better stress control has been accompanied by diet self-efficacy and higher life quality, although with no evident changes in the biochemical variables [68].
Treatment-devices
Continuous glucose monitor (CGM) devices were effective in the patients' blood sugar control and satisfaction [38]. Although telemonitoring was effective in controlling the blood sugar and improving the HbA1c level of type 2 diabetes patients, this effectiveness was weakened six months after the termination of such monitoring [69]. In GDM, telemedicine can be associated with better diabetes control and maternal and neonatal outcomes [70].
The diabetes monitoring device may include sensors to supervise one or more of the following items: Blood sugar level, physical activity, energy consumption, and insulin dose [71]. Although numerous interventions have reported the significance and effect of telemedicine and telemonitoring interventions on controlling and preventing diabetes complications [72-74], telemedicine services must facilitate infrastructure, including continuous support services and service guideline training, to be effective. Therefore, the capacity of telemedicine providers will be far more critical than the competence of their recipients in the success of telemedicine services [75].
Traditional treatment
Although the result of this study is indicative of the ineffectiveness of using cinnamon nutritional supplements [76] in reducing the blood sugar of type 2 diabetes patients, the consumption of bee propolis [77] and sesame seeds [78] achieved the fetal bovine serum reduction outcome besides reducing the HbA1c level.
Education
Targeted training in diabetes management (TTIM) improved psychiatric symptoms and heightened the knowledge level of diabetes [79, 80]. Diabetes self-management and education can, in addition to decreasing body weight, improve the HbA1c level [81, 82]. Although the training DVD was not effective in controlling blood sugar in type 2 diabetics, the video-based lifestyle education program was effective in improving glycemic control in patients with type 2 diabetes [83, 84].
Diabetes self-management and education support facilitate the knowledge, skill, and ability required for self-care in diabetics [85, 86]. Based on the results reported by numerous studies, education currently represents one of the most essential elements in preventing and controlling diabetes [87, 88]. Peer support for educational intervention and simulation education in diabetes control will be useful [89, 90]. However, assessing educational needs is necessary for the success of every educational program [91]. The self-management education must be appropriate to the specific population considering the ethnic, social, cognitive, literacy, and cultural factors. There is a need to improve access to and absorption of diabetes self-management programs across the globe [92], and comprehensive research should be conducted on the manner, period, and method of interaction with the trainer. It is recommended that in every educational group, first, the preliminary educational needs assessment is performed. Then, based on the literacy level, cultural and ethnic factors, and the groups' educational needs, the content and tools suitable to the training are selected, and the educational planning is executed.
5. Conclusion
Study findings show that applying non-pharmaceutical interventions effectively controls and prevents type 2 diabetes complications. The interventions, such as lifestyle correction, suitable diet, social support, application of treatment devices, traditional treatment, and education, all have a role in treating type-2 diabetes. However, depending on the patient’s condition, these interventions may need to be accompanied by medication. Most studies are in line with a low-carbohydrate diet. Still, this study demonstrated that in addition to the low glucose and high protein diet, consuming some foodstuffs, including brown rice, DAK beverages, β-carotene contained foods, and low-fat diets could decrease HbA1c levels. Structured physical activity, family support through their participation in the care programs, application of telemonitoring devices, and diabetes self-management education are all effective methods in controlling diabetes and preventing its complications. However, some of these components need further investigation to confirm a rigorous and consistent program. In addition, it seems that the most important issue is education because using all of the above methods requires patient education, so proper patient education should not be neglected.
Study limitations
We attempted to minimize the limitations of this study. We used several strategies to identify studies to limit publication bias's possible effect. The Inclusion criteria were chosen to increase the possibility that high-quality studies would be selected. However, there are many limitations. Firstly, a literature search was conducted in major electronic databases, Medline, Science Direct, Embase, Scopus, Cochrane Library, and the Google Scholar search engine. Still, no other databases were searched (gray literature). Therefore, some relevant studies are probably missing. Secondly, based on the search strategy in the study, we included all studies with available full text in English and Persian languages that investigated the non-pharmacological interventions in the control and treatment of type 2 diabetes with “clinical trial,” “treatment,” “type-2 diabetes,” ‘control,” and its equivalents in MeSH, namely “NIDDM” and “diabetes mellitus.” However, other interventions for treating this disease can be investigated in other studies, but due to the small number of them, they were not included in this study, and only the main interventions were used. Third, we excluded articles published in preprint databases due to a lack of peer review.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Sabzevar University of Medical Sciences (Code: IR.MEDSAB.REC.1399.145) and informed consent was obtained from every participant.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Writing–review and editing: Fatemeh Ghardashi and Roghayeh Zardosht; Data collection and writing–original draft: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Sabzevar University of Medical Sciences for their support.
References
Diabetes is one of the most critical health challenges worldwide. During the past three decades, the number of diabetic cases has increased more than twofold [1, 2]. The prevalence of vulnerability to diabetes is growing rapidly and will reach approximately 625 million people in all quarters of the globe by 2045 [3]. According to the estimations by the international diabetes federation in the year 2015, about 75% of adult diabetics are living in low-income countries [4]. Some risk factors of vulnerability to type 2 diabetes are unchanging, such as age and family background; however, other risk factors, such as weight gain, blood sugar, and triglyceride, change dramatically with lifestyle correction [5]. Monitoring the metabolic indicators, such as blood pressure, body weight, blood sugar, HbA1c, and lipid, is imperative for managing diabetics [6]. Studies have shown that pharmaceutical interventions and lifestyle modification can effectively control Hyperglycemia [7]. Correcting the lifestyle and mood factors, self-confidence, and social support can save pre-diabetics from the risk of vulnerability to this illness [8, 9]. About 50% to 80% of the people with diabetes have no adequate skills and knowledge of self-care and illness management [10]. Numerous studies have demonstrated that healthcare strategies engaging the diabetics' family members cause higher awareness and self-efficacy concerning self-care in patients with diabetes [11]. In recent years, the US and UK diabetes associations have confirmed the effect of a low carbohydrate diet in lowering weight and improving blood glucose and lipid regulation in mellitus diabetics [12, 13]. Combinatorial diet programs and physical activity promotion plans may hinder and delay the progress of type 2 diabetes [14-17]. Disease management programs have introduced particular instructions as the best strategy for diabetes prevention in which the increase in physical activity [18, 19], decrease of consumable calories, and training of patients together with the support by peer groups are among the most crucial disease management programs [20-26]. Despite the variety and frequency of the interventions to control and treat type 2 diabetes in different countries, the knowledge and awareness of the methods and the relevant consequences are crucial for the science community. They can be counted as a decisive step toward promoting this science. A systematic review is a comprehensive study based on a predetermined and accurate protocol. Many studies do not have good interpretive power for various reasons; however, the systematic review and meta-analysis that often follows will combine studies to reach a larger sample size; therefore, they can be examined with greater power and ultimately provide better conclusions. Accordingly, this study aims to determine effective non-pharmacological interventions in controlling and treating type 2 diabetes by systematic review method. This study has been conducted to find answers to the following questions:
1) What are the types of non-pharmacological interventions used in intervention studies to control or treat type 2 diabetes?
2) Which non-pharmacological intervention is primarily recommended in controlling or treating type 2 diabetes in intervention studies?
3) What have been the outcomes of non-pharmacological interventions in controlling or treating type 2 diabetes?
2. Methods
This study is a systematic review of the papers published on the non-pharmaceutical intervention arrangements in controlling and treating patients with type 2 diabetes. The authors have used the standard systematic review guideline (PRISMA), including 27 items [27].
The search included the electronic data banks, including Medline, Science Direct, Embase, Scopus, Cochrane Library, and the Google Scholar search engine. The main selected keywords were as follows: “Clinical trial,” “treatment,” “type-2 diabetes,” and “control.” Their equivalents were also searched in MeSH: “NIDDM” and “diabetes mellitus.” The words “AND” and “OR” were used to combine the keywords. Searching was restricted to all relevant English papers published and indexed from June 2014 to the end of 2020.
Inclusion criteria
The inclusion criteria of selected papers were from scientific research journals, the language of the paper was in English, and the documents were full-text papers. The criteria for selecting articles were as follows: Type of participants=type 2 diabetes, type of interventions=non-pharmaceutical interventions, type of comparator=intervention performed, type of outcome=control or treatment, study type=clinical trial or empirical.
Exclusion criteria
The exclusion criteria of papers were inaccessibility to the full text, letters to the editors, and exclusively descriptive and review papers.
Data extraction, variables, and data analysis
A researcher-made data extraction form based on the study objective was used to analyze the papers. This form included parts of the article details, including the authors’ names, publication year, paper’s objective, study design, study methodology, information relevant to type 2 diabetes, and final results and outputs. Two researchers were involved in the selection work and data extraction activities. The main features of the studies and their results have been summarized considering the following variables:
Type of study: The papers from clinical trials or empirical studies were selected.
Target population: The patients with type 2 diabetes and gestational diabetes (GDM).
Types of interventions
Types of interventions in this study were classified into four categories, namely “lifestyle,” “education,” “traditional treatment,” and “Treatment devices,” based on the World Health Organization (WHO) interventions category guidelines [28], and the study objectives that embraced only the non-pharmaceutical interventions.
Two reviewers worked independently to determine whether a study met the inclusion criteria. They collected information to assess each study's methodological validity (degree of protection against confounding and bias). They also extracted data from the included studies using structured and standardized data extraction forms. The reviewers resolved discrepancies by jointly reviewing any study in question. A third reviewer would enter as an external peer reviewer if no consensus were reached. The third author was unaware of the other reviewers’ determinations and functioned as an arbitrator.
3. Results
Searching of the data sources was performed for two months based on the keywords and searching strategies, and a total of 41 papers were selected from 529 articles after three selection steps. The authors systematically considered the title and abstract of all papers in the indices in the first step based on the relevancy to the study subject in addition to the inclusion and exclusion criteria. Accordingly, a total of 198 articles were entered into the study. Meanwhile, 35 articles were excluded from the study due to inaccessibility to the full text or duplication (indexed in different sites). An expert panel thoroughly analyzed the remaining articles (n=163) with two expert reviewers (after a full-text reading of the articles). Eventually, 68 articles with more comprehensive and relevant information were selected. The full text of the above 68 papers was then handed to two independent expert authors, and finally, 36 articles were selected. Then, 5 articles were added from among the articles’ references, and 41 papers were selected. The flow chart of article selection is presented in Figure 1. Table 1 represents the main features of the selected articles in addition to their aims and results.
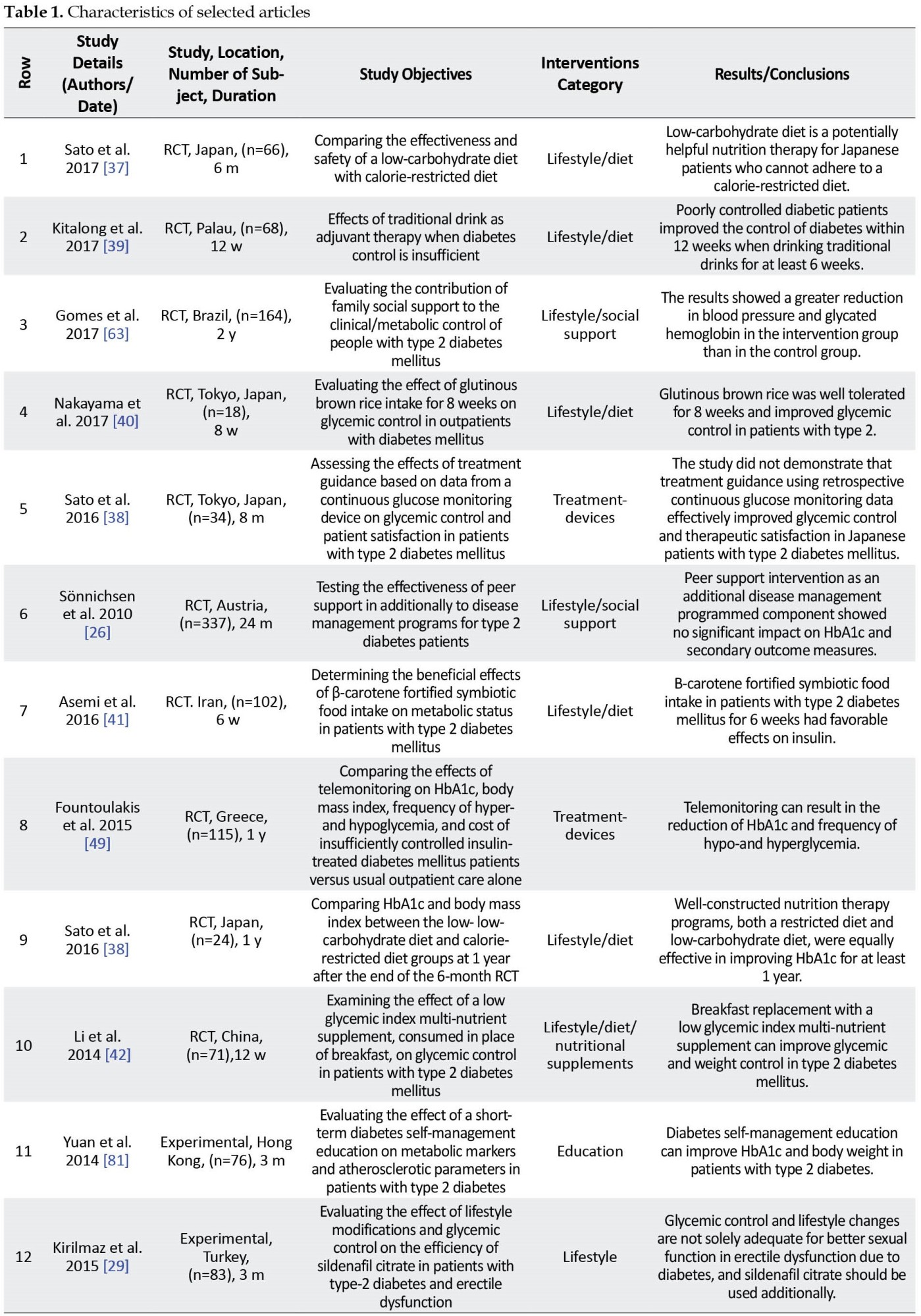
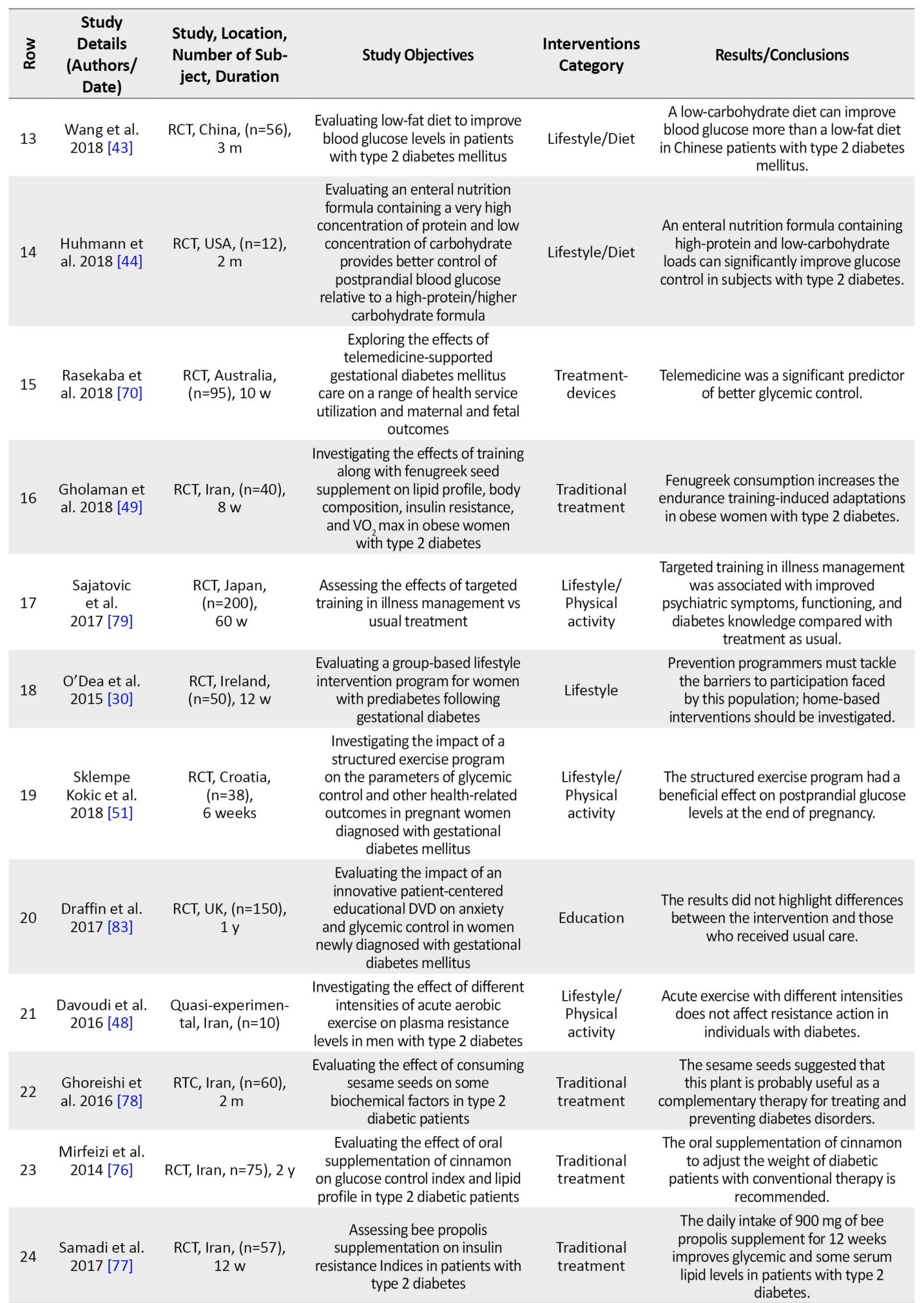
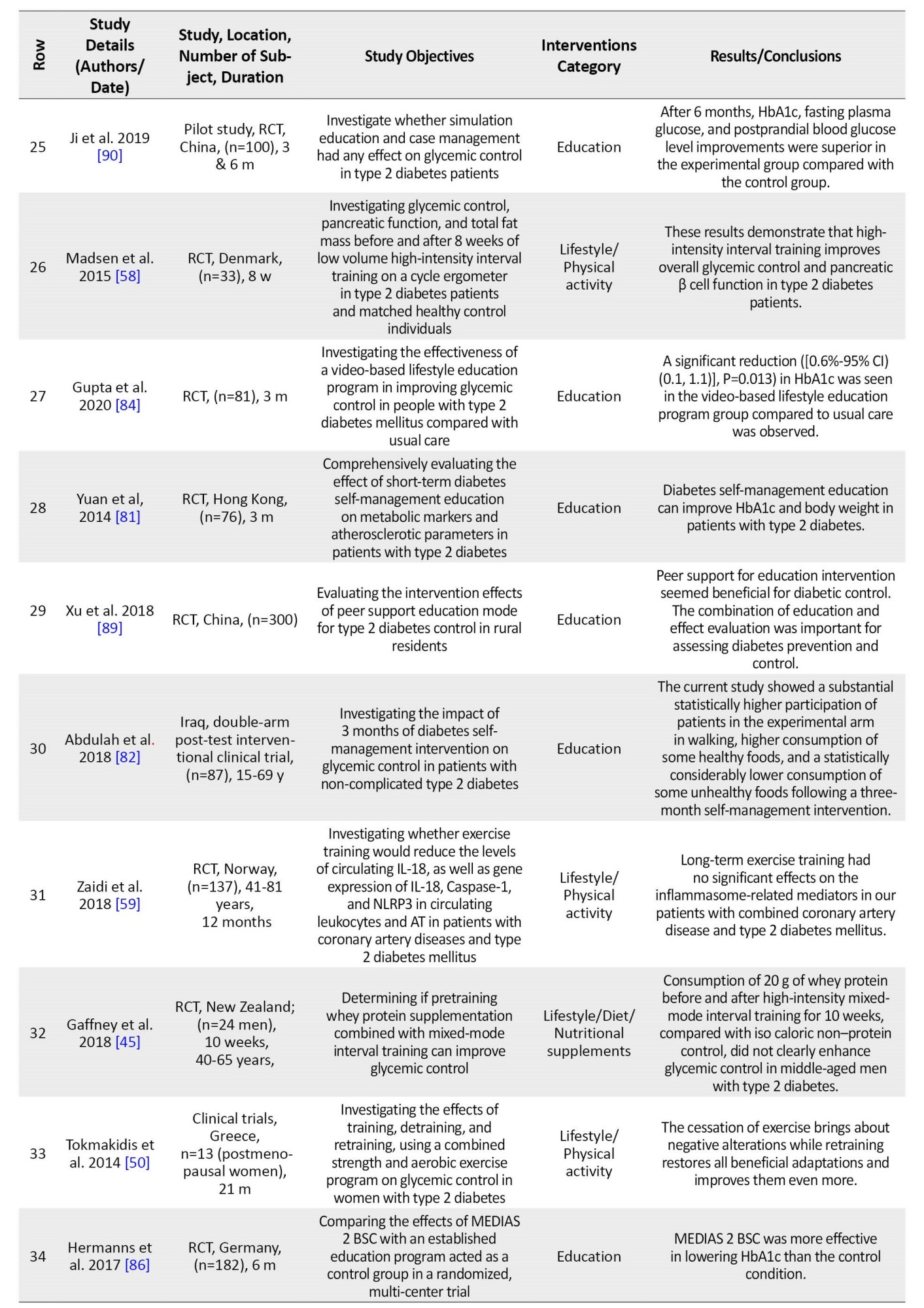
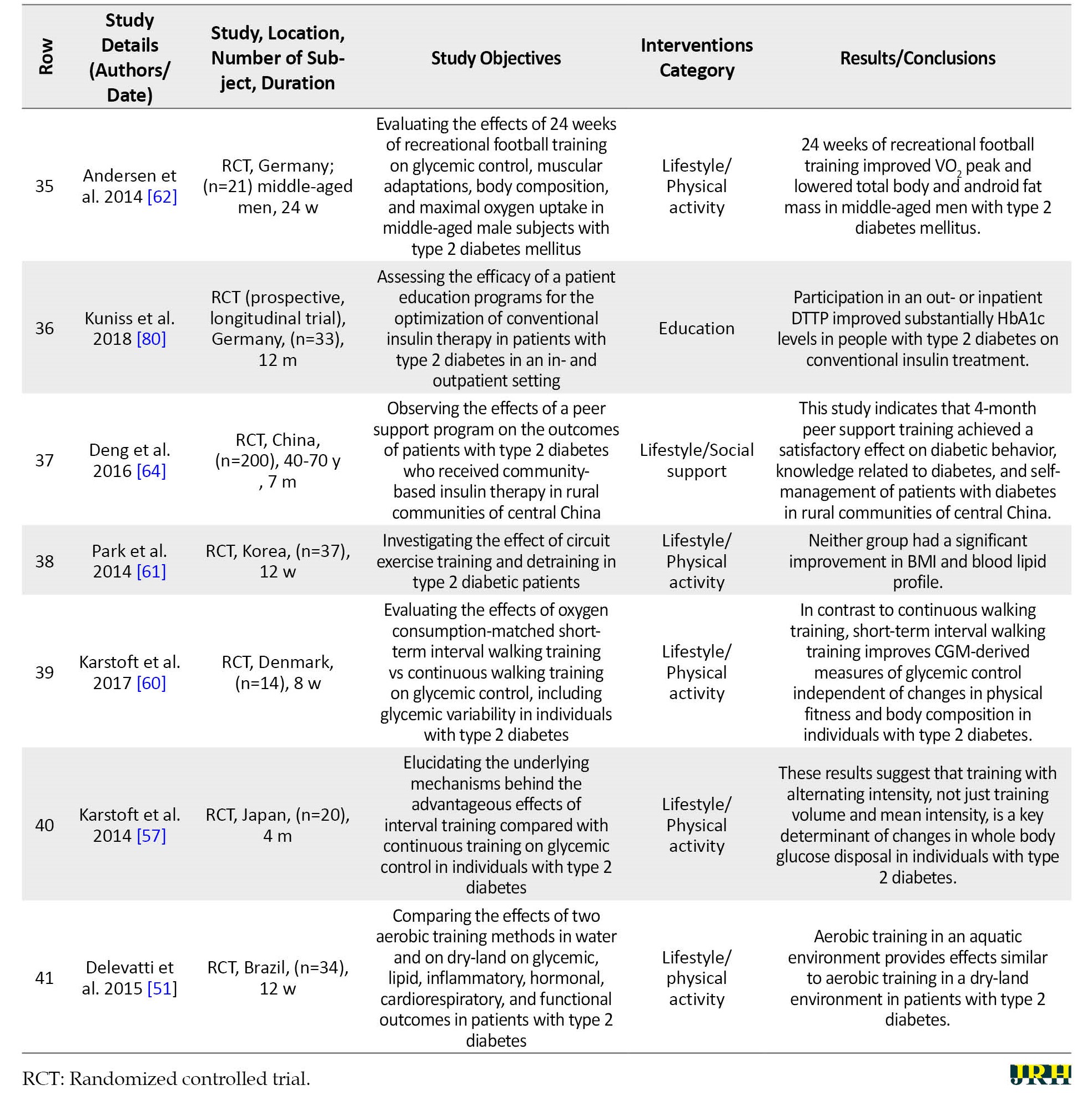
The result indicated that the above 41 selected articles were from the outcome of studies performed in 21 different countries. Most of the randomized controlled trial (RCT) studies (82.9%) and interventions were related to lifestyle (61%). Meanwhile, most studies (53.7%) represented an improvement in the patient’s status and a decrease in HbA1c, while the reduction of HbA1c accompanied the outcome of most diet intervention studies (88.9%). The percentage and frequency of the under-study variables in terms of the type of study, type of intervention, the comparison group, and the interventions’ outcomes are shown in Table 2.
In response to the first question of the study:
1) What are the types of non-pharmacological interventions used in intervention studies to control or treat type 2 diabetes?
In the present study, it was determined that the researchers had used the interventions, such as “changing the lifestyle (diet, physical activity, and social support),” “treatment devices,” “treatment-other,” “traditional treatment,” and other interventions (education).
In response to the second and third questions of the study:
2) In intervention studies, which non-pharmacological intervention is most recommended in controlling or treating type 2 diabetes?
3) What have been the outcomes of non-pharmacological interventions in controlling or treating type 2 diabetes?
Most non-pharmacological intervention to control and improve type 2 diabetes was related to lifestyle (60.9%), although only 4.9% of the studies had investigated all lifestyle elements. Among the lifestyle variables, the highest frequency was diet and nutritional supplements (19.5%). Subsequently, physical activity (26.8%) and social support (7.3%) had the highest frequencies, respectively.
About 65.9% of interventions resulted in controlling and improving blood sugar and decreasing HbA1c. Meanwhile, 7.3% of the studies represented satisfaction and increased patients’ quality of life; only 26.8% showed no significant statistical result. The study's results also demonstrated that all diet-related interventions produced the outcome of better control and improvement of blood sugar and decreased HbA1c, which indicates the importance of diet as an essential factor in controlling and preventing type 2 diabetes.
4. Discussion
Articles related to diabetes have dramatically increased worldwide in recent years. The Medline website contains more than 60 thousand papers published in the past seven years on this subject, hence confirming the importance of the issue and the concerns felt by all countries regarding the prevalence of diabetes and their serious attempt to find ways to prevent and control this disease. Using non-pharmaceutical interventions to treat and control diabetes while avoiding expenses for the patient and society prevents drug side effects. Hence, the use of non-pharmaceutical interventions is preferable to pharmaceutical ones.
WHO has classified the intervention types into 12 classes as follows: Behavior, diagnosis, early detection, lifestyle, placebo, prevention, rehabilitation, treatment devices, treatment-drugs, treatment-surgery, and treatment-other and other. The results of this study were classified into four categories: 1) Lifestyle, 2) Treatment-devices, 3) Treatment-other (traditional treatment), and 4) Other (education).
Lifestyle
US Diabetes Association considers lifestyle management a principal aspect of preventing and controlling type 2 diabetes [29]. Although lifestyle interventions are the major element of care in type 2 diabetes cases [30] and lifestyle can prevent the micro- and macro-vascular complications accompanied by type 2 diabetes [31], due to the complexity and time-consuming nature of complete intervention in lifestyle, a minimal number of studies are often conducted. Most studies consider only one of the elements involved in the lifestyle as an individual variable. This is while numerous factors, including smoking, alcohol consumption, physical activities, diet, social support and spiritual dimensions, and stress in lifestyle are also involved [32-34]. Based on the findings of this study, among the lifestyle components, most of the components, including physical activity, nutrition, and social support, have been studied.
Diet
Most of the articles reviewed in this study have investigated the diet component as an essential factor in lifestyle. Low carbohydrates, low-calorie diet [35-36], traditional beverages [37], brown rice [38], β carotene-enriched foods [39], nutritional supplements containing several low-glucose nutrients with breakfast [40], low-fat diet [41], and prepared food with high protein and low glucose concentration in enteral nutrition [42] have been effective in better blood sugar control and reduction of HbA1c level in type 2 diabetes patients. However, whey protein supplementation was not effective [43]. Vitamin D supplementation did not affect type 2 diabetes incidence or insulin resistance [44].
Accordingly, the results of this study are indicative of the essential role of diet in controlling the blood sugar of people with type 2 diabetes; therefore, it is recommended that considering the native and local nutritional cultures of each country and ease of access to foodstuffs, the necessary education is given to this type of diabetics. The latest guidelines for type 2 diabetes in China also introduce medical nutrition therapy as an essential component of the control and treatment of these patients [45].
Physical activity
In this study, it was confirmed that acute exercise with various intensities is ineffective in controlling the blood sugar of type 2 diabetes patients [46]; however, the use of vegetable supplements, such as fenugreek seed with physical activity, in addition to the reduction of blood sugar, would significantly decrease the body fat percentage [47]. The results of studies also indicate the effect of following a regular and uninterrupted exercise program throughout life on controlling glucose metabolism [48] and programmed structured exercise on the blood sugar level after delivery in the GDM [49].
Physical activity affects lipids, blood sugar, cardiovascular incidents, and life quality and is additionally considered an essential element in predicting and controlling type 2 diabetes. Physical activity with moderate weight loss can decrease the vulnerability risk of type 2 diabetes by up to 58% in high-risk populations [50]. Aerobic exercise, on land and in water, may improve blood sugar and nerve function in type 2 diabetes [51, 52]. Ghanbarzadeh (2017) also demonstrated that a balanced and low-fat diet maintained with (aerobic or anaerobic) exercise can be effective in decreasing the blood sugar of diabetics [53]. In some studies, the intensity of physical exercise is known as the main determinant of metabolic improvement and is also effective on blood sugar [54, 55].
According to the contradictory results of studies [56-60], the effective role of physical activity in decreasing weight and physical health is not unknown. Still, due to a lack of knowledge on the type of activity, intensity, and frequency of exercises that could be effective on the blood sugar of type 2 diabetes patients, the whole issue needs further investigation.
Social support
This study determined that the family's social support, especially with their participation in the health care program of type 2 diabetes patients, results in blood sugar control [61]. Peer social support had a satisfactory effect on diabetic behavior, diabetes-related knowledge, and self-management of diabetic patients in rural China [ ]; however, peer-supportive interventions were ineffective in controlling blood sugar and side effects [56].
The results of other studies are in line with the results of this study that community-based social support will be associated with better health [63] and is effective on the HbA1c level and lifestyle as well as self-efficacy [64-66].
Lifestyle
The study results indicate the effects of the lifestyle interventions on better sexual performance of the patients and their satisfaction [67]. Also, better stress control has been accompanied by diet self-efficacy and higher life quality, although with no evident changes in the biochemical variables [68].
Treatment-devices
Continuous glucose monitor (CGM) devices were effective in the patients' blood sugar control and satisfaction [38]. Although telemonitoring was effective in controlling the blood sugar and improving the HbA1c level of type 2 diabetes patients, this effectiveness was weakened six months after the termination of such monitoring [69]. In GDM, telemedicine can be associated with better diabetes control and maternal and neonatal outcomes [70].
The diabetes monitoring device may include sensors to supervise one or more of the following items: Blood sugar level, physical activity, energy consumption, and insulin dose [71]. Although numerous interventions have reported the significance and effect of telemedicine and telemonitoring interventions on controlling and preventing diabetes complications [72-74], telemedicine services must facilitate infrastructure, including continuous support services and service guideline training, to be effective. Therefore, the capacity of telemedicine providers will be far more critical than the competence of their recipients in the success of telemedicine services [75].
Traditional treatment
Although the result of this study is indicative of the ineffectiveness of using cinnamon nutritional supplements [76] in reducing the blood sugar of type 2 diabetes patients, the consumption of bee propolis [77] and sesame seeds [78] achieved the fetal bovine serum reduction outcome besides reducing the HbA1c level.
Education
Targeted training in diabetes management (TTIM) improved psychiatric symptoms and heightened the knowledge level of diabetes [79, 80]. Diabetes self-management and education can, in addition to decreasing body weight, improve the HbA1c level [81, 82]. Although the training DVD was not effective in controlling blood sugar in type 2 diabetics, the video-based lifestyle education program was effective in improving glycemic control in patients with type 2 diabetes [83, 84].
Diabetes self-management and education support facilitate the knowledge, skill, and ability required for self-care in diabetics [85, 86]. Based on the results reported by numerous studies, education currently represents one of the most essential elements in preventing and controlling diabetes [87, 88]. Peer support for educational intervention and simulation education in diabetes control will be useful [89, 90]. However, assessing educational needs is necessary for the success of every educational program [91]. The self-management education must be appropriate to the specific population considering the ethnic, social, cognitive, literacy, and cultural factors. There is a need to improve access to and absorption of diabetes self-management programs across the globe [92], and comprehensive research should be conducted on the manner, period, and method of interaction with the trainer. It is recommended that in every educational group, first, the preliminary educational needs assessment is performed. Then, based on the literacy level, cultural and ethnic factors, and the groups' educational needs, the content and tools suitable to the training are selected, and the educational planning is executed.
5. Conclusion
Study findings show that applying non-pharmaceutical interventions effectively controls and prevents type 2 diabetes complications. The interventions, such as lifestyle correction, suitable diet, social support, application of treatment devices, traditional treatment, and education, all have a role in treating type-2 diabetes. However, depending on the patient’s condition, these interventions may need to be accompanied by medication. Most studies are in line with a low-carbohydrate diet. Still, this study demonstrated that in addition to the low glucose and high protein diet, consuming some foodstuffs, including brown rice, DAK beverages, β-carotene contained foods, and low-fat diets could decrease HbA1c levels. Structured physical activity, family support through their participation in the care programs, application of telemonitoring devices, and diabetes self-management education are all effective methods in controlling diabetes and preventing its complications. However, some of these components need further investigation to confirm a rigorous and consistent program. In addition, it seems that the most important issue is education because using all of the above methods requires patient education, so proper patient education should not be neglected.
Study limitations
We attempted to minimize the limitations of this study. We used several strategies to identify studies to limit publication bias's possible effect. The Inclusion criteria were chosen to increase the possibility that high-quality studies would be selected. However, there are many limitations. Firstly, a literature search was conducted in major electronic databases, Medline, Science Direct, Embase, Scopus, Cochrane Library, and the Google Scholar search engine. Still, no other databases were searched (gray literature). Therefore, some relevant studies are probably missing. Secondly, based on the search strategy in the study, we included all studies with available full text in English and Persian languages that investigated the non-pharmacological interventions in the control and treatment of type 2 diabetes with “clinical trial,” “treatment,” “type-2 diabetes,” ‘control,” and its equivalents in MeSH, namely “NIDDM” and “diabetes mellitus.” However, other interventions for treating this disease can be investigated in other studies, but due to the small number of them, they were not included in this study, and only the main interventions were used. Third, we excluded articles published in preprint databases due to a lack of peer review.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Sabzevar University of Medical Sciences (Code: IR.MEDSAB.REC.1399.145) and informed consent was obtained from every participant.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Writing–review and editing: Fatemeh Ghardashi and Roghayeh Zardosht; Data collection and writing–original draft: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Sabzevar University of Medical Sciences for their support.
References
- Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus--present and future perspectives. Nature Reviews. Endocrinology. 2011; 8(4):228-36. [DOI:10.1038/nrendo.2011.183] [PMID]
- Zimmet PZ, Magliano DJ, Herman WH, Shaw JE. Diabetes: A 21st century challenge. The Lancet. Diabetes & Endocrinology. 2014; 2(1):56-64. [DOI:10.1016/S2213-8587(13)70112-8] [PMID]
- Duarte AA, Mohsin S, Golubnitschaja O. Diabetes care in figures: Current pitfalls and future scenario. The EPMA Journal. 2018; 9(2):125-31. [DOI:10.1007/s13167-018-0133-y] [PMID] [PMCID]
- International Diabetes Federation. Diabetes atlas. Belgium: International Diabetes Federation; 2015. [Link]
- Balducci S, Zanuso S, Nicolucci A, De Feo P, Cavallo S, Cardelli P, et al. Effect of an intensive exercise intervention strategy on modifiable cardiovascular risk factors in subjects with type 2 diabetes mellitus: A randomized controlled trial: The Italian diabetes and exercise study (IDES). Archives of Internal Medicine. 2010; 170(20):1794-803. [DOI:10.1001/archinternmed.2010.380] [PMID]
- Tripathi BK, Srivastava AK. Diabetes mellitus: Complications and therapeutics. Medical Science Monitor. 2006; 12(7):RA130-47. [PMID]
- Georgoulis M, Kontogianni MD, Yiannakouris N. Mediterranean diet and diabetes: Prevention and treatment. Nutrients. 2014; 6(4):1406-23. [DOI:10.3390/nu6041406] [PMID] [PMCID]
- Goldney RD, Phillips PJ, Fisher LJ, Wilson DH. Diabetes, depression, and quality of life: A population study. Diabetes Care. 2004; 27(5):1066-70. [DOI:10.2337/diacare.27.5.1066] [PMID]
- Stenlöf K, Cefalu WT, Kim KA, Alba M, Usiskin K, Tong C, Canovatchel W, Meininger G. Efficacy and safety of canagliflozin monotherapy in subjects with type 2 diabetes mellitus inadequately controlled with diet and exercise. Diabetes, Obesity & Metabolism. 2013; 15(4):372-82. [DOI:10.1111/dom.12054] [PMID] [PMCID]
- Clement S. Diabetes self-management education. Diabetes Care. 1995; 18(8):1204-14. [DOI:10.2337/diacare.18.8.1204] [PMID]
- Baig AA, Benitez A, Quinn MT, Burnet DL. Family interventions to improve diabetes outcomes for adults. Annals of the New York Academy of Sciences. 2015; 1353(1):89-112. [DOI:10.1111/nyas.12844] [PMID] [PMCID]
- Dyson PA, Kelly T, Deakin T, Duncan A, Frost G, Harrison Z, et al. Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabetic Medicine. 2011; 28(11):1282-8. [DOI:10.1111/j.1464-5491.2011.03371.x] [PMID]
- Wheeler ML, Dunbar SA, Jaacks LM, Karmally W, Mayer-Davis EJ, Wylie-Rosett J, et al. Macronutrients, food groups, and eating patterns in the management of diabetes: A systematic review of the literature, 2010. Diabetes Care. 2012; 35(2):434-45. [DOI:10.2337/dc11-2216] [PMID] [PMCID]
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England Journal of Medicine. 2002; 346(6):393-403. [DOI:10.1056/NEJMoa012512] [PMID] [PMCID]
- Lindström J, Louheranta A, Mannelin M, Rastas M, Salminen V, Eriksson J, et al. The Finnish diabetes prevention study (DPS): Lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care. 2003; 26(12):3230-6.[DOI:10.2337/diacare.26.12.3230] [PMID]
- Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997; 20(4):537-44. [DOI:10.2337/diacare.20.4.537] [PMID]
- Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V; Indian Diabetes Prevention Programme (IDPP). The Indian diabetes prevention programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006; 49(2):289-97. [DOI:10.1007/s00125-005-0097-z] [PMID]
- Ofman JJ, Badamgarav E, Henning JM, Knight K, Gano AD Jr, Levan RK, et al. Does disease management improve clinical and economic outcomes in patients with chronic diseases? A systematic review. The American Journal of Medicine. 2004; 117(3):182-92. [DOI:10.1016/j.amjmed.2004.03.018] [PMID]
- Pimouguet C, Le Goff M, Thiébaut R, Dartigues JF, Helmer C. Effectiveness of disease-management programs for improving diabetes care: A meta-analysis. CMAJ. 2011; 183(2):E115-27. [DOI:10.1503/cmaj.091786] [PMID] [PMCID]
- Esposito K, Giugliano D. Mediterranean diet and type 2 diabetes. Diabetes/Metabolism Research and Reviews. 2014; 30(Suppl 1):34-40. [DOI:10.1002/dmrr.2516] [PMID]
- Glasgow RE, Boles SM, McKay HG, Feil EG, Barrera M Jr. The D-Net diabetes self-management program: Long-term implementation, outcomes, and generalization results. Preventive Medicine. 2003; 36(4):410-9. [DOI:10.1016/S0091-7435(02)00056-7] [PMID]
- Anderson-Loftin W, Barnett S, Bunn P, Sullivan P, Hussey J, Tavakoli A. Soul food light: Culturally competent diabetes education. The Diabetes Educator. 2005; 31(4):555-63.[DOI:10.1177/0145721705278948] [PMID]
- Lorig K, Ritter PL, Villa F, Piette JD. Spanish diabetes self-management with and without automated telephone reinforcement: Two randomized trials. Diabetes Care. 2008; 31(3):408-14. [DOI:10.2337/dc07-1313] [PMID]
- Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: A randomized trial. The Diabetes Educator. 2009; 35(4):641-51. [DOI:10.1177/0145721709335006] [PMID]
- Murrock CJ, Higgins PA, Killion C. Dance and peer support to improve diabetes outcomes in African American women. The Diabetes Educator. 2009; 35(6):995-1003.[DOI:10.1177/0145721709343322] [PMID]
- Sönnichsen AC, Winkler H, Flamm M, Panisch S, Kowatsch P, Klima G, et al. The effectiveness of the Austrian disease management programme for type 2 diabetes: A cluster-randomised controlled trial. BMc Family Practice. 2010; 11:86. [DOI:10.1186/1471-2296-11-86] [PMID] [PMCID]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Plos Medicine. 2009; 6(7):e1000100. [DOI:10.1371/journal.pmed.1000100] [PMID] [PMCID]
- WHO. Diabetes. Geneva: World Health Organization; 2023. [Link]
- Kirilmaz U, Guzel O, Aslan Y, Balci M, Tuncel A, Atan A. The effect of lifestyle modification and glycemic control on the efficiency of sildenafil citrate in patients with erectile dysfunction due to type-2 diabetes mellitus. The Aging Male. 2015; 18(4):244-8. [DOI:10.3109/13685538.2015.1072154] [PMID]
- O'Dea A, Tierney M, McGuire BE, Newell J, Glynn LG, Gibson I, et al. Can the onset of type 2 diabetes be delayed by a group-based lifestyle intervention in women with prediabetes following gestational diabetes mellitus (GDM)? Findings from a randomized control mixed methods trial. Journal of Diabetes Research. 2015; 2015:798460. [DOI:10.1155/2015/798460] [PMID] [PMCID]
- Paulweber B, Valensi P, Lindström J, Lalic NM, Greaves CJ, McKee M, et al. A European evidence-based guideline for the prevention of type 2 diabetes. Horm Metab Res. 2010; 42(Suppl 1):S3-36. [DOI:10.1055/s-0029-1240928] [PMID]
- American Diabetes Association. Lifestyle management: Standards of medical care in diabetes-2018. Diabetes Care. 2018; 41(Suppl 1):S38-50. [DOI:10.2337/dc18-S004] [PMID]
- Chen L, Pei JH, Kuang J, Chen HM, Chen Z, Li ZW, et al. Effect of lifestyle intervention in patients with type 2 diabetes: A meta-analysis. Metabolism. 2015; 64(2):338-47. [DOI:10.1016/j.metabol.2014.10.018] [PMID]
- LAR G. Long term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes: Four year results of the Look AHEAD trial. Archives of Internal Medicine. 2010; 170(17):1566-75. [DOI:10.1001/archinternmed.2010.334]
- Bouchard DR, Langlois MF, Domingue MÈ, Brown C, LeBrun V, Baillargeon JP. Age differences in expectations and readiness regarding lifestyle modifications in individuals at high risk of diabetes. Archives of Physical Medicine and Rehabilitation. 2012; 93(6):1059-64. [DOI:10.1016/j.apmr.2011.12.028] [PMID]
- Adler A. Understanding human nature: Psychology revivals. London: Routledge; 2014. [DOI:10.4324/9780203438831]
- Sato J, Kanazawa A, Makita S, Hatae C, Komiya K, Shimizu T, et al. A randomized controlled trial of 130 g/day low-carbohydrate diet in type 2 diabetes with poor glycemic control. Clinical Nutrition. 2017; 36(4):992-1000. [DOI:10.1016/j.clnu.2016.07.003] [PMID]
- Sato J, Kanazawa A, Ikeda F, Shigihara N, Kawaguchi M, Komiya K, et al. Effect of treatment guidance using a retrospective continuous glucose monitoring system on glycaemic control in outpatients with type 2 diabetes mellitus: A randomized controlled trial. The Journal of International Medical Research. 2016; 44(1):109-21. [DOI:10.1177/0300060515600190] [PMID] [PMCID]
- Kitalong C, Nogueira RC, Benichou J, Yano V, Espangel V, Houriet J, et al. "DAK", a traditional decoction in Palau, as adjuvant for patients with insufficient control of diabetes mellitus type II. Journal of Ethnopharmacology. 2017; 205:116-22. [DOI:10.1016/j.jep.2017.05.003] [PMID]
- Nakayama T, Nagai Y, Uehara Y, Nakamura Y, Ishii S, Kato H, et al. Eating glutinous brown rice twice a day for 8 weeks improves glycemic control in Japanese patients with diabetes mellitus. Nutrition & Diabetes. 2017; 7(5):e273.[DOI:10.1038/nutd.2017.26] [PMID] [PMCID]
- Asemi Z, Alizadeh SA, Ahmad K, Goli M, Esmaillzadeh A. Effects of beta-carotene fortified synbiotic food on metabolic control of patients with type 2 diabetes mellitus: A double-blind randomized cross-over controlled clinical trial. Clinical Nutrition. 2016; 35(4):819-25. [DOI:10.1016/j.clnu.2015.07.009] [PMID]
- Li D, Zhang P, Guo H, Ling W. Taking a low glycemic index multi-nutrient supplement as breakfast improves glycemic control in patients with type 2 diabetes mellitus: A randomized controlled trial. Nutrients. 2014; 6(12):5740-55.[DOI:10.3390/nu6125740] [PMID] [PMCID]
- Wang LL, Wang Q, Hong Y, Ojo O, Jiang Q, Hou YY, et al. The effect of low-carbohydrate diet on glycemic control in patients with type 2 diabetes mellitus. Nutrients. 2018; 10(6):661. [DOI:10.3390/nu10060661] [PMID] [PMCID]
- Huhmann MB, Yamamoto S, Neutel JM, Cohen SS, Ochoa Gautier JB. Very high-protein and low-carbohydrate enteral nutrition formula and plasma glucose control in adults with type 2 diabetes mellitus: A randomized crossover trial. Nutrition & Diabetes. 2018 8(1):45. [DOI:10.1038/s41387-018-0053-x] [PMID] [PMCID]
- Gaffney KA, Lucero A, Stoner L, Faulkner J, Whitfield P, Krebs J, et al. Nil whey protein effect on glycemic control after intense mixed-mode training in type 2 diabetes. Medicine and Science in Sports and Exercise. 2018; 50(1):11-7. [DOI:10.1249/MSS.0000000000001404] [PMID]
- Wallace IR, Wallace HJ, McKinley MC, Bell PM, Hunter SJ. Vitamin D and insulin resistance. Clinical Endocrinology. 2016; 84(2):159-71. [DOI:10.1111/cen.12760] [PMID]
- Orlando G, Sacchetti M, D'Errico V, Haxhi J, Rapisarda G, Pugliese G, et al. Muscle fatigability in patients with type 2 diabetes: Relation with long-term complications. Diabetes/Metabolism Research and Reviews. 2020; 36(2):e3231. [DOI:10.1002/dmrr.3231] [PMID]
- Davoudi Z, Ghanbarzadeh M, Shakeriyan S, Habbibi A. [The effect of different intensities of acute aerobic exercise on plasma resistin concentration and insulin resistance index in type 2 diabetic males (Persian)]. Journal of Advanced Biomedical Sciences. 2016; 6(1):79-86. [Link]
- Gholaman M, Gholami M. [Effect of eight weeks’ endurance training along with fenugreek ingestion on lipid profile, body composition, insulin resistance and VO2max in obese women’s with type2 diabetes (Persian)]. Journal of Medicinal Plants. 2018; 17(65):83-92. [Link]
- Tokmakidis SP, Touvra AM, Douda HT, Smilios I, Kotsa K, Volaklis KA. Training, detraining, and retraining effects on glycemic control and physical fitness in women with type 2 diabetes. Hormone and Metabolic Research. 2014; 46(13):974-9.[DOI:10.1055/s-0034-1390483] [PMID]
- Sklempe Kokic I, Ivanisevic M, Biolo G, Simunic B, Kokic T, Pisot R. Combination of a structured aerobic and resistance exercise improves glycaemic control in pregnant women diagnosed with gestational diabetes mellitus. A randomised controlled trial. Women & Birth. 2018; 31(4):e232-8. [DOI:10.1016/j.wombi.2017.10.004] [PMID]
- Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, et al. Exercise and type 2 diabetes: The American college of sports medicine and the American diabetes association: Joint position statement. Diabetes Care. 2010; 33(12):e147-67. [DOI:10.2337/dc10-9990] [PMID] [PMCID]
- Ghanbarzadeh M, Omidi M. The effects of physical activity on serum visfatin level: A literature review. International Journal of Basic Science in Medicine. 2017; 2(2):83-9. [DOI:10.15171/ijbsm.2017.16]
- Gu Y, Dennis SM, Kiernan MC, Harmer AR. Aerobic exercise training may improve nerve function in type 2 diabetes and pre-diabetes: A systematic review. Diabetes/Metabolism Research and Reviews. 2019; 35(2):e3099. [DOI:10.1002/dmrr.3099] [PMID]
- Delevatti RS, Kanitz AC, Alberton CL, Marson EC, Lisboa SC, Pinho CD, et al. Glucose control can be similarly improved after aquatic or dry-land aerobic training in patients with type 2 diabetes: A randomized clinical trial. Journal of Science and Medicine in Sport. 2016; 19(8):688-93. [DOI:10.1016/j.jsams.2015.10.008] [PMID]
- Röhling M, Herder C, Stemper T, Müssig K. Influence of acute and chronic exercise on glucose uptake. Journal of Diabetes Research. 2016; 2016:2868652. [DOI:10.1155/2016/2868652] [PMID] [PMCID]
- Karstoft K, Winding K, Knudsen SH, James NG, Scheel MM, Olesen J, et al. Mechanisms behind the superior effects of interval vs continuous training on glycaemic control in individuals with type 2 diabetes: A randomised controlled trial. Diabetologia. 2014; 57(10):2081-93. [DOI:10.1007/s00125-014-3334-5] [PMID]
- Madsen SM, Thorup AC, Overgaard K, Jeppesen PB. High intensity interval training improves glycaemic control and pancreatic β cell function of type 2 diabetes patients. Plos One. 2015; 10(8):e0133286. [DOI:10.1371/journal.pone.0133286] [PMID] [PMCID]
- Zaidi H, Byrkjeland R, Njerve IU, Åkra S, Solheim S, Arnesen H, et al. Effects of exercise training on inflammasome-related mediators and their associations to glucometabolic variables in patients with combined coronary artery disease and type 2 diabetes mellitus: Sub-study of a randomized control trial. Diabetes & Vascular Disease Research. 2019; 16(4):360-8. [DOI:10.1177/1479164119836922] [PMID]
- Karstoft K, Clark MA, Jakobsen I, Müller IA, Pedersen BK, Solomon TP, et al. The effects of 2 weeks of interval vs continuous walking training on glycaemic control and whole-body oxidative stress in individuals with type 2 diabetes: A controlled, randomised, crossover trial. Diabetologia. 2017; 60(3):508-17. [DOI:10.1007/s00125-016-4170-6] [PMID]
- Park SY, Lee IH. Effects on training and detraining on physical function, control of diabetes and anthropometrics in type 2 diabetes; a randomized controlled trial. Physiotherapy Theory and Practice. 2015; 31(2):83-8. [DOI:10.3109/09593985.2014.958265] [PMID]
- Andersen TR, Schmidt JF, Thomassen M, Hornstrup T, Frandsen U, Randers MB, et al. A preliminary study: Effects of football training on glucose control, body composition, and performance in men with type 2 diabetes. Scandinavian Journal of Medicine & Science in Sports. 2014; 24(Suppl 1):43-56. [DOI:10.1111/sms.12259] [PMID]
- Gomes LC, Coelho ACM, Gomides DDS, Foss-Freitas MC, Foss MC, Pace AE. Contribution of family social support to the metabolic control of people with diabetes mellitus: A randomized controlled clinical trial. Applied Nursing Research. 2017; 36:68-76. [DOI:10.1016/j.apnr.2017.05.009] [PMID]
- Deng K, Ren Y, Luo Z, Du K, Zhang X, Zhang Q. Peer support training improved the glycemic control, insulin management, and diabetic behaviors of patients with type 2 diabetes in rural communities of central China: A randomized controlled trial. Medical Science Monitor. 2016; 22:267-75. [DOI:10.12659/MSM.895593] [PMID] [PMCID]
- Koetsenruijter J, van Lieshout J, Lionis C, Portillo MC, Vassilev I, Todorova E, et al. Social support and health in diabetes patients: an observational study in six European countries in an era of austerity. Plos One. 2015; 10(8):e0135079. [DOI:10.1371/journal.pone.0135079] [PMID] [PMCID]
- Rad GS, Bakht LA, Feizi A, Mohebi S. Importance of social support in diabetes care. Journal of Education and Health Promotion. 2013; 2:62. [DOI:10.4103/2277-9531.120864] [PMID] [PMCID]
- Shao Y, Liang L, Shi L, Wan C, Yu S. The effect of social support on glycemic control in patients with type 2 diabetes mellitus: The mediating roles of self-efficacy and adherence. Journal of Diabetes Research. 2017; 2017:2804178. [DOI:10.1155/2017/2804178] [PMID] [PMCID]
- van Dam HA, van der Horst FG, Knoops L, Ryckman RM, Crebolder HF, van den Borne BH. Social support in diabetes: A systematic review of controlled intervention studies. Patient Education and Counseling. 2005; 59(1):1-12. [DOI:10.1016/j.pec.2004.11.001] [PMID]
- Fountoulakis S, Papanastasiou L, Gryparis A, Markou A, Piaditis G. Impact and duration effect of telemonitoring on HbA1c, BMI and cost in insulin-treated diabetes mellitus patients with inadequate glycemic control: A randomized controlled study. Hormones. 2015; 14(4):632-43. [DOI:10.14310/horm.2002.1603]
- Rasekaba TM, Furler J, Young D, Liew D, Gray K, Blackberry I, et al. Using technology to support care in gestational diabetes mellitus: Quantitative outcomes of an exploratory randomised control trial of adjunct telemedicine for gestational diabetes mellitus (TeleGDM). Diabetes Research and Clinical Practice. 2018; 142:276-85. [DOI:10.1016/j.diabres.2018.05.049] [PMID]
- Yuval G, Uri S. System, device and method for diabetes treatment and monitoring. Shirlington: Patent Application; 2006. [Link]
- Istepanian RS, Zitouni K, Harry D, Moutosammy N, Sungoor A, Tang B, et al. Evaluation of a mobile phone telemonitoring system for glycaemic control in patients with diabetes. Journal of Telemedicine and Telecare. 2009; 15(3):125-8. [DOI:10.1258/jtt.2009.003006] [PMID]
- Jaana M, Paré G. Home telemonitoring of patients with diabetes: A systematic assessment of observed effects. Journal of Evaluation in Clinical Practice. 2007; 13(2):242-53. [DOI:10.1111/j.1365-2753.2006.00686.x] [PMID]
- Shea S, Weinstock RS, Teresi JA, Palmas W, Starren J, Cimino JJ, et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. Journal of the American Medical Informatics Association. 2009; 16(4):446-56. [DOI:10.1197/jamia.M3157] [PMID] [PMCID]
- Rho MJ, Kim HS, Chung K, Choi IY. Factors influencing the acceptance of telemedicine for diabetes management. Cluster Computing. 2015; 18(1):321-31. [DOI:10.1007/s10586-014-0356-1]
- Mirfeizi M, Mehdizadeh Tourzani Z, Mirfeizi SZ, Asghari Jafarabadi M, Rezvani H, Shoghi M. [Effects of cinnamon on controlling blood glucose and lipids in patients with type II diabetes mellitus: A double blind, randomized clinical trial (Persian)]. Medical Journal of Mashhad University of Medical Sciences. 2014; 57(3):533-41. [DOI:10.22038/mjms.2014.3008]
- Samadi N, Mozaffari-Khosravi H, Rahmanian M, Askarishahi M. Effects of bee propolis supplementation on glycemic control, lipid profile and insulin resistance indices in patients with type 2 diabetes: A randomized, double-blind clinical trial. Journal of Integrative Medicine. 2017; 15(2):124-34. [DOI:10.1016/S2095-4964(17)60315-7] [PMID]
- Ghoreishi AS, Mohammadian Shahrbabaki F, Toghroli N, Sheikh Fathollahi M, Hajizadeh MR, Khoshdel A, et al. [Investigating the effect of sesamum indicum consumption on biochemichal parameters in type 2 diabetic patients (Persian)]. Journal of Advanced Biomedical Sciences. 2016; 6(1):87-95. [Link]
- Sajatovic M, Gunzler DD, Kanuch SW, Cassidy KA, Tatsuoka C, McCormick R, et al. A 60-week prospective RCT of a self-management intervention for individuals with serious mental illness and diabetes mellitus. Psychiatric Services. 2017; 68(9):883-90. [DOI:10.1176/appi.ps.201600377] [PMID] [PMCID]
- Kuniss N, Müller UA, Kloos C, Müller R, Starrach G, Jörgens V, et al. Substantial improvement in HbA1c following a treatment and teaching programme for people with type 2 diabetes on conventional insulin therapy in an in- and outpatient setting. Acta Diabetologica. 2018; 55(2):131-7. [DOI:10.1007/s00592-017-1070-2] [PMID]
- Yuan C, Lai CW, Chan LW, Chow M, Law HK, Ying M. The effect of diabetes self-management education on body weight, glycemic control, and other metabolic markers in patients with type 2 diabetes mellitus. Journal of Diabetes Research. 2014; 2014:789761. [DOI:10.1155/2014/789761] [PMID] [PMCID]
- Abdulah DM, Hassan AB, Saadi FS, Mohammed AH. Impacts of self-management education on glycaemic control in patients with type 2 diabetes mellitus. Diabetes & Metabolic Syndrome. 2018; 12(6):969-75. [DOI:10.1016/j.dsx.2018.06.007] [PMID]
- Draffin CR, Alderdice FA, McCance DR, Maresh M, Harper R, Patterson CC, et al. Impact of an educational DVD on anxiety and glycaemic control in women diagnosed with gestational diabetes mellitus (GDM): A randomised controlled trial. Diabetes Research and Clinical Practice. 2017; 126:164-71. [DOI:10.1016/j.diabres.2017.02.016] [PMID]
- Gupta U, Gupta Y, Jose D, Mani K, Jyotsna VP, Sharma G, et al. Effectiveness of a video-based lifestyle education program compared to usual care in improving HbA1c and other metabolic parameters in individuals with type 2 diabetes: An open-label parallel arm randomized control trial (RCT). Diabetes Therapy. 2020; 11(3):667-79. [DOI:10.1007/s13300-020-00769-2] [PMID] [PMCID]
- Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, et al. 2017 National standards for diabetes self-management education and support. The Diabetes Educator. 2017; 43(5):449-64. [DOI:10.1177/0145721717722968] [PMID]
- Hermanns N, Ehrmann D, Schall S, Maier B, Haak T, Kulzer B. The effect of an education programme (MEDIAS 2 BSC) of non-intensive insulin treatment regimens for people with Type 2 diabetes: A randomized, multi-centre trial. Diabetic Medicine. 2017; 34(8):1084-91. [DOI:10.1111/dme.13346] [PMID]
- Coppola A, Sasso L, Bagnasco A, Giustina A, Gazzaruso C. The role of patient education in the prevention and management of type 2 diabetes: An overview. Endocrine. 2016; 53(1):18-27. [DOI:10.1007/s12020-015-0775-7] [PMID]
- Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, et al. Diabetes self-management education and support in type 2 diabetes. The Diabetes Educator. 2017; 43(1):40-53. [DOI:10.1177/0145721716689694] [PMID]
- Xu ZX, Geng K, Bai Y, Wang XY, Zhu LX. [Evaluation of peer support education mode for type 2 diabetes control in rural residents (Chinese)]. Zhonghua Liu Xing Bing Xue Za Zhi. 2018; 39(12):1560-4. [DOI:10.3760/cma.j.issn.0254-6450.2018.12.005] [PMID]
- Ji H, Chen R, Huang Y, Li W, Shi C, Zhou J. Effect of simulation education and case management on glycemic control in type 2 diabetes. Diabetes/Metabolism Research and Reviews. 2019; 35(3):e3112. [DOI:10.1002/dmrr.3112] [PMID] [PMCID]
- Hashemian M, Ghardashi F, Izadi AR, Akbarzadeh R. Prioritizing the health education needs based on community participation: AHP method. Journal of Education and Health Promotion. 2019; 8(1):127. [DOI:10.4103/jehp.jehp_7_19]
- Chatterjee S, Davies MJ, Heller S, Speight J, Snoek FJ, Khunti K. Diabetes structured self-management education programmes: A narrative review and current innovations. The Lancet. Diabetes & Endocrinology. 2018; 6(2):130-42. [DOI:10.1016/S2213-8587(17)30239-5] [PMID]
Type of Study: Review Article |
Subject:
● Health Education
Received: 2023/01/31 | Accepted: 2023/06/3 | Published: 2023/10/3
Received: 2023/01/31 | Accepted: 2023/06/3 | Published: 2023/10/3
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |