Volume 15, Issue 4 (Jul & Aug 2025)
J Research Health 2025, 15(4): 333-344 |
Back to browse issues page
Ethics code: 0
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sadeghi R, Momenabadi V, Masoodi M R, Zeid Abadinejad M R, Khanjani N. Educational Interventions to Control Hypertension: A Systematic Review. J Research Health 2025; 15 (4) :333-344
URL: http://jrh.gmu.ac.ir/article-1-2596-en.html
URL: http://jrh.gmu.ac.ir/article-1-2596-en.html
Reza Sadeghi1 

 , Victoria Momenabadi2
, Victoria Momenabadi2 

 , Mahmoud Reza Masoodi3
, Mahmoud Reza Masoodi3 

 , Mohammad Reza Zeid Abadinejad4
, Mohammad Reza Zeid Abadinejad4 

 , Narges Khanjani5
, Narges Khanjani5 




 , Victoria Momenabadi2
, Victoria Momenabadi2 

 , Mahmoud Reza Masoodi3
, Mahmoud Reza Masoodi3 

 , Mohammad Reza Zeid Abadinejad4
, Mohammad Reza Zeid Abadinejad4 

 , Narges Khanjani5
, Narges Khanjani5 


1- Department of Public Health, Sirjan School of Medical Sciences, Sirjan, Iran.
2- Department of Public Health, School of Health, Bam University of Medical Sciences, Bam, Iran.
3- Sirjan School of Medical Sciences, Sirjan, Iran.
4- Department of Medical Emergencies, School of Medical Sciences, Sirjan School of Medical Sciences, Sirjan, Iran.
5- Department of Medical Education, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, United States. ,narges.khanjani@gmail.com
2- Department of Public Health, School of Health, Bam University of Medical Sciences, Bam, Iran.
3- Sirjan School of Medical Sciences, Sirjan, Iran.
4- Department of Medical Emergencies, School of Medical Sciences, Sirjan School of Medical Sciences, Sirjan, Iran.
5- Department of Medical Education, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, United States. ,
Full-Text [PDF 815 kb]
(1106 Downloads)
| Abstract (HTML) (3298 Views)
Full-Text: (602 Views)
Introduction
Noncommunicable diseases are among the major causes of death in the world [1]. Today, hypertension (HTN), as one of the most important risk factors for cardiovascular disease, has become a growing health problem that affects people from different ethnicities [2]. Risk factors and predictors of high blood pressure (BP) include overweight, improper nutrition, alcohol consumption, low physical activity and psychological, social, environmental and genetic factors. HTN is a major risk factor for kidney disease, stroke, peripheral vascular disease and congestive heart failure [3]. The prevalence of HTN ranges from 15% to 37% worldwide. India and China have the highest prevalence rate of HTN [4]. In 2015, 13% of all global mortality (7.1 million), 62% of all strokes, and 49% of all myocardial infarctions were attributed to HTN [5].
HTN is a major modifiable risk factor for noncommunicable diseases. Effective treatment for HTN substantially reduces the risk of developing cardiovascular complications [6]. However, despite these benefits, the overall rate of HTN is alarmingly high worldwide, and this condition has caused a high burden of HTN‐related diseases [7]. HTN, although easily diagnosed and common, is often asymptomatic and can lead to death and disability if left unchecked [8].
There are several strategies for controlling HTN, including lifestyle modifications, drug therapy, or combined interventions. Therefore, empowering hypertensive patients by education may be an effective step in controlling HTN or reducing its complications [9]. One of the effective strategies for controlling high BP is educational interventions [10]. Many educational interventions are effective in controlling HTN. The common interventions for preventing HTN include behavioral modifications and lifestyle changes such as promoting a healthy diet, physical activity and avoiding stress and mental pressure [11]. The correct use of health education, health promotion models, and theories in teaching the public can effectively control HTN [12]. Correct education and regular educational programs can improve people’s knowledge and skills and improve their ability to make correct health decisions [13]. Research shows that the most effective educational programs are based on theory-based approaches rooted in behavior change models; therefore, choosing the appropriate health education model is the first step in the planning process of an educational program [14].
Since a major part of HTN control is the responsibility of individuals, informing patients on how to control HTN seems necessary. However, the value of any educational intervention depends on its efficiency in changing health behaviors. Educational effectiveness can be enhanced by using behavioral theories or models [15]. People’s knowledge and perceptions play an important role in controlling HTN. This systematic review summarizes the effectiveness of educational interventions in controlling high BP.
Methods
Search strategies
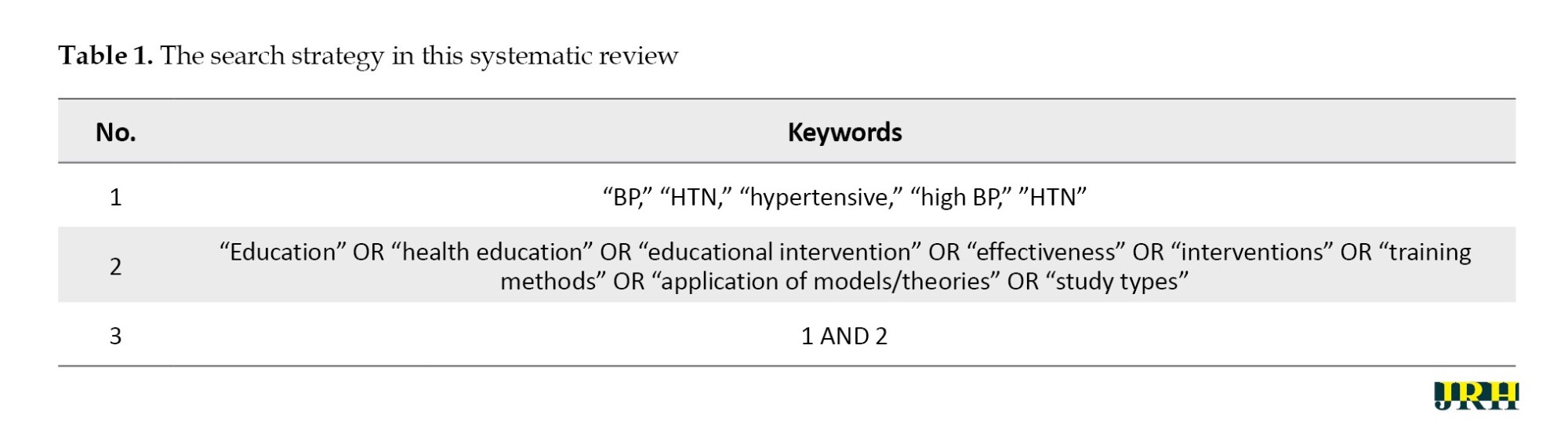
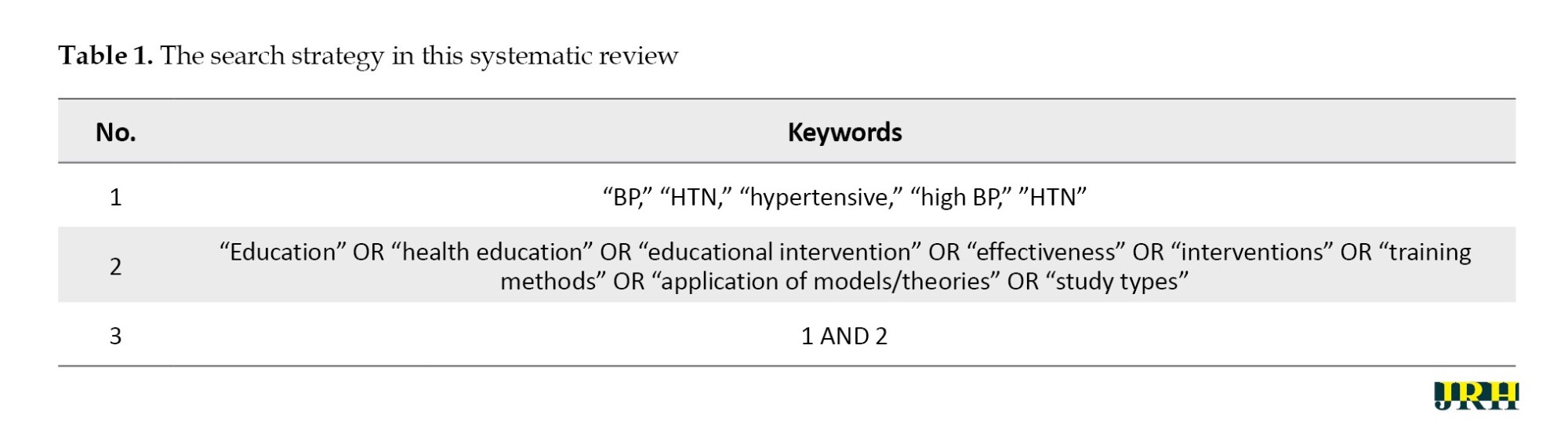
The study search was done between January 15, 2023, and June 20, 2023. Eight databases, including Scopus, Google Scholar, PubMed, Medline, Embase, Web of Science, SID, IranMedex and Magiran, were searched for English or Persian studies about educational interventions to control BP. The keywords used for the search are shown in Table 1. The only filter used while searching was the type of article, as we were looking for interventional studies.
Also, some gray literature, including trial registry resources and conference proceedings, was searched. In addition, we checked the bibliography of the relevant retrieved articles to find more eligible papers.
Inclusion and exclusion criteria
Inclusion criteria included an original educational intervention to control BP in inpatients aged >18 years.
Exclusion criteria included studies with the outcome of HTN and other noncommunicable disease control together, studies that tested interventions that were only adherence to BP medication, studies that included interventions that had been done for other diseases besides BP, review studies, protocols, and ongoing trials, and non-interventional studies.
Quality assessment
The preferred reporting items for systematic reviews and meta-analyses (PRISMA) was used to report standard studies. It is an evidence-based minimum set for reporting in systematic reviews and meta-analyses. The checklist contains 27 items on the content of a systematic review and meta-analysis [16]. Also, the Cochrane risk of bias (ROB) was used to determine the quality of selected studies. The biases evaluated can be seen in Table 2. Judgment of each item was either “unclear,” “high,” or “low” ROB [17].
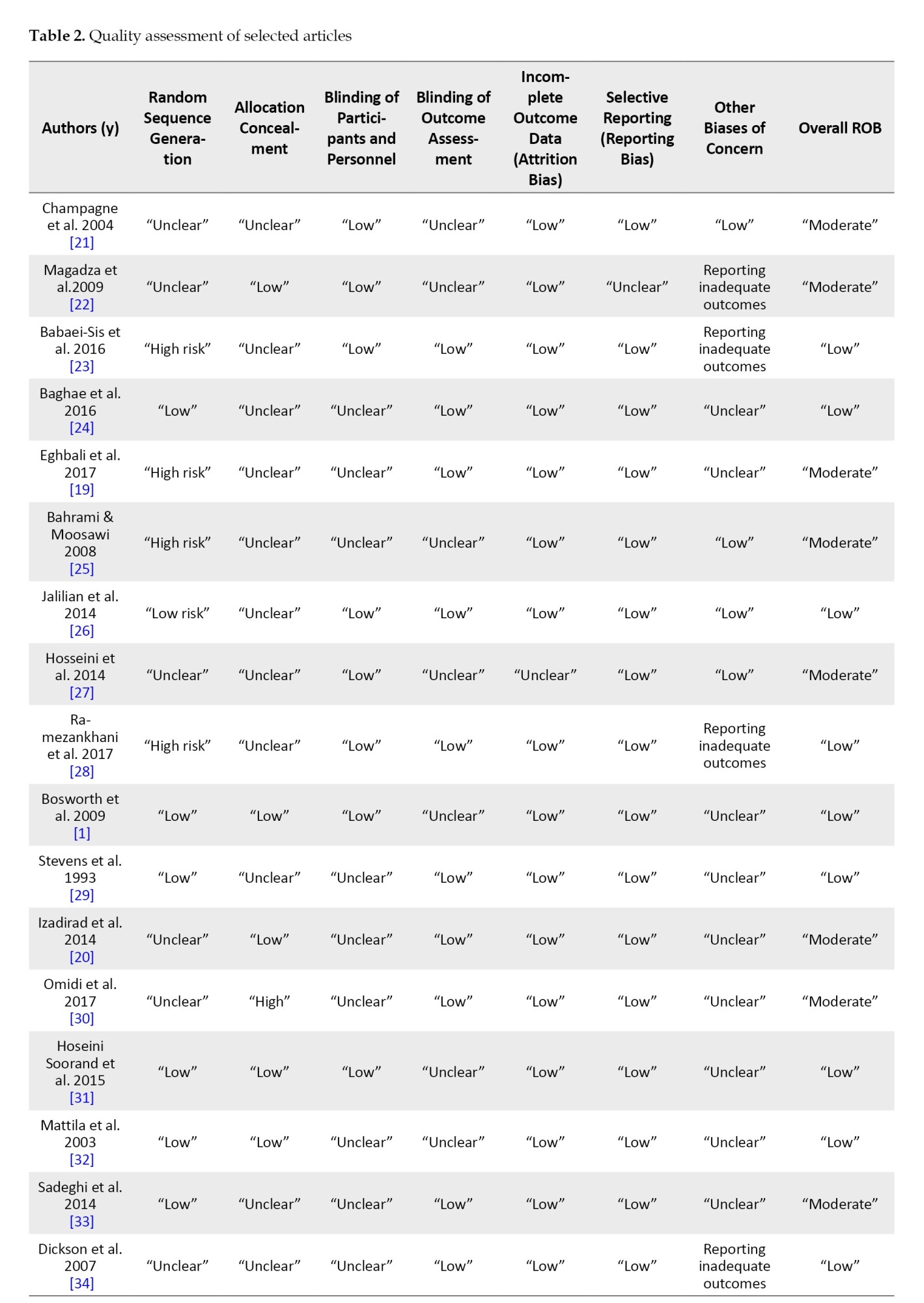

All studies meeting inclusion criteria for the review were assessed independently by two of the authors (Reza Sadeghi and Victoria Momenabadi) for random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data (attrition bias), selective reporting, and other biases of concern. Studies at high ROB in one or more domains were classified as overall high risk, while those with unclear information in any domain were classed as moderate risk. Low-risk studies met low-risk criteria for each domain [18].
Extracting data
Two authors (Reza Sadeghi and Mohammad Reza Zeid Abadinejad) assessed the quality of the studies, screened all abstracts and if necessary, independently screened the full-text articles. Disagreements were resolved by discussion and if no agreement was reached, a third independent person acted as an arbiter. All articles were checked according to the inclusion/exclusion criteria. How to deal with missing or incomplete data was handled by consensus and additional information about the study design was requested from the corresponding author if necessary.
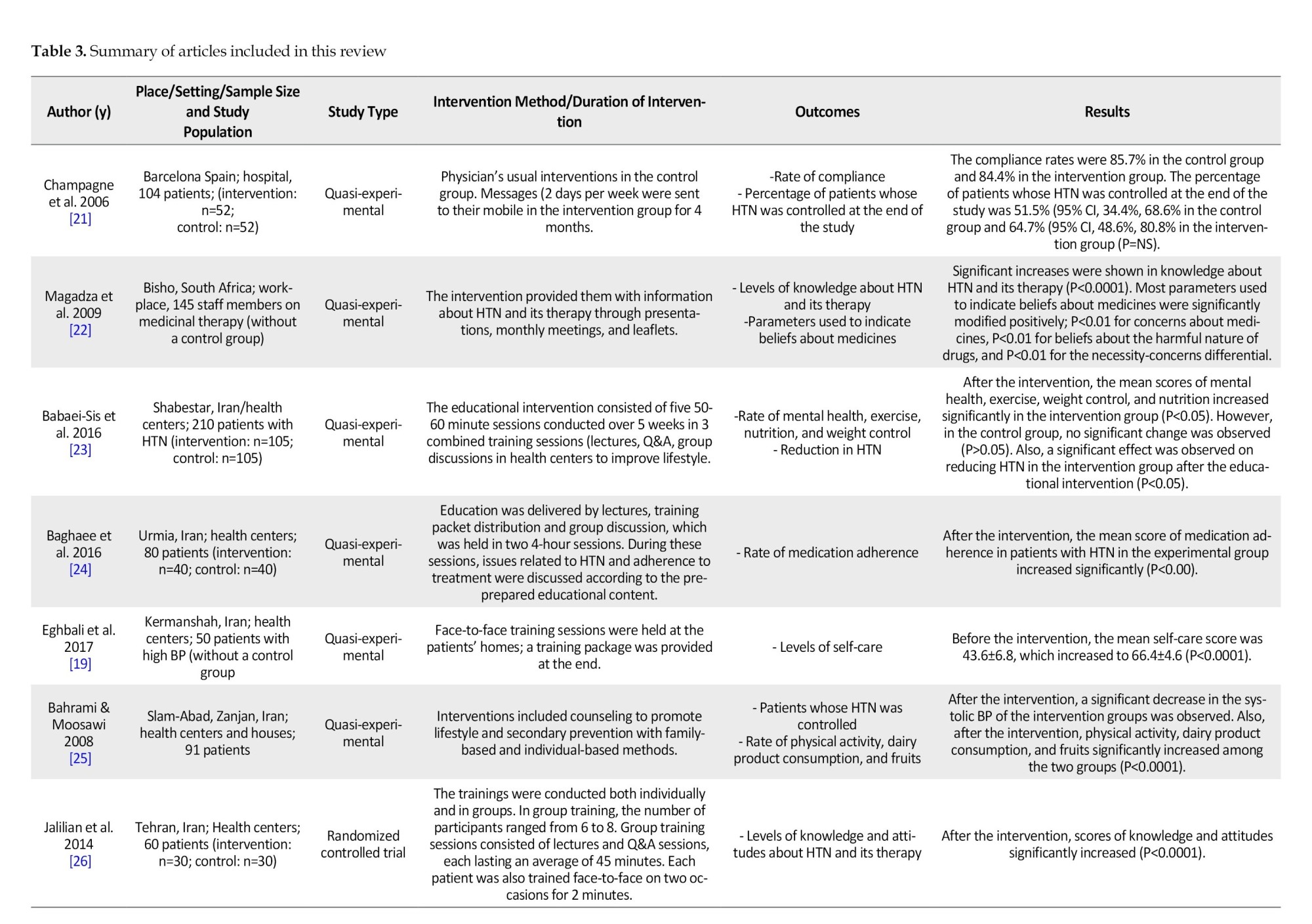
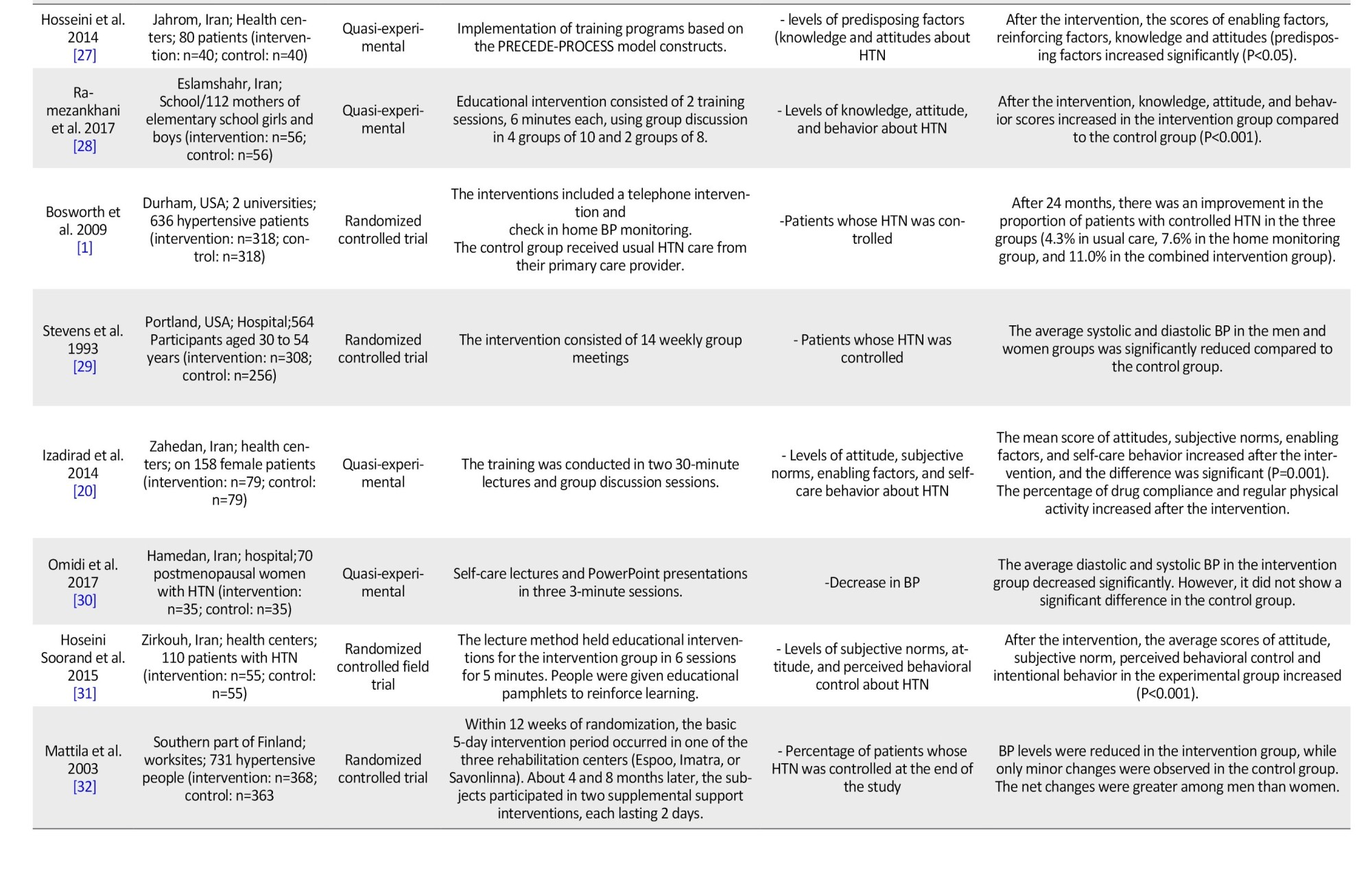
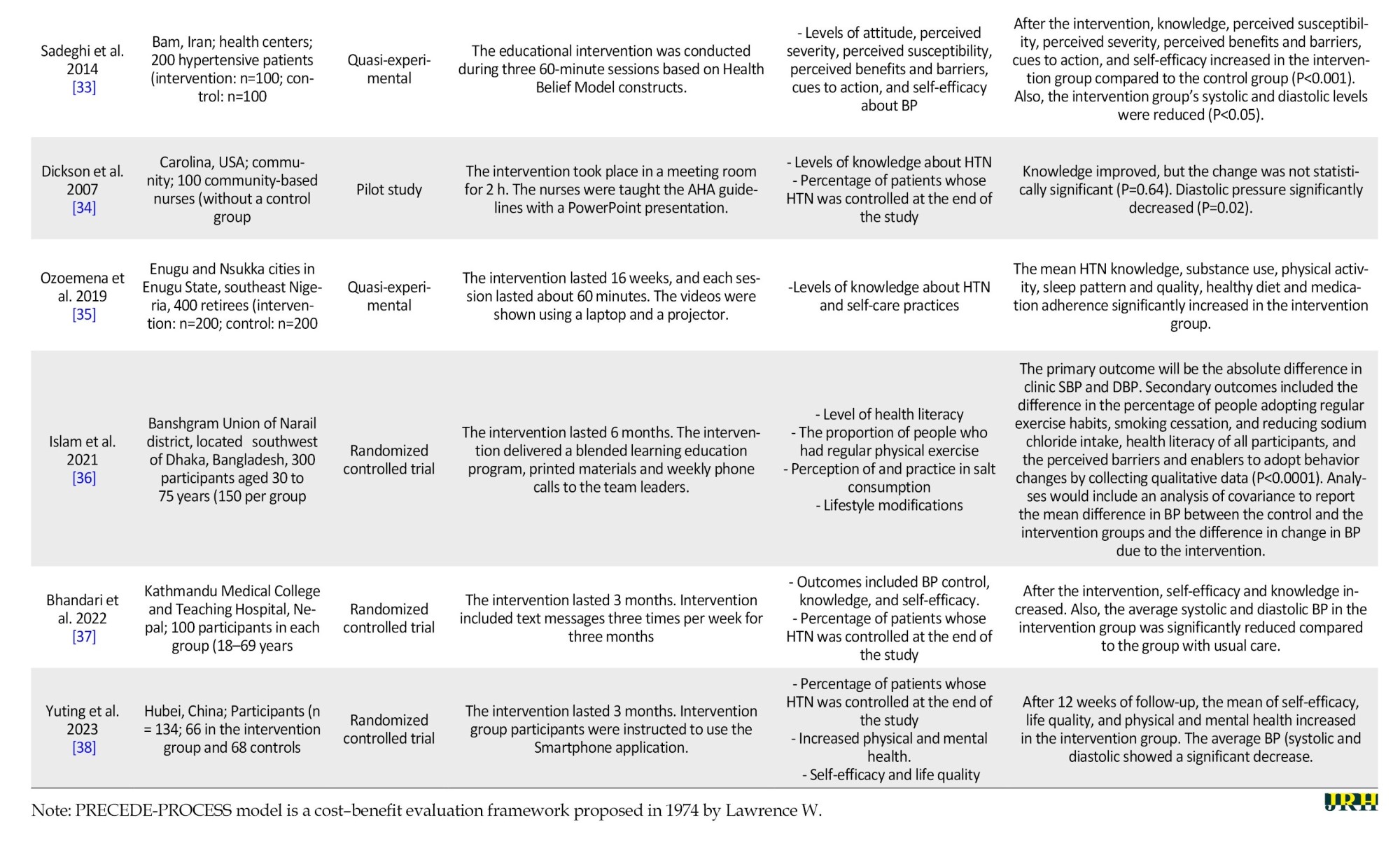
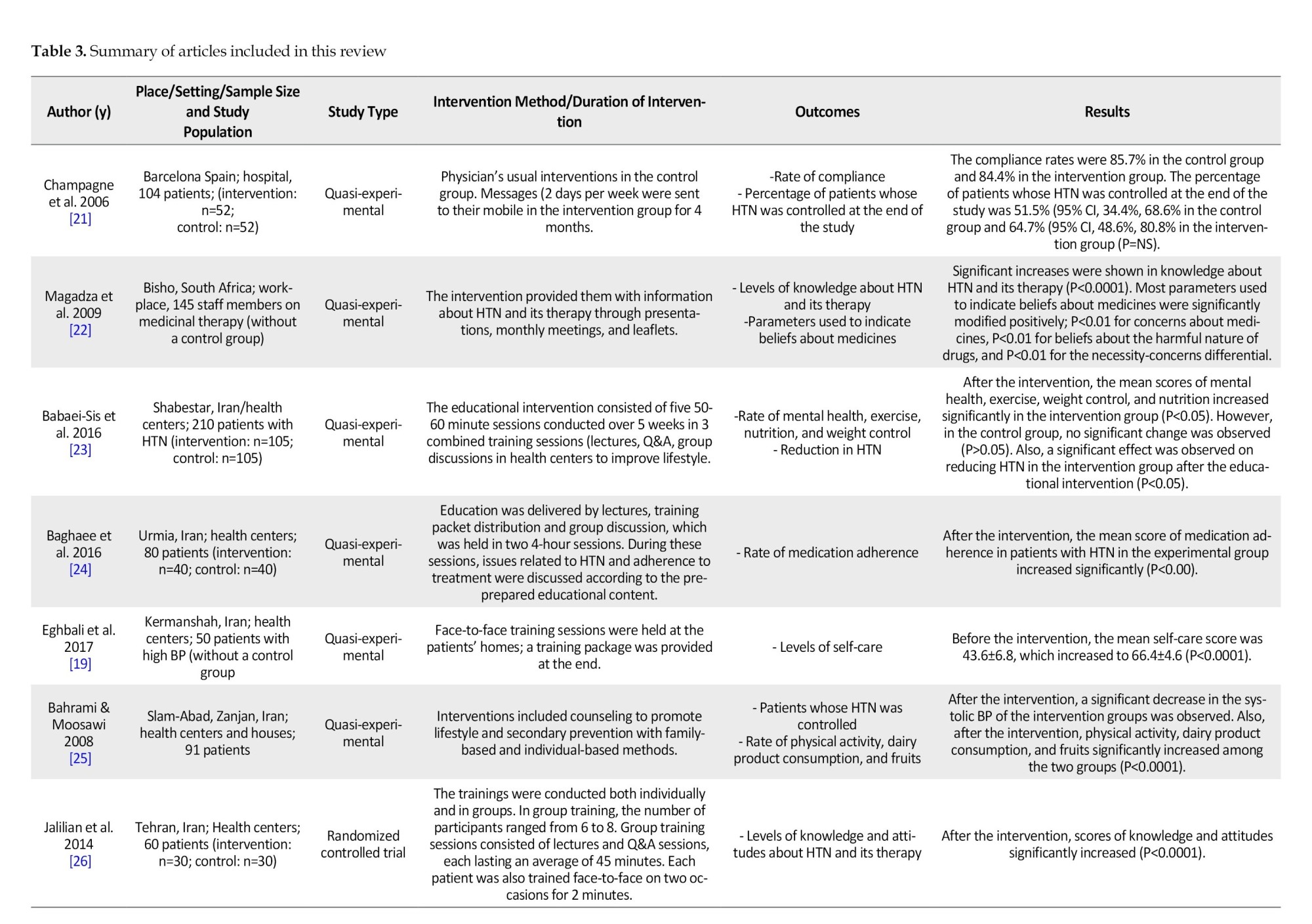
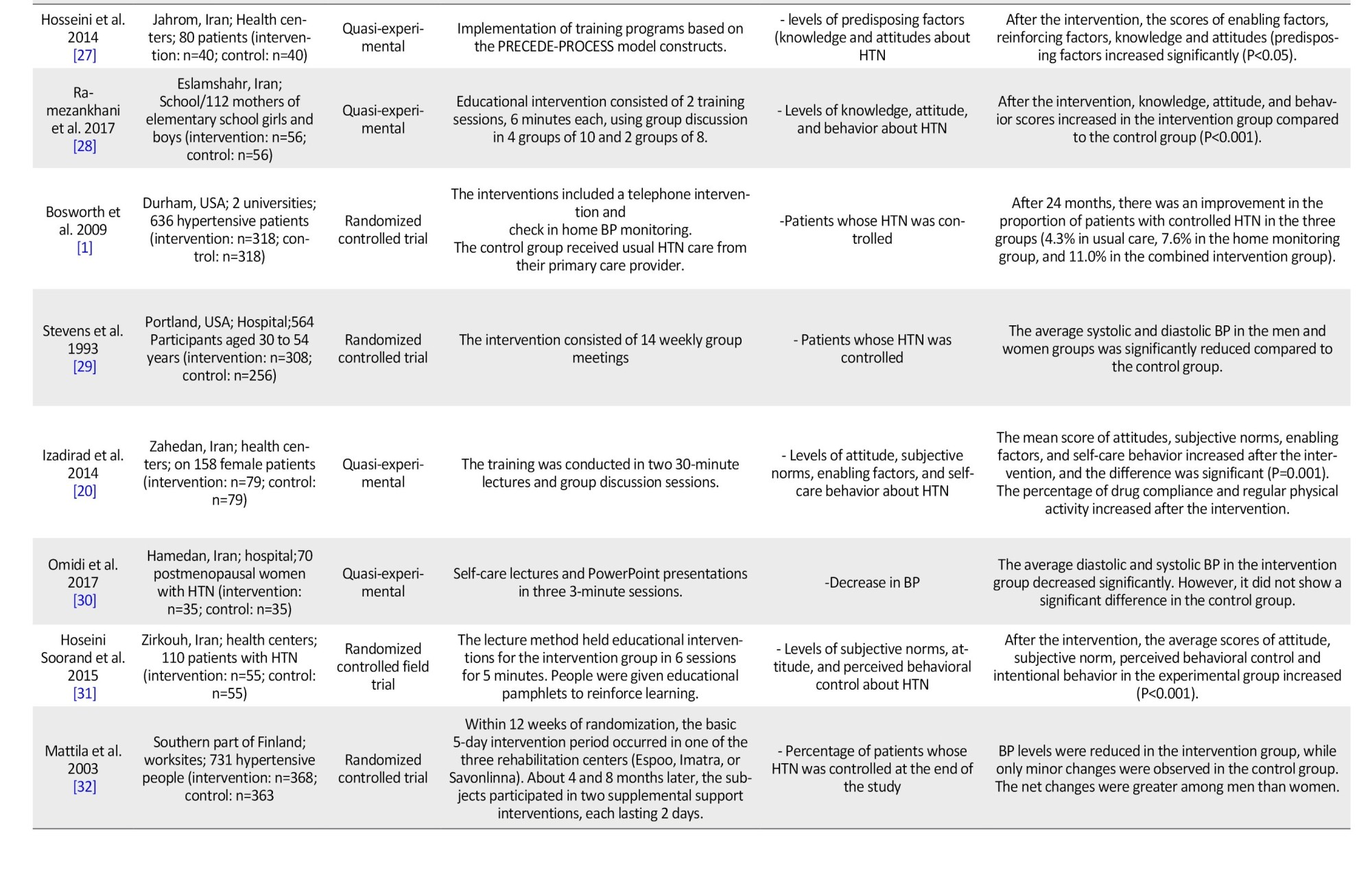
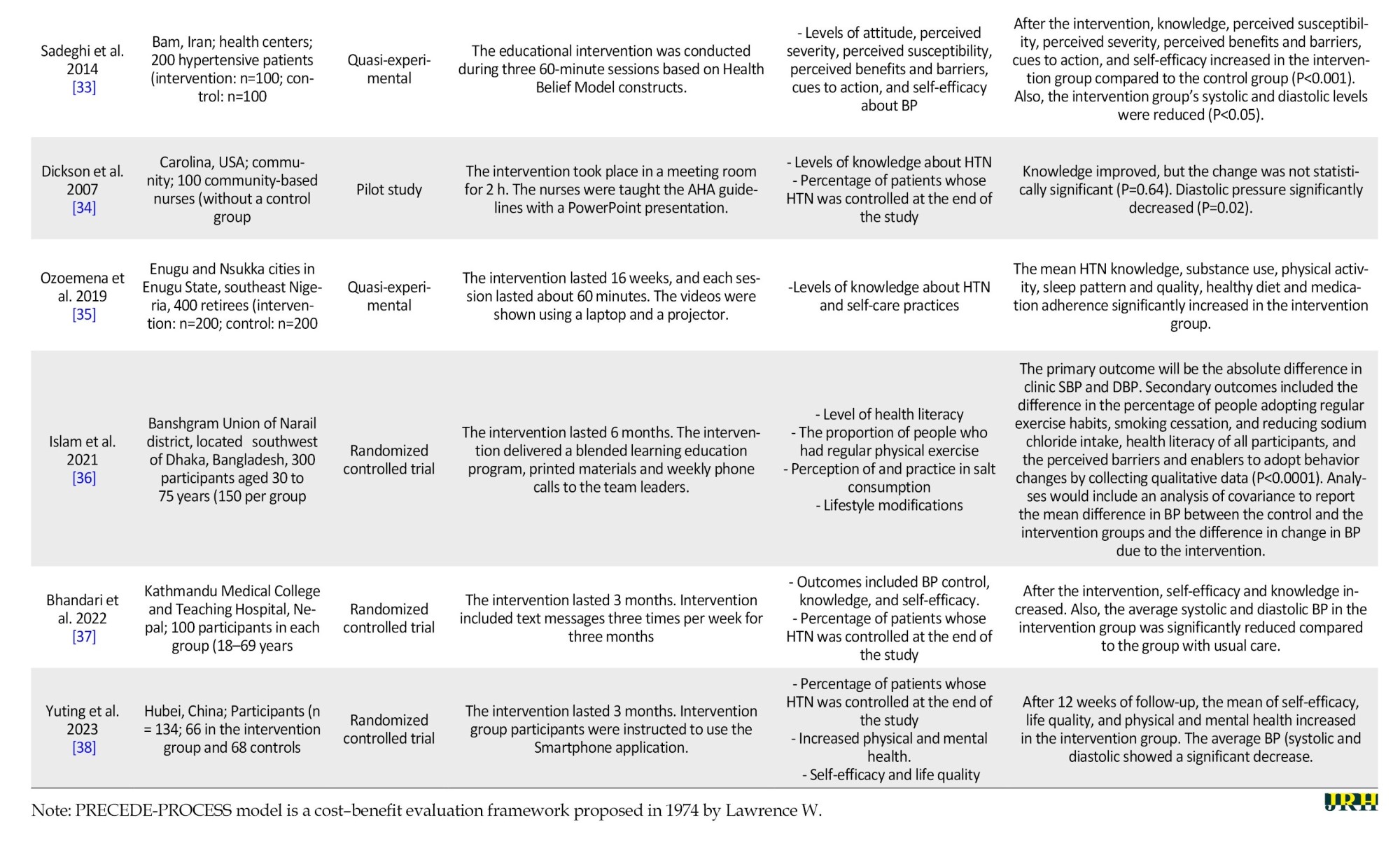
The information extracted was in a standard form. It included the location of the study, the year the study was conducted, the type of study, the population size and target group, characteristics of the intervention, and study results (Table 3).
Results
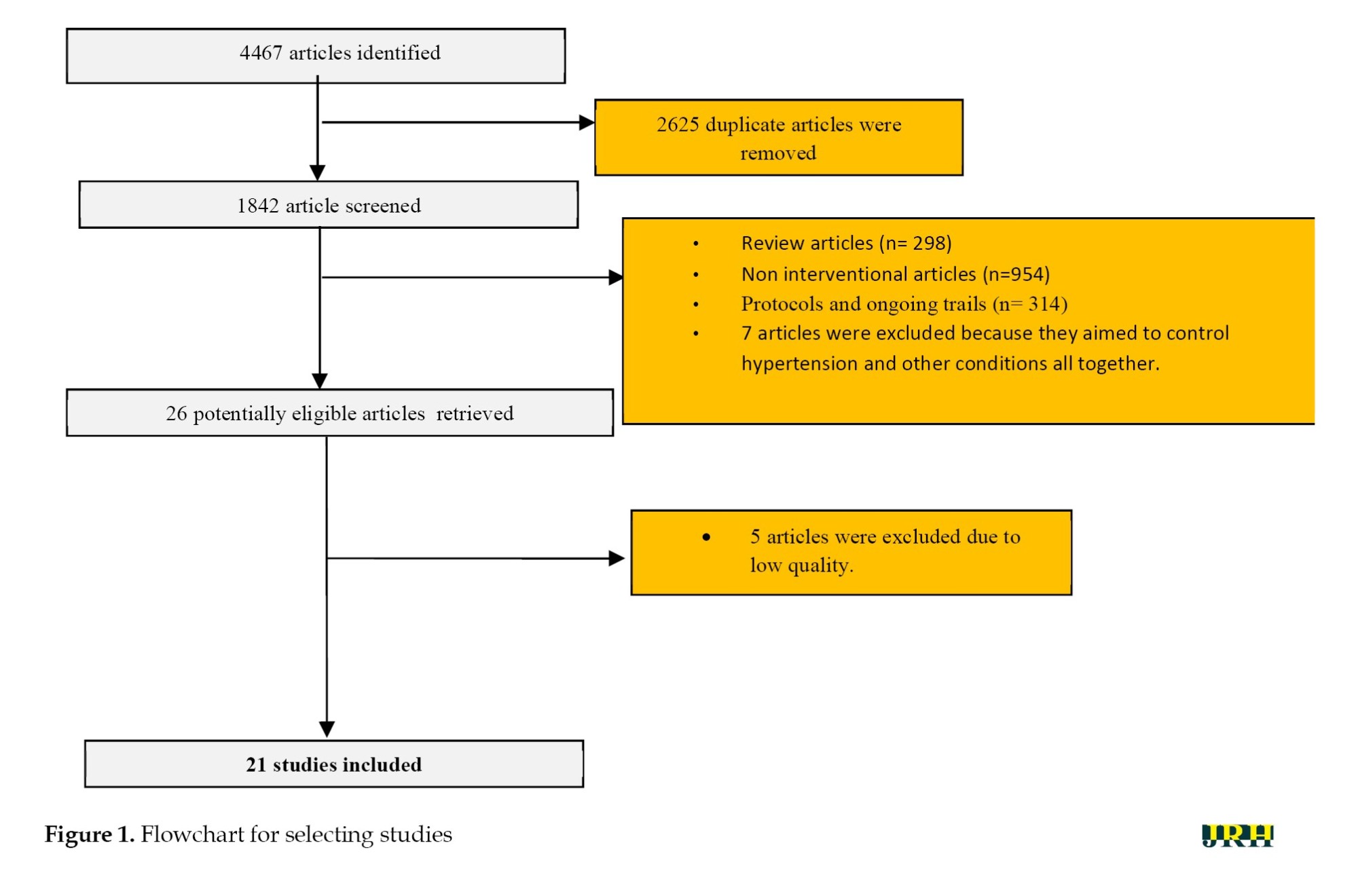
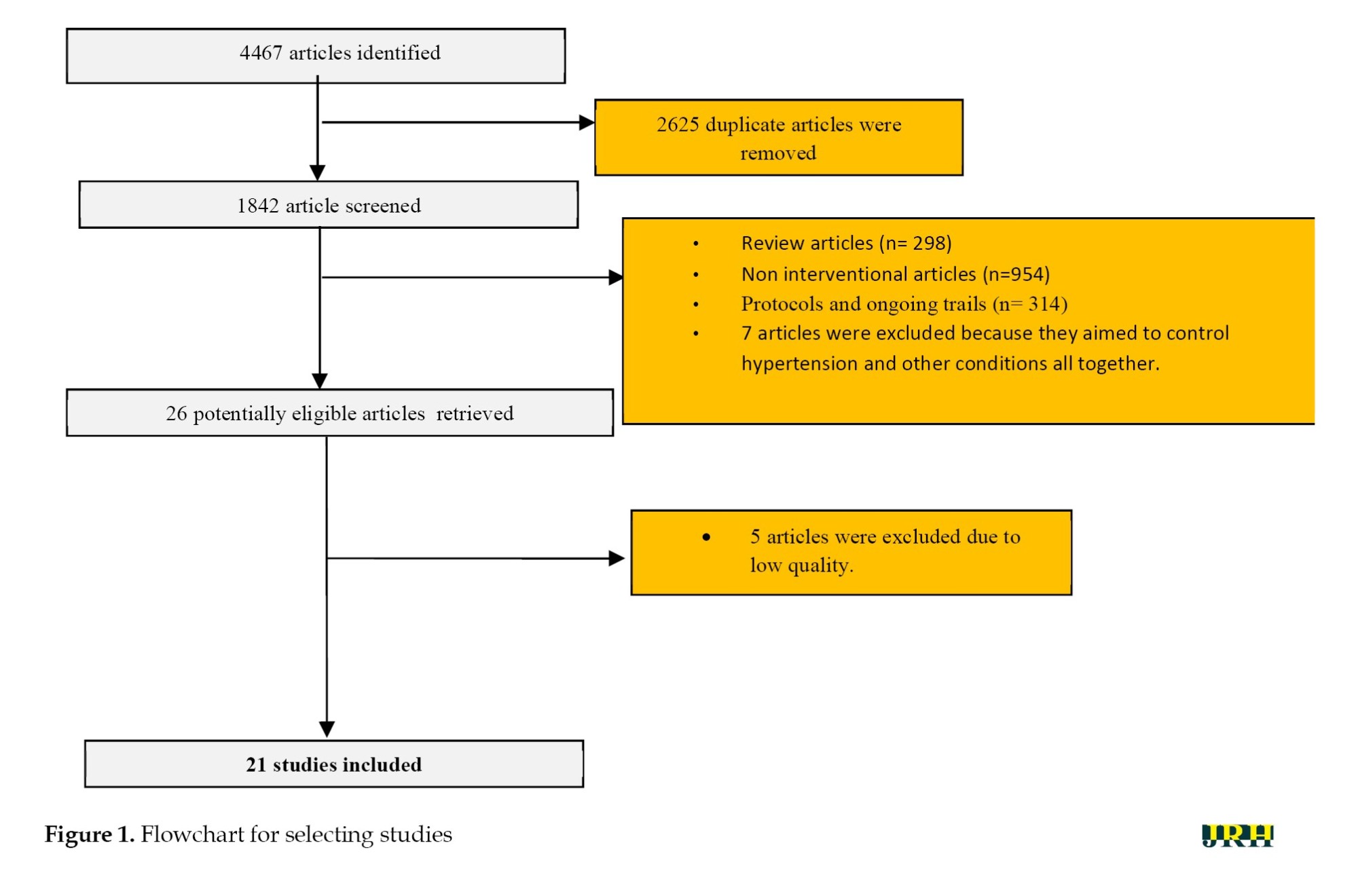
After searching the electronic databases, a total of 4467 related articles were retrieved, of which 1812 were Farsi and 2655 were English. Of these articles, 2625 articles were deleted due to duplication. Further, out of 1842 articles, 1821 were excluded from the study due to being a review, not having a consolidated standards of reporting trials (CONSORT) score, being a protocol, an ongoing trial, a non-interventional study, or being about controlling HTN and other conditions altogether. Five studies were excluded due to low quality. The quality assessment results are shown in Table 2. Finally, 21 studies entered the review (11 Persian and 10 English articles) (Figure 1).
The characteristics of 21 articles can be seen in Table 2. A positive effect of education on controlling HTN was shown in all educational interventions. Still, studies aimed at self-care education [19, 20] seemed more effective, because the difference between the intervention and the control group was higher (Table 3).
The follow-up time for the study participants was between 1 and 6 months. Different educational methods such as lectures, questions and answers (Q&A), group discussions [23, 24], face-to-face training sessions [19], counseling [25], telephone consultation [1] and PowerPoint presentation [34] were used as the intervention. Some studies used interventions that reinforced education, such as pamphlets, brochures, training packages, and text messages [19, 21, 22, 32, 36].
In some studies, no comparison (control) group was used [22, 26, 34, 19]; in some studies without a control group, no special intervention was done [20, 21, 23, 24, 27, 28, 32]. In all studies, the results of the pre- and post-intervention in the control group were not significantly different.
The aim of some studies were educating about lifestyle modification, such as decreasing excessive salt, and saturated [19] or trans fat consumption [36], increasing fruits and vegetables intake [19, 35, 36], decreasing stress [35, 36, 38], increasing physical activity [20, 23, 27, 36, 38], and reduced consumption of tobacco and alcohol [35, 36]. In Mattila’s study, a multidisciplinary lifestyle intervention was conducted in a rehabilitation center [32].
In the included studies, various individual or community-based interventions, including family-centered [25], person-centered [19], texting [31, 37, 38], training in group sessions [20, 22, 24], multiple interventions [23, 24] and community-based interventions [38] were applied. Victor et al. used barbershops as educational sites for African American men [44]. Two studies aimed to improve self-care or the self-management of HTN [19, 20].
The educational models used in the included studies were KAP (knowledge, attitude and practice) [26-28], the PRECEDE-PROCEED model [27], the health belief model [2], the BASNEF model [20, 31] and the theory of planned behavior [31].
Discussion
This systematic review included 21 studies on educational interventions to control HTN, with various individual or community-based interventions. These studies provided relevant information about the effectiveness of the different health education interventions.
Researchers have used various educational models for behavior change. Well-designed health education theories/models can help change behavior and improve health outcomes [31, 45]. The value of an education is determined by its effectiveness in modifying or creating positive health behaviors [46]. However, behavioral science models/theories should be used appropriately to show their maximum impact [44]. The readability and suitability of educational material and choosing the right communication route are the most important and neglected points in increasing the quality and quantity of education [47].
Some studies included in this review aimed to improve self-care or the self-management of HTN. Self-care provides disease prevention, maintains health, and complies with treatments, by the individual [48]. One of the goals of empowering people through education and increasing health literacy is promoting self-care [49]. Therefore, educational interventions should be designed to help people understand the aspects of their disease and perform appropriate self-care. Bosworth’s study showed that HTN self-care monitoring at home and tailored behavioral telephone interventions improved BP after 24 months [1]. Some researchers think a decrease in BP may encourage the patient to modify their lifestyle or continue treatment [9].
The aim of some studies included in this review was lifestyle modification. This objective included changing diet, decreasing stress, increasing physical activity, and consuming tobacco and alcohol. Lifestyle modifications can help normal and hypertensive patients prevent or reduce high BP [50]. The study results of Putri et al. showed that lifestyle factors affecting the incidence of HTN in adolescents are smoking, body mass index, physical inactivity, sleep duration, alcohol use and inappropriate diet [51]. Also, Ribeiro et al. study showed lifestyle modification is widely recommended as the first-line treatment for the management of HTN and includes smoking cessation, modifying the diet, increased physical activity and reduced alcohol consumption [52].
Controlling high BP is a challenge in public health. But HTN is a modifiable risk factor [19] and many educational interventions are effective in preventing and controlling HTN. The difference in effectiveness of the interventions may be due to the different nature of the interventions, complementary education material, follow-up time, individual or community-based, and the specific educational models used.
One of the limitations of this review was that it only searched Persian and English databases. Another limitation was that the included studies had a short follow-up time after the interventions, from 1 to 6 months. It is suggested that future studies conduct longer follow-ups to evaluate the long-term effects of these interventions. Another limitation of this study was that the studies were diverse regarding the model, theory, and method of education and the outcome measured; therefore, a meta-analysis was impossible.
Conclusion
Many educational interventions and training methods are effective in the control of HTN. Educational interventions are a cheap and applicable way to promote self-care behaviors in patients with high BP.
Ethical Considerations
Compliance with ethical guidelines
All information sources used in this study had been published before and were therefore in the public domain, but general ethical principles were applied. The researchers maintained integrity, objectivity, thoroughness in searching and adherence to the highest possible technical standards.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Reza Sadeghi, Victoria Momenabadi, Mohammad Reza Zeid Abadinejad and Narges Khanjani; Data collection, data analysis, data interpretation and drafting the manuscript: Reza Sadeghi and Narges Khanjani; Review and editing: Mahmoud Reza Masoodi, Narges Khanjani, and Reza Sadeghi.
Conflict of interest
The authors declared no conflict of interest.
References
Noncommunicable diseases are among the major causes of death in the world [1]. Today, hypertension (HTN), as one of the most important risk factors for cardiovascular disease, has become a growing health problem that affects people from different ethnicities [2]. Risk factors and predictors of high blood pressure (BP) include overweight, improper nutrition, alcohol consumption, low physical activity and psychological, social, environmental and genetic factors. HTN is a major risk factor for kidney disease, stroke, peripheral vascular disease and congestive heart failure [3]. The prevalence of HTN ranges from 15% to 37% worldwide. India and China have the highest prevalence rate of HTN [4]. In 2015, 13% of all global mortality (7.1 million), 62% of all strokes, and 49% of all myocardial infarctions were attributed to HTN [5].
HTN is a major modifiable risk factor for noncommunicable diseases. Effective treatment for HTN substantially reduces the risk of developing cardiovascular complications [6]. However, despite these benefits, the overall rate of HTN is alarmingly high worldwide, and this condition has caused a high burden of HTN‐related diseases [7]. HTN, although easily diagnosed and common, is often asymptomatic and can lead to death and disability if left unchecked [8].
There are several strategies for controlling HTN, including lifestyle modifications, drug therapy, or combined interventions. Therefore, empowering hypertensive patients by education may be an effective step in controlling HTN or reducing its complications [9]. One of the effective strategies for controlling high BP is educational interventions [10]. Many educational interventions are effective in controlling HTN. The common interventions for preventing HTN include behavioral modifications and lifestyle changes such as promoting a healthy diet, physical activity and avoiding stress and mental pressure [11]. The correct use of health education, health promotion models, and theories in teaching the public can effectively control HTN [12]. Correct education and regular educational programs can improve people’s knowledge and skills and improve their ability to make correct health decisions [13]. Research shows that the most effective educational programs are based on theory-based approaches rooted in behavior change models; therefore, choosing the appropriate health education model is the first step in the planning process of an educational program [14].
Since a major part of HTN control is the responsibility of individuals, informing patients on how to control HTN seems necessary. However, the value of any educational intervention depends on its efficiency in changing health behaviors. Educational effectiveness can be enhanced by using behavioral theories or models [15]. People’s knowledge and perceptions play an important role in controlling HTN. This systematic review summarizes the effectiveness of educational interventions in controlling high BP.
Methods
Search strategies
The study search was done between January 15, 2023, and June 20, 2023. Eight databases, including Scopus, Google Scholar, PubMed, Medline, Embase, Web of Science, SID, IranMedex and Magiran, were searched for English or Persian studies about educational interventions to control BP. The keywords used for the search are shown in Table 1. The only filter used while searching was the type of article, as we were looking for interventional studies.
Also, some gray literature, including trial registry resources and conference proceedings, was searched. In addition, we checked the bibliography of the relevant retrieved articles to find more eligible papers.
Inclusion and exclusion criteria
Inclusion criteria included an original educational intervention to control BP in inpatients aged >18 years.
Exclusion criteria included studies with the outcome of HTN and other noncommunicable disease control together, studies that tested interventions that were only adherence to BP medication, studies that included interventions that had been done for other diseases besides BP, review studies, protocols, and ongoing trials, and non-interventional studies.
Quality assessment
The preferred reporting items for systematic reviews and meta-analyses (PRISMA) was used to report standard studies. It is an evidence-based minimum set for reporting in systematic reviews and meta-analyses. The checklist contains 27 items on the content of a systematic review and meta-analysis [16]. Also, the Cochrane risk of bias (ROB) was used to determine the quality of selected studies. The biases evaluated can be seen in Table 2. Judgment of each item was either “unclear,” “high,” or “low” ROB [17].
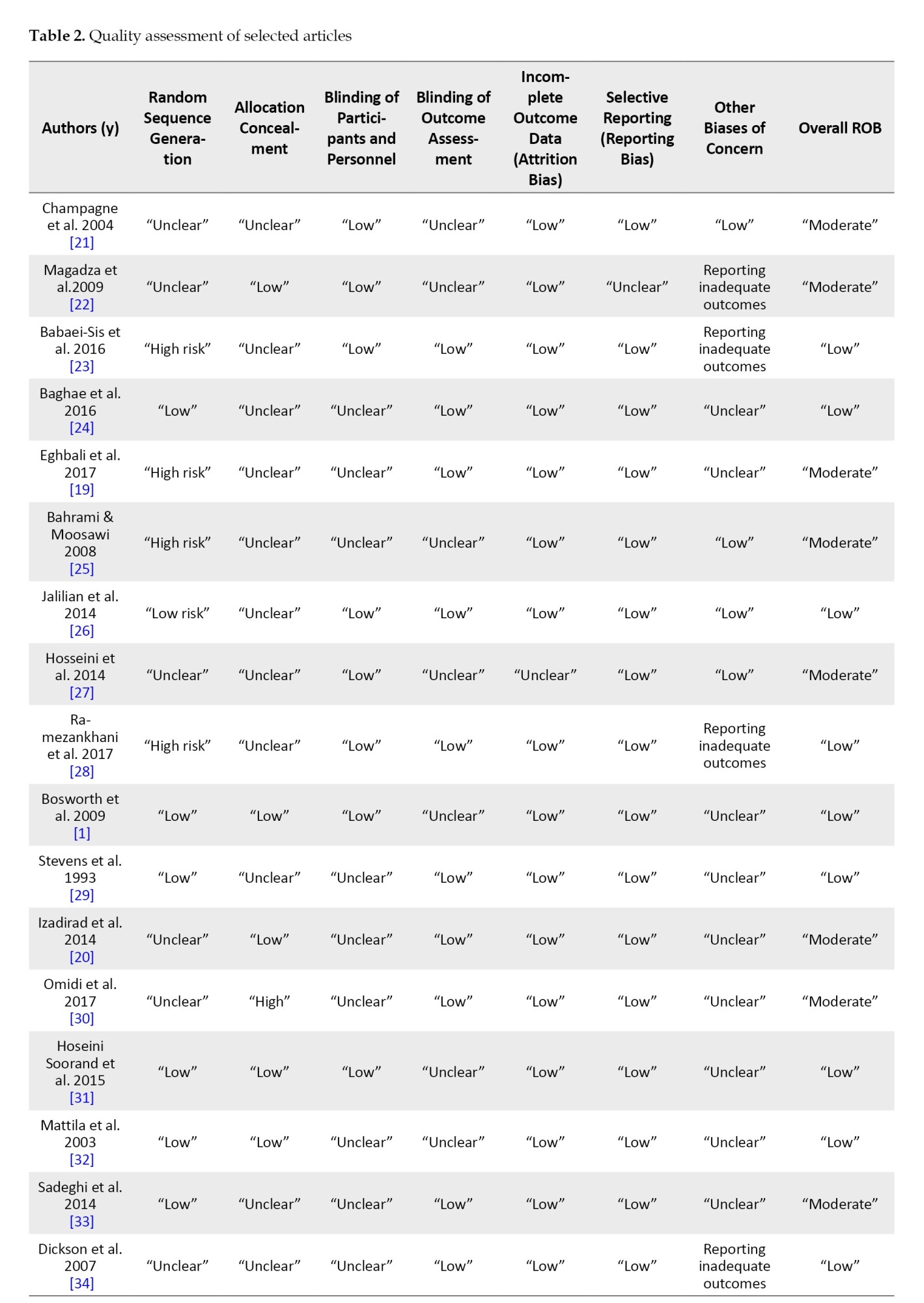

All studies meeting inclusion criteria for the review were assessed independently by two of the authors (Reza Sadeghi and Victoria Momenabadi) for random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data (attrition bias), selective reporting, and other biases of concern. Studies at high ROB in one or more domains were classified as overall high risk, while those with unclear information in any domain were classed as moderate risk. Low-risk studies met low-risk criteria for each domain [18].
Extracting data
Two authors (Reza Sadeghi and Mohammad Reza Zeid Abadinejad) assessed the quality of the studies, screened all abstracts and if necessary, independently screened the full-text articles. Disagreements were resolved by discussion and if no agreement was reached, a third independent person acted as an arbiter. All articles were checked according to the inclusion/exclusion criteria. How to deal with missing or incomplete data was handled by consensus and additional information about the study design was requested from the corresponding author if necessary.
The information extracted was in a standard form. It included the location of the study, the year the study was conducted, the type of study, the population size and target group, characteristics of the intervention, and study results (Table 3).
Results
After searching the electronic databases, a total of 4467 related articles were retrieved, of which 1812 were Farsi and 2655 were English. Of these articles, 2625 articles were deleted due to duplication. Further, out of 1842 articles, 1821 were excluded from the study due to being a review, not having a consolidated standards of reporting trials (CONSORT) score, being a protocol, an ongoing trial, a non-interventional study, or being about controlling HTN and other conditions altogether. Five studies were excluded due to low quality. The quality assessment results are shown in Table 2. Finally, 21 studies entered the review (11 Persian and 10 English articles) (Figure 1).
The characteristics of 21 articles can be seen in Table 2. A positive effect of education on controlling HTN was shown in all educational interventions. Still, studies aimed at self-care education [19, 20] seemed more effective, because the difference between the intervention and the control group was higher (Table 3).
The follow-up time for the study participants was between 1 and 6 months. Different educational methods such as lectures, questions and answers (Q&A), group discussions [23, 24], face-to-face training sessions [19], counseling [25], telephone consultation [1] and PowerPoint presentation [34] were used as the intervention. Some studies used interventions that reinforced education, such as pamphlets, brochures, training packages, and text messages [19, 21, 22, 32, 36].
In some studies, no comparison (control) group was used [22, 26, 34, 19]; in some studies without a control group, no special intervention was done [20, 21, 23, 24, 27, 28, 32]. In all studies, the results of the pre- and post-intervention in the control group were not significantly different.
The aim of some studies were educating about lifestyle modification, such as decreasing excessive salt, and saturated [19] or trans fat consumption [36], increasing fruits and vegetables intake [19, 35, 36], decreasing stress [35, 36, 38], increasing physical activity [20, 23, 27, 36, 38], and reduced consumption of tobacco and alcohol [35, 36]. In Mattila’s study, a multidisciplinary lifestyle intervention was conducted in a rehabilitation center [32].
In the included studies, various individual or community-based interventions, including family-centered [25], person-centered [19], texting [31, 37, 38], training in group sessions [20, 22, 24], multiple interventions [23, 24] and community-based interventions [38] were applied. Victor et al. used barbershops as educational sites for African American men [44]. Two studies aimed to improve self-care or the self-management of HTN [19, 20].
The educational models used in the included studies were KAP (knowledge, attitude and practice) [26-28], the PRECEDE-PROCEED model [27], the health belief model [2], the BASNEF model [20, 31] and the theory of planned behavior [31].
Discussion
This systematic review included 21 studies on educational interventions to control HTN, with various individual or community-based interventions. These studies provided relevant information about the effectiveness of the different health education interventions.
Researchers have used various educational models for behavior change. Well-designed health education theories/models can help change behavior and improve health outcomes [31, 45]. The value of an education is determined by its effectiveness in modifying or creating positive health behaviors [46]. However, behavioral science models/theories should be used appropriately to show their maximum impact [44]. The readability and suitability of educational material and choosing the right communication route are the most important and neglected points in increasing the quality and quantity of education [47].
Some studies included in this review aimed to improve self-care or the self-management of HTN. Self-care provides disease prevention, maintains health, and complies with treatments, by the individual [48]. One of the goals of empowering people through education and increasing health literacy is promoting self-care [49]. Therefore, educational interventions should be designed to help people understand the aspects of their disease and perform appropriate self-care. Bosworth’s study showed that HTN self-care monitoring at home and tailored behavioral telephone interventions improved BP after 24 months [1]. Some researchers think a decrease in BP may encourage the patient to modify their lifestyle or continue treatment [9].
The aim of some studies included in this review was lifestyle modification. This objective included changing diet, decreasing stress, increasing physical activity, and consuming tobacco and alcohol. Lifestyle modifications can help normal and hypertensive patients prevent or reduce high BP [50]. The study results of Putri et al. showed that lifestyle factors affecting the incidence of HTN in adolescents are smoking, body mass index, physical inactivity, sleep duration, alcohol use and inappropriate diet [51]. Also, Ribeiro et al. study showed lifestyle modification is widely recommended as the first-line treatment for the management of HTN and includes smoking cessation, modifying the diet, increased physical activity and reduced alcohol consumption [52].
Controlling high BP is a challenge in public health. But HTN is a modifiable risk factor [19] and many educational interventions are effective in preventing and controlling HTN. The difference in effectiveness of the interventions may be due to the different nature of the interventions, complementary education material, follow-up time, individual or community-based, and the specific educational models used.
One of the limitations of this review was that it only searched Persian and English databases. Another limitation was that the included studies had a short follow-up time after the interventions, from 1 to 6 months. It is suggested that future studies conduct longer follow-ups to evaluate the long-term effects of these interventions. Another limitation of this study was that the studies were diverse regarding the model, theory, and method of education and the outcome measured; therefore, a meta-analysis was impossible.
Conclusion
Many educational interventions and training methods are effective in the control of HTN. Educational interventions are a cheap and applicable way to promote self-care behaviors in patients with high BP.
Ethical Considerations
Compliance with ethical guidelines
All information sources used in this study had been published before and were therefore in the public domain, but general ethical principles were applied. The researchers maintained integrity, objectivity, thoroughness in searching and adherence to the highest possible technical standards.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Reza Sadeghi, Victoria Momenabadi, Mohammad Reza Zeid Abadinejad and Narges Khanjani; Data collection, data analysis, data interpretation and drafting the manuscript: Reza Sadeghi and Narges Khanjani; Review and editing: Mahmoud Reza Masoodi, Narges Khanjani, and Reza Sadeghi.
Conflict of interest
The authors declared no conflict of interest.
References
- Bosworth HB, Olsen MK, Grubber JM, Neary AM, Orr MM, Powers BJ, et al. Two self-management interventions to improve hypertension control: A randomized trial. Annals of Internal Medicine. 2009; 151(10):687-95. [DOI:10.7326/0000605-200911170-00148] [PMID] [PMCID]
- Sadeghi R, Masoudi MR, Patelarou A, Khanjani N. Predictive factors for the care and control of hypertension based on the health belief model among hypertensive patients during the COVID-19 epidemic in Sirjan, Iran. Current Hypertension Reviews. 2022; 18(1):78-84. [DOI:10.2174/1573402117666210603115309] [PMID]
- Daskalopoulou SS, Rabi DM, Zarnke KB, Dasgupta K, Nerenberg K, Cloutier L, et al. The 2015 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. The Canadian Journal of Cardiology. 2015; 31(5):549-68. [DOI:10.1016/j.cjca.2015.02.016] [PMID]
- Mirzaei M, Moayedallaie S, Jabbari L, Mohammadi M. Prevalence of hypertension in Iran 1980-2012: A systematic review. The Journal of Tehran Heart Center. 2016; 11(4):159-67. [PMID]
- Chimeddamba O, Peeters A, Walls HL, Joyce C. Noncommunicable disease prevention and control in Mongolia: A policy analysis. BMC Public Health. 2015; 15:660. [DOI:10.1186/s12889-015-2040-7] [PMID] [PMCID]
- Tocci G, Muiesan ML, Parati G, Agabiti Rosei E, Ferri C, Virdis A, et al. Trends in prevalence, awareness, treatment, and control of blood pressure recorded from 2004 to 2014 during world hypertension day in Italy. Journal of Clinical Hypertension. 2016; 18(6):551-6. [DOI:10.1111/jch.12711] [PMID] [PMCID]
- Sarafidis PA. Epidemiology of resistant hypertension. Journal of Clinical Hypertension. 2011; 13(7):523-8. [DOI:10.1111/j.1751-7176.2011.00445.x] [PMID] [PMCID]
- Osamor PE, Owumi BE. Factors associated with treatment compliance in hypertension in southwest Nigeria. Journal of Health, Population, and Nutrition. 2011; 29(6):619-28. [DOI:10.3329/jhpn.v29i6.9899] [PMID] [PMCID]
- Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the european society of hypertension (ESH) and of the European Society of Cardiology (ESC). European Heart Journal. 2013; 34(28):2159-219. [PMID]
- Schutte AE, Jafar TH, Poulter NR, Damasceno A, Khan NA, Nilsson PM, et al. Addressing global disparities in blood pressure control: Perspectives of the international society of hypertension. Cardiovascular Research. 2023; 119(2):381-409. [DOI:10.1093/cvr/cvac130] [PMID] [PMCID]
- Wamba AA, Takah NF, Johnman C. The impact of interventions for the primary prevention of hypertension in Sub-Saharan Africa: A systematic review and meta-analysis. Plos One. 2019; 14(7):e0219623. [DOI:10.1371/journal.pone.0219623] [PMID] [PMCID]
- Xia T, Zhao F, Nianogo RA. Interventions in hypertension: Systematic review and meta-analysis of natural and quasi-experiments. Clinical Hypertension. 2022; 28(1):13. [DOI:10.1186/s40885-022-00198-2] [PMID] [PMCID]
- Gerayllo S, Ali Morowatisharifabad M, Jouybari L, Karimiankakolaki Z, Sadeghi R. Design and evaluation of a theory-based intervention of knowledge and perceptions to improve self-care amongst relatives of esophageal cancer patients: A randomised controlled trial study protocol. International Journal of Surgery Protocols. 2020; 24:12-16. [DOI:10.1016/j.isjp.2020.09.001] [PMID] [PMCID]
- Glanz K, Rimer BK, Viswanath K. Health behavior: Theory, research, and practice. Hoboken: John Wiley & Sons; 2015.[Link]
- Cappuccio FP, Miller MA. Cardiovascular disease and hypertension in sub-Saharan Africa: Burden, risk and interventions. Internal and Emergency Medicine. 2016; 11(3):299-305. [DOI:10.1007/s11739-016-1423-9] [PMID] [PMCID]
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Journal of Pharmacology & Pharmacotherapeutics. 2010; 1(2):100-7. [DOI:10.4103/0976-500X.72352] [PMID] [PMCID]
- Moore TH, Higgins JP, Dwan K. Ten tips for successful assessment of risk of bias in randomized trials using the RoB 2 tool: Early lessons from Cochrane. Cochrane Evidence Synthesis and Methods. 2023; 1(10):e12031. [DOI:10.1002/cesm.12031]
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928. [DOI:10.1136/bmj.d5928] [PMID] [PMCID]
- Eghbali T, Salehi S. [The effect of nursing intervention education on self-care behaviors in patients with high blood pressure referred to healthcare centers in Kermanshah province (Persian)]. Iranian Journal of Rehabilitation Research. 2017; 4(1):32-7. [DOI:10.21859/ijrn-04015]
- Izadirad H, Masoudi GR, Zareban I. [Evaluation of efficacy of education program based on BASNEF model on Self-care behaviors of women with hypertension (Persian)]. Journal of Torbat Heydariyeh University of Medical Sciences. 2014; 1(2):22-31.[Link]
- Champagne CM. Dietary interventions on blood pressure: the Dietary Approaches to Stop Hypertension (DASH) trials. Nutrition Reviews. 2006; 64(2 Pt 2):S53-6. [DOI:10.1111/j.1753-4887.2006.tb00234.x] [PMID]
- Magadza C, Radloff SE, Srinivas SC. The effect of an educational intervention on patients' knowledge about hypertension, beliefs about medicines, and adherence. Research in Social & Administrative Pharmacy. 2009; 5(4):363-75. [DOI:10.1016/j.sapharm.2009.01.004] [PMID]
- Babaei-Sis M, Ranjbaran S, Mahmoodi H, Babazadeh T, Moradi F, Mirzaeian K. [The effect of educational intervention of life style modification on blood pressure control in patients with hypertension (Persian)]. Journal of Education and Community Health. 2016; 3(1):12-9. [DOI:10.21859/jech-03012]
- Baghaee R, Khaledian N, Didarloo A, Alinezhad V. [The effect of an educational intervention on the medication adherence in patients with hypertension: Based on BASNEF model (Persian)]. Nursing And Midwifery Journal. 2016; 14(9):811-21. [Link]
- Bahrami N, Moosawi N. [Comparing the effect of two family-and individual-based interventions on blood pressure and lifestyle (Persian)]. Journal of Inflammatory Diseases. 2008; 12(1):62-79. [Link]
- Jalilian N, Tavafian S, Aghamolaei T, Ahmadi S. [Educational intervention on the knowledge and attitudes of people with hypertension: A clinical trial (Persian)]. Quarterly Journal of Health Education and Health Promotion. 2014; 1(4):37-44. [Link]
- Hosseini F, Farshidi H, Aghamolaei T, Madani A, Ghanbarnejad A. [The impact of an educational intervention based on PRECEDE-PROCEED model on lifestyle changes among hypertension patients (Persian)]. Iranian Journal of Health Education and Health Promotion. 2014; 2(1):17-27. [Link]
- Ramezankhani A, Pooresmaeili A, Rakhshandehrou S, Khodakarim S. [The effect of group discussion method educational on knowledge, attitude and preventive behaviors of high blood pressure in women 20-49 years old Islamshahr City (Persian)]. Razi Journal of Medical Sciences. 2017; 24(155):11-9. [Link]
- Stevens VJ, Corrigan SA, Obarzanek E, Bernauer E, Cook NR, Hebert P, et al. Weight loss intervention in phase 1 of the trials of hypertension prevention. The TOHP collaborative research group. Archives of Internal Medicine. 1993; 153(7):849-58. [DOI:10.1001/archinte.1993.00410070039006] [PMID]
- Omidi A, Khodaveisi M, Mirzaei Z, Rezvani M, Moghimbeighi A. The effect of education self-care behaviors on the hypertension in postmenopausal women. Avicenna Journal of Nursing and Midwifery Care. 2017; 25(4):121-30. [DOI:10.30699/sjhnmf.25.4.121]
- Hoseini Soorand A, Miri MR, Sharifzadeh G. [Effect of curriculum based on theory of planned behavior, on components of theory in patients with hypertension (Persian)]. Journals of Birjand University of Medical Sciences. 2015; 22(3):199-208. [Link]
- Mattila R, Malmivaara A, Kastarinen M, Kivelä SL, Nissinen A. Effectiveness of multidisciplinary lifestyle intervention for hypertension: A randomised controlled trial. Journal of Human Hypertension. 2003; 17(3):199-205. [DOI:10.1038/sj.jhh.1001531] [PMID]
- Sadeghi R, Mohseni M, Khanjani N. [The effect of an educational intervention according to hygienic belief model in improving care and controlling among patients with hypertension (Persian)]. Journal of Rafsanjan University of Medical Sciences. 2014; 13(4):383-94. [Link]
- Dickson BK, Hajjar I. Blood pressure measurement education and evaluation program improves measurement accuracy in community-based nurses: A pilot study. Journal of the American Academy of Nurse Practitioners. 2007; 19(2):93-102. [DOI:10.1111/j.1745-7599.2006.00199.x] [PMID]
- Ozoemena EL, Iweama CN, Agbaje OS, Umoke PCI, Ene OC, Ofili PC, et al. Effects of a health education intervention on hypertension-related knowledge, prevention and self-care practices in Nigerian retirees: A quasi-experimental study. Archives of Public Health. 2019; 77:23. [DOI:10.1186/s13690-019-0349-x] [PMID] [PMCID]
- Islam FMA, Lambert EA, Islam SMS, Islam MA, Biswas D, McDonald R, et al. Lowering blood pressure by changing lifestyle through a motivational education program: A cluster randomized controlled trial study protocol. Trials. 2021; 22(1):438. [DOI:10.1186/s13063-021-05379-2] [PMID] [PMCID]
- Bhandari B, Narasimhan P, Jayasuriya R, Vaidya A, Schutte AE. Effectiveness and acceptability of a mobile phone text messaging intervention to improve blood pressure control (TEXT4BP) among patients with hypertension in Nepal: A Feasibility Randomised Controlled Trial. Global Heart. 2022; 17(1):13. [DOI:10.5334/gh.1103] [PMID] [PMCID]
- Yuting Z, Xiaodong T, Qun W. Effectiveness of a mHealth intervention on hypertension control in a low-resource rural setting: A randomized clinical trial. Frontiers in Public Health. 2023; 11:1049396. [DOI:10.3389/fpubh.2023.1049396] [PMID] [PMCID]
- Mills KT, Rubinstein A, Irazola V, Chen J, Beratarrechea A, Poggio R, et al. Comprehensive approach for hypertension control in low-income populations: Rationale and study design for the hypertension control program in Argentina. The American Journal of the Medical Sciences. 2014; 348(2):139-45. [DOI:10.1097/MAJ.0000000000000298] [PMID] [PMCID]
- Katende G, Groves S, Becker K. Hypertension education intervention with ugandan nurses working in hospital outpatient clinic: A pilot study. Nursing Research and Practice. 2014; 2014:710702. [DOI:10.1155/2014/710702] [PMID] [PMCID]
- da Silva SS, Colósimo FC, Pierin AM. [The effect of educational interventions on nursing team knowledge about arterial hypertension (Portuguese)]. Revista da Escola de Enfermagem da U S P. 2010; 44(2):488-96. [DOI:10.1590/S0080-62342010000200035] [PMID]
- Khosravi AR, Rowzati M, Gharipour M, Fesharaki MG, Shirani S, Shahrokhi S, et al. Hypertension control in industrial employees: Findings from SHIMSCO study. ARYA Atherosclerosis. 2012; 7(4):191-6. [PMID]
- Morisky DE, Levine DM, Green LW, Smith CR. Health education program effects on the management of hypertension in the elderly. Archives of Internal Medicine. 1982; 142(10):1835-8. [DOI:10.1001/archinte.1982.00340230077014] [PMID]
- Victor RG, Ravenell JE, Freeman A, Bhat DG, Storm JS, Shafiq M, et al. A barber-based intervention for hypertension in African American men: Design of a group randomized trial. American Heart Journal. 2009; 157(1):30-6. [DOI:10.1016/j.ahj.2008.08.018] [PMID] [PMCID]
- Hashemi M, Sadeghi R, Shamsi M. [An investigation of educational intervention impact on pregnant women for promote preventive behaviors of influenza H1N1: Using health belief model (Persian)]. Koomesh. 2017; 19(3):603-10. [Link]
- Sadeghi R, Mahmoodabad SSM, Fallahzadeh H, Rezaeian M, Bidaki R, Khanjani N. Readability and suitability assessment of adolescent education material in preventing hookah smoking. International Journal of High Risk Behaviors and Addiction. 2019; 8(1):e83117. [DOI:10.5812/ijhrba.83117]
- Sadeghi R, Masoudi MR, Khanjani N. A systematic review about educational campaigns on smoking cessation. The Open Public Health Journal. 2020; 13(1):748-55. [DOI:10.2174/1874944502013010748]
- Jones MC, MacGillivray S, Kroll T, Zohoor AR, Connaghan J. A thematic analysis of the conceptualisation of self-care, self-management and self-management support in the long-term conditions management literature. Journal of Nursing and Healthcare of Chronic Illness. 2011; 3(3):174-85.[DOI:10.1111/j.1752-9824.2011.01096.x]
- Sadeghi R, Khanjani N, Naghibzadeh-Tahami A, Kakolaki ZK. Education of Iranian pregnant women about prevention of influenza A. International Journal of Women's Health and Reproduction Sciences. 2018; 6(3):321-7. [DOI:10.15296/ijwhr.2018.53]
- Okwuonu C, Emmanuel C, Ojimadu N. Perception and practice of lifestyle modification in the management of hypertension among hypertensives in southeast Nigeria. International Journal of Medicine and Biomedical Research. 2014; 3(2):121-31. [DOI:10.14194/ijmbr.3.2.8]
- Putri FK, Tarigan RA, Roza N, Handayani TY. The impact of lifestyle on hypertension in adolescents: Literature review. Nusantara Science and Technology Proceedings. 2024; 2024:109-17. [DOI:10.11594/nstp.2024.4320]
- Ribeiro F, Teixeira M, Alves AJ, Sherwood A, Blumenthal JA. Lifestyle medicine as a treatment for resistant hypertension. Current Hypertension Reports. 2023; 25(10):313-28. [DOI:10.1007/s11906-023-01253-5] [PMID]
Type of Study: Review Article |
Subject:
● Health Education
Received: 2024/08/1 | Accepted: 2024/11/30 | Published: 2025/07/1
Received: 2024/08/1 | Accepted: 2024/11/30 | Published: 2025/07/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






